Abstract
Objectives
Parenting children with mental health problems poses multiple challenges, including coping with difficult behavior and negative child emotions. The impact on parents includes financial strain, negative social stigma, and negative feelings of guilt or blame, resulting in significant stress and lower levels of well-being. Given findings that self-compassion plays a significant role in reducing stress and improving well-being, the current study examined the role of self-compassion in the experience of parents raising a child with mental health problems. The study tested (1) whether child behavioral/emotional problem severity is associated with higher parental stress and lower parental well-being; (2) whether self-compassion is associated with lower parental stress and higher parental well-being; and (3) whether self-compassion is a stronger predictor of parental stress and well-being than child behavioral/emotional problem severity.
Methods
Three hundred and six mothers and two hundred and fifty-six fathers of children attending a hospital child and adolescent psychiatric center were assessed at admission. Consenting parents completed four questionnaires: child strength and difficulty, parent version; self-compassion; parent feeling inventory; and well-being.
Results
Child behavioral/emotional problem severity was associated with higher parental stress and lower parental well-being, and self-compassion was a stronger predictor of parental stress and well-being levels than child behavioral/emotional problem severity. For children with internalizing but not externalizing behavioral/emotional problems, parental self-compassion was the only predictor of parental well-being beyond the severity of child behavioral/emotional problems.
Conclusions
Cultivating self-compassion is important in reducing parental stress and increasing parental well-being, particularly with internalizing presentations, and should be considered when designing therapeutic interventions for parents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The rate of children and adolescents diagnosed with mental health problems has been increasing substantially, signifying an issue of serious proportions (Collishaw, 2015). Global epidemiological data from the past decade have consistently reported that up to 20% of children and adolescents suffer from a disabling mental illness (Belfer, 2008; Polanczyk et al., 2015; Westerlund et al., 2020) that affects nearly all aspects of parental life (Angold et al., 1998; Vohra et al., 2014). Parents must cope with financial strain and time constraints caused by their child’s condition (Lecavalier et al., 2006). They face social stigma related to mental disorders (e.g., Hinshaw & Stier, 2008; Moses, 2010), often exacerbated by feelings of blame for their child’s mental illness due to perceived deficits in their parenting (Crowe et al., 2011). Additionally, parents may internalize negative stereotyping and discrimination, which, in turn, may be reflected in feelings of guilt or blame related to their child’s illness (e.g., Hinshaw, 2007; Mak & Cheung, 2012). These feelings can lead to social isolation and rejection from society (Eaton et al., 2016; Hasson-Ohayona et al., 2014).
A significant source of parents’ stress resides in coping with their children’s difficult behavior and aroused emotions. These negative aspects often cloud positive or natural characteristics and might cause parents to become more impulsive and irritable toward their children (Bögels et al., 2010). Mental health problems in adolescents challenge parenting practices and may increase a variety of negative feelings, including frustration, helplessness, and blame for being an inadequate parent or for being unable to meet their child’s emotional needs (Crowe et al., 2011; Lindgren et al., 2016). Parenting a child with emotional and behavioral problems is accompanied by long-term stress and can compromise quality of life (e.g., Gerkensmeyer et al., 2011; Vaughan et al., 2013). Parents of children with mental health problems experience significantly lower levels of life satisfaction, an indicator of well-being (Athay, 2012), and marginally poorer well-being than parents raising children without disabilities (Oruche et al., 2012; Smith & Grzywacz, 2014).
One commonality between well-being and caregiver stress is their relationship to the severity of the child’s symptoms. A child’s symptom severity is a significant predictor of parenting stress (e.g., Barroso et al., 2018; McDonald et al., 1997) and parental well-being (e.g., Athay, 2012; Early et al., 2002). This finding is evident for various special needs populations (e.g., disabilities, autism; Ekas & Whitman, 2010; Neff & Faso, 2015). Since parental stress and parental well-being are influenced by children’s mental health problems and influence parents, parent–child relationships, and child adjustment, it is important to identify potential factors that help parents reduce stress and increase well-being. However, to the best of our knowledge, few studies have focused specifically on factors that may help parents of children with mental health problems reduce stress and enhance well-being (Rodríguez-Meirinhos et al., 2018).
Self-compassion plays an important role in individual stress and subjective well-being development (Neff, 2003). Self-compassion is an adaptive way of self-to-self relating (Gilbert & Procter, 2006; Neff, 2009, 2012). Neff (2003, 2009) described three dimensions of self-compassion: (1) self-kindness versus self-judgment, meaning being kind and understanding toward oneself in instances of hardship or perceived inadequacy rather than being harshly self-critical; (2) a sense of common humanity versus isolation, meaning perceiving one’s experiences as part of the larger human experience rather than seeing them as isolating; and (3) mindfulness versus overidentification, meaning holding painful thoughts and feelings in mindful awareness rather than overidentifying with them. The self-compassion dimensions facilitate an individual’s openhearted stance toward negative aspects of oneself and one’s experience, fostering a kind, forgiving, and empathetic attitude toward others (Neff, 2012). Therefore, self-compassion has been associated with a variety of positive individual outcomes, such as higher levels of optimism, happiness, and positive affect (Neff, 2003; Neff et al., 2007), as well as greater acceptance and caring in relationships and better relational well-being (Gouveia et al., 2016; Yarnell & Neff, 2013).
In the context of the parent–child relationship, self-compassion has the same positive relation to the feelings, behavior, and well-being of the parent (Moreira et al., 2015a, 2015b; Sirois et al., 2019). For example, Sirois et al. (2019) found that self-compassion improves parental well-being when dealing with the negative feelings of shame and blame. Gouveia et al. (2016) reported that higher levels of parental mindfulness and self-compassion are associated with lower levels of parenting stress and higher levels of an effective parenting style.
When facing an ongoing life stressor such as raising a child with mental health problems, parental self-compassion can be essential for developing an “immune system” to help parents manage their own as well as their child’s negative feelings (Gilbert, 2014). Bögels et al. (2010) proposed a mindful parenting program to foster changes in interactions between parents and children with mental health problems. The program emphasizes mindfulness and self-kindness, two of three components of self-compassion. Mindfulness and self-kindness help parents manage their stress and adopt a more accepting and nonjudgmental stance toward themselves as parents and toward their children, especially when their children express negative emotions. Mindfulness and self-kindness also increase parents’ positive attention to themselves and their children (Bögels et al., 2010). This overall positive effect of self-compassion might be reflected in parental well-being, although to the best of our knowledge, this specific variable has not been tested in the context of parents of children with mental health problems. For parents raising children with autism and learning disabilities, parental self-compassion has been found to contribute significantly to parental well-being. Neff and Faso (2015) found that among parents of children with autism aged 4 to 12, self-compassion predicted parental well-being over and above the effects of child symptom severity. Sumiati (2018) reported that among parents of children with learning disabilities, self-compassion was strongly and positively associated with well-being and moderated the association between emotion regulation strategy (problem or emotion focus) and well-being.
Self-compassion has positive potential for managing individual stress and subjective well-being (Neff, 2003); however, the bulk of previous research does not measure self-compassion specifically in relation to parenting a child with mental health problems. Our research focused on this particular junction between parental self-compassion and parenting children with mental health problems and examined whether parents’ self-compassion is associated with their levels of stress and well-being. To capture the subjective experience of parental stress, we used data on negative and positive feelings of parenting given that negative feelings toward the self and toward the child have been demonstrated to indicate parenting stress (Deater-Deckard, 1998). In light of prior findings that the severity of symptoms in children with mental health problems negatively impacts parental stress and well-being (Athay, 2012), our second objective was to determine whether self-compassion is a more accurate predictor of parental stress and well-being than symptom severity. We hypothesized that (1) child behavioral/emotional problem severity is associated with greater negative emotion and with overall lower levels of parental well-being; (2) self-compassion is associated with less negative and more positive parental emotion and higher levels of parental well-being; and (3) self-compassion is a stronger predictor of parental emotion and well-being than the child’s behavioral/emotional problem severity.
Method
Participants
The sample included 446 families of children attending the child and adolescent psychiatric center of a public hospital that serves a regional multiethnic population. The center provides assessment and treatment in individual outpatient clinics for a variety of mental health problems. Families attending the psychiatric center are assessed by a clinician and referred to the relevant clinic for a deeper assessment and treatment plan. The families of the current study were referred to anxiety and post-trauma, ADHD, eating disorders, depression, and sexual abuse clinics where they were given the questionnaires. In total, 406 mothers and 256 fathers completed the questionnaires. Of the mothers, 314 (77%) were married, 62 (15%) were divorced, 11 (3%) were widows, and 19 (5%) were single mothers. Of the fathers, 226 (88%) were married, 27 (11%) were divorced, and 3 (1%) were single fathers. For 216 (48%) children, both the mother and the father answered the questionnaires; for 190 (43%) children, only the mother responded; and for 40 (9%) children, only the father responded. The children, who were in elementary and secondary school grades, ranged in age from 10 to 18 years (M = 12.6, SD = 3.2). The mothers ranged in age from 27 to 65 (M = 43.0, SD = 6.5), and the fathers ranged in age from 29 to 68 (M = 46.5, SD = 6.7).
Procedure
The questionnaires are part of a broader set of questionnaires completed by parents and children attending the center and are used by center professionals in the evaluation process, not only for research purposes. The Helsinki Committee of Ziv Medical Center, Tzfat, Israel, approved the study.
Measures
Parental Feelings Inventory
The parental feelings inventory (PFI; Bradley et al., 2013) assesses parental emotions in the parenting role. Parents are presented with emotion adjectives and are asked to indicate the degree to which they experienced that emotion during the last week in their role as parents. Thirty-one emotion adjectives are assessed using a 7-point Likert scale (1 = not at all to 7 = extremely). The emotion adjectives are separated into three groups (happy, angry, anxious/sad). For the purpose of this study, parents’ feelings were separated into positive and negative groups. Correlation coefficients between PFI anger and PFI sadness were high (r = 0.65). The scale demonstrated good reliability (internal consistency in the current sample was α = 0.90 for the PFI-positive scale and α = 0.93 for the PFI-negative scale) and correlated with other measures of parent and child functioning, supporting the overall utility of the PFI as a measure of emotional experiences in the parenting role.
Personal Well-being Index (PWI-A; International Wellbeing Group, 2006)
The PWI-A for assessing the subjective sense of well-being is composed of one question inquiring about general life satisfaction and eight items measuring satisfaction in specific life domains: standard of living, personal health, achieving in life, personal relationships, personal safety, community connectedness, future security, and religion. All items are rated on a scale ranging from 0 = completely dissatisfied to 10 = completely satisfied. The scale has a Cronbach’s alpha ranging from 0.70 to 0.85 (International Wellbeing Group., 2006), and internal consistency in the current sample was α = 0.87.
Strengths and Difficulties Questionnaire Parent Version (SDQ; Goodman, 1997)
The SDQ is a widely used screening tool for assessing the symptom severity of behavioral and emotional disorders in children and adolescents (Niclasen et al., 2012), with good convergent validity with clinician-rated diagnoses (He et al., 2013). The 25-item measure includes five subscales that assess internalizing (emotional problems subscale) and externalizing (hyperactivity and conduct subscales) symptoms, a subscale measuring difficulties with peers, and a subscale assessing prosocial behavior. High scores on the four difficulty subscales represent a high degree of difficulty; a high score on the prosocial scale represents a high degree of prosocial behavior. The four difficulty subscales have been shown to be indicative of youth mental health service use (Koskelainen et al., 2000). Internal consistency in the current sample was α = 0.74 for prosocial, α = 0.78 for externalizing, and α = 0.71 for internalizing.
Self-Compassion Scale (SCS; Neff, 2003)
Self-compassion was measured using a 26-item self-report measure with responses ranging from 1 = almost never to 5 = almost always. The SCS contains six subscales: self-kindness (e.g., I try to be loving toward myself when I’m feeling emotional pain), self-judgment (e.g., I’m disapproving and judgmental about my own flaws and inadequacies), common humanity (e.g., When things are going badly for me, I see the difficulties as part of life that everyone goes through), isolation (e.g., When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world), mindfulness (e.g., When I’m feeling down, I try to approach my feelings with curiosity and openness), and overidentification (e.g., When I’m feeling down, I tend to obsess and fixate on everything that’s wrong). The SCS subscales may be examined separately, or a total self-compassion score can be used given that a single higher-order factor of “self-compassion” has been found to explain the intercorrelations between subscales (Neff, 2003). Note that the self-judgment, isolation, and overidentification subscales of the SCS are reverse coded so that higher scores indicate higher levels of self-compassion. The scale demonstrates convergent validity (e.g., correlates with partner ratings), discriminant validity (e.g., no correlation with social desirability), and good test–retest reliability (Neff, 2003; Neff & Beretvas, 2013). Internal consistency in the current sample for the SCS total score was α = 0.90.
Data Analyses
The outcome measures (parental well-being (PWB), PFI happy, and PFI negative) were reviewed for extreme values using boxplots, scatterplots, histograms, and normal probability plots and found to be normally distributed. Of the 662 respondents, 44 individuals did not complete the PWB questionnaire. No discernable patterns were found by visually inspecting the missing data, which suggested that they were missing at random. In a random pattern, a small percentage of data points missing from a large dataset is insignificant (Tabachnick & Fidell, 2007).
The internal consistency of each scale was calculated using Cronbach’s alpha. Pearson regression coefficients were calculated to assess the association between all subscales. Comparison of the results between mothers and fathers across the variables of interest was performed using a two-sample T-test. To determine whether SDQ subscales (prosocial, externalizing, internalizing) predicted the outcome measures, we conducted a series of mixed linear regressions. The predictor variables were pairwise interactions of parents (father vs. mother), each of the SDQ subscales and the corresponding main effects. To determine whether self-compassion predicted the outcome measures beyond those accounted for by SDQ subscales, we followed the first-stage mixed linear regressions described above with a second-stage series of mixed linear regressions. In the second stage, an additional pairwise interaction of parent and self-compassion and the corresponding main effect were added to the model. In both steps, child age and the mean parent age were entered as control variables. The significance of the interaction effects signifies a moderation effect of the parent in the relationship between each predictor variable and the outcome variable. Generalized linear models (using PROC GLIMMIX) were applied for the two-stage mixed linear regression models since they enable the modeling of hierarchical data (in this case, a mother and father nested in the same family and reporting for the same child). The multilevel model has the capacity to handle unbalanced data when the data are missing at random (Goldstein, 2003).
Post hoc power analysis was performed using a Gpower computer program (Buchner et al., 1998) to generate a linear multiple regression random model. The input parameters for the power calculation for each of the prediction models were the predictors’ correlation coefficients with the outcome measure and the total sample size of 622 participants. Power was above 95% for all three models. A p value of 0.05 was considered significant. Statistical analysis was performed by SAS for Windows version 9.4.
Results
All data are available as supplementary materials to this article. Consistent with our first hypothesis, the SDQ total score and its two subscales, internalizing and externalizing severity, were positively correlated with PFI negative, r = 0.38, r = 0.29, and r = 0.31, and negatively correlated with PFI positive, r = -0.18, r = -0.11, and r = 0.18, and PWB, r = -0.17, r = -0.12, and r = -0.14. SDQ prosocial was not significantly correlated with PFI negative but was positively correlated with PFI positive, r = 0.19, and PWB, r = 0.12. Consistent with our second hypothesis, self-compassion was negatively correlated with PFI negative, r = -0.34, and positively correlated with PFI positive, r = 0.30, and PWB, r = 0.56 (Table 1). Table 2 presents how mothers and fathers differed across the variables of interest. Fathers had significantly higher PFI-negative values than mothers (M = 3.49 vs. M = 3.08, p < 0.001). Given that the total SDQ score was found to be highly correlated with the SDQ externalizing and internalizing subscales and to gain more specific understanding as suggested by previous studies (Becker et al., 2018), the subsequent analysis refers to these SDQ subscales.
Predicting PWB and PFI
To determine whether self-compassion predicted PWB and PFI beyond that accounted for by SDQ subscales (the third hypothesis), we conducted a series of mixed linear regressions in two steps. Pairwise interactions of parent (father vs. mother), each of the SDQ subscales (prosocial, externalizing, internalizing) and their corresponding main effects were entered in the first step, and pairwise interactions of the parent and self-compassion and the corresponding main effect were entered in the second step. In both steps, child age and mean parent age were entered as control variables (Tables 3, 4, and 5).
Table 3 presents regression results for the outcome of negative parental emotion (PFI negative). In Step 1, SDQ subscales contributed significantly to the regression model, F (9,473) = 14.45, p < 0.001, and accounted for 21.6% of the variance in PFI negative. The following predictors significantly predicted PFI negative in step 1: parent, β = -0.28, p < 0.01, indicating higher PFI, SDQ externalizing, β = 0.26, p < 0.01, SDQ internalizing, β = 0.21, p < 0.05, indicating higher PFI negative values for increased SDQ externalizing and internalizing values. Adding self-compassion to the regression model accounted for an additional 9.1% of the variance in PFI negative, and this change in R2 was significant, F (1,593) = 43.95, p < 0.001. Adding self-compassion did not change the significance of the predictors in Step 1, with the exception of child age, which became a significant predictor, β = 0.09; p < 0.05, indicating higher PFI negative values for older children. Self-compassion was a significant predictor, β = -0.27; p < 0.05, indicating lower PFI negative values for increased self-compassion values. An examination of their standardized regression coefficients revealed that parent and self-compassion were stronger predictors than any other variables.
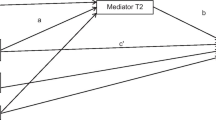
Table 4 presents the regression results for the outcome of positive parental emotion (PFI positive). In Step 1, SDQ subscales contributed significantly to the regression model, F (9,476) = 8.28, p < 0.001, and accounted for 13.5% of the variance in PFI positive. The following predictors significantly predicted PFI positive in step 1: SDQ prosocial, β = 0.11, p < 0.05, indicating that SDQ prosocial values were associated with higher PFI happiness values, parent, β = 0.18, p < 0.01, indicating higher PFI positive values for fathers than mothers, SDQ internalizing, β = -0.12, p < 0.05, indicating lower PFI positive values for increased SDQ internalizing values, and the interaction SDQ externalizing *parent, β = -0.16, p < 0.05. Figure 1 depicts the interaction between parent and SDQ externalizing. For mothers, as SDQ externalizing scores increased, PFI positive scores decreased, whereas for fathers, SDQ externalizing scores had a small positive effect. Additionally, younger child age, β = -0.13, p < 0.01, and mean parent age, β = -0.10, p < 0.05, were associated with higher PFI happiness values.
Adding self-compassion to the regression model accounted for an additional 7.5% of the variance in PFI positive, and this change in R2 was significant, F (1,590) = 27.48, p < 0.001. Adding self-compassion did not change the significance of the predictors in Step 1, and self-compassion was a significant predictor, β = 0.22, p < 0.001. An examination of the standardized regression coefficients revealed that self-compassion was a stronger predictor than all other predictors.
Table 5 presents the regression results for the outcome of personal well-being (PWB). In Step 1, SDQ subscales contributed significantly to the regression model, F (9,410) = 2.68, p < 0.01, and accounted for 5.5% of the variance in PWB. SDQ internalizing significantly predicted PWB, β = -0.14, p < 0.01, indicating that increased SDQ internalizing values were associated with decreased PWB values. Adding self-compassion to the regression model accounted for an additional 39.7% of the variance in PWB, and this change in R2 was significant, F (1,593) = 154.44, p < 0.001. After adding self-compassion, SDQ externalizing was no longer a significant predictor of PWB. Self-compassion was the only remaining significant predicator of PWB, β = 0.50, p < 0.001, indicating that increased self-compassion values were associated with increased PWB values. An examination of the standardized regression coefficients revealed that self-compassion was a significantly stronger predictor than all other predictors. This result mirrors the finding for the zero-order correlation analysis (Table 1), where the highest correlation coefficient was for self-compassion and PWB.
Discussion
This study examined the potential role of parents’ self-compassion in reducing their stress and increasing their well-being when raising children with mental health problems. Parent stress was examined by negative and positive feelings relating to parenthood. The first hypothesis was supported as follows: For parents of children with mental health problems, child externalizing and internalizing problems were positively correlated with negative parental feelings and negatively correlated with positive parental feelings and with parental well-being. This finding is consistent with previous studies that found that parenting stress is associated with both child externalizing and internalizing behavior problems (Dubois-Comtois et al., 2013; Rodriguez, 2011). Additionally, it is consistent with prior findings that child symptom severity is related to increased experiences of parenting stress (e.g., Angold et al., 1998; McDonald et al., 1997). Given that our sample included parents of children with a variety of psychiatric disorders, the results may indicate that parental stress relates to the severity of the clinical condition beyond the specific disorder. Similarly, in a meta-analysis conducted by Barroso et al. (2018), the authors documented the association between parenting stress and child behavior problems for different clinical groups.
The hypothesis that parent self-compassion is positively associated with less negative and more positive emotions and higher levels of well-being were supported by the study results. This finding highlights the important role of self-compassion in parenting children with special needs and expands it to children with mental health problems. Neff’s pioneering definition of self-compassion, comprising the three primary components of self-kindness, humanity, and mindfulness, enables researchers to measure and explain why and how self-compassion contributes to reducing parental stress and increasing well-being (Neff, 2003; Neff & Faso, 2015).
When raising a child with mental health problems, parents who experience their child with kindness and perceive their lives in the context of the larger human experience can cope with the social stigma and the feelings of shame and blame for their child’s mental illness in a more accepting, nonjudgmental way (e.g., Hinshaw & Stier, 2008; Moses, 2010; Van der Sanden et al., 2013). This could lead, in turn, to openness toward society, replacing the isolation and rejection that are common feelings among parents raising a child with mental health problems (Rodríguez-Meirinhos et al., 2018; Van der Sanden et al., 2013). Moreover, holding painful thoughts and feelings in mindful awareness rather than ruminating over them may reduce parents’ likelihood of being overwhelmed by the negative feelings and behaviors of their child and lead to greater awareness of the positive or natural aspects of their child’s life. The same can be true for the negative parental feelings of frustration and helplessness generated when dealing with negative feelings and behaviors of children with mental health problems (Crowe et al., 2011; Lindgren et al., 2016).
Self-compassion was found to be a stronger predictor of reduced negative and increased positive parental feelings and parental well-being than the severity of the child’s externalizing and internalizing symptoms, supporting the third hypothesis. These findings are consistent with previous studies of parents rearing children with autism (e.g., Neff & Faso, 2015) and expand the contribution of self-compassion to improving the experience of parenting children with a variety of emotional and behavioral problems. Significantly, self-compassion can serve as an acquirable, internal resource that enhances parents’ ability to cope with the unexpected and uncontrollable external demands that accompany raising a child with mental health problems (Bögels et al., 2010).
Our study yielded two interesting findings regarding parental well-being. First, child internalizing but not externalizing problems were associated with a lower level of parental well-being. This finding requires further differentiation between the association of child internalizing and externalizing problems with parental well-being. Previous studies have called for similar examinations of child internalizing and externalizing problems and their different links to parental stress (e.g., Barroso et al., 2018).
Second, after adding self-compassion to the regression model, the level of the internalizing behavior problem was no longer a significant predictor of parental well-being, and self-compassion remained the only significant predictor of parental well-being. This finding suggests that with regard to a child’s internalizing difficulties, self-compassion might act as a protective buffer between the child’s mental health problems and parental well-being. Previous research supports this idea (Bohadana et al., 2019; Neff & Faso, 2015).
Why parental self-compassion might be especially helpful for internalizing compared with externalizing problems remains unclear and should be further investigated. Interestingly, a meta-analysis conducted by Muris (2016) revealed that self-compassion is substantially linked with internalizing versus externalizing psychopathology, which may reinforce the assumption that self-compassion has a different effect on different mental health problems both at the interpersonal level and in the parental context.
The implications for clinical practice are significant, highlighting the treatment potential of integrating a self-compassion component in parenting guidance and therapy for parents of children with mental health problems (e.g., Jefferson et al., 2020).
Limitations and Future Research
The study findings should be interpreted with caution due to several limitations. First, since the relation between parenting factors and child mental health problems is bidirectional, as reported in relation to both parent stress (Neece et al., 2012) and mindful parenting (Bögels et al., 2010), it is difficult to determine the directionality of the association between parenting factors and child mental health problems. It is also possible that there is a transactional relationship in which both parenting factors and child mental health problems impact one another over time. For example, it is possible that parents who have higher self-compassion perceive their child’s emotional and behavior problems as less problematic. Longitudinal studies can measure parenting factors and child mental health problems and track the trajectory of these factors over time. Moreover, our study focuses on the role of self-compassion on parental stress and PWB. The role of parents’ self-compassion should be further investigated with regard to parental practices to gain more understanding of the role of self-compassion in parenting.
Second, given the multiplicity of types of diagnoses and the small sample size for some of the diagnostic categories, we were unable to separately examine the impact of different types of mental health problems. Future studies should refer to specific diagnostic categories to examine differential effects of various mental health problems and the extent to which they affect parental feeling and well-being and the role of parent self-compassion. Another limitation relates to the fact that the data are based on self-report measures and are subject to both response bias and common method bias. In future studies, a mixed methodology, including measures from different sources (e.g., clinician assessment) and qualitative investigation (e.g., open-ended questions), may help reduce the potential for such bias (Podsakoff et al., 2003).
Furthermore, an analysis of demographic variables not considered here, such as parental education and ethnicity, can contribute important information.
An additional direction for future research would be to examine each of the three self-compassion components separately to determine which variable contributes most significantly to parental feeling and well-being. These and other future studies may have important implications for mental healthcare practice, suggesting parental self-compassion as a target for assessment and therapy.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Angold, A., Messer, S. C., Stangl, D., Farmer, E. M., Costello, E. J., & Burns, B. J. (1998). Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health, 88(1), 75–80. https://doi.org/10.2105/AJPH.88.1.75
Athay, M. M. (2012). Satisfaction with Life Scale (SWLS) in caregivers of clinically-referred youth: Psychometric properties and mediation analysis. Administration and Policy in Mental Health and Mental Health Services Research, 39(1–2), 41–50. https://doi.org/10.1007/s10488-011-0390-8
Barroso, N. E., Mendez, L., Graziano, P. A., & Bagner, D. M. (2018). Parenting stress through the lens of different clinical groups: A systematic review and meta-analysis. Journal of Abnormal Child Psychology, 46(3), 449–461. https://doi.org/10.1007/s10802-017-0313-6
Becker, A., Wang, B., Kunze, B., Otto, C., Schlack, R., Hölling, H., ... & BELLA study group, T. (2018). Normative data of the self-report version of the German strengths and difficulties questionnaire in an epidemiological setting. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie, 46(6), 523-533. https://doi.org/10.1024/1422-4917/a000589
Belfer, M. L. (2008). Child and adolescent mental disorders: The magnitude of the problem across the globe. Journal of Child Psychology and Psychiatry, 49(3), 226–236. https://doi.org/10.1111/j.1469-7610.2007.01855.x
Bögels, S. M., Lehtonen, A., & Restifo, K. (2010). Mindful parenting in mental health care. Mindfulness, 1(2), 107–120. https://doi.org/10.1007/s12671-010-0014-5
Bohadana, G., Morrissey, S., & Paynter, J. (2019). Self-compassion: A novel predictor of stress and quality of life in parents of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 49(10), 4039–4052. https://doi.org/10.1007/s10803-019-04121-x
Bradley, E. G., Hurwitz, S. D., Harvey, E. A., Hodgson, S., & Perugini, E. M. (2013). Factor analytic structure and validity of the parental feelings inventory: A brief report. Journal of Child and Family Studies, 22(6), 801–806.
Buchner, A., Faul, F., & Erdfelder, E. (1998). A priori, post-hoc, and compromise power analyses for MS-DOS (German Version). http://www.psycho.uni-duesseldorf.de/ aap/projects/gpower
Collishaw, S. (2015). Annual research review: Secular trends in child and adolescent mental health. Journal of Child Psychology and Psychiatry, 56, 370–393. https://doi.org/10.1111/jcpp.12372
Crowe, M., Inder, M., Joyce, P., Luty, S., Moor, S., & Carter, J. (2011). Was it something I did wrong? A qualitative analysis of parental perspectives of their child’s bipolar disorder. Journal of Psychiatric and Mental Health Nursing, 18(4), 342–348. https://doi.org/10.1111/j.1365-2850.2010.01673.x
Deater-Deckard, K. (1998). Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice, 5(3), 314–332. https://doi.org/10.1111/j.1469-7610.2012.02582.x
Dubois-Comtois, K., Moss, E., Cyr, C., & Pascuzzo, K. (2013). Behavior problems in middle childhood: The predictive role of maternal distress, child attachment, and mother-child interactions. Journal of Abnormal Child Psychology, 41, 1311–1324. https://doi.org/10.1007/s10802-013-9764-6
Early, T. J., Gregoire, T. K., & McDonald, T. P. (2002). Child functioning and caregiver well-being in families of children with emotional disorders: A longitudinal analysis. Journal of Family Issues, 23, 374–391. https://doi.org/10.1177/0192513X02023003003
Eaton, K., Ohan, J. L., Stritzke, W., & Corrigan, P. W. (2016). Failing to meet the good parent ideal: Self-stigma in parents of children with mental health disorders. Journal of Child and Family Studies, 25, 3109–3123. https://doi.org/10.1007/s10826-016-0459-9
Ekas, N., & Whitman, T. L. (2010). Autism symptom topography and maternal socioemotional functioning. American Journal on Intellectual and Developmental Disabilities, 115(3), 234–249. https://doi.org/10.1352/1944-7558-115.3.234
Gerkensmeyer, J., Perkins, S. M., Day, J., Austin, J. K., Scott, E. L., & Wu, J. (2011). Maternal depressive symptoms when caring for a child with mental health problems. Journal of Child and Family Studies, 20, 685–695. https://doi.org/10.1007/s10826-011-9445-4
Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53, 6–41. https://doi.org/10.1111/bjc.12043
Gilbert, P., & Procter, S. (2006). Compassionate mind training for people with high shame and self-criticism: A pilot study of a group therapy approach. Clinical Psychology and Psychotherapy, 13, 353–379. https://doi.org/10.1002/cpp.507
Goldstein, H. (2003). Multilevel statistical models (3rd ed). Edward Arnold
Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x
Gouveia, M. J., Carona, C., Canavarro, M. C., & Moreira, H. (2016). Self-compassion and dispositional mindfulness are associated with parenting styles and parenting stress: The mediating role of mindful parenting. Mindfulness, 7(3), 700–712. https://doi.org/10.1007/s12671-016-0507-y
Hasson-Ohayona, I., Tuval-Mashiacha, R., Morag-Yaffe, M., Gaziel, M., Schapir, L., Zalsman, G., & Shoval, G. (2014). Parents of adolescents with psychiatric disorders: Insight into the disorder, self-stigma, and parental stress. Comprehensive Psychiatry, 55, 1106–1110. https://doi.org/10.1016/j.comppsych.2010.04.008
He, J. P., Burstein, M., Schmitz, A., & Merikangas, K. R. (2013). The Strengths and Difficulties Questionnaire (SDQ): The factor structure and scale validation in U.S. adolescents. Journal of Abnormal Child Psychology, 41, 583–595. https://doi.org/10.1007/s10802-012-9696-6
Hinshaw, S. P. (2007). The mark of shame: Stigma of mental illness and an agenda for change. Oxford University Press
Hinshaw, S. P., & Stier, A. (2008). Stigma as related to mental disorders. Annual Review of Clinical Psychology, 4, 367–393. https://doi.org/10.1146/ANNUREV.CLINPSY.4.022007.141245
International Wellbeing Group. (2006). Personal wellbeing index (4th ed.). Deakin University.
Jefferson, F. A., Shires, A., & McAloon, J. (2020). Parenting self-compassion: A systematic review and meta-analysis. Mindfulness, 11(9), 2067–2088. https://doi.org/10.1007/s12671-020-01401-x
Koskelainen, M., Sourander, A., & Kaljonen, A. (2000). The Strengths and Difficulties Questionnaire among Finnish school-aged children and adolescents. European Child & Adolescent Psychiatry, 9, 277–284. https://doi.org/10.1007/s007870070031
Lecavalier, L., Leone, S., & Wiltz, J. (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research, 50, 172–183. https://doi.org/10.1111/j.1365-2788.2005.00732.x
Lindgren, E., Söderberg, S., & Skär, L. (2016). Being a parent to a young adult with mental illness in transition to adulthood. Issues in Mental Health Nursing, 37(2), 98–105. https://doi.org/10.3109/01612840.2015.1092621
Mak, W. W. S., & Cheung, R. Y. M. (2012). Psychological distress and subjective burden of caregivers of people with mental illness: The role of affiliate stigma and face concern. Community Mental Health Journal, 48, 270–274. https://doi.org/10.1007/s10597-011-9422-9
McDonald, T. P., Gregoire, T. K., Poertner, J., & Early, T. J. (1997). Building a model of family caregiving for children with emotional disorders. Journal of Emotional and Behavioral Disorders, 5, 138–148. https://doi.org/10.1177/106342669700500302
Moreira, H., Carona, C., Silva, N., Nunes, J., & Canavarro, M. C. (2015a). Exploring the link between maternal attachment-related anxiety and avoidance and mindful parenting: The mediating role of self-compassion. Theory, Research and Practice. Advance online publication. https://doi.org/10.1111/papt.12082
Moreira, H., Gouveia, M. J., Carona, C., Silva, N., & Canavarro, M. C. (2015b). Maternal attachment and children’s quality of life: The mediating role of self-compassion and parenting stress. Journal of Child and Family Studies, 24, 2332–2344. https://doi.org/10.1007/s10826-014-0036-z
Moses, T. (2010). Being treated differently: Stigma experiences with family, peers, and school staff among adolescents with mental health disorders. Social Science & Medicine, 70(7), 985–993. https://doi.org/10.1111/j.1741-3729.2010.00589.x
Muris, P. (2016). A protective factor against mental health problems in youths? A critical note on the assessment of self-compassion. Journal of Child and Family Studies, 25(5), 1461–1465. https://doi.org/10.1007/s10826-015-0315-3
Neece, C. L., Green, S. A., & Baker, B. L. (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. https://doi.org/10.1352/1944-7558-117.1.48
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027
Neff, K. D. (2009). Self-compassion. In M. R. Leary & R. H. Hoyle (Eds.), Handbook of individual differences in social behavior (pp. 561–573). Guilford Press
Neff, K. D. (2012). The science of self-compassion. In C. Germer & R. Siegel (Eds.), Compassion and wisdom in psychotherapy (pp. 79– 92). Guilford Press
Neff, K. D., & Beretvas, S. (2013). The role of self-compassion in romantic relationships. Self and Identity, 12(1), 78–98. https://doi.org/10.1080/15298868.2011.639548
Neff, K. D., & Faso, D. J. (2015). Self-compassion and well-being in parents of children with autism. Mindfulness, 6(4), 938–947. https://doi.org/10.1007/s12671-014-0359-2
Neff, K. D., Rude, S. S., & Kirkpatrick, K. (2007). An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality, 41, 908–916. https://doi.org/10.1016/j.jrp.2006.08.002
Niclasen, J., Teasdale, T. W., Andersen, A.-M.N., Skovgaard, A. M., Elberling, H., & Obel, C. (2012). Psychometric properties of the Danish strength and difficulties questionnaire: The SDQ assessed for more than 70, 000 raters in four different cohorts. PLoS ONE, 7, e32025. https://doi.org/10.1371/journal.pone.0032025
Oruche, U. M., Gerkensmeyer, J., Stephan, L., Wheeler, C. A., & Hanna, K. M. (2012). The described experience of primary caregivers of children with mental health needs. Archives of Psychiatric Nursing, 26(5), 382–391. https://doi.org/10.1016/j.apnu.2011.12.006
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879–903.
Polanczyk, G., Salum, G., Sugaya, L. S., Caye, A., & Rohde, L. A. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56, 345–365. https://doi.org/10.1111/jcpp.12381
Rodriguez, C. M. (2011). Association between independent reports of maternal parenting stress and children’s Internalizing symptomatology. Journal of Child and Family Studies, 20, 631–639. https://doi.org/10.1007/s10826-010-9438-8
Rodríguez-Meirinhos, A., Antolín-Suárez, L., & Oliva, A. (2018). Support needs of families of adolescents with mental illness: A systematic mixed studies review. Archives of Psychiatric Nursing, 32(1), 152–163. https://doi.org/10.1016/j.apnu.2017.09.004
Sirois, F. M., Bögels, S., & Emerson, L. M. (2019). Self-compassion improves parental well-being in response to challenging parenting events. The Journal of Psychology, 153(3), 327–341. https://doi.org/10.1080/00223980.2018.1523123
Smith, A. M., & Grzywacz, J. G. (2014). Health and well-being in midlife parents of children with special health needs. Families, Systems, & Health, 32(3), 303. https://doi.org/10.1037/fsh0000049
Sumiati, N. T. (2018). The influence of self-compassion and coping strategies to subjective well-being of parents with intellectual disabled children. Atlantis Press, 153, 106–110. https://doi.org/10.2991/icddims-17.2018.22
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th ed.). Pearson Education
Van der Sanden, R., Bos, A., Stutterheim, S., Pryor, J., & Kok, G. (2013). Experiences of stigma by association among family members of people with mental illness. Rehabilitation Psychology, 58, 73–80. https://doi.org/10.1037/a0031752
Vaughan, E., Feinn, R., Bernard, S., Brereton, M., & Kaufman, J. S. (2013). Relationships between child emotional and behavioral symptoms and caregiver strain and parenting stress. Journal of Family Issues, 34, 534–556. https://doi.org/10.1177/0192513X12440949
Vohra, R., Madhavan, S., Sambamoorthi, U., & Peter, C. S. (2014). Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism, 18, 815–826. https://doi.org/10.1177/1362361313512902
Westerlund, A., Ivarsson, A., & Richter‐Sundberg, L. (2020). Evidence‐based practice in child and adolescent mental health services: The challenge of implementing national guidelines for treatment of depression and anxiety. Scandinavian Journal of Caring Scienceshttps://doi.org/10.1111/scs.12859
Yarnell, L. M., & Neff, K. D. (2013). Self-compassion, interpersonal conflict resolutions, and well-being. Self and Identity, 12, 146–159. https://doi.org/10.1080/15298868.2011.649545
Author information
Authors and Affiliations
Contributions
VS designed and executed the study, assisted with the data analyses, and wrote the paper. NW designed and executed the study, assisted with the data analyses, and wrote the paper. UY directed execution of the research onsite, including data collection. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics Approval
This research was approved by the Ethics Committee of Ziv Medical Center in Israel. Informed consent was obtained from all individual participants included in the study. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shenaar-Golan, V., Wald, N. & Yatzkar, U. Parenting a Child with Mental Health Problems: the Role of Self-Compassion. Mindfulness 12, 2810–2819 (2021). https://doi.org/10.1007/s12671-021-01744-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-021-01744-z