Abstract
Alzheimer’s disease is a common and devastating age-related disease with no effective disease-modifying treatments. Human genetics has implicated a wide range of cell surface receptors as playing a role in the disease, many of which are involved in the production or clearance of neurotoxins in the brain. Amyloid precursor protein, a membrane-bound signaling molecule, is at the very heart of the disease: hereditary mutations in its gene are associated with a greatly increased risk of getting the disease. A proteolytic breakdown product of amyloid precursor protein, the neurotoxic Aβ peptide, has been the target for many drug discovery efforts. Antibodies have been designed to target Aβ production with some success, although they have not proved efficacious in clinical trials with regards to cognitive benefits to date. Many of the recently identified genes associated with late-onset Alzheimer’s disease risk are integral to the innate immune system. Some of these genes code for microglial proteins, such as the strongest genetic risk factor for the disease, namely APOE, and the cell surface receptors CD33 and TREM2 which are involved in clearance of the Aβ peptide from the brain. In this review, we show how structural biology has provided key insights into the normal functioning of these cell surface receptors and provided a framework for developing novel treatments to combat Alzheimer’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most prevalent neurodegenerative disease with age being the biggest risk factor (Lindsay et al. 2002; Reeve et al. 2014). Over 50 million people worldwide are afflicted by dementia, of which AD is the major cause, and its prevalence is expected to almost double over the next 20 years as people live longer. The mechanisms by which AD progresses to cognitive decline are complex and not fully elucidated. A defining pathological feature of AD is the deposition of extracellular plaques in the brain composed primarily of a peptide called amyloid beta (Aβ); a proteolytic breakdown product of the amyloid precursor protein (APP; Fig. 1). Aβ exists as monomers, soluble oligomers, fibrils (Fig. 2), and plaques with evidence suggesting that Aβ pathology occurs decades before the onset of dementia (Villemagne et al. 2013). A second defining AD pathology is neurofibrillary tangles made of a hyperphosphorylated form of microtubule associating protein Tau. Aβ and Tau have been described as respectively the “trigger and bullet” of AD pathogenesis as Aβ is upstream of Tau in pathogenesis and triggers the conversion of Tau from a normal to a toxic state (Bloom 2014). This suggestion builds on earlier studies, for example, where primary mouse neurons, when exposed to the Aβ peptide, suffered neurite degeneration, and cell death for wild-type neurons but not for neurons from tau knock-out mice. When human tau was expressed in the tau knock-out neurons, the sensitivity to the peptide was restored (Rapoport et al. 2002). Recapitulation of AD pathogenesis has been reported, where Aβ-plaques and Tau-tangles were reproduced in a 3D human neural cell culture as a consequence of APP mutations that caused accumulating Aβ (Choi et al. 2014).
Diagrammatic representation of the known amyloid precursor protein (APP) structures, in the context of a cell membrane. Each structure shown is described here with its PDB ID. APP consists of an N-terminal growth factor-like domain (GFD) (red, 1MWP (Rossjohn et al. 1999)) and associated copper-binding domain (CuBD) (blue, 2FMA (Kong et al. 2007a)) which are commonly referred to as the “extracellular domain 1” or E1 (3KTM (Dahms et al. 2010)). This is followed by an anionic acid-rich region containing a Kunitz protease inhibitor domain (orange, 1AAP (Hynes et al. 1990)) that is absent, due to differential mRNA splicing, from the form of APP predominantly found in neurons. A helical bundle region, E2 (brown, 3UMH (Dahms et al. 2012)) is the last extracellular portion of APP, linked to the TM helical region that includes the Aβ peptide (rainbow, 1IYT (Crescenzi et al. 2002)). A short C-terminal intracellular domain is found to be partly helical (blue-white, 3DXC (Radzimanowski et al. 2008)) in complex with binding proteins such as Fe65 (tan, 3DXC (Radzimanowski et al. 2008)) and X11 (green, 1AQC (Zhang et al. 1997)) while other binding proteins are known but lack experimental structures (e.g., PAT1, dark green, AlphaFold2 model AF-Q92624-F1 (Jumper et al. 2021)). Processing of APP by β- and γ-secretases (gray, 5HD0, and colored by chain, 6IYC, respectively (Mandal et al. 2016; Zhou et al. 2019)) releases the Aβ peptide which is then able to polymerize into a range of different amyloid structures (shown are 5OQV, 6SHS, and 6W0O as examples (Ghosh et al. 2021; Gremer et al. 2017; Kollmer et al. 2019))
The Aβ peptide folds into a variety of conformations and comes together into multiple oligomeric states. Aβ monomers are found to have a partially helical structure (PDB ID: 1IYT (Crescenzi et al. 2002)), whereas protofibril (PDB ID: 2LMN (Paravastu et al. 2008)) and fibril (PDB IDs: 2LMP and 5OQV (Gremer et al. 2017; Paravastu et al. 2008)) structures of the peptide reveal a pleated β-sheet fold that can form between multiple peptide chains
Prevention of accumulation of Aβ in the pre-symptomatic stages of AD is a widely advocated strategy to treat the disease (Das et al. 2012; Moulder et al. 2013; Mullard 2012). However, the obvious protein targets to tackle Aβ accumulation are proving problematic. Antibodies that bind Aβ represent the most advanced approaches but have failed to prove efficacious in clinical trials although one of them, Biogen’s Aducanumab, was recently approved (https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-drug). Aβ is a proteolytic breakdown product of APP by the action of two proteases, β-secretase (BACE) and γ-secretase (Fig. 1). The Aβ peptide is not released as a single-sized species; rather, the proteolytic processing of APP produces peptides ranging in size from 39–43 residues and these are often referred to as Aβ isoforms. Of all the Aβ isoforms, Aβ40 (i.e., peptide comprised of Aβ residues 1–40) and Aβ42 (i.e., Aβ residues 1–42) appear to be the most important and they possess different physical and physiological characteristics such as conformation, aggregation propensity, metabolism, and cellular toxicity (Dunys et al. 2018; Qiu et al. 2015). The differences between Aβ40 and Aβ42 are described in more detail in the anti-Aβ antibodies section below. Therapies are being developed which aim to decrease Aβ production by inhibiting the action of BACE or γ-secretase on APP processing. Large phase III trials of Eli Lilly’s γ-secretase inhibitor, Semagacestat, were halted in 2011 because of an increased risk of skin cancer and infections (Doody et al. 2013). The problem with γ-secretase targeting is that it processes many other membrane proteins such as Notch (thought to be responsible for cancers seen in γ-secretase inhibitor treatment). Eli Lilly suspended development of a BACE inhibitor in phase II trials due to liver toxicity, possibly caused by inhibition of a liver enzyme (Lahiri et al. 2014). It is not surprising that targeting proteases, which cleave other proteins, is proving toxic and so strategies that target APP-specific processing are likely to be a better approach. It follows that APP itself might prove a more promising target to reduce Aβ production but a paucity of knowledge about APP biology has hampered this avenue of AD drug discovery.
The observation that plaques consist mostly of the Aβ peptide led to the amyloid cascade hypothesis in which deposition of the peptide in the brain is a crucial step in AD (Hardy and Higgins 1992). This hypothesis has been strongly supported by occurrence of plaques and tangles in individuals with a hereditary and aggressive form of AD, so-called early-onset familial AD which represents ~4% of AD patients (Alzheimer’s Association 2012), who possess mutations in the genes encoding APP and components of the γ-secretase complex. In addition, many patients with Down syndrome exhibit AD symptoms early in life and they have a triplication of the APP gene. Additional support has come in the form of the generation of numerous transgenic mouse models with the genetic mutations of APP and γ-secretase which display AD pathology (Myers and McGonigle 2019). Over the years, the hypothesis has been refined with the findings that soluble Aβ peptides, particularly low molecular weight oligomers, are neurotoxic and their levels correlate better with AD symptoms and severity than do the Aβ fibrils in plaques. The plaques are now thought to be protective by taking soluble toxic peptides out of circulation (Makin 2018; Fyfe 2021). However, many have questioned the validity of the amyloid hypothesis with the failure to date of Aβ directed treatments, such as those discussed above, to convincingly show cognitive benefit in clinical trials. Alternative approaches gaining increased attention are a focus on downstream effector molecules like Tau and inflammatory molecules, as well as clearance mechanisms for neurotoxins. Genome-wide association studies (GWAS) have identified AD risk genes associated with microglia, the immune cells of the brain, and neuroinflammation with the most common factor being apolipoprotein E4 (APOE4) gene with others such as the genes for microglia receptors, triggering receptor expressed on myeloid cells 2 (TREM2) and myeloid cell surface antigen cluster of differentiation 33 (CD33), that are involved in Aβ clearance from the brain (Leng and Edison 2021). In this review, we describe how structural biology has contributed to our understanding of some of the main players implicated in AD: the cell surface receptors APP and its breakdown product, the Aβ peptide, and microglia receptors that clear toxins from the brain.
Amyloid precursor protein
The normal physiological roles of APP are not well understood. It is known that the binding of APP to heparan sulfate proteoglycans (HSPGs) stimulates neurite outgrowth in cultured neurons (Small et al. 1994) and a secreted form of APP has potent neuroprotective actions against glutamate neurotoxicity, Aβ peptide-induced oxidative injury, and glucose deprivation (Chasseigneaux and Allinquant 2012). When APP processing is shifted towards the amyloidogenic pathway, not only is there a gain of toxicity with overproduction of Aβ, but also a loss of APP function in neuroprotection. The lack of understanding of APP biology prevents us from appreciating loss of function implications in AD pathology.
APP is a type-I transmembrane protein with a large extracellular portion (612 amino acids in the neuronal isoform) that has been structurally and functionally subdivided into several domains (Fig. 1). The highly conserved N-terminal growth factor-like domain (GFD) has been shown to bind heparin and the extracellular matrix protein fibulin (Ohsawa et al. 2001). The crystal structure of the GFD domain was determined in 1999 (Fig. 1) and revealed a highly charged basic region that may interact with glycosaminoglycans (Rossjohn et al. 1999). Structural similarities with cysteine-rich growth factors, taken together with its known growth-promoting properties, suggested this domain might function as a growth factor. Adjacent to the GFD is a copper-binding domain (CuBD) implicated in copper transport and regulation of APP processing by BACE (Spoerri et al. 2012). The structure of the CuBD was initially determined by nuclear magnetic resonance spectroscopy (NMR) (Barnham et al. 2003) and then copper-bound structures by X-ray crystallography (Fig. 1) (Kong et al. 2007a, b). These structures revealed how this domain recognizes copper and reduces it, suggesting that APP could function as a metallochaperone in transporting copper ions. These two domains constitute the so-called E1 domain. The crystal structure of the entire E1 domain has subsequently been determined revealing that the GFD and CuBD domains pack tightly together (Dahms et al. 2010). In non-neuronal isoforms of APP, there is a Kunitz type protease inhibitor domain for which a structure was determined in 1990 (Fig. 1) (Hynes et al. 1990). A long low complexity acidic-rich region connects the E1 domain to the core E2 domain. The E2 domain contains a second heparin-binding region and has been implicated in binding to HSPGs (Reinhard et al. 2013). Numerous structures of monomeric and dimeric forms of the E2 domain have been determined revealing an elongated helical stalk that is stabilized in the presence of metal ligands (Fig. 1) (Dahms et al. 2012; Wang and Ha 2004). APP is known to participate in homo- and hetero-oligomerization which is highly dependent on the local environment and is implicated in APP’s function and processing, in addition to dependence on co-localization with the secretases (Pasternak et al. 2003; Scheuermann et al. 2001).
The cleavage of APP proceeds via two alternative pathways: a so-called normal physiological pathway where it gets cleaved by α-secretase, an ADAM family member, or a pathological pathway where it gets cleaved by β-secretase or BACE (Fig. 1). The BACE structure was solved in 2000 (Fig. 1) (Hong et al. 2000) and subsequently has been followed by hundreds of BACE inhibitor complex structures as part of drug discovery campaigns. The extracellular domain of the α-secretase was more recently determined (Seegar et al. 2017). In each case, the large extracellular domain of APP is released from the membrane surface and the remaining C-terminal fragments are cleaved by γ-secretase, which in the case of the pathological pathway, releases the Aβ peptide. γ-Secretase is a membrane-embedded aspartyl protease comprised of four subunits: nicastrin, APH-1, presenilin, and PEN-2. The mechanism of APP recognition and cleavage by γ-secretase has been elegantly explained by two high-resolution atomic structures determined by cryo-electron microscopy (Fig. 1) (Yang et al. 2019; Zhou et al. 2019).
There is appreciable evidence that APP acts as a cell surface receptor (Deyts et al. 2016). It shares a similar architecture (Kang et al. 1987), cellular orientation, and localization (Schubert et al. 1991; Weidemann et al. 1989) to known (type-I) cell surface receptors. The APP cytoplasmic domain binds to Fe65, a protein related to oncogenic signal transducers (Fiore et al. 1995). Other binding partners have been discovered, including APP-BP1 (Chow et al. 1996), X11 (Borg et al. 1996) and UV-DDB (Watanabe et al. 1999). APP mutations associated with familial AD cause constitutive activation of Go, a member of the heteromeric G protein family that serves as signal transducers of cell surface receptors (Nishimoto et al. 1993; Okamoto et al. 1996). The APP-E1-directed antibody 22C11 is also known to trigger Go-mediated signal transduction (Brouillet et al. 1999), and recent reports have implicated a YENPTY motif in the APP cytoplasmic region in modulating several APP activities through phosphorylation and dephosphorylation of the first tyrosine residue (Nhan et al. 2015; Li et al. 2016; Bukhari et al. 2017). APP C-terminal fragments have been shown to interact with Gα subunits leading to signaling and the promotion of neurite outgrowth via adenylyl cyclase/PKA-dependent pathways (Copenhaver and Kögel 2017). The physiological relevance of these various signaling pathways is unclear but they do demonstrate that the APP molecule is capable of signaling across membranes. A predominant mechanism of signal transduction for many cell surface receptors involves dimerization (Brooks et al. 2014) and APP forms dimers (Isbert et al. 2012).
APP dimerization is known to modulate Aβ production (Eggert et al. 2009; Lefort et al. 2012; Scheuermann et al. 2001). These studies used antibodies or disulfides to artificially crosslink APP and to stabilize multimers. In addition, copper binding to the CuBD reduces Aβ production (Barnham et al. 2003) yet comparisons between our structures of ligand-free (apo) and copper-bound forms of the CuBD reveal no significant conformational changes that would explain this effect (Kong et al. 2008). This discrepancy likely arises due to the complexity of APP oligomerization, stemming from the fact that there are at least four dimerization motifs in APP, including E1 homo-dimerization induced by short-chain heparin, E2 homo-dimerization induced by long-chain heparin, in the juxtamembrane (JM) region (region of APP corresponding to Aβ residues 1–28) and the GxxxG dimerization motifs in the transmembrane (TM) region (Khalifa et al. 2010), as well as potential domain-domain hetero-dimerization modes, heparin dependent or not.
Anti-Aβ antibodies
The amyloid hypothesis proposes the deposition of extracellular Aβ peptides in the brain as the central event in the pathogenesis of AD (Hardy and Allsop 1991). Aβ is neurotoxic and has been found to kill cultured neurons (Yankner et al. 1990). A multitude of studies have now explored the deleterious effects this peptide has on neurons in vitro and in vivo, including oxidative stress, mitochondrial dysfunction, neurite degeneration, impaired synaptic plasticity, cation imbalances, and neuronal apoptosis (Anandatheerthavarada et al. 2003; Ezeani and Omabe 2016; Krishtal et al. 2017; Parihar and Brewer 2010; Song et al. 2006; Varadarajan et al. 2000). More recently, it has been shown that, in addition to direct effects, sustained deposition of Aβ can cause neuronal loss through chronic activation of the innate immune system. Microglia are an emerging central player in this process. Activated by Aβ, these cells mediate an inflammatory response by releasing pro-inflammatory cytokines, eicosanoids, chemokines, and complement factors; this can lead to neuronal dysfunction and death, direct phagocytosis of neurons, induction of Tau pathology, and reduced phagocytic clearance of Aβ (Ennerfelt and Lukens 2020; Heneka et al. 2015). Aβ is therefore a promising target for AD therapeutics, with the majority of potential disease-modifying treatments targeting this peptide (van Dyck 2018). Early studies demonstrated that vaccination against Aβ can reduce amyloid deposition and prevent memory loss in animal models of the disease (Morgan et al. 2000; Schenk et al. 1999). Now, passive immunotherapy through the administration of monoclonal antibodies (mAbs) directed against Aβ are among the most extensively developed, with aducanumab being the first U.S. Food and Drug Administration (FDA)–approved therapy to reportedly address the underlying biology of AD (https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-drug).
There have been several proposed mechanisms by which these antibodies work to reduce the amyloid burden and slow the progression of AD. By crossing the blood-brain barrier and directly opsonizing Aβ in the brain, these antibodies can initiate the phagocytosis of Aβ complexes and the activation of microglia through binding Fc receptors on these cells (Bard et al. 2000; Brazil et al. 2000; Wilcock et al. 2004a, b). By directly binding to Aβ these antibodies can prevent the aggregation of this peptide into fibrils (Figs. 1 and 2), and by binding pre-existing fibrils can cause their disaggregation and protect from their neurotoxic effects (Solomon et al. 1997, 1996). Finally, by binding and draining plasma Aβ, these antibodies can leech Aβ from the brain (Liu et al. 2015; Zhang and Lee 2011). This final mechanism relies on the peripheral sink hypothesis, whereby Aβ is able to be transported across the blood-brain barrier resulting in an equilibrium between Aβ in the brain and periphery.
Over the last decade, the X-ray crystal structures of several promising mAbs for AD treatment have been solved in complex with their Aβ target (Table 1) (Arndt et al. 2018; Crespi et al. 2015; Feinberg et al. 2014; La Porte et al. 2012; Miles et al. 2013; Ultsch et al. 2016). These studies revealed that, despite some sharing the same sequence epitope of Aβ, the conformational epitope recognized by these antibodies can differ markedly (Figs. 3 and 4). Taken with the knowledge that these mAbs have been tested in clinical studies with confusing results and often failure (van Dyck 2018), a deeper understanding of how the shape and conformation of the epitope can affect target engagement and clinical efficacy could lead to further improvements to this promising treatment strategy.
The Aβ epitopes recognized by the clinical anti-Aβ antibodies listed in Table 1 are depicted as molecular surfaces overlaid onto the helical Aβ42 monomer (PDB ID: 1IYT (Crescenzi et al. 2002)). Residue numbers of the epitope are shown in parentheses. The conformation adopted by each of the Aβ epitopes in the Aβ:antibody complexes are shown alongside in stick fashion, with those for crenezumab and solanezumab superimposed to illustrate their structural similarity. The location of residues F19 and V24 are indicated in the overlay of crenezumab and solanezumab; the linear Aβ conformation is disrupted at F19 and the remainder of the epitope adopts a more helical conformation in both antibodies, while V24 is the last Aβ residue observed in the crenezumab structure and the side-chain adopts a different orientation to that observed in solanezumab (see main text for details)
Structures of the clinical anti-Aβ antibodies listed in Table 1; the view is looking down onto the Aβ-binding cleft: (left-right, top-down) aducanumab (PDB ID: 6CO3 (Arndt et al. 2018)), bapineuzumab (PDB ID: 4HIX (Miles et al. 2013)), gantenerumab (PDB ID: 5CSZ (Bohrmann et al. 2012)), crenezumab (PDB ID: 5VZY (Ultsch et al. 2016)), solanezumab (PDB ID: 4XXD (Crespi et al. 2015)), and ponezumab (PDB ID: 3U0T (La Porte et al. 2012)), with the complexed Aβ ligand colored yellow in stick form. The antibodies are depicted as transparent molecular surfaces; the heavy and light chains are identified by dark and light shades, respectively. The N- and C-terminal Aβ residues observed in each crystal complex are labeled
Antibodies that target the N-terminus of Aβ and have had their complex structure solved include aducanumab, bapineuzumab, and gantenerumab (Figs. 3 and 4 and Table 1). Aducanumab was designed by screening libraries of human memory B cells for reactivity against aggregated Aβ; this eventually led to a human mAb that selectively reacts with Aβ aggregates (Sevigny et al. 2016). Bapineuzumab was developed by humanizing the mouse mAb 3D6, which was selected due to its specificity for the free amino terminus of Aβ (Feinberg et al. 2014). The developers of bapineuzumab noted that the greatest efficacy across several endpoints in preclinical studies came from antibodies that targeted N-terminal epitopes of Aβ (Bard et al. 2003; Schroeter et al. 2008; Zago et al. 2012). The developers of gantenerumab hypothesized that the most efficient amyloid clearance would come from antibodies that display high affinity for Aβ plaques and recruit brain effector cells (Bohrmann et al. 2012). In addition to recognizing an N-terminal Aβ epitope, gantenerumab has shown selectivity for residues 18–27 from the amyloid mid-region (Bohrmann et al. 2012). Both gantenerumab and aducanumab bind the N-terminus of Aβ in an extended conformation, as revealed by their crystal structures (Figs. 3 and 4), interacting with Aβ residues 1–11 and 2–7 respectively (Arndt et al. 2018; Bohrmann et al. 2012). Despite this, the linear epitope of Aβ recognized by each of these antibodies is unique and does not align with a root-mean-square deviation (RMSD) of 3.2 Å for all matched atoms. In comparison, bapineuzumab binds the N-terminus of Aβ as a 310 α-helix, with the N-terminal D1 residue buried deepest in the antibody binding pocket and the C-terminal H6 exposed at the entrance (Feinberg et al. 2014; Miles et al. 2013). The antibody likely binds to a population of Aβ peptides that has already adopted the conformation observed in the crystal structures and is unable to co-opt the peptide into this conformation, explaining the antibody’s selectivity for the free N-terminus of Aβ (Miles et al. 2013). Both aducanumab and gantenerumab have been reported to have strong selectivity for Aβ fibrils, while bapineuzumab is less selective for this species (Arndt et al. 2018; Bohrmann et al. 2012). In comparative binding studies, aducanumab and gantenerumab displayed strong selectivity for Aβ fibrils and efficiently bound immobilized oligomeric Aβ even in a surplus of free monomer, while bapineuzumab was less selective and binding to oligomeric Aβ was inhibited by soluble Aβ monomer (Arndt et al. 2018). In the same study, aducanumab was shown to have extremely weak monovalent Aβ-binding with a fast dissociation rate, while both gantenerumab and Bapineuzumab displayed higher affinities and much slower dissociation rates. An interesting finding was that aducanumab has a markedly higher affinity for a tetrameric branched Aβ multi-antigen peptide over dimeric multi-antigen peptide, while gantenerumab and bapineuzumab bound well to both, highlighting the impact of valency on the affinity of Aducanumab for Aβ (Arndt et al. 2018).
Two antibodies that target the mid-region of Aβ have had their complex structure solved, solanezumab and crenezumab (Figs. 3 and 4 and Table 1) (Crespi et al. 2015; Ultsch et al. 2016). Solanezumab is a humanized form of the murine antibody m266, which was shown in transgenic mouse models of AD to reduce brain Aβ burden without binding Aβ deposits, opening the possibility of targeting the soluble pool of Aβ (DeMattos et al. 2001). Crenezumab was developed by humanizing an anti-Aβ mAb of an IgG4 isotype, to minimize Fc gamma receptor activation of microglia and provide a safer therapeutic alternative for passive immunotherapy for AD (Adolfsson et al. 2012). Both crenezumab and solanezumab capture the mid-region of Aβ in an intermediate between observed β-sheet and helical forms, with almost perfectly conserved Aβ-binding residues (Crespi et al. 2015). The captured Aβ molecules of these antibodies align closely, with an RMSD of 0.44 Å for all matched atoms (Fig. 3). Both antibodies sequester the hydrophobic core of Aβ, with the KLVF region of the peptide adopting a conformation compatible with crystallographic β-sheet models of Aβ oligomerization. This conformation is disrupted by a rotation at residue F19 (Fig. 3), initiating a helical or coil conformation that is also observed in NMR-derived solution structures of monomeric Aβ, and eliminating features characteristic of Aβ oligomers and fibrils (Crespi et al. 2015; Ultsch et al. 2016). This central epitope is hypothesized to be involved early in the oligomerization of Aβ and would become unavailable to these antibodies in oligomeric Aβ (Crespi et al. 2015). In support of this, solanezumab was shown to recognize soluble monomeric Aβ, inhibit fibril formation by synthetic Aβ, and displayed a slight preference for binding to soluble Aβ40 over fibrils (Arndt et al. 2018; Legleiter et al. 2004). In contrast, and despite recognizing an overlapping epitope, crenezumab has been reported to bind multiple forms of Aβ with high affinity and a preference for oligomers over monomers, protect against Aβ oligomer-induced cytotoxicity, and increase the uptake of Aβ oligomers by microglia (Adolfsson et al. 2012). V24 is the final Aβ residue observed in the crenezumab structure and is the only Aβ residue to have an alternate conformation to that observed in the solanezumab structure, with the V24 Cβ atom of crenezumab swapping orientations with the V24 side chain in comparison to that observed in the solanezumab structure (Fig. 3). When observed in the solanezumab structure, the side chain of V24 makes hydrophobic interactions with the side chain of D28 from the antibody light chain, whereas this interaction is not observed in the crenezumab structure. It has been proposed that this alternate conformation is evidence to support crenezumab binding a random coil structure between residues 21 and 24 in comparison to the α-helical structure captured by Solanezumab (Ultsch et al. 2016). It has been further proposed that the α-helical epitope is present in monomeric Aβ but absent from aggregated species, potentially explaining the reported binding preferences of these antibodies for different Aβ species (Ultsch et al. 2016).
Ponezumab is the only antibody targeting the Aβ C-terminal region that has had its structure solved to date (Figs. 3 and 4 and Table 1) (La Porte et al. 2012). Ponezumab is a humanized IgG2 antibody that binds specifically to the C-terminus of Aβ40, with the recognized epitope being available for binding on the soluble Aβ present in the circulation (La Porte et al. 2012). The IgG2 region was selected over IgG1 as these mAbs have an intrinsically lower propensity to induce immune effector function (Armour et al. 2003; Landen et al. 2013). Ponezumab captures the C-terminus of Aβ in an extended conformation and makes extensive contacts with the Aβ40 carboxyl moiety, precluding it from being able to recognize unprocessed APP and Aβ42 peptide (La Porte et al. 2012). This is supported by binding assays in which ponezumab bound to monomeric, oligomeric, and fibrillar forms of Aβ40 equally well, while not binding to any form of Aβ42 (La Porte et al. 2012). Despite recognizing several forms of Aβ40, further studies have revealed strong selectivity of Ponezumab for monomeric species of Aβ (Landen et al. 2013).
A number of Aβ structural studies have elucidated the plethora of conformations and multimeric states this peptide is capable of adopting and allows the development of a structure-activity relationship with anti-Aβ antibodies. Aβ monomers aggregate into higher-order assemblies, including low-molecular-weight oligomers such as dimers, trimers, tetramers, and pentamers, to midrange molecular weight oligomers, including hexamers, nonamers, and dodecamers, to protofibrils, and fibrils (Fig. 2) (Chen et al. 2017). An early study of the structure of monomeric Aβ in water revealed it had no secondary structure, and instead collapsed into a compact series of loops, strands, and turns (Zhang et al. 2000). Studies of Aβ40 and Aβ42 in fluorinated alcohols and in SDS micelles have revealed the presence of two helical regions, connected through a flexible kink (Coles et al. 1998; Crescenzi et al. 2002). A recent NMR study showed that Aβ40 can adopt a compact, partially folded structure with the central hydrophobic region of the peptide forming a 310 α-helix and the N- and C-termini collapsing against it due to the clustering of hydrophobic residues (Vivekanandan et al. 2011). It should be noted that the conformation of soluble Aβ is likely influenced by the solvent system in which it is studied. While monomeric Aβ can exist in an ensemble of rapidly converting conformations, helical forms of Aβ have been predicted to be crucial on-pathway intermediates in amyloid fibrillogenesis (Fezoui and Teplow 2002; Kirkitadze et al. 2001).
Aβ fibrils share structural similarities and all contain β-sheets (Figs. 1 and 2), formed by parallel β-strand segments that run approximately perpendicular to the fibril growth axis in a “cross-β” motif (Tycko 2006). Early solid-state NMR studies using short peptide segments of Aβ have shown that amyloid fibril “cross-β” structures can exist in either a parallel or antiparallel pattern (Benzinger et al. 1998; Petkova et al. 2004). More recently, cryo-electron microscopy was used to determine the structure of an Aβ42 fibril composed of two intertwined proto-filaments composed of Aβ42 molecules stacked in a parallel, in-register cross-β structure (Gremer et al. 2017). Aβ fibrils are structurally polymorphic; both trimeric and dimeric models with an in-register parallel cross-β-sheet structure have been developed based on NMR and crystallographic data (Paravastu et al. 2008). The common cross-β motif of Aβ fibrils results in the hydrophobic mid-region and C-terminus being sequestered into the core of the structure, leaving the more hydrophilic N-terminal region solvent exposed (Fig. 2) (Gremer et al. 2017; Paravastu et al. 2008). One caveat of these studies is that to ensure a homogenous solution, optimizing conditions that can stabilize Aβ peptides are frequently used that may not be physiologically relevant (Chen et al. 2017).
The oligomeric states of Aβ are more transient than fibrils and preparing homogenous solutions of these species is difficult; as a result, little is known about the structure of these species (Chen et al. 2017). Aβ oligomers studied by circular dichroism and infrared spectroscopy feature extended coil or β-sheet structures (Tew et al. 2008; Lomont et al. 2018). In the presence of detergents, soluble oligomers have been found to have substantial β-sheet content with a mixed parallel and antiparallel character (Yu et al. 2009). Solid-state NMR studies have shown Aβ40 oligomerizes with the C-terminal sequestered and the N-terminus exposed for antibody binding, as is observed in fibril structures (Lu et al. 2013). It is still unknown whether Aβ monomers are able to directly form fibrils without an intermediate oligomeric structure, or if the oligomeric structures are basic units that can assemble into fibrils (Chen et al. 2017).
Despite only differing by two amino acids at the C-terminal region, it is known that Aβ42 forms fibrils significantly faster than Aβ40 (Jarrett et al. 1993). Most residues of the C-terminal region of Aβ are hydrophobic, and it is becoming clear this region is important in determining the aggregation mechanisms of the Aβ peptide. By comparing C-terminal fragments derived from Aβ40 and Aβ42, the C-terminal dipeptide I41-A42 was shown to strongly promote aggregation (Li et al. 2010). Dimer formation is the first step in peptide aggregation, and recent studies have shown the importance of this C-terminal region in determining this process. In particular, the Aβ42 dimer has a higher propensity than the Aβ40 dimer to form β-strands at the central and C-terminal regions, which are two segments crucial to the oligomerization of Aβ (Côté et al. 2012; Kim and Lyubchenko 2014). Tetramers formed of the Aβ40 peptide have been shown to resist further addition of molecules; as a result, Aβ40 fibril growth is much slower than that of Aβ42 (Bernstein et al. 2009). Aggregate free Aβ40 preparations have been shown to form monomers, dimers, trimers, and tetramers, while Aβ42 preparations preferentially form pentamer or hexamer units that assemble further (Bitan et al. 2003). Addition of I41 to Aβ40 may induce formation of the pentamer and hexamer units, but addition of A42 was required for further assembly. Molecular recycling of Aβ40 fibrils is also faster than Aβ42 fibrils, with a higher rate constant of dissociation of molecules from the fibril (Sánchez et al. 2011). These studies highlight the differences in the structure and aggregation mechanisms of different Aβ isoforms and support the increased potential of Aβ42 to form stable aggregates.
The Aβ oligomer hypothesis posits that soluble Aβ oligomers, rather than insoluble fibrils or plaques, trigger synaptic dysfunction and memory impairment (Hardy and Selkoe 2002; Klein et al. 2001; Walsh et al. 2002). Recent evidence supports this species as being the most neurotoxic (Selkoe and Hardy 2016; Tolar et al. 2021; Walsh and Selkoe 2007). Based on NMR and X-ray crystallographic studies, mAbs targeting the N-terminus would likely be most efficient in clearing Aβ oligomers (Montoliu-Gaya and Villegas 2016; van Dyck 2018). While both aducanumab and gantenerumab display high selectivity for aggregated Aβ over soluble monomeric peptide, bapineuzumab is markedly less specific (Arndt et al. 2018). Aducanumab and gantenerumab both bind an extended conformation of Aβ that is accessible in oligomeric and fibrillary forms and can likely co-opt this peptide into the binding pocket, while bapineuzumab requires the free N-terminus of Aβ in a specific conformation to bind. Despite selectivity for these aggregated species being a desired feature of anti-Aβ antibodies, the nomenclature to describe their relative selectivity for varying Aβ species has been inconsistent, and few direct comparisons have been reported (van Dyck 2018). Both crenezumab and solanezumab bind the mid-region of Aβ in an almost identical conformation (Fig. 3). This region of Aβ is predicted to be occluded during aggregation, and while solanezumab predictably favors soluble monomeric peptide, crenezumab is reportedly able to bind oligomeric species. A direct and quantitative comparison of the relative affinities for these species is therefore important to further understand the structure activity relationship of antibodies that target this region of the peptide (Table 1) (Arndt et al. 2018). Autocatalytic aggregate multiplication by secondary nucleation of monomers at the surface of fibrils is a critical source of Aβ oligomers, becoming the dominant source of this toxic species above a critical concentration of fibrils (Cohen et al. 2013). Comparative studies into the influence of therapeutic antibodies on the aggregation kinetics and production of multimeric Aβ offer new insights into their mechanism of action and supports affinity and stoichiometry analyses. In these studies, aducanumab was unique in its ability to selectively reduce the secondary nucleation rate of Aβ42 resulting in reduced free oligomer production, while in contrast, solanezumab selectively inhibits primary nucleation of monomers into aggregates (Linse et al. 2020). Both bapineuzumab and gantenerumab were found to act predominantly by reducing the growth of the fibrillar aggregates, resulting in a smaller reduction in free oligomer production (Linse et al. 2020). This is in agreement with the higher selectivity of aducanumab for aggregated forms of Aβ in comparison to bapineuzumab and gantenerumab, and the high specificity of solanezumab for monomeric peptide. The developing structure-activity relationship between Aβ and antibodies that target this polymorphic peptide can aid in the design of improved antibodies with conformational epitopes selective for the most neurotoxic soluble aggregated species (van Dyck 2018).
Microglial receptors implicated in Alzheimer’s disease
Genome-wide association studies (GWAS) of AD risk point glaringly at innate immunity (Kunkle et al. 2019). Microglial cells are innate immune cells of the central nervous system (CNS), comprising 5–10% of the glial cells in the brain (Kabba et al. 2018). Microglia are highly dynamic cells that, as the resident macrophage cells, act as the first and main form of active immune defense in the CNS (Filiano et al. 2015). Upon detection of pathogens or damage, microglia adopt an activated state resulting in an inflammatory response. The activated microglia respond to alterations in brain tissue homeostasis by changing their gene expression profile, leading to the release of a host of neuroactive signaling molecules, such as neuroinflammatory cytokines (Renno et al. 1995), that can contribute to the pathophysiology of a wide range of neurodegenerative diseases. A growing body of literature implicates microglial activation as a key point in the pathogenesis of a variety of neurodegenerative disorders and a potential avenue for the development of novel therapeutic agents (Lull and Block 2010; Subramaniam and Federoff 2017; von Bernhardi et al. 2015).
A number of key microglial proteins have been identified from GWAS studies including, but not limited to APOE (Kunkle et al. 2019), CD33 (Hollingworth et al. 2011), 1-phosphatidylinositol 4,5-bisphosphate phosphodiesterase gamma-2 (PLCG2) (Sims et al. 2017), and TREM2 (Guerreiro et al. 2013). APOE is the strongest genetic risk factor for the development of late-onset Alzheimer’s disease (LOAD) and has been shown to influence the average age of disease onset (Corder et al. 1993). PLCG2 is a membrane-associated enzyme that plays a crucial role in cell-surface receptor signal transduction (Hernandez et al. 1994). Specifically, PLCG2 is necessary for immune cell function and is highly expressed in microglia.
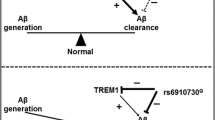
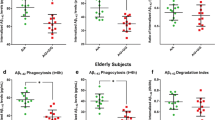
CD33, a cell surface receptor in microglial cells, has recently shown significant association with LOAD (Hollingworth et al. 2012; Naj et al. 2011). Binding of CD33 to sialic acid–modified ligands induces an inhibitory signal in microglia to reduce Aβ uptake by phagocytosis. Additionally, TREM2 and APOE have been identified as key microglial proteins. The TREM2-APOE pathway has recently been shown (Krasemann et al. 2017) to regulate the microglial switch from homeostatic to the damage-associated microglial phenotype. These pro-inflammatory damage-associated microglia are induced by neuronal damage and have a common gene expression signature established in a two-step process (Keren-Shaul et al. 2017). In one step, APOE levels rise dramatically, accompanied by suppression of genes associated with resting microglia. In a second step, a TREM2-dependent step induced by damaged or apoptotic neurons sees upregulation of protein markers characteristic of the damage-associated microglia phenotype distinct from typical proinflammatory M1 microglia. The genetic associations of CD33 and TREM2 converge whereby CD33 modulates the expression of TREM2 and TREM2 functions downstream of CD33 (Chatila and Bradshaw 2021; Griciuc et al. 2019).
CD33
As the name suggests, myeloid cell surface antigen cluster of differentiation 33 (CD33) is a cell surface receptor located on myeloid cells in the periphery and CNS. Since the late 1980s, CD33 has been a therapeutic target in acute myeloid leukemia due to it being highly expressed on acute myeloid leukemia progenitor cells but not normal stem cells (Maakaron et al. 2021; Walter et al. 2005). CD33-targeted immunotherapy agents have included unconjugated antibodies, antibody-drug conjugates, radioimmunoconjugates, and immunotoxins. Upon antibody binding, CD33 is internalized in the cell enabling toxins to be delivered (Walter et al. 2008a, b). One acute myeloid leukemia therapy approved by the FDA in 2000 capitalizes on this CD33 internalization mechanism to deliver a toxic payload (ozogamicin) conjugated to a CD33-directed antibody (gemtuzumab) (Appelbaum et al. 1992; Sabbath et al. 1985; Walter et al. 2005). In the CNS, CD33 is expressed by microglia; increased activation of CD33 suppresses microglial phagocytosis leading to accumulation of Aβ and other cellular toxins in the brain. In turn, the accumulation of Aβ results in neuroinflammation, now thought to be a major cause of neurodegenerative diseases such as LOAD (Chatila and Bradshaw 2021; Griciuc and Tanzi 2021; Miles et al. 2019). Although the details of the CD33 signaling cascade are not fully understood, inhibition of CD33 expression or function could increase the capacity of microglia to clear toxic species from the brain, including various forms of Aβ, providing an alternative effective therapy against the progression of AD and other neurodegenerative or neuroinflammatory diseases.
CD33 belongs to the sialic acid–binding immunoglobulin (Ig)-like lectin (siglec) receptor family, of which there are 15 human members (Duan and Paulson 2020; Miles et al. 2019). Also known as siglec-3, the canonical mature isoform of CD33 (i.e., signal peptide, residues 1–17, has been cleaved) is a 38-kDa type-I transmembrane receptor containing 347 residues. The extracellular region is comprised of an N-terminal IgV domain (residues 18–139, also known as the V-set domain) followed by an IgC domain (residues 145–232, also known as a C2-set domain). A flexible, disordered JM region (residues 233–264) connects the IgC domain to a TM α-helix (predicted by AlphaFold2 to be residues 265–295, model ID: AF-P20138-F1 (Jumper et al. 2021)); this is followed by an unstructured intracellular domain (residues 296–364) (Fig. 5).
Diagrammatic representation of microglial proteins CD33, TREM2, DAP12, and APOE4 structures in the context of a cell membrane. CD33 is thought to signal as a homodimer, or possibly a higher-order oligomer. The extracellular region of CD33 is comprised of an N-terminal IgV domain and a membrane-proximal IgC domain (PDB ID: 5IHB), followed by a flexible JM region connected to a helical TM and an intracellular region containing the signaling ITIM motifs. The insert box shows the polar interactions (black dashed lines) of the sialic acid mimetic P22 with CD33 IgV domain residues (PDB ID: 6D4A (Miles et al. 2019)). In addition to traditional antibodies targeting the extracellular region of CD33, scFv antibodies such as scFv P02_D09 (PDB ID: 6UUP (Park et al. 2021)) have been identified. TREM2 requires the DAP12 receptor to form a signaling complex. The extracellular region of TREM2 is comprised of an IgV domain (PDB ID: 5ELI, wild-type TREM2 (Kober et al. 2016)), followed by a flexible JM region connected to a helical TM domain and a very short non-signaling intracellular region. The TREM2 TM helix interacts with the two TM helices of DAP12 via salt bridge interactions (indicated by the + and −). DAP12 forms a homodimer with a very short N-terminal extracellular region, a disulfide bond connects the two N-terminal regions of the DAP12 monomers. The intracellular tails of each DAP12 monomer contain two signaling ITAM motifs. The extracellular IgV domain of TREM2 is the target for agonistic antibodies, such as scFv-2 (PDB ID: 6YYE (Szykowska et al. 2021)) whose epitope is indicated by the black bracket. Mutation of TREM2 R47 to histidine increases the risk of developing LOAD, the location of this residue is indicated and the structure of the R47H TREM2 mutant is depicted to the right of the wild-type protein (PDB ID: 5UD8 (Sudom et al. 2018)). The soluble (i.e., unlipidated) form and membrane-associated lipidated form of APOE4 are also shown, APOE4 interacts with the extracellular region of TREM2 as well as Aβ oligomers (Figs. 1 and 2). The location of the APOE4 interaction surface is indicated by the black curved line encompassing R47 in wild-type TREM2. The APOE4 structures (residues 19–317) depicted are models constructed using X-ray crystallography structures of APOE4 and APOA-I, for the soluble and lipidated forms respectively (PDB IDs: 6NCO (Petros et al. 2019) and 3R2P (Mei and Atkinson 2011)
The IgV and IgC domains adopt the typical immunoglobulin fold, each domain comprising a sandwich of two β-sheets formed by 7-9 antiparallel β-strands. As is typical of a siglec IgV domain, each β-sheet in this domain contains more β-strands than those in the IgC domain (Crocker et al. 2007; Miles et al. 2019). There are three disulfide bonds in the extracellular region, one each in the IgV (C41–C101) and IgC (C163–C212) domains and one connecting these two domains (C36–C169) to help stabilize the overall conformation. The extracellular region also contains five known N-glycosylation sites (N100, N113, N160, N209, and N230), with glycosylation at N100 modulating ligand binding to CD33 (Sgroi et al. 1996). The intracellular domain contains an immunoreceptor tyrosine–based inhibitory motif (ITIM) and one ITIM-like motif located at residues 338–343 and 356–361 respectively, with Y340 and Y358 within these motifs being phosphorylated by Src kinases and also docking sites for tyrosine phosphatases SHP-1 and SHP-2 or suppressor of cytokine signaling 3 (SOCS3) (Duan and Paulson 2020; Orr et al. 2007; Paul et al. 2000; Taylor et al. 1999; Ulyanova et al. 1999; Walter 2018). Within the IgV domain, sialic acid–bearing ligands bind to an arginine residue conserved among the siglec family; for CD33, this is R119 (Fig. 5, inset box). CD33 preferentially binds to α2–3 and α2–6 linked sialic acids; these can be components of a variety of ligands for example glycan chains on the cell surface, glycosylated proteins, gangliosides, and amyloid plaques (Chatila and Bradshaw 2021; Duan and Paulson 2020; Miles et al. 2019). In the context of microglia and AD, the most relevant binding partners for CD33 have yet to be identified. There are two main isoforms of CD33, the canonical isoform (also known as CD33M) and an isoform thought to be protective against AD which is missing the sialic acid–binding IgV domain (known as CD33m) (Chatila and Bradshaw 2021; Duan and Paulson 2020; Hernandez-Caselles et al. 2006).
There are currently seven crystal structures in the protein databank (PDB, https://www.rcsb.org) for the extracellular region of human CD33; these contain either the IgV domain alone (PDB IDs: 6D48, 6D49, and 6D4A (Miles et al. 2019)) or both the IgV and IgC domains (PDB IDs: 5IHB, 5J06, 5J0B, and 7AW6). To date, three ligands have been crystallized in complex with the extracellular region of CD33, the CD33-selective sialic acid mimetic P22 (also known as cpd22; Fig. 5, inset box; PDB IDs: 6D49 and 6D4A (Miles et al. 2019); 7AW6), 3̍-sialyllactose (PDB ID: 5J06) and 6̍-sialyllactose (PDB ID: 5J0B). Each of these ligands contains a single sialic acid moiety which engages R119 in the CD33 IgV domain via a salt bridge. P22 has μM affinity for CD33, whereas 3̍-sialyllactose and 6̍-sialyllactose are millimolar affinity ligands (Miles et al. 2019). Antibody cross-linking of the CD33 extracellular domain, together with forced phosphorylation within the intracellular domain, indicates that signaling of CD33 requires at least receptor dimerization (Orr et al. 2007; Paul et al. 2000; Taylor et al. 1999; Ulyanova et al. 1999). Higher-order oligomers may also be involved in CD33 signaling, as it has been demonstrated that the receptors cluster on the cell surface when presented with a multivalent sialic acid–bearing ligand (Miles et al. 2019; Siddiqui et al. 2017). The structures of the CD33 IgV+IgC domain by Dodd and coworkers (PDB IDs: 5IHB, 5J06, and 5J0B; space group P212121) contain four molecules of CD33 in the asymmetric unit and these form two distinct dimer: one where two molecules arrange in a IgC-IgC fashion, forming what could be a functional dimer (Fig. 5), while the other two molecules arrange in a IgV-IgC fashion (i.e., a non-functional dimer). In a different crystal form, Bradshaw and coworkers (PDB ID: 7AW6; space group C121) observed only two CD33 molecules in the asymmetric unit and these were orientated in the IgC-IgC fashion of the putative functional dimer. In this dimer, the sialic acid–binding surfaces are on opposite faces of the IgV domains and the distance between the R119 residues located in each CD33 molecule is ~40 Å. This distance can be spanned by multivalent sialic acid–bearing ligands and we have demonstrated that a biotinylated form of P22 conjugated to streptavidin-labeled microparticles increases the uptake of Aβ in CD33-transfected murine microglia cells as well as increasing phagocytosis (Miles et al. 2019).
While interest in CD33-targeted therapies remains high for acute myeloid leukemia and other hematological malignancies, downregulating CD33 expression or inhibiting its function in the CNS is a hotly pursued area for potential treatments for AD and other neurodegenerative/neuroinflammatory diseases. Despite FDA approval being pulled in 2010 due to severe side effects, gemtuzumab ozogamicin was re-approved by the FDA in 2017 for use in adults with newly diagnosed acute myeloid leukemia (Molica et al. 2021; Walter et al. 2005). CD33-targeted acute myeloid leukemia/cancer therapeutics under development are still largely antibody-based (Walter 2018); for example, chimeric antigen receptor T cell (CART) therapy comprised of a bifunctional single-chain variable fragment (scFv) antibody whose affinity for the CD33 extracellular region is controlled by binding of an FDA-approved small molecule (e.g., methotrexate) (Fig. 5, scFv P02_D09, PDB ID: 6UUP, and 6UY3 (Park et al. 2021)). These approaches could be adapted for use in the CNS, to this end next-generation anti-CD33 antibodies (e.g., AB-64.1.2-huG2, Alector LLC (Culp et al. 2019)) are in early development and also in clinical trials (e.g., AL003 phase I trial NCT03822208 (Imbimbo et al. 2020)) for the treatment of AD and other cognitive disorders. Apart from P22, the only reported small molecules with μM affinity for CD33 are analogs of P22 lacking the galactopyranosyl-glucopyranosyl C2-substituent (Li et al. 2018). The P22:CD33 complexes described above may provide the basis for structure-based design of small molecule modulators of CD33 activity.
TREM2
Like CD33, TREM2 is a cell surface receptor expressed on microglia in the brain; it is also expressed on dendritic cells and macrophages in the periphery (Biber et al. 2019; Kober et al. 2020; Neumann and Takahashi 2007). TREM2 is thought to be anti-inflammatory (Chatila and Bradshaw 2021; Kober et al. 2020; Neumann and Takahashi 2007) and plays a major role in the removal of toxic cellular debris in the brain by activating microglia; for example, it is required for phagocytosis of apoptotic neurons, removal of myelin debris after neuronal injury, and removal of neuronal synapses during the synapse elimination phase in brain development (Kleinberger et al. 2014; Kober et al. 2020; Takahashi et al. 2005). Mutations in TREM2 have been implicated as genetic risk factors for frontotemporal dementia and LOAD, and in recent years, it has drawn a great deal of attention in the pursuit of microglia-specific approaches to treating these diseases. TREM2 acts as a receptor for a number of proteins including Aβ (mediating microglial uptake and degradation of Aβ), lipoproteins (e.g., low-density lipoprotein (LDL), very-low-density lipoprotein (VLDL) and high-density lipoprotein (HDL)), and apolipoproteins, particularly APOE (Atagi et al. 2015; Bailey et al. 2015; Kober et al. 2020; Yeh et al. 2016; Zhao et al. 2018). TREM2 is also known to bind anionic phospholipids such as phosphatidylethanolamine, phosphatidylserine, and sphingomyelin (Kober et al. 2020; Sudom et al. 2018). Sudom and coworkers further demonstrated that binding of phosphatidylserine to TREM2 enhanced receptor oligomerization in solution and activated pSyk signaling in HEK 293T cells expressing TREM2.
In humans, there are four functional members of the TREM protein family, i.e., TREM1, TREM2, TREM-like-1 (TREML1), and TREML2. TREM2 is a type-I transmembrane receptor and the ~25.5 kDa canonical isoform contains 230 residues comprised of an 18 residue N-terminal signal peptide (cleaved to produce the mature protein), followed by a single extracellular IgV domain (residues 19–129) connected to an α-helical TM domain (residues 175–195) by an unstructured JM region (residues 130–174) (Fig. 5). The IgV domain contains two disulfide bonds, one is located between the two parallel β-sheets of the domain (C36–C110) and the second is located on the membrane-proximal ends of β-strands C and C ̍ (C51–C60). In addition, there are two N-glycosylation sites, N20 and N79, in the extracellular domain. A hydrophobic patch (M41, W44, L69, W70, and F74) on the surface of the IgV domain has been reported as the primary interaction surface for APOE, while monomeric Aβ42 has been demonstrated to bind to an adjacent electropositive patch (R47, R62, H67, and R77) on the domain surface (Kober et al. 2016, 2020). Interestingly, phosphatidylserine:TREM2 complex obtained by soaking the phospholipid into unliganded TREM2 crystals showed the phospholipid binding to residues in both the hydrophobic and electropositive surface patches of two adjacent TREM2 molecules in the asymmetric unit (PDB ID: 6B8O (Sudom et al. 2018)). The TREM2 interaction surface defined for APOE, Aβ, and phosphatidylserine contains crevices or hollows, rather than a single ligand-binding pocket. Kober and coworkers recently showed that TREM2 bound both lipidated and unlipidated (i.e., soluble) forms of APOE (both shown in Fig. 5); the highest affinities were observed for the unlipidated forms in the order of APOE4 (281 nM) > APOE3 (440 nM) > APOE2 (590 nM) (Kober et al. 2020). It is interesting to note that the order of TREM2 affinity for the unlipidated APOE isoforms also corresponds to their LOAD risk (Argyri et al. 2014; Yeh et al. 2016), as described in the APOE section below. Kober and co-workers also demonstrated that TREM2 bound monomeric Aβ42 with a KD = 5.1 μM and inhibited self-polymerization of this monomeric form (Kober et al. 2020). The short TREM2 intracellular region (residues 196–230) contains no known signaling motifs; hence, it requires a signaling partner protein.
TREM2 interacts with DNAX-activation protein 12 (DAP12, also known as TYROBP) at the cell membrane via electrostatic interaction between TREM2 K186 and DAP12 D50 (Fig. 5). DAP12 is a disulfide-bonded homodimer containing two intracellular immunoreceptor tyrosine-based activation motifs (ITAMs) and it acts as a signaling partner for a variety of receptor proteins (Duan and Paulson 2020; Kober et al. 2020). Upon ligand binding to TREM2, tyrosine residues within the DAP12 ITAM motifs are phosphorylated by Src kinases thereby initiating the TREM2-DAP12 signaling pathway (Kober et al. 2016; Paradowska-Gorycka and Jurkowska 2013; Sudom et al. 2018; Takahashi et al. 2005).
There are three known isoforms of TREM2: the canonical isoform (described above), a C-terminally truncated isoform where the amino acid sequence differs for residues 162–219 (isoform 2), and a soluble form which lacks the TM and intracellular region (isoform 3, sTREM2). sTREM2 is produced in two ways, translational splicing or proteolytic cleavage by ADAM10 and ADAM17 at residues 157–158 (Jin et al. 2014; Kober et al. 2020; Wunderlich et al. 2013). The membrane-bound fragment can be cleaved further by γ-secretases. Recently, Franzmeier and coworkers have demonstrated that higher levels of sTREM2 in cerebrospinal fluid are associated with attenuated APOE4-related risk for cognitive decline and neurodegeneration typically observed in AD (Franzmeier et al. 2020). Kober and co-workers found that sTREM2 bound APOE2, 3, and 4 with similar affinities (KD = 223–294 nM), unlike full-length TREM2, and bound monomeric Aβ42 with a KD = 3.8 μM (Kober et al. 2020). They also demonstrated that sTREM2 inhibited polymerization of monomeric Aβ42. Based on these observations Kober and co-workers suggested that, like full-length TREM2, sTREM2 also plays a protective role in AD pathogenesis. Interestingly, the level of sTREM2 in AD-affected brains is higher than in normal brains and correlates with Tau and phosphorylated-Tau levels, raising the possibility that inhibiting sTREM2 production or activity may actually be beneficial in reducing the risk of AD (Heslegrave et al. 2016; Piccio et al. 2016; Suarez-Calvet et al. 2016). We look forward to the roles of full-length TREM2 and sTREM2 in microglial activation and AD being clarified.
There are currently eight structures of the TREM2 IgV domain publicly available (PDB IDs: 5ELI, 5UD7, 5UD8, 6B8O, 6Y6C, 6YMQ, 6YYE, and 6XDS (Byrne et al. 2021; Kober et al. 2016; Sudom et al. 2018; Szykowska et al. 2021)), as well as structures of the TM α-helix (PDB IDs: 6Z0G, 6Z0H, and 6Z0I (Steiner et al. 2020)). The unliganded wild-type IgV domain (PDB IDs: 5ELI and 5UD7) is structurally similar (RMSD < 1 Å over all Cα atoms) to that observed in scFv antibody (PDB IDs: 6Y6C, 6YMQ, and 6YYE) and phosphatidylserine (PDB ID: 6B8O) complexes. Microglia expressing an R47H mutation have impaired phagocytosis (Kleinberger et al. 2014; Song et al. 2017; Yuan et al. 2016) and the R47H TREM2 variant increases the risk of developing LOAD by ~2–5-fold (Guerreiro et al. 2013; Jonsson et al. 2013). R47 is located in the electropositive patch of the wild-type TREM2 IgV domain and, while mutation to histidine (R47H) does not have a major impact on the overall domain structure (RMSD = 0.52 over all Cα atoms); there are significant localized structural alterations adjacent to R47H (Fig. 5, PDB ID: 5UD8 (Sudom et al. 2018)). The main structural difference occurs for TREM2 residues H67–T82, a sixteen amino acid section encompassing a loop and a β-strand in the wild-type IgV domain. In the R47H mutant, there is a remodeling of this entire section, the β-strand is lost and electron density is not observed for residues F74–S81. The R47H mutation destroys the electropositive patch surrounding R47 in the wild-type IgV domain, as well as disrupting an extensive hydrogen bond network, resulting in significant alterations to the proposed ligand-binding surface (Sudom et al. 2018). Biophysical studies indicate that the R47H mutation affects both TREM2 stability and structure (Kober et al. 2016; Sudom et al. 2018). Thus, it has been proposed that the TREM2 R47H AD risk variant disrupts ligand binding to the TREM2 IgV domain and, in turn, reduces activation of the TREM2-DAP12 signaling pathway (Kober et al. 2016; Sudom et al. 2018).
Modulating the activity of TREM2 in microglia may offer a new pathway to developing AD treatments and therapeutics for microglial-driven diseases. TREM2-agonistic antibodies like scFv-2 (Fig. 5 (Szykowska et al. 2021)) are the most developed, with one antibody currently in phase II clinical trial for the treatment of AD (i.e., AL002, clinicaltrials.gov ID: NCT04592874) and several antibodies in preclinical development (Chatila and Bradshaw 2021; Ellwanger et al. 2021; Schlepckow et al. 2020). Antisense oligonucleotide therapy and gene therapy candidates are in the early drug discovery phase (Chen et al. 2020; Schoch et al. 2021).
APOE
APOE is a protein expressed primarily in the brain (by astrocytes) and liver (by hepatocytes). It is one of the major proteins involved in lipoprotein transport in the brain and circulatory system (Argyri et al. 2014; Fitz et al. 2021). APOE is an amphipathic molecule that interacts with the aqueous plasma environment as well as lipid particles. In addition to TREM2 (described in the section above), there are many interacting protein partners for APOE including Aβ, heparin, VLDL, and the LDL receptor (LDLR) (Argyri et al. 2014; Henry et al. 2018). There are three isoforms of APOE (APOE2, APOE3, and APOE4); the order of LOAD risk has been determined as APOE4 > APOE3 > APOE2 (Argyri et al. 2014; Yeh et al. 2016). APOE4 is a major genetic risk factor for LOAD, whereas APOE2 appears to be protective against the disease. The binding affinities for lipidated and unlipidated (i.e., soluble) APOE isoforms for TREM2 and sTREM2 are listed in the TREM2 section above. While lipidated APOE is most likely to be monomeric, unlipidated APOE is a mixture of monomers, dimers, and tetramers; the species formed are concentration-dependent and tetramers dominate at concentrations greater than 1 μM (Argyri et al. 2014; Garai et al. 2011; Garai and Frieden 2010; Yeh et al. 2016).
Cleavage of an N-terminal signal peptide (residues 1-18) produces the mature ~34-kDa protein comprising 299 residues. The APOE secondary structure is a series of α-helices, of varying lengths, connected by flexible linkers (Fig. 5). The N-terminal domain (residues 19–185) forms a 4-helical bundle and is followed by the hinge region (residues 186–254) and the C-terminal domain (residues 255–317) contains a long helix encompassing residues 255–284 (Henry et al. 2018; Petros et al. 2019). The hinge region is important for converting the unlipidated helical bundle, or soluble form, to the hairpin conformation of the lipidated form (Fig. 5). APOE contains six O-glycosylation sites (T26, T36, T212, T307, S308, and S314) and one N-glycosylation site, K93. It exists in multiple glycosylated and sialylated forms, the extent of which is governed by its environment, and it is not required for proper APOE expression or secretion (Kockx et al. 2018; Wernette-Hammond et al. 1989). The binding site for LDLR and other lipoprotein receptors encompasses APOE residues 158–168; with R152, R160, R163, and R190 being important for high-affinity binding (Henry et al. 2018). Heparin has been reported to bind at residues 162–165 and 229–236. Residues 210–290 are involved in lipid binding and lipoprotein association, with APOE residues 278–290 having specificity for VLDL binding. Using truncation mutants of APOE3, Kober et al. (2020) demonstrated that hinge residues 210–256 were responsible for the primary interaction with TREM2 (Kober et al. 2020). There is a homo-oligomerization region in the C-terminal domain of APOE, located at residues 266–317.
The three isoforms of APOE differ at residues 130 and 176; APOE2 has cysteine residues at both positions and APOE3 has C130 and R176 while APOE4 has arginine residues at both positions (Argyri et al. 2014). The relative stability of the three isoforms is APOE2 > APOE3 > APOE4 and is likely related to the nature of the residues at positions 130 and 176. There are a multitude of APOE isoform variants, one of particular interest is the naturally occurring Pittsburgh variant APOE4 L46P (L28P in the mature protein, SNP ID:rs769452). Carriers of this APOE4 mutant have a substantially higher risk of developing LOAD. L46 is located near the start of a helix in the N-terminal domain 4-helix bundle and the proline mutation appears to reduce protein stability and affect conformation (Argyri et al. 2014). A search conducted in the PDB (August 2021) identified >100 structures of fragments of varying lengths of human APOE and other apolipoproteins, such as APOA, in lipidated and unlipidated conditions. Models for lipidated and unlipidated human APOE4 (residues 19–317) are shown in Fig. 5.
Summary/conclusions
There is no doubt that structural biology, in particular X-ray crystallography and more recently cryo-electron microscopy, has contributed key insights into the physiological and pathological functions of key proteins implicated in AD. In this review, we focused on cell surface receptors strongly implicated by human genetic studies in the pathogenesis of AD. We have shown that structural studies have given valuable insights into the normal function of the receptors, for example, revealing growth factor and metal-binding activities of APP, a snapshot of the many conformational states adopted by the Aβ peptide, and how CD33 recognizes carbohydrate molecules. We have also shown how these structures have provided key insights and guidance into the development of drugs, both biologics and small molecules, for example, BACE inhibitors, antibodies directed towards various epitopes and aggregation states of Aβ, and small molecule development of CD33 inhibitors. As genetic studies and omics technologies become more sophisticated, it is expected many more drug targets will be revealed as the complicated interactome networks underpinning AD are increasingly revealed. We expect structural biology will continue to make significant contributions to our understanding of the molecular events that underlie AD.
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- Aβ:
-
Amyloid-beta
- AD:
-
Alzheimer’s disease
- APOE:
-
Apolipoprotein E
- APP:
-
Amyloid precursor protein
- BACE:
-
β-secretase
- CD33:
-
Myeloid cell surface antigen cluster of differentiation 33
- CuBD:
-
Copper-binding domain
- CNS:
-
Central nervous system
- DAP12:
-
DNAX-activation protein 12
- FDA:
-
U. S. Food and Drug Administration
- GFD:
-
Growth factor–like domain
- GWAS:
-
Genome-wide association studies
- HDL:
-
High-density lipoprotein
- HSPG:
-
Heparin sulfate proteoglycan
- Ig:
-
Immunoglobulin
- ITAM:
-
Immunoreceptor tyrosine–based activation motif
- ITIM:
-
Immunoreceptor tyrosine–based inhibitory motif
- JM:
-
Juxtamembrane
- LDL:
-
Low-density lipoprotein
- LDLR:
-
LDL receptor
- LOAD:
-
Late-onset Alzheimer’s disease
- mAb:
-
Monoclonal antibody
- NMR:
-
Nuclear magnetic resonance
- PDB:
-
Protein databank
- PLCG2:
-
1-Phosphatidylinositol 4,5-bisphosphate phosphodiesterase gamma-2
- RMSD:
-
Root-mean-square-deviation
- scFv:
-
Single-chain variable fragment
- siglec:
-
Sialic acid–binding immunoglobulin (Ig)–like lectin
- sTREM2:
-
Soluble form of TREM2
- TREM2:
-
Triggering receptor expressed on myeloid cells 2
- TM:
-
Transmembrane
- VLDL:
-
Very-low-density lipoprotein
References
Adolfsson O, Pihlgren M, Toni N, Varisco Y, Buccarello AL, Antoniello K, Lohmann S, Piorkowska K, Gafner V, Atwal JK, Maloney J, Chen M, Gogineni A, Weimer RM, Mortensen DL, Friesenhahn M, Ho C, Paul R, Pfeifer A et al (2012) An effector-reduced anti-beta-amyloid (Abeta) antibody with unique abeta binding properties promotes neuroprotection and glial engulfment of Abeta. J Neurosci 32:9677–9689. https://doi.org/10.1523/JNEUROSCI.4742-11.2012
Alzheimer’s Association (2012) Alzheimer’s disease facts and figures. Alzheimer’s Dementia 8:131–168. https://doi.org/10.1016/j.jalz.2012.02.001
Anandatheerthavarada HK, Biswas G, Robin MA, Avadhani NG (2003) Mitochondrial targeting and a novel transmembrane arrest of Alzheimer’s amyloid precursor protein impairs mitochondrial function in neuronal cells. J Cell Biol 161:41–54. https://doi.org/10.1083/jcb.200207030
Appelbaum FR, Matthews DC, Eary JF, Badger CC, Kellogg M, Press OW, Martin PJ, Fisher DR, Nelp WB, Thomas ED et al (1992) The use of radiolabeled anti-CD33 antibody to augment marrow irradiation prior to marrow transplantation for acute myelogenous leukemia. Transplantation 54:829–833. https://doi.org/10.1097/00007890-199211000-00012
Argyri L, Dafnis I, Theodossiou TA, Gantz D, Stratikos E, Chroni A (2014) Molecular basis for increased risk for late-onset Alzheimer disease due to the naturally occurring L28P mutation in apolipoprotein E4. J Biol Chem 289:12931–12945. https://doi.org/10.1074/jbc.M113.538124
Armour KL, van de Winkel JG, Williamson LM, Clark MR (2003) Differential binding to human FcgammaRIIa and FcgammaRIIb receptors by human IgG wild-type and mutant antibodies. Mol Immunol 40:585–593. https://doi.org/10.1016/j.molimm.2003.08.004
Arndt JW, Qian F, Smith BA, Quan C, Kilambi KP, Bush MW, Walz T, Pepinsky RB, Bussiere T, Hamann S, Cameron TO, Weinreb PH (2018) Structural and kinetic basis for the selectivity of aducanumab for aggregated forms of amyloid beta. Sci Rep 8:6412. https://doi.org/10.1038/s41598-018-24501-0
Atagi Y, Liu CC, Painter MM, Chen XF, Verbeeck C, Zheng H, Li X, Rademakers R, Kang SS, Xu H, Younkin S, Das P, Fryer JD, Bu G (2015) Apolipoprotein E Is a ligand for triggering receptor expressed on myeloid cells 2 (TREM2). J Biol Chem 290:26043–26050. https://doi.org/10.1074/jbc.M115.679043
Bailey CC, DeVaux LB, Farzan M (2015) The triggering receptor expressed on myeloid cells 2 binds apolipoprotein E. J Biol Chem 290:26033–26042. https://doi.org/10.1074/jbc.M115.677286
Bard F, Barbour R, Cannon C, Carretto R, Fox M, Games D, Guido T, Hoenow K, Hu K, Johnson-Wood K, Khan K, Kholodenko D, Lee C, Lee M, Motter R, Nguyen M, Reed A, Schenk D, Tang P et al (2003) Epitope and isotype specificities of antibodies to beta-amyloid peptide for protection against Alzheimer’s disease-like neuropathology. Proc Natl Acad Sci U S A 100:2023–2028. https://doi.org/10.1073/pnas.0436286100
Bard F, Cannon C, Barbour R, Burke RL, Games D, Grajeda H, Guido T, Hu K, Huang J, Johnson-Wood K, Khan K, Kholodenko D, Lee M, Lieberburg I, Motter R, Nguyen M, Soriano F, Vasquez N, Weiss K et al (2000) Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat Med 6:916–919. https://doi.org/10.1038/78682
Barnham KJ, McKinstry WJ, Multhaup G, Galatis D, Morton CJ, Curtain CC, Williamson NA, White AR, Hinds MG, Norton RS, Beyreuther K, Masters CL, Parker MW, Cappai R (2003) Structure of the Alzheimer’s disease amyloid precursor protein copper binding domain. A regulator of neuronal copper homeostasis. J Biol Chem 278:17401–17407. https://doi.org/10.1074/jbc.M300629200
Benzinger TL, Gregory DM, Burkoth TS, Miller-Auer H, Lynn DG, Botto RE, Meredith SC (1998) Propagating structure of Alzheimer’s beta-amyloid (10-35) is parallel beta-sheet with residues in exact register. Proc Natl Acad Sci U S A 95:13407–13412. https://doi.org/10.1073/pnas.95.23.13407
Bernstein SL, Dupuis NF, Lazo ND, Wyttenbach T, Condron MM, Bitan G, Teplow DB, Shea JE, Ruotolo BT, Robinson CV, Bowers MT (2009) Amyloid-β protein oligomerization and the importance of tetramers and dodecamers in the aetiology of Alzheimer’s disease. Nat Chem 1:326–331. https://doi.org/10.1038/nchem.247
Biber K, Bhattacharya A, Campbell BM, Piro JR, Rohe M, Staal RGW, Talanian RV, Moller T (2019) Microglial drug targets in AD: opportunities and challenges in drug discovery and development. Front Pharmacol 10:840. https://doi.org/10.3389/fphar.2019.00840
Bitan G, Kirkitadze MD, Lomakin A, Vollers SS, Benedek GB, Teplow DB (2003) Amyloid β-protein (Aβ) assembly: Aβ40 and Aβ42 oligomerize through distinct pathways. PNAS 100:330–335. https://doi.org/10.1073/pnas.222681699
Bloom GS (2014) Amyloid-beta and tau: the trigger and bullet in Alzheimer disease pathogenesis. JAMA Neurol 71:505–508. https://doi.org/10.1001/jamaneurol.2013.5847
Bohrmann B, Baumann K, Benz J, Gerber F, Huber W, Knoflach F, Messer J, Oroszlan K, Rauchenberger R, Richter WF, Rothe C, Urban M, Bardroff M, Winter M, Nordstedt C, Loetscher H (2012) Gantenerumab: a novel human anti-Abeta antibody demonstrates sustained cerebral amyloid-beta binding and elicits cell-mediated removal of human amyloid-beta. J Alzheimers Dis 28:49–69. https://doi.org/10.3233/JAD-2011-110977
Borg JP, Ooi J, Levy E, Margolis B (1996) The phosphotyrosine interaction domains of X11 and FE65 bind to distinct sites on the YENPTY motif of amyloid precursor protein. Mol Cell Biol 16:6229–6241. https://doi.org/10.1128/MCB.16.11.6229
Brazil MI, Chung H, Maxfield FR (2000) Effects of incorporation of immunoglobulin G and complement component C1q on uptake and degradation of Alzheimer’s disease amyloid fibrils by microglia. J Biol Chem 275:16941–16947. https://doi.org/10.1074/jbc.M000937200
Brooks AJ, Dai W, O’Mara ML, Abankwa D, Chhabra Y, Pelekanos RA, Gardon O, Tunny KA, Blucher KM, Morton CJ, Parker MW, Sierecki E, Gambin Y, Gomez GA, Alexandrov K, Wilson IA, Doxastakis M, Mark AE, Waters MJ (2014) Mechanism of activation of protein kinase JAK2 by the growth hormone receptor. Science 344:1249783. https://doi.org/10.1126/science.1249783
Brouillet E, Trembleau A, Galanaud D, Volovitch M, Bouillot C, Valenza C, Prochiantz A, Allinquant B (1999) The amyloid precursor protein interacts with Go heterotrimeric protein within a cell compartment specialized in signal transduction. J Neurosci 19:1717–1727
Bukhari H, Glotzbach A, Kolbe K, Leonhardt G, Loosse C, Müller T (2017) Small things matter: Implications of APP intracellular domain AICD nuclear signaling in the progression and pathogenesis of Alzheimer’s disease. Prog Neurobiol 156:189–213. https://doi.org/10.1016/j.pneurobio.2017.05.005
Byrne NJ, Lee AC, Kostas J, Reid JC, Partridge AT, So SS, Cowan JE, Abeywickrema P, Huang H, Zebisch M, Barker JJ, Soisson SM, Brooun A, Su HP (2021) Development of a robust crystallization platform for immune receptor TREM2 using a crystallization chaperone strategy. Protein Expr Purif 179:105796. https://doi.org/10.1016/j.pep.2020.105796
Chasseigneaux S, Allinquant B (2012) Functions of Abeta, sAPPalpha and sAPPbeta: similarities and differences. J Neurochem 120(Suppl 1):99–108. https://doi.org/10.1111/j.1471-4159.2011.07584.x
Chatila ZK, Bradshaw EM (2021) Alzheimer’s disease genetics: a dampened microglial response? Neuroscientist. https://doi.org/10.1177/10738584211024531
Chen GF, Xu TH, Yan Y, Zhou YR, Jiang Y, Melcher K, Xu HE (2017) Amyloid beta: structure, biology and structure-based therapeutic development. Acta Pharmacol Sin 38:1205–1235. https://doi.org/10.1038/aps.2017.28
Chen W, Hu Y, Ju D (2020) Gene therapy for neurodegenerative disorders: advances, insights and prospects. Acta Pharm Sin B 10:1347–1359. https://doi.org/10.1016/j.apsb.2020.01.015
Choi SH, Kim YH, Hebisch M, Sliwinski C, Lee S, D’Avanzo C, Chen H, Hooli B, Asselin C, Muffat J, Klee JB, Zhang C, Wainger BJ, Peitz M, Kovacs DM, Woolf CJ, Wagner SL, Tanzi RE, Kim DY (2014) A three-dimensional human neural cell culture model of Alzheimer’s disease. Nature 515:274–278. https://doi.org/10.1038/nature13800
Chow N, Korenberg JR, Chen XN, Neve RL (1996) APP-BP1, a novel protein that binds to the carboxyl-terminal region of the amyloid precursor protein. J Biol Chem 271:11339–11346. https://doi.org/10.1074/jbc.271.19.11339
Cohen SI, Linse S, Luheshi LM, Hellstrand E, White DA, Rajah L, Otzen DE, Vendruscolo M, Dobson CM, Knowles TP (2013) Proliferation of amyloid-beta42 aggregates occurs through a secondary nucleation mechanism. Proc Natl Acad Sci U S A 110:9758–9763. https://doi.org/10.1073/pnas.1218402110
Coles M, Bicknell W, Watson AA, Fairlie DP, Craik DJ (1998) Solution structure of amyloid beta-peptide(1-40) in a water-micelle environment. Is the membrane-spanning domain where we think it is? Biochemistry 37:11064–11077. https://doi.org/10.1021/bi972979f
Copenhaver PF, Kögel D (2017) Role of APP interactions with heterotrimeric G proteins: physiological functions and pathological consequences. Front Mol Neurosci 10:3. https://doi.org/10.3389/fnmol.2017.00003
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261:921–923. https://doi.org/10.1126/science.8346443
Côté S, Laghaei R, Derreumaux P, Mousseau N (2012) Distinct dimerization for various alloforms of the amyloid-beta protein: Aβ1-40, Aβ1-42, and Aβ1-40(D23N). J Phys Chem B 116:4043–4055. https://doi.org/10.1021/jp2126366
Crescenzi O, Tomaselli S, Guerrini R, Salvadori S, D’Ursi AM, Temussi PA, Picone D (2002) Solution structure of the Alzheimer amyloid beta-peptide (1-42) in an apolar microenvironment. Similarity with a virus fusion domain. Eur J Biochem 269:5642–5648. https://doi.org/10.1046/j.1432-1033.2002.03271.x
Crespi GA, Hermans SJ, Parker MW, Miles LA (2015) Molecular basis for mid-region amyloid-beta capture by leading Alzheimer’s disease immunotherapies. Sci Rep 5:9649. https://doi.org/10.1038/srep09649
Crocker PR, Paulson JC, Varki A (2007) Siglecs and their roles in the immune system. Nat Rev Immunol 7:255–266. https://doi.org/10.1038/nri2056
Culp P, Lam H, Rosenthal A, Lee S-J, Nielson NP, Pejchal R (2019) Anti-CD33 antibodies and methods of use thereof wo/2019/028283, ALECTOR LLC
Dahms SO, Hoefgen S, Roeser D, Schlott B, Guhrs KH, Than ME (2010) Structure and biochemical analysis of the heparin-induced E1 dimer of the amyloid precursor protein. Proc Natl Acad Sci U S A 107:5381–5386. https://doi.org/10.1073/pnas.0911326107
Dahms SO, Konnig I, Roeser D, Guhrs KH, Mayer MC, Kaden D, Multhaup G, Than ME (2012) Metal binding dictates conformation and function of the amyloid precursor protein (APP) E2 domain. J Mol Biol 416:438–452. https://doi.org/10.1016/j.jmb.2011.12.057
Das P, Verbeeck C, Minter L, Chakrabarty P, Felsenstein K, Kukar T, Maharvi G, Fauq A, Osborne BA, Golde TE (2012) Transient pharmacologic lowering of Abeta production prior to deposition results in sustained reduction of amyloid plaque pathology. Mol Neurodegener 7:39. https://doi.org/10.1186/1750-1326-7-39
DeMattos RB, Bales KR, Cummins DJ, Dodart JC, Paul SM, Holtzman DM (2001) Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A 98:8850–8855. https://doi.org/10.1073/pnas.151261398
Deyts C, Thinakaran G, Parent AT (2016) APP receptor? To be or not to be. Trends Pharmacol Sci 37:390–411. https://doi.org/10.1016/j.tips.2016.01.005
Doody RS, Raman R, Farlow M, Iwatsubo T, Vellas B, Joffe S, Kieburtz K, He F, Sun X, Thomas RG, Aisen PS, Alzheimer’s Disease Cooperative Study Steering C, Siemers E, Sethuraman G, Mohs R, Semagacestat Study G (2013) A phase 3 trial of semagacestat for treatment of Alzheimer’s disease. N Engl J Med 369:341–350. https://doi.org/10.1056/NEJMoa1210951
Duan S, Paulson JC (2020) Siglecs as immune cell checkpoints in disease. Annu Rev Immunol 38:365–395. https://doi.org/10.1146/annurev-immunol-102419-035900
Dunys J, Valverde A, Checler F (2018) Are N- and C-terminally truncated Aβ species key pathological triggers in Alzheimer’s disease? J Biol Chem 293:15419–15428. https://doi.org/10.1074/jbc.R118.003999
Eggert S, Midthune B, Cottrell B, Koo EH (2009) Induced dimerization of the amyloid precursor protein leads to decreased amyloid-beta protein production. J Biol Chem 284:28943–28952. https://doi.org/10.1074/jbc.M109.038646
Ellwanger DC, Wang S, Brioschi S, Shao Z, Green L, Case R, Yoo D, Weishuhn D, Rathanaswami P, Bradley J, Rao S, Cha D, Luan P, Sambashivan S, Gilfillan S, Hasson SA, Foltz IN, van Lookeren CM, Colonna M (2021) Prior activation state shapes the microglia response to antihuman TREM2 in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2017742118
Ennerfelt HE, Lukens JR (2020) The role of innate immunity in Alzheimer’s disease. Immunol Rev 297:225–246. https://doi.org/10.1111/imr.12896
Ezeani M, Omabe M (2016) A new perspective of lysosomal cation channel-dependent homeostasis in Alzheimer’s disease. Mol Neurobiol 53:1672–1678. https://doi.org/10.1007/s12035-015-9108-3
Feinberg H, Saldanha JW, Diep L, Goel A, Widom A, Veldman GM, Weis WI, Schenk D, Basi GS (2014) Crystal structure reveals conservation of amyloid-beta conformation recognized by 3D6 following humanization to bapineuzumab. Alzheimers Res Ther 6:31. https://doi.org/10.1186/alzrt261
Fezoui Y, Teplow DB (2002) Kinetic studies of amyloid beta-protein fibril assembly. Differential effects of alpha-helix stabilization. J Biol Chem 277:36948–36954. https://doi.org/10.1074/jbc.M204168200
Filiano AJ, Gadani SP, Kipnis J (2015) Interactions of innate and adaptive immunity in brain development and function. Brain Res 1617:18–27. https://doi.org/10.1016/j.brainres.2014.07.050
Fiore F, Zambrano N, Minopoli G, Donini V, Duilio A, Russo T (1995) The regions of the Fe65 protein homologous to the phosphotyrosine interaction/phosphotyrosine binding domain of Shc bind the intracellular domain of the Alzheimer’s amyloid precursor protein. J Biol Chem 270:30853–30856. https://doi.org/10.1074/jbc.270.52.30853
Fitz NF, Nam KN, Wolfe CM, Letronne F, Playso BE, Iordanova BE, Kozai TDY, Biedrzycki RJ, Kagan VE, Tyurina YY, Han X, Lefterov I, Koldamova R (2021) Phospholipids of APOE lipoproteins activate microglia in an isoform-specific manner in preclinical models of Alzheimer’s disease. Nat Commun 12:3416. https://doi.org/10.1038/s41467-021-23762-0
Franzmeier N, Suarez-Calvet M, Frontzkowski L, Moore A, Hohman TJ, Morenas-Rodriguez E, Nuscher B, Shaw L, Trojanowski JQ, Dichgans M, Kleinberger G, Haass C, Ewers M, Alzheimer’s Disease Neuroimaging I (2020) Higher CSF sTREM2 attenuates ApoE4-related risk for cognitive decline and neurodegeneration. Mol Neurodegener 15:57. https://doi.org/10.1186/s13024-020-00407-2
Fyfe I (2021) Dense-core plaques could be beneficial in AD. Nat Rev Neurol 17:328. https://doi.org/10.1038/s41582-021-00513-9
Garai K, Baban B, Frieden C (2011) Dissociation of apolipoprotein E oligomers to monomer is required for high-affinity binding to phospholipid vesicles. Biochemistry 50:2550–2558. https://doi.org/10.1021/bi1020106
Garai K, Frieden C (2010) The association-dissociation behavior of the ApoE proteins: kinetic and equilibrium studies. Biochemistry 49:9533–9541. https://doi.org/10.1021/bi101407m
Ghosh U, Thurber KR, Yau WM, Tycko R (2021) Molecular structure of a prevalent amyloid-beta fibril polymorph from Alzheimer’s disease brain tissue. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2023089118
Gremer L, Scholzel D, Schenk C, Reinartz E, Labahn J, Ravelli RBG, Tusche M, Lopez-Iglesias C, Hoyer W, Heise H, Willbold D, Schroder GF (2017) Fibril structure of amyloid-beta(1-42) by cryo-electron microscopy. Science 358:116–119. https://doi.org/10.1126/science.aao2825
Griciuc A, Patel S, Federico AN, Choi SH, Innes BJ, Oram MK, Cereghetti G, McGinty D, Anselmo A, Sadreyev RI, Hickman SE, El Khoury J, Colonna M, Tanzi RE (2019) TREM2 acts downstream of CD33 in modulating microglial pathology in Alzheimer’s disease. Neuron 103(820-835):e827. https://doi.org/10.1016/j.neuron.2019.06.010
Griciuc A, Tanzi RE (2021) The role of innate immune genes in Alzheimer’s disease. Curr Opin Neurol 34:228–236. https://doi.org/10.1097/WCO.0000000000000911
Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, Cruchaga C, Sassi C, Kauwe JS, Younkin S, Hazrati L, Collinge J, Pocock J, Lashley T, Williams J, Lambert JC, Amouyel P, Goate A, Rademakers R et al (2013) TREM2 variants in Alzheimer’s disease. N Engl J Med 368:117–127. https://doi.org/10.1056/NEJMoa1211851
Hardy J, Allsop D (1991) Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends Pharmacol Sci 12:383–388. https://doi.org/10.1016/0165-6147(91)90609-v
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297:353–356. https://doi.org/10.1126/science.1072994
Hardy JA, Higgins GA (1992) Alzheimer’s disease: the amyloid cascade hypothesis. Science 256:184–185. https://doi.org/10.1126/science.1566067
Heneka MT, Golenbock DT, Latz E (2015) Innate immunity in Alzheimer’s disease. Nat Immunol 16:229–236. https://doi.org/10.1038/ni.3102
Henry N, Krammer EM, Stengel F, Adams Q, Van Liefferinge F, Hubin E, Chaves R, Efremov R, Aebersold R, Vandenbussche G, Prevost M, Raussens V, Deroo S (2018) Lipidated apolipoprotein E4 structure and its receptor binding mechanism determined by a combined cross-linking coupled to mass spectrometry and molecular dynamics approach. PLoS Comput Biol 14:e1006165. https://doi.org/10.1371/journal.pcbi.1006165
Hernandez-Caselles T, Martinez-Esparza M, Perez-Oliva AB, Quintanilla-Cecconi AM, Garcia-Alonso A, Alvarez-Lopez DM, Garcia-Penarrubia P (2006) A study of CD33 (SIGLEC-3) antigen expression and function on activated human T and NK cells: two isoforms of CD33 are generated by alternative splicing. J Leukoc Biol 79:46–58. https://doi.org/10.1189/jlb.0205096
Hernandez D, Egan SE, Yulug IG, Fisher EM (1994) Mapping the gene that encodes phosphatidylinositol-specific phospholipase C-gamma 2 in the human and the mouse. Genomics 23:504–507. https://doi.org/10.1006/geno.1994.1533
Heslegrave A, Heywood W, Paterson R, Magdalinou N, Svensson J, Johansson P, Ohrfelt A, Blennow K, Hardy J, Schott J, Mills K, Zetterberg H (2016) Increased cerebrospinal fluid soluble TREM2 concentration in Alzheimer’s disease. Mol Neurodegener 11:3. https://doi.org/10.1186/s13024-016-0071-x
Hollingworth P, Harold D, Sims R, Gerrish A, Lambert JC, Carrasquillo MM, Abraham R, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Jones N, Stretton A, Thomas C, Richards A, Ivanov D, Widdowson C, Chapman J, Lovestone S et al (2011) Common variants at ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP are associated with Alzheimer’s disease. Nat Genet 43:429–435. https://doi.org/10.1038/ng.803
Hollingworth P, Sweet R, Sims R, Harold D, Russo G, Abraham R, Stretton A, Jones N, Gerrish A, Chapman J, Ivanov D, Moskvina V, Lovestone S, Priotsi P, Lupton M, Brayne C, Gill M, Lawlor B, Lynch A et al (2012) Genome-wide association study of Alzheimer’s disease with psychotic symptoms. Mol Psychiatry 17:1316–1327. https://doi.org/10.1038/mp.2011.125
Hong L, Koelsch G, Lin X, Wu S, Terzyan S, Ghosh AK, Zhang XC, Tang J (2000) Structure of the protease domain of memapsin 2 (beta-secretase) complexed with inhibitor. Science 290:150–153. https://doi.org/10.1126/science.290.5489.150
Hynes TR, Randal M, Kennedy LA, Eigenbrot C, Kossiakoff AA (1990) X-ray crystal structure of the protease inhibitor domain of Alzheimer’s amyloid beta-protein precursor. Biochemistry 29:10018–10022. https://doi.org/10.1021/bi00495a002
Imbimbo BP, Lozupone M, Watling M, Panza F (2020) Discontinued disease-modifying therapies for Alzheimer’s disease: status and future perspectives. Expert Opin Investig Drugs 29:919–933. https://doi.org/10.1080/13543784.2020.1795127
Isbert S, Wagner K, Eggert S, Schweitzer A, Multhaup G, Weggen S, Kins S, Pietrzik CU (2012) APP dimer formation is initiated in the endoplasmic reticulum and differs between APP isoforms. Cell Mol Life Sci 69:1353–1375. https://doi.org/10.1007/s00018-011-0882-4
Jarrett JT, Berger EP, Lansbury PT Jr (1993) The carboxy terminus of the β amyloid protein is critical for the seeding of amyloid formation: implications for the pathogenesis of Alzheimer’s disease. Biochemistry 32:4693–4697. https://doi.org/10.1021/bi00069a001
Jin SC, Benitez BA, Karch CM, Cooper B, Skorupa T, Carrell D, Norton JB, Hsu S, Harari O, Cai Y, Bertelsen S, Goate AM, Cruchaga C (2014) Coding variants in TREM2 increase risk for Alzheimer’s disease. Hum Mol Genet 23:5838–5846. https://doi.org/10.1093/hmg/ddu277
Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, Bjornsson S, Huttenlocher J, Levey AI, Lah JJ, Rujescu D, Hampel H, Giegling I, Andreassen OA, Engedal K, Ulstein I, Djurovic S, Ibrahim-Verbaas C, Hofman A et al (2013) Variant of TREM2 associated with the risk of Alzheimer’s disease. N Engl J Med 368:107–116. https://doi.org/10.1056/NEJMoa1211103
Jumper J, Evans R, Pritzel A, Green T, Figurnov M, Ronneberger O, Tunyasuvunakool K, Bates R, Zidek A, Potapenko A, Bridgland A, Meyer C, Kohl SAA, Ballard AJ, Cowie A, Romera-Paredes B, Nikolov S, Jain R, Adler J et al (2021) Highly accurate protein structure prediction with AlphaFold. Nature 596:583–589. https://doi.org/10.1038/s41586-021-03819-2
Kabba JA, Xu Y, Christian H, Ruan W, Chenai K, Xiang Y, Zhang L, Saavedra JM, Pang T (2018) Microglia: housekeeper of the central nervous system. Cell Mol Neurobiol 38:53–71. https://doi.org/10.1007/s10571-017-0504-2
Kang J, Lemaire HG, Unterbeck A, Salbaum JM, Masters CL, Grzeschik KH, Multhaup G, Beyreuther K, Muller-Hill B (1987) The precursor of Alzheimer’s disease amyloid A4 protein resembles a cell-surface receptor. Nature 325:733–736. https://doi.org/10.1038/325733a0
Keren-Shaul H, Spinrad A, Weiner A, Matcovitch-Natan O, Dvir-Szternfeld R, Ulland TK, David E, Baruch K, Lara-Astaiso D, Toth B, Itzkovitz S, Colonna M, Schwartz M, Amit I (2017) A unique microglia type associated with restricting development of Alzheimer’s disease. Cell 169(1276-1290):e1217. https://doi.org/10.1016/j.cell.2017.05.018
Khalifa NB, Van Hees J, Tasiaux B, Huysseune S, Smith SO, Constantinescu SN, Octave JN, Kienlen-Campard P (2010) What is the role of amyloid precursor protein dimerization? Cell Adh Migr 4:268–272. https://doi.org/10.4161/cam.4.2.11476
Kim BH, Lyubchenko YL (2014) Nanoprobing of misfolding and interactions of amyloid β 42 protein. Nanomedicine 10:871–878. https://doi.org/10.1016/j.nano.2013.11.016
Kirkitadze MD, Condron MM, Teplow DB (2001) Identification and characterization of key kinetic intermediates in amyloid beta-protein fibrillogenesis. J Mol Biol 312:1103–1119. https://doi.org/10.1006/jmbi.2001.4970
Klein WL, Krafft GA, Finch CE (2001) Targeting small Abeta oligomers: the solution to an Alzheimer’s disease conundrum? Trends Neurosci 24:219–224. https://doi.org/10.1016/s0166-2236(00)01749-5
Kleinberger G, Yamanishi Y, Suarez-Calvet M, Czirr E, Lohmann E, Cuyvers E, Struyfs H, Pettkus N, Wenninger-Weinzierl A, Mazaheri F, Tahirovic S, Lleo A, Alcolea D, Fortea J, Willem M, Lammich S, Molinuevo JL, Sanchez-Valle R, Antonell A et al (2014) TREM2 mutations implicated in neurodegeneration impair cell surface transport and phagocytosis. Sci Transl Med 6:243ra286. https://doi.org/10.1126/scitranslmed.3009093
Kober DL, Alexander-Brett JM, Karch CM, Cruchaga C, Colonna M, Holtzman MJ, Brett TJ (2016) Neurodegenerative disease mutations in TREM2 reveal a functional surface and distinct loss-of-function mechanisms. Elife 5 https://doi.org/10.7554/eLife.20391
Kober DL, Stuchell-Brereton MD, Kluender CE, Dean HB, Strickland MR, Steinberg DF, Nelson SS, Baban B, Holtzman DM, Frieden C, Alexander-Brett J, Roberson ED, Song Y, Brett TJ (2020) Functional insights from biophysical study of TREM2 interactions with apoE and Abeta1-42. Alzheimers Dement. https://doi.org/10.1002/alz.12194
Kockx M, Traini M, Kritharides L (2018) Cell-specific production, secretion, and function of apolipoprotein E. J Mol Med (Berl) 96:361–371. https://doi.org/10.1007/s00109-018-1632-y
Kollmer M, Close W, Funk L, Rasmussen J, Bsoul A, Schierhorn A, Schmidt M, Sigurdson CJ, Jucker M, Fandrich M (2019) Cryo-EM structure and polymorphism of Abeta amyloid fibrils purified from Alzheimer’s brain tissue. Nat Commun 10:4760. https://doi.org/10.1038/s41467-019-12683-8
Kong GK, Adams JJ, Cappai R, Parker MW (2007a) Structure of Alzheimer’s disease amyloid precursor protein copper-binding domain at atomic resolution. Acta Crystallogr Sect F Struct Biol Cryst Commun 63:819–824. https://doi.org/10.1107/S1744309107041139
Kong GK, Adams JJ, Harris HH, Boas JF, Curtain CC, Galatis D, Masters CL, Barnham KJ, McKinstry WJ, Cappai R, Parker MW (2007b) Structural studies of the Alzheimer’s amyloid precursor protein copper-binding domain reveal how it binds copper ions. J Mol Biol 367:148–161. https://doi.org/10.1016/j.jmb.2006.12.041
Kong GK, Miles LA, Crespi GA, Morton CJ, Ng HL, Barnham KJ, McKinstry WJ, Cappai R, Parker MW (2008) Copper binding to the Alzheimer’s disease amyloid precursor protein. Eur Biophys J 37:269–279. https://doi.org/10.1007/s00249-007-0234-3
Krasemann S, Madore C, Cialic R, Baufeld C, Calcagno N, El Fatimy R, Beckers L, O’Loughlin E, Xu Y, Fanek Z, Greco DJ, Smith ST, Tweet G, Humulock Z, Zrzavy T, Conde-Sanroman P, Gacias M, Weng Z, Chen H et al (2017) The TREM2-APOE pathway drives the transcriptional phenotype of dysfunctional microglia in neurodegenerative diseases. Immunity 47(566-581):e569. https://doi.org/10.1016/j.immuni.2017.08.008
Krishtal J, Bragina O, Metsla K, Palumaa P, Tougu V (2017) In situ fibrillizing amyloid-beta 1-42 induces neurite degeneration and apoptosis of differentiated SH-SY5Y cells. PLoS One 12:e0186636. https://doi.org/10.1371/journal.pone.0186636
Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, Boland A, Vronskaya M, van der Lee SJ, Amlie-Wolf A, Bellenguez C, Frizatti A, Chouraki V, Martin ER, Sleegers K, Badarinarayan N, Jakobsdottir J, Hamilton-Nelson KL, Moreno-Grau S et al (2019) Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Abeta, tau, immunity and lipid processing. Nat Genet 51:414–430. https://doi.org/10.1038/s41588-019-0358-2
La Porte SL, Bollini SS, Lanz TA, Abdiche YN, Rusnak AS, Ho WH, Kobayashi D, Harrabi O, Pappas D, Mina EW, Milici AJ, Kawabe TT, Bales K, Lin JC, Pons J (2012) Structural basis of C-terminal beta-amyloid peptide binding by the antibody ponezumab for the treatment of Alzheimer’s disease. J Mol Biol 421:525–536. https://doi.org/10.1016/j.jmb.2011.11.047
Lahiri DK, Maloney B, Long JM, Greig NH (2014) Lessons from a BACE1 inhibitor trial: off-site but not off base. Alzheimers Dement 10:S411–S419. https://doi.org/10.1016/j.jalz.2013.11.004
Landen JW, Zhao Q, Cohen S, Borrie M, Woodward M, Billing CB Jr, Bales K, Alvey C, McCush F, Yang J, Kupiec JW, Bednar MM (2013) Safety and pharmacology of a single intravenous dose of ponezumab in subjects with mild-to-moderate Alzheimer disease: a phase I, randomized, placebo-controlled, double-blind, dose-escalation study. Clin Neuropharmacol 36:14–23. https://doi.org/10.1097/WNF.0b013e31827db49b
Lefort R, Pozueta J, Shelanski M (2012) Cross-linking of cell surface amyloid precursor protein leads to increased beta-amyloid peptide production in hippocampal neurons: implications for Alzheimer’s disease. J Neurosci 32:10674–10685. https://doi.org/10.1523/JNEUROSCI.6473-11.2012
Legleiter J, Czilli DL, Gitter B, DeMattos RB, Holtzman DM, Kowalewski T (2004) Effect of different anti-Abeta antibodies on Abeta fibrillogenesis as assessed by atomic force microscopy. J Mol Biol 335:997–1006. https://doi.org/10.1016/j.jmb.2003.11.019
Leng F, Edison P (2021) Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here? Nat Rev Neurol 17:157–172. https://doi.org/10.1038/s41582-020-00435-y
Li H, Monien BH, Fradinger EA, Urbanc B, Bitan G (2010) Biophysical characterization of Aβ42 C-terminal fragments: inhibitors of Aβ42 neurotoxicity. Biochemistry 49:1259–1267. https://doi.org/10.1021/bi902075h
Li Y, Li Z, Wang X, Yan X, Guo G (2018) D L Sialic acid derivative with CD33 affinity and application thereof CN108676044B, Xiamen Nkd Biotech Co ltd
Li Y, Sun H, Chen Z, Xu H, Bu G, Zheng H (2016) Implications of GABAergic neurotransmission in Alzheimer’s disease. Front Aging Neurosci 8:31. https://doi.org/10.3389/fnagi.2016.00031
Lindsay J, Laurin D, Verreault R, Hébert R, Helliwell B, Hill GB, McDowell I (2002) Risk factors for Alzheimer’s disease: a prospective analysis from the Canadian Study of Health and Aging. Am J Epidemiol 156:445–453. https://doi.org/10.1093/aje/kwf074
Linse S, Scheidt T, Bernfur K, Vendruscolo M, Dobson CM, Cohen SIA, Sileikis E, Lundqvist M, Qian F, O’Malley T, Bussiere T, Weinreb PH, Xu CK, Meisl G, Devenish SRA, Knowles TPJ, Hansson O (2020) Kinetic fingerprints differentiate the mechanisms of action of anti-Abeta antibodies. Nat Struct Mol Biol 27:1125–1133. https://doi.org/10.1038/s41594-020-0505-6
Liu YH, Wang YR, Xiang Y, Zhou HD, Giunta B, Manucat-Tan NB, Tan J, Zhou XF, Wang YJ (2015) Clearance of amyloid-beta in Alzheimer’s disease: shifting the action site from center to periphery. Mol Neurobiol 51:1–7. https://doi.org/10.1007/s12035-014-8694-9
Lomont JP, Rich KL, Maj M, Ho JJ, Ostrander JS, Zanni MT (2018) Spectroscopic signature for stable β-amyloid fibrils versus β-sheet-rich oligomers. J Phys Chem B 122:144–153. https://doi.org/10.1021/acs.jpcb.7b10765
Lu JX, Qiang W, Yau WM, Schwieters CD, Meredith SC, Tycko R (2013) Molecular structure of beta-amyloid fibrils in Alzheimer’s disease brain tissue. Cell 154:1257–1268. https://doi.org/10.1016/j.cell.2013.08.035
Lull ME, Block ML (2010) Microglial activation and chronic neurodegeneration. Neurotherapeutics 7:354–365. https://doi.org/10.1016/j.nurt.2010.05.014
Maakaron JE, Rogosheske J, Long M, Bachanova V, Mims AS (2021) CD33-targeted therapies: beating the disease or beaten to death? J Clin Pharmacol 61:7–17. https://doi.org/10.1002/jcph.1730
Makin S (2018) The amyloid hypothesis on trial. Nature 559:S4–S7. https://doi.org/10.1038/d41586-018-05719-4
Mandal M, Wu Y, Misiaszek J, Li G, Buevich A, Caldwell JP, Liu X, Mazzola RD, Orth P, Strickland C, Voigt J, Wang H, Zhu Z, Chen X, Grzelak M, Hyde LA, Kuvelkar R, Leach PT, Terracina G et al (2016) Structure-based design of an iminoheterocyclic beta-site amyloid precursor protein cleaving enzyme (BACE) inhibitor that lowers central abeta in nonhuman primates. J Med Chem 59:3231–3248. https://doi.org/10.1021/acs.jmedchem.5b01995
Mei X, Atkinson D (2011) Crystal structure of C-terminal truncated apolipoprotein A-I reveals the assembly of high density lipoprotein (HDL) by dimerization. J Biol Chem 286:38570–38582. https://doi.org/10.1074/jbc.M111.260422
Miles LA, Crespi GA, Doughty L, Parker MW (2013) Bapineuzumab captures the N-terminus of the Alzheimer’s disease amyloid-beta peptide in a helical conformation. Sci Rep 3:1302. https://doi.org/10.1038/srep01302
Miles LA, Hermans SJ, Crespi GAN, Gooi JH, Doughty L, Nero TL, Markulic J, Ebneth A, Wroblowski B, Oehlrich D, Trabanco AA, Rives ML, Royaux I, Hancock NC, Parker MW (2019) Small molecule binding to Alzheimer risk factor CD33 promotes Abeta phagocytosis. iScience 19:110–118. https://doi.org/10.1016/j.isci.2019.07.023
Molica M, Perrone S, Mazzone C, Niscola P, Cesini L, Abruzzese E, de Fabritiis P (2021) CD33 expression and gentuzumab ozogamicin in acute myeloid leukemia: two sides of the same coin. Cancers (Basel) 13 https://doi.org/10.3390/cancers13133214
Montoliu-Gaya L, Villegas S (2016) Abeta-immunotherapeutic strategies: a wide range of approaches for Alzheimer’s disease treatment. Expert Rev Mol Med 18:e13. https://doi.org/10.1017/erm.2016.11
Morgan D, Diamond DM, Gottschall PE, Ugen KE, Dickey C, Hardy J, Duff K, Jantzen P, DiCarlo G, Wilcock D, Connor K, Hatcher J, Hope C, Gordon M, Arendash GW (2000) A beta peptide vaccination prevents memory loss in an animal model of Alzheimer’s disease. Nature 408:982–985. https://doi.org/10.1038/35050116
Moulder KL, Snider BJ, Mills SL, Buckles VD, Santacruz AM, Bateman RJ, Morris JC (2013) Dominantly inherited Alzheimer network: facilitating research and clinical trials. Alzheimers Res Ther 5:48. https://doi.org/10.1186/alzrt213
Mullard A (2012) Sting of Alzheimer’s failures offset by upcoming prevention trials. Nat Rev Drug Discov 11:657–660. https://doi.org/10.1038/nrd3842
Myers A, McGonigle P (2019) Overview of transgenic mouse models for Alzheimer’s disease. Curr Protoc Neurosci 89:e81. https://doi.org/10.1002/cpns.81
Naj AC, Jun G, Beecham GW, Wang LS, Vardarajan BN, Buros J, Gallins PJ, Buxbaum JD, Jarvik GP, Crane PK, Larson EB, Bird TD, Boeve BF, Graff-Radford NR, De Jager PL, Evans D, Schneider JA, Carrasquillo MM, Ertekin-Taner N et al (2011) Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet 43:436–441. https://doi.org/10.1038/ng.801
Neumann H, Takahashi K (2007) Essential role of the microglial triggering receptor expressed on myeloid cells-2 (TREM2) for central nervous tissue immune homeostasis. J Neuroimmunol 184:92–99. https://doi.org/10.1016/j.jneuroim.2006.11.032
Nhan HS, Chiang K, Koo EH (2015) The multifaceted nature of amyloid precursor protein and its proteolytic fragments: friends and foes. Acta Neuropathol 129:1–19. https://doi.org/10.1007/s00401-014-1347-2
Nishimoto I, Okamoto T, Matsuura Y, Takahashi S, Okamoto T, Murayama Y, Ogata E (1993) Alzheimer amyloid protein precursor complexes with brain GTP-binding protein G(o). Nature 362:75–79. https://doi.org/10.1038/362075a0
Ohsawa I, Takamura C, Kohsaka S (2001) Fibulin-1 binds the amino-terminal head of beta-amyloid precursor protein and modulates its physiological function. J Neurochem 76:1411–1420. https://doi.org/10.1046/j.1471-4159.2001.00144.x
Okamoto T, Takeda S, Giambarella U, Murayama Y, Matsui T, Katada T, Matsuura Y, Nishimoto I (1996) Intrinsic signaling function of APP as a novel target of three V642 mutations linked to familial Alzheimer’s disease. EMBO J 15:3769–3777
Orr SJ, Morgan NM, Elliott J, Burrows JF, Scott CJ, McVicar DW, Johnston JA (2007) CD33 responses are blocked by SOCS3 through accelerated proteasomal-mediated turnover. Blood 109:1061–1068. https://doi.org/10.1182/blood-2006-05-023556
Paradowska-Gorycka A, Jurkowska M (2013) Structure, expression pattern and biological activity of molecular complex TREM-2/DAP12. Hum Immunol 74:730–737. https://doi.org/10.1016/j.humimm.2013.02.003
Paravastu AK, Leapman RD, Yau WM, Tycko R (2008) Molecular structural basis for polymorphism in Alzheimer’s beta-amyloid fibrils. Proc Natl Acad Sci U S A 105:18349–18354. https://doi.org/10.1073/pnas.0806270105
Parihar MS, Brewer GJ (2010) Amyloid-beta as a modulator of synaptic plasticity. J Alzheimers Dis 22:741–763. https://doi.org/10.3233/JAD-2010-101020
Park S, Pascua E, Lindquist KC, Kimberlin C, Deng X, Mak YSL, Melton Z, Johnson TO, Lin R, Boldajipour B, Abraham RT, Pons J, Sasu BJ, Van Blarcom TJ, Chaparro-Riggers J (2021) Direct control of CAR T cells through small molecule-regulated antibodies. Nat Commun 12:710. https://doi.org/10.1038/s41467-020-20671-6
Pasternak SH, Bagshaw RD, Guiral M, Zhang S, Ackerley CA, Pak BJ, Callahan JW, Mahuran DJ (2003) Presenilin-1, nicastrin, amyloid precursor protein, and gamma-secretase activity are co-localized in the lysosomal membrane. J Biol Chem 278:26687–26694. https://doi.org/10.1074/jbc.m304009200
Paul SP, Taylor LS, Stansbury EK, McVicar DW (2000) Myeloid specific human CD33 is an inhibitory receptor with differential ITIM function in recruiting the phosphatases SHP-1 and SHP-2. Blood 96:483–490
Petkova AT, Buntkowsky G, Dyda F, Leapman RD, Yau WM, Tycko R (2004) Solid state NMR reveals a pH-dependent antiparallel beta-sheet registry in fibrils formed by a beta-amyloid peptide. J Mol Biol 335:247–260. https://doi.org/10.1016/j.jmb.2003.10.044
Petros AM, Korepanova A, Jakob CG, Qiu W, Panchal SC, Wang J, Dietrich JD, Brewer JT, Pohlki F, Kling A, Wilcox K, Lakics V, Bahnassawy L, Reinhardt P, Partha SK, Bodelle PM, Lake M, Charych EI, Stoll VS et al (2019) Fragment-based discovery of an apolipoprotein E4 (apoE4) stabilizer. J Med Chem 62:4120–4130. https://doi.org/10.1021/acs.jmedchem.9b00178
Piccio L, Deming Y, Del-Aguila JL, Ghezzi L, Holtzman DM, Fagan AM, Fenoglio C, Galimberti D, Borroni B, Cruchaga C (2016) Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status. Acta Neuropathol 131:925–933. https://doi.org/10.1007/s00401-016-1533-5
Qiu T, Liu Q, Chen YX, Zhao YF, Li YM (2015) Aβ42 and Aβ40: similarities and differences. J Pept Sci 21:522–529. https://doi.org/10.1002/psc.2789
Radzimanowski J, Simon B, Sattler M, Beyreuther K, Sinning I, Wild K (2008) Structure of the intracellular domain of the amyloid precursor protein in complex with Fe65-PTB2. EMBO Rep 9:1134–1140. https://doi.org/10.1038/embor.2008.188
Rapoport M, Dawson HN, Binder LI, Vitek MP, Ferreira A (2002) Tau is essential to β-amyloid-induced neurotoxicity. Proc Natl Acad Sci USA 9:6364–6369. https://doi.org/10.1073/pnas.092136199
Reeve A, Simcox E, Turnbull D (2014) Ageing and Parkinson’s disease: why is advancing age the biggest risk factor? Ageing Res Rev 14:19–30. https://doi.org/10.1016/j.arr.2014.01.004
Reinhard C, Borgers M, David G, De Strooper B (2013) Soluble amyloid-beta precursor protein binds its cell surface receptor in a cooperative fashion with glypican and syndecan proteoglycans. J Cell Sci 126:4856–4861. https://doi.org/10.1242/jcs.137919
Renno T, Krakowski M, Piccirillo C, Lin JY, Owens T (1995) TNF-alpha expression by resident microglia and infiltrating leukocytes in the central nervous system of mice with experimental allergic encephalomyelitis. Regulation by Th1 cytokines. J Immunol 154:944–953
Rossjohn J, Cappai R, Feil SC, Henry A, McKinstry WJ, Galatis D, Hesse L, Multhaup G, Beyreuther K, Masters CL, Parker MW (1999) Crystal structure of the N-terminal, growth factor-like domain of Alzheimer amyloid precursor protein. Nat Struct Biol 6:327–331. https://doi.org/10.1038/7562
Sabbath KD, Ball ED, Larcom P, Davis RB, Griffin JD (1985) Heterogeneity of clonogenic cells in acute myeloblastic leukemia. J Clin Invest 75:746–753. https://doi.org/10.1172/JCI111756
Sánchez L, Madurga S, Pukala T, Vilaseca M, López-Iglesias C, Robinson CV, Giralt E, Carulla N (2011) Aβ40 and Aβ42 amyloid fibrils exhibit distinct molecular recycling properties. J Am Chem Soc 133:6505–6508. https://doi.org/10.1021/ja1117123
Schenk D, Barbour R, Dunn W, Gordon G, Grajeda H, Guido T, Hu K, Huang J, Johnson-Wood K, Khan K, Kholodenko D, Lee M, Liao Z, Lieberburg I, Motter R, Mutter L, Soriano F, Shopp G, Vasquez N et al (1999) Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature 400:173–177. https://doi.org/10.1038/22124
Scheuermann S, Hambsch B, Hesse L, Stumm J, Schmidt C, Beher D, Bayer TA, Beyreuther K, Multhaup G (2001) Homodimerization of amyloid precursor protein and its implication in the amyloidogenic pathway of Alzheimer’s disease. J Biol Chem 276:33923–33929. https://doi.org/10.1074/jbc.M105410200
Schlepckow K, Monroe KM, Kleinberger G, Cantuti-Castelvetri L, Parhizkar S, Xia D, Willem M, Werner G, Pettkus N, Brunner B, Sulzen A, Nuscher B, Hampel H, Xiang X, Feederle R, Tahirovic S, Park JI, Prorok R, Mahon C et al (2020) Enhancing protective microglial activities with a dual function TREM2 antibody to the stalk region. EMBO Mol Med 12:e11227. https://doi.org/10.15252/emmm.201911227
Schoch KM, Ezerskiy LA, Morhaus MM, Bannon RN, Sauerbeck AD, Shabsovich M, Jafar-Nejad P, Rigo F, Miller TM (2021) Acute Trem2 reduction triggers increased microglial phagocytosis, slowing amyloid deposition in mice. Proc Natl Acad Sci U S A 118 https://doi.org/10.1073/pnas.2100356118
Schroeter S, Khan K, Barbour R, Doan M, Chen M, Guido T, Gill D, Basi G, Schenk D, Seubert P, Games D (2008) Immunotherapy reduces vascular amyloid-beta in PDAPP mice. J Neurosci 28:6787–6793. https://doi.org/10.1523/JNEUROSCI.2377-07.2008
Schubert W, Prior R, Weidemann A, Dircksen H, Multhaup G, Masters CL, Beyreuther K (1991) Localization of Alzheimer beta A4 amyloid precursor protein at central and peripheral synaptic sites. Brain Res 563:184–194. https://doi.org/10.1016/0006-8993(91)91532-6
Seegar TCM, Killingsworth LB, Saha N, Meyer PA, Patra D, Zimmerman B, Janes PW, Rubinstein E, Nikolov DB, Skiniotis G, Kruse AC, Blacklow SC (2017) Structural basis for regulated proteolysis by the alpha-secretase ADAM10. Cell 171(e1637):1638–1648. https://doi.org/10.1016/j.cell.2017.11.014
Selkoe DJ, Hardy J (2016) The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med 8:595–608. https://doi.org/10.15252/emmm.201606210
Sevigny J, Chiao P, Bussiere T, Weinreb PH, Williams L, Maier M, Dunstan R, Salloway S, Chen T, Ling Y, O’Gorman J, Qian F, Arastu M, Li M, Chollate S, Brennan MS, Quintero-Monzon O, Scannevin RH, Arnold HM et al (2016) The antibody aducanumab reduces Abeta plaques in Alzheimer’s disease. Nature 537:50–56. https://doi.org/10.1038/nature19323
Sgroi D, Nocks A, Stamenkovic I (1996) A single N-linked glycosylation site is implicated in the regulation of ligand recognition by the I-type lectins CD22 and CD33. J Biol Chem 271:18803–18809. https://doi.org/10.1074/jbc.271.31.18803
Siddiqui S, Schwarz F, Springer S, Khedri Z, Yu H, Deng L, Verhagen A, Naito-Matsui Y, Jiang W, Kim D, Zhou J, Ding B, Chen X, Varki N, Varki A (2017) Studies on the detection, expression, glycosylation, dimerization, and ligand binding properties of mouse siglec-E. J Biol Chem 292:1029–1037. https://doi.org/10.1074/jbc.M116.738351
Sims R, van der Lee SJ, Naj AC, Bellenguez C, Badarinarayan N, Jakobsdottir J, Kunkle BW, Boland A, Raybould R, Bis JC, Martin ER, Grenier-Boley B, Heilmann-Heimbach S, Chouraki V, Kuzma AB, Sleegers K, Vronskaya M, Ruiz A, Graham RR et al (2017) Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer’s disease. Nat Genet 49:1373–1384. https://doi.org/10.1038/ng.3916
Small DH, Nurcombe V, Reed G, Clarris H, Moir R, Beyreuther K, Masters CL (1994) A heparin-binding domain in the amyloid protein precursor of Alzheimer’s disease is involved in the regulation of neurite outgrowth. J Neurosci 14:2117–2127
Solomon B, Koppel R, Frankel D, Hanan-Aharon E (1997) Disaggregation of Alzheimer beta-amyloid by site-directed mAb. Proc Natl Acad Sci U S A 94:4109–4112. https://doi.org/10.1073/pnas.94.8.4109
Solomon B, Koppel R, Hanan E, Katzav T (1996) Monoclonal antibodies inhibit in vitro fibrillar aggregation of the Alzheimer beta-amyloid peptide. Proc Natl Acad Sci U S A 93:452–455. https://doi.org/10.1073/pnas.93.1.452
Song MS, Saavedra L, de Chaves EI (2006) Apoptosis is secondary to non-apoptotic axonal degeneration in neurons exposed to Abeta in distal axons. Neurobiol Aging 27:1224–1238. https://doi.org/10.1016/j.neurobiolaging.2005.06.007
Song W, Hooli B, Mullin K, Jin SC, Cella M, Ulland TK, Wang Y, Tanzi RE, Colonna M (2017) Alzheimer’s disease-associated TREM2 variants exhibit either decreased or increased ligand-dependent activation. Alzheimers Dement 13:381–387. https://doi.org/10.1016/j.jalz.2016.07.004
Spoerri L, Vella LJ, Pham CL, Barnham KJ, Cappai R (2012) The amyloid precursor protein copper binding domain histidine residues 149 and 151 mediate APP stability and metabolism. J Biol Chem 287:26840–26853. https://doi.org/10.1074/jbc.M112.355743
Steiner A, Schlepckow K, Brunner B, Steiner H, Haass C, Hagn F (2020) gamma-Secretase cleavage of the Alzheimer risk factor TREM2 is determined by its intrinsic structural dynamics. EMBO J 39:e104247. https://doi.org/10.15252/embj.2019104247
Suarez-Calvet M, Araque Caballero MA, Kleinberger G, Bateman RJ, Fagan AM, Morris JC, Levin J, Danek A, Ewers M, Haass C, Dominantly Inherited Alzheimer N (2016) Early changes in CSF sTREM2 in dominantly inherited Alzheimer’s disease occur after amyloid deposition and neuronal injury. Sci Transl Med:8, 369ra178. https://doi.org/10.1126/scitranslmed.aag1767
Subramaniam SR, Federoff HJ (2017) Targeting microglial activation states as a therapeutic avenue in Parkinson’s disease. Front Aging Neurosci 9:176. https://doi.org/10.3389/fnagi.2017.00176
Sudom A, Talreja S, Danao J, Bragg E, Kegel R, Min X, Richardson J, Zhang Z, Sharkov N, Marcora E, Thibault S, Bradley J, Wood S, Lim AC, Chen H, Wang S, Foltz IN, Sambashivan S, Wang Z (2018) Molecular basis for the loss-of-function effects of the Alzheimer’s disease-associated R47H variant of the immune receptor TREM2. J Biol Chem 293:12634–12646. https://doi.org/10.1074/jbc.RA118.002352
Szykowska A, Chen Y, Smith TB, Preger C, Yang J, Qian D, Mukhopadhyay SM, Wigren E, Neame SJ, Graslund S, Persson H, Atkinson PJ, Di Daniel E, Mead E, Wang J, Davis JB, Burgess-Brown NA, Bullock AN (2021) Selection and structural characterization of anti-TREM2 scFvs that reduce levels of shed ectodomain. Structure. https://doi.org/10.1016/j.str.2021.06.010
Takahashi K, Rochford CD, Neumann H (2005) Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. J Exp Med 201:647–657. https://doi.org/10.1084/jem.20041611
Taylor VC, Buckley CD, Douglas M, Cody AJ, Simmons DL, Freeman SD (1999) The myeloid-specific sialic acid-binding receptor, CD33, associates with the protein-tyrosine phosphatases, SHP-1 and SHP-2. J Biol Chem 274:11505–11512. https://doi.org/10.1074/jbc.274.17.11505
Tew DJ, Bottomley SP, Smith DP, Ciccotosto GD, Babon J, Hinds MG, Masters CL, Cappai R, Barnham KJ (2008) Stabilization of neurotoxic soluble beta-sheet-rich conformations of the Alzheimer’s disease amyloid-beta peptide. Biophys J 94(7):2752–2766. https://doi.org/10.1529/biophysj.107.119909
Tolar M, Hey J, Power A, Abushakra S (2021) Neurotoxic soluble amyloid oligomers drive Alzheimer’s pathogenesis and represent a clinically validated target for slowing disease progression. Int J Mol Sci 22. https://doi.org/10.3390/ijms22126355
Tycko R (2006) Molecular structure of amyloid fibrils: insights from solid-state NMR. Q Rev Biophys 39:1–55. https://doi.org/10.1017/S0033583506004173
Ultsch M, Li B, Maurer T, Mathieu M, Adolfsson O, Muhs A, Pfeifer A, Pihlgren M, Bainbridge TW, Reichelt M, Ernst JA, Eigenbrot C, Fuh G, Atwal JK, Watts RJ, Wang W (2016) Structure of crenezumab complex with Abeta shows loss of beta-hairpin. Sci Rep 6:39374. https://doi.org/10.1038/srep39374
Ulyanova T, Blasioli J, Woodford-Thomas TA, Thomas ML (1999) The sialoadhesin CD33 is a myeloid-specific inhibitory receptor. Eur J Immunol 29:3440–3449. https://doi.org/10.1002/(SICI)1521-4141(199911)29:11,<3440::AID-IMMU3440>3.0.CO;2-C
van Dyck CH (2018) Anti-amyloid-beta monoclonal antibodies for Alzheimer’s disease: pitfalls and promise. Biol Psychiatry 83:311–319. https://doi.org/10.1016/j.biopsych.2017.08.010
Varadarajan S, Yatin S, Aksenova M, Butterfield DA (2000) Review: Alzheimer’s amyloid beta-peptide-associated free radical oxidative stress and neurotoxicity. J Struct Biol 130:184–208. https://doi.org/10.1006/jsbi.2000.4274
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, Szoeke C, Macaulay SL, Martins R, Maruff P, Ames D, Rowe CC, Masters CL, Australian Imaging B, Lifestyle Research G (2013) Amyloid beta deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol 12:357–367. https://doi.org/10.1016/S1474-4422(13)70044-9
Vivekanandan S, Brender JR, Lee SY, Ramamoorthy A (2011) A partially folded structure of amyloid-beta(1-40) in an aqueous environment. Biochem Biophys Res Commun 411:312–316. https://doi.org/10.1016/j.bbrc.2011.06.133
von Bernhardi R, Eugenin-von Bernhardi L, Eugenin J (2015) Microglial cell dysregulation in brain aging and neurodegeneration. Front Aging Neurosci 7:124. https://doi.org/10.3389/fnagi.2015.00124
Walsh DM, Klyubin I, Fadeeva JV, Cullen WK, Anwyl R, Wolfe MS, Rowan MJ, Selkoe DJ (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 416:535–539. https://doi.org/10.1038/416535a
Walsh DM, Selkoe DJ (2007) A beta oligomers - a decade of discovery. J Neurochem 101:1172–1184. https://doi.org/10.1111/j.1471-4159.2006.04426.x
Walter RB (2018) Investigational CD33-targeted therapeutics for acute myeloid leukemia. Expert Opin Investig Drugs 27:339–348. https://doi.org/10.1080/13543784.2018.1452911
Walter RB, Hausermann P, Raden BW, Teckchandani AM, Kamikura DM, Bernstein ID, Cooper JA (2008a) Phosphorylated ITIMs enable ubiquitylation of an inhibitory cell surface receptor. Traffic 9:267–279. https://doi.org/10.1111/j.1600-0854.2007.00682.x
Walter RB, Raden BW, Kamikura DM, Cooper JA, Bernstein ID (2005) Influence of CD33 expression levels and ITIM-dependent internalization on gemtuzumab ozogamicin-induced cytotoxicity. Blood 105:1295–1302. https://doi.org/10.1182/blood-2004-07-2784
Walter RB, Raden BW, Zeng R, Hausermann P, Bernstein ID, Cooper JA (2008b) ITIM-dependent endocytosis of CD33-related Siglecs: role of intracellular domain, tyrosine phosphorylation, and the tyrosine phosphatases, Shp1 and Shp2. J Leukoc Biol 83:200–211. https://doi.org/10.1189/jlb.0607388
Wang Y, Ha Y (2004) The X-ray structure of an antiparallel dimer of the human amyloid precursor protein E2 domain. Mol Cell 15:343–353. https://doi.org/10.1016/j.molcel.2004.06.037
Watanabe T, Sukegawa J, Sukegawa I, Tomita S, Iijima K, Oguchi S, Suzuki T, Nairn AC, Greengard P (1999) A 127-kDa protein (UV-DDB) binds to the cytoplasmic domain of the Alzheimer’s amyloid precursor protein. J Neurochem 72:549–556. https://doi.org/10.1046/j.1471-4159.1999.0720549.x
Weidemann A, Konig G, Bunke D, Fischer P, Salbaum JM, Masters CL, Beyreuther K (1989) Identification, biogenesis, and localization of precursors of Alzheimer’s disease A4 amyloid protein. Cell 57:115–126. https://doi.org/10.1016/0092-8674(89)90177-3
Wernette-Hammond ME, Lauer SJ, Corsini A, Walker D, Taylor JM, Rall SC Jr (1989) Glycosylation of human apolipoprotein E. The carbohydrate attachment site is threonine 194. J Biol Chem 264:9094–9101
Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, Morgan D (2004a) Microglial activation facilitates Abeta plaque removal following intracranial anti-Abeta antibody administration. Neurobiol Dis 15:11–20. https://doi.org/10.1016/j.nbd.2003.09.015
Wilcock DM, Rojiani A, Rosenthal A, Levkowitz G, Subbarao S, Alamed J, Wilson D, Wilson N, Freeman MJ, Gordon MN, Morgan D (2004b) Passive amyloid immunotherapy clears amyloid and transiently activates microglia in a transgenic mouse model of amyloid deposition. J Neurosci 24:6144–6151. https://doi.org/10.1523/JNEUROSCI.1090-04.2004
Wunderlich P, Glebov K, Kemmerling N, Tien NT, Neumann H, Walter J (2013) Sequential proteolytic processing of the triggering receptor expressed on myeloid cells-2 (TREM2) protein by ectodomain shedding and gamma-secretase-dependent intramembranous cleavage. J Biol Chem 288:33027–33036. https://doi.org/10.1074/jbc.M113.517540
Yang G, Zhou R, Zhou Q, Guo X, Yan C, Ke M, Lei J, Shi Y (2019) Structural basis of Notch recognition by human gamma-secretase. Nature 565:192–197. https://doi.org/10.1038/s41586-018-0813-8
Yankner BA, Duffy LK, Kirschner DA (1990) Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides. Science 250:279–282. https://doi.org/10.1126/science.2218531
Yeh FL, Wang Y, Tom I, Gonzalez LC, Sheng M (2016) TREM2 binds to apolipoproteins, including APOE and CLU/APOJ, and thereby facilitates uptake of amyloid-beta by microglia. Neuron 91:328–340. https://doi.org/10.1016/j.neuron.2016.06.015
Yu L, Edalji R, Harlan JE, Holzman TF, Lopez AP, Labkovsky B, Hillen H, Barghorn S, Ebert U, Richardson PL, Miesbauer L, Solomon L, Bartley D, Walter K, Johnson RW, Hajduk PJ, Olejniczak ET (2009) Structural characterization of a soluble amyloid beta-peptide oligomer. Biochemistry 48:1870–1877. https://doi.org/10.1021/bi802046n
Yuan P, Condello C, Keene CD, Wang Y, Bird TD, Paul SM, Luo W, Colonna M, Baddeley D, Grutzendler J (2016) TREM2 haplodeficiency in mice and humans impairs the microglia barrier function leading to decreased amyloid compaction and severe axonal dystrophy. Neuron 90:724–739. https://doi.org/10.1016/j.neuron.2016.05.003
Zago W, Buttini M, Comery TA, Nishioka C, Gardai SJ, Seubert P, Games D, Bard F, Schenk D, Kinney GG (2012) Neutralization of soluble, synaptotoxic amyloid beta species by antibodies is epitope specific. J Neurosci 32:2696–2702. https://doi.org/10.1523/JNEUROSCI.1676-11.2012
Zhang S, Iwata K, Lachenmann MJ, Peng JW, Li S, Stimson ER, Lu Y, Felix AM, Maggio JE, Lee JP (2000) The Alzheimer’s peptide a beta adopts a collapsed coil structure in water. J Struct Biol 130:130–141. https://doi.org/10.1006/jsbi.2000.4288
Zhang Y, Lee DH (2011) Sink hypothesis and therapeutic strategies for attenuating Abeta levels. Neuroscientist 17:163–173. https://doi.org/10.1177/1073858410381532
Zhang Z, Lee CH, Mandiyan V, Borg JP, Margolis B, Schlessinger J, Kuriyan J (1997) Sequence-specific recognition of the internalization motif of the Alzheimer’s amyloid precursor protein by the X11 PTB domain. EMBO J 16:6141–6150. https://doi.org/10.1093/emboj/16.20.6141
Zhao Y, Wu X, Li X, Jiang LL, Gui X, Liu Y, Sun Y, Zhu B, Pina-Crespo JC, Zhang M, Zhang N, Chen X, Bu G, An Z, Huang TY, Xu H (2018) TREM2 is a receptor for beta-amyloid that mediates microglial function. Neuron 97(e1027):1023–1031. https://doi.org/10.1016/j.neuron.2018.01.031
Zhou R, Yang G, Guo X, Zhou Q, Lei J, Shi Y (2019) Recognition of the amyloid precursor protein by human gamma-secretase. Science 363. https://doi.org/10.1126/science.aaw0930
Acknowledgements
We thank all past and present members of our laboratory, and our collaborators, for their contributions to some of the studies described in this review. This work was supported by the National Health and Medical Research Council of Australia (NHMRC) Project (APP981170, APP156701, APP296201, APP1021935, APP1103026), Research Fellowship (APP1021645, APP1117183) and Investigator (APP1194263) grants, the Alzheimer’s Drug Discovery Foundation, the Angior Family Foundation, Bethlehem Griffiths Research Foundation, the L.E.W. Carty Charitable Fund, the Mason Foundation, the National Foundation for Medical Research and Innovation, and the Yulgilbar Foundation. Infrastructure support from the NHMRC Independent Research Institutes Infrastructure Support Scheme and the Victorian State Government Operational Infrastructure Support Program to St. Vincent’s Institute is gratefully acknowledged. M.W.P. is an NHMRC Leadership Fellow.
Funding
This study was financially supported by the National Health and Medical Research Council (NHMRC) of Australia Investigator Grant (APP1194263, 2021–2025) and the National Foundation for Medical Research and Innovation Research Grant (2021–2022).
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
We have a collaboration and license agreement with Janssen Pharmaceuticals on some of our microglia work. Dr Chen Gao is now an employee of Wren Therapeutics Ltd.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Stefan J. Hermans, Tracy L. Nero, Craig J. Morton, and Jonathan H. Gooi are joint first authors.
Rights and permissions
About this article
Cite this article
Hermans, S.J., Nero, T.L., Morton, C.J. et al. Structural biology of cell surface receptors implicated in Alzheimer’s disease. Biophys Rev 14, 233–255 (2022). https://doi.org/10.1007/s12551-021-00903-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12551-021-00903-9