Abstract
Pregnant women with iron deficiency and those who are carriers of haemoglobinopathies present with anaemia of varying severity. There is no antenatal screening for haemoglobinopathies in India. The objective of this study was to determine the prevalence of undiagnosed haemoglobinopathy carriers in a random sample of pregnant women attending antenatal care clinics in Pune city, India. Biobanked DNA of 360 randomly selected pregnant women was genotyped for six common mutations and two common haemoglobin variants, HbS and HbE. Odds ratios (OR) with 95% confidence intervals were computed to determine association of carrier status with socio-demographic, haematological and clinical characteristics. The prevalence of undiagnosed haemoglobinopathy carriers was 6.3% (95% CI 4.2–9.4%) of which 3.3% (95% CI 1.9–5.7%) were beta thalassaemia carriers. There was an increased odds that beta thalassaemia carriers had moderate anaemia (OR 10.59, 95% CI 1.15–96.90). This study reveals the high prevalence of undiagnosed haemoglobinopathy carriers among pregnant women, indicating the need to immediately implement carrier screening and genetic counselling services across the country.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anaemia is a persistent public health problem worldwide affecting around 27% (95% CI 26.9–27.0) of the global population (Kassebaum et al. 2016). The causes of anaemia are broadly attributed to nutritional deficiencies, infections and genetic disorders, particularly the haemoglobinopathies, beta thalassaemia and sickle cell anaemia. Globally, iron deficiency accounts for the highest cause of anaemia (63%), followed by thalassaemia trait (5.4%), malaria (4%) and sickle cell trait (2.2%) (Kassebaum et al. 2016). India has a dual burden of nutritional anaemia and haemoglobinopathies (Weatherall and Clegg 2008). A nationwide survey conducted in 2015–2016 reported that 53% women, 24% men and 58% pregnant women in India had anaemia of varying severity (International Institute for Population Sciences and ICF 2017). The Comprehensive National Nutrition Survey (CNNS), a nationwide study that measured the prevalence of anaemia in the age group of 1–19 years, reported beta thalassaemia and sickle cell carrier prevalence to be 4·9% (95%CI 3·6–6·5) and 1·6% (95%CI 1·1–2·4) in the 1–4 year age group respectively, 9·3% (95%CI 7·2–12·1) and 1·9% (95%CI 1·3–2·9) in the 5–9 year age group and 7·3% (95%CI 5·8–9·2) and 1.6% (95%CI 1·0–2·4) in the 10–14 year age group (Sarna et al. 2020).
Studies to estimate the prevalence of beta thalassemia carriers in India have been challenged by lack of systematic sampling and lack of use of international diagnostic criteria and laboratory standards. As such, wide variations in beta thalassaemia carrier prevalence ranging from 1.5% (Achoubi et al. 2012) to 10.4% (Dolai et al. 2012) have been reported. The prevalence of sickle cell carriers ranged between 0.7% in urban areas (Mohanty et al. 2013) and as high as 14% in tribal areas (Mohanty et al. 2015). Among all age groups, estimates suggest that in absolute numbers, there may be nearly 24.7 million carriers of beta thalassaemia and 16.9 million carriers of sickle cell anaemia. The annual numbers of cases of beta thalassaemia major and sickle cell anaemia in India are estimated to be 5500 and 11,000 respectively (Modell et al. 2018).
Despite this underlying burden of haemoglobinopathies, India is yet to implement a carrier screening programme, although national guidelines for the prevention and control of haemoglobinopathies have been published (Ministry of Health and Family Welfare, Government of India 2016). Carrier screening provides the opportunity for making informed reproductive decisions and has been the key strategy for prevention and control of haemoglobinopathies in several high burden countries (Goonasekera et al. 2018). Among pregnant women, haemoglobinopathy carriers present with mild to moderate anaemia, similar to women with nutritional anaemia. Beta thalassaemia carrier diagnosis is necessary to empower prospective parents to take informed reproductive decisions, as well as alert the clinician about the carrier status. A limited number of studies identified that 7% (Verma et al. 2014) to 22% (Munshi et al. 2009) of anaemia cases was due to beta thalassaemia trait and 1.6% (Bhukhanvala et al. 2012) to 29.7% (Choubisa 1991) of anaemia was due to sickle cell carriers. These wide range of prevalence estimates were caused by non-random samples and different diagnostic criteria used in the studies. The aim of this study therefore was to determine the prevalence of undiagnosed haemoglobinopathy carriers among a random sample of pregnant women attending antenatal clinics in government hospitals in Pune city, India.
Materials and methods
Study design
The study genotyped a random sample of DNA that was biobanked as a part of the Pune Urban Birth Outcome Study (PUBOs) (Bhide et al. 2016). PUBOs was a cohort study to measure the birth prevalence of congenital anomalies and other adverse foetal outcomes. The study recruited 2107 pregnant women at 11 ± 3 weeks of gestation registering for antenatal care (ANC) at four government hospitals in Pune city, India. Pune is the second largest city in the western Indian state of Maharashtra, with a population of nearly five million in 2011. Data on socio-demographic characteristics, nutritional status (anthropometric measurements and haemoglobin levels at registration and before delivery), lifestyle factors, existing maternal health conditions and obstetric history was collected (Gund et al. 2016). Women were followed up till birth outcome. Blood samples of 1726 pregnant women were collected at baseline after informed consent, anonymized, coded and de-linked from the clinical data prior to banking of the samples. DNA was extracted, quantified, coded and banked as has been published elsewhere (Bhide et al. 2016).
Samples and sampling
A 4% prevalence of beta thalassaemia carriers was used based on earlier studies (Choubisa 2006; Patel et al. 2012; Mohanty et al. 2013). Using an online calculator (Naing et al. 2006), the sample size was calculated to be 360. These 360 samples were drawn from the 1726 banked samples, using the random number generation method in MS Excel. Sample codes were used to retrieve data on socio-demographic characteristics of pregnant women, haemoglobin levels, clinical and pregnancy outcome from the PUBO data set. Anthropometric data was used to categorize women as being underweight, normal or overweight based on their body mass index (BMI).
Anaemia classification and haemoglobin change
Classification of women into different categories of anaemia (severe, moderate and mild anaemia) was based on their haemoglobin levels using the WHO classification (World Health Organization 2011). This classification is also used in the Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCHA+) programme in India. Haemoglobin change between first trimester and at term was compared between carriers and non-carriers receiving IFA supplementation. A change in haemoglobin level was defined as differences of more than 0.5 g/dL as measured at baseline (recruitment) and at delivery (Rao et al. 2017).
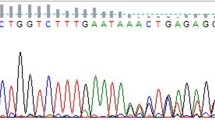
Mutation analysis
DNA samples were analysed for the presence of six common mutations causing beta thalassaemia in western India and for mutations causing HbE disorder and sickle cell anaemia (Sinha et al. 2009). Mutation analysis was done using the Amplification Refractory Mutation System Polymerase Chain Reaction (ARMS PCR) (Old et al. 1990) for the mutations IVS 1–5 (G➔C), Cd8/9 (+G), Cd 41/42 (-TCTT), IVS 1-1 (G➔T), Cd 15 (G➔A) and 619 bp del causative for beta thalassaemia, Cd 6 (A➔T) mutation (HbS variant causing sickle cell anaemia) and the Cd 26 (G➔A) mutation (HbE variant causing HbE disorder) as has been reported previously from Maharashtra, India (Mohanty et al. 2013).
A 20-μL PCR reaction was set up using the TopTaq Master Mix kit (Qiagen, Germany) with 1X PCR MasterMix (containing PCR buffer, 1.5 mM MgCl2, 200 μM dNTPs and 1.25 U TopTaq polymerase), 1X Coralload buffer, 0.5 pM/μL primers and 100–200 ng/μL of DNA. Amplification was done for 25 cycles at 94 °C for 1 min, 65 °C for 1 min and 72 °C for 1.5 min in a PCR thermocycler (Eppendorf MasterCycler, Germany). Subsequently, 10 μL of amplification product was electrophoresed in a 1.5% gel at 50 V/cm and stained in 0.5 μg/mL ethidium bromide. The gel was visualized, stored and analysed using the BioRad Gel Doc XR+ system (Bio-Rad Laboratories, USA). A negative control was set up with each reaction. After PCR amplifications of every 30 samples, the primers were checked for specificity by setting up a reaction with DNA from an individual who did not have the mutation causing beta thalassaemia. A random number of samples were re-amplified to determine the reliability of the results.
Data analysis
Carrier prevalence was calculated as the proportion of DNA samples heterozygous for a haemoglobin mutation to the total number of pregnant women. Means were presented with 95% confidence intervals (CI). Odds ratios (OR) with 95% confidence intervals were computed in order to determine if there was any association of carrier status with socio-demographic characteristics, nutritional, haematological, clinical characteristics and pregnancy outcomes. Change in haemoglobin levels was examined using a paired t test and OR was computed between change in haemoglobin levels and carrier status. p values less than 0.05 were considered to be statistically significant. Statistical Package for Social Sciences version 22 was used for statistical analysis.
Ethical considerations
Due to the ethical issues associated with identification of thalassaemia carriers in the prenatal period, the study was conducted using anonymous samples from pregnant women, approximately 1 year after the sample had been biobanked. During recruitment, each participant in the PUBO study was explained in detail regarding the study and consent was obtained to use the DNA sample for academic research. The study was approved by the Institutional Ethics Committee of Savitribai Phule Pune University.
Results
Characteristics of study population
The mean age of the 360 women whose DNA was analysed was 22.9 years (95% C.I. 22.5–23.3). Majority of women had greater than 10 years of education, were above the poverty line and belonged to the Hindu religion (Table 1). The prevalence of consanguinity was 20%, of which among non-carriers, 45/67 (67%) were first cousin marriages, 4/67 (6%) were second cousin marriages, 1/67 (1.5%) was a niece-uncle marriage and 17/67 (25%) could not give an adequate description of their relationship (or data on relationship not available). The only haemoglobinopathy carrier reporting consanguinity had a first cousin marriage. Majority of women had normal BMI and were nulliparous. There were 4% (16/360) women who reported having some chronic illness, 4% (16/360) women who had a bad obstetric history and 5% (17/360) women reported a relative with a birth defect (congenital locomotor, sensory or cognitive disability). None reported having a family history of a haemoglobinopathy. Majority of pregnancies resulted in live births. There were 5% (16) miscarriages and 3% (10) still births (Table 1).
Prevalence of haemoglobin mutations
The 360 DNA samples were screened for the six common mutations causing beta thalassaemia, and mutations causing sickle cell anaemia and HbE disorders (Table 2). Of these, 6% (23/360) samples were heterozygous for a HBB mutation. The most frequent mutation observed was the IVS1-5 (G➔C) mutation (39%, 9/23), followed by the Cd 26 (G➔A) mutation (26%,6/23), the Cd 6 (A➔T) mutation (22%, 5/23), the IVS 1-1 (G➔T) mutation (4%, 1/23), the Cd 8/9 (+G) mutation(4%, 1/23) and the Cd 15 (G➔A) allele (4%, 1/23) (Table 2).
Prevalence of haemoglobinopathy carriers
The DNA analysis indicated that the prevalence of undiagnosed haemoglobinopathy carriers was 6.3% (95% CI 4.2–9.4%). Prevalence of undiagnosed beta thalassaemia carriers was 3.3% (95% CI 1.9–5.7%), prevalence of undiagnosed sickle cell carriers was 1.7% (95% CI 0.8–3.6%) and the prevalence of undiagnosed HbE carriers was 1.4% (95% CI 0.6–3.2%) (Table 1). When data was disaggregated by type of haemoglobinopathy carriers, there was an increased odds that beta thalassaemia carriers belonged to the Scheduled Caste category (OR 4.13, 95% CI 1.01–16.92) (Scheduled Castes refer to officially designated underprivileged social groups). No such association was observed for sickle cell and HbE carriers. There was no association of carrier status with other socio-demographic characteristics that is age, education and economic level, consanguinity, body mass index, clinical characteristics and pregnancy outcomes.
Haemoglobin concentrations and changes during gestation
Majority of haemoglobinopathy carriers 80% (16/20) had anaemia, with 60% having mild anaemia (OR 3.54, 95% CI 1.11–11.27) (Table 1). Mean haemoglobin concentrations were not significantly different between non-carriers (10.5 g/dL; 95% CI 10.5–10.7) and haemoglobinopathy carriers (10.1 g/dL; 95% CI 9.8–10.5). However, disaggregated data identified a statistically significant difference between haemoglobin levels of beta thalassaemia carriers (9.5 g/dL; 95% CI 8.9–10.07) as compared to women who were not carriers (10.5 g/dL; 95% CI 10.5–10.7; p < 0.05). Beta thalassaemia carriers had higher odds of having moderate anaemia (OR 10.59; 95% CI 1.15–96.90) and the difference was statistically significant (p < 0.05).
Data on haemoglobin levels at first antenatal checkup (baseline, before IFA supplementation) and at term (after IFA supplementation) was available for 157 women (145 non-carriers and 12 carrier women). When analysed for change in haemoglobin levels post-supplementation, 27% non-carriers (40/145) and one carrier showed improvement in haemoglobin levels at term. There were 39% (58/145) non-carriers and 83% (10/12) haemoglobinopathy carriers who showed no change in haemoglobin levels after IFA supplementation (OR 1.82 95% CI 0.85–56.02) (Table 3).
Discussion
In light of the magnitude of nutritional anaemia among pregnant women in India, haemoglobinopathies are underprioritized as issues of public health concern. The findings of this study reiterate the need to immediately implement carrier screening, as 6.6% of a random sample of pregnant women attending government antenatal clinics were found to be haemoglobinopathy carriers. The estimates are consistent with beta thalassaemia carrier prevalence from other studies (Colah et al. 2010, 3%; Bhukhanvala et al. 2012, 3.2%; Bhukhanvala et al. 2013, 3.4%; Mohanty et al. 2013, 3.7%). The study detected 1.7% prevalence of undiagnosed carriers of sickle cell anaemia, even though this condition is considered to be predominantly prevalent in the tribal regions in India. Earlier studies have reported a wide range of prevalence estimates, from 0.7% in urban areas (Mohanty et al. 2013) to as high as 14% from tribal areas (Mohanty et al. 2015). The study also identified HbE carriers, even though the highest proportion of such carriers have been previously reported from eastern (4% carrier prevalence) and north-eastern (24% carrier prevalence) India (Mohanty et al. 2013). These results underline the widespread nature of these conditions in the country. As compared to their previously assumed localized prevalence, the data from this study indicates that these conditions are widespread, urging the need to implement carrier screening as a part of antenatal care services for all women presenting for ANC. It is noteworthy that India reports 25 million pregnancies annually (Ministry of Health and Family Welfare. Government of India. 2020), so that the number of carriers is likely to be considerable.
Carrier screening through a national service (that is a community genetics service) can empower individuals and provide information for better patient management. Carrier screening with the goal of prevention and control is however associated with several ethical issues. Beta thalassaemia prevention programmes are implemented in countries where this disorder is a public health problem (Goonasekera et al. 2018). Community genetic interventions have been successful in reducing the incidence of beta thalassaemia major in several of these countries (Firdous et al. 2011; Saffi and Howard 2015; Goonasekera et al. 2018). Thalassemia carrier screening programmes may be voluntary or mandatory, and the screening may be conducted prior to pregnancy, or in the antenatal period. The timing of the screening programme is usually influenced by availability of abortion services, and the acceptability of the programme by cultural leaders and the community at large (Cousens et al. 2010).
Indian guidelines propose carrier screening with the implicit purpose of prevention of haemoglobinopathies (Ministry of Health and Family Welfare. Government of India 2016). This approach appears to be an obvious solution to the lack of care for patients with haemoglobinopathies in India (Modell 2020; Sinha et al. 2020). Beyond the ethical issues underlying such assumptions, the national guidelines discuss the issue of timing of carrier screening to minimize psychosocial risk. Several large studies that have screened school and college students across the country have demonstrated that premarital screening is ineffectual if not supported with appropriate community knowledge on the benefits of screening. A study reported that majority of the respondents screened during high school did not remember or reveal their carrier status to their spouse when followed up after 20 years (Colah et al. 2007). Screening in the antenatal period is another possibility, but needs to be carefully implemented as termination of pregnancy is permitted till 24 weeks of gestation (Government of India 2020). The national guidelines do not make antenatal screening mandatory, thereby respecting the autonomy of beneficiaries.
Ethical implementation of the carrier screening programme is however largely dependent on policy makers, planners and public health service staff. The sickle cell programme of several states of India has a highly unethical practice of providing coloured cards to carriers as a part of marriage counselling. The card, which carries a high risk of stigmatizing the individual, is purported to be an appropriate intervention in poorly literate communities for discouraging marriage between two carriers (State Health Society Government of Gujarat 2020; State Health Society Maharashtra 2020). Such practices indicate that programme managers and staff involved in carrier screening programmes need to be sensitized on issues of ethics, and the autonomy and right of women to choose whether to get themselves tested or not (Tamhankar et al. 2009). As a first step, however, the national policy will alert state governments on the need to keep in mind ethical considerations while implementing haemoglobinopathy prevention and control programmes.
The cost of screening pregnant women across India versus the benefits to public health investment may be debated. Screening need not be an expensive activity. A complete blood count can be the first step for identifying at-risk individuals through public health programmes. Subsequently, carriers can be diagnosed by HbA2 analysis or mutation analysis. The technical capacity for diagnostic testing of haemoglobinopathies is well in place in India at government hospitals and government research institutes. A clearly laid out referral pathway for diagnostic testing needs to be put in place as a component of a well-organized genetic counselling service (Phadke et al. 2017). A recent study estimates that the cost of a screening programme is less than 4% of the cost required for treatment of patients (Sinha et al. 2020).
One of the observations of this study was that administration of IFA for 100 days had no impact on reducing anaemia in carriers. However, it needs to be pointed out that the observation was limited by the small number of carriers for whom changes in haemoglobin level was measured. Administration of IFA for 100 days is not likely to affect haemoglobinopathy carriers, and will address the issue of co-existing nutritional anaemia. At the same time, persistent anaemia in spite of adherence to IFA supplementation can serve as an indicator for further investigation. This is especially true for school aged children in India, who are provided weekly IFA under the anaemia control programme (Anaemia Mukt Bharat) (Ministry of Health and Family Welfare. Government of India. 2018). Carrier screening of all children with persistent anaemia would provide an opportunity for better management. Prolonged weekly iron therapy in this age group may require monitoring by estimation of haemoglobin, complete blood counts and serum ferritin to prevent the complications of iron overload.
Although the small sample size is a limitation of the study, the strengths of our study are that the samples were randomly selected, and all samples were genotyped for the six mutations that are prevalent in Western India, and the HbS and HbE mutations. Genotyping of these six mutations can detect nearly 90% of carriers, implying that our study may only slightly underestimate the prevalence of haemoglobinopathies. We were unable to report red blood cell indices and iron/ferritin levels, as these data were not collected in the PUBO study, which did not have haemoglobinopathy as its primary objective. Nevertheless, the data reported in this study identify the magnitude of the problem in India and the need for immediately implementing the national guidelines for prevention and control of haemoglobinopathies. As urgent is the need for carrier screening, it is essential to ensure at the same time that the services are implemented in an ethical manner, so that the programme does not impose on the autonomy of women registering for carrier screening. Sensitization of programme managers on ethical issues should be made an essential component of the national programme for prevention and control of haemoglobinopaties in India, so that health service staff are aware that well-intentioned programmes may have the potential of stigmatizing individuals and causing psychosocial harm.
References
Achoubi N, Asghar M, Saraswathy KN, Murry B (2012) Prevalence of β-thalassemia and hemoglobin E in two migrant populations of Manipur, North East India. Genet Test Mol Biomarkers 16:1195–1200. https://doi.org/10.1089/gtmb.2011.0373
Bhide P, Gund P, Kar A (2016) Prevalence of congenital anomalies in an Indian maternal cohort : healthcare, prevention, and surveillance implications. PLoS One 11:e0166408. https://doi.org/10.1371/journal.pone.0166408
Bhukhanvala DS, Sorathiya SM, Shah AP, Patel AG, Gupte SC (2012) Prevalence and hematological profile of β-thalassemia and sickle cell anemia in four communities of Surat city. Indian J Hum Genet 18:167–171. https://doi.org/10.4103/0971-6866.100752
Bhukhanvala DS, Sorathiya SM, Sawant P, Colah R, Ghosh K, Gupte SC (2013) Antenatal screening for identification of couples for prenatal diagnosis of severe hemoglobinopathies in Surat, South Gujarat. J Obstet Gynaecol India 63:123–127. https://doi.org/10.1007/s13224-012-0271-4
Choubisa SL (1991) Abnormal haemoglobins, thalassaemia and G-6-PD enzyme deficiency in Rajasthan (western-India). Haematologia (Budap) 24:153–165
Choubisa SL (2006) Erythrocyte mutant genes in inhabitants of arid-environment of Western Rajasthan (India). Indian J Phys Anthropol Hum Genet 25:15–30
Colah R, Thomas M, Mayekar P (2007) Assessing the impact of screening and counselling high school children for β-thalassaemia in India. J Med Screen 14:158. https://doi.org/10.1258/096914107782066202
Colah R, Gorakshakar A, Phanasgaonkar S, D’Souza E, Nadkarni A, Surve R, Sawant P, Master D, Patel R, Ghosh K, Mohanty D (2010) Epidemiology of beta-thalassaemia in Western India: mapping the frequencies and mutations in sub-regions of Maharashtra and Gujarat. Br J Haematol 149:739–747. https://doi.org/10.1111/j.1365-2141.2010.08131.x
Cousens NE, Gaff CL, Metcalfe SA, Delatycki MB (2010) Carrier screening for beta-thalassaemia: a review of international practice. Eur J Hum Genet 18:1077–1083. https://doi.org/10.1038/ejhg.2010.90
Dolai TK, Dutta S, Bhattacharyya M, Ghosh MK (2012) Prevalence of hemoglobinopathies in rural Bengal, India. Hemoglobin 36:57–63
Firdous N, Gibbons S, Modell B (2011) Falling prevalence of beta-thalassaemia and eradication of malaria in the Maldives. J Community Genet 2:173–189. https://doi.org/10.1007/s12687-011-0054-0
Goonasekera HW, Paththinige CS, Dissanayake VHW (2018) Population screening for hemoglobinopathies. Annu Rev Genomics Hum Genet 19:355–380. https://doi.org/10.1146/annurev-genom-091416-035451
Government of India (2020) The Medical Termination of Pregnancy (Amendment) Bill, 2020. https://www.prsindia.org/sites/default/files/bill_files/The%20Medical%20Termination%20of%20Pregnancy%20%28Amendment%29%20Bill%2C%202020.pdf. Accessed 5 Oct 2020
Gund P, Bhide P, Kar A (2016) Prevalence of periconception risk factors for adverse pregnancy outcomes in a cohort of urban Indian women: implications for preconception health education. J Women’s Heal Care 5:1–5. https://doi.org/10.4172/2167-0420.1000296
International Institute for Population Sciences (IIPS) and ICF (2017) National Family Health Survey (NFHS-4), 2015–16: India. IIPS, Mumbai
Kassebaum NJ, Fleming TD, Flaxman A, Phillips DE, Steiner C, Barber RM, Hanson SW, Moradi-Lakeh M, Coffeng LE, Haagsma J, Kyu HH, Graetz N, Lim SS, Vos T, Naghavi M, Murray C, Yonemoto N, Singh J, Jonas JB, Santos IS, Bensenor IM, Lotufo PA, Rana SM, Gessner BD, Ukwaja KN, Piel FB, Khader YS, Bhala N, Antonio CAT, Thrift AG, Mendoza W, Zaki MES, Larsson A, Nand D, Malekzadeh R, Li Y, Jin KY, Levy TS (2016) The global burden of anemia. Hematol Oncol Clin North Am 30:247–308. https://doi.org/10.1016/j.hoc.2015.11.002
Ministry of Health and Family Welfare. Government of India (2016) Prevention and control of hemoglobinopathies in india - thalassemias, sickle cell disease and other variant hemoglobins
Ministry of Health and Family Welfare. Government of India. (2018) Anaemia Mukt Bharat. https://anemiamuktbharat.info/home/6x6x6-strategy/. Accessed 5 Oct 2020
Ministry of Health and Family Welfare. Government of India (2020) Health Management Information System. https://nrhm-mis.nic.in/SitePages/Home.aspx. Accessed 5 Oct 2020
Modell B (2020) Haemoglobin disorders—a point of entry for community genetics services in India? J Community Genet 11:7–9. https://doi.org/10.1007/s12687-019-00441-8
Modell B, Darlison MW, Malherbe H, Moorthie S, Blencowe H, Mahaini R, El-Adawy M (2018) Congenital disorders: epidemiological methods for answering calls for action. J Community Genet 9:335–340. https://doi.org/10.1007/s12687-018-0390-4
Mohanty D, Colah RB, Gorakshakar AC, Patel RZ, Master DC, Mahanta J, Sharma SK, Chaudhari U, Ghosh M, Das S, Britt RP, Singh S, Ross C, Jagannathan L, Kaul R, Shukla DK, Muthuswamy V (2013) Prevalence of β-thalassemia and other haemoglobinopathies in six cities in India: a multicentre study. J Community Genet 4:33–42. https://doi.org/10.1007/s12687-012-0114-0
Mohanty D, Mukherjee MB, Colah RB, Wadia M, Ghosh K, Chottray GP, Jain D, Italia Y, Ashokan KS, Kaul R, Shukla DK, Muthuswamy V (2015) Spectrum of hemoglobinopathies among the primitive tribes: a multicentric study in India. Asia-Pacific J Public Heal 27:NP562–NP571. https://doi.org/10.1177/1010539513480231
Munshi A, Anandraj MPJS, Joseph J, Shafi G, Anila AN, Jyothy A (2009) Inherited hemoglobin disorders in Andhra Pradesh, India: a population study. Clin Chim Acta 400:117–119. https://doi.org/10.1016/j.cca.2008.10.025
Naing L, Winn T, Rusli BN (2006) Sample size calculator for prevalence studies. Arch Orofac Sci 1:9–14
Old JM, Varawalla NY, Weatherall DJ (1990) Rapid detection and prenatal diagnosis of beta-thalassaemia: studies in Indian and Cypriot populations in the UK. Lancet 336:834–837. https://doi.org/10.1016/0140-6736(90)92338-i
Patel AG, Shah AP, Sorathiya SM, Gupte SC (2012) Hemoglobinopathies in South Gujarat population and incidence of anemia in them. Indian J Hum Genet 18:294–298. https://doi.org/10.4103/0971-6866.107979
Phadke SR, Puri RD, Ranganath P (2017) Prenatal screening for genetic disorders: suggested guidelines for the Indian scenario. 689–699 . https://doi.org/10.4103/ijmr.IJMR
Rao S, Joshi S, Bhide P, Puranik B, Asawari K (2017) Dietary diversification for prevention of anaemia among women of childbearing age from rural India. 17:939–947. https://doi.org/10.1017/S1368980013001006
Saffi M, Howard N (2015) Exploring the effectiveness of mandatory premarital screening and genetic counselling programmes for β-thalassaemia in the Middle East: a scoping review. Public Health Genomics 18:193–203. https://doi.org/10.1159/000430837
Sarna A, Porwal A, Ramesh S, Agrawal PK, Acharya R, Johnston R, Khan N, Sachdev HPS, Nair KM, Ramakrishnan L, Abraham R, Deb S, Khera A, Saxena R (2020) Characterisation of the types of anaemia prevalent among children and adolescents aged 1–19 years in India: a population-based study. Lancet Child Adolesc Heal 4:515–525. https://doi.org/10.1016/S2352-4642(20)30094-8
Sinha S, Black ML, Agarwal S, Colah R, Das R, Ryan K, Bellgard M, Bittles AH (2009) Profiling β-thalassaemia mutations in India at state and regional levels: implications for genetic education, screening and counselling programmes. HUGO J 3:51–62. https://doi.org/10.1007/s11568-010-9132-3
Sinha S, Seth T, Colah RB, Bittles AH (2020) Haemoglobinopathies in India: estimates of blood requirements and treatment costs for the decade 2017–2026. J Community Genet 11:39–45. https://doi.org/10.1007/s12687-019-00410-1
State Health Society Government of Gujarat (2020) Gujarat nhm.pdf. https://nhm.gujarat.gov.in/sickle-cell.htm. Accessed 9 Dec 2020
State Health Society Maharashtra (2020) Maharashtra NHM.pdf. https://www.nrhm.maharashtra.gov.in/nrhm/sickle.htm. Accessed 9 Dec 2020
Tamhankar PM, Agarwal S, Arya V, Kumar R, Gupta UR, Agarwal SS (2009) Prevention of homozygous beta thalassemia by premarital screening and prenatal diagnosis in India. Prenat Diagn 29:83–88. https://doi.org/10.1002/pd
Verma S, Talukdar B, Gupta R (2014) ‘Reflex’ HPLC testing as a screening modality for variant hemoglobins : a pilot study of 1310 cases at a pediatric referral hospital. Hematology 19:299–303
Weatherall DJ, Clegg JB (2008) Distribution and population genetics of the thalassaemias. In: Weatherall DJ, Clegg JB (eds) The Thalassaemia syndromes, 4th edn. Wiley, Oxford, pp 237–284
World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. http://www.who.int/vmnis/indicators/haemoglobin. pdf,. Accessed 5 Oct 2020
Acknowledgements
The authors gratefully acknowledge the anonymous reviewers for their comments. We acknowledge the assistance of Pooja Gund and Lipi Joshi in the study.
Funding
INSPIRE fellowship from the Department of Science and Technology to SD.
Author information
Authors and Affiliations
Contributions
SD designed the study, analysed the DNA, collated and cleaned the data sheets, linked the data, analysed the data and drafted the manuscript; AP undertook mutation analysis of some of the samples; PB isolated the DNA and was responsible for collection of the PUBO data; AK conceptualized and supervised the study, shared the anonymized data and biobanked samples, monitored the analyses and wrote the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all patients for being included in the study. This study was approved by the Institutional Ethics Committee of Savitribai Phule Pune University. This article does not contain any studies with animals performed by any of the authors. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Consent was taken from each participant for use of their data for academic research.
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dharmarajan, S., Pawar, A., Bhide, P. et al. Undiagnosed haemoglobinopathies among pregnant women attending antenatal care clinics in Pune, India. J Community Genet 12, 337–344 (2021). https://doi.org/10.1007/s12687-021-00505-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-021-00505-8



