Abstract
Purpose
Diabetic patients with chronic kidney disease (CKD) frequently develop cardiac events within several years of the initiation of haemodialysis. The present study assesses the prognostic significance of stress myocardial ECG-gated perfusion imaging (MPI) in patients with diabetic CKD requiring haemodialysis.
Methods
Fifty-five asymptomatic patients with diabetic stage V CKD and no history of heart disease scheduled to start haemodialysis were enrolled in this study (56 ± 11 years old; 49 with type 2 diabetes mellitus). All patients underwent 201Tl stress ECG-gated MPI 1 month before or after the initiation of haemodialysis to assess myocardial involvement. We evaluated SPECT images using 17-segment defect scores graded on a 5-point scale, summed stress score (SSS) and summed difference scores (SDS). The patients were followed up for at least 2 years (42 ± 15 months) to determine coronary intervention (CI) and heart failure (HF) as soft events and acute myocardial infarction (AMI) and all causes of deaths as hard events.
Results
The frequencies of myocardial ischaemia, resting perfusion defects, low ejection fraction and left ventricular (LV) dilatation were 24, 20, 29 and 49%, respectively. Ten events (18%) developed during the follow-up period including four CI, one HF, one AMI and four sudden deaths. Multivariate Cox analysis selected SDS (p = 0.0011) and haemoglobin A1c (HbA1c) (p = 0.0076) as independent prognostic indicators for all events.
Conclusion
Myocardial ischaemia, in addition to glycaemic control, is a strong prognostic marker for asymptomatic patients with diabetic CKD who are scheduled to start haemodialysis. Stress MPI is highly recommended for the management and therapeutic stratification of such patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic chronic kidney disease (CKD) is associated with a higher risk of ischaemic heart disease and/or congestive heart failure, which sometimes leads to fatal cardiac events. Koch et al. reported that actuarial survival 3 years after the beginning of dialysis is 40 and 43% among patients with type 1 and type 2 diabetes, respectively [1]. The major causes of death are myocardial infarction (18%), sudden death (18%) and other cardiac events (18%). Many diabetic patients with a poor prognosis might be unaware of a cardiac condition after starting dialysis because they are frequently asymptomatic. Therefore, appropriate clinical management for diabetic patients with cardiac diseases is very important.
Myocardial perfusion imaging (MPI) can accurately and non-invasively diagnose ischaemic and other cardiac diseases. Furthermore, quantitative ECG-gated single photon emission tomography (QGS) is a useful option for measuring left ventricular size or left ventricular ejection fraction (LVEF). The frequency of cardiac involvement using stress QGS at the start of haemodialysis and how the cardiac condition proceeds to cardiac events or death have not been investigated. Hase et al. reported that diabetic (61%) and non-diabetic end-stage kidney disease at the beginning of haemodialysis treatment proceeded to frequent cardiac events in patients with perfusion defect on MPI [2]. However, the report included patients with known coronary heart disease (CHD) or history of heart failure. Our present study evaluates the involvement of cardiac conditions such as reversible ischaemia, myocardial infarction or cardiac dysfunction in patients with diabetic stage V CKD and no known heart disease at the start of haemodialysis and assesses how these MPI parameters relate to prognosis.
Materials and methods
Patients
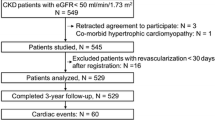
Among consecutive patients with diabetic stage V CKD who started haemodialysis between September 2001 and January 2006 at the Diabetes Centre at our University Hospital, 55 with no apparent history of heart disease or heart attack and who had never undergone cardiac catheterization or MPI to detect heart disease were enrolled in the study. The study protocol was approved by our Institutional Ethics Committee. All patients who provided written, informed consent and who were approved for this study underwent 201Tl stress MPI with quantitative ECG-gated SPECT 1 month before or after starting haemodialysis. Clinical parameters including body mass index (BMI), haemoglobin A1c (HbA1c), duration of diabetes, insulin therapy and resting ECG abnormalities were investigated. The ECG was defined as abnormal if there were abnormal Q wave, ST-T abnormality and complete left bundle branch block (CLBBB). Benign arrhythmias such as single premature atrial or ventricular contraction (PAC or PVC) and lone CRBBB were not defined as an abnormal ECG.
Imaging and stress protocol
For stress imaging, 14 of the patients underwent symptom-limited ergometer exercise testing. At near-maximal exercise, 74–111 MBq of 201Tl was injected, and exercise continued for 1 min. Forty-one patients underwent pharmacological stress testing using 0.14 mg/kg per min of dipyridamole for 4 min instead of exercise testing because of low exercise capacity or lower limb disturbances. Seven minutes later, 74–111 MBq of 201Tl was injected. All patients underwent rest 201Tl imaging 4 h after both types of stress imaging. Perfusion images were acquired by quantitative ECG-gated SPECT (QGS) with dual-head or triple-head gamma cameras (ADAC Vertex, ADAC Laboratories, Milpitas, CA, USA or Toshiba GCA9300, Tokyo, Japan).
Image interpretation
The SPECT images were divided into 17 segments, and visual perfusion of tracer uptake in individual segments was scored as follows: 0, normal; 1, mildly reduced; 2, moderately reduced; 3, severely reduced; and 4, absent [3]. Two nuclear medicine experts interpreted transient myocardial ischaemia and permanent perfusion defects based on the defect score. Summed stress (SSS) and rest (SRS) scores were calculated based on the stress and rest findings. The summed difference score (SDS) was defined as the difference between the SSS and SRS. Myocardial ischaemia was defined as ≥ 2 of SDS.
Values for LV function, namely end-diastolic volume (EDV), end-systolic volume (ESV) and EF, were generated using QGS software. Reduced LV function was defined as EF < 51% and LV dilation was defined as EDV > 105 ml based on our institutional average values of EF and EDV for QGS (LVEF 64 ± 6.4%, EDV 75 ± 15 ml) obtained from individuals without apparent cardiac diseases.
Patient follow-up
The patients were followed up for at least 2 years to determine cardiac events including coronary intervention (CI) such as percutaneous transluminal coronary intervention (PCI) or coronary arterial bypass grafting (CABG). Hard events were defined as acute myocardial infarction (AMI) and all causes of death. Soft events were defined as heart failure (HF) requiring hospitalization and CI at > 3 months after the SPECT study. CI within 3 months after the SPECT was not defined as a cardiac event.
Statistical analysis
Demographic and clinical information is tabulated for patients with or without events. Categorical variables were compared using χ2 tests. Values are expressed as means ± SD. The impact of myocardial ischaemia on hard and total events was computed using the Kaplan-Meier method and compared using the log-rank test. The impact of CI therapy on patients with myocardial ischaemia was similarly computed and compared. Relationships between cardiac events and all continuous variables were analysed using univariate and multivariate Cox proportional hazards regression models.
Results
Twenty-nine patients underwent gated SPECT before haemodialysis, and 26 patients underwent the procedure after haemodialysis. Haemodialysis was introduced 2.0 ± 18 days after the SPECT study. No significant difference in clinical background such as age, HbA1c and SPECT data such as perfusion defect score, EDV, ESV and EF was observed between the predialytic and the postdialytic groups.
Among all 55 patients, QGS MPI revealed transient myocardial ischaemia in 22%, resting perfusion defects in 20%, low EF (< 51%) in 29% and LV dilation (EDV > 105 ml ) in 49%. The SSS, SRS and SDS were 3.51 ± 4.75, 2.22 ± 2.63 and 1.55 ± 3.32, respectively. The EDV, ESV and EF were 110 ± 39 ml, 54 ± 30 ml and 56 ± 11%, respectively. At the start of haemodialysis, 65% of the patients had at least one abnormality indicating cardiac involvement.
We divided the whole cohort of patients into ischaemia positive (n = 12) and negative groups (n = 43). There was a significant difference in HbA1c (higher in ischaemia positive, p = 0.036), ECG abnormality, stress EF and rest EF (p = 0.0075; 0.0035; 0.0072), whereas there was no difference in age, sex, BMI, insulin use and diabetes mellitus (DM) type (1 or 2).
Eleven patients (20%) showed an ECG abnormality including abnormal Q wave (n = 1), LVH-type ECG (high voltage + strain type ST depression) (n = 3) and inverted T wave (n = 7). The abnormality was associated with ESV (χ2 = 11.3) and SDS (χ2 = 6.34) by multivariate stepwise regression analysis (χ2 = 12.5, p < 0.0001).
During a mean follow-up period of 42 ± 15 months (range: 14–75 months), five soft events including four CI (> 3 months after the MPI study) and one severe HF and five hard events including one AMI and four sudden deaths occurred.
Of six patients who underwent CI (five PCI and one CABG), five had no hard events after therapy. Of five patients with hard events, PCI was recommended for three of them based on the MPI results, but all three refused this option. One patient underwent PCI, but died 4.8 years after MPI and one patient had no abnormalities on MPI, but died of unknown causes. Table 1 shows the characteristics of the study patients with and without events.
There were two patients who received PCI at over 3 months after SPECT imaging. One underwent CABG 4.4 months after the imaging because she still sometimes had chest pain even after medical therapy, and another awaiting haemodialysis underwent intervention 4.2 months after the imaging. There were two patients who underwent PCI within 3 months after SPECT imaging. One of the patients proceeded to unstable angina 56 months after the first PCI, and another had no cardiac event during the follow-up (36 months) afterward.
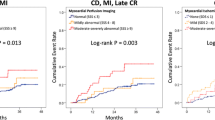
Figure 1 compares event-free survival curves in patients with ischaemia and no ischaemia on MPI. The total event rate was significantly higher in the group with ischaemia than in the group without (58 vs 7.0%, p < 0.0001, log-rank test). The hard event rate was also significantly higher in the group with ischaemia than in the group without (33 vs 2.3%, p = 0.0006, log-rank test).
Univariate Cox hazard analysis revealed that the dependent variables for total events were SDS, HbA1c, EF, abnormal ECG and SSS, whereas those for hard events were HbA1c and SDS (Tables 2 and 3). A multivariate model was applied based on these results using variables with p < 0.05 in a forward stepwise fashion. The independent variables were SDS and HbA1c for total events (χ2 = 11.7, p = 0.0029).
The proper cut-off point of HbA1c for both soft and hard cardiac events was 7.5% according to the statistical analysis. Event-free survival curves divided by the cut-off point of HbA1c among patients with myocardial ischaemia are shown in Fig. 2. Event-free survival rates are significantly higher among patients with HbA1c < 7.5% than in those with HbA1c ≥ 7.5% (p = 0.0123).
Discussion
The present results indicated that asymptomatic patients with diabetic stage V CKD at the start of haemodialysis frequently have cardiac abnormalities such as myocardial ischaemia, infarction, reduced cardiac function or LV dilation.
Diabetes is a strong risk factor for CHD because of coronary macrovascular stenosis based on progressive atherosclerosis. A significant proportion of diabetic patients are unaware of myocardial ischaemia, which frequently leads to silent myocardial infarction or coronary multiple vessel disease. Diabetic patients with CKD, which is an independent risk factor for CHD [4], are at much higher risk. Stress MPI found that 24% of our study population had reversible ischaemia, which was the most significant predictor for cardiac events among all types of myocardial involvement. A study using coronary angiography has shown that 63% (15/24) of enrolled Japanese patients had coronary stenosis before starting haemodialysis [5]. The difference in the prevalence of CHD between that and the present study depends on the estimation method, since MPI is functional imaging based on myocardial blood flow, whereas coronary stenosis is only a morphological estimation, which does not always mean insufficient myocardial blood flow under stress. The prognosis of patients with CHD can be good if perfusion imaging findings are normal [6, 7]. The present study found that the event rate of patients with ischaemia was higher (total event rate: 58%, death rate: 33%), whereas the prognosis of patients without ischaemia was much better (total event rate: 7.0%, death rate: 2.3%). Myocardial ischaemia is a reliable predictor for prognosis and a higher negative predictive value is of considerable significance for clinicians. In the present study, patients with myocardial ischaemia had significantly higher HbA1c and lower LVEF. Furthermore, an ECG abnormality was more frequently observed in the ischaemic patients. Therefore, stress SPECT imaging is indispensable to the patients with either high HbA1c or an ECG abnormality among patients at the start of haemodialysis.
Some patients develop severe cardiac dysfunction without reversible ischaemia, which is considered diabetic cardiomyopathy with no apparent macrovascular coronary lesions [8]. Previous studies suggest that ESV and EF measured by gated SPECT are independent predictors of cardiac events [9, 10]. We performed the SPECT study for the patients in hospital for the initiation of haemodialysis within 1 month before or after the start of haemodialysis. During the periods, however, such patients generally still have unstable haemodynamics, and the LV cavity particularly tends to be enlarged. Therefore, EDV is likely to be overestimated, and some patients may show underestimation of EF during the periods. A low EF, which was observed in 29% of our patients, is supposed to induce HF during follow-up, but only one of our patients progressed to HF. In addition, the patient had no severely depressed LV function and LV dilatation (EF: 59%, EDV: 124 ml), thus the situation does not seem to have affected the prognostic evaluation. Actually EF was not an independent predictor for this event according to multivariate analysis. This result might be due to regular and strict management of the water balance during haemodialysis determined from the understanding of cardiac status revealed by MPI. EDV was not a significant predictor of HF because an enlarged ventricular cavity can be caused generally not only by compensatory dilatation against severely depressed LV function (remodelling) but also volume overload due to dysregulation of the water balance in the presence of severe kidney disease. A higher EDV alone without low EF would be improved after removing fluid overload by ultrafiltration during haemodialysis.
CI reduces the mortality of patients with CHD on haemodialysis, especially among those with high-risk diabetes [11, 12]. The present study found that three patients with myocardial ischaemia according to MPI, but who refused CI therapy, died within 3 years. CI should be recommended for high-risk diabetic patients with myocardial ischaemia who are on haemodialysis to prevent cardiac events at least in the short term. However, a recent paper suggests that patients on haemodialysis who undergo PCI have higher restenosis rates (22%) even when using drug-eluting stents (DES) [13]. Another study found that 38% of enrolled patients on haemodialysis developed de novo coronary stenotic lesions (> 50%) at 6 months after PCI [14]. Therefore, diabetic patients on haemodialysis should be carefully followed up after PCI by regular MPI to reduce long-term mortality. CABG is also an important alternative for coronary revascularization for multi-vessel coronary disease. It is reported that dialysis patients had better long-term survival after CABG surgery than after PCI (2-year mean survival rate: 56.4 vs 48.4 %) [15]. CABG may be recommended for patients with multi-vessel disease or large area of ischaemia as determined by stress SPECT, who are waiting for start of haemodialysis.
HbA1c was also a predictive factor for the event in the present study. A single blood HbA1c value obtained during the same period as MPI might not reflect glycaemic control during follow-up. However, a recent report suggests that poor glycaemic control (≥ HbA1c 8.0%) during the first 3 months after starting haemodialysis is an independent predictor of prognosis among diabetic stage V CKD patients on regular haemodialysis [16]. Our results support some of these published results. Actually when patients with myocardial ischaemia were further categorized by the cut-off point of 7.5% of HbA1c, patients with a higher HbA1c value had more cardiac events, which suggests the usefulness of prognostic evaluation by a combination of myocardial ischaemia with serum marker of HbA1c.
Abnormal resting ECG findings were also a significant predictor for events in the present study. ST-T change such as ST depression or inverted T wave was a main abnormal finding of resting ECG (7 of 11 patients), which generally reflects LV hypertrophy or repeated episodes of myocardial ischaemia. Actually the abnormality was not associated with SRS, but ESV and SDS, which indicated that LV remodelling together with myocardial ischaemia might result in electrocardiographic changes among diabetic patients with stage V CKD.
The present finding of a 9.1% hard event rate over an average 3.5 years of follow-up was much lower than the 43% death rate described in a surveillance study including patients with previous ischaemic heart disease in Germany [1]. The difference in the event rate between the findings of that study and ours could be due to several factors such as the 20-year interval between the studies, lifestyle differences between Germany and Japan [10] and/or a post-screening management bias as well as the patient selection bias. Hase et. al reported from Japan that diabetic and non-diabetic stage V CKD patients without previous history of heart disease had around an 8% hard event rate (AMI and cardiac death) for 2 years [17], which is about the same event rate as that in our study. The recent Japanese multi-centre J-ACCESS study of patients with suspected CHD [10] indicated that MPI and gated SPECT findings are significant prognostic indicators, and the hard event rate in Japan was much lower than that found in a US study (2.4%/3 years vs 2.6%/year) [7]. Although our study population did not include patients with known CHD, the higher hard event rate (9.1%/3.5 years) than that found by J-ACCESS indicated that Japanese diabetic patients with stage V CKD scheduled for haemodialysis are still at high risk for CHD or sudden cardiac death. Careful monitoring during follow-up and screening for myocardial involvement are warranted to extend long-term survival.
One limitation of our study is that few patients were enrolled from a single institution. However, the outcome of the study might be reasonable as speculated from the numbers of prognostic CHD studies [7, 10, 18]. A multi-centre trial is required to confirm the prognostic significance of our findings in the same clinical setting.
Conclusion
Our study suggested that myocardial involvement is frequent among patients with diabetic stage V CKD and no known CHD according to stress gated MPI who are scheduled to start haemodialysis. Among many risk parameters, myocardial ischaemia, in addition to glycaemic control, was a strong prognostic marker for events during follow-up. Stress MPI is highly recommended for patient management and for the therapeutic stratification of patients with diabetic stage V CKD before starting haemodialysis.
References
Koch M, Thomas B, Tschöpe W, Ritz E. Survival and predictors of death in dialysed diabetic patients. Diabetologia 1993;36:1113–7. doi:10.1007/BF02374508.
Hase H, Joki N, Ishikawa H, Fukuda H, Imamura Y, Saijyo T, et al. Prognostic value of stress myocardial perfusion imaging using adenosine triphosphate at the beginning of haemodialysis treatment in patients with end-stage renal disease. Nephrol Dial Transplant 2004;19:1161–7. doi:10.1093/ndt/gfh037.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539–42. doi:10.1161/hc0402.102975.
Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med 2004;164:659–63. doi:10.1001/archinte.164.6.659.
Joki N, Hase H, Nakamura R, Yamaguchi T. Onset of coronary artery disease prior to initiation of haemodialysis in patients with end-stage renal disease. Nephrol Dial Transplant 1997;12:718–23. doi:10.1093/ndt/12.4.718.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535–43.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Stress myocardial perfusion single-photon emission computed tomography is clinically effective and cost effective in risk stratification of patients with a high likelihood of coronary artery disease (CAD) but no known CAD. J Am Coll Cardiol 2004;43:200–8. doi:10.1016/j.jacc.2003.07.043.
Poornima IG, Parikh P, Shannon RP. Diabetic cardiomyopathy: the search for a unifying hypothesis. Circ Res 2006;98:596–605. doi:10.1161/01.RES.0000207406.94146.c2.
Sharir T, Germano G, Kavanagh PB, Lai S, Cohen I, Lewin HC, et al. Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation 1999;100:1035–42.
Nishimura T, Nakajima K, Kusuoka H, Yamashina A, Nishimura S. Prognostic study of risk stratification among Japanese patients with ischemic heart disease using gated myocardial perfusion SPECT: J-ACCESS study. Eur J Nucl Med Mol Imaging 2008;35:319–28. doi:10.1007/s00259-007-0608-x.
Hase H, Joki N, Nakamura M, Tsunoda T, Tanaka Y, Fukazawa M, et al. Favourable long-term outcome by repeated percutaneous coronary revascularization in diabetic haemodialysis patients. Nephrol Dial Transplant 2002;17:100–5. doi:10.1093/ndt/17.1.100.
Yasuda K, Kasuga H, Aoyama T, Takahashi H, Toriyama T, Kawade Y, et al. Comparison of percutaneous coronary intervention with medication in the treatment of coronary artery disease in hemodialysis patients. J Am Soc Nephrol 2006;17:2322–32. doi:10.1681/ASN.2005090958.
Aoyama T, Ishii H, Toriyama T, Takahashi H, Kasuga H, Murakami R, et al. Sirolimus-eluting stents vs bare metal stents for coronary intervention in Japanese patients with renal failure on hemodialysis. Circ J 2008;72:56–60. doi:10.1253/circj.72.56.
Nishimura M, Tokoro T, Nishida M, Hashimoto T, Kobayashi H, Yamazaki S, et al. Association of insulin resistance with de novo coronary stenosis after percutaneous coronary artery intervention in hemodialysis patients. Nephron Clin Pract 2008;109:c9–17. doi:10.1159/000132391.
Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation 2002;106:2207–11. doi:10.1161/01.CIR.0000035248.71165.EB.
Oomichi T, Emoto M, Tabata T, Morioka T, Tsujimoto Y, Tahara H, et al. Impact of glycemic control on survival of diabetic patients on chronic regular hemodialysis: a 7-year observational study. Diabetes Care 2006;29:1496–500. doi:10.2337/dc05-1887.
Hase H, Tsunoda T, Tanaka Y, Takahashi Y, Imamura Y, Ishikawa H, et al. Risk factors for de novo acute cardiac events in patients initiating hemodialysis with no previous cardiac symptom. Kidney Int 2006;70:1142–8. doi:10.1038/sj.ki.5001726.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900–7. doi:10.1161/01.CIR.0000072790.23090.41.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Momose, M., Babazono, T., Kondo, C. et al. Prognostic significance of stress myocardial ECG-gated perfusion imaging in asymptomatic patients with diabetic chronic kidney disease on initiation of haemodialysis. Eur J Nucl Med Mol Imaging 36, 1315–1321 (2009). https://doi.org/10.1007/s00259-009-1110-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1110-4