Abstract
Burnout syndrome is a common occurrence among oncologists. Doctors enrolled in residency programs in clinical oncology are exposed to similar risk factors; however, few data are available in this population. This study assessed the occurrence of burnout and associated factors among first-year residents at Brazilian institutions. The present prospective, multicenter, cohort study was conducted with doctors enrolled in residency programs in clinical oncology at Brazilian institutions affiliated with the public health system. The participants answered a sociodemographic questionnaire, the Maslach Burnout Inventory (MBI), Lipp’s Stress Inventory, and the Beck Depression Inventory (BDI), upon admission to the program and 6 and 12 months later. Of 37 eligible residency programs in 2009, 11 (30.6 %) agreed to participate in the study. Fifty-four residents, representing 100 % of new admissions to the participating institutions, were included. Most of the participants met the criteria for severe burnout upon admission to the residency programs (emotional exhaustion in 49.0 % and depersonalization in 64.7 %). The scores on MBI domains emotional exhaustion and depersonalization increased significantly (p < 0.01) during the first year of residency, and the prevalence of burnout increased to 88 % at the end of that first year. The present study found a high prevalence of burnout among doctors enrolled in residency programs in clinical oncology at Brazilian institutions. A large fraction of the participants met the criteria for burnout syndrome upon admission to the program, which suggests that the problem began during the course of the previous residency program in internal medicine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burnout syndrome results from stress in professional life and is characterized by emotional exhaustion, depersonalization (interacting with patients and people in general as if they were objects), and feelings of poor personal accomplishment [1]. The term “burnout syndrome” was proposed in 1974 by the psychologist H.J. Freudenberger and has been used in a wide variety of medical fields for many decades [2–4].
Individuals who interact extensively with the public and/or manage patients with severe and chronic diseases are at particular risk of developing burnout syndrome [3, 5]. Oncology is one of the medical fields in which the severity of the patients’ disease, use of toxic and prolonged treatments, and close contact with terminal patients and their relatives can subject health care professionals to considerable stress. It is thus not by chance that studies demonstrate that burnout syndrome is frequent among oncologists, with a stable index of approximately 50 % in the past decades [6–9]. This high prevalence of burnout syndrome in the oncology setting impairs not only the quality of professional and personal life of the health care professionals involved but also the quality of care delivered to patients and their relatives.
The occurrence of burnout syndrome is also frequent in medical residency programs, with a prevalence above 40 %, and is associated with negative effects on the residents and the quality of the medical care they provide [10–15]. Although participants in clinical oncology residency programs are exposed to work conditions similar to those of trained oncologists, the prevalence of burnout syndrome and its risk factors in this population of medical residents are poorly known. Some data indicate that the prevalence of burnout syndrome may be higher during the first year of residency [10, 11].
In the present study, we followed a cohort of doctors newly admitted to clinical oncology residency programs at Brazilian institutions to identify the incidence of burnout syndrome and its associated risk factors. The secondary objective was to assess the prevalence of depression and stress among these individuals.
Materials and Methods
A cohort of oncology residents was selected from Brazilian institutions affiliated with the public health system.
The coordinators of all the clinical oncology residency programs available in Brazil in 2009 were sent invitations (by e-mail) to participate in the study. Only services at public or philanthropic hospitals were selected.
The coordinators who agreed to participate received approval from the corresponding institutional research ethics committees in 2009.
During the following two years (2010 and 2011), doctors newly admitted to the participating residency programs were invited to read an informed consent form. Participation in the study was optional, and the participants were assured regarding the confidentiality of the information, as it was not made available to the program coordinators at any time, even after the end of the study.
Residents who had entered the program more than 1 month earlier were excluded from the study. Residents enrolled in programs other than internal medicine (a mandatory requirement for admission to clinical oncology programs according to the Brazilian legislation in effect) were also excluded.
After they signed an informed consent form, the volunteers were requested to answer the following four questionnaires:
-
1.
Sociodemographic questionnaire: consisted of questions to investigate epidemiological data, health habits, fields of interest and satisfaction, and characteristics of the work routine.
-
2.
Maslach Burnout Inventory (MBI) [1]: standardized questionnaire consisting of 22 assertions regarding feelings and attitudes relative to the three main characteristics of burnout syndrome. The following cutoff points were used in the present study: emotional exhaustion (low level, ≤18; intermediate level, 19–26; high level, ≥27); depersonalization (low level, ≤ 5; intermediate level, 6–9; high level, ≥10); and perceived personal accomplishment (low level, ≥40; intermediate level 39–34; high level ≤33). Burnout syndrome is considered present when high levels of emotional exhaustion and/or depersonalization are attained [16, 17].
-
3.
Beck Depression Inventory (BDI) [18]: standardized questionnaire to assess depressive symptoms. It comprises 21 sets of assertions that reflect the state of mind of respondents during the previous week.
-
4.
Lipp’s Inventory of Stress Symptoms in Adults (nventário de Sintomas de Stress de Lipp (ISSL)) [19]: standardized questionnaire to assess stress. It is based on a four-phase model of stress, represented by alertness, resistance, near exhaustion, and exhaustion. Interpretation of the responses allows identifying the presence or absence of stress and the stress phase in the respondent as well as establishing whether the symptoms are predominantly physical or psychological.
The questionnaires were applied at the beginning (T1), 6 months later (T2), and at the end of the first year of residency (T3), for a total of three evaluations.
The questionnaires were to be answered anonymously and individually without any interference by other people. The completed questionnaires were placed in envelopes and sealed by the respondents. Data compilation was performed by a single professional exclusively hired for this purpose who was not involved in the study. The envelopes were opened only after the data corresponding to the last volunteer were collected.
Statistical Analysis
The qualitative variables were expressed as absolute and relative frequencies, and the quantitative variables were expressed as measures of central tendency and dispersion.
The chi-squared test was used to analyze the factors associated with stress upon admission to the residency programs. To investigate factors associated with depression (BDI) and burnout syndrome (domains of emotional exhaustion, depersonalization, and low perceived personal accomplishment), we used the unpaired t test or the Mann-Whitney test when the assumption of normality of data distribution or of homogeneity of variance was not met.
To reduce the odds of type I errors from using multiple statistical tests, we restricted the number of possible risk factors for burnout, depression, and stress upon admission to the residency programs to 10. These factors were selected based on data reported by studies on residency programs in other medical specialties [20, 21].
The scores on MBI (burnout) and BDI (depression) upon admission to the residency program (T1) and at the end of the first year of residency (T3) were compared using the paired t test when the data exhibited a normal distribution or with the Wilcoxon test when the data were not normally distributed. The normality of distribution of the data and of the homogeneity of variance was investigated using the Shapiro-Wilk test and the test of equality of variances, respectively.
The proportions of individuals considered to have stress at T1 and T3 were compared using McNemar’s test.
Whenever the data corresponding to the end of the first year of residency (T3) were missing, the data corresponding to T2 (6 months after admission to the residency program) were used.
The significance level was set at 0.05 in all of the tests. Analyses were performed using the Stata 12.0 statistical package (StataCorp, College Station, TX, USA).
Results
Of 37 residency programs at institutions affiliated with the public health system in 2009, 11 (30.6 %) agreed to participate in the study. These institutions were located at the Brazilian South, Southeast, and Northeast regions, whereas the North, Center-West, and Center regions were not represented.
In total, 54 doctors admitted to the first year of clinical oncology residency programs during 2010 and 2011 were included in the study, representing 100 % of newly admitted residents at the 11 participating institutions. Table 1 describes the main sociodemographic characteristics of the sample. Most of the residents were young, with a median age of 28.4 years, single (83.3 %), without children (94.4 %), and had family support (67.3 %). No gender was predominant. Most residents did not engage in physical activities (82.7 %), reported the consumption of three or fewer alcoholic drinks per week (75 %), and were nonsmokers (100 %).
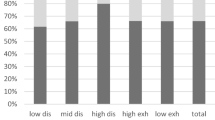
Table 2 describes the data relative to the residents’ workload and to the prevalence of burnout, depression, and stress. All of the residents worked more than 44 h per week, and 55.8 % worked more than 60 h per week
Based on the cutoff points recommended by Maslach in 1996 for doctors [1], it was found that 49 % of the participants exhibited high levels of emotional exhaustion and 64.7 % exhibited high levels of depersonalization upon admission to the residency programs, while most (56.9 %) still exhibited high perceived levels of personal accomplishment. Thus, 76 % of the sample met the current criteria for burnout, i.e., high levels of emotional exhaustion and/or depersonalization, upon admission to the residency program.
Nevertheless, only 4 % of the participants exhibited moderate or severe depression and 6.1 % exhibited severe stress (near exhaustion and exhaustion phases).
Excessive workload, as represented by the number of patients seen per day superior to 15 and more than 60 h of work a week, had a significant relationship with high levels of the burnout syndrome components: emotional exhaustion (t test, p = 0.036 and 0.013, respectively) and depersonalization (t test, p = 0.005 and 0.015, respectively).
The Catholic religion exhibited a relationship with high levels of depersonalization (t test, p = 0.006) and depression (Mann-Whitney, p = 0.017). Availability of family support was protective relative to emotional exhaustion (t test, p = 0.026), while psychotherapy was protective relative to depersonalization (t test, p = 0.029). Higher income exhibited a relationship with a higher level of personal accomplishment and a lower level of depression (Mann-Whitney, p = 0.044 and 0.007, respectively). No other factors were found to be associated with burnout syndrome, stress, or depression upon admission to clinical oncology residency programs.
The scores on the MBI domains emotional exhaustion and depersonalization increased significantly during the first year of residency (Table 3).
Discussion
The present study provides epidemiological data relative to doctors entering clinical oncology residency programs at Brazilian institutions; these data were not available in the literature up to the present time. Our investigation also provides relevant information regarding the prevalence of burnout syndrome, depression, and stress in this population.
Approximately 49 % of the residents exhibited high levels of emotional exhaustion and 64.7 % exhibited high levels of depersonalization upon admission to the programs. Based on the definition of burnout syndrome available in the literature [16, 17], a worrisome prevalence of 76 % was found in the investigated population. This result was attained with cutoff points established for doctors, whose MBI scores are higher compared with other professionals [1].
Given that most of the volunteers exhibited burnout upon admission to the residency programs, it was not possible to assess eventual risk factors for the appearance of this condition during the first year of residency. Nevertheless, the severity of the components emotional exhaustion and depersonalization worsened significantly during the course of the first year of residency (p = 0.003 and p = 0.009, respectively). The prevalence of burnout syndrome increased from 76 to 88 % between the beginning and end of the first year of residency.
In agreement with the literature, the present study found a significant association between workload (measured by the number of patients seen per day and the number of work hours per week) and prevalence of burnout syndrome upon admission to the residency programs.
The burnout rate found upon admission to the programs is confirmed by that reported by Shanafelt et al. for a sample of 115 doctors enrolled in an internal medicine residency program [10]. Given that the residents had been in the program for less than one month, the high rates of burnout found in the present study cannot be attributed to conditions peculiar to the oncology setting. It is more plausible that the volunteers were still under the effect of the internal medicine residency program, which oncology residents must first attend according to Brazilian legislation.
Data on the prevalence of burnout syndrome in oncology residents are scarce in the international literature. Such data were reported by Blanchard et al. in a cross-sectional study conducted in France. In that study, questionnaires were sent by e-mail and regular mail to 340 oncology residents, consisting of 125 in hematology, 120 in radiotherapy, and 95 in medical oncology. In contrast with our study, the volunteers assessed by Blanchard et al. were attending all years of the residency programs. In total, 204 residents (60 %) answered questionnaires, including 67 enrolled in medical oncology programs. The overall rate of burnout syndrome was 44 %, being 37 % in the group of clinical oncology residents; the data corresponding to first-year residents were not reported separately [16].
The authors of a study conducted with 4402 medical students, 1701 residents, and 7288 doctors at the beginning of their professional career suggest that the training period coincides with the peak of burnout syndrome prevalence, and residency was noted as an independent risk factor [11].
In addition to their negative impact on the individual’s quality of life, depression, stress, and burnout syndrome may also affect the quality of care delivered to patients. In a study conducted with 123 pediatric residents, 20 % of whom exhibited depression and 74 % of whom met the criteria for burnout, the frequency of prescription errors was 6.2 times higher among the residents with depression [12]. Confirming those data, 53 % of the internal medicine residents exhibiting burnout reported the occurrence of at least one episode of suboptimal patient care during the previous month [10]. By contrast, a study with 2620 patients and 166 doctors showed that the patients whose doctors reported high levels of satisfaction with their career were most satisfied with the treatment given [22].
In our study, the high prevalence of burnout among the oncology residents poses a serious problem for their quality of life and represents potential risk for the quality of medical care provided by them. However, the present study did not include instruments to assess the effect of the burnout syndrome on the professional activity of the participants. A further limitation of the present study derives from the fact that the sociodemographic questionnaire did not assess the period preceding admission to the residency programs in clinical oncology, i.e., it did not assess the work conditions during the preceding residency program in internal medicine.
In spite of this limitations, the present study provides important information on the prevalence of burnout syndrome and related factors among doctors enrolled in oncology programs at Brazilian institutions. We conclude that a large fraction of the participants met the criteria for burnout syndrome upon admission to the oncology residency programs. Because of that, future studies aiming to identify risk factors for this syndrome should include a joint assessment of the internal medicine residency program.
The subject of the present study is of interest for any institution that trains oncologists. Because of the scarcity of data in the international literature, further investigations are necessary to more accurately assess the occurrence of burnout syndrome in this population.
References
Maslach C, Jackson SE, Leiter MP (1996) Maslach Burnout Inventory Manual, 3rd edn. Mind Garden, Palo Alto
Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM, Leaning MS, Snashall DC, Timothy AR (1995) Burnout and psychiatric disorder among cancer clinicians. Br J Cancer 71(6):1263–1269
Felton JS (1998) Burnout as a clinical entity—its importance in health care workers. Occup Med (Lond) 48(4):237–250
Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52:397–422
Mingote Adán JC, Moreno Jiménez B, Gálvez Herrer M (2004) Burnout and the health of the medical professionals: review and preventive options. Med Clin (Barc) 123(7):265–270
Whippen DA, Canellos GP (1991) Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol 9(10):1916–1920
Trufelli DC, Bensi CG, Garcia JB, Narahara JL, Abrão MN, Diniz RW, Miranda Vda C, Soares HP, Del Giglio A (2008) Burnout in cancer professionals: a systematic review and meta-analysis. Eur J Cancer Care (Engl) 17(6):524–531. doi:10.1111/j.1365-2354.2008.00927.x
Shanafelt TD, Gradishar WJ, Kosty M, Satele D, Chew H, Horn L, Clark B, Hanley AE, Chu Q, Pippen J, Sloan J, Raymond M (2014) Burnout and career satisfaction among US oncologists. J Clin Oncol 32(7):678–686. doi:10.1200/JCO.2013.51.8480
Glasberg J, Horiuti L, Novais MA, Canavezzi AZ, da Miranda Costa V, Chicoli FA, Gonçalves MS, Bensi CG, del Giglio A (2007) Prevalence of the burnout syndrome among Brazilian medical oncologists. Rev Assoc Med Bras 53(1):85–89
Shanafelt TD, Bradley KA, Wipf JE, Back AL (2002) Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 136(5):358–367
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89(3):443–451. doi:10.1097/ACM.0000000000000134
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, Edwards S, Wiedermann BL, Landrigan CP (2008) Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ 336(7642):488–491. doi:10.1136/bmj.39469.763218.BE
West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, Shanafelt TD (2006) Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA 296(9):1071–1078
McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA (2008) Resident physician burnout: is there hope? Fam Med 40(9):626–632
Gonz Aacute Lez-Aacute Vila G, Bello-Villalobos H (2014) Burnout effect on academic progress of Oncology medical residents. Rev Med Inst Mex Seguro Soc 52(4):468–473
Blanchard P, Truchot D, Albiges-Sauvin L, Dewas S, Pointreau Y, Rodrigues M, Xhaard A, Loriot Y, Giraud P, Soria JC, Kantor G (2010) Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer 46(15):2708–2715. doi:10.1016/j.ejca.2010.05.014
Grunfeld E, Zitzelsberger L, Coristine M, Whelan TJ, Aspelund F, Evans WK (2005) Job stress and job satisfaction of cancer care workers. Psychooncology 14(1):61–69
Gorenstein C, Andrade L (1996) Validation of a Portuguese version of the Beck Depression Inventory and the State-Trait Anxiety Inventory in Brazilian subjects. Braz J Med Biol Res 29(4):453–457
Lipp ME (2000) Manual do Inventário de Sintomas de stress para Adultos de Lipp (ISSL) [Manual for Lipp’s Inventory of Stress Symptoms in Adults]. Casa do Psicólogo, São Paulo, pp 11–39
Benson S, Sammour T, Neuhaus SJ, Findlay B, Hill AG (2009) Burnout in Australasian younger fellows. ANZ J Surg 79(9):590–597. doi:10.1111/j.1445-2197.2009.05012.x
Thomas NK (2004) Resident burnout. JAMA 292(23):2880–2889
Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA (2000) Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med 15(2):122–128
Financial Support
Department of Oncology and Hematology, ABC Foundation School of Medicine (Academic founding without profit intentions).
Conflict of Interest
The corresponding author (Daniel I G Cubero) has full control of all primary data and he agrees to allow the journal to review the data if requested. The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article was translated from Portuguese to English by American Journal Experts. Previous presentations: 2013 Brazilian Society of Clinical Oncology Meeting in Brasilia - Brazil - Oral Presentation.
Rights and permissions
About this article
Cite this article
Cubero, D.I.G., Fumis, R.R.L., de Sá, T.H. et al. “Burnout in Medical Oncology Fellows: a Prospective Multicenter Cohort Study in Brazilian Institutions”. J Canc Educ 31, 582–587 (2016). https://doi.org/10.1007/s13187-015-0850-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-015-0850-z