Abstract
The Czech Republic occupies the first place in the world in the frequency of renal and other urinary tract tumours, but their aetiology is unknown. To explore whether carcinogenic and nephrotoxic mycotoxins may contribute to kidney diseases in the Czech population, biomarkers of ochratoxin A (OTA) and citrinin (CIT) exposure were determined in biological specimens from a cohort of 50 patients with malignant renal tumours. Biomarker analyses in blood and urine samples used validated targeted methods for measuring OTA and CIT plus dihydrocitrinone (DH-CIT) after enrichment of analytes by specific immunoaffinity clean-up. OTA and CIT plus its metabolite DH-CIT were frequently detected in patient urine samples (OTA 62%; CIT 91%; DH-CIT 100%). The concentration ranges in urine were 1–27.8 ng/L for OTA, 2–87 ng/L for CIT and 2–160 ng/L for DH-CIT. The analyses of blood samples revealed also a frequent co-occurrence of OTA and CIT, in the ranges of 40–870 ng/L serum for OTA and 21–182 ng/L plasma for CIT. This first analysis of biomarkers in blood and urine samples of Czech patients revealed no major differences in comparison with published data for the general healthy Czech and European populations. Nonetheless, a frequent co-occurrence of CIT and OTA biomarkers in patient samples may be of interest with regard to potential interactions with other risk factors for renal disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Based on epidemiological information on malignant diseases, the incidence in the Czech Republic of renal tumours and other urinary tract tumours is very high in comparison with other countries (e.g. Germany, see Robert Koch-Institut 2017). The incidence of malignant neoplasms of the kidney and of renal pelvis and ureter (diagnosis C64–C66) is 29.5 renal tumours/100,000 inhabitants of the Czech Republic (Dusek et al. 2017). The tumours diagnosed are mainly renal carcinoma/adenocarcinoma arising from the proximal tubule cells (clear cell renal cell carcinoma, ccRCC, formerly called Grawitz tumour) and papillary renal carcinoma of the renal pelvis (Tesar et al. 2015). Balkan endemic nephropathy (BEN), a unique chronic renal disease, is often associated with upper urinary tract tumours arising from the urothelium (Grollman and Jelakovic 2007). Factors suspected of inducing this disease are nephrotoxins, primarily mycotoxins and aristolochic acid, metals and metalloids as well as possibly an individual genetic predisposition (Pfohl-Leszkowicz et al. 2002; Peraica et al. 2008; Pfohl-Leszkowicz 2009; Stiborova et al. 2016; Chan et al. 2018).
Different factors can play a role in the incidence of ccRCCs and other kidney tumours, e.g. hypertension and obesity (Sanfilippo et al. 2014), lifestyle and health behaviours such as physical activity, alcohol consumption and smoking (Chow et al. 2010) but also genetic factors (Reaume et al. 2013; Schmidt and Linehan 2016). Other, mainly occupational risk factors for renal cancer include high exposure to cadmium, lead and solder fumes as well as paints, mineral oils, cutting fluids, benzene, polycyclic aromatic hydrocarbons, trichloroethylene and tetrachloroethylene (Pesch et al. 2000; Radford et al. 2013). In short, the aetiology of renal cancer is not well understood, and the impact of various risk factors on disease may vary in different cohorts. In a Czech cohort of patients with kidney tumours (main diagnosis C64), we have studied their exposure to carcinogenic and nephrotoxic mycotoxins, namely ochratoxin A (OTA) and citrinin (CIT). The contamination of food commodities with OTA is quite frequent in Europe including the Czech Republic (EFSA 2006; Ostry et al. 2013; Ostry et al. 2015), whereas available data on CIT levels in food and feed is rather scarce (EFSA 2012).
Since CIT has similar toxic properties as OTA, their co-occurrence has raised concerns regarding possible combined effects on animals and humans, in particular porcine nephropathy and BEN (Pfohl-Leszkowicz et al. 2002; Pfohl-Leszkowicz et al. 2008; Peraica et al. 2008; Ostry et al. 2013). An experimental co-administration of CIT and OTA in rodents or in vitro can increase OTA-DNA adducts in kidney (Manderville and Pfohl-Leszkowicz 2008; Pfohl-Leszkowicz et al. 2008) and also oxidative DNA damage (Segvic-Klaric et al. 2013). Depending on doses and the relative proportion of CIT and OTA, either antagonism or synergy has been observed (Pfohl-Leszkowicz et al. 2008; Föllmann et al. 2014). Thus, it is of interest to assess the exposure to both mycotoxins in humans.
A valuable tool to investigate human exposure to mycotoxins is biomonitoring, i.e. the analysis of parent compounds and/or metabolites in biological fluids such as blood, urine or breast milk samples. It has served to study exposure to mycotoxins in different countries and cohorts, and to study the success of intervention measures aimed to reduce dietary intake (Duarte et al. 2011; Turner et al. 2012). Analysis by means of suitable biomarkers of exposure is considered to be the preferable tool for human exposure assessment as it covers mycotoxin intake from all sources and routes, and better reflects the individual exposure situation, toxicokinetics and bioavailability (Duarte et al. 2011; Malir et al. 2012; Fromme et al. 2016).
In this study, biomarkers of OTA and CIT exposure have been determined in 50 patients with renal tumours from the Czech Republic. We applied validated specific methods for analyses of OTA, CIT and its metabolite dihydrocitrinone (DH-CIT) in blood and urine samples collected prior to surgery. The structures of the analytes are depicted in Fig. 1. Their levels in the patient cohort are compared with those of healthy populations to explore if exposure to nephrotoxic mycotoxins may be a contributing factor to the high frequency of renal tumours observed in the Czech Republic. This first biomarker analyses in Czech tumour patients revealed current mycotoxin exposures well below the tolerable daily intake values for OTA and CIT. The results will be also discussed in relation to remaining uncertainties such as potential risks from past exposure, not reflected in our present study, or combined exposures.
Materials and methods
Chemicals and materials
Glacial acetic acid, hydrochloric acid, ortho-phosphoric acid 85%, magnesium sulphate hexahydrate, sodium chloride, anhydrous sodium acetate (all in p.a. purity), methanol and acetonitrile (both gradient grade for HPLC) were obtained from Merck KGaA (Prague, Czech Republic), and acetic acid (96%) from Merck KGaA (Darmstadt, Germany). Acetonitrile and methanol (LC-MS grade) were from Promochem (Wesel, Germany). Chloroform and sodium hydrogen carbonate (both p.a.) were purchased from Riedel-de Haen (Prague, Czech Republic). OTA standard material (1 mg, purity > 98%) and phosphate-buffered saline of pH 7.4 were obtained from Sigma-Aldrich (Prague, Czech Republic). Ultrapure water was prepared by Milli-Q Plus (Millipore, Billerica, MA, USA).
OTA was dissolved in methanol and spectrophotometrically calibrated at 333 nm using the molar extinction coefficient (ε) of 6400 (Reinhard and Zimmerli 1999). A basic OTA solution was prepared by dissolving 1 mg of OTA in 5 mL of methanol, and an OTA stock standard solution (40 ng/mL) was prepared by further dilution in methanol. The working standard solutions of OTA in a range of 0.1–20.0 ng/mL were prepared weekly from the OTA stock solution as dilutions in the mobile phase (methanol/acetonitrile/0.005 mol/L sodium acetate/acetic acid, 300/300/400/14, v/v/v/v).
CIT standard material (5 mg, purity > 98%) was from Sigma-Aldrich (Taufkirchen, Germany); CIT stock solution in methanol was calibrated at 321 nm using the absorptivity ε = 5490 (Reinhard and Zimmerli 1999). The CIT metabolite DH-CIT (purity 98.9%) was obtained from AnalytiCon Discovery GmbH (Potsdam, Germany). CIT and DH-CIT working standard solutions were prepared weekly from their stock solutions (CIT, 200 μg/mL acetonitrile; DH-CIT, 500 μg/mL acetonitrile) by dilution in methanol in a range of 1–20 ng/mL (1000–20,000 ng/L).
Cohort and collection of samples
Biological samples (blood and urine) were collected from November 2015 to April 2017 from 50 randomly selected patients (a group of 39 men and 11 women) with diagnosis of kidney cancer and aged between 40 and 81 years (see Table 1). For the purposes of this study, on the basis of the previous standard laboratory and medical examinations, only those patients without overall metabolic disruption and cardiovascular complications were randomly selected. Blood and urine samples for this study were collected just before surgical operation as part of standard clinical sampling so that patients were not excessively burdened (one of the conditions of approval by the Ethics Commission). Samples of urine were collected from the patients in all standard preoperative examinations, starting from their arrival at the Department of Urology until the morning of the next day when the operation was performed. Blood samples were divided in three containers from Sarstedt: (i) two S-Monovettes (2.7 mL, K2EDTA—for obtaining optimally about 4 mL of plasma overall) were centrifuged (at 3000 rpm, approximately about 1620×g) for 15 min for separation of plasma using a B4i Jouan (France) centrifuge, and then the separated plasma was placed into a vial; (ii) another container marked S-Monovette (5.5 mL Z, Clotting Activator/serum) was used for obtaining the serum, and then the sample of separated serum was placed into a vial. Urine samples were collected into a non-sterile container (1.5 L) stored in the refrigerator. Each urine sample was mixed, and from it approximately 100 mL of urine after centrifugation (at 3000 rpm) was placed into a polypropylene container, and these samples were immediately stored at − 80 °C until analysis. All samples were sent anonymously (using a numerical code) to the laboratories. Personal data on gender, the year of birth and the body weight of the patient were recorded.
OTA extraction, detection and quantification
Prior to detection and quantification of OTA in serum and OTA in urine, aliquoted samples of 3 mL of acidified blood serum (Zimmerli and Dick 1995; Dohnal et al. 2013) and 20 mL of filtered urine sample (Ostry et al. 2010) were extracted and cleaned on Ochraprep® R immunoaffinity columns (Biopharm Rhone Ltd., Great Britain).
As in previous studies of other cohorts (Malir et al. 2006; Ostry et al. 2010; Dohnal et al. 2013), the validated and accredited method (CSN EN ISO/IEC 17025) of reversed-phase high-performance liquid chromatography with fluorescence detection was employed for purposes of OTA detection and quantification. OTA was analysed on a liquid chromatograph consisting of a vacuum degasser SCM400, gradient pump P2000, autosampler AS 3000 (all from Spectra System, USA), fluorescence detector 920 FP (Jasco, Japan) and Solvent Saver 2907 (Jour Research, Sweden) coupled with the analytical column Inertsil ODS-3V (5 μm × 150 mm × 4.6 mm; Hichrom Ltd., UK) with a guard column (3.0 × 4.0 mm filled with C18 material of particle size 5 μm, Phenomenex, USA) and—for calculations and evaluations—equipped with a computer and CSW 32 (DataApex, Prague, Czech Republic) software. OTA fluorescence was measured at an excitation wavelength of 333 nm, and an emission wavelength of 465 nm for serum analysis or 443 nm for urine analysis. The injection volumes were 50 μL for serum samples and 100 μL for urine samples. The mobile phase for OTA analysis consisted of methanol/acetonitrile/0.005 mol/L sodium acetate/acetic acid (300/300/400/14, v/v/v/v). The flow rate was 1.5 mL/min (Dohnal et al. 2013). Under these chromatographic conditions, the retention time of OTA for serum samples was about 7.1 min and for urine samples about 7.9 min. For OTA in serum, the LOD was 40 ng/L and LOQ was 100 ng/L. For OTA in the urine, the LOD was 1.0 ng/L and LOQ was 2 ng/L. The linear calibration curve was constructed by measurement of OTA peak areas of standard solutions in mobile phase with concentrations of 0.125 to 4.000 ng OTA/mL for serum analysis, and of 0.1 to 20 ng OTA/L for urine analysis. Blank samples were mobile phases. Each point of the calibration curve was measured in triplicate. The recoveries for OTA were 82–86% in the range of 0.5–1.0 μg/L (500–1000 ng/L) in spiked blood serum samples and 92.6–85.1% in the range of 20–50 ng/L in spiked urine samples. The average relative standard deviations of repeatability (RSDr) for OTA were 4.5% at 0.5 ng/mL (500 ng/L) and 1.5% at 1 ng/mL (1000 ng/L) for serum and 4.2% at 20 ng/L and 2% at 50 ng/L for urine.
CIT and DH-CIT extraction, detection and quantification
CIT and DH-CIT in urine were analysed by the validated method of Blaszkewicz et al. (2013) after extraction and cleanup with CitriTest® columns (Vicam provided by Ruttmann, Hamburg, Germany), with minor modifications. A mixture of 5 mL urine diluted with 5 mL of 1 mM acetic acid was loaded on a CitriTest® column; see Ali et al. (2015a, 2015b). CIT and DH-CIT in plasma were analysed by the method of Blaskewicz et al. (2013) and Ali et al. (2018). In short, for protein precipitation, 1 mL plasma was mixed with 1 mL acetonitrile (1/1, v/v) and then centrifuged at 9800×g for 3 min; 1 mL of the upper layer was transferred into a vial and evaporated to dryness under a gentle stream of nitrogen at a temperature of 40 °C. Then, the sample was reconstituted in 350 μL methanol, vortexed, and centrifuged at 9800×g for 3 min; the extract was filtered through a 0.45-μm pore size Teflon syringe filter (WICOM, Germany) before LC-MS/MS analysis.
Detection of CIT and DH-CIT was performed with a Varian 1200L Quadrupole MS/MS equipped with an electrospray ionization (ESI) source and a Prostar® Varian HPLC system and Varian MS Workstation version 6.9.1 data system (Agilent Technologies, Germany) after separation on a Nucleosil® 100-5 C18 HD column (125 × 3 mm, Macherey-Nagel, Düren, Germany). The mobile phase consisted of water containing 1 mmol/L ammonium formate and methanol containing 1 mmol/L ammonium formate. Instrumental settings and chromatographic conditions were identical with those used before for urine and plasma extract analyses (Ali et al. 2015a, 2015b; Ali et al. 2018). A gradient elution was performed, and the retention times of CIT and DH-CIT were 9.3 and 8.7 min, respectively.
The method was validated using spiked blank urine and plasma samples. Recoveries were 79% and 82% in the urine, and 82% and 84% in plasma, for CIT and DH-CIT, respectively. The LOD and LOQ were determined by an external calibration curve in the urine and plasma matrix. The LOD and LOQ were 0.02 ng/mL (20 ng/L) and 0.05 ng/mL (50 ng/L) for CIT, and those for DH-CIT were 0.05 ng/mL (50 ng/L) and 0.1 ng/mL (100 ng/L) in the urine matrix. In plasma samples, the LODs of CIT and DH-CIT were 0.07 ng/mL (70 ng/L) and 0.15 ng/mL (150 ng/L), respectively, and their LOQs were 0.15 ng/mL (150 ng/L) and 0.30 ng/mL (300 ng/L), respectively. Reproducibility was determined by inter-day assays on three different days at a level of 0.25 ng/mL (250 ng/L) in urine and 0.5 ng/mL (500 ng/L) in plasma for the analytes; the RSDr range was 4.2 to 7.4% for the analytes. Calibration curves for quantification were done by spiking urine and plasma matrix that showed no detectable analyte background.
Creatinine analysis in urines
Urinary creatinine was determined by the Jaffe reaction method with alkaline picrate at a wavelength of 520 nm using the spectrometer Cintra 101 (GBC Scientific Equipment Ltd., Australia). Creatinine levels were controlled by Lyphochek® Quantitative Urine Control, levels 1 and 2 (Bio-Rad, Prague, Czech Republic). Levels of OTA, CIT and DH-CIT in urines (ng/L) were then adjusted for creatinine content and expressed as nanograms per gram of creatinine.
OTA exposure calculation
The average OTA daily intake in patients with malignant neoplasms was calculated on the basis of OTA serum concentrations as done in previous assessments (e.g. Märtlbauer et al. 2009; Coronel et al. 2009; Duarte et al. 2011) by means of the Klaassen equation:
K0 = Clp × Cp/A and in the version K0 = 0.99 × Cp/0.5 = 1.97where K0 is the continuous dietary intake (ng/kg b.w./day), Clp is the plasma clearance (0.99 mL/kg b.w./day), Cp is the plasma OTA concentration (ng/mL) and A is the toxin bioavailability, estimated at 50%. We opted also to use the more conservative conversion factor of 1.97 (Miraglia et al. 1996), since this version of the Klaassen equation has resulted in a better match of biomarker-based intake assessments for OTA with estimates based on food analysis data (Märtlbauer et al. 2009).
where COTA is the OTA concentration measured in serum (ng/mL).
CIT exposure calculation
For CIT exposure assessment, the urine concentrations for both CIT and its main metabolite DH-CIT were summed up (“total CIT”) for each individual and then converted to CIT intake. It was calculated as follows (Degen et al. 2018):
where PDI is the provisional daily intake, C is the concentration measured in the urine sample, W is the standard body weight of 70 kg (EFSA 2012) and V is the average daily urine volume of 1.6 L excreted by adults. As for the assumption for V, one favours a higher i.e. conservative intake estimate, although the urine volume excreted by patients who are kept from drinking or eating 12 h before surgery was lower. The fraction excreted in the urine is the percentage of an oral CIT dose found in the urine within 24 h and set here to 40%, the median value in the study of Degen et al. (2018).
Statistical analysis
Obtained data were processed using the universal statistical software Statistica version 11 (StatSoft). The results as mean ± standard deviation, median and ranges are presented on the basis of descriptive analysis. The samples with OTA concentrations below the limit of detection (LOD) were calculated as one-half the detection limit for calculation of mean and median values (Hornung and Reed 1990).
Results
Biomarkers in blood and urine samples: OTA, CIT and DH-CIT
OTA was frequently detected in body fluids (serum 48%; urine 62%) from the patient cohort. OTA amounts measured in blood serum and urine are summarized in Table 2. The OTA serum concentrations ranged from 40 ng/L (LOD) to 830 ng/L, with a mean value 145 ± 213.8 ng/L, median 20 ng/L. OTA concentrations in the corresponding urines ranged from 1 ng/L (LOD) to 27.8 ng/L, with a mean value for all urines of 5.9 ± 5.97 ng/L, median 5.4 ng/L. OTA concentrations in both matrices are higher in the male than the smaller subgroup of female patients (Table 2), yet the differences did not reach statistical significance. This is also the case for creatinine-adjusted OTA levels in urine.
Determining OTA in blood and urine is very useful for a comparison with published data from other cohorts. Yet, biomarker analyses data in the two matrices of an individual are not necessarily strictly correlated with each other due to the rather complex kinetics of OTA in the human organisms. Figure 2 and Fig. 3 depict the OTA concentrations determined in serum and urine samples of all individuals. Patients with higher OTA serum amounts generally excreted more OTA aglycone, the unconjugated OTA form (which was analysed) in urine than those with lower circulating amounts of OTA.
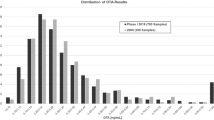
In blood and urine of the same cohort, CIT is detected in almost all patients. Table 3 summarizes the data. The CIT plasma concentrations of all 50 Czech patients ranged from 20 (LOD) to 182 ng/L, median of 51 ng/L, a mean value 61 ± 35 ng/L and similar concentrations in both subgroups of men and women. Due to a high LOD for DH-CIT in plasma (200 ng/L), the metabolite was not detected in any of the patient blood samples. CIT concentrations in urine ranged from 2 (LOD) to 87 ng/L, with a mean value for all patients of 16 ± 20 ng/L, median 8 ng/L and higher mean concentrations for the metabolite DH-CIT of 48 ± 35 ng/L, median 38.5 ng/L (for 100% of samples in a range of 6 to 160 ng/L), with similar amounts in males and females (see Table 3).
Figures 4 and 5 illustrate the variability in biomarker concentrations among this cohort for biomarkers measured in plasma and in urine samples of individuals. The biomarker pattern in both matrices, with higher CIT concentrations in blood than in urine of patients, and higher urinary levels of DH-CIT than CIT, resembles that observed in reference cohorts.
Exposure assessments for OTA and CIT
These data have been used to estimate the exposure to OTA and CIT of the patients before surgery, and have been compared to the tolerable intake (TDI) for OTA and CIT. Using the OTA serum concentrations of Czech patients, we calculate a probable daily intake, using a conversion factor of 1.97 for the Klaassen equation as applied in previous exposure assessments for this mycotoxin. The mean blood OTA concentrations of 145 ± 214 pg/mL (or ng/L) correspond to a mean daily dietary OTA intake for the entire cohort of 286 ± 421 pg/kg b.w/day (i.e. 0.29 ± 0.42 ng/kg b.w./day). This daily intake is lower than the TDI value which was set by several regulatory bodies for OTA.
For CIT exposure, the urine concentrations for CIT and its main metabolite DH-CIT were summed up (“Total CIT”) for each individual (see Fig. 4) and then converted to CIT intake as explained in “Materials and methods”. The probable daily CIT intake for the cohort is 3.5 ± 2.3 ng/kg b.w./day, with no significant difference between males and females. The estimated exposure is far lower than the “level of no concern for nephrotoxicity” (a provisional TDI) derived by EFSA (2012) for this mycotoxin.
Comparisons with healthy populations
Results of this first biomarker analysis for nephrotoxic mycotoxins in Czech patients with renal tumours are compared with data for OTA and CIT biomonitoring in reference cohorts; more details on the latter studies are provided in “Discussion”.
OTA concentrations both in urine and in serum of Czech patients in this study and the group representing the Czech healthy population—reference cohort (236 examined individuals; male/female, 45–60 years old, blood donors) (Ostry et al. 2010)—were compared by the independent sample t test. No statistically significant difference was observed (p > 0.05).
Comparisons of CIT and DH-CIT urinary concentrations were made by independent sample t test between Czech patients and those reported in a cohort of German healthy adults (23 males, 27 females) (Ali et al. 2015a), because similar data were not available in a healthy cohort in the Czech Republic. CIT and DH-CIT concentrations in urine of Czech patients were statistically significantly lower (p < 0.05) compared with the German control group, but no significant difference was observed in their blood levels.
Discussion
The aim of this collaborative study was to estimate the exposure of kidney cancer patients (clinical diagnoses: C64–C66) to two nephrotoxic mycotoxins (OTA and CIT) by sensitive targeted biomarker analyses in both blood and urine samples. As sample collection was made in hospital before surgery, the measured OTA and CIT biomarkers reflect only recent exposure but not the past exposure. Yet, analysis of paired blood and urine samples from patients allows to consider biomarker levels in both matrices and compare the outcome to studies in non-diseased cohorts (e.g. MacDonald et al. 2001; Ostry et al. 2010; Ali et al. 2015a). Table 4 summarizes data from some studies that used the same or very similar methodology as applied in the present investigation.
OTA biomarker concentrations in Czech kidney tumour patients and in other cohorts
For the Czech patients, the mean OTA serum concentration and the range are similar to those found in a large survey of serum samples obtained between 1994 and 2002 from healthy Czech blood donors (Malir et al. 2006), and from another more recent survey on healthy Czech persons (Ostry et al. 2010). The data for Czech adults are also similar to OTA values found in a large German study (Rosner et al. 2000) and a retrospective study of 102 serum samples from 36 healthy persons (Märtlbauer et al. 2009). Higher OTA mean blood plasma levels and ranges than in the Czech and German adults have been reported in a 1-month diet duplicate study carried out in the UK some years ago (MacDonald et al. 2001). This study analysed also unconjugated OTA in 24-h urines collected by the volunteers. OTA concentrations in urine were far lower than those measured in the blood plasma, yet showed a good correlation with dietary OTA intake of UK adults (Gilbert et al. 2001; MacDonald et al. 2001).
OTA levels now determined in urines from 50 Czech patients are close to the mean concentration and range were found previously for the healthy Czech population (Ostry et al. 2010). In the patient cohort, OTA concentrations in urine were also much lower than in blood. This is in line with data from the UK (Table 4) and further biomonitoring data in healthy persons (reviewed in Fromme et al. 2016; Malir et al. 2016; Ali et al. 2017).
The fact that both blood and urinary OTA levels in patients suffering from kidney cancer are not significantly different from the healthy Czech population or lower than in healthy persons from other countries is in line with the present knowledge on OTA kinetics. Only a small fraction of the circulating OTA is excreted in a given time, due to its pronounced binding to serum proteins (about 99%) which hinders its glomerular filtration (Gekle et al. 2005). The free (unbound) OTA fraction is filtered, but reabsorption of the non-ionized form along all nephron segments delays its elimination (Castegnaro et al. 2006; Ringot et al. 2006). The fraction of OTA bound to serum proteins constitutes a mobile OTA reserve that can be released as soon as the fraction of free OTA decreases, e.g. when more polar metabolites are formed and excreted (Pfohl-Leszkowicz and Manderville 2007; Ali et al. 2017). An increase in OTA blood concentrations after high intake can be compensated by increasing urinary OTA excretion, which brings the OTA concentration back to the former steady-state level in blood (Castegnaro et al. 2006; Pfohl-Leszkowicz et al. 2006). In patients with impaired renal function and decreased filtration capacity, one would expect an increase in OTA concentration in blood compared to healthy persons with a similar OTA intake (Duarte et al. 2011). Yet, this was not the case, except for 30% of patients having a low creatinine excretion, probably because the steady state was not reached.
Estimation of the OTA intake before surgery, based on OTA blood concentrations, is low with about 0.3 ng/kg b.w./day: This is about 10-fold lower than the most conservative limit value of 4 ng/kg b.w./day proposed by Health Canada for a negligible cancer risk intake (Kuiper-Goodman et al. 2010) and 50 times lower than the tolerable weekly intake (TWI) of 120 ng/kg b.w. proposed by EFSA (2006). OTA biomarker analysis in urine seems to better reflect short-term variations in OTA exposure of adults and children (Gilbert et al. 2001; Castegnaro et al. 2006; Muñoz et al. 2014). Whilst urines can be obtained by non-invasive sampling, one must keep in mind that only a very small fraction of the ingested OTA is excreted with urine, less than 3% within a day (Studer-Rohr et al. 2000; Degen 2016). Based on this information, the estimated daily intake is about 2.37 ng/kg b.w./day, which corresponds to half of the most conservative limit value for cancer risk.
Due to limited financial sources, the diet of the patients was not tested for OTA and CIT. But the dietary regimen (which can influence OTA and CIT levels) of all patients was assessed on the basis of a special questionnaire. There were no apparent differences in the consumption of OTA-containing foodstuffs in comparison to the referent Czech population (Ostry et al. 2015). As the average calculated OTA intake in the Czech Republic was about 3.9 ng/kg b.w./day (Ostry et al. 2015), the above urine OTA-based intake estimate is in accord with this value.
CIT biomarker concentrations in Czech kidney tumour patients and in other cohorts
In contrast with rather good databases on the dietary intake of certain mycotoxins such as aflatoxins or OTA, data on the occurrence of CIT in food commodities are still too limited to reliably estimate human exposure (EFSA 2012). Hence, there is a need to assess human exposure to CIT to enable a better characterization of related risks, e.g. by biomarker-based analysis of its intake (Degen et al. 2018). Recent studies that applied targeted methods for detection of CIT biomarkers revealed quite frequent exposure to this food contaminant in cohorts from different countries and also concurrent exposure to OTA (Pfohl-Leszkowicz 2009; Ali et al. 2015a; Ali et al. 2016a, 2016b; Ali et al. 2018). Yet, with biomarker analysis for CIT being more recently established, there are only few data compared to OTA data in European cohorts (Table 4).
The new results in plasma and urine samples from the Czech patients confirm dietary exposure to CIT. CIT was detected in 98% of blood plasma from 50 Czech patients in a similar, yet somewhat lower range of concentrations than those found in some healthy German volunteers (Blaszkewicz et al. 2013). Also in urines of the Czech patients, their CIT and DH-CIT levels indicate a lower exposure to this mycotoxin than in a cohort of healthy German adults (Ali et al. 2015a). This pertains to unadjusted concentrations (ng/L) as well as creatinine-adjusted biomarker levels in Czech and German urine samples. Average CIT biomarker levels in urines of Czech patients are significantly (p < 0.05) lower than those of German adults, but no significant difference exists between blood samples. The biomarker pattern in paired samples, with higher CIT concentrations in blood than in urine of patients, and higher urinary levels of DH-CIT than CIT, is similar to reference cohorts (Ali et al. 2015a, 2015b; Ali et al. 2018). A recent kinetic study in volunteers found that a high fraction (about 40%) of an ingested dose of CIT is excreted in the urine as the sum of CIT and its metabolite DH-CIT (‘total CIT’) within a day (Degen et al. 2018). This allows to estimate human dietary CIT exposure based on urine biomarker data, and compare it with the provisional tolerable daily intake (‘TDI’) proposed by the EFSA (2012). The CIT daily intake derived from urine analyses of the Czech patients is 3.5 ± 2.3 ng/kg bw/day; this corresponds to 1.8 ± 1.1% of the ‘TDI’ set for this mycotoxin whereas the German exposure is slightly higher, but nevertheless represents only 3.7 ± 3.0% of the ‘TDI’ (Degen et al. 2018).
Concluding remarks: Overall, the presented data indicate a frequent, but low dietary exposure to CIT and OTA, although we cannot exclude that higher exposures to nephrotoxic mycotoxins may have occurred in previous years in the Czech patient cohort. Biomarker-based intake estimates for CIT and OTA are well below the respective health-based guidance values. Thus, we consider combinatory effects, found in rodents or in vitro at rather high mycotoxin doses (see “Introduction”), to be of low concern for the present human exposure scenario. Due to the short half-life of CIT in human blood (about 9 h), CIT is unlikely to accumulate in the organism (Degen et al. 2018). In contrast, OTA has a rather long half-life in human blood (about 35 days) (Studer-Rohr et al. 2000), and accumulates in the kidneys. As discussed elsewhere, there is the possibility of OTA uptake in proximal tubules leading to accumulation in kidney target cells (Gekle et al. 2005; Mally 2012). An analysis of OTA in renal adenocarcinoma samples is thus of interest, also regarding the OTA ratio between kidney and serum. Tissue samples of the Czech tumour patient cohort could also provide a chance for tracing changes related to past exposures and for further research on other factors involved in this multifactorial disease.
References
Ali N, Blaszkewicz M, Degen GH (2015a) Occurrence of the mycotoxin citrinin and its metabolite dihydrocitrinone in urines of German adults. Arch Toxicol 89:573–578. https://doi.org/10.1007/s00204-014-1363-y
Ali N, Blaszkewicz M, Mohanto NC, Rahman M, Alim A, Hossain K, Degen GH (2015b) First results on analysis of citrinin biomarkers in urines from two cohorts in Bangladesh. Mycotoxin Res 31:9–16. https://doi.org/10.1007/s12550-014-0217-z
Ali N, Blaszkewicz M, Alim A, Hossain K, Degen GH (2016a) Urinary biomarkers of ochratoxin A and citrinin exposure in two Bangladeshi cohorts: follow-up study on regional and seasonal influences. Arch Toxicol 90:2683–2697. https://doi.org/10.1007/s00204-015-1654-y
Ali N, Blaszkewicz M, Manirujjaman M, Degen GH (2016b) Biomonitoring of concurrent exposure to ochratoxin A and citrinin in pregnant women in Bangladesh. Mycotoxin Res 32:163–172. https://doi.org/10.1007/s12550-016-0251-0
Ali N, Muñoz K, Degen GH (2017) Ochratoxin A and its metabolites in urines of German adults – an assessment of variables in biomarker analysis. Toxicol Lett 275:19–26. https://doi.org/10.1016/j.toxlet.2017.04.013
Ali N, Hossain K, Degen GH (2018) Blood plasma biomarkers of citrinin and ochratoxin A exposure in young adults in Bangladesh. Mycotoxin Res 34:59–67. https://doi.org/10.1007/s12550-017-0299-5
Blaszkewicz M, Muñoz K, Degen GH (2013) Methods for analysis of citrinin in human blood and urine. Arch Toxicol 87:1087–1094. https://doi.org/10.1007/s00204-013-1010-z
Castegnaro M, Canadas D, Vrabcheva T, Petkova-Bocharova T, Chernozemsky I, Pfohl-Leszkowicz A (2006) Balkan endemic nephropathy: role of ochratoxins A through biomarkers. Mol Nutr Food Res 50:519–529. https://doi.org/10.1002/mnfr.200500182
Chan C-K, Liu Y, Pavlovic NM, Chan W (2018) Etiology of Balkan endemic nephropathy: an update on aristolochic acids exposure mechanisms. Chem Res Toxicol 31:1109–1110. https://doi.org/10.1021/acs.chemrestox.8b00291
Chow WH, Dong LM, Devesa SS (2010) Epidemiology and risk factors for kidney cancer. Nat Rev Urol 7:245–257. https://doi.org/10.1038/nrurol.2010.46
Coronel MB, Sanchiz A, Ramos J, Marin S (2009) Assessment of the exposure to ochratoxin A in the province of Lleida, Spain. Food Chem Toxicol 47:2847–2852. https://doi.org/10.1016/j.fct.2009.09.005
Degen GH (2016) Are we ready to estimate daily ochratoxin A intake based on urinary concentrations? Environ Int 97:254–255. https://doi.org/10.1016/j.envint.2015.10.010
Degen GH, Ali N, Gundert-Remy U (2018) Preliminary data on citrinin kinetics in humans and their use to estimate citrinin exposure based on biomarkers. Toxicol Lett 282:43–48. https://doi.org/10.1016/j.toxlet.2017.10.006
Dohnal V, Dvorak V, Malir F, Ostry V, Roubal T (2013) A comparison of ELISA and HPLC methods for determination of ochratoxin A in human blood serum in the Czech Republic. Food Chem Toxicol 62:427–431. https://doi.org/10.1016/j.fct.2013.09.010
Duarte SC, Pena A, Lino CM (2011) Human ochratoxin A biomarkers–from exposure to effect. Crit Rev Toxicol 41:187–212. https://doi.org/10.3109/10408444.2010.529103
Dusek L, Muzik J, Kubasek M, Koptikova J, Zaloudik J, Vyzula R (2017) Epidemiology of malignant tumours in the Czech Republic. Available online: http://www.svod.cz/?sec=aktuality&lang=en (accessed on 29 June 2018)
European Food Safety Authority [EFSA] (2006) Opinion of the scientific panel on contaminants in the food chain on request from the commission related to ochratoxin A in food. EFSA J 365:1–56
European Food Safety Authority [EFSA] (2012) Scientific opinion on the risks for public and animal health related to the presence of citrinin in food and feed. EFSA J 10:2605–2687 Available online: www.efsa.europa.eu/efsajournal (accessed on 25 June 2018)
Föllmann W, Behm C, Degen GH (2014) Toxicity of the mycotoxin citrinin and its metabolite dihydrocitrinone and mixtures of citrinin and ochratoxin A in vitro. Arch Toxicol 88:1097–1107. https://doi.org/10.1007/s00204-014-1216-8
Fromme H, Gareis M, Völkel W, Gottschalk C (2016) Overall internal exposure to mycotoxins and their occurrence in occupational and residential settings. Int J Hyg Environ Health 219(2):143–165. https://doi.org/10.1016/j.ijheh.2015.11.004
Gekle M, Sauvant C, Schwerdt G (2005) Ochratoxin A at nanomolar concentrations: a signal modulator in renal cells. Mol Nutr Food Res 49:118–130. https://doi.org/10.1002/mnfr.200400062
Gilbert J, Brereton P, MacDonald S (2001) Assessment of dietary exposure to ochratoxin A in the UK using a duplicate diet approach and analysis of urine and plasma samples. Food Addit Contam 18:1088–1093. https://doi.org/10.1080/02652030110070030
Grollman AP, Jelakovic B (2007) Role of environmental toxins in endemic (Balkan) nephropathy. J Am Soc Nephrol 18:2817–2823. https://doi.org/10.1681/ASN.2007050537
Hornung RW, Reed LD (1990) Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg 5:46–51. https://doi.org/10.1080/1047322X.1990.10389587
Koch-Institut R (2017) Krebs in Deutschland für 2013/2014. Robert Koch-Institut, Berlin available online: https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/krebs_in_deutschland_node.html
Kommission Humanbiomonitoring des Umweltbundesamtes (2005) Normierung von Stoffgehalten in Urin - Kreatinin. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 48:616–618. https://doi.org/10.1007/s00103-005-1029-2
Kuiper-Goodman T, Hilts C, Billiard SM, Kiparissis Y, Richard ID, Hayward S (2010) Health risk assessment of ochratoxin A for all age-sex strata in a market economy. Food Addit Contam Part A 27:212–240. https://doi.org/10.1080/02652030903013278
MacDonald SJ, Langton S, Brereton PA (2001) Assessment of human exposure to ochratoxin A in the UK-relationship between dietary intake and plasma and urine levels. In: de Koe WJ, Samson RA, van Egmond HP, Gilbert J, Sabino M (eds) Mycotoxins and Phycotoxins in Perspective at the Turn of the Millenium. Ponsen and Looyen, Wageningen, pp 181–188 ISBN 90–9014801-9
Malir F, Ostry V, Grosse Y, Roubal T, Skarkova J, Ruprich J (2006) Monitoring the mycotoxins in food and their biomarkers in the Czech Republic. Mol Nutr Food Res 50:513–518. https://doi.org/10.1002/mnfr.200500175
Malir F, Ostry V, Pfohl-Leszkowicz A, Roubal T (2012) Ochratoxin A exposure biomarkers in the Czech Republic and comparison with foreign countries. Biomarkers 17:577–589. https://doi.org/10.3109/1354750X.2012.692392
Malir F, Ostry V, Pfohl-Leszkowicz A, Malir J, Toman J (2016) Ochratoxin A: 50 years of research. Toxins 8:1–49. https://doi.org/10.3390/toxins8070191
Mally A (2012) Ochratoxin A and mitotic disruption: mode of action analysis of renal tumor formation by ochratoxin A. Toxicol Sci 127:315–330. https://doi.org/10.1093/toxsci/kfs105
Manderville RA, Pfohl-Leszkowicz A (2008) Bioactivation and DNA adduction as a rationale for ochratoxin A carcinogenesis. World Mycotoxin J 1:357–367. https://doi.org/10.3920/WMJ2008.x039
Märtlbauer E, Usleber E, Dietrich R, Schneider E (2009) Ochratoxin A in human blood serum- retrospective long-term data. Mycotoxin Res 25:75–186. https://doi.org/10.1007/s12550-009-0025-z
Miraglia M, Brera C, Colatosti M (1996) Application of biomarkers to assessment of risk to human health from exposure to mycotoxins. Microchem J 54:472–477. https://doi.org/10.1006/mchj.1996.0124
Muñoz K, Blaszkewicz M, Campos V, Vega M, Degen GH (2014) Exposure of infants to ochratoxin A with breast milk. Arch Toxicol 88:837–846. https://doi.org/10.1007/s00204-013-1168-4
Ostry V, Skarkova J, Malir F, Ruprich J (2010) An occurrence of ochratoxin A, a biomarker of dietary exposure, in human biological materials. In: Mykotoxíny 2010, 14–15 October 2010. Prague, Czech Republic. Proceedings, 32–40. ISBN: 978-80-7080-764-4
Ostry V, Malir F, Ruprich J (2013) Producers and important dietary sources of ochratoxin A and citrinin. Toxins 5:1574–1586. https://doi.org/10.3390/toxins5091574
Ostry V, Malir F, Dofkova M, Skarkova J, Pfohl-Leszkowicz A, Ruprich J (2015) Ochratoxin A dietary exposure of ten population groups in the Czech Republic: comparison with data over the world. Toxins 7:3608–3635. https://doi.org/10.3390/toxins7093608
Peraica M, Domijan AM, Sarić M (2008) Mycotoxic and aristolochic acid theories of the development of endemic nephropathy. Arh Hig Rada Toksikol 59:59–65. https://doi.org/10.2478/10004-1254-59-2008-1865
Pesch B, Haerting J, Ranft U, Klimpel A, Oelschlägel B, Schill W (2000) Occupational risk factors for renal cell carcinoma: agent-specific results from a case-control study in Germany. MURC Study Group Multicenter urothelial and renal cancer study. Int J Epidemiol 29:1014–1024
Pfohl-Leszkowicz A (2009) Ochratoxin A and aristolochic acid in the nephropathies and associated urothelial tract tumours development. Arh Hig Rada Toksikol 60:465–483. https://doi.org/10.2478/10004-1254-60-2009-2000
Pfohl-Leszkowicz A, Manderville RA (2007) Ochratoxin A: an overview on toxicity and carcinogenicity in animals and humans. Mol Nutr Food Res 51:61–99. https://doi.org/10.1002/mnfr.200600137
Pfohl-Leszkowicz A, Petkova-Bocharova T, Chernozemsky IN, Castegnaro M (2002) Balkan endemic nephropathy and the associated urinary tract tumours: review on etiological causes, potential role of mycotoxins. Food Addit Contam 19:282–302. https://doi.org/10.1080/02652030110079815
Pfohl-Leszkowicz A, Vrabcheva T, Petkova-Bocharova T, Garren L, Grosso F, Nikolov I, Dragacci S, Chernozemsky IN, Castegnaro M (2006) Analysis of ochratoxin A in serum, urine and food consumed by inhabitants from an area with Balkan endemic nephropathy: a one month follow up study. In: Njapau H, Trujillio S, Van Egmond HP, Park DL editors. Mycotoxins and Phycotoxins. Proceeding of the XIth International IUPAC Symposium on Mycotoxins and Phycotoxins, May 17–21, 2004, Bethesda, Maryland, USA: Wageningen Academic Publishers, 217–224
Pfohl-Leszkowicz A, Moliniè A, Tozlovanu M, Manderville RA (2008) Combined toxic effects of ochratoxin A and citrinin in vitro and in vivo. In: Siantar DP, Trucksess MW, Scott PM, Herman EM (eds) Food contaminants: mycotoxins & food allergens, ACS Symposium series, vol 1001. American Chemical Society, Washington, DC, pp 56–80. https://doi.org/10.1021/bk-2008-1001.ch003
Radford R, Frain H, Ryan MP, Slattery C, McMorrow T (2013) Mechanisms of chemical carcinogenesis in the kidneys. Int J Mol Sci 14:19416–19433. https://doi.org/10.3390/ijms141019416
Reaume MN, Graham GE, Tomiak E, Kamel-Reid S, Jewett MAS, Bjarnason GA, Bleis N, Care M, Drachenberg D, Gedye C, Grant R, Heng DYC, Kapoor A, Kollmannsberger C, Lattouf JB, Maher ER, Pause A, Ruether D, Soulieres D, Tanguay S, Turcotte S, Violette PD, Lori W, Basiuk J, Pautler SE (2013) Canadian guideline on genetic screening for hereditary renal cell cancers. Can Urol Assoc J 77:319–323. https://doi.org/10.5489/cuaj.1496
Reinhard H, Zimmerli B (1999) Reversed-phase liquid chromatographic behaviour of the mycotoxins citrinin and ochratoxin A. J Chromatogr A 862:147–159
Ringot D, Chango A, Schneider YJ, Larondelle Y (2006) Toxicokinetics and toxicodynamics of ochratoxin A. Chem Biol Interact 159:18–46. https://doi.org/10.1016/j.cbi.2005.10.106
Rosner H, Rohrmann B, Peiker G (2000) Ochratoxin A in human serum. Arch Leb 51:104–107
Sanfilippo KM, McTigue KM, Fidler CJ, Neaton JD, Chang Y, Fried LF, Liu S, Kuller LH (2014) Hypertension and obesity and the risk of kidney cancer in 2 large cohorts of US men and women. Hypertension 63:934–941. https://doi.org/10.1161/HYPERTENSIONAHA.113.02953
Schmidt LS, Linehan WM (2016) Genetic predisposition to kidney cancer. Semin Oncol 43:566–574. https://doi.org/10.1053/j.seminocol.2016.09.001
Stiborova M, Arlt VM, Schmeiser HH (2016) Balkan endemic nephropathy: an update on its aetiology. Arch Toxicol 90:2595–2615. https://doi.org/10.1007/s00204-016-1819-3
Studer-Rohr I, Schlatter J, Dietrich DR (2000) Kinetic parameters and intraindividual fluctuations of ochratoxin A plasma levels in humans. Arch Toxicol 74:499–510. https://doi.org/10.1007/s002040000157
Tesar V, Viklicky O, Bartonickova K, Boucek P, Bürgelova M, Certikova-Chabova V, Dusilova Sulkova S, Honsova E, Hruskova Z, Jancova E, Lyerova L, Matejovic M, Monhart V, Parikova A, Reiterova J, Rychlik I, Rysava R, Vachek J (2015) Klinická nefrologie (Clinical nephrology). Grada Publishing, Praha ISBN: 978–80–247-4367-7
Turner PC, Flannery B, Isitt C, Ali M, Pestka J (2012) The role of biomarkers in evaluating human health concerns from fungal contaminants. Nutr Res Rev 25:162–175. https://doi.org/10.1017/S095442241200008X
Zimmerli B, Dick R (1995) Determination of ochratoxin A at the ppt level in human blood, serum, milk and some foodstuffs by high-performance liquid chromatography with enhanced fluorescence detection and immunoaffinity column cleanup: methodology and Swiss data. J Chromatogr B 666:85–99. https://doi.org/10.1016/0378-4347(94)00569-Q
Funding
This study received financial support from the specific research projects (no. 2118/2015; 2113/2016; 2105/2017) from University of Hradec Kralove, Czech Republic, and from the project of Ministry of Health, Czech Republic, conceptual development of research organization (National Institute of Public Health—NIPH, IN 75010330).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study design was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Conflict of interest
The authors confirm that there are no conflicts of interest associated with this publication.
Ethical approval
Approval for the biomonitoring study protocol was obtained from the Ethics Commission of the University Teaching Hospital, Sokolska 581, CZ–500 05 Hradec Kralove (Reg. No. 201406 S02P). Written informed consent was obtained from all patients included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malir, F., Louda, M., Ostry, V. et al. Analyses of biomarkers of exposure to nephrotoxic mycotoxins in a cohort of patients with renal tumours. Mycotoxin Res 35, 391–403 (2019). https://doi.org/10.1007/s12550-019-00365-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12550-019-00365-9