Abstract
Background
Left ventricular diastolic dyssynchrony (LVDD) can be assessed by gated myocardial perfusion single-photon emission computed tomography (GMP-SPECT). LVDD is an area of interest in subjects who underwent cardiac resynchronization therapy (CRT). The aim of this post hoc analysis was to assess the role of LVDD in subjects with CRT who were followed up at 6-month period.
Material & Methods
Left ventricular diastolic dyssynchrony was assessed by GMP-SPECT at baseline and after CRT procedure in 160 subjects from 10 different cardiological centers. CRT procedure was performed as per current guidelines. Outcomes were defined as improvement in ≥1 New York Heart Association (NYHA) class, left ventricular ejection fraction (LVEF) by 5%, and reduction in end-systolic volume (ESV) by 15% and 5% points in Minnesota Living with Heart Failure Questionnaire. LVDD was defined as diastolic phase standard deviation ≥40 ± 14°.
Results
Improvement in NYHA functional class occurred in 105 (65.6%), LVEF in 74 (46.3%), decrease in ESV in 86 (53.8%), and Minnesota score in 85 (53.1%) cases. Baseline LV diastolic standard deviation was 53.53° ± 20.85 and at follow-up 40.44° ± 26.1283; (P < 0.001). LVDD was not associated with improvement in clinical outcomes at follow-up.
Conclusion
CRT improves both systolic and diastolic dyssynchrony values at 6-month follow-up. LVDD at baseline is correlated with cardiac functionality at follow-up, but not with overall favorable clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular systolic dyssynchrony (LVSD) is an important pathophysiological condition in subjects with heart failure due to its correlation with cardiac adverse events.1,2 Additionally, left ventricular diastolic dyssynchrony (LVDD), a dyssynchronous relaxation pattern, plays an important role in subjects with heart failure.3,4,5 In subjects with acute heart failure, left bundle branch block can cause LVDD leading to a marked alteration of left ventricular filling, which could compromise the hemodynamic function in subjects with heart failure.3,4 LVDD is associated with adverse clinical outcomes in patients with dilated cardiomyopathy.6 Furthermore, LVDD improves in responders but not in non-responders after cardiac resynchronization therapy (CRT), resulting in reduction of morbidity and mortality.7,8 The mechanical dyssynchrony of the left ventricle, the site of latest mechanical activation site, and the myocardial scarring are important parameters related to the CRT response.9,10 Image methods to assess both LVSD and LVDD, cardiac functionality, and prognosis include tissue Doppler imaging, which is a safe and cost-viable method for the assessment of left ventricular diastolic relaxation patterns. Nevertheless, this technique remains observer-dependent and requires substantial experience for its interpretation.7,11,12 Gated Myocardial Perfusion Single-Photon Emission Computed Tomography (GMP-SPECT) is another non-invasive technique for the evaluation of mechanical LVSD and LVDD.13,14 Currently, the phase analysis of GMP-SPECT has received increasing attention, because it provides robust, reproducible, and high inter-observer correlation measurements of mechanical LVDD using automated approach that is correlated with other image methods.15,16 The International Atomic Energy Agency (IAEA) has sponsored a non-randomized multicenter trial: “Value of the assessment of intraventricular synchronism by GMP-SPECT in the management of patients with heart failure undergoing cardiac resynchronization therapy.”17 This novel branch of the previous study is a post hoc retrospective analysis of diastolic dyssynchrony values obtained from the IAEA VISION-CRT study aimed to assess the clinical role of LVDD quantified by GMP-SPECT in the prediction of 6-month clinical outcomes in subjects with ischemic cardiomyopathy who underwent CRT.
Subjects and Methods
Subject Assessment
This is a collaborative prospective study that involved 10 cardiological centers in eight different countries (Brazil, Chile, Colombia, Cuba, India, Mexico, Pakistan and Spain). We included subjects ≥ 18 years old with NYHA functional class II, III, or ambulatory IV, for at least 4 months before enrollment, LVEF ≤ 35% independently of ischemic cause, QRS duration ≥ 120 ms with morphology of left bundle branch block and in sinus rhythm. We excluded subjects with any type of arrhythmia that prevented GMP-SPECT acquisition, comorbidities that limited their life expectative for less than one year, women who were pregnant or breastfeeding at the moment of the enrollment, and subjects whom underwent coronary artery bypass grafting or percutaneous coronary intervention in the last 3 months before the CRT implantation. These subjects were assessed at baseline and at 6-month follow-up by GMP-SPECT and a complete clinical evaluation using standardized questionnaires by qualified physicians. We directly asked for self-reported history of arterial hypertension, dyslipidemia, smoking, and previously reported myocardial infarction. Furthermore, we assessed Minnesota Living with Heart Failure Questionnaire (MLHFQ).18 We evaluate cardiac functionality through GMP-SPECT including left ventricular ejection fraction (LVEF), left ventricular end-systolic (LVESV) and end-diastolic volume (LVEDV), left ventricular mass (LV Mass), left ventricular systolic phase standard deviation (LVSPSD), left ventricular diastolic phase standard deviation (LVDPSD), end-systolic eccentricity index (ESEI), and end-diastolic eccentricity index (EDEI). At follow-up, we reported the use of medication and the incidence of cardiovascular events, the complications, and deaths. Complete study design, clinical measurements, and CRT methodology are published elsewhere.18 The study was approved by the ethics committee of each center. All subjects where anonymized during the data analysis. All subjects signed informed consent and all procedures were done according to the Declaration of Helsinki.
GMP-SPECT Assessment
Emory University (USA) was the core lab for centralized GMP-SPECT reconstruction, processing, and phase analysis. The core lab was blinded as to each patient’s clinical and CRT information. The GMP-SPECT scans were assessed using 740 to 1100 MBq (20 to 30 mCi) of 99mTc-sestamibi or tetrofosmin protocols. The patients came to the study without previous use of caffeine and alcohol and they were instructed to stop smoking. All the images were acquired in a dual-headed camera using 180° orbits with a complementary 8 or 16 frames ECG-gating, according to current guideline.19 All the images were reconstructed using the OSEM method with three iterations and ten subsets and filtered by a Butterworth filter, power 10, using a cut-off frequency of 0.3 cycles/mm. Reorientation into short-axis images were sent to Emory Cardiac Toolbox (ECTb4, Atlanta, GA) for automatized processing of perfusion, function, and phase dyssynchrony analysis. GMP-SPECT was assessed before CRT implantation (median days before GMP-SPECT acquisition: 5 [IR: 2 to 16]) and 6-months follow-up.
Clinical Outcomes
Improvement of clinical response was defined as at least one of the following outcomes at 6-month follow-up: improvement in at least 1 NYHA functional class score; improvement of LVEF (%) by 5%, reduction of LVESV (mL) by ≥ 15% and improvement in at least five points in MLHFQ. Absolute change at follow-up was defined as the difference between values at follow-up minus the values at baseline. Incident events included myocardial infarction, cardiac transplantation, hospitalization due to any cause related to heart failure, and CRT complications. Left ventricular diastolic dyssynchrony (LVDD) was defined as diastolic phase standard deviation ≥ 40 ± 14°.14,20
Statistical Analysis
Paired Student’s t test and Wilcoxon rank sign test was used to evaluate differences at baseline and follow-up wherever appropriate. Frequency distribution of categorical variables is presented as absolute frequency and percentage. Data are presented as mean (± SD) or median (interquartile range) wherever appropriate. Logarithmic transformation was performed in variables that did not achieve normal distribution. We seek to evaluate the incidence of events (favorable clinical outcomes) due to a specific follow-up time, and therefore we used Poisson regression analysis to estimate the incidence rate ratio of clinical outcomes as model accorded time. Furthermore, we performed linear regression analysis to assess the association and variability with absolute changes (Δ) in clinical outcomes and the association of LVDD and cardiac functionality at follow-up. The Akaike information criterion (AIC) was also calculated for extracting better model and evaluation of increases in informative capacity of our fitted models. Statistical analysis was performed using Statistical Package for Social Sciences Software (SPSS, version 21.0), R software (Version 3.5.1), and GraphPad Prism (Version 6.0). A P value < 0.05 was taken as statistically significant.
Results
Study Population
At baseline, we enrolled 198 subjects who underwent CRT procedure; nevertheless, only 160 subjects had complete clinical and GMP-SPECT information at baseline. Twenty patients died before second visit (Figure 1). There was male predominance (60.6%) with high prevalence of comorbidities including arterial hypertension (55.6%), smoking (16.3%), dyslipidemia (27.5%), and type 2 diabetes (23.8%). At least 30 (18.8%) subjects have had previous history of coronary artery disease (CAD). Ethnicity was Hispanic predominant (55.6%).
Medication history at follow-up included use of beta blockers (85.2%), angiotensin II receptor blocker (ARB) (23.1 %), diuretics (75.6%), ACE inhibitors (59.4%), aspirin (43.8%), and statins (31.3%). Only 4 (2.5%) subjects were using both ARB and ACE inhibitors at the same time (Table 1). Predominant NYHA functional class at baseline was III in 59.1%.
Subjects had reduced LVEF at baseline (25%; IR: 17 to 35.5) with increased LVESV (162 mL; IR: 114 to 243), LVEDV (220 mL; IR: 166 to 316), LV Mass (200 gr; IR: 169 to 243.5), and LVSPSD (58°; IR: 36.2 to 75.2) (Table 2). There was a statistically significant change in LVEF, LVESV, LVEDV, LV Mass, LVSPSD, and LVDPSD at follow-up. ESEI and EDEI did not shown significant changes at follow-up. As an example, we chose a patient whose values are portrayed in Figure 2.
This is an example of the automatized analysis made with 99mTc-MIBI SPECT and reported no evidence of infarction or ischemia, LVEF-34%, LVEDV-193 mL, LVESV-128 mL, diastolic standard deviation-58.4°. San Jude cardiac resynchronizer was placed in DDD mode. At follow-up, the patient improved LVEF to 40%, LVEDV decreased to 160 mL, LVESV decreased to 97 mL, and diastolic standard deviation improved to 26.2°
Clinical Outcomes
NYHA functional class improved in 105 (65.6%) subjects by at least 1 NYHA functional class. There was an improvement in LVEF by at least ≥ 5% in 74 (46.3%) subjects and decrease in LVESV by at least 15% in 86 (53.8%) subjects. Improvement in Minnesota score by at least five points occurred in 85 (53.1%) cases. Totally, there was a favorable clinical outcome in 132 (82.5%) subjects, in which 25 (16.6%) archive one, 45 (28.1%) two, 45 (28.1%) three, and 22 (13.8%) four favorable clinical outcomes. Incident myocardial infarction occurred in 1 (0.6%) subject, 19 (9.5%) required hospitalization for any cause and nobody underwent cardiac transplantation.
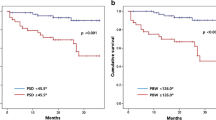
Left Ventricular Diastolic Dyssynchrony
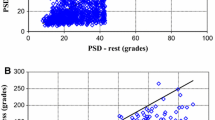
Complete and detailed values of segmental walls of the GMP-SPECT diastolic dyssynchrony of the population of study are presented in Supplementary Table 1. At baseline, LVDPSD was 53.53° (± 20.85), ESEI 0.613 (IR: 0.490 to 0.697), and EDEI 0.570 (IR: 0.646 to 0.449). Baseline LVDD was present in 81 (50.6%) and at follow-up in 42 (32.3%) subjects (P < 0.001). Left ventricular systolic dyssynchrony (LVSD) was present in 124 (77.5%) subjects and at follow-up in 91 (57.9%) (P < 0.001) (Table 2). There was a statistically significant change in LVDPSD at follow-up (P < 0.001), but no for ESEI (P = 0.408) and EDEI (P = 0.897) (Figure 3). Furthermore, all segments had a statistically significant change at follow-up, except for the basal-inferior (P = 0.561) and the apical-lateral (P = 0.981) segments (Supplementary Table 1). We found a significant correlation between LVDPSD at baseline and LVEF (r = − 0.541, 95% CI − 0.652 to − 0.406), LVESV (r = 0.562, 95% CI 0.431 to 0.670), LVEDV (r = 0.531, 95% CI 0.395 to 0.645), and LV Mass (r = 0.461, 95% CI 0.312 to 0.587) at follow-up. In the linear regression analysis, we found that LVDPSD at baseline was associated with LVEF (β = − 0.336), LVESV (β = − 2.161), LVEDV (β = − 1.991), and LV Mass (β = − 0.849) at follow-up after adjusting for ESEI and EDEI, age, and sex (Figure 4). Furthermore, in the Poisson regression analysis, we found that there was not a significant association between any diastolic dyssynchrony values for improvement of clinical response, even in the stratification for clinical outcomes (Table 3). These results were replicable in the absolute changes in clinical outcomes at follow-up (Supplementary Tables 2, 3). Finally, in our linear regression models, EDEI and LVDPSD were associated with changes in NYHA functional class and LVEF, respectively, but did not reach statistical significance (Supplementary Table 3).
Systolic and diastolic phase standard deviation values (A), dyssynchrony frequency and percentage (B), end-systolic (C) and end-diastolic, (D) eccentricity indexes at baseline and follow-up in subjects of VISION-CRT. LVSD left ventricular systolic dyssynchrony; LVDD left ventricular diastolic dyssynchrony; ES end systolic; ED end diastolic. ***P value < 0.001; systolic dyssynchrony as defined as phase SD ≥ 43° and diastolic phase standard deviation ≥ 40 ± 14°
Correlation of diastolic phase SD at baseline with LVEF (A), LVESV (B), LVEDV (C), and LV Mass (D) at follow-up. LVEF-FU left ventricular ejection fraction at follow-up; LVESV-FU left ventricular end-systolic volume at follow-up; LVEDV-FU left ventricular end-diastolic volume at follow-up; LV mass at follow-up; SD standard deviation. R2 adjusted for ES and ED eccentricity, sex, and age
In addition, we also found that the standard deviation of the systolic phase was not associated as an independent predictor for clinical outcomes (Supplementary Table 4).
Discussion
This study compiles the results of cardiac dyssynchrony in subjects who underwent CRT and were followed by 6 months. We found that CRT improves cardiac functionality in both systolic and diastolic dyssynchrony assessed with GMP-SPECT. Furthermore, we found that most of the subjects had a favorable clinical response at follow-up in which the improvement of functional class was the most frequent (65.6%). Finally, we found a strong association of LVDPSD with cardiac functionally (LVEF, LVESV, LVEDV, and LV Mass) at follow-up. We also report that LVDPSD was not associated with any favorable outcome in the period of study.
Previous studies have shown that LVDD plays an important role in subjects with heart failure, independently of the cause.3,4,5 As a consequence, LV diastolic dyssynchrony is related to alterations in the diastolic filling pattern of the left ventricle, which may further compromise the hemodynamic function of the failing heart.3,4
Phase analysis in GMP-SPECT has proven to be a novel method with high robust, reproductible, and accurate measurements to evaluate mechanical dyssynchrony, mechanical activation pattern, and myocardial perfusion using an automated approach.7,11 Previous studies have compared its correlation and performance with tissue Doppler imaging and real-time 3-dimensional echocardiography, showing good correlation with systolic and diastolic standard deviation in subjects with heart failure.9,20,21 Nevertheless, the main focus of mechanical dyssynchrony has been in LV systolic phase, leaving the evaluation of LVDD as an area of opportunity for further studies. A previous study has evaluated the effect of LV systolic phase and its role in subjects with CRT and found that at follow-up, there was an improvement in both LV remodeling and diastolic dyssynchrony, especially in those with lateral lead location.22 It has been previously suggested that CRT implantation should be considered for subjects with baseline LV mechanical dyssynchrony and performed with LV pacing lead placed in the site of latest mechanical activation with viable myocardium with favorable response; nevertheless, this evaluation had been shown to be retrospectively.20 A recent review suggests that targeting mechanical dyssynchrony instead of electrical dyssynchrony can potentially improve the prognosis in subjects who underwent CRT and these could also be a predictable factor for clinical outcomes.23 The use of diastolic dyssynchrony as an independent predictor to evaluate adverse clinical outcomes and mortality has been previously explored in subjects with history of CAD.24 Although our results shown that LVDD and LVSD were not associated with overall favorable clinical response, the improvement in both systolic and diastolic dyssynchrony was significant, suggesting its importance in the evaluation of subjects who underwent CRT.
Strengths and Limitations
This study was an international multicenter collaboration of eight countries receiving diverse representative population, so it can be reproduced in other countries. Second, the phase analysis of both systolic and diastolic cardiac dyssynchrony values were made using automatized central core lab without the interference of any physician, leading to a high reproductible technique and results.
Nevertheless, some limitations need to be acknowledged. The study was not designed as a randomized clinical trial due to the intervention of electrophysiologists in the implantation of CRT guided by their respective guidelines and not by the GMP-SPECT results. Second, the time of follow-up was established under the hypothesis for assessment of the favorable clinical outcomes in these subjects; nevertheless, this may be a potential explanation in the poor association between diastolic dyssynchrony and favorable outcomes, meaning that a longer period of follow-up may be necessary to evaluate real changes in clinical outcomes. Third, the echocardiographic data were incomplete, and therefore the comparison between GMP-SPECT and Echo could not be made. Fourth, we used phase standard deviation values for our analysis leaving other parameters for measure dyssynchrony that are less dependent of histogram shape, such as entropy, as an area of opportunity for further studies.
Conclusion
In our study, CRT improves both systolic and diastolic dyssynchrony values at 6-month follow-up. LVDD at baseline is correlated with cardiac functionality at follow-up, but not with overall favorable clinical outcomes. Further investigation with longer follow-up period is needed to assess LVDD in CRT response.
New Knowledge Gained
In our study, CRT improves both systolic and diastolic dyssynchrony values assessed by GMP-SPECT, but does not predict favorable clinical outcomes at 6-month follow-up.
Abbreviations
- MLHFQ:
-
Minnesota living with heart failure questionnaire
- CRT:
-
Cardiac resynchronization therapy
- LVSD:
-
Left ventricular systolic dyssynchrony
- LVDD:
-
Left ventricular diastolic dyssynchrony
- LVSPSD:
-
Left ventricular systolic phase standard deviation
- LVDPSD:
-
Left ventricular diastolic phase standard deviation
- ESEI:
-
End-systolic eccentricity index
- EDEI:
-
End-diastolic eccentricity index
- GMP-SPECT:
-
Gated myocardial perfusion single-photon emission computed tomography
References
Bader H, Garrigue S, Lafitte S, Reuter S, Jais P, Haissaguerre M, et al. Intra-left ventricular electromechanical asynchrony. A new independent predictor of severe cardiac events in heart failure patients. J Am Coll Cardiol 2004;43:248-56.
Cho GY, Song JK, Park WJ, Han SW, Choi SH, Doo YC, et al. Mechanical dyssynchrony assessed by tissue Doppler imaging is a powerful predictor of mortality in congestive heart failure with normal QRS duration. J Am Coll Cardiol 2005;46:2237-43.
Schuster I, Habib G, Jego C, Thuny F, Avierinos JF, Derumeaux G, et al. Diastolic asynchrony is more frequent than systolic asynchrony in dilated cardiomyopathy and is less improved by cardiac resynchronization therapy. J Am Coll Cardiol 2005;46:2250-7.
Xiao HB, Lee CH, Gibson DG. Effect of left bundle branch block on diastolic function in dilated cardiomyopathy. Br Heart J 1991;66:443-7.
Waggoner AD, Rovner A, de las Fuentes L, Faddis MN, Gleva MJ, Sawhney N, et al. Clinical outcomes after cardiac resynchronization therapy: Importance of left ventricular diastolic function and origin of heart failure. J Am Soc Echocardiogr 2006;19:307-13.
Friedberg MK, Roche SL, Mohammed AF, Balasingam M, Atenafu EG, Kantor PF. Left ventricular diastolic mechanical dyssynchrony and associated clinical outcomes in children with dilated cardiomyopathy. Circ Cardiovasc Imaging 2008;1:50-7.
Shanks M, Bertini M, Delgado V, Ng AC, Nucifora G, van Bommel RJ, et al. Effect of biventricular pacing on diastolic dyssynchrony. J Am Coll Cardiol 2010;56:1567-75.
Cleland JGF, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539-49.
Boogers MJ, Chen J, van Bommel RJ, Borleffs CJ, Dibbets-Schneider P, van der Hiel B, et al. Optimal left ventricular lead position assessed with phase analysis on gated myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 2011;38:230-8.
Khan FZ, Virdee MS, Palmer CR, Pugh PJ, O’Halloran D, Elsik M, et al. Targeted left ventricular lead placement to guide cardiac resynchronization therapy: The TARGET study: A randomized, controlled trial. J Am Coll Cardiol 2012;59:1509-18.
Wang J, Kurrelmeyer KM, Torre-Amione G, Nagueh SF. Systolic and diastolic dyssynchrony in patients with diastolic heart failure and the effect of medical therapy. J Am Coll Cardiol 2007;49:88-96.
Yu CM, Zhang Q, Yip GW, Lee PW, Kum LC, Lam YY, et al. Diastolic and systolic asynchrony in patients with diastolic heart failure: a common but ignored condition. J Am Coll Cardiol 2007;49:97-105.
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med 2007;48:1104-11.
Henneman MM, Chen J, Ypenburg C, Dibbets-Schneider P, Bleeker GB, Boersma E, et al. Phase analysis of gated myocardial perfusion single-photon emission computed tomography compared with tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol 2007;49:1708-14.
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, et al. Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssyn-chrony. Nucl Med Commun 2008;29:374-81.
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P, et al. Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol 2010;17:811-6.
Peix A, Karthikeyan G, Massardo T, Kalaivani M, Patel C, Pabon LM, et al. Value of intraventricular dyssynchrony assessment by gated-SPECT myocardial perfusion imaging in the management of heart failure patients undergoing cardiac resynchronization therapy (VISION-CRT). J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-018-01589.
Rector T. Patient’s self-assessment of their congestive heart failure: Reliability and validity of a new measure-The Minnesota Living with Heart Failure Questionnaire. Heart Fail 1987;3:198.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016;23:606-39. https://doi.org/10.1007/s12350-015-0387-x.
Boogers MJ, Chen J, Veltman CE, van Bommel RJ, Mooyaart EA, Al Younis I, et al. Left ventricular diastolic dyssynchrony assessed with phase analysis of gated myocardial perfusion SPECT: A comparison with tissue Doppler imaging. Eur J Nucl Med Mol Imaging 2011;38:2031-9. https://doi.org/10.1007/s00259-011-1870-5.
Marsan NA, Henneman MM, Chen J, Ypenburg C, DibbetsSchneider P, Ghio S, et al. Real-time 3-dimensional echocardiography as a novel approach to quantify left ventricular dyssynchrony: A comparison study with phase analysis of gated myocardial perfusion single photon emission computed tomography. J Am Soc Echocardiogr 2008;21:801-7.
Rovner A, de Las Fuentes L, Faddis MN, Gleva MJ, Davila-Roman VG, Waggoned AR. Relation of left ventricular lead placement in cardiacresynchronization therapy to left ventricular reverse remodelingand to diastolic dyssynchrony. Am J Cardiol 2007;99:239-41.
Fudim M, Dalgaard F, Fathallah M, Iskandrian AE, Borges-Neto S. Mechanical dyssynchrony: How do we measure it, what it means, and what we can do about it. J Nucl Cardiol 2019
Fudim M, Fathallah M, Shaw LK, Liu PR, James O, Samad Z, et al. The prognostic value of diastolic and systolic mechanical left ventricular dyssynchrony among patients with coronary heart disease. JACC Cardiovasc Imaging 2019;12:1215-26.
Disclosure
Nothing to disclose.
Funding
This study presents the results of an International Atomic Energy Agency (IAEA) multicenter trial: ‘‘Value of intraventricular synchronism assessment by gated-SPECT myocardial perfusion imaging in the management of heart failure patients submitted to cardiac resynchronization therapy’’ (IAEA VISION-CRT), Coordinated Research Protocol E1.30.34, and received funds from IAEA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alexanderson-Rosas, E., Espinola-Zavaleta, N., Garcia, E.V. et al. Diastolic dyssynchrony assessment by gated myocardial perfusion-SPECT in subjects who underwent cardiac resynchronization therapy. J. Nucl. Cardiol. 28, 1413–1421 (2021). https://doi.org/10.1007/s12350-019-01845-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01845-2