Abstract
Background
Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in children. With the gradual expansion of the incidence of JIA in the population, the pathogenesis and treatment of JIA were further explored and analyzed, and JIA has achieved some success in drug therapy.
Data sources
A systemic literature search was conducted on PubMed, Cochrane Library, EMBASE, ISI Web of Science, the US National Institutes of Health Ongoing Trials Register, and the EU Clinical Trials Register. Through the searching of clinical trials of JIA in recent years, we summarized the progress of the clinical treatment of JIA.
Results
The main treatment drugs for JIA include non-steroidal anti-inflammatory drugs, glucocorticoids, disease-modifying antirheumatic drugs and biological agents. So far, a variety of biological agents targeting the cytokines and receptors involved in its pathogenesis have been gradually approved for JIA in many countries. The application of biological agents in JIA showed good efficacy and safety, bringing unprecedented experience to children and adolescents with JIA.
Conclusions
The potential and advantages of biologic agents in the treatment of JIA are significant, and the application of biologic agents in the treatment of JIA will be more and more common.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis (JIA) is a systemic inflammatory disease that occurs in children under the age of 16 and lasts for more than 6 weeks [1]. JIA is a common autoimmune disease with the highest rate of childhood disability and is associated with systemic multisystem involvement [2]. JIA disease is based on chronic inflammation of the synovium and connective tissue of the joint, which can last for weeks, months or even years [3]. Its pathogenesis is still unclear [4]. JIA may not be a single disease, but a syndrome caused by different etiologies [5, 6]. The combination of individual genetic susceptibility, environmental factors (possibly infection) and immunological factors leads to disease, that is, infection induces abnormal immune inflammatory responses in susceptible people, resulting in autoimmune tissue damage or degeneration [7, 8]. The pathologic features of JIA are chronic synovitis, formation of vascular whiskers, and destruction of cartilage and bone tissue [9, 10]. The affected synovial tissue is swollen and hyperemic, and there are a large number of synovial cells in the synovial tissue, and a variety of inflammatory cell infiltration [11].
Children with JIA may have arthritis and other systemic manifestations, including flaccid fever, rash with fever, enlargement of liver, spleen and lymph nodes, and serositis [12, 13]. Treatment of JIA includes drug, surgical and psychological rehabilitation, which requires multidisciplinary collaboration and individualized treatment to meet the needs of each child [14, 15]. Evaluation of the disease is the basis for the selection of treatment plan and drug dose [16]. It is necessary to evaluate the effect ratio of the selected drugs and doses to the children and seek the most appropriate drugs and dose [17]. The goals of JIA treatment are to maximize the protection of children’s daily functional activities, relieve discomfort, prevent, or reduce organ damage, and to avoid or minimize drug toxicity [18]. JIA is a chronic disease that cannot be cured by all current treatments [19]. The importance of early treatment of JIA, the necessity of early combination of disease-modifying antirheumatic drugs (DMARDs) in addition to non-steroidal anti-inflammatory drugs (NSAIDs), and the effectiveness of cytokine acting agents have become a consensus among pediatric clinical rheumatologists [20, 21].
In JIA children with fever as the main symptom, the condition is complex. In clinical treatment and personal care, joint, heart, lung, blood and nervous system should be evaluated. Clinical treatment and nursing should be based on the severity of systemic symptoms, the number of active arthritis and adverse prognosis in children with JIA, to evaluate the safety, efficacy, tolerance, treatment cost and acceptance of children and their families, and formulate the corresponding treatment plan. With the development of JIA treatment technology, the treatment plan is also gradually personalized, pediatricians can also correctly select the appropriate treatment plan for patients. Therefore, a systemic literature search was conducted on PubMed, Cochrane Library, EMBASE, ISI Web of Science, the U.S. National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www. clinicaltrials.gov), and the EU Clinical Trials Register (www.clinicaltrialsregister.eu). Through the searching of the ongoing and published clinical trials of JIA in recent years, we summarized the progress of the clinical treatment of JIA, hoping to provide supporting materials for the treatment of JIA.
Nonsteroidal anti-inflammatory drugs
Although the treatment of JIA has entered the era of biological targeted therapy, NSAIDs drugs are still indispensable drugs to alleviate the joint symptoms of JIA patients [22]. NSAIDs could reduce joint pain, swelling, stiffness and fever, but they do not ease or prevent joint destruction [23]. NSAIDs are analgesic at low doses and anti-inflammatory at high doses [24]. The pain was relieved within 1–3 days of initial treatment, and the symptoms improved significantly within 3 months [25]. The incidence of gastrointestinal adverse reactions with cyclooxygenase-2 (COX-2) selective inhibitors such as celecoxib and rofecoxib is lower than that with traditional NSAIDs such as naproxen and ibuprofen, while the combination of glucocorticoid, leflunomide (LEF) and methotrexate (MTX) could increase the incidence of gastrointestinal injury [26]. The incidence of adverse cardiovascular reactions caused by NSAIDs depends on the degree of selective inhibition of COX-2 by drugs [27]. The U.S. Food and Drug Administration (FDA) have required that instructions for all NSAIDs should include a warning about the risk of serious cardiovascular events because of their adverse effects on cardiovascular events [28].
Glucocorticoid
Glucocorticoid is the most effective anti-inflammatory drug, which can rapidly reduce joint inflammation and systemic reactions [29]. However, the usage of glucocorticoid is limited due to its obvious side effects and inability to prevent destructive joint damage, unable to alleviate the disease, and unable to change the course and outcome of the disease [30, 31]. The administration route and dose of glucocorticoid are determined according to the clinical classification and severity of the disease [32]. In severe clinical symptoms, when the clinical efficacy of DMARDs is not well, the lowest effective dose of glucocorticoid can quickly relieve the disease [33].
Glucocorticoids are necessary when systemic juvenile idiopathic arthritis (sJIA) fails to be treated with NSAIDs or life-threatening complications such as severe anemia, pericarditis, and macrophage activation syndrome (MAS) occur. Prednisone is an oral glucocorticoid commonly used in childhood because its short half-life minimizes toxicity. The dosage is 1–2 mg/kg/day (maximum dose: 60 mg), generally dividing into one or two or three times, and the standard treatment is daily rather than every other day. Taking glucocorticoids after breakfast is more in line with the circadian rhythm of cortisol. The best life-threatening administration for children with sJIA was methylprednisolone at 30 mg/kg/day (maximum dose: 1 g) for 3 consecutive days, which rapidly controlled systemic symptoms of the disease and achieved complete remission in 55% of patients, and could be repeated in subsequent weeks depending on disease activity if necessary [34]. For the oligoarticular JIA, polyarticular JIA (rheumatoid factor negative), polyarticular JIA (rheumatoid factor positive), psoriatic arthritis and enthesitis-related arthritis with non-inflammatory bowel disease, it is generally not recommended to use glucocorticoids throughout the body, because it is not conducive to prevent the progress of bone erosion, but also increase the corresponding adverse drug reactions. Topical glucocorticoids are mainly used for active synovitis, and are mainly used to control inflammation of only one or more joints without systemic symptoms, including hip, knee, ankle, subtalar joint, wrist, interphalangeal joint, and temporomandibular joint. Triamcinolone acetonide is the best option, the effect of which can last for a long time and can quickly relieve pain or dysfunction [35]. JIA patients with ocular involvement can be treated with external glucocorticoids and dilatation agents.
Disease-modifying antirheumatic drugs
NSAIDs alone cannot alleviate or prevent the progression of JIA disease, but combined treatment with DMARDs can stabilize the disease and reduce joint destruction and disability rate. The commonly used drugs are MTX, sulfasalazine (SSZ), LEF, cyclophosphamide (CTX) and so on.
Methotrexate
MTX, a folic acid blocker, is widely used in the treatment of JIA. MTX is a long-acting drug that can be given orally, subcutaneously, and intramuscularly with less side effects, which can significantly improve the process of JIA. MTX has anti-inflammatory effects by inhibiting interleukin (IL)-1 production and many cell functions [36]. The dosage regimen of MTX is 10–15 mg/m2, once a week. Most patients have treatment response 2–3 weeks after the treatment of MTX. The American College of Rheumatology (ACR) guidelines recommend MTX as initial therapy for JIA patients with high disease activity and poor prognosis [37]. A single-center, questionnaire-based assessment of MTX efficacy and tolerability was conducted in 126 children with JIA followed up for more than 6 months. The study found that 83 of 126 (65.9%) children responded to treatment, and for JIA patients with MTX intolerance, switching from oral to subcutaneous MTX may increase response rates [38]. A regressive cohort study from Italy showed that MTX monotherapy for JIA-associated uveitis (JIA-U), while effective in the early stage, was associated with long-term poor control of JIA-U, with new ocular complications in a quarter of patients [39]. Based on these findings, long-term MTX monotherapy does not fully control the course of uveitis. Therefore, they suggest that patients who develop uveitis despite ongoing MTX therapy should be treated with biological agent at the first onset of uveitis. In patients newly treated with MTX, uveitis should be carefully observed over time, even when MTX initially responds well.
Sulfasalazine
SSZ inhibits the activity of inflammatory cells by inhibiting the key enzyme in the process of purine synthesis, then increasing release of adenosine in cells. The released adenosine then binds to the A2 adenosine receptor on the surface of inflammatory cells [40, 41]. SSZ can inhibit the release of many inflammatory cytokines, such as IL-1, IL-6, and tumor necrosis factor (TNF)-α [42, 43]. SSZ can also reduce the chemotaxis and proliferation of endothelial cells, decrease vascular proliferation, cut down the expression of nuclear factor kappa-B (NF-κB) ligand and increase the expression of osteoprotegerin, thereby inhibiting osteoclast formation and protecting joint bone [44]. The dosage usually is 30–50 mg/kg/day (maximum dose: 2 g), dividing into 2–3 times. In 2015, the Pediatric Committee of the Canadian Rheumatology Association suggested that SSZ might play a role in the treatment of children with appendicitis-associated arthritis [45]. A randomized controlled study of SSZ versus placebo was conducted to test its efficacy and safety in patients with oligopoly and polyarticular JIA [46]. This trial showed that SSZ was superior to placebo in inhibiting disease activity. van Rossum et al. [47] conducted a long-term follow-up result confirming that the health status of patients in SSZ group was better than that in placebo group, indicating that SSZ has a beneficial effect on JIA for many years. Another clinical study found that SSZ was more effective than placebo in inhibiting joint inflammation and reducing radiologically visible joint injury in children with JIA [48].
Leflunomide
LEF is an isozole immunomodulator with anti-proliferative activity [49]. LEF inhibits T and B cell proliferation by inhibiting dihydrolactate dehydrogenase in the body, resulting in reduced synthesis of DNA and RNA [50]. In vitro studies indicated that it inhibited the proliferation of T lymphocytes and B lymphocytes directly by inhibiting the IL-2-mediated process and pyrimidine biosynthesis [51]. In addition, it can also inhibit the activity of tyrosine kinase, reduce the activation of NF-κB and the expression of cytokines, as well as decrease the production and secretion of antigen–antibody and the production of nitric oxide, thus producing anti-inflammatory effects [52]. The routine dosage of LEF is: body weight < 20 kg, 10 mg oral every other day; 20–40 kg, 10 mg per day; > 40 kg, 10–20 mg, oral once a day. A recent retrospective clinical study showed that LEF may be an effective treatment for patients with MTX intolerance or toxicity [53]. It is safe when used concomitantly with biologic agents and may reduce the demand for biological agents in the case of low disease activity of JIA.
Cyclophosphamide
CTX is a cytotoxic drug, which has a good effect on killing lymphocytes [54]. It can reduce the number of T cells and B lymphocytes, inhibit cellular and humoral immune responses, and reduce the production of antibodies [55]. To a certain extent, CTX can reduce the expression of inflammatory pathway proteins and downstream inflammatory factors, decrease the infiltration of neutrophils in the lung, alleviate the pulmonary inflammatory response in JIA-related interstitial pneumonia, and delay pulmonary interstitial fibrosis. de Castro et al. [56] reported that CTX combined with glucocorticoid was effective in the treatment of 4 children with refractory JIA. Another study found that 4 patients were treated with CTX combined with glucocorticoid, and 3 patients achieved clinical remission [57].
Cyclosporine A (CsA)
CsA is a potent immunosuppressant, which can specifically inhibit the production of IL-2 by T lymphocytes and play a selective role in cellular immunosuppression [58]. Compared with other immunosuppressants, CsA has the advantage of fast acting, and is often used in the treatment of patients with severe JIA [59]. In 2021, Chinese Regulations for the Diagnosis and Treatment of Rheumatic Diseases (in press) proposed that cyclosporine can be used to treat patients with hormone resistance of JIA complicated with MAS. The usual dose is 4–6 mg/kg/day, and attention should be paid to detect its blood concentration. Ruperto et al. [60] investigated the efficacy and safety of JIA patients treated with CsA. A small number of patients (9%, 13/151) were found to have significantly improved clinical presentation. In addition, another study found that CsA can effectively achieve and maintain remission in 75% of patients with hormone dependent sJIA who often relapse. Patients with systemic symptoms such as fever and rash improved much better than with articular inflammation. Moreover, for drug-resistant sJIA patients who often relapse due to systemic symptoms, CsA is much cheaper than biological agents, and will not induce obvious side effects [61]. The most commonly reported side effects include hirsutism, elevated serum creatinine levels, hypertension, gastrointestinal reactions, and gingival hyperplasia.
Thalidomide (Thal)
Thal is a synthetic derivative of glutamate, which cannot only reduce the content of cluster of differentiation (CD) 4+ cells, but also increase the content of CD8+ cells, and play a specific immunomodulatory role by reducing the ratio of CD4 cells to CD8 cells [62]. In addition, Thal could the transition from helper T cell (Th) 1 response to Th2 response. Thal can effectively relieve joint swelling and control body temperature in children with sJIA. The usual dosage is 1.5–2.0 mg/kg/day, dividing into two oral doses. Sathe et al. [63] used Thal to treat three children with JIA. After treatment, the patients all had significant symptom improvement. In the acute phase, the inflammatory markers [e.g., hemoglobin, total count, platelet and erythrocyte sedimentation rate (ESR)] returned to normal, the average joint count decreased, and the clinical manifestation and growth status improved obviously. Another study used Thal to treat 13 children with systemic disease of JIA [64]. After 6 months of treatment, these children had reduced hormone use, and their ESR was significantly lower, hemoglobin levels are elevated, and arthritis scores were significantly higher.
Hydroxychloroquine (HCQ)
Similar to chloroquine, HCQ works against malaria by preventing heme from polymerizing into plasmodium pigments [65]. HCQ inhibits T cell proliferation, reduces pro-inflammatory cytokine production, and prevents toll-like receptor and nucleic acid ligand interactions, thereby reducing innate immune activation [66]. If biologics are not available, HCQ in combination with MTX can be considered [67]. The routine dosage is 4–6 mg/kg/day (maximum dose: 0.2 g), dividing into 1 to 2 oral doses. Clinical common side effects of HCQ drugs including gastrointestinal reactions, skin damage, and ocular adjustment reflex disorder, which usually disappear after drug withdrawal [68].
Biological agents
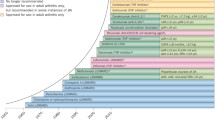
Conventional therapy for JIA is less effective and has permanent joint damage, so new treatment options are urgently needed [69]. Despite the use of early intensive therapy in many patients over the past 20 years, chronic active disease persists into adulthood [70]. Biological agents are a newly developed class of drugs, which have highly effective and well-tolerated treatment, including TNF-α inhibitors, IL-1 receptor antagonists, IL-6 receptor antagonists, anti-T cell-specific inhibitors, CD20 monoclonal antibodies, and histone deacetylase inhibitors. [71]. Rational use of biologics should be considered for any child with JIA who fails to respond to long-acting drug therapy for 3–6 months [72]. The target and effect size of these biological agents are summarized in Table 1.
Tumor necrosis factor-α inhibitors
TNF-α plays a mediating role in inflammation and immune regulation by activating lymphocytes, releasing inflammatory cytokines IL-1 and IL-6, prostaglandin, and metalloproteinase, promoting angiogenesis and regulating adhesion factors [73,74,75]. It increases both in plasma and synovial fluid of JIA and plays an important role in the pathogenesis of JIA [76]. Therefore, anti-TNF-α therapy is meaningful. In 2019, the ACR also recommended the use of TNF inhibitors instead of MTX or SSZ conditionally for children and adolescents with active JIA, despite the treatment of NSAIDs [77]. The drugs include etanercept, infliximab and adalimumab.
Etanercept
Etanercept, a soluble recombinant human TNF-α receptor antagonist, is the first biological agent to be used for the treatment of JIA. It reduces the level of TNF-α by forming a macromolecular complex with TNF-α and plays an important role in controlling inflammation and blocking disease progression [78]. Etanercept was approved by FDA in 1999 for JIA treatment in children 2 years and older. In March 2010, it was approved to be imported and marketed in China. The current recommended dosage in China is 0.8 mg/kg per week, given subcutaneously in 1–2 times, with a total dose of no more than 50 mg per week. Last year, a consensus of experts from Hong Kong, China recommended etanercept for JIA patients with psoriatic arthritis more than 12 years after onset [79]. A prospective clinical study found that etanercept and adalimumab did not significantly increase the risk of malignancy compared with MTX. Patients treated with etanercept alone were more likely to develop inflammatory bowel disease or uveitis than treated with etanercept combined with MTX or MTX alone [80]. It is generally not appropriate for JIA patients with systemic seizures because different pro-inflammatory cytokines play key roles in the pathogenesis of the disease. A cross-sectional and retrospective study showed that about half of children with nonsystematic JIA had complete remission under etanercept treatment [81]. Overall, the drug was well tolerated because only a quarter of patients had clinically significant adverse events, and less than 10% of patients stopped treatment due to toxicity. The most common adverse events were uveitis, infection, injection site reaction, neuropsychiatric disease, and gastrointestinal reaction [82].
Infliximab
Infliximab is a human/mouse chimeric monoclonal antibody against TNF-α [83]. It binds to TNF receptors on the cell surface, destroys TNF-α producing cells through complement mediated cytotoxicity, and exerts anti-inflammatory effects by decreasing serum IL-6, myeloperoxidase, and soluble adhesion molecules [84]. The usual dosage of this drug is 3–6 mg/kg, 0, 2, 6 weeks, and then every 8 weeks intravenously. A case-series study reported significant improvements in ESR and active joint count in 40 children with JIA treated with infliximab and suggested that the drug should be given as early as possible in clinical treatment [85]. The research of Lahdenne et al. [86] points out that infliximab can significantly improve the joint swelling and pain of children with JIA and reduce ESR. Adverse reactions included infusion, chest pain, dyspnea and urticaria. Another randomized controlled study found significant reductions in IL-6, intercellular cell adhesion molecule-1, matrix metalloproteinase-3, and C-reactive protein (CRP) levels in children with JIA after given infliximab compared with placebo [87].
Adalimumab
Adalimumab, a humanized monoclonal antibody against TNF-α, specifically blocks its interaction with TNF receptors on the surface of P55 and P75 cells, which are receptors expressed on the surface of chondrocytes [88]. It also regulates TNF-induced or regulated biological responses and alters the level of adhesive molecules responsible for leukocyte displacement. Adalimumab is administered in the absence of response to other TNF antagonists [89]. At the same time, adalimumab is recommended as the first choice of biological immunosuppressive agents for JIA relevant anterior uveitis [90]. In contrast to infliximab, the drug does not contain a murine component and therefore does not have specific immunogenicity and is less likely to cause autoimmune syndromes. Compared with etanercept, adalimumab is more economical, with a lower treatment burden and higher compliance. Adalimumab is approved in Europe in combination with MTX for multiarticular JIA over 2 years of age who do not respond well to one or more conventional DMARDs. In 2019, China also approved the indication of adalimumab in multiarticular JIA over 2 years old. The therapeutic dosage is: body weight 10 to < 30 kg, subcutaneously injected 20 mg every 2 weeks; body weight ≥ 30 kg, 40 mg subcutaneously every 2 weeks. The result of a 2-year follow-up study reported the safety and efficacy of anti-TNF-α therapy in JIA-associated uveitis [91]. In terms of efficacy, they found that anti-TNF-α agents responded well, with a higher response rate among patients receiving adalimumab than infliximab (60.0% versus 20.0%, P < 0.01). During this 2 years of follow-up, 63 new ocular complications were reported (38 of 24 patients treated with adalimumab and 25 of 13 patients treated with infliximab). Cataract was the most common complication (infliximab 25%, adalimumab 11.1%), followed by banded keratopathy, synechiae, ocular hypertension, and vitreitis.
Golimumab
Golimumab is an intravenously administered, humanized monoclonal antibody against TNF-α [92]. It can target and neutralize soluble and transmembrane active forms of TNF-α, prevent binding to TNF receptors and thereby inhibit the biological activity of TNF [93]. The drug appears to significantly improve the symptoms and signs, physical function, and inhibit the further development of structural damage in children with JIA [94]. The result of a randomized controlled trial confirmed that golimumab can rapidly improve the condition of children with active JIA [95]. The study lasted 48 weeks. All patients received subcutaneous injection of golimumab every 4 weeks at a dose of 30 mg/m2 body surface area (maximum dose: 50 mg). Compared with the control group, the clinical remission rate of children with JIA was higher, and the difference was statistically significant. Golimumab was well tolerated, and no unexpected safety events occurred.
Interleukin-1 inhibitors
IL-1 is a major pro-inflammatory cytokine secreted by fibroblasts, macrophages, and neutrophils [96]. IL-1 induces the production of other inflammatory cytokines such as IL-6 and TNF-α, as well as secretion of other inflammatory mediators such as cyclooxygenase-2 nitric oxide synthase and prostaglandin E2 [97]. Some studies [98, 99] have shown that IL-1 is a kind of heat source and is closely related to the fever of children with JIA. The serological level of IL-1 in children with JIA is significantly increased and is correlated with the thermal peak curve of children with JIA [100]. IL-1 can activate the body temperature center, causing fever. Activation of the IL-1 receptor on the endothelial surface leads to the occurrence of rash, and affects the hematopoietic function of bone marrow, activation, and maturation of granulocytes, resulting in increase of peripheral blood neutrophilia [101]. IL-1 can also cause increased platelet levels, leading to thrombocytopenia, and lower erythropoietin levels in vivo, which causes anemia and other manifestations [102]. In addition, the researchers analyzed gene expression profiles in JIA children and compared them with healthy controls and other children with febrile disease and concluded that IL-1 receptor gene levels were significantly upregulated in JIA children, thus demonstrating the specificity of IL-1 in their febrile symptoms [103]. At last, patients with sJIA generally respond well to IL-1 inhibitors, whereas anti-TNF drugs are less effective in this JIA subtype.
Rilonacept
Rilonacept is a recombinant fusion protein that eliminates the efficiency of the TNF-α receptor protein, which has a powerful anti-inflammatory effect, can treat JIA synovitis and bone erosion, and the effect is very significant [104]. A clinical study confirmed that rilonacept had a far-reaching impact on the clinical manifestations of joints in children with JIA, and could reduce the levels of CRP, myeloid-related protein (MRP)-8/MRP-14 and D-dimer [105]. In addition, the study also found that rilonacept treatment had a steroid retention effect, 10 (58.8%) of the 17 patients taking steroids at the beginning of the study were able to completely stop steroid treatment at the end of the study. Another randomized, double-blind, multicenter clinical study used rilonacept subcutaneous injection of 2.2 mg/kg per week for 4 weeks. The results showed that rilonacept had a better effect than placebo [106].
Anakinra
Anakinra is a recombinant human IL-1 receptor antagonist [107]. Due to the important role of IL-1 in pathogenesis, the treatment of sJIA is preferred. Anakinra is the first recombinant directly selective IL-1 blocker that can be used alone or in combination with antirheumatic agents other than TNF blockers [108]. With a half-life of 4–6 h, so it is necessary to inject anakinra every day. At present, the drug is commonly used 1–2 mg/kg each time, up to 100 mg, once a day, subcutaneous injection [109]. Of course, anakinra can also cause some adverse reactions. Serious adverse reactions are severe infection and neutropenia. The most common adverse reactions are injection site reactions, which are usually mild to moderate, showing redness, swelling and pain. A multicenter, randomized, double-blind controlled trial of anakinra (2 mg/kg subcutaneous, up to 100 mg/day) in children with JIA found significant relief in symptoms and a significant reduction in ESR and CRP [110]. Compared with MTX, another recent cohort study showed that anakinra could bring a significantly increased risk of infection [111].
Canakinumab
Canakinumab is a selective, high-affinity, humanized monoclonal antibody targeting IL-1β [112]. Due to its low adverse reactions and lower half-life than anakinra, it is the preferred adopted IL-1 antagonist [113]. Two parallel studies were conducted to evaluate the efficacy and safety of canakinumab in the treatment of sJIA [114]. The results showed that the patients in the canakinumab group had better efficacy than the control group, and among the patients who received randomization during the withdrawal phase, the patients who continued to receive canakinumab had a lower risk of disease recurrence than those who switched to placebo. Adverse reactions include arm pain, lymphadenopathy, leucopenia, elevated transaminase, and respiratory tract infection.
Interleukin-6 inhibitors
IL-6 is a cytokine secreted by T cells, B cells, monocytes, fibroblasts, osteoblasts, keratinocytes, endothelial cells, mesangial cells, and some tumor cells [115]. Abnormal activation of phagocytes can lead to increased serum IL-6 level [116]. It has been reported that IL-6 is an important marker of JIA disease activity and is associated with inflammatory response products in the acute phase [117]. It is involved in systemic inflammatory manifestations of all types of juvenile idiopathic arthritis and is involved in chronic joint destruction [118]. A clinical study showed that IL-6 can activate the membrane-bound receptor gp130 by binding to transmembrane proteins, and then gp130 can activate the expression of various genes leading to cell proliferation and differentiation by activating the tyrosine kinases and stimulating the transformation of B cells into plasma cells [119, 120]. Stimulate the proliferation of T lymphocytes and differentiate into Th17, which participate in systemic inflammation. IL-6 was significantly elevated in serum and synovial fluid of JIA children [121]. Based on the important role of IL-6 in the pathogenesis of JIA children, IL-6 antagonist was produced, and the efficacy of this drug just proves the important significance of IL-6 in the pathogenesis of JIA [122].
Tocilizumab
Tocilizumab is a monoclonal antibody against IL-6 receptor. Growth catch-up and increased bone mass were observed in sJIA patients treated with tocilizumab [123]. In 2013, ACR guidelines recommended tocilizumab for the treatment of patients with active systemic symptoms or active arthritis who did not respond to initial treatment. In addition to sJIA, tocilizumab is recommended for polyarticular JIA patients with poor MTX efficacy and intolerance [124]. In China, tocilizumab is approved for the treatment of active polyarticular JIA. Tocilizumab is one of the few biological agents that have been shown to be superior to methotrexate. A randomized controlled trial of 75 children aged 2 to 17 years with JIA treated with tocilizumab found that 85% met the American College of Rheumatology Pediatric (ACR Pedi) criteria 30 percentages response rates, a significant difference compared with placebo [125]. Major adverse events included infection, neutrophils, and increased aminotransferase levels. Another medical record of 11 consecutive JIA patients who received tocilizumab in the outpatient clinic, included 7 sJIA patients and 4 polyarticular JIA patients. Results showed that in most patients, symptoms improved, with no recurrence of arthritis or other symptoms [126].
Sarilumab
Sarilumab is the first fully human monoclonal immunoglobulin (Ig) G antibody approved to directly target the IL-6 receptor complex α subunit (IL-6Rα) [127]. Sarilumab binds with IL-6Rα with high affinity and inhibits the formation of the IL-6/IL-6Rα complex, thereby interrupting the cascade of cytokine-mediated inflammatory signals [128]. Studies of sarilumab for JIA are still ongoing and patients are currently being recruited [129].
Interleukin-2 inhibitor
IL-2 is a cytokine secreted by activated Th1 cells, which can induce lymphocyte proliferation and immune response. Excessive Th1 cytokines can cause local chronic inflammation and matrix destruction, and then promote the progress of synovial inflammation and joint destruction [130].
Daclizumab is a recombinant humanized IgG1 anti-TAC antibody. It functions like an IL-2 receptor antagonist, highly specifically binding to the a-subunit or TAC subunit of the IL-2 receptor complex (expressed on the surface of activated T cells), thereby inhibiting IL-2 mediated lymphocyte activation [131]. In an open-label, prospective clinical study, six patients with JIA-associated uveitis were treated with daclizumab, and intraocular inflammation was significantly relieved in four patients and improved in one case [132]. This study suggests that daclizumab helps reduce active inflammation in active JIA associated with anterior uveitis. However, larger randomized trials are needed to better assess the efficacy and safety of treatment.
Interleukin-17A inhibitor
IL-17A is a pro-inflammatory cytokine and a regulator of inflammatory response. IL-17A can induce epithelial cells to secrete granulocyte colony-stimulating factor and chemokine ligand 20. These factors recruit large numbers of neutrophils to the site of injury, contributing to an early inflammatory response. IL-17A also acts synergistically with other cytokines IL-1, IL-6, and TNF-α to greatly enhance its action and promote the activation of infiltrated neutrophils in tissues, thereby maintaining the arthritic state. In addition, IL-17A promotes osteoclast formation, causing local cartilage and bone destruction in the joint [133].
Secukinumab is a fully humanized monoclonal antibody that selectively binds to IL-17A and prevents IL-17A from binding to its receptor, thereby preventing it from inducing the inflammatory response that causes JIA. A retrospective study of children with JIA who had failed to respond to TNF-α inhibitors with secukinumab showed significant improvement in disease activity and symptom scores after 24 months of follow-up, and no serious adverse events were observed [134].
Interleukin-12/interleukin-23 inhibitor
IL-12 binds to the IL-12 receptor on T cells to induce the classical Thl immune response represented by IFN-γ production, and IL-23 induces and maintains the Th17 immune response. IL-12/IL-23 plays an important role in leukocyte migration and activation, osteoclast activation and bone destruction in inflammatory response [135].
Ustekinumab is a humanized monoclonal antibody against IL-12/IL-23. Ustekinumab binds to the P40 subunit of IL-12 and IL-23 and inhibits the biological activity of IL-12/IL-23. Mannion et al. [136] first reported the use of ustekinumab in children with JIA. They retrospectively analyzed 5 children with JIA who had not responded well to multiple TNF inhibitors and were treated with ustekinumab. In addition to the improvement of signs and symptoms of arthritis, attachment inflammation and pain, no serious adverse reactions occurred in these 5 subjects after treatment.
Janus kinase (JAK) inhibitors
JAK is an intracellular enzyme that transmits signals produced by cytokine or growth factor-receptor interactions across cell membranes to influence hematopoiesis and immune cell function. In signaling pathways, JAK phosphorylates and activates signal transducers and transcriptional activators (STATs), which regulate intracellular activity, including gene expression. JAK enzymes transmit cytokine signaling through JAK pairing (e.g., JAK1/JAK3, JAK1/JAK2, JAK1/TYK2, and JAK2/JAK2). JAK/STAT signaling pathway has an important relationship with the pathogenesis of JIA [137]. At present, several JAK inhibitors have entered clinical research in the treatment of JIA, most of which have poor selectivity and generally inhibit the four kinases of JAK family [138].
Tofacitinib
Tofacitinib targets intracellular signal transduction pathway and acts on the core part of cytokine network. Tofacitinib can inhibit JAK1/JAK2, JAK1/JAK3, and JAK2/JAK2 combinations in vitro. The inhibitory intensity of tofacitinib on JAK3 is 5–100 times higher than that on JAK1 and JAK2 [139]. In September 2020, FDA-approved tofacitinib for the treatment of adolescent idiopathic arthritis patients aged 2 and over with active polyarticular JIA disease. Since then, the European Commission has also announced that tofacitinib has been approved for the treatment of patients aged 2 years and older with active polyarticular JIA and juvenile psoriatic arthritis who have responded poorly to treatment prior to DMARDs [140]. Oral dose for children is 5–7 kg body weight: 2 mg each time, twice a day; > 7–10 kg: 2.5 mg each time, twice a day; > 10–15 kg: 3 mg each time, twice a day; > 15–25 kg: 3.5 mg each time, twice a day; > 25 to < 40 kg: 4 mg each time, twice a day; ≥ 40 kg, according to the adult dose, 5 mg each time, twice a day. Huang et al. [141] used tofacitinib to treat a child with JIA, and found that joint inflammation and systemic lesions were gradually relieved after treatment. Clinical symptoms disappeared completely 3 months later, and no evidence of disease activity or adverse reactions was found at 6 months of follow-up. Their study revealed the effectiveness of tofacitinib in the treatment of refractory sJIA.
Baricitinib
Baricitinib is a once-daily oral selective and reversible inhibitor of JAK1, JAK2, and TYK2 [142]. Miserocchi et al. [143] treated JIA-associated uveitis with JAK inhibitors, with three patients receiving baricitinib and one patient receiving tofacitinib. After treatment, arthritis and ocular inflammation were significantly reduced and without recurrence. The safety of the drug was good, with no adverse symptoms, laboratory abnormalities or infections during a mean follow-up period of 7 months. A multicenter, phase III trial will be conducted using an open-label Bayesian design. The researchers will enroll at least 40 patients between the ages of 2 and 18, after which patients with JIA will receive baricitinib treatment. The primary end point was the proportion of patients who responded at week 24. The patients with JIA can get continuous medication for up to 5 years [144].
Ruxolitinib
Ruxolitinib is the first clinically effective, selective JAK1/2 inhibitor. Its selectivity on JAK1 and JAK2 is more than 130 times higher than that on JAK3 [145]. Bader-Meunier et al. [146] used ruxolitinib to treat a child with sJIA-like associated with high-fatality lung diseases. After treatment, the shadow area of bilateral lung interstitium on chest computed tomography decreased, the bronchovascular bundle decreased, and the oxygen saturation increased from 92 to 100%.
Biological agents acting on target cells
In addition, biologic agents targeting T and B cells can be used in the treatment of children with JIA, and their effectiveness and efficacy have been confirmed by several studies [147].
Abatacept
Abatacept is a selective T cell stimulation modulator that inhibits T cell activation by binding to CD80 and CD86 on antigen-presenting cells [148]. Abatacept has been approved by FDA for use in children with refractory JIA over 6 years of age or who cannot tolerate TNF inhibitors. ACR guidelines recommend abatacept for multiarticular JIA who have failed to respond to TNF-α inhibitors and for sJIA with active arthritis symptoms who have failed to respond to initial MTX, LEF, or anakinra. The dosage is general < 75 kg, 10 mg/kg each time and > 75 kg, 750 mg each time. After drug given in 0, 2 and 4 weeks, injections were given once every 4 weeks. A randomized controlled study found that arthritis became improved or stabilized in JIA patients treated with abatacept, and lots of patients had met the ACR Pedi 70 responses, while the illness state of many patients in the control group got worse. The main adverse reactions included headache, nausea, cough, and diarrhea [149]. Another clinical trial pointed out that abatacept significantly improved the health-related quality of life of JIA patients [150].
Rituximab
Rituximab is the only human mouse chimeric monoclonal antibody targeting B lymphocyte (CD20) [151]. It mainly targets mature B cells and can increase apoptosis of B cells and reduce CD20 carrying in mature B cells [152]. The ACR guidelines recommend that rituximab be indicated for children with JIA who remain highly or moderately active with poor prognostic factors after sequential treatment with TNF-α inhibitors and abatacept [153]. A cohort study showed that rituximab could reduce the level of joint inflammation and pain in children with JIA. The adverse reactions were infusion reaction and infection [154]. Another case-series study found that after using rituximab to treat 6 children with JIA, the symptoms of 5 children in them got reduced significantly, and rituximab has also proved to be an effective treatment option [155].
Givinostat
Histone deacetylases (HDACs) play an important role in chromosome structural modification and gene expression regulation [156]. It can inhibit the relaxation of nucleosomes and inhibit the binding of inflamed transcription factors and synergistic transcription factors to DNA sites. Givinostat is a potent oral bioavailable inhibitor of HDACs and reduces JAK2/STAT5 phosphorylation, so as to inhibit the production of pro-inflammatory cytokines TNF-α, IL-1, IL-6, and IFN-γ [157]. Vojinovic et al. [158] first reported the clinical efficacy of givinostat in the treatment of JIA. Givinostat was administered orally in 17 patients with sJIA at a dose of 1.5 mg/kg per day for 12 weeks. After treatment, joint swelling and pain were significantly alleviated, ESR and CRP were alleviated to varying degrees, and the improvement rates of ACR Pedi 30, ACR Pedi 50 and ACR Pedi 70 were 77.8%, 55.6% and 22.2%, respectively. Adverse reactions included nausea, vomiting, and fatigue.
Conclusions
With the deepening of the research on the treatment of JIA, researchers have discovered a variety of new biological agents that can control inflammation quickly and effectively and have been applied in the clinic to effectively relieve JIA. The rational use of biologics may be considered for any JIA patients that fails to respond to long-term drug therapy after 3–6 months. More and more new, effective, and safe biologics are being used in the clinic, providing more options for the treatment of JIA, and making it possible to recommend personalized treatment plans for each child.
In recent years, the birth of biological therapy, targeted therapy, and other methods, brought hope to a part of the treatment of refractory JIA children. New treatments offer valuable opportunities for some refractory JIA patients. The best treatment plan should be selected sequentially, individually, and accurately. Most important, and uncontroversial, is the care of patients by experienced pediatric and young rheumatologists in competent multidisciplinary teams. The team’s job is to tailor treatment to the patient’s medical, non-medical, and psychosocial support.
There is not enough space in this article to discuss in detail every drug used to treat JIA, and there is no mention of traditional medical treatment or nonsurgical treatment. However, the key points are selected to clarify the advances in drug research of effect and adverse reactions. Overall, the therapeutic changes allow us to better rationalize the use of existing therapies and improve JIA outcomes.
Data availability
All data generated or analysed during this study are included in this published article.
References
Beukelman T, Nigrovic PA. Juvenile idiopathic arthritis: an idea whose time has gone? J Rheumatol. 2019;46:124–6.
Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021;19:135.
Beukelman T, Lougee A, Matsouaka RA, Collier D, Rumsey DG, Schenfeld J, et al. Patterns of etanercept use in juvenile idiopathic arthritis in the Childhood Arthritis and Rheumatology Research Alliance Registry. Pediatr Rheumatol Online J. 2021;19:131.
Carlsson E, Midgley A, Perkins S, Caamano-Gutierrez E, Gritzfeld JF, Beresford MW, et al. Serum protein signatures differentiate paediatric autoimmune/inflammatory disorders. Clin Immunol. 2021;229:108790.
Adrovic A, Yildiz M, Köker O, Şahin S, Barut K, Kasapçopur Ö. Biologics in juvenile idiopathic arthritis-main advantages and major challenges: a narrative review. Arch Rheumatol. 2020;36:146–57.
Yue X, Huang B, Hincapie AL, Wigle PR, Li Y, Qiu T, et al. Comparative effectiveness and persistence of TNFi and non-TNFi in juvenile idiopathic arthritis: a large paediatric rheumatology centre in the USA. Rheumatology (Oxford). 2021;60:4063–73.
Papasavvas I, Gehrig B, Herbort CP Jr. Clinical course and treatment paradigms for JIA-related uveitis and pars planitis uveitis using precise ocular investigational methods. Klin Monbl Augenheilkd. 2021;238:458–68.
Yue X, Huang B, Hincapie AL, Wigle PR, Qiu T, Li Y, et al. Prescribing patterns and impact of factors associated with time to initial biologic therapy among children with non-systemic juvenile idiopathic arthritis. Paediatr Drugs. 2021;23:171–82.
Alzyoud RM, Alsuweiti MO, Almaaitah HQ, Aladaileh BN, Alnoubani MK, Alwahadneh AM. Juvenile idiopathic arthritis in Jordan: single center experience. Pediatr Rheumatol Online J. 2021;19:90.
Jia Y, Li M, Wang H, Zhang M, Wang Y. The peculiar clinical symptoms and treatment of limbic encephalitis associated with AMPA receptor antibody. Eur Neurol. 2021;84:206–11.
Kau CH, Allareddy V, Stoustrup P, Pedersen T, Kinard B, Cron RQ, et al. Management of juvenile idiopathic arthritis: preliminary qualitative findings from the National Dental Practice-Based Research Network. J World Fed Orthod. 2021;10:70–3.
Mahmud SA, Binstadt BA. Autoantibodies in the pathogenesis, diagnosis, and prognosis of juvenile idiopathic arthritis. Front Immunol. 2019;9:3168.
Kim JW, Ahn MH, Jung JY, Suh CH, Kim HA. An update on the pathogenic role of neutrophils in systemic juvenile idiopathic arthritis and adult-onset Still’s disease. Int J Mol Sci. 2021;22:13038.
Thomas M, Bonacorsi S, Simon AL, Mallet C, Lorrot M, Faye A, et al. Acute monoarthritis in young children: comparing the characteristics of patients with juvenile idiopathic arthritis versus septic and undifferentiated arthritis. Sci Rep. 2021;11:3422.
Rosenberg AM. Do we need a new classification of juvenile idiopathic arthritis? Clin Immunol. 2020;211:108298.
Foeldvari I, Constantin T, Vojinović J, Horneff G, Chasnyk V, Dehoorne J, et al. Etanercept treatment for extended oligoarticular juvenile idiopathic arthritis, enthesitis-related arthritis, or psoriatic arthritis: 6-year efficacy and safety data from an open-label trial. Arthritis Res Ther. 2019;21:125.
Sestan M, Grguric D, Sedmak M, Frkovic M, Kifer N, Grubic M, et al. Quality of life in children suffering from juvenile idiopathic arthritis-associated uveitis. Rheumatol Int. 2020;40:1117–21.
Khraishi M, Millson B, Woolcott J, Jones H, Marshall L, Ruperto N. Reduction in the utilization of prednisone or methotrexate in Canadian claims data following initiation of etanercept in pediatric patients with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2019;17:64.
Shoop-Worrall SJW, Hyrich KL. Predicting remission remains a challenge in patients with juvenile idiopathic arthritis. J Rheumatol. 2019;46:552–4.
Montefiori E, Modenese L, Di Marco R, Magni-Manzoni S, Malattia C, Petrarca M, et al. Linking joint impairment and gait biomechanics in patients with juvenile idiopathic arthritis. Ann Biomed Eng. 2019;47:2155–67.
Scheer T, Klotsche J, Len CA, Foeldvari I. Validation and adaptation of a German screening tool to identify patients at risk of juvenile idiopathic arthritis. Rheumatol Int. 2020;40:643–50.
Silvagni E, Bortoluzzi A, Ciancio G, Govoni M. Biological and synthetic target DMARDs in psoriatic arthritis. Pharmacol Res. 2019;149:104473.
Seaman SC, Hong S, Dlouhy BJ, Menezes AH. Current management of juvenile idiopathic arthritis affecting the craniovertebral junction. Childs Nerv Syst. 2020;36:1529–38.
Correll CK. Role of environment in pediatric rheumatic diseases. Rheum Dis Clin North Am. 2022;48:287–304.
Kramer M, Tomkins-Netzer O. Cataract risk and topical corticosteroids among children with juvenile idiopathic arthritis-related uveitis. Ophthalmology. 2020;127:S19-20.
Stoustrup P, Twilt M, Herlin T. Systemic treatment for temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol. 2020;47:793–5.
Thorne JE, Woreta FA, Dunn JP, Jabs DA. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids. Ophthalmology. 2010;117:1436–41.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020;72:220–33.
Angeles-Han ST, Ringold S, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. Arthritis Rheumatol. 2019;71:864–77.
Rebane K, Aalto K, Haanpää M, Puolakka K, Virta LJ, Kautiainen H, et al. Initiating disease-modifying anti-rheumatic drugs rapidly reduces purchases of analgesic drugs in juvenile idiopathic arthritis. Scand J Rheumatol. 2021;50:28–33.
Naveen R, Jain A, Muhammed H, Gupta L, Misra DP, Lawrence A, et al. Macrophage activation syndrome in systemic lupus erythematosus and systemic-onset juvenile idiopathic arthritis: a retrospective study of similarities and dissimilarities. Rheumatol Int. 2021;41:625–31.
Räisänen L, Viljakainen H, Sarkkola C, Kolho KL. Perinatal risk factors for pediatric onset type 1 diabetes, autoimmune thyroiditis, juvenile idiopathic arthritis, and inflammatory bowel diseases. Eur J Pediatr. 2021;180:2115–23.
Van Gelder RN. Drug costs, effectiveness, and kids in the crossfire: adalimumab in juvenile idiopathic arthritis-associated uveitis. Ophthalmology. 2019;126:425–7.
Loganathan S, Banday A, Jindal AK, Sudhakar M, Patra N, Pulipaka S, et al. Tapering doses of methylprednisolone pulse in the treatment of macrophage activation syndrome associated with systemic juvenile idiopathic arthritis. Indian J Pediatr. 2021;88:1056.
Beverstock A, Kelly A. Severe acute ocular hypertension following pulsed methylprednisolone for juvenile idiopathic arthritis. BMJ Case Rep. 2019;12:e229803.
Solebo AL, Rahi JS, Dick AD, Ramanan AV, Ashworth J, Edelsten C, et al. Areas of agreement in the management of childhood non-infectious chronic anterior uveitis in the UK. Br J Ophthalmol. 2020;104:11–6.
Smith CA, Toupin-April K, Jutai JW, Duffy CM, Rahman P, Cavallo S, et al. A systematic critical appraisal of clinical practice guidelines in juvenile idiopathic arthritis using the appraisal of guidelines for research and evaluation II (AGREE II) instrument. PLoS One. 2015;10:e0137180.
Żuber Z, Turowska-Heydel D, Sobczyk M, Banach-Górnicka M, Rusnak K, Piszczek A, et al. Methotrexate efficacy and tolerability after switching from oral to subcutaneous route of administration in juvenile idiopathic arthritis. Reumatologia. 2016;54:19–23.
Ramanan AV, Dick AD, Jones AP, Guly C, Hardwick B, Hickey H, et al. A phase II trial protocol of tocilizumab in anti-TNF refractory patients with JIA-associated uveitis (the APTITUDE trial). BMC Rheumatol. 2018;2:4.
Kim EH, Shin D, Lee J, Jung AR, Roh JL. CISD2 inhibition overcomes resistance to sulfasalazine-induced ferroptotic cell death in head and neck cancer. Cancer Lett. 2018;432:180–90.
Shi S, Guo P, Anwar MI, Zhang W, Zhang W, Yang G. Copper mixed-triazolate frameworks featuring the thiophene-containing ligand towards enhanced photodegradation of organic contaminants in water. J Hazard Mater. 2021;406:124757.
Tanaka Y. Stopping tumour necrosis factor-targeted biological DMARDs in rheumatoid arthritis. Rheumatology. 2016;55(Suppl 2):ii15-22.
Chang S, Cao Y. Sulfasalazine maintains blood-brain barrier integrity and relieves lipopolysaccharide-induced inflammation in hCMEC/D3 cells. NeuroReport. 2021;32:672–7.
Yousefi-Ahmadipour A, Ebrahimi-Barough S, Niknia S, Allahverdi A, Mirzahosseini-Pourranjbar A, Tashakori M, et al. Therapeutic effects of combination of platelet lysate and sulfasalazine administration in TNBS-induced colitis in rat. Biomed Pharmacother. 2020;125:109949.
Cellucci T, Guzman J, Petty RE, Batthish M, Benseler SM, Ellsworth JE, et al. Management of juvenile idiopathic arthritis 2015: a position statement from the Pediatric Committee of the Canadian Rheumatology Association. J Rheumatol. 2016;43:1773–6.
Tynjälä P, Vähäsalo P, Tarkiainen M, Kröger L, Aalto K, Malin M, et al. Aggressive combination drug therapy in very early polyarticular juvenile idiopathic arthritis (ACUTE-JIA): a multicentre randomised open-label clinical trial. Ann Rheum Dis. 2011;70:1605–12.
van Rossum MA, van Soesbergen RM, Boers M, Zwinderman AH, Fiselier TJ, Franssen MJ, et al. Long-term outcome of juvenile idiopathic arthritis following a placebo-controlled trial: sustained benefits of early sulfasalazine treatment. Ann Rheum Dis. 2007;66:1518–24.
Ting TV, Lovell DJ. Does early sulfasalazine treatment provide long-term benefits to patients with juvenile idiopathic arthritis? Nat Clin Pract Rheumatol. 2008;4:344–5.
Wan Z, Li H, Wu X, Zhao H, Wang R, Li M, et al. Hepatoprotective effect of gentiopicroside in combination with leflunomide and/or methotrexate in arthritic rats. Life Sci. 2021;265:118689.
Zewail M, Nafee N, Helmy MW, Boraie N. Synergistic and receptor-mediated targeting of arthritic joints via intra-articular injectable smart hydrogels containing leflunomide-loaded lipid nanocarriers. Drug Deliv Transl Res. 2021;11:2496–519.
Huang H, Ran H, Liu X, Yu L, Qiu L, Lin Z, et al. Leflunomide ameliorates experimental autoimmune myasthenia gravis by regulating humoral and cellular immune responses. Int Immunopharmacol. 2021;93:107434.
Muhammad T, Zafar M, Quiroga J, Whitehead M. Leflunomide-induced delayed onset colitis. Br J Hosp Med (Lond). 2021;82:1–3.
Ayaz NA, Karadağ ŞG, Çakmak F, Çakan M, Tanatar A, Sönmez HE. Leflunomide treatment in juvenile idiopathic arthritis. Rheumatol Int. 2019;39:1615–9.
Ahlmann M, Hempel G. The effect of cyclophosphamide on the immune system: implications for clinical cancer therapy. Cancer Chemother Pharmacol. 2016;78:661–71.
Teles KA, Medeiros-Souza P, Lima FAC, Araújo BG, Lima RAC. Cyclophosphamide administration routine in autoimmune rheumatic diseases: a review. Rev Bras Reumatol Engl Ed. 2017;57:596–604 (in English, Portuguese).
de Castro TC, Terreri MT, Len C, Hilário MO. Treatment of refractory juvenile idiopathic arthritis via pulse therapy using methylprednisolone and cyclophosphamide. Sao Paulo Med J. 2003;121:117–20.
Chen CY, Chen LC, Yeh KW, Ou LS, Yang MH, Huang JL. Sequential changes to clinical parameters and adhesion molecules following intravenous pulse cyclophosphamide and methylprednisolone treatment of refractory juvenile idiopathic arthritis. Clin Exp Rheumatol. 2004;22:259–64.
Schulert GS, Grom AA. Pathogenesis of macrophage activation syndrome and potential for cytokine- directed therapies. Annu Rev Med. 2015;66:145–59.
Shimizu M, Mizuta M, Yasumi T, Iwata N, Okura Y, Kinjo N, et al. Validation of classification criteria of macrophage activation syndrome in Japanese patients with systemic juvenile idiopathic arthritis. Arthritis Care Res. 2018;70:1412–5.
Ruperto N, Ravelli A, Castell E, Gerloni V, Haefner R, Malattia C, et al. Cyclosporine A in juvenile idiopathic arthritis. Results of the PRCSG/PRINTO phase IV post marketing surveillance study. Clin Exp Rheumatol. 2006;24:599–605.
Pal P, Giri PP, Sinha R. Cyclosporine in resistant systemic arthritis-a cheaper alternative to biologics. Indian J Pediatr. 2019;86:590–4.
Ye P, Chi X, Cha JH, Luo S, Yang G, Yan X, et al. Potential of E3 ubiquitin ligases in cancer immunity: opportunities and challenges. Cells. 2021;10:3309.
Sathe K, Khubchandani RP. Thalidomide for systemic onset juvenile idiopathic arthritis. Indian Pediatr. 2013;50:237–9.
García-Carrasco M, Fuentes-Alexandro S, Escárcega RO, Rojas-Rodriguez J, Escobar LE. Efficacy of thalidomide in systemic onset juvenile rheumatoid arthritis. Jt Bone Spine. 2007;74:500–3.
Ponticelli C, Moroni G. Hydroxychloroquine in systemic lupus erythematosus (SLE). Expert Opin Drug Saf. 2017;16:411–9.
Jorge A, Ung C, Young LH, Melles RB, Choi HK. Hydroxychloroquine retinopathy-implications of research advances for rheumatology care. Nat Rev Rheumatol. 2018;14:693–703.
Nirk EL, Reggiori F, Mauthe M. Hydroxychloroquine in rheumatic autoimmune disorders and beyond. EMBO Mol Med. 2020;12:e12476.
Haapasaari J, Kautiainen H, Isomäki H, Hakala M. Hydroxychloroquine does not decrease serum methotrexate concentrations in children with juvenile idiopathic arthritis. Arthritis Rheum. 2005;52:1621–2.
Dumaine C, Bekkar S, Belot A, Cabrera N, Malik S, von Scheven A, et al. Infectious adverse events in children with juvenile idiopathic arthritis treated with biological agents in a real-life setting: data from the JIRcohorte. Jt Bone Spine. 2020;87:49–55.
Strand V, Balsa A, Al-Saleh J, Barile-Fabris L, Horiuchi T, Takeuchi T, et al. Immunogenicity of biologics in chronic inflammatory diseases: a systematic review. BioDrugs. 2017;31:299–316.
Cabrera N, Lega JC, Kassai B, Wouters C, Kondi A, Cannizzaro E, et al. Safety of biological agents in paediatric rheumatic diseases: a real-life multicenter retrospective study using the JIRcohorte database. Jt Bone Spine. 2019;86:343–50.
Giancane G, Muratore V, Marzetti V, Quilis N, Benavente BS, Bagnasco F, et al. Disease activity and damage in juvenile idiopathic arthritis: methotrexate era versus biologic era. Arthritis Res Ther. 2019;21:168.
Peng Y, Liu X, Duan Z, Duan J, Zhou Y. The association of serum IL-10 levels with the disease activity in systemic-onset juvenile idiopathic arthritis patients. Mediat Inflamm. 2021;2021:6650928.
Thiele F, Klein A, Windschall D, Hospach A, Foeldvari I, Minden K, et al. Comparative risk of infections among real-world users of biologics for juvenile idiopathic arthritis: data from the German BIKER registry. Rheumatol Int. 2021;41:751–62.
Leong JY, Chen P, Yeo JG, Ally F, Chua C, Nur Hazirah S, et al. Immunome perturbation is present in patients with juvenile idiopathic arthritis who are in remission and will relapse upon anti-TNFα withdrawal. Ann Rheum Dis. 2019;78:1712–21.
Verstegen RHJ, McMillan R, Feldman BM, Ito S, Laxer RM. Towards therapeutic drug monitoring of TNF inhibitors for children with juvenile idiopathic arthritis: a scoping review. Rheumatology (Oxford). 2020;59:386–97.
Ringold S, Angeles-Han ST, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic polyarthritis, sacroiliitis, and enthesitis. Arthritis Care Res. 2019;71:846–63.
Grazziotin LR, Currie G, Kip MMA, IJzerman MJ, Twilt M, Lee R, et al. Health state utility values in juvenile idiopathic arthritis: what is the evidence? Pharmacoeconomics. 2020;38:913–26.
Ho ACH, Wong SN, Leung LCK, Chan WKY, Chong PCY, Tse NKC, et al. Biological disease-modifying antirheumatic drugs in juvenile idiopathic arthritis of polyarticular course, enthesitis-related arthritis, and psoriatic arthritis: a consensus statement. Hong Kong Med J. 2020;26:56–65.
Murdaca G, Negrini S, Magnani O, Penza E, Pellecchio M, Gulli R, et al. Update upon efficacy and safety of etanercept for the treatment of spondyloarthritis and juvenile idiopathic arthritis. Mod Rheumatol. 2018;28:417–31.
Alexeeva EI, Namazova-Baranova LS, Bzarova TM, Valieva SI, Denisova RV, Sleptsova TV, et al. Predictors of the response to etanercept in patients with juvenile idiopathic arthritis without systemic manifestations within 12 months: results of an open-label, prospective study conducted at the National Scientific and Practical Center of Children’s Health. Russia Pediatr Rheumatol Online J. 2017;15:51.
Arvonen M, Vänni P, Sarangi AN, Tejesvi VM, Vähäsalo P, Aggarwal A, et al. Microbial orchestra in juvenile idiopathic arthritis: sounds of disarray? Immunol Rev. 2020;294:9–26.
Liu DW, Chen JJ, Tang XM, Zhang Y, Zhou J. Infliximab therapy and outcomes in patients with polyarticular juvenile idiopathic arthritis: a single-center study in China. World J Pediatr. 2020;16:68–73.
Favalli EG, Pontikaki I, Becciolini A, Biggioggero M, Ughi N, Romano M, et al. Real-life 10-year retention rate of first-line anti-TNF drugs for inflammatory arthritides in adult- and juvenile-onset populations: similarities and differences. Clin Rheumatol. 2017;36:1747–55.
Tarkiainen M, Tynjälä P, Vähäsalo P, Kröger L, Aalto K, Lahdenne P. Health-related quality of life during early aggressive treatment in patients with polyarticular juvenile idiopathic arthritis: results from randomized controlled trial. Pediatr Rheumatol Online J. 2019;17:80.
Lahdenne P, Vähäsalo P, Honkanen V. Infliximab or etanercept in the treatment of children with refractory juvenile idiopathic arthritis: an open label study. Ann Rheum Dis. 2003;62:245–7.
Visvanathan S, Wagner C, Marini JC, Lovell DJ, Martini A, Petty R, et al. The effect of infliximab plus methotrexate on the modulation of inflammatory disease markers in juvenile idiopathic arthritis: analyses from a randomized, placebo-controlled trial. Pediatr Rheumatol Online J. 2010;8:24.
Horton S, Jones AP, Guly CM, Hardwick B, Beresford MW, Lee RW, et al. Adalimumab in juvenile idiopathic arthritis-associated uveitis: 5-year follow-up of the Bristol participants of the SYCAMORE trial. Am J Ophthalmol. 2019;207:170–4.
Klotsche J, Niewerth M, Haas JP, Huppertz HI, Zink A, Horneff G, et al. Long-term safety of etanercept and adalimumab compared to methotrexate in patients with juvenile idiopathic arthritis (JIA). Ann Rheum Dis. 2016;75:855–61.
Smith JR, Matthews JM, Conrad D, Hall AJ, Niederer RL, Singh-Grewal D, et al. Recommendations for the management of childhood juvenile idiopathic arthritis-type chronic anterior uveitis. Clin Exp Ophthalmol. 2021;49:38–45.
Cecchin V, Zannin ME, Ferrari D, Pontikaki I, Miserocchi E, Paroli MP, et al. Longterm safety and efficacy of adalimumab and infliximab for uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2018;45:1167–72.
William M, Faez S, Papaliodis GN, Lobo AM. Golimumab for the treatment of refractory juvenile idiopathic arthritis-associated uveitis. J Ophthalmic Inflamm Infect. 2012;2:231–3.
Webb K, Wedderburn LR. Advances in the treatment of polyarticular juvenile idiopathic arthritis. Curr Opin Rheumatol. 2015;27:505–10.
Hersh AO, Prahalad S. Immunogenetics of juvenile idiopathic arthritis: a comprehensive review. J Autoimmun. 2015;64:113–24.
Brunner HI, Ruperto N, Tzaribachev N, Horneff G, Chasnyk VG, Panaviene V, et al. Subcutaneous golimumab for children with active polyarticular-course juvenile idiopathic arthritis: results of a multicentre, double-blind, randomised-withdrawal trial. Ann Rheum Dis. 2018;77:21–9.
Mejbri M, Theodoropoulou K, Hofer M, Cimaz R. Interleukin-1 blockade in systemic juvenile idiopathic arthritis. Paediatr Drugs. 2020;22:251–62.
Yasin S, Schulert GS. Systemic juvenile idiopathic arthritis and macrophage activation syndrome: update on pathogenesis and treatment. Curr Opin Rheumatol. 2018;30:514–20.
Miserocchi E, Modorati G, Berchicci L, Pontikaki I, Meroni P, Gerloni V. Long-term treatment with rituximab in severe juvenile idiopathic arthritis-associated uveitis. Br J Ophthalmol. 2016;100:782–6.
Krainer J, Siebenhandl S, Weinhäusel A. Systemic autoinflammatory diseases. J Autoimmun. 2020;109:102421.
Jamilloux Y, Gerfaud-Valentin M, Martinon F, Belot A, Henry T, Sève P. Pathogenesis of adult-onset Still’s disease: new insights from the juvenile counterpart. Immunol Res. 2015;61:53–62.
Stevens BE, Torok KS, Li SC, Hershey N, Curran M, Higgins GC, et al. Clinical characteristics and factors associated with disability and impaired quality of life in children with juvenile systemic sclerosis: results from the Childhood Arthritis and Rheumatology Research Alliance Legacy Registry. Arthritis Care Res (Hoboken). 2018;70:1806–13.
Kaegi C, Wuest B, Schreiner J, Steiner UC, Vultaggio A, Matucci A. Systematic review of safety and efficacy of rituximab in treating immune-mediated disorders. Front Immunol. 2019;10:1990.
Nara H, Watanabe R. Anti-inflammatory effect of muscle-derived interleukin-6 and its involvement in lipid metabolism. Int J Mol Sci. 2021;22:9889.
Vecchié A, Del Buono MG, Chiabrando GJ, Dentali F, Abbate A, Bonaventura A. Interleukin-1 and the NLRP3 inflammasome in pericardial disease. Curr Cardiol Rep. 2021;23:157.
Lovell DJ, Giannini EH, Reiff AO, Kimura Y, Li S, Hashkes PJ, et al. Long-term safety and efficacy of rilonacept in patients with systemic juvenile idiopathic arthritis. Arthritis Rheum. 2013;65:2486–96.
Ilowite NT, Prather K, Lokhnygina Y, Schanberg LE, Elder M, Milojevic D, et al. Randomized, double-blind, placebo-controlled trial of the efficacy and safety of rilonacept in the treatment of systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2014;66:2570–9.
Smith CJF, Chambers CD. Five successful pregnancies with antenatal anakinra exposure. Rheumatology (Oxford). 2018;57:1271–5.
Beukelman T, Xie F, Baddley JW, Chen L, Mannion ML, Saag KG, et al. The risk of hospitalized infection following initiation of biologic agents versus methotrexate in the treatment of juvenile idiopathic arthritis. Arthritis Res Ther. 2016;18:210.
Ramírez J, Cañete JD. Anakinra for the treatment of rheumatoid arthritis: a safety evaluation. Expert Opin Drug Saf. 2018;17:727–32.
Quartier P, Allantaz F, Cimaz R, Pillet P, Messiaen C, Bardin C, et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Ann Rheum Dis. 2011;70:747–54.
Ozen S, Demir S, Batu ED. Testing the model for predicting effectiveness of anakinra in systemic juvenile idiopathic arthritis. J Rheumatol. 2019;46:1422–4.
Peitz J, Horneff G. Treatment of systemic-onset juvenile arthritis with canakinumab. Open Access Rheumatol. 2015;7:23–31.
Grom AA. Canakinumab for the treatment of systemic juvenile idiopathic arthritis. Expert Rev Clin Immunol. 2014;10:1427–35.
Ruperto N, Brunner HI, Quartier P, Constantin T, Wulffraat N, Horneff G, et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2396–406.
Kang S, Tanaka T, Kishimoto T. Therapeutic uses of anti-interleukin-6 receptor antibody. Int Immunol. 2015;27:21–9.
Kearsley-Fleet L, Davies R, Baildam E, Beresford MW, Foster HE, Southwood TR, et al. Factors associated with choice of biologic among children with juvenile idiopathic arthritis: results from two UK paediatric biologic registers. Rheumatology. 2016;55:1556–65.
Calvo-Río V, Santos-Gómez M, Calvo I, González-Fernández MI, López-Montesinos B, Mesquida M, et al. Anti-interleukin-6 receptor tocilizumab for severe juvenile idiopathic arthritis-associated uveitis refractory to anti-tumor necrosis factor therapy: a multicenter study of twenty-five patients. Arthritis Rheumatol. 2017;69:668–75.
Bulatović Ćalasan M, Vastert SJ, Scholman RC, Verweij F, Klein M, Wulffraat NM, et al. Methotrexate treatment affects effector but not regulatory T cells in juvenile idiopathic arthritis. Rheumatology (Oxford). 2015;54:1724–34.
Leong JY, Guan YJ, Albani S, Arkachaisri T. Recent advances in our understanding of the pathogenesis of juvenile idiopathic arthritis and their potential clinical implications. Expert Rev Clin Immunol. 2018;14:933–44.
Cifaldi L, Prencipe G, Caiello I, Bracaglia C, Locatelli F, De Benedetti F, et al. Inhibition of natural killer cell cytotoxicity by interleukin-6: implications for the pathogenesis of macrophage activation syndrome. Arthritis Rheumatol. 2015;67:3037–46.
Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Clin Immunol. 2020;211:108322.
Choy EH, De Benedetti F, Takeuchi T, Hashizume M, John MR, Kishimoto T. Translating IL-6 biology into effective treatments. Nat Rev Rheumatol. 2020;16:335–45.
Narazaki M, Kishimoto T. The two-faced cytokine IL-6 in host defense and diseases. Int J Mol Sci. 2018;19:3528.
Ringold S, Weiss PF, Beukelman T, DeWitt EM, Ilowite NT, Kimura Y, et al. 2013 update of the 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: recommendations for the medical therapy of children with systemic juvenile idiopathic arthritis and tuberculosis screening among children receiving biologic medications. Arthritis Rheum. 2013;65:2499–512.
De Benedetti F, Brunner HI, Ruperto N, Kenwright A, Wright S, Calvo I, et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2385–95.
Yazılıtaş F, Özdel S, Şimşek D, Aydoğ Ö, Çakıcı EK, Can GG, et al. Tocilizumab for juvenile idiopathic arthritis: a single-center case series. Sao Paulo Med J. 2019;137:517–22.
Rubbert-Roth A, Furst DE, Nebesky JM, Jin A, Berber E. A review of recent advances using tocilizumab in the treatment of rheumatic diseases. Rheumatol Ther. 2018;5:21–42.
Pelechas E, Voulgari PV, Drosos AA. Clinical evaluation of the safety, efficacy and tolerability of sarilumab in the treatment of moderate to severe rheumatoid arthritis. Ther Clin Risk Manag. 2019;15:1073–9.
Lamb YN, Deeks ED. Sarilumab: a review in moderate to severe rheumatoid arthritis. Drugs. 2018;78:929–40.
Hoeppli RE, Pesenacker AM. Targeting Tregs in juvenile idiopathic arthritis and juvenile dermatomyositis-insights from other diseases. Front Immunol. 2019;10:46.
Meng X, Hou X, Wang P, Glessner JT, Qu HQ, March ME, et al. Association of novel rare coding variants with juvenile idiopathic arthritis. Ann Rheum Dis. 2021;80:626–31.
Sen HN, Levy-Clarke G, Faia LJ, Li Z, Yeh S, Barron KS, et al. High-dose daclizumab for the treatment of juvenile idiopathic arthritis-associated active anterior uveitis. Am J Ophthalmol. 2009;148:696–703.
Ferguson ID, Griffin P, Michel JJ, Yano H, Gaffen SL, Mueller RG, et al. T cell receptor-independent, CD31/IL-17A-driven inflammatory axis shapes synovitis in juvenile idiopathic arthritis. Front Immunol. 2018;9:1802.
Alimanovic D, Pedersen TK, Matzen LH, Stoustrup P. Comparing clinical and radiological manifestations of adolescent idiopathic condylar resorption and juvenile idiopathic arthritis in the temporomandibular joint. J Oral Maxillofac Surg. 2021;79:774–85.
Chyuan IT, Lai JH. New insights into the IL-12 and IL-23: from a molecular basis to clinical application in immune-mediated inflammation and cancers. Biochem Pharmacol. 2020;175:113928.
Mannion ML, McAllister L, Cron RQ, Stoll ML. Ustekinumab as a therapeutic option for children with refractory enthesitis-related arthritis. J Clin Rheumatol. 2016;22:282–4.
Li HW, Zeng HS. Regulation of JAK/STAT signal pathway by miR-21 in the pathogenesis of juvenile idiopathic arthritis. World J Pediatr. 2020;16:502–13.
Shibata T, Muto J, Hirano Y, Takama H, Yanagishita T, Ohshima Y, et al. Palmoplantar pustulosis-like eruption following tofacitinib therapy for juvenile idiopathic arthritis. JAAD Case Rep. 2019;5:518–21.
Caporali R, Zavaglia D. Real-world experience with tofacitinib for the treatment of rheumatoid arthritis. Clin Exp Rheumatol. 2019;37:485–95.
Li X, Pathadka S, Man KK, Wong ICK, Chan EWY. Budget impact of introducing tofacitinib to the public hospital formulary in Hong Kong, 2017–2021. Hong Kong Med J. 2019;25:201–8.
Huang Z, Lee PY, Yao X, Zheng S, Li T. Tofacitinib treatment of refractory systemic juvenile idiopathic arthritis. Pediatrics. 2019;143:e20182845.
Taylor PC, Keystone EC, van der Heijde D, Weinblatt ME, Del Carmen ML, Reyes Gonzaga J, et al. Baricitinib versus placebo or adalimumab in rheumatoid arthritis. N Engl J Med. 2017;376:652–62.
Miserocchi E, Giuffrè C, Cornalba M, Pontikaki I, Cimaz R. JAK inhibitors in refractory juvenile idiopathic arthritis-associated uveitis. Clin Rheumatol. 2020;39:847–51.
Ramanan AV, Guly CM, Keller SY, Schlichting DE, de Bono S, Liao R, et al. Clinical effectiveness and safety of baricitinib for the treatment of juvenile idiopathic arthritis-associated uveitis or chronic anterior antinuclear antibody-positive uveitis: study protocol for an open-label, adalimumab active-controlled phase 3 clinical trial (JUVE-BRIGHT). Trials. 2021;22:689.
Harrison CN, Schaap N, Mesa RA. Management of myelofibrosis after ruxolitinib failure. Ann Hematol. 2020;99:1177–91.
Bader-Meunier B, Hadchouel A, Berteloot L, Polivka L, Béziat V, Casanova JL, et al. Effectiveness and safety of ruxolitinib for the treatment of refractory systemic idiopathic juvenile arthritis like associated with interstitial lung disease: a case report. Ann Rheum Dis. 2022;81:e20.
Fischer J, Dirks J, Haase G, Holl-Wieden A, Hofmann C, Girschick H, Morbach H. IL-21+ CD4+ T helper cells co-expressing IFN-γ and TNF-α accumulate in the joints of antinuclear antibody positive patients with juvenile idiopathic arthritis. Clin Immunol. 2020;217:108484.
Beukelman T, Patkar NM, Saag KG, Tolleson-Rinehart S, Cron RQ, DeWitt EM, et al. 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care Res. 2011;63:465–82.
Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Pérez N, Silva CA, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372:383–91.
Ruperto N, Lovell DJ, Li T, Sztajnbok F, Goldenstein-Schainberg C, Scheinberg M, et al. Abatacept improves health-related quality of life, pain, sleep quality, and daily participation in subjects with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2010;62:1542–51.
Koç R, Sönmez HE, Çakan M, Karadağ ŞG, Tanatar A, Çakmak F, et al. Drug reactions in children with rheumatic diseases receiving parenteral therapies: 9 years’ experience of a tertiary pediatric rheumatology center. Rheumatol Int. 2020;40:771–6.
Gueudry J, Touhami S, Quartier P, Bodaghi B. Therapeutic advances in juvenile idiopathic arthritis-associated uveitis. Curr Opin Ophthalmol. 2019;30:179–86.
Takakura M, Shimizu M, Mizuta M, Inoue N, Tasaki Y, Ohta K, et al. Successful treatment of rituximab- and steroid-resistant nephrotic syndrome with leukocytapheresis. J Clin Apher. 2018;33:409–11.
Kearsley-Fleet L, Sampath S, McCann LJ, Baildam E, Beresford MW, Davies R, et al. Use and effectiveness of rituximab in children and young people with juvenile idiopathic arthritis in a cohort study in the United Kingdom. Rheumatology. 2019;58:331–5.
Sakamoto AP, Pinheiro MM, Barbosa CM, Fraga MM, Len CA, Terreri MT. Rituximab use in young adults diagnosed with juvenile idiopathic arthritis unresponsive to conventional treatment: report of 6 cases. Rev Bras Reumatol. 2015;55:536–41 (in English, Portuguese).
Milan M, Pace V, Maiullari F, Chirivì M, Baci D, Maiullari S, et al. Givinostat reduces adverse cardiac remodeling through regulating fibroblasts activation. Cell Death Dis. 2018;9:108.
Giovarelli M, Zecchini S, Catarinella G, Moscheni C, Sartori P, Barbieri C, et al. Givinostat as metabolic enhancer reverting mitochondrial biogenesis deficit in Duchenne Muscular Dystrophy. Pharmacol Res. 2021;170:105751.
Vojinovic J, Damjanov N, D’Urzo C, Furlan A, Susic G, Pasic S, et al. Safety and efficacy of an oral histone deacetylase inhibitor in systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 2011;63:1452–8.
Acknowledgements
We would like to express our sincere gratitude to anonymous reviewers for their valuable comments, which have greatly improved this paper.
Funding
There is no funding in this article.
Author information
Authors and Affiliations
Contributions
LCF developed the concept. ZWJ and DJH drafted the manuscript. All authors have read and approved the final version of the manuscriptfor publication.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, WJ., Deng, JH. & Li, CF. Research progress in drug therapy of juvenile idiopathic arthritis. World J Pediatr 18, 383–397 (2022). https://doi.org/10.1007/s12519-022-00530-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00530-8