Abstract
Mastitis is the most economically important disease affecting the dairy industry worldwide. Lactobacillus plantarum, an important probiotic with a wide range of applications, has potential anti-inflammatory properties and has become a currently strong candidate for mastitis therapies. In the current study, we evaluated the prevention effect of Lactobacillus plantarum 17–5 on Escherichia coli-induced mastitis in mice. The results showed that pretreatment with L. plantarum 17–5 maintained the integrity of tight junctions; improved inflammatory injury; decreased MPO activity and the mRNA expression levels of IL1β, IL6, and TNFα; and inhibited the NF-κB and MAPK signaling pathways in mice mammary tissue. The results indicated that Lactobacillus plantarum 17–5 had excellent anti-inflammatory activities and could be developed into microecological preparation for clinical use to prevent mastitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dairy cow mastitis is an inflammatory disease worldwide and causes severe economic losses in the dairy industry due to decreased milk production, higher veterinary care costs, and increased culling of dairy cows [1, 2]. Escherichia coli is one of the main pathogens in dairy cow mastitis and is widely present in bovine feces, humid soil, and composts [3]. Recent studies revealed that E. coli often causes acute inflammatory responses and might contribute to extensive mammary tissue damage [4]. There are currently no medications or other prophylactic methods effective against this disease, and common treatments are antibiotic treatment [5]. However, misuse of antibiotics inevitably leads to multi-antibiotic resistance and antibiotic residue, which causes threats to human and animal health globally [6]. Therefore, there is an urgent need to find effective and safe alternative antimicrobial agents for conventional antibiotics.
Lactobacillus plantarum is one of the most widely used probiotics with great beneficial effects on human and animal health [7]. Existing studies have shown that L. plantarum can produce lactic acid and various metabolites during colonization, which can effectively abrogate pathogenic bacteria growth and modulate immune functions [8]. In addition, some metabolites of L. plantarum may have anti-inflammatory properties in addition to their antimicrobial effects; this feature provides its therapeutic potential for various inflammatory diseases [9]. Fernsndez et al. found that oral administration of L. salivarius PS2 positively affected the prevention of infectious mastitis in late pregnancy [10]. Frola et al. have stated that intramammary infusion of L. plantarum CRL 1716 was an effective way of treating dairy cow mastitis [11]. Previous studies performed by our research team showed that L. plantarum 17–5 could attenuate E. coli-induced inflammatory responses in bovine mammary epithelial cells [12]. However, the effect of intramammary infusion of L. plantarum 17–5 on mice mastitis and its mechanism of action remains unclear. Here, our study establishes the murine model of mastitis using E. coli. The aim is to determine whether L. plantarum 17–5 has prevention effects on mastitis in vivo and provide a basis for developing and utilizing microecological agents.
Materials and Methods
Bacteria and the Culture Conditions
The Lactobacillus plantarum 17–5 strain (ATCC 8014, provided by American Type Culture Collection, Manassas, VA, USA) was cultivated statically in de Man, Rogosa, and Sharpe (MRS) broth (Aobox, Beijing, China) at 37 ℃ under microaerobic conditions. Escherichia coli O111:K58 (CVCC1450, provided by China Constitute of Veterinary Drug Centre, Beijing, China) was grown overnight in Luria Broth (LB) medium (Aobox, Beijing, China) at 37 ℃ with shaking. The number of colony-forming units (CFUs) was counted after three generations.
Animals and Experiment Design
SPF-grade male and female Kunming mice (8 weeks old) were purchased from Liaoning Changsheng Biotechnology Corporation (Benxi, China). Females and males were placed in the same microisolator cage at a ratio of 2:1 until the females were pregnant, and water and food were provided ad libitum. Animal assays were approved by the Animal Ethics Committee of Hebei Agricultural University (protocol number 2020044). The mouse mastitis model was established by referring to previous studies [13, 14]. Briefly, after ether anesthesia, the tip of the L4 and R4 abdominal mammary glands was carefully snipped, and bacteria or PBS was injected into the mammary ducts 7 days after delivery. The lactating mice were randomly divided into six groups (n = 8): the control group (PBS), the E. coli group (107 CFU/100 µL), L. plantarum (105, 106, and 107 CFU/100 µL) + E. coli and the L. plantarum group (107 CFU/100 µL). The L. plantarum or PBS was injected into each side of the nipple for 3 h prior to adding E. coli and then injected with E. coli using the same method. At 24 h after the last injection, mice were sacrificed, and the mammary gland tissues were collected and stored at − 80 ℃ until further analysis.
Histopathological Evaluation
The mammary tissues of the mice were observed for general condition and scored using a clinical scoring system ranging from 1 to 5, with higher scores indicating greater tissue damage. Specifically, 1 represents no damage, 2 represents slight redness, 3 represents slight redness and minor bleeding, 4 represents moderate redness and bleeding, and 5 represents severe redness and bleeding. Subsequently, tissue samples were fixed in 4% paraformaldehyde solution, dehydrated with gradient ethanol, and then embedded in paraffin.
The paraffin-embedded tissue sections were cut into 5 µm thickness, stained with hematoxylin and eosin (HE), and examined under an optical microscope. The same histological score (1 to 5) previously described was used for evaluating the degrees of tissue damage (necrosis and neutrophil and macrophage infiltration). The higher the score, the more serious the injury.
Immunofluorescence Staining
Paraffin sections were dewaxed with water, antigen repaired with sodium citrate, and blocked with 5% BSA (Solarbio, Beijing, China). Then, slides were incubated with primary antibody against claudin-3 (1:500; Bioss, Beijing, China) overnight at 4 ℃, then in FITC-labeled secondary antibody (1:200; Solarbio, Beijing, China) for 1 h at room temperature. After counterstaining with DAPI (Solarbio, Beijing, China), the fluorescence was observed under a fluorescence microscope.
MPO Activity Determination
The mammary tissues were homogenized, and the homogenates were centrifuged at 2500 rpm for 10 min at 4 ℃ to obtain supernatants. The activity of MPO in mammary tissue homogenates was assayed using MPO Detection Kit (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) according to the manufacturer’s protocol.
qRT–PCR Analysis
Total RNA was extracted from mammary tissue using the Ultrapure RNA extraction kit (CWBio, Beijing, China). The concentration and purity of RNA samples were measured by NanoDrop-2000 (Thermo Scientific, DE, USA), and the integrity was detected by agarose gel electrophoresis. Then, RNA was reversely transcribed into cDNA using a reverse transcription kit (US Everbright Inc, CA, USA), and quantitative real-time PCR was performed according to the following procedures: 300 s at 95 ℃ followed by 45 cycles of 5 s at 95 ℃, 30 s at 57 ℃ and 15 s at 72 ℃. The efficiency of the amplification was evaluated by establishing the standard curve. Gene relative expression levels were calculated using the 2−ΔΔCt method and normalized to the expression of GAPDH and β-actin. Primer sequences were listed in Table 1.
Western Blot Analysis
Total protein from mammary tissue was extracted using RIPA lysis buffer (Solarbio, Beijing, China), and its concentration was quantified by BCA protein assay kit (Solarbio, Beijing, China). A total of 30 µg of protein from each sample were separated by 10% SDS-PAGE gels, electrotransferred onto nitrocellulose membranes (Beyotime, Shanghai, China) and then blocked with 5% skim milk. The membranes were incubated with primary antibodies against claudin-3 (1:1000), occludin (1:1000), NF-κB p65 (1:1000), NF-κB phospho-p65 (1:1000), phospho-IκBα (1:500), and β-actin (1:1000) from Bioss Biotech Limited Company (Beijing, China) and antibodies against p38 (1:1000), phospho-p38 (1:1000), ERK (1:1000), phospho-ERK (1:2000), JNK (1:1000), phospho-JNK (1:1000), and IκBα (1:1000) from Cell Signaling Technology (MA, USA). After incubation with a secondary antibody (1:2000; Zhongshan Golden Bridge, Beijing, China), the NBT/BCIP color development kit (Solarbio, Beijing, China) was used to visualize the stainings, and ImageJ software (ImageJ Software Inc., MD, USA) was used for densitometric analyses of western blot bands.
Statistical Analysis
All data in this study was shown as means ± standard error of the mean (SEM). Comparisons between multiple independent groups were performed by one-way ANOVA and Tukey’s or Dunnett’s T3 tests. P values < 0.05 were considered significantly different.
Results
Effect of L. plantarum 17–5 on Histopathological Changes in Mice Mammary Tissue
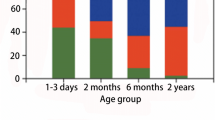
No visible redness, swelling, or bleeding were seen in the mammary tissues in the control group, high dose of L. plantarum pretreatment group, and the L. plantarum group, and the tissue injury scores were significantly lower (P < 0.05) in three doses of L. plantarum pretreatment groups compared with the E. coli group (Fig. 1). Obvious inflammatory changes were observed in the mammary tissues of the E. coli group with infiltration of neutrophils and macrophages in the mammary acini, ducts, and connective tissue. However, these histopathological changes were ameliorated in the L. plantarum pretreatment group, with a significant reduction (P < 0.05) in histological scores among medium and high doses of L. plantarum pretreatment groups (Fig. 2).
Effect of L. plantarum 17–5 on the histopathological impairment in the mice mammary tissue. A The control group. B The E. coli group. C–E 105, 106, and 107 CFU/100 µL L. plantarum + E. coli group. F The L. plantarum group. The injury score from each group ranged from 1 to 5 with higher scores indicating greater tissue damage. Data shown as means ± SEM (n = 5) and different letters indicate significance at P < 0.05. The same as the following figures
Effect of L. plantarum 17–5 on the histopathological changes in the mice mammary tissue (H&E 100 ×). A The control group. B The E. coli group. C–E 105, 106, and 107 CFU/100 µL L. plantarum + E. coli group. F The L. plantarum group. Scale bars: 100 µm. The histological score from each group ranged from 1 to 5 with higher scores indicating greater tissue damage. Data were the mean ± SEM (n = 5)
Effect of L. plantarum 17–5 on the MPO Activity in the Mammary Glands
As shown in Fig. 3, the MPO activity in the E. coli group increased significantly (P < 0.05) compared with the control group. Pretreatment with different doses of L. plantarum 17–5 significantly (P < 0.05) reduced these increases.
Effect of L. plantarum 17–5 on Tight Junction Proteins in the Mammary Glands
Immunofluorescence staining for the claudin-3 was performed in mammary gland sections (Fig. 4A). In control and L. Plantarum groups, claudin-3 was localized to the cell membrane at cell–cell contacts and showed a complete and continuous structure. In the E. coli group, the claudin-3 positive signals were intermittent and markedly weaker than the above groups showing that the tight junctions were disrupted. Pretreatment with L. plantarum alleviated the E. coli-induced damage in tight junction proteins.
Effects of L. plantarum 17–5 on the structure and protein expression in the tight junction proteins. A Representative images of the FITC albumin staining in each group. Green shows the claudin-3 signal and blue shows the DAPI signal. (a) The control group. (b) The E. coli group. (c-e) 105, 106, and 107 CFU/100 µL L. plantarum + E. coli group. (f) The L. plantarum group. Scale bars: 100 µm. B Representative western blots showed expression of claudin-3 and occludin in each group. Data were expressed as means ± SEM from three independent experiments
To further evaluate the effect of L. plantarum 17–5 on tight junction protein level, we examined the levels of claudin-3 and occludin by western blot (Fig. 4B). As expected, the protein levels of claudin-3 and occludin in the E. coli group were significantly (P < 0.05) lower than those in the control group. However, the reduction of claudin-3 and occludin levels was alleviated in the L. plantarum pretreatment group.
Effect of L. plantarum 17–5 on the mRNA Expression of Inflammatory Cytokines in the Mammary Glands
The results in Fig. 5 showed that the expression levels of IL1β, IL6, and TNFα in the E. coli group were significantly (P < 0.05) enhanced. However, these E. coli-induced expression alterations were partially inhibited (P < 0.05) by pretreatment with L. plantarum 17–5.
Protein Expression of the NF-κB and MAPK Signaling Pathways in the Mammary Glands
The western blot analysis of NF-κB and MAPK signaling pathway protein expression is shown in Figs. 6 and 7. The results showed that compared with the control group, the phosphorylation levels of p65, IκBα, p38, ERK, and JNK increased significantly (P < 0.05) after E. coli stimulation. However, the L. Plantarum pretreatment group suppressed these increases to varying degrees.
Discussion
E. coli is the most common environmental pathogen causing dairy cow mastitis in dairy herds [3]. Coliform mastitis is often characterized by a severe local and systemic inflammatory response, which causes huge economic losses for dairy farmers due to reduced milk production and premature culling [15]. Lactobacillus plantarum has been continuously studied as a potential novel anti-inflammatory agent. The current studies show that L. plantarum can produce organic acids and bacteriocins, inhibit the growth of different pathogens, and exert an anti-inflammatory effect during the proliferation process [16]. At present, the management of dairy cow mastitis is predominantly accomplished through intramammary infusion [17, 18]. Although some scholars have expressed concerns about the intramammary infusion of active probiotics [19], more and more studies have shown that intramammary injection of Lactococcus not induces inflammation but enhances the expression of immune proteins in the mammary glands of healthy cows [20, 21]. Thus, this study explores the preventive effect of intramammary infusion of L. plantarum 17–5 on mice mastitis and sets the L. plantarum group to verify the safety of this method.
Mastitis is characterized by the destruction of the acinar structure and neutrophil infiltration in mammary tissue, accompanied by the secretion of pro-inflammatory factors [22, 23]. We next performed the histological evaluation of mice mammary glands to evaluate the effect of L. plantarum 17–5 on histological changes in mice mammary tissue. The results showed that the mammary gland tissue in the E. coli group had obvious redness, swelling and bleeding, and massive infiltration of inflammatory cells in the mammary tissue. However, these characteristics were significantly attenuated in the L. plantarum pretreatment group. This indicated that L. plantarum 17–5 might protect against inflammation and was consistent with the report by Chen et al. that Lactobacillus plantarum can alleviate the inflammatory response of LPS-induced murine mastitis [7]. Notably, there were no obvious pathological changes in the mammary gland tissue in the L. plantarum 17–5 group, indicating that Lactobacillus plantarum 17–5 does not cause an inflammatory response in mice mammary tissue; this is coincident with previously reported results [20].
The blood–milk barrier is an important physical barrier in organisms, which maintains normal lactation function and is an important barrier against pathogen invasion [24, 25]. The integrity of the blood–milk barrier primarily depends on mammary epithelial tight junctions (TJs) [26]. There are studies indicating that inflammation can disrupt the integrity of TJs and increase its permeability [27, 28]. To investigate the effect of Lactobacillus plantarum 17–5 on TJs in mice mammary tissue, we focused on changes in the transmembrane protein family claudin-3 and occludin closely related to TJs. Immunofluorescence staining showed that the claudin-3 signal in the E. coli group was significantly weakened, and the tight junction structure was disrupted. In contrast, the claudin-3 signal in the L. plantarum 17–5 pretreatment group appeared stronger, and the tight junction structure was improved to some extent. Subsequently, we further detected the protein levels of claudin-3 and occludin in mice mammary tissue by western blot. As expected, claudin-3 and occludin levels were lower in the E. coli group and higher in the L. plantarum 17–5 pretreatment group, this suggests that the loss of aforementioned proteins led to the decrease in claudin-3 and occludin levels seen in the E. coli group. Similar findings were yielded by Zheng et al. [29].
MPO plays an important role in the process of inflammatory cells resisting microbial infection and is an important indicator for assessing neutrophil infiltration and damage in tissues [30]. In the present study, MPO activity was significantly higher in the E. coli group, indicating that inflammatory cells clustered around the injection site; this also validates the histopathological changes in mammary gland sections. Pretreatment with L. plantarum 17–5 could decrease the elevation of MPO activity, further ameliorating the aggregation of inflammatory cells and inflammatory injury in mice mammary tissue; this corresponds to previous reports [31]. Moreover, some pro-inflammatory cytokines such as IL1β, IL6, and TNFα are involved in the induction, amplification, and regulation of other inflammatory factors and play an important role in the development of inflammation and pathological processes [32,33,34]. Previous studies have shown that L. plantarum can reduce the secretion of IL1β, IL6, and TNFα in the mammary tissue [7]. Our results also indicated that L. plantarum 17–5 could inhibit the expression of the above cytokines and alleviate the inflammatory process in E. coli-induced mastitis.
To further clarify the mechanism of L. plantarum anti-inflammatory, we next detected the NF-κB and MAPK signaling pathways. NF-κB is a transcription factor with various biological activities involved in cell differentiation, inflammation, and immunomodulation [35, 36]. NF-κB normally exists in the cytoplasm in the inactive state; when stimulated by upstream signals, IκBα is rapidly degraded, and NF-κB is released into the nucleus to regulate downstream genes. Simultaneously, this effect is accompanied by increases in NF-κB and IκB phosphorylation [37]. In addition, the MAPK signaling pathways, which include p38 MAPK, ERK1/2, and JNK, are regulated by diverse transduction cascades [38]. It regulates inflammatory genes via phosphorylation of ERK, JNK, and p38 [39, 40]. In this study, we demonstrated that E. coli activated the NF-κB and MAPK signaling pathways in mice mammary tissue. However, pretreatment with L. plantarum 17–5 inhibited the phosphorylation levels of key proteins in these pathways. We speculate that the anti-inflammatory effect of L. plantarum 17–5 may involve inhibiting the NF-κB and MAPK signaling pathways.
Conclusion
In summary, our study indicated that pretreatment with L. plantarum 17–5 could alleviate inflammatory damage to the mammary tissue, decrease the expression of pro-inflammatory genes, and inhibit the activation of the NF-κB and MAPK signaling pathways in mice mammary tissue. Therefore, we believe that L. plantarum 17–5 has protective effects against E. coli-induced mastitis in mice and may be useful as a potential therapeutic agent for mastitis. Finally, a more comprehensive model evaluation should be conducted in vivo to advance their clinical applications further.
Data Availability
The original, full-length western blots were listed in the supplementary information (Additional file 1). Data generated during the presented study are available from the corresponding author (YZM) upon reasonable request.
References
Jamali H, Barkema HW, Jacques M, Lavallée-Bourget EM, Malouin F, Saini V, Stryhn H, Dufour S (2018) Invited review: incidence, risk factors, and effects of clinical mastitis recurrence in dairy cows. J Dairy Sci 101:4729–4746. https://doi.org/10.3168/jds.2017-13730
Ashraf A, Imran M (2018) Diagnosis of bovine mastitis: from laboratory to farm. Trop Anim Health Prod 50:1193–1202. https://doi.org/10.1007/s11250-018-1629-0
Gao J, Barkema HW, Zhang L, Liu G, Deng Z, Cai L, Shan R, Zhang S, Zou J, Kastelic JP, Han B (2017) Incidence of clinical mastitis and distribution of pathogens on large Chinese dairy farms. J Dairy Sci 100:4797–4806. https://doi.org/10.3168/jds.2016-12334
Zhao X, Lacasse P (2008) Mammary tissue damage during bovine mastitis: causes and control. J Anim Sci 86:57–65. https://doi.org/10.2527/jas.2007-0302
Barlow J (2011) Mastitis therapy and antimicrobial susceptibility: a multispecies review with a focus on antibiotic treatment of mastitis in dairy cattle. J Mammary Gland Biol Neoplasia 16:383–407. https://doi.org/10.1007/s10911-011-9235-z
Muziasari WI, Pitkänen LK, Sørum H, Stedtfeld RD, Tiedje JM, Virta M (2016) The resistome of farmed fish feces contributes to the enrichment of antibiotic resistance genes in sediments below baltic sea fish farms. Front Microbiol 7:2137. https://doi.org/10.3389/fmicb.2016.02137
Chen Q, Wang S, Guo J, Xie Q, Evivie SE, Song Y, Li B, Huo G (2021) The protective effects of Lactobacillus plantarum Klds 1.0344 on Lps-induced mastitis in vitro and in vivo. Front Immunol 12: 770822. https://doi.org/10.3389/fimmu.2021.770822
Peter K, Rehli M, Singer K, Renner-Sattler K, Kreutz M (2015) Lactic acid delays the inflammatory response of human monocytes. Biochem Biophys Res Commun 457:412–418. https://doi.org/10.1016/j.bbrc.2015.01.005
Yeganegi M, Watson CS, Martins A, Kim SO, Reid G, Challis JR, Bocking AD (2009) Effect of Lactobacillus rhamnosus Gr-1 supernatant and fetal sex on lipopolysaccharide-induced cytokine and prostaglandin-regulating enzymes in human placental trophoblast cells: implications for treatment of bacterial vaginosis and prevention of preterm labor. Am J Obstet Gynecol 200:532.e531-538. https://doi.org/10.1016/j.ajog.2008.12.032
Fernández L, Cárdenas N, Arroyo R, Manzano S, Jiménez E, Martín V, Rodríguez JM (2016) Prevention of infectious mastitis by oral administration of Lactobacillus salivarius Ps2 during late pregnancy. Clin Infect Dis 62:568–573. https://doi.org/10.1093/cid/civ974
Frola ID, Pellegrino MS, Espeche MC, Giraudo JA, Nader-Macias ME, Bogni CI (2012) Effects of intramammary inoculation of Lactobacillus perolens Crl1724 in lactating cows’ udders. J Dairy Res 79:84–92. https://doi.org/10.1017/s0022029911000835
Li K, Yang M, Tian M, Jia L, Du J, Wu Y, Li L, Yuan L, Ma Y (2022) Lactobacillus plantarum 17–5 attenuates escherichia coli-induced inflammatory responses via inhibiting the activation of the Nf-κb and MAPK signalling pathways in bovine mammary epithelial cells. BMC Vet Res 18:250. https://doi.org/10.1186/s12917-022-03355-9
Li D, Zhang N, Cao Y, Zhang W, Su G, Sun Y, Liu Z, Li F, Liang D, Liu B, Guo M, Fu Y, Zhang X, Yang Z (2013) Emodin ameliorates lipopolysaccharide-induced mastitis in mice by inhibiting activation of Nf-κb and Mapks signal pathways. Eur J Pharmacol 705:79–85. https://doi.org/10.1016/j.ejphar.2013.02.021
Mignacca SA, Dore S, Spuria L, Zanghì P, Amato B, Duprè I, Armas F, Biasibetti E, Camperio C, Lollai SA, Capucchio MT, Cannas EA, Presti VDML, Marianelli C (2017) Intramammary infusion of a live culture of Lactococcus lactis in ewes to treat staphylococcal mastitis. J Med Microbiol 66:1798–1810. https://doi.org/10.1099/jmm.0.000641
Liu M, Song S, Li H, Jiang X, Yin P, Wan C, Liu X, Liu F, Xu J (2014) The protective effect of caffeic acid against inflammation injury of primary bovine mammary epithelial cells induced by lipopolysaccharide. J Dairy Sci 97:2856–2865. https://doi.org/10.3168/jds.2013-7600
Zhu X, Zhao Y, Sun Y, Gu Q (2014) Purification and characterisation of plantaricin Zj008, a novel bacteriocin against Staphylococcus Spp. From Lactobacillus Plantarum Zj008. Food Chem 165:216–223. https://doi.org/10.1016/j.foodchem.2014.05.034
Kitching M, Mathur H, Flynn J, Byrne N, Dillon P, Sayers R, Rea MC, Hill C, Ross RP (2019) A live bio-therapeutic for mastitis, containing Lactococcus lactis Dpc3147 with comparable efficacy to antibiotic treatment. Front Microbiol 10:2220. https://doi.org/10.3389/fmicb.2019.02220
Pellegrino M, Berardo N, Giraudo J, Nader-Macías MEF, Bogni C (2017) Bovine mastitis prevention: humoral and cellular response of dairy cows inoculated with lactic acid bacteria at the dry-off period. Benef Microbes 8:589–596. https://doi.org/10.3920/bm2016.0194
Camperio C, Armas F, Biasibetti E, Frassanito P, Giovannelli C, Spuria L, D'Agostino C, Tait S, Capucchio MT, Marianelli C (2017) A mouse mastitis model to study the effects of the intramammary infusion of a food-grade Lactococcus lactis strain. PLoS One 12: e0184218. https://doi.org/10.1371/journal.pone.0184218
Crispie F, Alonso-Gómez M, O’Loughlin C, Klostermann K, Flynn J, Arkins S, Meaney W, Paul Ross R, Hill C (2008) Intramammary infusion of a live culture for treatment of bovine mastitis: effect of live Lactococci on the mammary immune response. J Dairy Res 75:374–384. https://doi.org/10.1017/s0022029908003385
Eckersall PD, Young FJ, Nolan AM, Knight CH, McComb C, Waterston MM, Hogarth CJ, Scott EM, Fitzpatrick JL (2006) Acute phase proteins in bovine milk in an experimental model of Staphylococcus aureus subclinical mastitis. J Dairy Sci 89:1488–1501. https://doi.org/10.3168/jds.S0022-0302(06)72216-0
Bradley A (2002) Bovine mastitis: an evolving disease. Vet J 164:116–128. https://doi.org/10.1053/tvjl.2002.0724
Zhao C, Wu K, Bao L, Chen L, Feng L, Liu Z, Wang Y, Fu Y, Zhang N, Hu X (2021) Kynurenic acid protects against mastitis in mice by ameliorating inflammatory responses and enhancing blood-milk barrier integrity. Mol Immunol 137:134–144. https://doi.org/10.1016/j.molimm.2021.06.022
Zhang C, Zhai S, Wu L, Bai Y, Jia J, Zhang Y, Zhang B, Yan B (2015) Induction of size-dependent breakdown of blood-milk barrier in lactating mice by Tio2 nanoparticles. PLoS One 10: e0122591. https://doi.org/10.1371/journal.pone.0122591
Stelwagen K, Singh K (2014) The role of tight junctions in mammary gland function. J Mammary Gland Biol Neoplasia 19:131–138. https://doi.org/10.1007/s10911-013-9309-1
Macias H, Hinck L (2012) Mammary gland development. Wiley Interdiscip Rev Dev Biol 1:533–557. https://doi.org/10.1002/wdev.35
Kobayashi K, Oyama S, Numata A, Rahman MM, Kumura H (2013) Lipopolysaccharide disrupts the milk-blood barrier by modulating claudins in mammary alveolar tight junctions. PLoS One 8: e62187. https://doi.org/10.1371/journal.pone.0062187
Oguro M, Koike M, Ueno T, Asaoka D, Mori H, Nagahara A, Uchiyama Y, Watanabe S (2011) Dissociation and dispersion of claudin-3 from the tight junction could be one of the most sensitive indicators of reflux esophagitis in a rat model of the disease. J Gastroenterol 46:629–638. https://doi.org/10.1007/s00535-011-0390-1
Zheng Y, Liu G, Wang W, Wang Y, Cao Z, Yang H, Li S (2021) Lactobacillus casei zhang counteracts blood-milk barrier disruption and moderates the inflammatory response in Escherichia coli-induced mastitis. Front Microbiol 12: 675492. https://doi.org/10.3389/fmicb.2021.675492
Aratani Y (2018) Myeloperoxidase: its role for host defense, inflammation, and neutrophil function. Arch Biochem Biophys 640:47–52. https://doi.org/10.1016/j.abb.2018.01.004
Li D, Fu Y, Zhang W, Su G, Liu B, Guo M, Li F, Liang D, Liu Z, Zhang X, Cao Y, Zhang N, Yang Z (2013) Salidroside attenuates inflammatory responses by suppressing nuclear factor-κb and mitogen activated protein kinases activation in lipopolysaccharide-induced mastitis in mice. Inflamm Res 62:9–15. https://doi.org/10.1007/s00011-012-0545-4
Shah KN, Valand P, Nauriyal DS, Joshi CG (2018) Immunomodulation of Il-1, Il-6 and Il-8 cytokines by Prosopis juliflora alkaloids during bovine sub-clinical mastitis. 3 Biotech 8: 409. https://doi.org/10.1007/s13205-018-1438-1
Cheng Y, Desse S, Martinez A, Worthen RJ, Jope RS, Beurel E (2018) Tnfα disrupts blood brain barrier integrity to maintain prolonged depressive-like behavior in mice. Brain Behav Immun 69:556–567. https://doi.org/10.1016/j.bbi.2018.02.003
Rochfort KD, Collins LE, Murphy RP, Cummins PM (2014) Downregulation of blood-brain barrier phenotype by proinflammatory cytokines involves Nadph oxidase-dependent ROS generation: consequences for interendothelial adherens and tight junctions. PLoS One 9: e101815. https://doi.org/10.1371/journal.pone.0101815
Hayden MS, Ghosh S (2012) Nf-κb, the first quarter-century: remarkable progress and outstanding questions. Genes Dev 26:203–234. https://doi.org/10.1101/gad.183434.111
Liu YC, Gao XX, Chen L, You XQ (2017) Rapamycin suppresses Aβ(25–35)- or LPS-induced neuronal inflammation via modulation of Nf-κb signaling. Neuroscience 355:188–199. https://doi.org/10.1016/j.neuroscience.2017.05.005
Vallabhapurapu S, Karin M (2009) Regulation and function of Nf-κappab transcription factors in the immune system. Annu Rev Immunol 27:693–733. https://doi.org/10.1146/annurev.immunol.021908.132641
Thalhamer T, McGrath MA, Harnett MM (2008) MAPKs and their relevance to arthritis and inflammation. Rheumatology (Oxford) 47:409–414. https://doi.org/10.1093/rheumatology/kem297
Chen J, Xu J, Li J, Du L, Chen T, Liu P, Peng S, Wang M, Song H (2015) Epigallocatechin-3-gallate attenuates lipopolysaccharide-induced mastitis in rats via suppressing mapk mediated inflammatory responses and oxidative stress. Int Immunopharmacol 26:147–152. https://doi.org/10.1016/j.intimp.2015.03.025
Kyriakis JM, Avruch J (2012) Mammalian Mapk signal transduction pathways activated by stress and inflammation: a 10-year update. Physiol Rev 92:689–737. https://doi.org/10.1152/physrev.00028.2011
Acknowledgements
We thank the Animal Clinical Laboratory of Hebei Agricultural University for providing technical support.
Funding
This research was supported by the Hebei Key Research and Development Program (19226611D).
Author information
Authors and Affiliations
Contributions
Ke Li designed the study. Ming Yang and Li Jia prepared materials. Ming Yang, Yinghao Wu, Lining Yuan, and Lianmin Li performed all experiments. Ke Li, Ming Yang, and Li Jia analyzed the data. Mengyue Tian, Jinliang Du, and Yuzhong Ma supervised and validated the project. Ke Li drafted the manuscript, and Yuzhong Ma revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All the animal experiments were approved by the guidelines of the Animal Care and Use Committee of Hebei Agricultural University (protocol number 2020044).
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, K., Yang, M., Jia, L. et al. The Prevention Effect of Lactobacillus plantarum 17–5 on Escherichia coli-Induced Mastitis in Mice. Probiotics & Antimicro. Prot. 15, 1644–1652 (2023). https://doi.org/10.1007/s12602-023-10047-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-023-10047-9