Abstract
Despite well-established variations in the health risks posed by visceral vs. subcutaneous abdominal (SCABD) fat depots, surprisingly little is known on the differences within a given adipose tissue (AT) among severely obese patients displaying varying metabolic dysfunction. We thus compared, by quantitative PCR, the expression profile of a number of genes in the SCABD, omental (OME), and mesenteric (MES) depots of severely obese women with (DYS; n = 25) or without (NDYS; n = 23) a dysmetabolic profile. Fasting insulinemia and HOmeostasis Model Assessment-insulin resistance (HOMA-IR) were higher and plasma adiponectin level lower in DYS women (p < 0.05). Among enzymes involved in fatty acid metabolism and local cortisol production, phosphodiesterase-3B expression was lower in SCABD and MES fat, while 11β-hydroxysteroid dehydrogenase type 1 mRNA levels were higher in visceral depots of DYS women (p < 0.05). Regarding vascular homeostasis and inflammation, plasminogen activator inhibitor-1 and interleukin-6 mRNA levels were higher in OME fat, while adiponectin expression was lower in SCABD and OME ATs of DYS women (p < 0.05). Finally, HOMA-IR was positively associated with SCABD AT IL6 mRNA, only in DYS women (r = 0.47; p < 0.05). In conclusion, although metabolic and secretory characteristics of all depots vary with subjects’ metabolic profile, we find little evidence for a protective role of SCABD AT and no evidence for a further deleterious role of MES fat in DYS vs. NDYS severely obese women. Regional variation in the overall gene expression revealed that OME and MES fat were more closely related to each other in DYS women, while SCABD and MES depots showed greater resemblance in NDYS women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of severe obesity continues to dramatically increase in Canada [18]. However, more important than adiposity per se for health is the distribution of adipose tissue (AT). In this regard, the accumulation of visceral abdominal fat is known to be closely associated with increased coronary heart disease (CHD) risk and premature death [10]. This is likely the result of the differential secretion and function of the various fat depots found throughout the organism [1, 37].
Obesity is considered a low-grade inflammatory state, reflected by AT secretion of numerous factors among which high interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) vs. low adiponectin levels may be involved in the development of metabolic syndrome (MetS) and its related comorbidities [2]. The increased obesity-related CHD risk has previously been related to a higher AT expression and production of angiotensinogen and plasminogen activator inhibitor-1 (PAI-1) [17, 20]. AT is a major site for glucocorticoid metabolism through the 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), a key enzyme involved in local production of cortisol [24] which activates a class of nuclear receptors, the peroxisome proliferator-activated receptors-gamma (PPAR-γ) that control adipogenesis and modulate fat mass accretion [14]. AT mass expansion is also determined by the functional balance between lipid storage and mobilization, mainly through lipoprotein lipase (LPL) and hormone-sensitive lipase (HSL) activities [15] whose main regulatory hormones are catecholamines acting on both α2- and β-adrenoceptors (ARs), but also via PDE-3B through which insulin exerts its antilipolytic and lipogenic effects [22].
Although regional variation in AT metabolism and secretory function is well recognized in obese individuals [21, 42], few studies have examined the potential contribution of visceral vs. subcutaneous abdominal (SCABD) AT to the development of a dysmetabolic profile and CHD risk in severely obese patients. In this regard, insulin resistance (IR) rather than obesity has already shown to be associated with altered gene expression of the insulin signaling cascade, especially in omental (OME) fat of morbidly obese women [26]. Also, OME AT of severely obese women with IR was characterized by an increased inflammatory state, when compared to SCABD fat [25]. Although OME is considered as a major contributor to cardiometabolic risk compared to the SCABD AT [1, 37], whether mesenteric (MES) fat dysfunction plays an important role in IR and MetS was not extensively studied, mainly because of difficulties in accessing this depot for sampling.
To our knowledge, only two studies have examined MES fat in the context of obesity-related complications such as IR and type 2 diabetes (T2D). In the first, examining morbidly obese patients with or without T2D paired for age, adiposity, and blood pressure, adiponectin gene expression was found to be down-regulated in MES fat of diabetic subjects. However, 11β-HSD1 and PPAR-γ mRNA levels were up-regulated in the MES depot but not in the SCABD and OME fat of these subjects [45]. In contrast, the second study, also conducted on morbidly obese patients paired for age, sex, and physical and metabolic characteristics, showed very few changes with IR in mRNA levels for a wide variety of genes involved in inflammation, cell signaling, and metabolism in the MES fat, despite a number of changes in OME and SCABD depots [44].
Therefore, whether abnormal metabolic and secretory characteristics of MES fat occur with and could be involved in the development of a dysmetabolic profile, and thus pose a cardiometabolic risk, need to be more fully investigated in the context of severe obesity. The aims of this study were thus (1) to compare AT gene expression of fatty acid (FA) metabolism biomarkers and secretory factors in various depots between severely obese women with or without a dysmetabolic profile, and (2) to explore relationships between AT gene expression and IR in DYS and NDYS patients.
Materials and methods
Selection of patients
This study included Caucasian pre-menopausal severely obese women characterized by body mass index (BMI) values greater than 40 kg/m2, who were candidates for biliopancreatic diversion with duodenal switch surgery [29] at the Quebec Heart and Lung Institute. Subjects with hepatotoxic medication, history of hepatitis, prior weight-loss surgery, smoking and/or consuming more than 100 g of alcohol per week were excluded. The experimental design was approved by our local hospital and university ethics committees (Laval University Ethics Committee approval CERUL # 2004-108), and all participants provided their written informed consent.
Forty-eight women paired for age and adiposity were selected for our study. They were classified into two subgroups according to the presence (DYS; n = 25) or absence (NDYS; n = 23) of a dysmetabolic profile, defined here as the presence of the three following fixed criteria: fasting glucose ≥6.1 mmol/L, triacylglycerol (TAG) ≥1.69 mmol/L, and high-density lipoprotein (HDL)-cholesterol levels <1.29 mmol/L (Table 1). These criteria are a subset of the clinical features of the metabolic syndrome as defined in the NCEP-ATPIII report [33]. Resting blood pressure (BP) was not used as more than half of all of our subjects were hypertensive [11]. Waist circumference was also not used due to its poor ability to predict the prevalence of metabolic abnormalities in severely obese women, as previously shown by our group [12]. For these reasons, we chose to use the term “dysmetabolic profile” instead of MetS to describe our metabolically deteriorated subjects. Thirteen of the 25 DYS women were diabetic according to WHO guidelines [43], although none was treated with glitazones.
Anthropometric, body fat distribution and blood pressure measurements
Patients were weighed in a light gown on an electronic Toledo scale adapted for body weight higher than 136 kg, and BMI was calculated as the ratio of weight (kg) to height squared (m2). Body fat distribution was assessed using waist circumference measured in a standard position at the widest circumference of the umbilical level. Resting BP measurements were performed at the Quebec Heart and Lung Institute, the day before bariatric surgery by the nursing staff using Life Sign (Welch Allyn Co., Skaneatles, NY) with a large cuff while subjects were recumbent [6].
Lipid-lipoprotein and inflammatory profiles
Blood sampling was performed in the morning after a 12 h-overnight fast. Plasma cholesterol, HDL-cholesterol, low-density lipoprotein (LDL)-cholesterol, TAG, and fasting glucose concentrations were evaluated by routine methods in the clinical laboratories of the Quebec Heart and Lung Institute. Plasma insulin concentrations were determined by a high-sensitivity enzyme-linked immunosorbent assay (ELISA) (Cedarlane Laboratories Ltd, Hornby, Ontario, Canada). Insulin resistance based on the HOmeostasis Model Assessment (HOMA) index was evaluated according to the following equation: insulin (μUI/mL) × glucose (mmol/L)/22.5 [30]. Plasma TNF-α and IL-6 concentrations were measured by a high-sensitivity ELISA (R&D Systems Inc., Minneapolis, MN). The run-to-run coefficients of variation were less than 10 % for IL-6 and TNF-α [6]. Plasma adiponectin concentrations were determined by ELISA (B-Bridge International, Inc., San José, CA), and intra- and inter-assay coefficients of variation were 3.3 and 7.4 %, respectively [6]. Finally, another blood sample was collected in plastic tubes containing trisodium citrate anticoagulant with great care in order to minimize platelet activation. Plasma PAI-1 antigen levels were measured by ELISA using Asserachrom PAI-1 kits from Diagnostica Stago (Asnières, France), and both intra- and inter-assay coefficients of variation were less than 5 % [5].
Adipose tissue biopsies
All adipose tissue samples were recovered following an overnight (12-h) fast. General balanced anesthesia was induced by a short-acting barbiturate and maintained by fentanyl and a mixture of oxygen and nitrous oxide. Patients did not receive drugs acting on the autonomic nervous system or modifying catecholamine levels [6]. After surgical excision, AT samples of 200 mg approximately were obtained from the three adipose depots under consideration: the superficial SCABD AT (near the umbilicus), an extraperitoneal fat drained by the systemic circulation, as well as the OME and MES ATs, two intraperitoneal depots drained by the portal vein to the liver [37]. SC ABD fat was removed at the start of the surgery, whereas OME and MES ATs were taken 15–30 min later. From these samples, 100 mg were used for quantification of selected AT gene mRNA levels. All measurements were performed in duplicate.
RNA preparation and quantification of AT gene mRNA levels
Briefly, about 5 to 10 μg of total RNA was extracted from 100 mg of each AT sample using RNeasy Mini Kits (Qiagen, Mississauga, Ontario, Canada). This technique integrates phenol-guanidine lysis and silica gel-membrane purification of total RNA. The isolated total RNA concentration was quantified by absorbance at 260 nm, and its integrity was verified using agarose gels (1 %) stained with ethidium bromide. The 260/280 nm absorption of all preparations ranged between 1.9 and 2.1. For each sample, 1 μg of total RNA was reverse transcribed into complementary DNA (cDNA), using SuperScript II Reverse Transcriptase kit (Invitrogen Canada, Burlington, Ontario), and 50 ng of cDNA were used for quantitative polymerase chain reaction (qPCR). AT mRNA levels were quantified by fluorescent quantitative PCR on a Rotor Gene 3000 (Corbett Research, Montreal Biotech, Kirkland, Québec, Canada), using the SYBR Green Jump Start TAQ ready mix (Sigma-Aldrich, Oakville, Ontario, Canada) [6]. The 13 genes examined were classified into four “families”: FA metabolism (LPH, HSL, PDE-3B, α2- and β2-ARs), inflammation (TNF-α, IL-6, and adiponectin), vascular homeostasis (PAI-1 and angiotensinogen), adipogenesis (PPAR-γ1/γ2) and local cortisol production (11β-HSD1). Primer forward and reverse sequences for the genes of interest and the housekeeping gene, as well as the corresponding PCR conditions for their use, are shown in Table 2. PCR reactions consisted of an initial denaturation step at 95 °C for 2 min, followed by x cycles (specified in Table 2) composed of 20 s at 95 °C, 20 s annealing at 60 or 64 °C depending on the gene, and 20 s elongation at 72 °C. Reactions were then heated to between 72 and 99 °C in steps of 1 °C for 5 s to obtain the melting curve and to confirm a single PCR product. The mRNA levels were calculated using the standard curve method (Rotor Gene 3000) and normalized to glyceraldehyde phosphate dehydrogenase which was used as the housekeeping gene.
Statistical analyses
Results are presented as means ± standard deviation (SD) in tables and as means ± standard error (SE) in figures. Student t tests were used to compare group (DYS vs. NDYS) characteristics. Between-group differences and regional variation were evaluated by two-way analysis of variance (ANOVA). Post hoc analysis using Bonferroni correction was used to compare expression of genes between the three fat depots and across conditions. Hierarchical clustering analysis in JMP 9 (SAS Institute) software was used to determine the relatedness of adipose depots, based on the patterns of overall gene expression, in DYS and NDYS patients considered separately. Associations between variables of interest were quantified by linear regression analysis using Pearson’s product moment correlation coefficients. Analyses were conducted using SAS software (version 9.1.6 for Windows) or JMP software (version 9 for Macintosh), and statistical significance was considered attained at p < 0.05.
Results
Characteristics of DYS and NDYS patients
Comparisons between DYS and NDYS women are shown in Table 1. As expected by our pairing procedure, no between-group difference was observed for age, body weight, and BMI. Also, DYS women showed higher fasting glucose and triacylglycerol levels as well as lower HDL-cholesterol concentrations than NDYS women. Although being higher than the healthy thresholds defined according to the NCEP-ATPIII guidelines [33], resting systolic and diastolic blood pressures were comparable in both groups. Also, waist circumference tended to be higher in DYS than in NDYS women. The cholesterol/HDL-cholesterol ratio was higher in DYS than in NDYS patients. IR, as reflected by a higher fasting insulinemia and HOMA index, was greater in DYS women. Plasma adiponectin concentrations were lower in DYS than in NDYS women, while trends for higher TNF-α concentrations were observed in the former. Finally, neither IL-6 nor PAI-1 concentrations differed between groups.
Between-group differences and regional variation in AT gene expression of FA metabolism biomarkers
As illustrated in Fig. 1, neither LPL nor HSL expression differed between groups, irrespective of fat depot. PDE-3B expression was, however, lower in SC ABD and MES adipose depots of DYS women (p < 0.05). Although LPL expression did not show regional variation, HSL mRNA levels were higher in the SCABD than in the OME fat (0.01 < p < 0.05), regardless of patients’ metabolic profile. Also, PDE-3B expression was the highest in SCABD and MES depots (0.0001 < p < 0.005), in NDYS women, only.
Between-group differences and regional variation in AT mRNA levels of key enzymes involved in lipid storage and mobilization. Values are means ± SE. LPL lipoprotein lipase, HSL hormone-sensitive lipase, PDE-3B phosphodiesterase-3B, SCABD subcutaneous abdominal, OME omental, MES mesenteric, DYS dysmetabolic, NDYS non dysmetabolic. Between-group differences at *p < 0.05 and regional variation at a p < 0.05, b p < 0.01, c p < 0.005, and d p < 0.0001 are indicated
As shown in Fig. 2, mRNA levels of the antilipolytic α2-ARs were lower in SCABD and OME fat depots of DYS women (0.005 < p < 0.05). Also, mRNA levels of the lipolytic β2-ARs were respectively higher in SCABD and lower in OME AT of these patients (p < 0.05).
Between-group differences and regional variation in AT mRNA levels of antilipolytic α2-ARs and lipolytic β2-ARs. Values are means ± SE. ARs adrenoreceptors, DYS dysmetabolic, NDYS non dysmetabolic. Between-group differences at *p < 0.05 and **p < 0.005 and regional variation at c p < 0.005 and d p < 0.0001 are indicated
The highest α2-AR expression was found in the SCABD and OME depots (p < 0.0001), while the lowest β2-AR expression was observed in the SCABD fat of NDYS women, exclusively (0.0001 < p < 0.005).
Between-group differences and regional variation in AT gene expression of inflammatory factors
As shown in Fig. 3, TNF-α expression did not differ between groups and sites, while IL-6 mRNA levels were higher in OME fat of DYS patients, only (p < 0.05). Adiponectin expression was lower in both SCABD and OME fat depots of DYS women (0.005 < p < 0.05). MES fat displayed the highest TNF-α expression (p < 0.0001), while IL-6 expression was higher in MES than in SCABD fat of DYS women (p < 0.05). Adiponectin mRNA levels were the highest in the SCABD AT of NDYS women (p < 0.05).
Between-group differences and regional variation in AT mRNA levels of inflammatory factors. Values are means ± SE. TNF-α tumor necrosis factor-α, IL-6 interleukin-6, Acrp30 adiponectin, DYS dysmetabolic, NDYS non dysmetabolic. Between-group differences at *p < 0.05 and **p < 0.005 and regional variation at a p < 0.05 and d p < 0.0001 are indicated
Between-group differences and regional variation in AT gene expression of pro-thrombotic factors
Figure 4 shows a greater PAI-1 expression in OME fat of DYS than in NDYS women (p < 0.05), despite a lack of between-group difference in angiotensinogen expression. PAI mRNA levels were the highest in OME fat of DYS women (p < 0.0001), while they were higher in the OME than in the SCABD AT of NDYS women (p < 0.05). The highest angiotensinogen expression was observed in visceral fat depots, irrespective of the group (0.0001 < p < 0.05).
Between-group differences and regional variation in AT mRNA levels of pro-thrombotic factors. Values are means ± SE. AGT angiotensinogen, PAI-1 plasminogen activator inhibitor-1, DYS dysmetabolic, NDYS non dysmetabolic. Between-group differences at *p < 0.05 and regional variation at a p < 0.05, b p < 0.01, and d p < 0.0001 are indicated
Between-group differences and regional variation in AT gene expression of adipogenesis and local cortisol production
Neither PPAR-γ1 nor PPAR-γ2 expression differed according to patients’ metabolic profile. However, 11β-HSD1 AT mRNA levels were higher in visceral fat depots of DYS women (0.005 < p < 0.05). PPAR-γ2 mRNA levels were the highest in the MES fat, irrespective of the group (0.005 < p < 0.05). In both groups, 11β-HSD1 mRNA levels were higher in OME than in other depots (0.0001 < p < 0.01) (Fig. 5).
Between-group differences and regional variation in AT mRNA levels of adipogenic factors and of 11β-HSD1. Values are means ± SE. PPAR-γ peroxisome proliferator-activated receptors-gamma, 11β-HSD1 11β-hydroxysteroid dehydrogenase type 1, DYS dysmetabolic, NDYS non dysmetabolic. Between-group differences at *p < 0.05 and **p < 0.005 and regional variation at a p < 0.05, b p < 0.01, c p < 0.005, and d p < 0.0001 are indicated
As summarized in Table 3, differences in the expression of genes between DYS and NDYS women are found for all three depots studied. MES AT showed the fewest differences between groups, with only two genes differentially expressed. In the SCABD AT and OME depots, four and six genes, respectively, were differently expressed between groups.
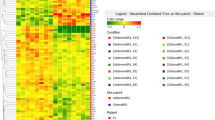
Resemblance in overall gene expression within two fat depots
Cluster analysis was used to measure the relatedness of the fat depots on the basis of the greatest similarities in the expression profiles for the 13 genes investigated, and to verify whether this relatedness was different in DYS and NDYS patients considered separately. As shown in Fig. 6, OME and MES fat were more closely related to each other than to SCABD AT in DYS women. Of note, visceral fat depots displayed comparable low LPL and high IL-6 expressions. In contrast, SCABD and MES ATs showed greater resemblance, when compared to OME fat, in NDYS women. Of particular interest, the expression of key enzymes involved in FA metabolism (LPL, HSL, and PDE-3B) was closer in SCABD and MES fat than in OME AT.
Clustering in overall gene expression between fat depots in DYS and NDYS women. Briefly, each dendrogram is read from the left to the right and vertical lines showed joined clusters. For abbreviations, see legends of Figs. 1, 2, 3, 4, and 5. The 13 genes examined were classified into four families: FA metabolism: 1 LPL, 2 HSL, 3 PDE-3B, 4 α2-ARs, 5 β2-ARs; inflammation: 6 TNF-α, 7 IL-6, 8 adiponectin; vascular homeostasis: 9 angiotensinogen, 10 PAI-1; and adipogenesis and local cortisol production: 11 PPAR-γ1, 12 PPAR-γ2, 13 11β-HSD1
Relationships between IR and plasma or AT mRNA levels of selected adipokines
As DYS women showed IR reflected by fasting hyperglycemia, hyperinsulinemia, and higher HOMA-IR, compared to NDYS subjects (Table 1), whether these metabolic indices were associated with plasma or AT mRNA levels of selected adipokines, irrespective of the anatomic location of fat, was examined in each group. Only HOMA-IR was found to be positively but weakly associated with IL6 mRNA levels in the SCABD AT (r = 0.47; p < 0.05) but not in visceral depots of DYS women (0.05 < r < 0.26). For all women combined (DYS and NDYS), HOMA-IR was also positively and weakly related to IL-6 mRNA levels in the SCABD AT (r = 0.41; p < 0.005) but not in visceral fat (0.20 < r < 0.31) (not shown).
Discussion
The main purpose of our study was to examine SCABD vs. visceral AT gene expression of selected factors in severely obese women of similar age and adiposity, with or without a dysmetabolic profile defined by higher fasting glycemia and triglyceridemia as well as lower HDL-cholesterol levels [6]. We measured a number of markers of FA metabolism and local cortisol production, as well as of inflammatory, pro-thrombotic, and adipogenic factors.
Results clearly showed that DYS women were characterized by different AT gene expression patterns according to the anatomic location of fat, when compared to NDYS women. Indeed, lower expression of PDE-3B and α2-ARs as well as of adiponectin vs. higher expression of β2-ARs were observed in the SCABD AT of DYS patients. Although lower mRNA levels of α2-ARs, β2-ARs, and adiponectin vs. higher mRNA levels of IL-6, PAI-1, and 11β-HSD1 were seen in the OME depot of DYS subjects, lower expression of PDE-3B and higher expression of 11β-HSD1 were the only between-group differences found in the MES fat (Table 3).
Differences between SCABD, OME, and MES fat have been little examined in this context, with the exception of two studies performed on morbidly obese subjects with or without T2D [45], being IR or insulin sensitive (IS) [44]. Our data are partly concordant with those of Xu et al. [44] who reported very few differences in the expression of numerous genes associated with inflammation, metabolism, and cell signaling in the MES depot of IR vs. IS morbidly obese subjects. However, the lack of between-group differences in TNF-α, angiotensinogen, and PPAR-γ1/γ2 expression, irrespective of the fat depot, and the increased one of PAI-1 in the OME AT are in contrast with the observations of Xu et al. [44]. In the latter study, TNF-α expression increased in the MES fat, only, while angiotensinogen expression decreased in OME and SCABD ATs of IR individuals, exclusively. In addition, PAI-1 expression increased in SCABD and decreased in OME fat, while it remained unchanged in the MES AT of IR subjects. PPAR-γ increased in both SCABD and MES ATs of IR patients, only. These discordances could be explained by a number of differences between studies. For instance, Xu et al. [44] studied a small number of IR vs. IS subjects (of both genders) who displayed lower BMI values than ours and differed only according to fasting insulinemia and HOMA-IR, and total PPAR-γ, instead of its main isoforms 1 and 2, was investigated. Also, the lack of between-group differences in PPAR-γ1/γ2 and adiponectin AT gene expression in our study is not consistent with the highest PPAR-γ and the lowest adiponectin mRNA levels in the MES fat of diabetic subjects reported by Yang et al. [45]. Once again, differences between these data and ours could be due to the above-cited reasons and to the fact that they studied outright diabetic patients.
Moreover, the greater expression of 11β-HSD1 found in both visceral depots of DYS women is not fully concordant with the higher mRNA levels in MES than in OME and SCABD ATs of diabetic patients reported by Yang et al. [45]. The enhanced enzyme expression we observed probably reflects elevated local cortisol production resulting from an increased hypothalamic-pituitary-adrenal axis, as reported almost 20 years ago [4]. This does not, however, necessarily imply that SCABD fat is not involved in cortisol secretion, as 11β-HSD1 was shown to be overexpressed in this depot when compared to the OME fat of morbidly obese subjects, irrespective of the presence of MetS [32].
Taken together, our data suggest that gene expression profile of the MES fat is not further deteriorated and thus does not exert a greater deleterious impact on obesity-related metabolic complications than OME AT, in DYS women. Whether the dysmetabolic profile modulates depot-specific AT gene expression or, on the contrary, changes in depot-specific AT gene expressions lead to a dysmetabolic state cannot be easily answered and requires further investigation. This is not surprising when comparing subcutaneous to visceral depots, as their different patterns of gene expression have been related to their embryological origin, the lateral plate mesoderm serving as a major source of visceral AT [7]. However, the heterogeneity of visceral fat progenitors remains one of the main unanswered questions in this field. In one study performed on human depots, pre-adipocytes of MES AT were shown to display an expression profile closer to that of SCABD rather than OME fat [38]. Our data would appear to offer support for differences in the origin of MES and OME depots, given their different responses according to the dysmetabolic status of the patient. As severely obese individuals accumulate large amounts of fat at both visceral and subcutaneous sites, it is of interest to question whether the balance between potential protective (favorable) and deleterious (adverse) effects of subcutaneous and visceral ATs might influence metabolic disorders [21, 42]. In this regard, whether OME fat represents a major “culprit,” in contrast to SCABD AT that is often considered as an innocent “bystander,” requires further investigation. Our data are also interesting in the context of the AT expandability hypothesis [41] which states that a failure in the capacity for fat mass expansion, rather than obesity per se, is the key factor linking positive energy balance and metabolic dysfunction. The observation that the gene expression profile of the SCABD fat depot studied here presents a potentially decreased response to antilipolytic (PDE-3B, α2-AR) and increased response to lipolytic (β2-AR) signals in the dysmetabolic state is concordant with this hypothesis. The SCABD fat depot would thus be less able of answering the need to store fatty acids, leading to eventual ectopic fat deposition in visceral AT and peripheral tissues such as liver and muscle and its resulting metabolic effects [9, 31, 35]. That MES and OME adipose depots are more closely related to each other, in that they do not display the coordinated increased lipolytic and decreased antilipolytic gene expression seen in the SCABD AT, could support that they are indeed acting as sites for ectopic spillover lipid accumulation in DYS women.
Previous experiments conducted on SCABD and OME fat have demonstrated that IR could affect both the gene expression and protein levels of metabolic and secretory factors [8, 25–27, 39, 40]. In our study, the observation that OME fat in DYS patients showed an increased expression of IL-6 and PAI-1 and a decreased one of adiponectin, compared to SC ABD AT, fits well with the higher inflammatory profile of the visceral depot reported in IR morbidly women by Liu et al. [25]. Still, SCABD AT was recently suggested to potentially have a greater contribution than OME fat to the pro-inflammatory milieu associated with severe obesity, as expression of 12 on 19 critical pro-inflammatory genes (such as IL-6, IL-8, and IL-18 for example) as well of anti-inflammatory genes such as adiponectin was substantially higher in subcutaneous than in visceral AT of morbidly obese patients [36]. Although our data are not in full accordance with these observations, a few patients in the study of Spoto et al. [36] had T2D and thus did not show a wide range of HOMA-IR values, possibly explaining differences in our results.
The absence of between-group differences and regional variation in gene expression of the main lipases regulating FA metabolism is concordant with the similar HSL and LPL mRNA levels found in morbidly obese subjects with low or high IR [8, 39]. Although adipose triglyceride lipase (ATGL) expression could have been measured, it is not regulated by obesity in contrast to HSL [28, 34] and does not show differences between subcutaneous and omental fat in obese individuals [3]. Another reason why we decided to measure HSL expression was that it accounts for most of the stimulated lipolysis in contrast to ATGL which rather refers to basal lipolysis [23, 28]. Also, the reduced expression we observe for PDE-3B in SCABD AT of DYS women agrees with its lower mRNA levels observed in morbidly obese patients with high IR [39], thus emphasizing an impaired antilipolytic effect of insulin observed not only in vitro [46] but also in vivo [16]. The higher β2-AR (lipolytic) and lower α2-AR (antilipolytic) mRNA levels, combined with reduced PDE-3B expression (reflecting an altered insulin pathway) in the SCABD AT of DYS women, could reflect a hyperlipolytic state which could lead to an increased release of FAs into the systemic venous circulation, and eventually to their transport to the arterial circulation. Although neither the protein or activity level of these two ARs nor the physiological response of adipose cells to catecholamines was investigated in this study, one could hypothesize that the SCABD AT was as or even more important than OME fat in supplying FAs to the liver and thus in participating in the development of obesity-related metabolic complications. Indeed, it has been estimated that approximately 20 % of portal vein FAs originates from visceral AT, the remaining 80 % arriving from upper- and lower-body subcutaneous fat in obese individuals [19].
The absence of between-group differences in PPAR-γ1/γ2 mRNA levels we found irrespective of the fat depot is concordant with total PPARγ expression reported by Tinahones et al. [39] but discordant with the reduced levels in both visceral and subcutaneous fat of IR vs. IS morbidly obese and normal-weight subjects observed by McLaren et al. [26]. Similarly, our results do not agree with previous data showing decreased PPAR-γ2 expression in OME (but not in SCABD) fat of high vs. low IR morbidly obese subjects [27, 40]. Such discrepancies could be attributed to differences in patients’ physical and metabolic characteristics, the low number of subjects examined, the fact that both genders were pooled in some of the protocols, and the different cut-off values of HOMA index chosen to determine IR vs. IS.
Our study has some limitations that deserve further mention. First, we were not able to measure body composition or directly assess subcutaneous and visceral (omental, mesenteric, or both) adipose depots sizes as obese patients weighing more than 130 kg cannot be subjected to dual energy X-ray absorptiometry and computed tomography at our research center due to equipment limitations. Second, as this study was limited to severely obese women, results cannot be extrapolated to moderately obese or overweight subjects or to men. Third, as we measured mRNA expression only, we cannot with certainty claim equivalent changes to protein levels. Fourth, as AT contains adipocytes and stromal cells including pre-adipocytes, monocytes, and lymphocytes (i.e., the stromal vascular fraction), heterogeneity in the proportion of each cell type [13] might explain the varying gene expression pattern we observed between sites, without actual differences occurring within a given cell type between depots. Lastly, the weak relationships between metabolic status and AT gene expression should be interpreted with caution, as there were few subjects per group and associations reported were between tissue mRNA and circulating protein levels.
Conclusion
Taken together, our data suggest that, in DYS severely obese women, (1) MES AT does not seem to play a further deleterious role in the development of a dysmetabolic profile, when compared to OME fat, and (2) that SCABD AT does not appear to be a protective depot. In addition, metabolic and secretory characteristics of the three depots studied are variably modulated by IR.
References
Bastien M, Poirier P, Lemieux I, Després JP (2014) Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis 56:369–381
Bays HE (2009) “Sick fat,” metabolic disease, and atherosclerosis. Am J Med 122:S26–S37
Berndt J, Kralisch S, Klötting N, Ruschke K, Kern M, Fasshauer M, Schön MR, Stumvoll M, Blüher M (2008) Adipose triglyceride lipase gene expression in human visceral obesity. Exp Clin Endocr Diabetes 116:203–210
Björntorp P (1996) The regulation of adipose tissue distribution in humans. Int J Obes 20:291–302
Bouchard L, Vohl MC, Lebel S, Hould F-S, Marceau P, Bergeron J, Pérusse L, Mauriège P (2010) Contribution of genetic and metabolic syndrome to omental adipose tissue PAI-1 gene mRNA and plasma levels in obesity. Obes Surg 20:492–499
CasparBauguil S, Fioroni A, Galinier A, Allenbach S, Pujol MC, Salvayre R, Cartier A, Lemieux I, Richard D, Biron S, Marceau P, Casteilla L, Pénicaud L, Mauriège P (2012) Pro-inflammatory phospholipid arachidonic acid/eicosapentaenoic acid ratio of dysmetabolic severely obese women. Obes Surg 22:935–944
Chau Y-Y, Bandiera R, Serrels A, Martinez-estrada OM, Qing W, Lee M, Slight J, Thornburn A, Berry R, McHaffie S, Stimson RH, Walker BR, Munoz Chapuli R, Schedl A, Hastie N (2014) Visceral and subcutaneous fat have different origins and evidence supports a mesothelial source. Nature Cell Biol 16:367–375
Clemente-Postigo M, Queipo-Ortuno MI, Fernandez-Garcia D, Gomez-Huelgas R, Tinahones FJ, Cardona F (2011) Adipose tissue gene expression of factors related to lipid processing in obesity. PloS ONE 6:e24783
Cortés VA, Fernandez-Galilea M (2015) Lipodystrophies: adipose tissue disorders with severe metabolic implications. J Physiol Biochem 71:471–478
Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodés-Cabau J, Bertrand OF, Poirier P (2008) Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol 28:1039–1049
Drapeau V, Lemieux I, Richard D, Bergeron J, Tremblay A, Biron S, Marceau P, Mauriège P (2006) Metabolic profile in severely obese women is less deteriorated than expected when compared to moderately obese women. Obes Surg 16:501–509
Drapeau V, Lemieux I, Richard D, Bergeron J, Tremblay A, Biron S, Marceau P, Mauriège P (2007) Waist circumference is useless to assess the prevalence of metabolic abnormalities in severely obese women. Obes Surg 17:905–909
Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW (2004) Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology 145:2273–2282
Farmer SR (2005) Regulation of PPARγ activity during adipogenesis. Int J Obes 29:S13–S16
Fried SK, Ross RR (2004) Biology of visceral adipose tissue. In: Bray GA, Bouchard C (eds) Handbook of obesity. Etiology and Pathophysiology, 2nd edn. M. Dekker Inc, New York, Basel, pp 589–614
Flechtner-Mors M, Jenkinson CR, Alt A, Biesalski HK, Adler G, Ditschuneit HH (2005) Studies of phosphodiesterase effects on adipose tissue metabolism in obese subjects by the microdialysis technique. J Physiol Pharmacol 56:355–368
Gorzelniak K, Engeli S, Janke J, Luft FC, Sharma AM (2002) Hormonal regulation of the human adipose tissue renin-angiotensin system: relationship to obesity and hypertension. J Hypertens 20:965–973
Katzmarzyk PT, Mason C (2006) Prevalence of class I, II and III obesity is increasing in Canada. CMAJ 174:156–157
Klein S (2010) Is visceral fat responsible for the metabolic abnormalities associated with obesity? Diabetes Care 33:1693–1694
Juhan-Vague I, Alessi MC, Mavri A, Morange PE (2003) Plasminogen activator inhibitor-1, inflammation, obesity, insulin resistance and vascular risk. J Thromb Haemost 1:1575–1579
Lafontan M, Berlan M (2003) Do regional differences in adipocyte biology provide new pathophysiological insights? Trends Pharmacol Sci 24:276–283
Lafontan M (2008) Advances in adipose tissue metabolism. Int J Obes 32:S39–S51
Langin D, Dicker A, Tavernier G, Hoffstedt J, Mairal A, Ryden M, Arner E, Sicard A, Jenkins CM, Viguerie N, van Harmelen V, Gross RW, Holm C, Arner P (2005) Adipocyte lipases and defect of lipolysis in human obesity. Diabetes 54:3190–3197
Lee MJ, Fried SK, Mundt SS, Wang Y, Sullivan S, Stefanni A, Daugherty BL, Hermanowski-Vosatka A (2008) Depot-specific regulation of the conversion of cortisone to cortisol in human adipose tissue. Obesity 16:1178–1185
Liu A, McLaughlin T, Liu T, Sherman A, Yee G, Abbasi F, Lamendola C, Cushman SW, Reaven GM, Tsao PS (2009) Differential intra-abdominal adipose tissue profiling in obese, insulin-resistant women. Obes Surg 19:1564–1573
MacLaren R, Cui W, Simard S, Cianflone K (2008) Influence of obesity and insulin sensitivity on insulin signaling genes in human omental and subcutaneous adipose tissue. J Lipid Res 49:308–323
Macias-Gonzalez M, Moreno-Santos I, Garcia-Almeida JM, Tinahones FJ, Garcia-Fuentes E (2009) PPARγ2 protects against obesity by means of a mechanism that mediates insulin resistance. Eur J Clin Invest 39:972–979
Mairal A, Langin D, Arner P, Hoffstedt J (2006) Human adipose triglyceride lipase (PNPLA2) is not regulated by obesity and exhibits low in vitro triglyceride hydrolase activity. Diabetologia 48:1629–1636
Marceau P, Hould F-S, Potvin M, Lebel S, Biron S (1999) Biliopancreatic diversion (duodenal switch procedure). Eur J Gastroenterol Hepatol 11:99–103
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner DC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Moreno-Indias I, Tinahones FJ (2015) Impaired adipose tissue expandability and lipogenic capacities as ones of the main causes of metabolic disorders. J Diab Res doi.org/10.1155/2015/970375
Munoz R, Carvajal C, Escalona A, Boza C, Pérez G, Ibànez L, Fardella C (2009) 11β-Hydroxysteroid dehydrogenase type 1 is overexpressed in subcutaneous adipsoe tissue of morbidly obese patients. Obes Surg 19:764–770
National Cholesterol Education Program (2001) Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood Cholesterol in adults (Adult Treatment Panel III). JAMA 285:2486–2497
Ryden M, Jocken J, van Harmelen V, Dicker A, Hoffstedt J, Wiren M, Blomqvist L, Mairal A, Langin D, Blaak E, Arner P (2007) Comparative studies of the role of hormone-sensitive lipase and adipose triglyceride lipase in human fat cell lipolysis. Am J Physiol Endocr Metab 292:E1847–E1855
Smith U (2015) Abdominal obesity: a marker of ectopic fat accumulation. J Clin Invest 125:1790–1792
Spoto B, Di Betta E, Mattace-Raso F, Sijbrands E, Vilardi A, Parlongo RM, Pizzini P, Pisano A, Vermi W, Testa A, Cutrupi S, D'Arrigo G, Lonardi S, Tripepi G, Cancarini G, Zoccali C (2014) Pro- and anti-inflammatory cytokine gene expression in subcutaneous and visceral fat in severe obesity. Nutr Metab Cardiovasc Dis 24:1137–1143
Tchernof A, Després JP (2013) Pathophysiology of human visceral adipose tissue: an update. Physiol Rev 93:359–404
Tchkonia T, Lenburg M, Thomou T, Giorgadze N, Frampton G, Pirtskhalava T, Cartwright A, Cartwright M, Flanagan J, Karagiannnides I, Gerry N, Forse RA, Tchoukalova Y, Jensen MD, Pothoulakis C, Kirkland JL (2007) Identification of depot-specific human fat cell progenitors through distinct expression profiles and developmental gene patterns. Am J Physiol Endocr Metab 292:E298–E30
Tinahones FJ, Garrido-Sanchez L, Miranda M, Garcia-Almeida JM, Macias-Gonzalez M, Ceperuelo V, Gluckmann E, Rivas-Marin J, Vendrell J, Garcia-Fuentes E (2010) Obesity and insulin resistance-related changes in the expression of lipogenic and lipolytic genes in morbidly obese subjects. Obes Surg 20:1559–1567
Tinahones FJ, Moreno-Santos I, Vendrell J, Chacon MR, Garrido-Sanchez L, Garcia-Fuentes E, Macias-Gonzalez M (2012) The retinoic acid receptor-related orphan nuclear receptor γ1 (ROR γ1): a novel player determinant of insulin sensitivity in morbid obesity. Obes Surg 20:488–497
Virtue S, Vidal-Puig A (2010) Adipose tissue expandability, lipotoxicity and the metabolic syndrome—an allostatic perspective. Biochim Biophys Acta - Mol Cell Biol Lipid 1801:338–349
Wajchenberg BL, Giannella-Neto D, daSilva MER, Santos RF (2002) Depot-specific hormonal characteristics of subcutaneous and visceral adipose tissue and their relation to the metabolic syndrome. Horm Metab Res 34:616–621
World Health Organization (WHO) (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. Report of a WHO Consultation. Part 1: Diagnosis and classification of diabetes mellitus. WHODepartment of Noncommunicable Disease Surveillance, Geneva, pp 1–59
Xu WJ, Gauthier M-S, Hess DT, Apovian CM, Cacicedo JM, Gokce N, Farb M, Valentine RJ, Ruderman NB (2012) Insulin sensitive and resistant obesity in humans: AMPK activity, oxidative stress, and depot-specific changes in gene expression in adipose tissue. J Lipid Res 53:792–801
Yang Y-K, Chen M, Clements RH, Abrams GA, Aprahamian CJ, Harmon CM (2008) Human mesenteric adipose tissue plays unique role versus subcutaneous and omental fat in obesity related diabetes. Cell Physiol Biochem 22:531–538
Zierath JR, Livingston JN, Thörne A, Bolinder J, Reynisdottir S, Lönnqvist F, Arner P (1998) Regional difference in insulin inhibition of non-esterified fatty acid release from human adipocytes: relation to insulin receptor phosphorylation and intracellular signalling through the insulin receptor substrate-1 pathway. Diabetologia 41:1343–1354
Acknowledgments
The severely obese cohort was supported, over the years, by the Laval University Merck-Frosst/CIHR Research Chair in Obesity. We would like to express our gratitude to Y. Gélinas and M. Lacaille for their technical assistance in AT gene mRNA experiments. Many thanks also to Drs. V. Drapeau and F. Therrien for their very helpful assistance in AT and plasma bank management. Special thanks are addressed to C. Leblanc, deceased in November 2013, for his statistical analyses. The cooperation of subjects who participated to this study was also greatly appreciated. Part of this work was supported by the operating grant OHP # 67388 obtained from the Canadian Institutes of Health Research by P. Mauriège.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mauriège, P., Joanisse, D.R., CasparBauguil, S. et al. Gene expression of different adipose tissues of severely obese women with or without a dysmetabolic profile. J Physiol Biochem 71, 719–732 (2015). https://doi.org/10.1007/s13105-015-0436-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-015-0436-6