Abstract
Apolipoprotein E (apoE) is a 34-kDa glycoprotein that is secreted from many cells throughout the body. ApoE is best known for its role in lipoprotein metabolism. Recent studies underline the association of circulating lipoprotein-associated apoE levels and the development for cardiovascular disease (CVD). Besides its well-established role in pathology of CVD, it is also implicated in neurodegenerative diseases and recent new data on adipose-produced apoE point to a novel metabolic role for apoE in obesity. The regulation of apoE production and secretion is remarkably cell and tissue specific. Here, we summarize recent insights into the differential regulation apoE production and secretion by hepatocytes, monocytes/macrophages, adipocytes, and the central nervous system and relevant variations in apoE biochemistry and function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
apoE is a multifunctional protein
ApoE is best known for its role in lipid metabolism, regulating production, conversion, as well as clearance of lipoproteins (Fig. 1). In the liver, apoE associates with very low-density lipoprotein (VLDL) during its assembly. VLDL and other lipoproteins may also acquire apoE via exchange with other lipoproteins. As a component of lipoproteins, apoE mediates uptake of chylomicrons, VLDL remnants, and apoE-containing high-density lipoprotein (HDL) via the low-density lipoprotein receptor (LDLr), LDLr-related protein 1 (LRP1), and heparin sulfate proteoglycans (HSPGs) into the liver. In the periphery, apoE in VLDL also mediates binding to the VLDL receptor present on muscle, heart, and adipose tissue delivering triglycerides for energy or storage. Other roles include the following: (1) displacement of apoCII from triglyceride-rich lipoproteins, leading to inhibited lipolysis and conversion; and (2) stimulation of reverse cholesterol transport, whereby cholesterol from peripheral tissues is transported via HDL to the liver for excretion (for review, see [1]). Recently, a strong association of VLDL-associated apolipoproteins, including apoE, with incident CVD was identified, underlining the importance of apoE in CVD [2].
Contribution of different tissues to plasma apoE and its role in lipid and lipoprotein metabolism. Hepatic-produced apoE associates with VLDL intracellularly and regulates VLDL production (1). Intestinal-produced chylomicrons (chylo) acquire apoE by exchange with other lipoproteins (2). apoE mediates the hepatic uptake of lipoproteins by binding to lipoprotein receptors LDLr, LRP1, and/or HSPGs, with uptake via the LRP1 receptor being dependent on local hepatocyte-secreted apoE (3). Lipoprotein-contained apoE inhibits lipolysis by displacing apoCII (4). Adipose-produced apoE associates with VLDL, but not with HDL. It is unknown whether it associates with chylos (5). Adipose apoE regulates uptake of lipids from triglyceride-rich lipoproteins (TLR) including VLDL, IDL, and remnants (6). Hepatic and macrophage apoE contributes to the formation of HDL and HDL uptake into the liver via the LDLr (7)
Local tissue-secreted apoE also has important biological and pathological functions. Macrophage-specific expression of apoE can inhibit atherosclerosis without affecting plasma lipid levels [3]. ApoE has anti-inflammatory, anti-proliferative, immune-modulatory properties which may contribute to its anti-atherogenic effect [4,5,6]. ApoE regulates adipose differentiation, adipocyte cell size, adipose tissue expansion, and triglyceride accumulation [7]. Adipose tissue-derived apoE plays a clear role in diet-induced obesity, affecting insulin sensitivity and mediating adipose tissue inflammation in mice [8, 9], but unlike macrophage-derived apoE, does not appear to be anti-atherogenic. In the central nervous system, apoE is the main apolipoprotein responsible for lipid transport. Secreted predominantly by astrocytes, lipidated apoE delivers cholesterol and phospholipids to neurons and is crucial in maintaining brain integrity and homeostasis. Studies using the apoE knockout mouse indicated an important role of apoE in restoring neuronal function after injury [10]. These tissue-specific functions of apoE are underpinned by cell-specific regulation of production and secretion.
Regulation of apoE transcription
ApoE transcription is tissue-, differentiation-, and cell-specific and can be induced by many different factors such as cytokines, hormones, or lipids. Transcription is controlled by the proximal promoter, by proximal/distal enhancer elements, and through epigenetic control.
The proximal promoter contains binding sites for common transcription factors [11,12,13,14,15,16,17] (Fig. 2). However, the activation of the proximal promoter is insufficient for expression of apoE in most cell types. Hepatocytes, adipocytes, astrocytes, and macrophages all require specific enhancer elements to induce promoter activity [18]. Three proximal enhancer elements, upstream regulatory elements (URE) 1, 2, and 3, one intron regulatory element (IRE1), several distal enhancer elements, multi enhancers (ME) 1 and 2, and hepatocyte regulatory elements (HRC) 1 and 2 have been identified [19,20,21,22]. Tissue/cell specificity is driven predominantly by the distal enhancers, with HRC.1 and HRC.2 inducing gene expression in hepatocytes, and ME.1 and ME.2 being necessary for expression in macrophages, adipocytes, and astrocytes. Within these enhancers, binding sites for specific transcription factors are localized (Fig. 2) and explain why certain triggers modulate apoE expression in some tissues but not others [23, 24]. Cell-specific transcription can also be modulated through interaction with repressors [25, 26]. For example, a recent study found that after glucocorticoids bind a glucocorticoid element in the apoE promoter, negative regulators suppressed transcription in the hepatocyte but not in macrophages [26]. Interestingly, glucocorticoids raise apoE plasma levels without affecting hepatic apoE mRNA levels indicating further regulation at the level of protein formation and/or secretion.
Tissue-/cell-specific control of apoE transcription. Proximal and distal transcription factor binding sites and enhancer elements regulating apoE transcription in macrophages, hepatocytes, adipocytes, and astrocytes are shown. CpGI, CpG island involved in epigenetic control; ME.1-2, multi enhancers 1 and 2, driving expression in macrophages, adipocytes, and astrocytes. NF-κB, nuclear factor-κB; PPAR, peroxisome proliferator-activated receptor; RXR, retinoid X receptor; STAT, signal transducer and activator of transcription; LXR, liver X receptor; HRC, hepatocyte regulatory element; ME, multi enhancer; TR, thyroid hormone receptor; URE, upstream regulatory element; SP, specificity protein; Zic, zinc finger of the cerebellum; AP, activating protein; GR, glucocorticoid receptor; USF, upstream stimulatory factor; BEF, BK virus enhancer factor
Neurons demonstrate a unique way of controlling apoE expression. Retention of intron-3 gives rise to an apoE splice variant (apoE-I3) that is not translated into protein. After injury, astrocyte-secreted factor(s) induce processing of apoE-I3 to generate normal apoE mRNA that is translated into protein [27]. Whether cells outside the CNS use similar control of apoE production has not been investigated.
Several studies suggest a role for epigenetic control of apoE expression especially via DNA methylation. Thirteen CpG sites have been identified in the apoE promotor, exons, and introns. Methylation generally is associated with reduced expression and differences in methylation patterns have been observed between tissues, regions within tissues, and after exposure to environmental factors such as cadmium [28]. Less well studied are sense/antisense and miRNA regulation of apoE [29, 30]. Three potential sense and one antisense mRNA transcript were identified in mice and humans [29]. It is unclear whether these are translated into protein or have a physiological function. The 40-kDa apoE product in mouse serum corresponding to the predicted size of one of the antisense transcripts described by Seitz et al. [29] is most likely a glycosylated apoE glycoform rather than the suggested alternative transcript (see Role of apoE glycosylation and sialylation section and Fig. 3).
PNGaseF treatment of mouse, rat, rabbit, and human apoE. 0.5 μl of plasma was incubated with 500 U PNGaseF and incubated at 37 °C for 16 h. apoE glycosylation was analyzed by Western blotting. Note disappearance of higher molecular weight apoE in mouse, but not in rat, rabbit, and human plasma indicating N-linked glycan attachment in mouse apoE only. Glycosylated apoE in mouse is 9.4% (8.7–10.1%) of total apoE before PNGaseF and not visible after PNGaseF treatment (*p < 0.05). Graph shown is mean ± range of two independent experiments and blot shown is representative of one of these experiments
In summary, apoE transcription involves an intricate network of many interacting regulatory elements, which regulate apoE expression to different biological requirements and stimuli in a cell-specific manner. Understanding the detail of apoE transcription will enable cell-specific modulation of apoE production.
Post-translational control of apoE
ApoE follows the classical secretory pathway, in which synthesis in the ER is followed by movement through the Golgi and trans-Golgi network, during which apoE is glycosylated and sialylated. From the Golgi, apoE is transported in tubular vesicular compartments along the microtubule network to the plasma membrane and secreted [31]. A proportion of secreted apoE can be found bound to the cell surface, particularly in association with HSPGs [32, 33]. Cell surface pools can be re-internalized and subsequently be degraded, or alternatively be transported to the Golgi network for further modification or re-release into the extracellular medium via recycling endosomes.
Although constitutively secreted from most cells, secretion can be stimulated by extracellular triggers and apoE secretion demonstrates aspects of typical regulated secretion. In macrophages, apoE is synthesized in excess of cellular requirements with a large proportion directed for degradation after leaving the Golgi. Exposure to stimuli, such as apolipoprotein A-I (apoA-I) or HDL, can lead to redirection of apoE from this degradational pathway into the secretory pathway resulting in a rapid increase in secretion [34, 35].
We previously showed that constitutive secretion from human macrophages is regulated by protein kinase A (PKA), phospholipase C (PLC), and intracellular calcium [31]. Further studies identified a role for protein phosphatase 2B (PP2B/calcineurin) and protein kinase C (PKC) and its effector myristolated alanine-rich C-kinase substrate MARCKS [36, 37]. Recently, dynamin II, a fission protein that regulates exocytic and endocytic membrane events, was also identified as a regulator of apoE secretion [38]. PKC/MARCKS plays an important role in brain development, cellular migration, Aβ formation, neutrophil degranulation, and mucin secretion. It is possible, but currently unknown, if PKC/MARCKS acts through regulation of apoE secretion in brain or adipose tissue. PP2B is the target by which immunosuppressants exert their inhibition of T cell function [39]. Therefore, one of the main side effects of long-term treatment with these drugs is an increased risk of cardiovascular disease, which may involve inhibition of macrophage apoE secretion.
There seems to be some specificity in the pathways that regulate apoE secretion in different cell types. For example, cytokines do not affect apoE secretion in hepatoma cells [40] and although PKA and dynamin regulate apoE secretion in HepG2 cells, these cells were less sensitive to PP2B inhibition than were macrophages [37].
In the central nervous system, secretion of apoE by neurons is also calcium- and microtubule-dependent [41]. Recently, binding of apoE to the cadherin, alcadein beta, was reported in neurons [42]. Being a docking receptor for kinesin-1, alcadeins can mediate traffic of vesicular cargo along the microtubule network. Through alcadein binding, apoE affected transport and processing of amyloid β-protein precursor indicating that apoE can modulate vesicle transport of other proteins and possibly of itself by binding to cadherins.
A recent a high-throughput screen identified various compounds that enhance apoE secretion in primary human astrocytes via novel mechanisms [43]. Although the exact pathway by which apoE secretion was affected were not identified, the pathway was independent of LXR-ABCA1 activation, a common apoE-enhancing pathway in astrocytes. Importantly, some compounds failed to induce apoE secretion in the astrocytoma cell line CCF-STTG1, pointing to the need to verify findings in different cell model systems, especially primary cells.
The mechanisms regulating apoE secretion from adipocytes and hepatocytes have not been extensively studied. apoE is colocalized with caveolin in adipocytes and astrocytes [44], targeting apoE to the plasma membrane [45], although the functional significance is not known.
Role of apoE glycosylation and sialylation
ApoE is post-translationally glycosylated. For human, apoE is exclusively O-linked, either via serine or threonine residues and may be capped with sialic acid, a negatively charged carbohydrate frequently involved in mediating the interactions with various receptors, ligands, and cofactors.
The extent of human apoE glycosylation and sialylation is heterogeneous, reflecting not only its tissue/cell type origin, but also its extracellular environment. A high proportion of apoE secreted from hepatocytes is glycosylated and sialylated, yet plasma apoE is largely devoid of carbohydrates [46], suggesting these sugars are partially removed in the circulation by unknown glycosidases [47]. In contrast, apoE in cerebrospinal fluid remains extensively glycosylated and sialylated, closely reflecting the form secreted from astrocytes [48, 49]. Similar contrasts in the degree of apoE glycosylation exist in other mammalian species. For example, all apoE secreted by primary rat aortic smooth muscle cells is sialylated, as compared with only 10% by rat hepatocytes [50]. Despite being heavily glycosylated in human brain tissue and CSF, murine brain apoE is sparingly glycosylated.
The tissue-specific diversity of apoE glycosylation extends to the specific sites of attachment. For human apoE in the circulation, or overexpressed and secreted from cells, threonine 194 was initially identified as the sole point of O-glycan attachment [51]. This site is also occupied by O-glycans in primary human macrophage apoE, together with a novel site, Ser290 [52]. As this site is in the C-terminal lipid-binding domain of apoE, it is possible that O-glycosylation regulates the interaction of apoE with lipids. Thr194 and Ser290 also represent the two major sites of glycosylation in the CSF where additionally Ser296, S289, and the N-terminal sites Thr8 and Thr18 contain glycans [53, 54].
The diversity of apoE glycosylation is not limited to the attachment site or glycan composition. In mice, apoE glycans are of the N-linked type, attached at Asn130 [55]. Rather than requiring the classical N-linked sequon Asn-X-Ser/Thr, murine apoE glycosylation occurs at a rare non-canonical motif of Asn-Glu-Val. The attached glycan structure is di-sialylated, as is found in O-linked apoE [56]. The apoE sequence between rodent species is closely related. Rat apoE also contains a non-canonical Asn-Glu-Val sequon, suggesting N-glycosylation of apoE may be a shared feature. To test this, we treated mouse, rat, human, and rabbit plasma with PNGaseF and examined the effect on apoE molecular mass using Western blotting. Only mouse plasma apoE was sensitive to PNGaseF treatment (Fig. 3), indicating that as for human apoE, the glycosylation of rat and rabbit apoE is likely O-linked. Given the prominence of mouse models in studies in lipid metabolism, atherosclerosis, and neurodegeneration, the distinctive nature of murine apoE glycosylation should be considered in particular when tissue- and isoform-specific effects of apoE are described.
Despite advances in mass spectrometry and genetic manipulation techniques providing an increasingly detailed portrait of apoE glycan heterogeneity, the impact of this variation on its biology and physiology remains unclear. An apoE mutant lacking known O-glycosylation sites is efficiently translated and secreted, as is apoE expressed in a mutant cell line defective in O-linked glycosylation [51]. Interestingly, both the secretion and glycosylation of human apoE are increased when macrophages are treated with oleic acid [57]. When O-glycosylation of apoE is prevented, the upregulation of its secretion by oleic acid treatment is abolished. Others have indicated changes in apoE sialylation and secretion. Chronic alcohol exposure decreased apoE sialylation and secretion in rat macrophages and this was linked to less efficient binding of desialylated apoE to HDL [58]. In CSF, the terminal sialic acid at Thr194 significantly enhances the binding of apoE to the amyloidβ 1-42 peptide. This effect is highly specific, as it did not affect the association of apoE with the shorter, less toxic Aβ 1-40 peptide [59]. Others have confirmed changes in glycosylation associated with increased Aβ42 deposition in a Niemann Pick mouse model [60], suggesting that glycosylation may affect amyloid plaque formation. Thus, while glycosylation does not play a strictly essential role in the trafficking or secretion of apoE, it may act as an important post-translational mechanism for “fine-tuning” the final delivery of apoE in response to changes in extracellular lipid levels and its interaction with receptors and other proteins.
apoE secretion
ApoE secretion from hepatocytes
Hepatocytes are the main producers of apoE in the body and plasma apoE is primarily liver-derived. ApoE is secreted on VLDL and in lipid-free form in the space of Disse. A large proportion of apoE (up to 40%) is also bound to HSPGs at the cell surface. While clearance via the LDLr can be mediated by apoE from different sources, uptake via the LRP1 is solely dependent on hepatic-produced apoE, whereby locally secreted apoE in the space of Disse associates with remnants and facilitates LRP1-mediated uptake [1]. Deficiency of apoE or apoE isoforms with defective receptor binding lead to hyperlipidemia and the development atherosclerosis which can be restored after reconstitution of liver- or macrophage-specific apoE expression [1].
apoE secretion from monocytes and macrophages
Although expressed at low levels in monocytes, it is not until monocytes differentiate into macrophages that apoE expression increases and substantial amounts of apoE are secreted [61, 62]. Macrophage subtypes vary qualitatively and quantitatively in their secretion of apoE [63]. For example, apoE is a major secretory product from resident peripheral tissue macrophages but was minimally secreted from bacterially activated macrophages [64].
Circulating human monocytes are classified into classical (CD14++CD16−), intermediate (CD14+CD16+), and non-classical (CD14++CD16+) subsets [65]. In mice, two populations are recognized Ly-6Chigh and Ly-6Clow corresponding to the classical and non-classical monocyte subpopulations, respectively. Human macrophages are also commonly classified as pro-inflammatory M1 and anti-inflammatory M2; however, they display enormous plasticity and are able to switch between phenotypes in response to their environment [65].
In humans, apoE secretion is largely restricted to classical monocytes [40]. However, even within this population, phenotypical subpopulations exist. In contrast, in mice, non-classical monocytes are the main producers of apoE [66, 67]. How this relates to functional differences between mouse and human monocyte populations is unclear, but may have important implications for interpreting the biological effect of changes to monocyte populations in humans and in mouse models of human disease (Table 1).
When exposed to cytokines, macrophages respond by modulating the amount of apoE secreted from each cell and the number of secreting cells [40]. As macrophages and T cells secrete cytokines, secretion of apoE may change depending on the local immune environment such as within atherosclerotic lesions. In contrast, secretion of apoE from hepatocytes is minimally affected by exposure to cytokines [40], suggesting that inflammatory effects on apoE secretion are of particular significance in tissues enriched with macrophages.
ApoE itself may affect macrophage phenotype. Bone marrow-derived macrophages (BMDM) from apoE−/− mice were found to be more M2 like than BMDM isolated from C57Bl6 mice [71]. Paradoxically, apoE can induce conversion from M1 to the M2 phenotype through interaction with cellular lipoprotein receptors [72], implying a novel anti-inflammatory role for apoE mediated by macrophage phenotype. In microenvironments such as the atherosclerotic plaque, macrophage phenotype switching may be critical. As most studies investigating macrophage phenotypes within atherosclerotic lesions have used apoE knockout mice, this may be less relevant to conditions where apoE is constitutively expressed.
ApoE also regulates monocyte production. apoE−/− mice show progressive monocytosis and increased numbers of circulating Ly-6Chigh monocytes [70]. Hyperlipidemic mice expressing normal levels of apoE displayed 30% fewer monocytes than their apoE-deficient counterparts [81], suggesting that apoE controls monocyte production in the bone marrow. Monocytosis was associated with hyperproliferation of myeloid progenitor stem cells, via autocrine action of HSPG-bound apoE and the expression of the ATP-binding cassette transporters ABCA1 and ABCG1. Recently, cellular apoE expression in monocytes/macrophages was shown to induce miR-146a, an important suppressor of NF-κB-driven inflammation [66]. Systemic delivery of a miR-146a mimetic peptide reduced macrophage activation and monocytosis, indicating that the effects of apoE on miR-146a may be biologically important. In humans, monocytosis is associated with clinical CVD [82], although there is presently no evidence that in humans, this is regulated by apoE (Table 1). These studies imply that apoE expression in monocyte/macrophages may contribute to acute and chronic inflammatory diseases where monocytosis occurs.
apoE secretion from adipocytes—a novel metabolic role for adipose tissue-derived apoE
Adipocytes express and secrete substantial amounts of apoE. Expression is induced during differentiation with apoE being undetectable in pre-adipocytes [83]. Studies in humans, mice, rats, and baboons revealed higher expression of apoE in subcutaneous fat than in visceral fat depots [84], although macrophages within adipose tissue may also contribute to differences in apoE production. There is a clear role for endogenous adipocyte apoE in regulating cell size, triglyceride content, adipose-specific gene expression, and inflammation [74,75,76]. Adipocytes isolated from apoE−/− mice are smaller, show decreased adipogenic gene expression, and have decreased triglyceride and fatty acid content, relative to apoE-competent mice [74, 76]. This phenotype can be reversed but only partially by adenoviral transfection restoring hepatic apoE expression, indicating a critical role for endogenous apoE in adipocyte function [74, 76]. Interestingly, although transplantation of apoE-expressing bone marrow into apoE−/− mice inhibits dyslipidemia and atherosclerosis, transplantation of apoE-secreting adipose tissue does not [73]. Furthermore, transplantation of apoE-expressing bone marrow into obese apoE−/− mice inhibited dyslipidemia and atherosclerosis but had no impact on adipose tissue expansion or inflammatory status [85], indicating functional differences between macrophage- and adipocyte-derived apoE.
Selective suppression of adipose apoE secretion in the presence of normal circulating apoE levels in mice leads to increased insulin sensitivity, decreased lipid storage in muscle and liver, and shift from M1 towards M2 macrophages while plasma lipid levels were unaltered, indicating systemic metabolic and pro-inflammatory effects of adipose-derived apoE [8]. A prodiabetogenic role for apoE is supported by observations in global apoE−/− mice, which are resistant to diet-induced obesity and have lower plasma glucose levels and improved insulin sensitivity even on a diabetogenic diet (Table 1). This has been linked to decreased delivery and uptake of plasma lipids into adipose tissue and insulin target tissues such as muscle in the absence of apoE. As apoE deficiency in humans is extremely rare, these findings have not been corroborated in man and thus far, no definite association between plasma apoE levels and obesity or insulin resistance has been established. An association between the apoE4 isoform and metabolic syndrome, including elevated plasma glucose and insulin, has been observed but only in obese men (Table 1). The precise role for apoE, especially adipose-expressed apoE, in diet-induced obesity and insulin resistance will need to be explored further.
apoE secretion in the brain
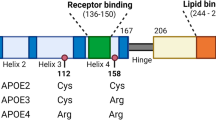
A strong link between apoE and neurodegenerative diseases is established, with the apoE4 polymorphism being one of the main risk factors for the development of Alzheimer’s disease (AD) [86]. The mechanism(s) is unclear but effects on amyloid β peptide metabolism, clearance, aggregation, and deposition as well as Aβ-independent mechanisms and direct transcriptional effects of apoE4 have been suggested. The structural and functional differences between the apoE4 isoform and the two other main isoforms, apoE2 and apoE3, have been extensively reviewed by others [79, 87].
In the brain, apoE is synthesized and secreted mainly from astrocytes, and to a lesser, extent neurons and microglia [88,89,90], although not all astrocytes express apoE, suggesting subtype-specific differences. Similarly, some but not all microglia increase apoE expression after activation [10]. Expression of apoE is increased during brain development, and most areas of the brain express apoE [91]. ApoE expression is also highly increased by injury in astrocytes, in microglia, and in neurons [92].
It has been suggested that apoE derived from different cells within the CNS has distinct physiological and pathophysiological functions [10]. For example, while neuronal-derived apoE4 stimulates parenchymal amyloid β plaque formation, glial-derived apoE4 does not [92]. Similarly, astrocyte-derived apoE4 has neuroprotective effects against excitotoxic injuries whereas neuronal-derived apoE4 promotes excitotoxic cell death [93]. The basis for these differences in cell-derived apoE is not presently known.
It is unclear whether levels of apoE within the brain are causally associated with neurodegenerative diseases such as dementia and Alzheimer’s disease, with some, but not all, studies demonstrating differences in apoE mRNA or protein levels in different regions of the brain when diseased and healthy brains were compared [94, 95]. Interestingly, significant region-specific differences in the overall methylation of apoE DNA in the brain have been reported recently, suggesting regional epigenetic control of apoE [96].
Modulation of apoE secretion by cellular cholesterol status and the role of ABCA1
Cholesterol is an important component of membranes and required for normal cell homeostasis. Cells can produce cholesterol or acquire it from their environment by endocytosis of cholesterol-rich particles. However, excessive cholesterol accumulation causes ER stress, and eventually apoptosis. In the presence of an extracellular acceptor, export of excess cholesterol can be mediated by ABCA1 and/or ABCG1. Although lipid-free or lipid-poor apoA-I is the best characterized acceptor for cholesterol exported via ABCA1, apoE will also mediate cholesterol removal through this pathway [35].
In vitro, cholesterol enrichment of macrophages increases apoE transcription and secretion and this promotes cholesterol efflux. However, macrophages isolated from high-fat fed mice have indicated reduced apoE secretion compared to macrophages from chow-fed mice [97], suggesting that in vivo regulation of apoE secretion is subject to other regulatory mechanisms. Using a cell model in which there was no effect of cholesterol on apoE transcription, we found that accumulation of excess free cholesterol in the ER inhibited transport of apoE from the ER to the Golgi [98]. This was reversed when excess cholesterol was removed. In vitro, cholesterol enrichment of cells can be achieved by various methods, which differentially regulate apoE expression and secretion. We observed increased apoE transcription and a modest increase in secretion in primary human macrophages after cholesterol enrichment using acetylated LDL, while delivery of cholesterol complexed to cyclodextrin did not affect apoE synthesis and decreased apoE secretion (unpublished data). Heterogeneity within pools of intracellular cholesterol has been well described and these may play important and competing roles in apoE secretion [99].
Cholesterol homeostasis is integral to normal brain function. Cholesterol and apoE are secretion from glial cells and are ABCA1-dependent, forming nascent discoidal apoE-containing HDLs. However, apoE is also secreted in an ABCA1-independent, lipid-poor form which involves recycling via the LDLr [100]. The mechanism underlying apoE lipidation in the brain has been of much interest, as lipidated apoE facilitates the removal of amyloid β peptides while lipid-poor apoE stimulates the formation of amyloid plaque [101]. Just as for glial cells, apoE secretion from neurons [102, 103] involves ABCA1-mediated cholesterol efflux to apoE discs, which suppress amyloid precursor protein processing. Recently, a loss-of-function mutation in ABCA1 was associated with high risk of AD and cerebrovascular disease in the general population [80]. As this mutation was associated with 13% lower apoE levels, an apoE-mediated risk increase was suggested. Stimulation of apoE production/secretion and ABCA1-mediated lipidation are therefore sought after targets for therapy against AD and neurodegenerative diseases.
Conclusions
Regulation of apoE production and secretion is remarkably cell and tissue specific with many aspects of cell-specific regulation being unidentified. Considering the cell and tissue specificity in apoE function related to atherosclerosis, obesity, and neurodegenerative diseases (Fig. 4), understanding these pathways is important to allow targeted therapies aiming at cell-specific modulation of apoE to occur in the future.
Functional aspects of apoE in hepatocytes, monocytes/macrophages, adipocytes, and cells in the CNS. Hepatic apoE affects various aspects of lipid metabolism and regulates plasma lipid levels. Deficiency leads to decreased lipoprotein clearance, while increased hepatic expression leads to increased VLDL production. Macrophage apoE has anti-inflammatory and immune-modulatory effects and affects foam cell formation, all contributing to protection against atherosclerosis. In adipocytes, apoE mediates cell size, tissue expansion, and adipocyte differentiation and plays a role in adipose tissue inflammation and diet-induced obesity. In the CNS, apoE is mainly secreted from astrocytes delivering lipoproteins to neurons and plays a role in maintaining brain integrity. ApoE secretion is highly increased after injury in astrocytes, microglia, and neurons to provide neuroprotection and aid in repair
References
van Dijk KW, Hofker MH, Havekes LM (1999) Dissection of the complex role of apolipoprotein E in lipoprotein metabolism and atherosclerosis using mouse models. Curr Atheroscler Rep 1:101–107
Pechlaner R, Tsimikas S, Yin X, Willeit P, Baig F, Santer P, Oberhollenzer F, Egger G, Witztum JL, Alexander VJ et al. (2017) Very-low-density lipoprotein-associated apolipoproteins predict cardiovascular events and are lowered by inhibition of APOC-III. J Am Coll Cardiol 69:789–800
Bellosta S, Mahley RW, Sanan DA, Murata J, Newland DL, Taylor JM, Pitas RE (1995) Macrophage-specific expression of human apolipoprotein E reduces atherosclerosis in hypercholesterolemic apolipoprotein E-null mice. J Clin Invest 96:2170–2179
Ali K, Middleton M, Puré E, Rader DJ (2005) Apolipoprotein E suppresses the type I inflammatory response in vivo. Circ Res 97:922–927
van den Elzen P, Garg S, León L et al (2005) Apolipoprotein-mediated pathways of lipid antigen presentation. Nature 437:906–910
Kothapalli D, Fuki I, Ali K, Stewart SA, Zhao L, Yahil R, Kwiatkowski D, Hawthorne EA, FitzGerald GA, Phillips MC et al. (2004) Antimitogenic effects of HDL and APOE mediated by Cox-2-dependent IP activation. J Clin Invest 113:609–618
Li Y-H, Liu L (2014) Apolipoprotein E synthesized by adipocyte and apolipoprotein E carried on lipoproteins modulate adipocyte triglyceride content. Lipids Health Dis 13:136
Huang ZH, Reardon CA, Getz GS, Maeda N, Mazzone T (2015) Selective suppression of adipose tissue apoE expression impacts systemic metabolic phenotype and adipose tissue inflammation. J Lipid Res 56:215–226
Arbones-Mainar JM, Johnson LA, Altenburg MK, Maeda N (2008) Differential modulation of diet-induced obesity and adipocyte functionality by human apolipoprotein E3 and E4 in mice. Int J Obes 32:1595–1605
Xu Q, Bernardo A, Walker D, Kanegawa T, Mahley RW, Huang Y (2006) Profile and regulation of apolipoprotein E (ApoE) expression in the CNS in mice with targeting of green fluorescent protein gene to the ApoE locus. J Neurosci 26:4985–4994
Gafencu AV, Robciuc MR, Fuior E, Zannis VI, Kardassis D, Simionescu M (2007) Inflammatory signaling pathways regulating ApoE gene expression in macrophages. J Biol Chem 282:21776–21785
Chang DJ, Paik YK, Leren TP, Walker DW, Howlett GJ, Taylor JM (1990) Characterization of a human apolipoprotein E gene enhancer element and its associated protein factors. J Biol Chem 265:9496–9504
Berg DT, Calnek DS, Grinnell BW (1995) The human apolipoprotein E gene is negatively regulated in human liver HepG2 cells by the transcription factor BEF-1. J Biol Chem 270:15447–15450
García MA, Vázquez J, Giménez C, Valdivieso F, Zafra F (1996) Transcription factor AP-2 regulates human apolipoprotein E gene expression in astrocytoma cells. J Neurosci 16:7550–7556
Salero E, Pérez-Sen R, Aruga J, Giménez C, Zafra F (2001) Transcription factors Zic1 and Zic2 bind and transactivate the apolipoprotein E gene promoter. J Biol Chem 276:1881–1888
Salero E, Giménez C, Zafra F (2003) Identification of a non-canonical E-box motif as a regulatory element in the proximal promoter region of the apolipoprotein E gene. Biochem J 370:979–986
Stavri S, Simionescu M, Kardassis D, Gafencu AV (2015) Krüppel-like factor 4 synergizes with CREB to increase the activity of apolipoprotein E gene promoter in macrophages. Biochem Biophys Res Commun 468:66–72
Simonet WS, Bucay N, Lauer SJ, Taylor JM (1993) A far-downstream hepatocyte-specific control region directs expression of the linked human apolipoprotein E and C-I genes in transgenic mice. J Biol Chem 268:8221–8229
Paik YK, Chang DJ, Reardon CA, Walker MD, Taxman E, Taylor JM (1988) Identification and characterization of transcriptional regulatory regions associated with expression of the human apolipoprotein E gene. J Biol Chem 263:13340–13349
Allan CM, Walker D, Taylor JM (1995) Evolutionary duplication of a hepatic control region in the human apolipoprotein E gene locus. Identification of a second region that confers high level and liver-specific expression of the human apolipoprotein E gene in transgenic mice. J Biol Chem 270:26278–26281
Shih SJ, Allan C, Grehan S, Tse E, Moran C, Taylor JM (2000) Duplicated downstream enhancers control expression of the human apolipoprotein E gene in macrophages and adipose tissue. J Biol Chem 275:31567–31572
Grehan S, Tse E, Taylor JM (2001) Two distal downstream enhancers direct expression of the human apolipoprotein E gene to astrocytes in the brain. J Neurosci 21:812–822
Laffitte BA, Repa JJ, Joseph SB, Wilpitz DC, Kast HR, Mangelsdorf DJ, Tontonoz P (2001) LXRs control lipid-inducible expression of the apolipoprotein E gene in macrophages and adipocytes. Proc Natl Acad Sci U S A 98:507–512
Liang Y, Lin S, Beyer TP, Zhang Y, Wu X, Bales KR, DeMattos RB, May PC, Li SD, Jiang XC et al. (2004) A liver X receptor and retinoid X receptor heterodimer mediates apolipoprotein E expression, secretion and cholesterol homeostasis in astrocytes. J Neurochem 88:623–634
Ramos MC, Matías S, Artiga MJ et al (2005) Neuronal specific regulatory elements in apolipoprotein E gene proximal promoter. Neuroreport 16:1027–1030
Trusca VG, Fuior EV, Fenyo IM, Kardassis D, Simionescu M, Gafencu AV (2017) Differential action of glucocorticoids on apolipoprotein E gene expression in macrophages and hepatocytes. PLoS One 12:e0174078
Xu Q, Walker D, Bernardo A, Brodbeck J, Balestra ME, Huang Y (2008) Intron-3 retention/splicing controls neuronal expression of apolipoprotein E in the CNS. J Neurosci 28:1452–1459
Ma Y, Smith CE, Lai C-Q, Irvin MR, Parnell LD, Lee YC, Pham L, Aslibekyan S, Claas SA, Tsai MY et al. (2015) Genetic variants modify the effect of age on APOE methylation in the Genetics of Lipid Lowering Drugs and Diet Network study. Aging Cell 14:49–59
Seitz A, Gourevitch D, Zhang X-M, Clark L, Chen P, Kragol M, Levenkova N, Rux J, Samulewicz S, Heber-Katz E (2005) Sense and antisense transcripts of the apolipoprotein E gene in normal and ApoE knockout mice, their expression after spinal cord injury and corresponding human transcripts. Hum Mol Genet 14:2661–2670
Pencheva N, Tran H, Buss C, Huh D, Drobnjak M, Busam K, Tavazoie SF (2012) Convergent multi-miRNA targeting of ApoE drives LRP1/LRP8-dependent melanoma metastasis and angiogenesis. Cell 151:1068–1082
Kockx M, Guo DL, Huby T, Lesnik P, Kay J, Sabaretnam T, Jary E, Hill M, Gaus K, Chapman J et al. (2007) Secretion of apolipoprotein E from macrophages occurs via a protein kinase A and calcium-dependent pathway along the microtubule network. Circ Res 101:607–616
Burgess JW, Gould DR, Marcel YL (1998) The HepG2 extracellular matrix contains separate heparinase- and lipid-releasable pools of ApoE. Implications for hepatic lipoprotein metabolism. J Biol Chem 273:5645–5654
Zhao Y, Mazzone T (2000) Transport and processing of endogenously synthesized ApoE on the macrophage cell surface. J Biol Chem 275:4759–4765
Dory L (1991) Regulation of apolipoprotein E secretion by high density lipoprotein 3 in mouse macrophages. J Lipid Res 32:783–792
Kockx M, Rye K-A, Gaus K, Quinn CM, Wright J, Sloane T, Sviridov D, Fu Y, Sullivan D, Burnett JR et al. (2004) Apolipoprotein A-I-stimulated apolipoprotein E secretion from human macrophages is independent of cholesterol efflux. J Biol Chem 279:25966–25977
Karunakaran D, Kockx M, Owen DM, Burnett JR, Jessup W, Kritharides L (2013) Protein kinase C controls vesicular transport and secretion of apolipoprotein E from primary human macrophages. J Biol Chem 288:5186–5197
Kockx M, Guo DL, Traini M, Gaus K, Kay J, Wimmer-Kleikamp S, Rentero C, Burnett JR, le Goff W, van Eck M et al. (2009) Cyclosporin A decreases apolipoprotein E secretion from human macrophages via a protein phosphatase 2B-dependent and ATP-binding cassette transporter A1 (ABCA1)-independent pathway. J Biol Chem 284:24144–24154
Kockx M, Karunakaran D, Traini M, Xue J, Huang KY, Nawara D, Gaus K, Jessup W, Robinson PJ, Kritharides L (2014) Pharmacological inhibition of dynamin II reduces constitutive protein secretion from primary human macrophages. PLoS One 9:e111186
Liu J, Farmer JD, Lane WS et al (1991) Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes. Cell 66:807–815
Braesch-Andersen S, Paulie S, Smedman C, Mia S, Kumagai-Braesch M (2013) ApoE production in human monocytes and its regulation by inflammatory cytokines. PLoS One 8:e79908
Dekroon RM, Armati PJ (2002) The effects of oxidative stress and altered intracellular calcium levels on vesicular transport of apoE-EGFP. Cell Biol Int 26:407–420
Kimura A, Hata S, Suzuki T (2015) Stabilization of intracellular trafficking and metabolism of amyloid β-protein precursor and Alcadein β by apolipoprotein E. FEBS Lett 589:2394–2400
Finan GM, Realubit R, Chung S, Lütjohann D, Wang N, Cirrito JR, Karan C, Kim TW (2016) Bioactive compound screen for pharmacological enhancers of apolipoprotein E in primary human astrocytes. Cell Chem Biol 23:1526–1538
Ito J-I, Nagayasu Y, Miura Y, Yokoyama S, Michikawa M (2014) Astrocyte′s endogenous apoE generates HDL-like lipoproteins using previously synthesized cholesterol through interaction with ABCA1. Brain Res 1570:1–12
Yue L, Mazzone T (2011) Endogenous adipocyte apolipoprotein E is colocalized with caveolin at the adipocyte plasma membrane. J Lipid Res 52:489–498
Zannis VI, Breslow JL, SanGiacomo TR et al (1981) Characterization of the major apolipoproteins secreted by two human hepatoma cell lines. Biochemistry 20:7089–7096
Ghiselli G, Beigel Y, Soma M, Gotto AM (1986) Plasma catabolism of human apolipoprotein E isoproteins: lack of conversion of the doubly sialylated form to the asialo form in plasma. Metab Clin Exp 35:399–403
Pitas RE, Boyles JK, Lee SH, Foss D, Mahley RW (1987) Astrocytes synthesize apolipoprotein E and metabolize apolipoprotein E-containing lipoproteins. Biochim Biophys Acta 917:148–161
Yamauchi K, Tozuka M, Hidaka H, Hidaka E, Kondo Y, Katsuyama T (1999) Characterization of apolipoprotein E-containing lipoproteins in cerebrospinal fluid: effect of phenotype on the distribution of apolipoprotein E. Clin Chem 45:1431–1438
Hussain MM, Bucher NL, Faris B, Franzblau C, Zannis VI (1988) Tissue-specific posttranslational modification of rat apoE. Synthesis of sialated apoE forms by neonatal rat aortic smooth muscle cells. J Lipid Res 29:915–923
Wernette-Hammond ME, Lauer SJ, Corsini A, Walker D, Taylor JM, Rall SC Jr (1989) Glycosylation of human apolipoprotein E. The carbohydrate attachment site is threonine 194. J Biol Chem 264:9094–9101
Lee Y, Kockx M, Raftery MJ, Jessup W, Griffith R, Kritharides L (2010) Glycosylation and sialylation of macrophage-derived human apolipoprotein E analyzed by SDS-PAGE and mass spectrometry: evidence for a novel site of glycosylation on Ser290. Mol Cell Proteomics 9:1968–1981
Halim A, Rüetschi U, Larson G, Nilsson J (2013) LC-MS/MS characterization of O-glycosylation sites and glycan structures of human cerebrospinal fluid glycoproteins. J Proteome Res 12:573–584
Nilsson J, Rüetschi U, Halim A, Hesse C, Carlsohn E, Brinkmalm G, Larson G (2009) Enrichment of glycopeptides for glycan structure and attachment site identification. Nat Methods 6:809–811
Zielinska DF, Gnad F, Wiśniewski JR, Mann M (2010) Precision mapping of an in vivo N-glycoproteome reveals rigid topological and sequence constraints. Cell 141:897–907
Medzihradszky KF, Kaasik K, Chalkley RJ (2015) Tissue-specific glycosylation at the glycopeptide level. Mol Cell Proteomics 14:2103–2110
Huang ZH, Gu D, Mazzone T (2004) Oleic acid modulates the post-translational glycosylation of macrophage ApoE to increase its secretion. J Biol Chem 279:29195–29201
Marmillot P, Rao MN, Liu QH, Lakshman MR (1999) Desialylation of human apolipoprotein E decreases its binding to human high-density lipoprotein and its ability to deliver esterified cholesterol to the liver. Metab Clin Exp 48:1184–1192
Aleshkov SB, Li X, Lavrentiadou SN, Zannis VI (1999) Contribution of cysteine 158, the glycosylation site threonine 194, the amino- and carboxy-terminal domains of apolipoprotein E in the binding to amyloid peptide beta (1-40). Biochemistry 38:8918–8925
Chua C-C, Lim M-L, Wong B-S (2010) Altered apolipoprotein E glycosylation is associated with Abeta(42) accumulation in an animal model of Niemann-Pick Type C disease. J Neurochem 112:1619–1626
Basu SK, Brown MS, Ho YK, Havel RJ, Goldstein JL (1981) Mouse macrophages synthesize and secrete a protein resembling apolipoprotein E. Proc Natl Acad Sci U S A 78:7545–7549
Werb Z, Chin JR (1983) Onset of apoprotein E secretion during differentiation of mouse bone marrow-derived mononuclear phagocytes. J Cell Biol 97:1113–1118
Tedla N, Glaros EN, Brunk UT, Jessup W, Garner B (2004) Heterogeneous expression of apolipoprotein-E by human macrophages. Immunology 113:338–347
Takemura R, Werb Z (1984) Secretory products of macrophages and their physiological functions. Am J Phys 246:C1–C9
Leitinger N, Schulman IG (2013) Phenotypic polarization of macrophages in atherosclerosis. Arterioscler Thromb Vasc Biol 33:1120–1126
Li K, Ching D, Luk FS, Raffai RL (2015) Apolipoprotein E enhances microRNA-146a in monocytes and macrophages to suppress nuclear factor-κB-driven inflammation and atherosclerosis. Circ Res 117:e1–e11
Bouchareychas L, Pirault J, Saint-Charles F, Deswaerte V, le Roy T, Jessup W, Giral P, le Goff W, Huby T, Gautier EL, Lesnik P (2015) Promoting macrophage survival delays progression of pre-existing atherosclerotic lesions through macrophage-derived apoE. Cardiovasc Res 108:111–123
Huang Y, Liu XQ, Rall SC et al (1998) Overexpression and accumulation of apolipoprotein E as a cause of hypertriglyceridemia. J Biol Chem 273:26388–26393
Zhang SH, Reddick RL, Piedrahita JA, Maeda N (1992) Spontaneous hypercholesterolemia and arterial lesions in mice lacking apolipoprotein E. Science 258:468–471
Murphy AJ, Akhtari M, Tolani S, Pagler T, Bijl N, Kuo CL, Wang M, Sanson M, Abramowicz S, Welch C et al. (2011) ApoE regulates hematopoietic stem cell proliferation, monocytosis, and monocyte accumulation in atherosclerotic lesions in mice. J Clin Invest 121:4138–4149
Khallou-Laschet J, Varthaman A, Fornasa G, Compain C, Gaston AT, Clement M, Dussiot M, Levillain O, Graff-Dubois S, Nicoletti A, Caligiuri G (2010) Macrophage plasticity in experimental atherosclerosis. PLoS One 5:e8852
Baitsch D, Bock HH, Engel T, Telgmann R, Muller-Tidow C, Varga G, Bot M, Herz J, Robenek H, von Eckardstein A, Nofer JR (2011) Apolipoprotein E induces antiinflammatory phenotype in macrophages. Arterioscler Thromb Vasc Biol 31:1160–1168
Huang ZH, Reardon CA, Subbaiah PV, Getz GS, Mazzone T (2013) ApoE derived from adipose tissue does not suppress atherosclerosis or correct hyperlipidemia in apoE knockout mice. J Lipid Res 54:202–213
Huang ZH, Reardon CA, Mazzone T (2006) Endogenous ApoE expression modulates adipocyte triglyceride content and turnover. Diabetes 55:3394–3402
Huang ZH, Gu D, Mazzone T (2009) Role of adipocyte-derived apoE in modulating adipocyte size, lipid metabolism, and gene expression in vivo. Am J Physiol Endocrinol Metab 296:E1110–E1119
Lasrich D, Bartelt A, Grewal T, Heeren J (2015) Apolipoprotein E promotes lipid accumulation and differentiation in human adipocytes. Exp Cell Res 337:94–102
Hofmann SM, Perez-Tilve D, Greer TM, Coburn BA, Grant E, Basford JE, Tschop MH, Hui DY (2008) Defective lipid delivery modulates glucose tolerance and metabolic response to diet in apolipoprotein E-deficient mice. Diabetes 57:5–12
Elosua R, Demissie S, Cupples LA, Meigs JB, Wilson PWF, Schaefer EJ, Corella D, Ordovas JM (2003) Obesity modulates the association among APOE genotype, insulin, and glucose in men. Obes Res 11:1502–1508
Mahley RW (2016) Apolipoprotein E: from cardiovascular disease to neurodegenerative disorders. J Mol Med 94:739–746
Nordestgaard LT, Tybjærg-Hansen A, Nordestgaard BG, Frikke-Schmidt R (2015) Loss-of-function mutation in ABCA1 and risk of Alzheimer’s disease and cerebrovascular disease. Alzheimers Dement 11:1430–1438
Gaudreault N, Kumar N, Posada JM, Stephens KB, Reyes de Mochel NS, Eberle D, Olivas VR, Kim RY, Harms MJ, Johnson S et al. (2012) ApoE suppresses atherosclerosis by reducing lipid accumulation in circulating monocytes and the expression of inflammatory molecules on monocytes and vascular endothelium. Arterioscler Thromb Vasc Biol 32:264–272
van der Valk FM, Kuijk C, Verweij SL, Stiekema LCA, Kaiser Y, Zeerleder S, Nahrendorf M, Voermans C, Stroes ESG (2017) Increased haematopoietic activity in patients with atherosclerosis. Eur Heart J 38:425–432
Zechner R, Moser R, Newman TC, Fried SK, Breslow JL (1991) Apolipoprotein E gene expression in mouse 3T3-L1 adipocytes and human adipose tissue and its regulation by differentiation and lipid content. J Biol Chem 266:10583–10588
Huang ZH, Espiritu DJ, Uy A, Holterman AX, Vitello J, Mazzone T (2011) Adipose tissue depot-specific differences in adipocyte apolipoprotein E expression. Metab Clin Exp 60:1692–1701
Atkinson RD, Coenen KR, Plummer MR, Gruen ML, Hasty AH (2008) Macrophage-derived apolipoprotein E ameliorates dyslipidemia and atherosclerosis in obese apolipoprotein E-deficient mice. Am J Physiol Endocrinol Metab 294:E284–E290
Giau VV, Bagyinszky E, An SSA, Kim SY (2015) Role of apolipoprotein E in neurodegenerative diseases. Neuropsychiatr Dis Treat 11:1723–1737
Chang T-Y, Chang C (2017) ApoE and lipid homeostasis in Alzheimer’s disease: introduction to the thematic review series. J Lipid Res 58:823
Boyles JK, Pitas RE, Wilson E, Mahley RW, Taylor JM (1985) Apolipoprotein E associated with astrocytic glia of the central nervous system and with nonmyelinating glia of the peripheral nervous system. J Clin Invest 76:1501–1513
Dekroon RM, Armati PJ (2001) Synthesis and processing of apolipoprotein E in human brain cultures. Glia 33:298–305
Keren-Shaul H, Spinrad A, Weiner A et al (2017) A unique microglia type associated with restricting development of Alzheimer’s disease. Cell 169:1276–1290.e17
Elshourbagy NA, Liao WS, Mahley RW, Taylor JM (1985) Apolipoprotein E mRNA is abundant in the brain and adrenals, as well as in the liver, and is present in other peripheral tissues of rats and marmosets. Proc Natl Acad Sci U S A 82:203–207
Van Dooren T, Muyllaert D, Borghgraef P et al (2006) Neuronal or glial expression of human apolipoprotein e4 affects parenchymal and vascular amyloid pathology differentially in different brain regions of double- and triple-transgenic mice. Am J Pathol 168:245–260
Buttini M, Masliah E, Yu G-Q, Palop JJ, Chang S, Bernardo A, Lin C, Wyss-Coray T, Huang Y, Mucke L (2010) Cellular source of apolipoprotein E4 determines neuronal susceptibility to excitotoxic injury in transgenic mice. Am J Pathol 177:563–569
Bekris LM, Galloway NM, Montine TJ, Schellenberg GD, Yu CE (2010) APOE mRNA and protein expression in postmortem brain are modulated by an extended haplotype structure. Am J Med Genet B Neuropsychiatr Genet 153B:409–417
Dean B, Laws SM, Hone E, Taddei K, Scarr E, Thomas EA, Harper C, McClean C, Masters C, Lautenschlager N et al. (2003) Increased levels of apolipoprotein E in the frontal cortex of subjects with schizophrenia. Biol Psychiatry 54:616–622
Yu C-E, Foraker J (2015) Epigenetic considerations of the APOE gene. [corrected]. Biomol Concepts 6:77–84
Becker L, Gharib SA, Irwin AD, Wijsman E, Vaisar T, Oram JF, Heinecke JW (2010) A macrophage sterol-responsive network linked to atherogenesis. Cell Metab 11:125–135
Kockx M, Dinnes DL, Huang K-Y, Sharpe LJ, Jessup W, Brown AJ, Kritharides L (2012) Cholesterol accumulation inhibits ER to Golgi transport and protein secretion: studies of apolipoprotein E and VSVGt. Biochem J 447:51–60
Liscum L, Underwood KW (1995) Intracellular cholesterol transport and compartmentation. J Biol Chem 270:15443–15446
Fan J, Stukas S, Wong C, Chan J, May S, DeValle N, Hirsch-Reinshagen V, Wilkinson A, Oda MN, Wellington CL (2011) An ABCA1-independent pathway for recycling a poorly lipidated 8.1 nm apolipoprotein E particle from glia. J Lipid Res 52:1605–1616
Jiang Q, Lee CYD, Mandrekar S, Wilkinson B, Cramer P, Zelcer N, Mann K, Lamb B, Willson TM, Collins JL et al. (2008) ApoE promotes the proteolytic degradation of Abeta. Neuron 58:681–693
Kim WS, Rahmanto AS, Kamili A, Rye KA, Guillemin GJ, Gelissen IC, Jessup W, Hill AF, Garner B (2007) Role of ABCG1 and ABCA1 in regulation of neuronal cholesterol efflux to apolipoprotein E discs and suppression of amyloid-beta peptide generation. J Biol Chem 282:2851–2861
Burgess BL, Parkinson PF, Racke MM, Hirsch-Reinshagen V, Fan J, Wong C, Stukas S, Theroux L, Chan JY, Donkin J et al. (2008) ABCG1 influences the brain cholesterol biosynthetic pathway but does not affect amyloid precursor protein or apolipoprotein E metabolism in vivo. J Lipid Res 49:1254–1267
Funding
This work has been funded by NHMRC Program Grant 482820.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kockx, M., Traini, M. & Kritharides, L. Cell-specific production, secretion, and function of apolipoprotein E. J Mol Med 96, 361–371 (2018). https://doi.org/10.1007/s00109-018-1632-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-018-1632-y