Abstract
Background
Mechanical left ventricular dyssynchrony (MLVD) might contribute in the therapeutic decision-making in patients with heart failure (HF) prior to cardiac resynchronization therapy (CRT). Our aim was to assess MLVD in patients with HF prior to implantable cardioverter-defibrillator (ICD) compared to patients with CRT-D.
Methods
In a prospective study, patients with LVEF ≤ 35% who were scheduled for ICD or CRT-D, underwent gated SPECT myocardial perfusion imaging with technetium 99m sestamibi within 3 months prior procedure. MLVD was measured by phase analysis.
Results
The study cohort consisted of 143 patients, 71 with ICD and 72 with CRT-D. Age 68.3 ± 11 and LVEF 24 ± 6%. Phase standard deviation (SD) was 62.5 ± 18 and 59.7 ± 20 (P = NS), respectively. During follow-up of 23.7 ± 12.1 months, there were 10 vs 14 cardiac death in ICD and CRT-D, respectively (P = NS), hospitalization for HF, in 34 vs 53 (P < .001). In multivariate analysis, Phase SD was the independent predictor for cardiac death [HR 2.66 (95% CI 1.046-6.768), P = .04]. Kaplan-Meier curves of phase SD of 60° significantly identified ICD patients with and without cardiac deaths and hospitalization for HF exacerbation.
Conclusions
MLVD by phase SD can identify patients with cardiac events and predict cardiac death in patients treated with ICD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The main reasons for cardiac mortality are HF or fatal arrhythmia. Among solutions to reduce cardiac mortality and improve symptoms of heart failure, there are two electromechanical solutions that improve the quality of life and reduce cardiac mortality. One is cardiac resynchronization therapy (CRT) which is suitable for patients with heart failure, depressed left ventricular ejection fraction (LVEF) (≤35%), and a wide QRS complex on the surface electrocardiogram (≥120 milliseconds),1-5 and the other is an implantable cardiac defibrillator (ICD) for patients with LV dysfunction with reduced ejection fraction and/or life-threatening arrhythmias.6,7
Recent data have indicated that mechanical left ventricular dyssynchrony (MLVD) may be mandatory for the prediction of CRT responses as well as for prediction of poor outcome in patients with HF.8-10 MLVD can be assessed by phase analysis that has been developed from gated single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI).11 The advantage of this phase analysis technology is its automaticity and reproducibility. Several studies demonstrated that gated SPECT by phase analysis detected MLVD and predicted cardiac events in patients with HF with LV dysfunction and in response to CRT.12-17
Regarding ICD for primary prevention, it is estimated that two-third of patients with ICD do not benefit from it.6 Recently, Aljaroudi et al reported on the relation of LV dyssynchrony by phase analysis of gated SPECT images and cardiovascular events in patients with ICD.18 The hypothesis of our study is that patients with reduced LVEF who were scheduled for ICD for primary prevention, have more life-threatening arrhythmias, worsening of HF, and cardiac death. We speculate that the assessment of MLVD can be used to predict cardiac outcome in patients with ICD and might be useful in therapeutic decision-making.
The aim of the present study was to assess MLVD in patients with LV dysfunction who were scheduled to undergo either ICD or CRT-D and to examine its relationship with cardiac outcome.
Methods
Study Design
We prospectively studied 143 patients who were referred to our university-affiliated medical center with LVEF of ≤35% and were scheduled to undergo ICD for primary prevention or CRT-D within a 3-month period. The patient selection for each procedure (ICD, CRT, or CRT-D) was done by electrophysiologic and HF teams, according to ACC guidelines. For the purpose of this study, patients installed with ICD or CRT-D were included. Patients were referred from the electrophysiology laboratory to the nuclear cardiology laboratory of the same medical center. Gated SPECT MPI with technetium (Tc) 99m sestamibi (rest or stress/rest protocol) was performed as part of LV assessment prior to procedure. Comprehensive LV assessment was done and included myocardial perfusion, function, and phase analysis.
Exclusion criteria were patients with chronic atrial fibrillation, congenital heart disease, and vascular intervention between MPI and ICD/CRT-D procedure.
MPI Study
The study was done under fasting conditions and on medications including ACE/ERB, diuretics, beta blockers, and statins. Patients who were scheduled for rest imaging only, beta blockers were continued.
The study was done at rest with high-dose Tc 99m sestamibi in patients with HF who were not suitable for stress testing. It was done for assessing viability, LV function, and phase analysis. The remaining patients underwent stress-rest sequence, starting with the injection of low dose of Tc 99m (8-12 mCi) sestamibi and followed by high-dose Tc 99m (24-36 mCi) after an interval of 3-4 hours. Two patients underwent 2-day protocol. Details on acquisition of gated SPECT and image processing including phase analysis as performed in our laboratory were reported previously by Zafrir et al.17
Imaging Procedure
A complete gated SPECT of 8 frames (60 views; 30 views per head) was acquired for rest and post-stress using a dedicated cardiac Ventri system (GE Healthcare) equipped with low-energy/high-resolution collimators.
Each SPECT image was interpreted at different times by one of 3 dedicated nuclear cardiologists, independently, using a 17-segment model and 5° (0-4) severity score. The sum stress score (SSS) and the sum rest score (SRS) were calculated. SSS value of zero was considered normal; values between 1 and 3 were defined as equivocal; and values of 4 or more, as abnormal. The clinical scan results were categorized as normal, equivocal, or ischemia (with or without MI) and MI (scar). Scar or ischemia size was scored from 0 to 4 (0 = no scar/ischemia, 4 = large scar/ischemia, according to SSS and SRS).
Assessment of Left Ventricular Dyssynchrony
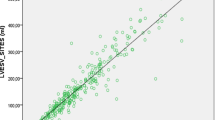
Phase analysis was performed with Emory Cardiac Toolbox software (Emory University/Syntermed, Atlanta, Georgia, and USA).11 MLVD was assessed by phase standard deviation (SD) and phase histogram bandwidth (HB). Our group validated and studied these phase analysis parameters in a previous study.17
Data Analysis
Parameters for analysis included the following: demographic characteristics; clinical characteristics, including CAD risk factors, myocardial infarction, coronary intervention, and New York Heart Association (NYHA) functional class; electrocardiography criteria (Q waves, bundle branch block, QRS width); and MPI data (infarct size, ischemia size, LVEF, end-diastolic volume (EDV), end-systolic volume (ESV), and phase SD phase HB).
Follow-up
Data were extracted from the patient medical files and electronic data from hospitalization and from visits in the electrophysiology and HF clinics. The cardiac events were classified as primary MACE; major cardiac endpoints including cardiac death, HF exacerbation requiring hospitalization, and appropriate VT/VF. Secondary MACE was attributed for each of these endpoints.
Statistical Analysis
Statistical analysis was performed using SPSS software; version 16.0. Continuous variables were expressed as mean ± SD. The unpaired Student t test was performed for comparative analysis of normally distributed variables, and the Mann-Whitney U test was used for nonparametric analysis. Categorical variables were expressed as percentage and comparisons between groups were made using the χ 2 test and the Fisher’s exact test, when the absolute number of events is less than 5. Univariate and multivariate Cox-proportional hazard regression models were used to identify independent predictors for primary and secondary MACE. Unadjusted Kaplan-Meier survival curves were plotted and compared. Cox-proportional hazard survival plots were done with adjusted HR (95% CI). Statistical significance was set at a level of <0.05.
Results
Of the 143 patients, 72 underwent CRT-D installment and 71 underwent ICD installment. The demographic and clinical data of the whole patients and of each group are demonstrated in Table 1. Gated SPECT MPI measures prior to procedure are shown in Table 2. Rest imaging only was done in 86 (60%) patients and the remaining 57 (40%) underwent stress-rest imaging. Of them, 45 (79%) was done by dipyridamole test and 12 (21%) by treadmill exercise test. The two groups were similar in age, female prevalence, diabetes mellitus, and hypertension. Mean QRS width, prevalence of left bundle branch block (LBBB), and NYHA functional class were significantly higher in patients with CRT-D than those with ICD only. Four patients from the ICD group had LBBB and did not receive CRT-D because they had no symptoms of HF and were in NYHA functional class 1. Mean LVEF of all patient study was 24% ± 7%, and was lower in patients with CRT-D than those with ICD. Infarct size was larger in the patients with ICD. Of note, MLVD measured by phase SD and phase HB was markedly prolonged, and their mean values were similar prior to procedure (phase SD values were 62.5 ± 18 in ICD vs 59.7 ± 20 in CRT-D, P = .4; phase HB 189 ± 79 in ICD vs 182 ± 65 in CRT-D P = .5) (Table 2).
Cardiac Events
The patients were followed for up to 3 years for primary and secondary MACE. No case was dropped out from follow-up. Of the all 143 study patients, there were 24 cardiac deaths, 83 HF exacerbation requiring hospitalization, and 28 events of appropriate ICD shock for VT/VF. In comparison between the 2 groups, there were more primary MACE in CRT-D vs ICD patients, 59 vs 43 patients, respectively (P = .002) . Secondary MACE were 10 cardiac deaths in the ICD patients compared with 14 in the CRT-D patients (P = .37). Less cases of exacerbation of HF requiring hospitalization, 34 vs 53, respectively (P = .001), and similar rate of appropriate ICD shock for VT/VF, 16 vs 12, respectively (P = .51).
Prediction analysis of primary MACE in all patients was as follows:
In univariate analysis including EDV, LVEF, LBBB, QRS width, QRS of 120 and above, infarct size and phase SD. It was shown that EDV, LVEF, QRS width, and phase SD were significantly higher in patients with primary MACE, while in multivariate analysis, only LVEF [HR 0.96 (95% CI 0.92-0.99) P = .047] and QRS width [HR 1.008 (95% CI 1.001-1.014) P = .023] were independent predictors for primary MACE (Table 3a). However, for cardiac death in all patient study, phase SD 60 [HR 2.66 (95% CI 1.046-6.768) P = .04] and QRS width [HR 1.014 (95% CI 1.003-1.025) P = .016] were the independent predictors (Table 3b).
MLVD was expressed by phase SD with cut off 60, according to previous analysis. Primary and secondary endpoints in relation to phase SD 60 in all patients study and those with ICD alone and CRT-D are summarized in Table 4. Phase SD 60 was more frequent in patients with all endpoints as well in cardiac death and HF endpoints. Moreover, it was also shown that patients with ICD with phase SD ≥ 60 as well have more cardiac death and hospitalization for exacerbation of HF as endpoints compared to patients with lower phase SD, but this cut off phase SD 60 was nonsignificant in CRT-D patients with and without cardiac events (Table 4).
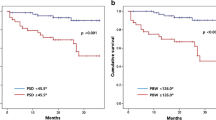
Kaplan-Meier survival curves of all patients study in relation to phase SD of 60 (Figure 1A) showed significant differentiation in primary MACE, and also in cardiac death (Figure 1B) and HF deterioration (Figure 1C), however, no effect in the occurrence of VT/VF.
Kaplan-Meier survival curves of ICD patients in relation to phase SD of 60 showed significant differentiation with cardiac death (Figure 2A) as well as with HF hospitalization (Figure 2B). Of note, using phase SD with a cutoff of 40° did not demonstrate correlation with cardiac events.
In order to examine the prognostic value of Phase SD in ICD prior procedure, univariate and multivariate analyses were performed (Table 5). As shown, the independent predictors for cardiac death were as follows: QRS width [HR 1.014 (95% CI 1.003-1.025) P = .016] and phase SD [HR 2.66 (95% CI 1.046-6.768) P = .04]. However, taking into account that the QRS width parameter was prerequisite criteria for selection to either procedure, we remain with phase SD of 60 cut off as the only independent predictor for cardiac death. Figure 3 is an example of phase analysis and ECG tracing of a patient post μI who underwent ICD installment. It shows marked MLDV while QRS width was slightly widened.
Discussion
The results of this study show that patients treated with ICD or CRT-D for HF and reduced LVEF were discriminated by NYHA class, QRS width, and LVEF at baseline. Nevertheless, the measurements of MLVD by phase analysis were similar but prolonged in both ICD and CRT-D patients at baseline.
During the 3-year follow-up, there was more MACE in CRT-D patients than in ICD patients. This was on account of HF exacerbation in the CRT-D during follow-up. However, the accumulative event rate of cardiac death and VT/VF with appropriate shock was similar in both groups. This can be explained by the fact that CRT-D patients have been already in poor health and with advanced NYHA class prior to procedure and only some of them were improved by resynchronization therapy, while the others remained stable or deteriorated.
In the present study, we found that MLVD as measured by phase SD was useful in the assessment of ICD patients. Using phase SD, we were able to identify patients who were prone to cardiac death and HF exacerbation. Moreover, phase SD with a cutoff of 60° could predict cardiac death in ICD patients. This might suggest that patients with MLVD who are treated with ICD only could have a better outcome if they were receiving CRT in addition to ICD.
Of note, the mean phase SD and phase HB were prolonged in the CRT-D group, similar to the ICD patients, but the survival curves of these patients using phase SD with a cutoff of 60° could not discriminate CRT patients. The possible reason is that MLVD was improved by the CRT activation in some patients.
The association of acute change in LV synchrony after CRT and patient outcome using a single injection of gated SPECT was shown in a pilot study.19 Several studies have shown improvement in HF and reduced cardiac death in patients who demonstrated dyssynchrony.9,11,12
Aljaroudi et al showed the severity of LV Dyssynchrony by phase analysis in patients with LV dysfunction and ICD which were associated with an increased risk of death, and that appropriate ICD shock and a phase SD of <50° were associated with no events at 1 year.18 In the present study, cardiac events were associated with phase SD of ≥60°. However, all patients in our study had severe LV dysfunction with lower values of LVEF compared to the previous study, as such the MLVD might be worse with widening of phase SD in some of the patients.
In our previous study of nonselected patients (with and without LV dysfunction) who underwent gated SPECT MPI with phase analysis, phase SD of 40° was a cutoff to predict cardiac death.17 However, in the present study, in which all patients had marked LV dysfunction and abnormal dyssynchrony, the cutoff for differentiating outcome was higher (60°) as shown in this study.
Limitations
Our study was limited by its small sample size. Another limitation was that there was no control group with LV dysfunction without device. However, the aim of the study was to show the characteristics of ICD patients with LV dysfunction compared to CRT-D patients in correlation to dyssynchrony.
New Knowledge Gained
Previous studies addressed to the value of measuring MLVD in patients prior CRT. In this study, we showed the value of measuring MLVD in patients with LV dysfunction, who are candidate for ICD. As already known, the majority of patients do not benefit from the ICD as there are no proper criteria to select these patients. It is possible that patients with MLVD with phase SD of 60 and above may have a better outcome if they receive CRT-D instead of ICD only.
Conclusions
Patients with systolic LV dysfunction with ICD or CRT-D have similar and prolonged MLVD prior to procedure and similar incidence of cardiac death and VT/VF after 3 years. MLVD can predict cardiac death in patients with ICD who might benefit from CRT as well.
Abbreviations
- CRT-D:
-
Cardiac resynchronization therapy with a defibrillator
- ICD:
-
Implantable cardiac defibrillator
- LVEF:
-
Left ventricular ejection fraction
- MLVD:
-
Mechanical left ventricular dyssynchrony
- MPI:
-
Myocardial perfusion imaging
- NYHA:
-
New York Heart Association
- SPECT:
-
Single-photon emission computed tomography
- Tc:
-
Technetium
- VT/VF:
-
Ventricular tachycardia/ventricular fibrillation
- HF:
-
Heart failure
- SD:
-
Standard deviation
References
Leclercq C, Kass DA. Retiming the failing heart: Principles and current clinical status of cardiac resynchronization. J Am Coll Cardiol 2002;39:194-201.
Abraham WT, Hayes DL. Cardiac resynchronization therapy for heart failure. Circulation 2003;108:2596-603.
Leclercq C, Hare JM. Ventricular resynchronization: current state of the art. Circulation 2004;109:296-9.
Abraham WT, Fiber WG, Smith AL, Delurgio DB, Leon AR, Loh E, et al. Cardiac resynchronization in chronic heart failure. N Eng J Med 2002;346:1845-53.
Chung ES, Leon AR, Tavazzi L, Sun JP, Merlino J, Abraham WT, et al. Results of the predictor of response to cardiac resynchronization therapy (PROSPECT) trial. J Cardiol Failure 2007;13:793.
Fisher JD, Buxton AE, Lee KL, Packer DL, Echt DS, Denes P, et al. MUSTT Events Committee. Designation and distribution of events in the Multicenter Unsustained Tachycardia Trial (MUSTT). Am J Cardiol 2007;100:76-83.
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877-83.
Bax JJ, Bleeker GB, Marwick TH, Molhoek SG, Boersma E, Steendijk P, et al. Left ventricular dyssynchrony predicts response and prognosis after cardiac resynchronization therapy. J Am Coll Cardiol 2004;44:1834-40.
Bax JJ, Marwick TH, Molhoek SG, Bleeker GB, van Erven L, Boersma E, et al. Left ventricular dyssynchrony predicts benefit of cardiac resynchronization therapy in patients with end-stage heart failure before pacemaker implantation. Am J Cardiol 2003;92:1238-40.
Penicka M, Bartunek J, Lang O, Medilek K, Tousek P, Vanderheyden M, et al. Severe left ventricular dyssynchrony is associated with poor prognosis in patients with moderate systolic heart failure undergoing coronary artery bypass. J Am Coll Cardiol 2007;50:1315-23.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:687-95.
Henneman MM, Chen J, Dibbets-Schneider P, Dibbets-Schneider P, Stokkel MP, Bleeker GB, et al. Can LV dyssychrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med 2007;48:1104-11.
Boogers MM, Van Kriekinge SD, Hennemam MM, Ypenburg C, Van Bommel RJ, Boersma E, et al. Quantitative gates SPECT derived phase analysis on gated myocardial perfusion SPECT detects left ventricular dyssynchrony and predicts response to cardiac resynchronization therapy. J Nucl Med 2009;50:718-25.
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R, et al. Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2011;18:24-30.
Pazhenkottil AP, Buechel RR, Husmann L, Nkoulou RN, Wolfrum M, Ghadri JR, et al. Long-term prognostic value of left ventricular dyssyncriny assessment by phase analysis from myocardial perfusion imaging. Heart 2011;97:33-7.
Uebleis C, Hellweger S, Laubender RP, Becker A, Shon HY, Lehner S, et al. Left ventricular dyssynchrony assessed by gated SPECT phase analysis in an independent predictor of death in patients with advanced coronary artery disease and reduced left ventricular function not undergoing cardiac resynchronization therapy. Eur J Nucl Med Mol Imaging 2012;39:1561-9.
Zafrir N, Nevzorov R, Bental T, Strasberg B, Gutstein A, Mats I, et al. Prognostic value of left ventricular dyssynchrony by myocardial perfusion gated SPECT in patients with normal and abnormal left ventricular function. J Nucl Cardiol 2014;21:532-40.
Aljaroudi WA, Hage FG, Hermann D, Doppalapudi H, Venkatarama R, Heo J, et al. Relation of left ventricular dyssynchrony by phase analysis of gated SPECT images and cardiovascular events in patients with implantable cardiac defibrillators. J Nucl Cardiol 2010;17:298-304.
Friehling M, Chen J, Saba S, Bazaz R, Scharrzman D, Adelstein EC, et al. A prospective pilot study to evaluate the relationship between acute change in left ventricular synchrony after cardiac resynchronization therapy and predict outcome using a single injection gated SPECT protocol. Circ Cardiovasc Imaging 2011;4:532-9.
Conflict of interest
The authors report no potential conflict of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-015-0326-x.
Rights and permissions
About this article
Cite this article
Zafrir, N., Bental, T., Strasberg, B. et al. Yield of left ventricular dyssynchrony by gated SPECT MPI in patients with heart failure prior to implantable cardioverter-defibrillator or cardiac resynchronization therapy with a defibrillator: Characteristics and prediction of cardiac outcome. J. Nucl. Cardiol. 24, 122–129 (2017). https://doi.org/10.1007/s12350-015-0310-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0310-5