Abstract
Carriers of haemoglobin disorders have protection against falciparum malaria. Therefore, where this is common, carrier prevalence rises until this selective advantage is offset by deaths of affected children. Theory predicts a corresponding fall in carrier frequency following malaria eradication, but this has not been reported in practice. In the Maldives, malaria eradication (in 1972–1975) unmasked highly prevalent beta-thalassaemia and led to services for patient care and outreach carrier screening. Analysis of 68,986 laboratory screening records for subjects born between 1960 and 1990 showed carrier prevalences ranging from 10.1% to 28.2% by atoll (related to the prevalence of falciparum malaria before eradication) and a steady fall in average carrier prevalence from 21.3% among those born in 1970 to 16% in those born in 1989. Data for individuals born before 1970 suggest that earlier, when malaria was uncontrolled, carrier prevalence was 23–25%. The observed fall in carrier prevalence was broadly consistent with a model based on genetic theory, allowing for the heterogeneous distribution of carrier prevalence and the potential contribution of consanguineous marriage. The possible effects of population mixing and reproductive compensation were calculated, and any contribution to falling carrier prevalence was excluded. It is concluded that the observed fall in thalassaemia carrier prevalence in the Maldives is consistent with the predicted effect of malaria eradication and supportive of the population genetic theory. The observed fall in average carrier prevalence corresponds to a fall in minimum affected birth prevalence from approximately 12/1,000 in 1970 to approximately 6.9/1,000 in 2007. Allowing for this effect, the National Thalassaemia Register has documented a more than 60% fall in affected birth prevalence since outreach population screening was established in 1997. The main contributing factors are considered to be limitation of final family size by informed at-risk couples and utilisation of prenatal diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Haemoglobin disorders (thalassaemias and sickle cell disorders) offer the best-known example of a “balanced polymorphism”, where a common gene variant provides carriers with a selective advantage but is lethal in homozygotes (Haldane 1949; Allison 1954; Raper 1956; Luzzatto 1979; Weatherall 2008). Carriers of haemoglobin disorders have protection against dying from falciparum malaria. Therefore, where this is common, excess mortality among non-carriers drives carrier prevalence upwards until variant genes leave the population equally rapidly through deaths of affected children (Haldane 1949; Livingstone 1967; Harris 1970; Bodmer and Cavalli-Sforza 1976; Clegg and Weatherall 1999; Weatherall 2008). Thus, the prevalence of haemoglobin disorders in a population is considered to reflect past or present malaria mortality (Livingstone 1967).
When malaria is eradicated, the differential mortality of non-carriers is abolished, but variant genes continue to leave the population if homozygotes still die early or fail to reproduce. Carrier prevalence of a lethal recessive variant is therefore predicted to fall, as in Fig. 1 (Livingstone 1967; Harris 1970; Bodmer and Cavalli-Sforza 1976), but this has not so far been observed in practice. This article reports falling beta-thalassaemia carrier prevalence in the Maldives, where malaria was eradicated in the early 1970s.
Predicted fall in the birth prevalence of carriers of a lethal recessive with heterozygote advantage when selection pressure is removed, calculated using the Hardy–Weinberg equation. Conventionally, a generation is around 20 years. A starting carrier prevalence of 24% has been chosen as this appears close to the original average carrier prevalence in the Maldives. The upper curve shows the prediction for random mating (coefficient of consanguinity, F = 0.00). The bottom curve shows a hypothetical maximum rate of fall (F = 0.065, equivalent to 100% first cousins). The middle curve shows an intermediate rate when F = 0.03, a relatively common value (Bittles 1990)
The Republic of Maldives consists of a string of 21 coral atolls including over 1,000 islands in the Indian Ocean west of Sri Lanka. They are well known to mariners since ancient times as a dangerous barrier to be crossed safely only through three well-defined channels. The population is now over 300,000 (UN Demographic Yearbook 2008), 27% located on the capital island Malé and the rest scattered through 200 of the islands. Islam is the national religion. Education and health services are well developed, infant mortality is 14/1,000, literacy is high, and average final family size fell from 6.8 to 2.8 between 1990 and 2000 (UN Demographic Yearbook 2008). Despite advances in communication by sea, air, mobile phone and the Internet, inter-island travel remains time-consuming, difficult and often dangerous, and most marriages still take place within island communities. The prevalence of consanguineous marriage has not been documented: It is likely to be common, but there is no cultural preference for it.
Until the early 1970s, malaria (including falciparum malaria) was hyper-endemic. At that time, chloroquine was administered by island health workers and island chiefs (Schepens 1980), but vector control was limited outside Malé and Addu atoll, which hosted a British air base. Falciparum malaria was eradicated between 1972 and 1974 and no indigenous case has been reported since, though other types of malaria persisted somewhat longer (Cardenas 1985)
Malaria eradication unmasked a high prevalence of beta-thalassaemia major, as also recorded in Cyprus (Banton 1951). However, most affected children died because the limited facilities for treatment were inaccessible for most of the population (Modell et al. 1990). The situation changed radically in 1994 when a National Thalassaemia Centre was established to provide treatment, including regular blood transfusions and iron chelation therapy, for all patients according to international standards (Firdous 2005; UK Thalassaemia Society 2005). There are now few early deaths, and by the end of 2007, there were 444 living registered patients.
The Society for Health Education (SHE), a non-governmental organisation, was the first to highlight the true scale of the thalassaemia problem and advocate carrier screening and genetic counselling. Most existing screening programmes for haemoglobin disorders offer carrier testing premaritally or during pregnancy and include the option of prenatal diagnosis (Alwan and Modell 2003). However, three considerations led SHE to focus on early information and voluntary testing for young people, as practised in Montreal (Zeesman et al. 1984). (1) Young people need to learn about their carrier status early enough to consider all available options, including marriage and undertaking a pregnancy. (2) In the Maldives, physical barriers dictate that testing can only be offered at 5-year intervals, rather than opportunistically before marriage or starting a pregnancy (Firdous 2005). (3) Prenatal diagnosis was not seen as an option for an Islamic community at the time—but the molecular basis for β-thalassaemia was studied to assess its future feasibility (Furumi et al. 1998).
SHE initiated a programme of education, voluntary carrier screening and genetic counselling for school leavers (grade 10) in Malé in 1992. Next, the offer of testing was extended to anyone of pre-reproductive or reproductive age. Finally, in 1997, SHE activated a strategic outreach screening programme for the whole population (Firdous 2005). By 2002, all 200 islands had been covered. A second cycle was completed in 2007, and over 65% of Maldivians aged 16–45 years of age have now been tested.
An increasing demand for prenatal diagnosis emerged as the screening programme unfolded, and advocacy with governmental and religious authorities led to the release in 1999 of a fatwa permitting abortion for severe foetal abnormality (Firdous 2005), as earlier in Pakistan (Ahmed et al. 2000) and Iran (Samavat and Modell 2004). A DNA laboratory is already functioning, and prenatal diagnosis will be routinely available when local obstetricians are able to provide chorionic villus sampling.
In order to micro-map service needs and assess the impact of carrier screening, we reviewed laboratory records for the entire first screening round (1997–2002) and part of the second round, plus data from the National Thalassaemia Register. The analysis revealed rapidly falling carrier prevalence, and a marked reduction in affected birth prevalence since outreach screening was started.
Methods
Population screening
An outreach team of seven to eight people, including volunteers, conduct 10 to 12 field trips annually, each lasting 2 to 3 days and covering five to seven islands (Firdous 2005). Each island visit starts with an information session in the school. The primary targets are those aged 12–35 years, but it is emphasised that testing is important for anyone planning to have (further) children, and anyone can request it. Blood is collected on the spot, and samples are taken directly to the laboratory in Malé.
Full blood count, high-performance liquid chromatography (HPLC, Bio-Rad) and blood morphology are done on all samples according to international standards (BCSH 1998). Beta-thalassaemia carriers are diagnosed by microcytosis (MCH <27 pg) plus haemoglobin A2 ≥ 3.5%. Haemoglobin variants are typed using HPLC. Electrophoresis, DNA analysis and other tests are done when indicated. Each person’s results are placed in a sealed envelope with a laminated result card, and batches are hand-carried to each island. Carriers receive an information sheet and an invitation to telephone the laboratory (free of charge for the islands). Carrier couples receive genetic counselling face-to-face in Malé or by telephone in the islands. Laboratory findings, age, sex and island of residence for each participant are recorded in a Microsoft Excel database.
Analysis of laboratory data
The Ministry of Health gave ethical permission for a study of laboratory screening records. After an age gradient in carrier prevalence was noted among the 62,007 subjects in the first screening round (to 2002), additional records for 6,820 subjects from the second screening round and 1,973 subjects born before 1966 were included in order to increase numbers in the youngest and oldest age groups.
Uptake of testing, carrier prevalences and gene frequencies were calculated by island, atoll and the whole country, and by sex and age. Service requirements (Modell and Darlison 2007) were calculated by island using 1995 census data.
Potential birth prevalence (i.e. prevalence in the absence of intervention) of non-carriers, carriers and affected infants were calculated from observed gene frequencies by island, atoll and the whole country using the Hardy–Weinberg equation (Bodmer and Cavalli-Sforza 1976). The basic equation is \( {p^2} + 2pq + {q^2} = 1 \)where p and q are the “wild-type” and variant gene frequencies among parents, respectively. The equation is modified as follows to allow for effects of parental consanguinity\( \left( {{p^2} + Fpq} \right) + 2\left( {pq-Fpq} \right) + \left( {{q^2} + Fpq} \right) = 1 \)where F is the population coefficient of consanguinity (the additional proportion of gene pairs that are homozygous by descent, calculated from observed parental relationships).
With entirely random mating, F = 0. An F of 0.0625, equivalent to 100% first cousin marriage, may be taken to represent a notional upper limit. A coefficient of consanguinity of 0.025–0.03 is common in the Middle East (Bittles 1990), and F = 0.0412 among British Pakistanis and in Pakistan (Bundey et al. 1990; Ahmed et al. 2002). Parental consanguinity is clearly common in the Maldives, though no formal evaluation has been made. Therefore, when indicated, in the absence of observational data, calculations were made for F = 0, F = 0.03 and F = 0.0625.
The relationship between year of birth and carrier prevalence was investigated using the nonparametric Nadaraya–Watson kernel regression estimator (Hardle 1992). Data for subjects born between 1960 and 1990 were analysed to show the trend in carrier probability in relation to year of birth. The kernel regression shows the weighted average carrier probability computed from subjects born in and close to a sequence of predetermined birth year grid points. These grid points were set at 1-year intervals between 1960 and 1990 and the regression estimated using a Gaussian kernel weighting function with bandwidth set to 1 year. Weights are also applied such that the distribution of the sample size across atolls for each age cohort corresponds to the population distribution from the census in 1995. Upper and lower 5% confidence bands were computed by bootstrap resampling, with 100 repetitions. Estimation was implemented using a modified “kernreg” algorithm in STATA 11.0.
Other data
For demographic data, population numbers by sex and island and atoll of residence are from the national 1995 census. Maternal age distributions are from the United Nations Demographic Yearbook series (UN Demographic Yearbook 1997, 2008). Total fertility rates are from UN Population Prospects (UNPP 2008). Atoll-specific malaria prevalence before eradication is from the report of the Maldivian Malaria Eradication Programme (Schepens 1980). Patient numbers and years of birth are from the National Thalassaemia Register maintained by the National Thalassaemia Centre.
Results
Carrier prevalences
The study dataset included 70,800 subjects aged 12 years or more at testing, the youngest being born in 1990. After review, 1,814 records (2.6%) were excluded because a piece of data was missing or mis-entered, leaving 68,986 records for analysis. These included 26% of the Maldivian population and 44% of those born between 1970 and the end of 1990.
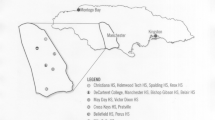
The proportion of the population tested varied by atoll from 13.8% (Fuvamula) to 40.1% (Malé atoll; Table 1). Average carrier prevalence was 19.0% (17.2% β-thalassaemia, 1.8% haemoglobins D, E and S), but carriers were heterogeneously distributed, with prevalence ranging from 0% to 41% by island and from 8.9% to 27.1% by atoll (Table 1 and Fig. 2). Atoll prevalence is correlated with the pre-eradication prevalence of falciparum malaria (Schepens 1980; Fig. 3).
The Republic of the Maldives covers a sea area 823 × 135 km. Total prevalence of beta globin gene variants by island. The 201 islands inhabited at the time of the study are shown—one was abandoned following the 2005 tsunami. There is a clear north and east to south and west gradient in total prevalence, with substantial inter-island differences. All variants are found in Malé (total prevalence = 19.9%). No variant was detected on two islands with 108 and 113 residents. Beta-thalassaemia was found on all other islands, Hb E was also present on 70 (maximum 23%) and Hb D was present on 34 (maximum 8%). Hb S was found on 14 islands in low prevalence (e.g. 0.3% in Male) and in 7.5% of the population of the island of Thoddoo (North Ari atoll)
Relationship between the proportion of children 2–9 years old with Plasmodium falciparum parasites in their blood in 1970–1974 and present prevalence of carriers of haemoglobin disorders in the Maldives, by atoll. The coefficient of correlation is 0.61. Successful pilot spraying programmes were carried out in Malé (box 1) and Malé atoll (box 2) in 1966. Malaria was also under control in Addu atoll (box 3) which hosted a British airbase (4). When these atolls are excluded, the coefficient of correlation is 0.67
When data were examined by subjects’ year of birth, a steady fall in carrier prevalence was observed (Table 2). This was the case when data were analysed by atoll as well as for the whole country. The Nadaraya–Watson statistical analysis, adjusted for geographical sampling bias, confirmed a highly significant overall trend from 25% carrier prevalence among subjects born in 1965 to 16% among those born in 1988–1989 (Fig. 4).
Observed and expected affected birth prevalences
The National Thalassaemia Register was initiated in 1993 and was considered to have achieved complete ascertainment by 2001. Table 3 shows the number of new cases recorded from 1993 to the end of 2007.
It was possible to calculate expected affected births for the period 1993–2007 because women bearing children in these years were (broadly speaking) born in 1967–1981, and this period is included in the study of carrier prevalences (see Table 2). Table 3 includes expected affected births for 1993–2007 calculated from maternal carrier prevalences for F = 0.0 and 0.03. The 50% fall (from 122 to 58) in the 8 years 1993 to 2000 inclusive reflects an approximately 25% fall in parental carrier prevalence plus a 37% fall in total annual births. Since then, a modest increase in annual births has balanced the continuing fall in parental carrier prevalence, and potential affected births have settled at 50–60 per year.
The proportion of observed to expected affected births rose from 17–21% in 1993 to 65–83% in 2001, reflecting improving ascertainment. Since 2001 (when patient registration was considered near-complete), there have been on average 20 affected births per year, 33–42% of expectation (Table 3 and Fig. 5).
Expected annual new cases by years 1997–2007 compared with observed new cases (3-year rolling averages). Only years where the mother’s year of birth is estimated to be 1971 or later are included to avoid possible selection bias in earlier years. Expected annual new cases are calculated for coefficients of consanguinity of 0.00 and 0.03. The sharp fall in expected new cases between 1997 and 2001 reflects both falling crude birth rate (26/1,000 in 1996 to 21.5/1,000 by 2007 (UN Demographic Yearbook series) and an estimated fall in carrier prevalence among mothers from 20.6% in 1997 to 18.3% in 2007 (see Table 2). The Maldivian Thalassaemia Register was initiated in 1993. The initial increase in the proportion of estimated cases reflects increasing ascertainment. Ascertainment was considered near-complete by 2000, and the first 5-year round of outreach information, screening and counselling was completed by 2002. Since then, the annual number of new cases has been constant at approximately 20 per year. This corresponds to between 30% and 40% of expectation, depending on the assumed population coefficient of consanguinity
Discussion
The observations of falling carrier prevalence and falling thalassaemia major birth prevalence are discussed separately.
Falling carrier prevalence
The first question is how reliable are the findings? Here, we consider the possibility of three types of bias.
Exclusion bias
The exclusion of 1,814 incomplete records did not introduce bias: Carrier prevalence fell with year of birth in the same way in the excluded group and in the main study.
Geographical bias
Since carrier prevalence differs by atoll and island, differential representation of atolls or islands could introduce bias when calculating average country carrier prevalence. All atolls were reasonably proportionately represented in the study (Table 1). This was also true for all age groups except the youngest, those born in 1990: Higher prevalence atolls were overrepresented in this group because the data came from the second screening round, which was incomplete at the time.
In calculating average country prevalence, geographical bias can be corrected by adjusting for the proportion of the population resident in each atoll. All calculations of age-related carrier prevalence were adjusted for geographical bias at the atoll level, according to the population distribution in the Maldivian 1995 census. This adjustment tends, if anything, to increase average carrier prevalence in the oldest groups (born before 1965), makes little difference for those born 1965–1989 and lowers the anomalously high carrier prevalence in those born in 1990 (Table 4).
Self-selection bias
The fact that screening is voluntary could introduce bias, e.g. if relatives of children known or suspected to have thalassaemia present selectively for screening. The possible effect of family bias is influenced by the proportion of each group tested, general carrier prevalence and local kinship pattern.
Self-selection bias is unlikely for subjects born between 1970 and 1989 (88% of the total) because over half of this age group were tested (Table 5). In an extreme scenario in which this group included all eligible relatives of all affected children, observed carrier prevalence might rise by 2–3% (see Electronic supplementary material (ESM) Fig. 1), but this would not alter the observed trend in prevalence. This scenario is in fact unlikely because the programme emphasises the importance of screening for all young people. It is therefore reasonable to accept observed prevalences as representative for the large 1970–1989 age group.
The same considerations may not apply for the smaller “pre-eradication” group aged 35 plus at testing. As the screening programme specifically targets younger people, older subjects may have particular reasons for requesting testing. The observed sex ratio suggests one type of bias. Table 5 shows that at pre-reproductive age, more females than males present for testing (a usual finding), the sex ratio is balanced in those of conventional reproductive age (reflecting the thrust of the programme), but males preponderate in the oldest group (an unusual finding). This observation suggests that testing was sought selectively by older men starting a second family (divorce is common in the Maldives), but this type of bias should not affect observed carrier prevalence. However, selective presentation of older relatives of affected children has not been excluded, so observed carrier prevalences in the older age group should be viewed with some reservations.
Since there is no evidence of bias for subjects born in 1970–1989, including the “post-eradication” group born 1974–1989, observed carrier prevalences in this group may be compared with those predicted by population genetic theory.
Population genetic theory
A balanced polymorphism is the product of two opposing types of selection: loss of variant genes through the deaths of homozygotes and loss of wild-type genes through excess deaths of wild-type homozygotes (from falciparum malaria in the present case).
For example, when 19% of the population carry a significant beta-globin gene variant and almost no homozygotes survive to reproduce (as in the Maldives at present), variant gene frequency (q) = half the carrier frequency (0.19) = 0.0950 and “wild-type” gene frequency (p) = 0.9050. Using the Hardy–Weinberg equation, the expected genotype distribution among offspring, with random mating, is:
-
q2 = 0.00903 = affected birth prevalence 9.03/1,000 (i.e. 1.8% of variant genes are “lost” per generation)
-
2pq = 0.172 = carriers 17.2% (10% less than parents)
-
p2 = 0.819 = 81.9% homozygous “wild type” (1.14% more than parents)
A return of carrier prevalence from the neonatal to the parental level requires the early deaths of 10.5% of non-carrier offspring (=8.6% of all offspring) from malaria.
Parental consanguinity increases the birth prevalence of both types of homozygote at the expense of heterozygote birth prevalence, and so increases the intensity of both types of selection. Corresponding rates for 19% carriers when F = 0.03 are:
-
Affected 11.6/1,000 (i.e. 2.3% of variant genes lost per generation)
-
Carriers 16.7% (12.3% less than parents)
-
Non-carriers 82.2% (1.46% more than parents)
In this case, a return of carrier prevalence to the parental level would require the early deaths of 13.5% of non-carrier offspring (=11.1% of all offspring) from malaria.
This study suggests a carrier prevalence of at least 23% in the Maldives in the recent past. This corresponds to 13% excess mortality among non-carriers (10.2% for the whole population) with random mating, or 15.9% excess mortality among non-carriers (12.5% for the whole population) when F = 0.03.
The restoration of adult carrier prevalence can be very rapid. When falciparum malaria is endemic, newborns are protected by maternal immunity for the first few months. Observations on haemoglobin S in rural Africa have shown that after this, non-carrier (AA) children either die or develop immunity and adult carrier (AS) prevalence is restored before 5 years of age (Allison 1954; Fleming et al. 1979; Bradley 1991): Frequent re-exposure is required to maintain immunity (Allison 1954).
Excess mortality is reduced by anti-malaria measures and definitively halted by malaria eradication. Eradication therefore divides a population into two groups: a pre-eradication group in which excess deaths of non-carriers raised carrier prevalence from the neonatal level to the adult level over an indeterminate number of years and a post-eradication group in which carrier prevalence at birth persists life-long. If the condition remains lethal in homozygotes (as with thalassaemia in the Maldives until very recently), carrier prevalence will fall progressively in subsequent generations due to loss of genes in affected homozygotes (see Fig. 1). The rate of fall is exponential because homozygote birth prevalence is related to the square of carrier frequency. How do the present observations relate to these predictions?
The present observations
Since Maldivians born after 1974 were never exposed to falciparum malaria, carrier prevalence at birth is expected to persist life-long. It is therefore possible to estimate affected birth and carrier prevalences among the parents and future offspring of the 1973–1989 birth cohort (the “anchor cohort”) using the Hardy–Weinberg equation. Table 6 shows the results assuming a coefficient of consanguinity of 0.03 (for calculations for F = 0 and F = 0.0625, see ESM Table). Despite its crudeness, this calculation makes it possible to relate carrier prevalence to year of birth from 1953 to 2009—a span of more than 50 years. It indicates a steady rise in carrier prevalence from 19–20% in Maldivians born in 1973 to 23–24% in those born 20 years earlier (1959) and a steady fall from 16.8% among those born in 1990 to 14–15% among those born 20 years later.
Figure 6 compares observed carrier prevalences with calculated carrier prevalences based on the anchor 1973–1989 birth cohort. The calculation tends to flatten the curve of changing carrier prevalence somewhat, yielding lower carrier prevalences in the older group and marginally higher carrier prevalences in the younger age group. However, the slope of the (retrograde) curves of rising carrier prevalence are similar, with the calculated curve lying some years to the left of the observed curve.
Such calculations can only yield very approximate results because of numerous uncertainties. For example, the mothers of children born in any year cover a wide age range, so a specific year of birth cannot be attributed to the mothers or offspring of the anchor cohort. In addition, there are gaps between the three sets of curves in Fig. 6 because the observations cover 17 years but a 20-year generation time is assumed: If generation time in the past was shorter (which it may well have been), these gaps would tend to close. There is also uncertainty about parental consanguinity: The best fit of observed carrier prevalences is with prevalences calculated for a high coefficient of consanguinity. Finally, we do not know what actual carrier prevalence was before 1960 because neither the observed nor the calculated curve of carrier prevalence ever reaches a clear plateau.
Nevertheless, with this calculation, it is possible to compare the observed and calculated rates of fall in carrier prevalence with a model based on genetic theory.
Modelling changing carrier prevalence
To create a simple baseline model, information is required on (a) carrier prevalence in adults pre-eradication, (b) effects of heterogeneous carrier distribution, (c) extent of parental consanguinity and (d) maternal age distribution (which determines the rate at which couples enter and leave the reproductive cohort).
-
(a)
Adult carrier prevalence prior to malaria eradication. In order to avoid overestimating adult carrier prevalence prior to malaria eradication, the 23% figure obtained by calculation is used as the starting value in the model rather than the 25% observed in the oldest subjects (see Fig. 4).
-
(b)
Effects of heterogeneous carrier distribution. The observed unequal distribution of carriers by island and atoll must be allowed for in calculating carrier prevalences in earlier and later generations. Table 7 shows that with aggregated island-specific calculations, affected birth prevalence in the next generation is around 1/1,000 higher, and carrier prevalence around 0.32% lower, than in calculations based on average carrier prevalence for the whole country. Since island-based calculations are most truly representative, they are used in the model.
-
(c)
Potential effect of parental consanguinity. In the absence of observational data, the model includes calculations for F = 0, F = 0.03 and F = 0.0625.
-
(d)
Maternal age distribution. Table 8 shows maternal age distribution in the Maldives for 1984—the oldest available record—and in 2008. In the model, 1984 figures are used for calculating the rate at which birth cohorts with a lower carrier prevalence than their parents entered reproductive age.
The baseline model
Figure 7 presents a crude model assuming hyper-endemic falciparum malaria, no prior anti-malaria measures, 23% adult carrier prevalence and African-style early malaria mortality in non-carriers. The calculation starts 20 years before malaria eradication.
Group born before malaria eradication
Neonatal carrier prevalence is 18–22%, but the parental 23% level is regained before 10 years of age due to excess deaths of non-carriers. This creates a sharp retrograde step-up in carrier prevalence immediately prior to eradication. At first glance, this suggests that carrier prevalence was falling before malaria eradication, but in fact the gradient represents rising carrier prevalence among malaria survivors, frozen at the moment malaria was eradicated.
Those born after malaria eradication
In this group, the lower 18–22% carrier prevalence at birth is maintained life-long. In the model, this creates a plateau that lasts about 20 years, until the new generation gradually take over the reproductive cohort and produce offspring with an even lower neonatal carrier prevalence. This leads to a steady fall in carrier prevalence at birth, determined by mortality in homozygotes and the level of parental consanguinity, and smoothed by overlapping generations.
Expected deviations from the crude model in practice
Malaria eradication divides a population into two groups. In those born before eradication, the model predicts an apparent fall in carrier prevalence prior to eradication because the usual rise in carrier prevalence with age is frozen in time. The slope of this rise reflects both the duration of vulnerability to death from malaria and the success of any previous anti-malarial measures in the observed population. In those born after eradication, the flatness or otherwise of the predicted 20-year plateau depends on carrier prevalence among their parents, who were born prior to eradication. If the increase in carrier prevalence before eradication was slower than that observed in Africa, or was reduced by anti-malarial measures, the expected plateau will be replaced by a gradient. In this case, the overall result would be a relatively steady fall in carrier prevalence from an indeterminate number of years prior to eradication to the present, as observed in the Maldives.
Comparison of the model with present observations
It would be naive to expect exact correspondence between a theoretical model and field observations. Figure 7 compares the model with “observed” carrier prevalences (i.e. including prevalences calculated from observation in those born 1974–1989) assuming F = 0.03. In a direct comparison (Fig. 8a), the modelled and observed curves are similar, but the observed curve lies to the left of the modelled curve. The difference is partly because the observed curve shows a gradual (retrograde) rise from 1973 to 1959, i.e. over 14 years, instead of a sharp step-up as in the model. However, the African observations may not be universally applicable: In the Maldives, differences in vectors and geographical conditions may have extended the period of natural vulnerability to malaria, even life-long, whilst increasing deployment of chloroquine (Schepens 1980) is likely to have reduced early mortality. No records are available to support either suggestion, but in either case, the result would be a more gradual rise in carrier prevalence in those born before malaria eradication. If the observed curve is shifted 10 years to the right, it lies on top of the modelled curve (Fig. 8b), i.e. the two are acceptably consistent, allowing for known uncertainties.
a Comparison of the model with observed carrier prevalences for subjects born 1974–1989 and calculated prevalences in their parents and children. For clarity, only the calculation for F = 0.03 is shown. The overall slope of the curve based on observations is similar to the model, but is displaced 5–10 years to the left. This could indicate a longer period of vulnerability to death from malaria in those born before malaria eradication, or the effects of prior anti-malaria measures, or a combination of the two. b If the curve for observed carrier prevalence is shifted 10 years to the right, it falls broadly within the modelled ranges
Considering the many variables that can intrude between simple genetic theory and complicated human reality, we conclude that the observation of falling thalassaemia carrier prevalence in the Maldives is consistent with the predicted effect of malaria eradication and supports the population genetic theory.
Other factors that might affect carrier prevalence
It has been suggested that population mixing or reproductive compensation could have contributed to changing carrier prevalence.
Population mixing
Population mixing cannot have contributed significantly to the present observations. Even complete mixing within the Maldivian population would not affect average carrier prevalence in the short-term—such change would require mixing with lower-prevalence populations, but immigration is negligible. In 1990, only 1.23% of the population were born outside the Maldives (World Bank Development Indicators 2009).
In the long term, in theory, complete mixing within the Maldivian population could reduce affected birth prevalence by ironing out geographical variations in carrier prevalence. This would tend to retain gene variants in the population and would oppose falling carrier prevalence (maximum effect = 0.3% per generation, see Table 4). However, in practice, inter-island journeys remain difficult, expensive and sometimes dangerous for most people, and some islands are inaccessible for months at a time due to weather conditions. The 1995 census showed limited internal migration of male workers, mainly from the most northern and southern atolls where there are airports.
Reproductive compensation
When parents replace children who die of a recessive disorder, two thirds of replacement unaffected children are carriers, tending to retain gene variants in the population. In theory, this effect could reduce the rate of fall of carrier prevalence by up to 0.3% per generation (see ESM Fig. 2), but there is unlikely to have been any significant effect in this case.
-
In a baseline situation with endemic uncontrolled falciparum malaria, reproductive compensation by parents of non-carrier children who died from malaria would swamp compensation for children dying of thalassaemia.
-
Risk information for parents of affected children has been available since the 1980s, and carrier screening has been widely available since the mid-1990s. Since informed at-risk couples tend to have smaller families than the population norm (Angastiniotis and Hadjiminas 1981; Petrou et al. 2000), risk information has almost certainly neutralised any effect of reproductive compensation since the mid-1980s.
-
This leaves a narrow window of 15 or so years (1974 to mid-1980s) when reproductive compensation might have operated. Even so, a significant effect is unlikely because the effect is greatest when affected children die soon after birth, but untreated thalassaemic children often survive for several years.
In conclusion, neither population mixing nor reproductive compensation has had any significant effect on carrier prevalence in the Maldives. Even if they had, the tendency would be to maintain carrier prevalence: They cannot have contributed to the observed fall.
Changing affected birth prevalence
Calculation from observed carrier prevalences indicates a 50% fall in potential affected birth prevalence (i.e. in the absence of intervention) from 1.6% before 1960 to around 0.8% by the year 2000 (see Table 6), but actual affected birth prevalence has only been reliably documented since around 2000. Since then, though 48 to 60 affected births might be expected per year, only 20 have been observed, leaving 30–40 potential affected births unaccounted for annually (Table 3 and Fig. 5). The difference must be attributed to the availability of risk information for prospective parents and the uses they make of it.
The objective of genetic counselling is informed choice. Table 9 shows the choices available to informed carriers in relation to the life stage at which they learn of their risk. By 2007, 65% of Maldivians of reproductive age had been tested and informed, but only very limited information is available on the choices carriers have made. Discussion of the contribution of different choices to the observed fall in affected birth prevalence must therefore be largely hypothetical.
Circumstances of continuing affected births
At present, up to 35% of Maldivians of reproductive age are unaware of their carrier status, and this group probably contributed many of the registered affected births. No information is available on the proportion of parents of affected children who were aware of their risk prior to pregnancy: This can be established by enquiry about the circumstances surrounding the birth of affected children (Modell et al. 2000).
Utilisation of prenatal diagnosis
Some data are available on utilisation of prenatal diagnosis. This is presently available only to couples who can afford to travel to India. At least 40 Maldivian couples make the journey annually, and most affected pregnancies are terminated (average eight per year): This could account for 20–25% of the 30–40 annual “missing” cases. The remaining reduction below expectation must be due to avoidance of at-risk pregnancies, either because carriers avoid marriage with another carrier or because informed at-risk couples limit their family size.
Avoiding marriage between carriers
This choice is available only for those tested prior to marriage, and any effect on affected birth prevalence would appear gradually as informed young people enter the reproductive age group. The commonest age at testing is 16 years, and present maternal age distribution indicates a mean age of about 20 years at marriage. With these parameters, assuming 100% premarital testing, it would take almost 20 years for 50% of parents to be informed and up to 40 years for all parents to be informed. The first screening round covered 50% of individuals aged 15–20: If all identified carriers in this age group chose a non-carrier partner, the maximum effect by 2002–2007 would be a 20% reduction in affected birth prevalence (Fig. 9).
Proportion of potential parents with risk information in relation to carrier screening. The upper curve shows a model in which 100% premarital screening is introduced in a single year (in this case 1990), average age at marriage = 20 and maternal age distribution = observed distribution in the Maldives in 2008. The curve “Maldives outreach observed” shows the proportion of potential parents with risk information prior to marriage. The curve “Maldives outreach projected” shows the estimated continuing increase in proportion with premarital risk information, assuming that outreach screening continues. By the years of interest, 2000–2007, an estimated 25–30% of potential parents had risk information prior to marriage
In practice, the effect is almost certainly smaller because (a) studies in other populations have shown that knowledge of carrier status prior to marriage has a relatively small effect on partner choice (Stamatoyannopoulos 1974; Angastiniotis and Hadjiminas 1981; Samavat and Modell 2004; Alhamdan et al. 2007) and (b) in the Maldives the task of finding a non-carrier partner would be particularly challenging in view of the very high carrier prevalence and the limited number of possible partners in small island populations.
Other options
Options for informed couples for risk reduction when prenatal diagnosis is unavailable or termination of pregnancy is unacceptable include the following.
-
Avoiding children altogether: This choice rarely proves acceptable in the long run.
-
Waiting to start a family until prenatal diagnosis (or a more acceptable option) becomes available. This behaviour was observed in Cyprus when screening was started before prenatal diagnosis was available, and may well be operating in the Maldives at present.
-
Limiting final family size: It has been observed that informed couples at risk for thalassaemia often limit themselves to one or two healthy children—a reasonable choice in the circumstances since 75% of at-risk couples with only one child and over 50% with two children will never have an affected child (Angastiniotis and Hadjiminas 1981; Petrou et al. 2000; Samavat and Modell 2004). Table 10 shows that the effect of this behaviour on affected birth prevalence depends on the population norm for final family size because any effect depends on differences in reproductive behaviour between those at risk and the rest of the population. Before 1985, the average Maldivian family size was about seven: If (hypothetically) all affected children had been diagnosed and their parents limited their family to two healthy children, affected birth prevalence might have fallen by around 30%. Family spacing was introduced around 1985; average family size fell to 3.5 in the next 10 years, and this greatly reduced the potential reduction in affected birth prevalence. Prospective carrier screening, introduced at this point, might have led to a 30% fall in affected birth prevalence, but the effect has been greatly reduced by a continuing fall in average final family size (2.06 in 2008).
In conclusion, altered partner choice has probably made only a minor contribution to falling affected birth prevalence. Limitation of family size has probably made a larger contribution, but its effect is waning with falling final family size. Thus, any substantial future reduction in the number of affected births is likely to depend on increased access to prenatal diagnosis.
What will happen in the future?
The potential prevalence of affected conceptions will continue to fall in coming decades as young people with lower carrier prevalences reach reproductive age. For example, Table 6 predicts a prevalence of 4.4–6.3/1,000 conceptions among the offspring of the 1990 birth cohort, a reduction of 75% below the 1950s level.
On the other hand, with modern care, most patients with thalassaemia are expected to survive well into adult life and to have a family of their own (Modell et al. 2008). In theory, this could tend to stabilise carrier frequency by preventing loss of gene variants. However, in practice, gene frequency will continue to decline as long as informed at-risk couples take steps to avoid affected births.
Why has falling carrier prevalence only just been noticed?
It seems surprising that falling carrier prevalence has not been observed more widely in view of the large amount of epidemiological data that are available for haemoglobin disorders (Livingstone 1985; Weatherall and Clegg 2001; Modell and Darlison 2007). However, age-related change is easy to miss because most surveys and carrier screening programmes target a narrow age range (newborns, schoolchildren, military recruits, those about to marry, pregnant women) and exclude older people. In such situations, age-related change can only be detected by comparing prevalences at different points in time, and in fact, a decrease in thalassaemia carrier prevalence from 17% to 15.5% over 25 years has been noted in Cyprus (Kyrri 2007).
A particular combination of circumstances facilitated the observation of changing carrier prevalence in the Maldives. Beta-thalassaemia is the commonest haemoglobin variant, with a carrier prevalence among the highest in the world, most homozygotes died until very recently, mortality from falciparum malaria was halted by total eradication in 1971–1995 (Schepens 1980), the population is stable with little immigration or emigration (World Bank Development Indicators 2009), the thalassaemia screening policy covers a wide age range (Firdous 2005), and electronic recording enabled ready analysis by year of birth.
Possible relevance for sickle cell disorders
The general principles illustrated here also apply for sickle cell disorders. Malaria has been eradicated or is controlled to various degrees in many populations where haemoglobin S is common, including the entire American continent and much of the Middle East, but it cannot be automatically assumed that a comparable reduction in carrier prevalence is occurring or has occurred in these areas, for a number of reasons.
Firstly, sickle cell disorders vary in severity. In the absence of services, typical severe sickle cell anaemia (SS, African genotype) and some forms of S/beta-thalassaemia cause death in early childhood, but when basic services are available, the majority of patients live well into adult life. In contrast, sickle cell anaemia of the Asian type (common in India and the Middle East), SC and some forms of S/beta-thalassaemia cause a milder disorder with fewer childhood deaths and lower risks in adult life, even in the absence of services (Perrine et al. 1978). Therefore, one may expect sickle cell genotype to exert a substantial effect on changing carrier prevalence following malaria eradication.
Secondly, malaria itself is an important cause of early death in sickle cell disorders (Fleming et al. 1979). Therefore, malaria control may reduce homozygote mortality as well as carrier advantage, and this could modify the effect on gene frequency.
Studies in Jamaica have confirmed a historical fall in haemoglobin S (but not haemoglobin C) gene frequency (Hanchard et al. 2005). However, no difference in carrier prevalence could be found between cohorts of newborns tested 20 years apart. The conclusion is that HbS gene frequency has now stabilised in Jamaica due to a combination of improved homozygote survival and fertility, and a reduction in the local population norm for family size (Hanchard et al. 2006; McKenzie et al. 2009).
In light of these considerations, it would be interesting to study age-related haemoglobin S carrier prevalence both in Africa and also in localities where malaria is controlled and mild sickle cell disorders are common (e.g. Bahrain, parts of Iran).
Comparable changes are probably occurring worldwide in the gene frequency of other disorders maintained at high prevalence by heterozygote advantage, including glucose-6-phosphate dehydrogenase deficiency (Luzzato and Mehta 1995) and cystic fibrosis (Poolman and Galvani 2007). Age-related prevalence studies may yield interesting information in populations where these are common.
General relevance of the study for community genetics
This study illustrates a number of general principles that are relevant for community genetics theory and practice, including the following.
Carrier screening for haemoglobin disorders, currently practised in a very wide range of cultural and economic settings, offers an outstanding opportunity for gaining experience with the practical, social and ethical implications of screening for genetic reproductive risk—i.e. haemoglobin disorders are pilot conditions for learning about appropriate uses of genetic risk information.
An understanding of basic population genetics is required both for service planning and for correct interpretation of surveillance data. For example, in the Maldives, it would be easy, mistakenly, to attribute all of the observed fall in affected births to the outreach screening programme, when in reality it reflects the interaction of several different factors.
Disease registers provide an essential tool for assessing the effects of genetic public health interventions.
Genetic data collected for ostensibly different purposes can be used to follow events at the population level.
The extraordinary speed with which haemoglobin gene variants can respond to changes in malaria prevalence demonstrates continuing human evolution, and this can be observed through monitoring clinical services.
A holistic outlook is essential. The biological link between malaria and haemoglobin disorders underlines the fact that the genetic component in health cannot be considered in isolation. The distribution of haemoglobin gene variants in a population constitutes a living record of its malaria history, whilst malaria control both unmasks haemoglobin disorders (confronting populations with the need for treatment and prevention) and reduces their prevalence (sometimes quite rapidly). Both aspects need to be considered when designing and evaluating programmes for the control of either group of disorders.
Finally, the age distribution of a population is a historical record that offers a 60- to 70-year window into the past. Genetic epidemiological studies should exploit this opportunity by including the elderly, who cannot be revisited in the future.
References
Ahmed S, Saleem M, Sultana N, Raashid A, Waqar A, Anwar M, Modell B, Karamat KA, Petrou M (2000) Prenatal diagnosis of beta thalassaemia in Pakistan: experience in a Muslim country. Prenat Diagn 20:378–383
Ahmed S, Saleem M, Modell B, Petrou M (2002) Screening extended families for genetic haemoglobin disorders in Pakistan. N Engl J Med 347:1162–1168
Alhamdan NA, Almazrou YY, Alswaidi FM, Choudhry AJ (2007) Premarital screening for thalassemia and sickle cell disease in Saudi Arabia. Genet Med 9:372–377
Allison AC (1954) The distribution of the sickle cell trait in East Africa and elsewhere, and its apparent relationship to the incidence of sub-tertian malaria. Trans R Soc Trop Med Hyg 48:312–318
Alwan A, Modell B (2003) Recommendations for introducing genetics services into developing countries. Nat Rev Genet 4:61–68
Angastiniotis MA, Hadjiminas MG (1981) Prevention of thalassaemia in Cyprus. Lancet 1(8216):369–370
Banton AH (1951) A genetic study of Mediterranean anaemia in Cyprus. American Journal of Human Genetics 3:47
BCSH (1998) Guideline. The laboratory diagnosis of haemoglobinopathies. Brit J Haematol 101:783–792
Bittles AH (1990) Consanguineous marriage: current global incidence and its relevance to demographic research. Population Studies Center, University of Michigan. Research report no 90-186. Updated data at www.consang.org
Bodmer WF, Cavalli-Sforza LL (1976) Genetics, evolution, and man. W.H. Freeman, San Francisco
Bradley DJ (1991) Malaria. In: Feacham RG, Jamison DT (eds) Disease and mortality in sub-Saharan Africa. Oxford University Press, Oxford, pp 196–197
Bundey S, Alam H, Kaur A, Mir S, Lancashire RJ (1990) Race, consanguinity and social features of Birmingham babies: a basis for a prospective study. J Epidemiol Community Health 44:130–135
Cardenas H (1985) Report on duty travel to the Maldives. WHO consultant’s report, Maldivian Ministry of Health
Clegg JB, Weatherall DJ (1999) Thalassaemia and malaria: new insights into an old problem. Proc Assoc Am Physicians 111:278–282
Firdous N (2005) Prevention of thalassaemia and haemoglobinopathies in remote and isolated communities—the Maldives experience. Ann Hum Biol 32:131–137
Fleming AF, Storey J, Molineaux L, Iroko EA, Attai EDE (1979) Abnormal haemoglobins in the Sudan savannah of Nigeria. 1. Prevenance of haemoglobins and relationships between sickle cell trait, malaria, and survival. Ann Trop Med Parasitol 73:161–172
Furumi H, Firdous N, Inoue T, Ohta H, Winichagoon P, Fucharoen S et al (1998) Molecular basis of beta-thalassemia in the Maldives. Hemoglobin 22:141–151
Haldane JBS (1949) Disease and evolution. Ricerca Scientifica Roma 19(Supplement 1):3
Hanchard NA, Hambleton I, Harding RM, McKenzie CA (2005) The frequency of the sickle cell allele in Jamaica has not declined over the last 22 years. Br J Haematol 130:939–942
Hanchard NA, Hambleton I, Harding RM, McKenzie CA (2006) Predicted declines in sickle allele frequency in Jamaica using empirical data. American Journal of Haematology 81:817–823
Hardle W (1992) Applied nonparametric regression. Cambridge University Press, Cambridge
Harris H (1970) The principles of human biochemical genetics. North Holland, Amsterdam
Kyrri AR (2007) The molecular epidemiology of α and β globin variants in Cyprus. PhD thesis, University of London
Livingstone FB (1967) Abnormal hemoglobins in human populations. Aldine, Chicago
Livingstone FB (1985) Frequencies of hemoglobin variants. Thalassemia, G6PD variants and ovalocytosis in human populations. Oxford University Press, New York
Luzzato L, Mehta A (1995) Glucose-6-phosphate dehydrogenase deficiency. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic basis of inherited disease, 7th edn. McGraw Hill, New York, pp 3367–3398
Luzzatto L (1979) Genetics of red cells and susceptibility to malaria. Blood 54:976–981
McKenzie C, Hanchard N, Harding R, Hambleton I, Modell B (2009) Rate of change of sickle allele frequency may be influenced by total fertility rate: a sesquicentenary reflection on human micro-evolution. Br J Haematol 147:582–583
Modell B, Darlison M (2007) Global epidemiology of haemoglobin disorders, and derived service indicators. Bulletin of the WHO 86:480–487
Modell B, Hindley N, Razzak A (1990) Thalassaemia in the Maldives. Lancet 335:1169–1170
Modell B, Harris R, Lane B, Khan M, Darlison M, Petrou M, Old J, Layton M, Varnavides L (2000) Informed choice in genetic screening for thalassaemia during pregnancy: audit from a national confidential enquiry. Br Med J 320:325–390
Modell B, Khan M, Darlison M, Westwood MA, Ingram DI, Pennell DJ (2008) Improved survival of thalassaemia major in the UK and relation to T2* cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance 10:42. http://www.jcmr-online.com/content/10/1/42
Perrine RP, Pembrey ME, John P, Perrine S, Shoup F (1978) Natural history of sickle cell anemia in Saudi Arabs. A study of 270 subjects. Ann Intern Med 88:1–6
Petrou B, Modell B, Shetty S, Ward RHT (2000) Long-term effects of prospective detection of high genetic risk on couples’ reproductive life: data for thalassaemia. Prenat Diagn 20:469–474
Poolman EM, Galvani AP (2007) Evaluating candidate agents of selective pressure for cystic fibrosis. J R Soc Interface 4:91–98
Raper AB (1956) Sickling in relation to morbidity from malaria and other diseases. Br Med J 1(4973):965–966
Samavat A, Modell B (2004) Iranian national thalassaemia screening programme. Br Med J 329:1134–1137
Schepens JRM (1980) Malaria control in the Maldives. WHO Consultant’s Assignment Report, October 1974–July 1980. WHO Project MAV MPD 001
Stamatoyannopoulos G (1974) Problems of screening and counselling in the hemoglobinopathies. In: Motulsky AG, Lenz W (eds) Birth defects. Excerpta Medica, Amsterdam, pp 268–276
UK Thalassaemia Society (2005) Standards for the clinical care of children and adults with thalassaemia in the UK. The UK Thalassaemia Society. ISBN 1 900254 18 2. http://www.haemoglobin.org.uk/pdf/guidelines/2005-thal-standards-2sided.pdf
UN Demographic Yearbook (1997) Historical supplement. http://unstats.un.org/unsd/demographic/products/dyb/special_issues.html
UN Demographic Yearbook (2008) United Nations, New York. http://unstats.un.org/unsd/demographic/products/dyb/
UNPP (UN World Population Prospects) (2008) The 2008 Revision Population Database. http://esa.un.org/unpp/
Weatherall DJ (2008) Genetic variation and susceptibility to infection: the red cell and malaria. Br J Haematol 141(3):276–286
Weatherall DJ, Clegg JB (2001) The thalassaemia syndromes, 4th edn. (Chapter 6. Distribution and population genetics of the thalassaemias). Blackwell Science, Oxford. ISBN 0-86542-664-3
World Bank Development Indicators (2009) World Bank development indicator data 2009. http://web.worldbank.org/WBSITE/EXTERNAL/DATASTATISTICS/
World Population Prospects (2008) The 2008 revision. United Nations Population Division. http://esa.un.org/unpp
Zeesman S, Clow CL, Cartier L, Scriver CR (1984) A private view of heterozygosity: eight-year follow-up study on carriers of the Tay-Sachs gene detected by high-school screening in Montreal. Am J Med Genet 18:769–778
Acknowledgements
We thank the former First Lady of the Maldives Nasreena Ibrahim for her consistent support for the thalassaemia screening programme. We also record our deep appreciation of the dedication of the staff of the SHE laboratory who spend time far beyond their laboratory commitment in organising mobile screening trips and providing genetic counselling and whose meticulous records made this article possible. We thank the staff of the National Thalassaemia Centre for their cooperation in providing and updating information from the National Thalassaemia Register. We are very grateful to Dr Carolyn Williams of Asthma Research Institute of Western Australia, Perth, for help in establishing DNA facilities at SHE, to Professor Suthat Fucharoen of Mahidol University Thailand for support in initiating screening and laboratory analysis, and to Professor Alok Srivastava of the Christian Medical College, Vellore, India, for help with setting up the DNA laboratory and consistently supporting staff and patients in performing prenatal diagnosis.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Bernadette Modell is a retired Wellcome Principal Research Fellow.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
Annex figures and table (DOC 100 kb)
Rights and permissions
About this article
Cite this article
Firdous, N., Gibbons, S. & Modell, B. Falling prevalence of beta-thalassaemia and eradication of malaria in the Maldives. J Community Genet 2, 173–189 (2011). https://doi.org/10.1007/s12687-011-0054-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-011-0054-0