Abstract
Introduction
Oral cancer ranks sixth place worldwide among other cancers and is known for its high morbidity and mortality rates. Among oral cancer, oral squamous cell carcinomas (OSCC) remains the most common. Expression of specific biomarkers are known to be related to the prognosis of the OSCC.
Methodology
An immunohistochemistry study was performed to evaluate the expression of Cyclin D1 and CENPF for their prognostic significance in twenty OSCC patients. The follow-up period ranged from 10 to 18 months. The expression of these proliferative markers was correlated with demographic, clinical and histopathological grade of the disease.
Results
The results revealed 28% mortality rates in relation to OSCC involving retro-molar trigone. Based on the Cyclin D1 and CENPF expression, high mortality rate (Pearson coefficient = 0.800) was seen with grade 3 and 4 expressions of the markers. Decreased survival rates (Pearson coefficient = 0.824) were observed with stage III and IV disease with grade 3 and 4 expressions of the markers.
Conclusion
Cyclin D1 and CENPF have shown promising results as proliferative markers which can be linked with prognosis of OSCC in this study. Further studies with larger sample size are needed to extrapolate our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral cancer is a leading global cause of morbidity and mortality. According to the GLOBOCAN 2020, the burden of oral cancer in developing countries is highly frequent in South Central Asia and was recorded as 10.2 per 100,000 [1, 2]. 90% of oral carcinoma is squamous cell carcinoma. It results from the multistep accumulation of heterogeneous genetic changes in squamous cells. These changes progressively increase the ability of transformed cells to proliferate and invade. Despite the various treatment modalities available, the overall 5-year survival rate after oral cancer treatment is around 50%. Locoregional recurrence is the most common cause of treatment failure [3].
Though histopathology remains the gold standard for major diagnostic and therapeutic decisions, immunohistochemistry (IHC) aids as an additive tool by detecting gene expression at the protein level. Advances in the understanding of Cancer at the regulatory protein expression level have resulted in the identification of some prognostic tumour biomarkers associated with the clinical outcome of OSCC. There are diverse types of cell and tissue molecular biomarkers that can provide information supportive to data which can be obtained from clinical examination and histopathological studies. Among them, Cyclin D1 and CENPF were chosen for evaluation as they get manifested during various stages of cell cycle proliferation.
The G1 Cyclins (a subtype of Cyclin D1) regulate cell passage through the G1 phase and their entry into the S phase. The CCND1 gene, which encodes Cyclin D1, is a proto-oncogene found on chromosome 11q13. The protein activates CDK4 and CDK6 and triggers pRb to phosphorylate and progress the cell cycle from the G1 to the S phase. CCND1 amplification and overexpression are typical in various types of tumours, including head and neck cancers [4, 5]. Noorlag et al. and Zao et al. observed a correlation between Cyclin D1 overexpression and lymph node metastasis, local recurrence, advanced histological grade (G2/G3) and poor survival [6, 7].
The centromere protein F (CENPF) is a 367-kDa nuclear protein with low expression G0/G1 cells and accumulates in the nuclear matrix during the S-phase with maximal expression G2/M cells. CENPF was identified as a marker of cell proliferation in several human malignancies. In addition, CENPF has been correlated with dysplasia grade and ploidy status, although, unlike Cyclin D1, it has not been correlated with malignant transformation in oral cancers.
Studies pertaining to Cyclin D1 are scarce in scientific literature, and the role of CENPF has not been studied in oral potentially malignant disorders and OSCC. Therefore, this study aimed to evaluate the expression of Cyclin D1 and CENPF in a single cohort of patients with oral squamous cell carcinomas (OSCC) and relate them to clinical-pathologic characteristics and patient outcome.
Patients and Methods
Patient Population
This observational study included 20 patients diagnosed and treated for primary OSCC at Vinayaka Mission's Sankarachariyar Dental College. The study was undertaken following the approval of the institutional ethical board of the Vinayaka Mission’s Sankarachariyar Dental College, (VMRF-DU) (IEC Ref.no: VMSDC/IEC/Approval No.204). All samples were obtained with informed consent from the participants.
Data collection of patients were taken from the case registers, which included age, gender, tumour location, TNM stage classification (8th edition of the American Joint Committee on Cancer). Tissues were fixed in 10% buffered formalin, which was further processed for haematoxylin and eosin staining. Immunohistochemistry analysis was conducted in the Department of Oral Pathology and Microbiology, SRIHER- DU.
Immunohistochemistry
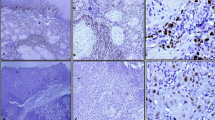
Immunohistochemical staining was carried out manually in the IHC laboratory. Five-μm-thick tissue sections of formalin-fixed paraffin tissue were mounted on APES (3-aminopropyl triethoxy silane)-coated charged frosted slide (Leica biosystem). Deparaffinization with xylene and dehydration through alcohol was followed by blocking tissue endogenous peroxidase activity with 0.3% hydrogen peroxide. Antigen retrieval was done by autoclaving in sodium citrate buffer (pH 6.0). The sections were incubated with the primary antibodies (Dako Monoclonal Mouse Anti-Human Cyclin D1 and Monoclonal mouse Anti-CENPF). The sections were stained using the modified labelled avidin–biotin (LAB) technique of the DakoTMLSAB kit with DAB (3.3'-diaminobenzidine) as the chromogen and counterstained with Harris haematoxylin and mounted with DPX.
Evaluation of Immunohistochemistry Expression
The immunohistochemistry expressions were evaluated by two senior oral and maxillofacial pathologists. The presence of brown-coloured cells showed positive immunoreactivity. In each slide, selection of ten hot spots was done under higher (400 ×) magnification. The IHC-positive tumour cells were calculated, and the mean percentage per slide was determined. A grading index ranging from 1 to 4 was given for the percentage of positive cells. Grade 1-(0–25%) positive stained cells: Grade 2-(26–50%); Grade 3-(51–75%); Grade 4-(76–100%) [8].
Follow-Up Evaluation
The average follow-up period was 13.65 months, ranging from 10 to 18 months. The patients diagnosed with oral squamous cell carcinoma underwent surgery, radiotherapy and/or chemotherapy as decided by the tumour board. Based on the survival of the patients (with or without disease) and death rate, the data were analysed statistically with Pearson coefficients.
Results
Among the 20 OSCC patients, the 55% were between 45 and 55 years and 45% were between 55 and 65 years. Patients within 45–55 years had higher survival rate by 81% than 55–65 years. There were 12 males (60%) and 8 females (40%) with a mean age of 54 years (54 ± 6.22). Comparing the follow-up status based on the gender of the patient, the death rate among males (33%) was higher while 25% of females were alive with the disease and 62% of females were alive without the disease (Fig. 1). At the end of the research, 8 (66%) of male patients and 7 (87%) of female patients were alive. The males in this study had a mean survival time of 14 to 18 months (Fig. 2).
The most prevalent site of the tumour in our study was lower retromolar trigone (35%) and gingivobuccal sulcus (GBS) (35%), followed by buccal mucosa (30%). Patients with the retro molar trigone (Fig. 3) as the site of the lesion reported a 28% mortality rate, with 5 patients dead and the remaining 2 patients alive with disease. Significantly mortality or survival distribution differed between the three sites (P = 0.029). Mean survival time among patients with RMT disease was 40% up to 16 months.
According to the TNM staging, 10 patients (50%) were in Stage 4 followed by 8 (40%) in stage 3 and 2 (10%) were in stage 2. The increasing stage of disease correlated with increased death rate which showed statistical significance of Pearson correlation of 0.824 with the expression of the markers.
The follow-up of 20 OSCC patients was done for 10–18 months. The maximum number of patients follow-up was done at the 16th month followed by the 12th month. The comparison of Cyclin D1 grading during the last follow-up status showed 40% of patients with grade 4 and 25% in grades 2 and 3. Cyclin D1 survival distribution between grade 1 and 2 was not statistically significant. The CENPF score compared during the last follow-up showed 35% with grade 4 and 15% were in grade 3. Increasing expression Cyclin D1 and CENPF expression was correlated with increasing stages of the disease with correlation coefficient of 0.800 and P value of 0.00. Survival analysis showed statistically significant association between Cyclin D1 and CENPF grading with disease-free survival, which clinically infers that the high Cyclin D1 and CENPF grading indicates low disease-free survival (Table 1, Figs. 4, 5).
Discussion
Tumourigenesis is associated with genetic alterations in cell cycle molecules that control cell cycle activity. Understanding the mechanism of tumourigenesis may contribute to the identification of new proteins that can be used as cancer diagnostic and prognostic markers, as well as potential targets for treatment therapies in OSCC patients. Our study was on the expression of Cyclin D1 and CENPF in oral squamous cell carcinoma patients and correlate the expression of the markers with physiological, pathologic and prognosis characteristics of patients who were managed and followed up for a period of 10 to 18 months.
In our study, it was found that males (60%) were more affected than females (40%). The mortality rate was also found to be higher in males (80%) compared to females (20%). This result was similar to the studies done by Khandekar et al. [9], Ganesh et al. [10]. Higher male predominance in our cohort may be due to the high prevalence of tobacco consumption among males [11, 12].
In the present study, it was found that the patients were between 5th (55%) and 7th (45%) decade of life, similar to the study conducted by Ganesh et al. [10]. The high incidence of oral cancer between 45 and 65 years of age indicates that people in this age group were exposed to the most harmful etiological factors for cancer development, such as tobacco, alcohol, paan, Betel nuts, poor oral hygiene and dentures. The level of cell instability increases with age, so a stimulus that in a younger age group would go unnoticed could induce a change in an older age group that may cause malignancy [13].
In our study, it was found that the major sites were the retromolar trigone (35%), lower gingivobuccal sulcus (35%) and the buccal mucosa (30%). As the result of the habit of placing the tobacco quid in the lower gingivobuccal sulcus (GBS), GBS carcinoma also known "Indian oral cancer" is the most common type of oral cancer in the Indian subcontinent as seen in our study group [13]. It is also noted that patients with cancer in the retromolar area were found to have a higher mortality rate (71%) than the patients with other sites. Late-stage presentation of the lesion, absence of early symptoms and involvement of adjacent subsites along with the bone invasion were the attributed causes for this high mortality rate.
Studies done by Anna et al. coincide with the results of present study with respect to cancer staging and survival [14]. In our study, 50% of the patients were in stage IV, 40% in stage III and 10% in stage II. The mean survival rate was higher in stage II patients, (50%) in our study which was similar to Santos et al. and Bórquez et al. [11, 12]. In stage I of the disease (T1N0), cure rate of Oral SCC was 80% while it decreased to 20% in stage IV [15, 16]. Obviously early detection of oral cancer is crucial to improving survival rates.
Cyclin D1 and CENPF are molecules that show a pivotal role in cell cycle control, and its overexpressions are common genetic event in OSCC. Therefore, their relation to site and survival rates obtains more accurate information about the clinical importance of these proteins in OSCC. In the present study, the Cyclin D1 proteins were highly expressed in 40% of OSCC patients. Our results showed that Cyclin D1 expression has been associated with several clinical and pathological stages of tumour development such as site, clinical stage and histological grade. In the present study, the Cyclin D1 expression was more in retromolar region similar to the studies of Lam and Akerval et al. [17, 18]. Based on gender, Cyclin D1 expression in males (60%) was higher although it was not statistically significant. Our findings were similar to the studies conducted by Lam et al. and Luis et al. [17, 19]. Punya et al. [20] reported an association of Cyclin D1 with histological grade. In our study, the patients with Cyclin D1 grade 3 and grade 4 were in the stage IV of the disease. Our study provides new insight into the relationship between overexpression of Cyclin D1 with respect to prognosis. We observed that OSCC patients with high expression of Cyclin D1 in their cell tumours presented a significantly lower survival rate.
There were very few studies regarding CENPF and OSCC in the scientific literature. Guardia et al. and Chen et al. stated that no correlation was noted between CENPF amplification and clinicopathologic parameters in OSCC [21, 22]. However, in our study, the correlation of CENPF expression with site and stage was shown as 35% with lesions involving RMT and with stage IV disease. In some other studies, CENPF expression was associated with poor prognosis in breast cancer and prostate Cancer [23, 24]. In our study, it is found that the high expression of the CENPF had worse survival rate. It was similar to the study reported by Li et al. in lung carcinoma [25].
As seen in our cohort, gender and age had no statistical significance on the follow-up status of oral cancer patients at 10 to 18 months. In this cohort, it was observed that stage III, IV of OSCC and Carcinoma RMT had high mortality rate which was statistically significant. Although no statistical significance was seen with the expression of Cyclin D1 and CENPF as seen in stages III and IV of OSCC which correlated with a higher mortality rate. This could be because of the sample size, and hence the study may have to be done with larger sample to reiterate our findings.
Conclusion
The two proteins Cyclin D1 and CENPF are indeed expressed in the oral squamous cell carcinoma. Through this study, it was understood that these two proliferative markers that are involved in the proliferation stage of cell cycle correlate with the prognosis of the disease, when it occurs at stage III or IV especially in the retromolar trigone.
References
Ferlay J, Ervik M, Lam F, et al. (eds) (2020) Global cancer observatory: cancer today. International Agency for Research on Cancer. Accessed 25 Nov 2020. gco.iarc.fr/today
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Pignon JP, le Maître A, Maillard E, Bourhis J (2009) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomized trials 17,346 patients. Radiother Oncol 92(1):4–14. https://doi.org/10.1016/j.radonc.2009.04.014
Monteiro LS, Diniz-Freitas M, Warnakulasuriya S, Garcia-Caballero T, Forteza-Vila J, Fraga M (2018) Prognostic significance of cyclins A2, B1, D1, and E1 and CCND1 numerical aberrations in oral squamous cell carcinomas. Anal Cell Pathol (Amst) 2018:7253510. https://doi.org/10.1155/2018/7253510
Choi Y, Anders L (2014) Signaling through cyclin D-dependent kinases. Oncogene 33:1890–1903. https://doi.org/10.1038/onc.2013.137
Noorlag R, van Kempen PM, Stegeman I, Koole R, van Es RJ, Willems SM (2015) The diagnostic value of 11q13 amplification and protein expression in the detection of nodal metastasis from oral squamous cell carcinoma: a systematic review and meta-analysis. Virchows Arch 466(4):363–373
Zhao Y, Yu D, Li H et al (2014) Cyclin D1 overexpression is associated with poor clinicopathological outcome and survival in oral squamous cell carcinoma in Asian populations: insights from a meta-analysis. PLoS ONE 9(3):e3210
John RR et al (2018) Evaluation of the role played by Cyclin D1 as a diagnostic and prognostic marker in the progression of oral carcinogenesis. J Maxillofac Oral Surg 17(3):389–395. https://doi.org/10.1007/s12663-018-1087-2
Khandekar SP, Bagdey PS, Tiwari RR (2006) Oral cancer and some epidemiological factors: a hospital-based study. Indian J Community Med 31:157–159
Ganesh R, John J, Saravanan S (2013) Socio-demographic profile of oral cancer patients residing in Tamil Nadu—a hospital-based study. Indian J Cancer 50:9. https://doi.org/10.4103/0019-509x.112270
Santos VTG, Santos VS, Cravalho RAS, Guedes SAG, Trento CL (2013) Mortality from oral cancer in Aracaju/SE. In: Aracaju/SE, vol 42, pp 204–210. Rev Odontol UNESP, Brazil. View at: Google Scholar
Bórquez P, Capdeville F, Madrid A, Veloso M, Cßrcamo M (2011) Analysis of survival of 137 patients with oral cancer. Rev Chil Cir 63(4):351–355
Misra S, Chaturvedi A, Misra NC (2008) Management of gingivobuccal complex cancer. Ann R Coll Surg Engl 90:546–553 ([Europe PMC free article] [Abstract] [Google Scholar])
Le Campion ACOV, Ribeiro CMB, Luiz RR, da Silva Júnior FF, Barros HCS, de Cássia Batista dos Santos K, Ferreira SJ, Gonçalves LS, Ferreira SMS (2017) Low survival rates of oral and oropharyngeal squamous cell carcinoma. Int J Dent. https://doi.org/10.1155/2017/5815493
Rogers SN, Brown JS, Woolgar JA et al (2009) Survival following primary surgery for oral cancer. Oral Oncol 45(3):201–211
van der Waal I, de Bree R, Brakenhoff R, Coebergh J-W (2011) Early diagnosis in primary oral cancer: is it possible? Medicina Oral, Patologia Oral y Cirugia Bucal 16(3):e300–e305
Lam KY, Ng IO, Yuen AP, Kwong DL, Wei W (2000) Cyclin D1 expression in oral squamous cell carcinomas: clinicopathological relevance and correlation with p53 expression. J Oral Pathol Med 29(4):167–172. https://doi.org/10.1034/j.1600-0714.2000.290404.x
Akervall JA, Michalides RJ, Mineta H et al (1997) Amplification of Cyclin D1 in squamous cell carcinoma of the head and neck and the prognostic value of chromosomal abnormalities and Cyclin D1 overexpression. Cancer 79:380–389
Monteiro LS, Diniz-Freitas M, Warnakulasuriya S, Garcia-Caballero T, Forteza-Vila J, Fraga M (2018) Prognostic significance of Cyclins A2, B1, D1, and E1 and CCND1 numerical aberrations in oral squamous cell carcinomas. Anal Cell Pathol. https://doi.org/10.1155/2018/7253510
Angadi Punnya V, Krishnapillai R (2007) Cyclin D1 expression in oral squamous cell carcinoma and verrucous carcinoma: correlation with histological differentiation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(3):e30–e35. https://doi.org/10.1016/j.tripleo.2006.09.011
de la Guardia C, Casiano CA, Trinidad-Pinedo J, Báez A (2001) CENP-F gene amplification and overexpression in head and neck squamous cell carcinomas. Head Neck 23(2):104–112. https://doi.org/10.1002/1097-0347(200102)23:2%3c104::aid-hed1005%3e3.0.co;2-0
Chen W, Cui Q, Zhang Q, Zou Z, Sun S, Yuan K (2017) Centromere protein F (CENPF) is upregulated and related to tumor differentiation in laryngeal squamous cell carcinoma. Transl Cancer Res 6(5):920–928
O’Brien SL, Fagan A, Fox EJ, Millikan RC, Culhane AC, Brennan DJ, McCann AH, Hegarty S, Moyna S, Duffy MJ, Higgins DG, Jirström K, Landberg G, Gallagher WM (2007) CENP-F expression is associated with poor prognosis and chromosomal instability in patients with primary breast cancer. Int J Cancer 120(7):1434–1443. https://doi.org/10.1002/ijc.22413
Zhuo Y, Xi M, Wan Y, Hua W, Liu Y, Wan S, Zhou Y, Luo H, Wu S, Zhong W, Wu C (2015) Enhanced expression of centromere protein F predicts clinical progression and prognosis in patients with prostate cancer. Int J Mol Med 35:966–972. https://doi.org/10.3892/ijmm.2015.2086
Li MX, Zhang MY, Dong HH, Li AJ, Teng HF, Liu AL, Xu N, Qu YQ (2021) Overexpression of CENPF is associated with progression and poor prognosis of lung adenocarcinoma. Int J Med Sci 18(2):494–504. https://doi.org/10.7150/ijms.49041
Funding
This Research Project was supported by the Vinayaka Mission’s Research Foundation (VMRF-DU) Seed Money Grant (Grant Number-VMRF/SeedMoney/2020/VMSDC-Salem/8).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The concepts, designs and methodology for this study were approved by Ethical committee of the institution. This study was ethically approved with Reference Number: VMSDC/IEC/Approval No.204.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
John, R.R., Sam, N. & Chandrasekaran, B. Prognostic Significance of Proliferative Markers: Cyclin D1 and CENPF in Oral Squamous Cell Carcinoma Patients—A Cohort Study. J. Maxillofac. Oral Surg. 22, 734–740 (2023). https://doi.org/10.1007/s12663-023-01884-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-023-01884-w