Abstract
The aim of this study was to assess the prognostic value of normal ultra-low-dose exercise MPI with a CZT camera.
Methods
1901 consecutive patients without known CAD referred for exercise MPI with 1.8 MBq/kg (0.05 mCi) of Tc99m sestamibi or tetrofosmin and a CZT camera were included prospectively. Patients with an abnormal scan requiring an additional resting image (230) or a submaximal exercise test (271) were excluded. The 1400 remaining patients were followed for 39 months. The primary end-point was cardiac events (cardiac death, nonfatal myocardial infarction, and revascularization). The secondary end-point was noncardiac death.
Results
The mean injected activity was 145 ± 37 MBq (3.9 ± 1 mCi), the mean acquisition duration was 10 ± 0.7 minutes, and the mean effective dose was 0.91 ± 0.13 mSv. 1288 patients (92%) achieved full follow-up. We observed 22 cardiac events and 16 noncardiac deaths. The annualized rates were equivalent to 0.55% for cardiac events and 0.37% for noncardiac mortality.
Conclusions
Normal ultra-low-dose exercise MPI with a CZT camera has a high negative predictive value. The effective dose was less than 1 mSv, and the study thus allays concerns about radiation burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radionuclide myocardial perfusion imaging (MPI) is a key tool for the diagnosis and assessment of coronary artery disease (CAD).1,2 However, there are concerns about its relatively high radiation exposure.3,4 In response, professional societies have recommended decreasing the radiation dose for MPI.5,6 Cadmium-Zinc-Telluride (CZT) cameras were introduced in 2008, allowing for high speed imaging.7–9 The high sensitivity of CZT cameras can alternatively be used to decrease the injected radionuclide activity.10 These new protocols have been validated by comparing with conventional SPECT or with invasive coronary angiography in the case of pathological results.11,12 However, in patients with a low or intermediate pretest likelihood of CAD, no data about the validity of normal ultra-low-dose MPI are yet available. Additionally, the use of stress-only imaging for normal scans in patients without previous known coronary disease is now recommended, which also contributes to decreasing radiation exposure.13,14 With conventional SPECT, the prognostic value of a normal myocardial perfusion radionuclide scan is well-established.15–18 Verification of the prognostic value of normal ultra-low-dose stress-only MPI is a necessary and an additional tool to assess the validity of the ultra-low-dose protocol with a CZT camera. The aim of this study was therefore to follow patients without known coronary artery disease, included prospectively in 2011, after normal exercise ultra-low-dose MPI. The main goal was to validate the high negative predictive value of a normal exercise-only scan. A secondary goal was to identify potential subgroups with a higher risk of cardiac events.
Methods
Study Population
Between January 2011 and December 2011, 4841 consecutive patients were referred to our institution for an exercise myocardial perfusion scan. 1901 of them had no known coronary artery disease and were considered for this study. We excluded from the main analysis the 230 patients who had an abnormal stress myocardial perfusion scan and the 271 patients who did not achieve 85% of the maximal predicted heart rate (MPHR: 220 minus age). The main analysis thus focused on the 1400 remaining patients with normal exercise myocardial perfusion scans (Figure 1). The 501 excluded patients (230 with abnormal scans and 271 with submaximal tests) were also followed up and analyzed separately. The study was approved by the local board, and informed consent was obtained from all patients.
Exercise Test
Patients performed a maximal exercise test, i.e., heart rate ≥85% of MPHR, using standard protocols on a treadmill (Bruce, Bruce modified or Kattus protocols) or an ergometer bicycle (initial power output of 30 Watts, followed by increases of 30 Watts every 2 minutes).19 Patients were asked to discontinue cardiac drugs (i.e., beta blockers, calcium antagonists) at least 48 hours before the test. The exercise test was considered normal when the ST-segment remained isoelectric, positive when horizontal or downsloping ST-segment depression >1 mm, measured 0.08 seconds after the J point occurred, with or without chest pain, and nondiagnostic in the case of other ECG abnormality (for example upsloping ST-depression or ST-depression ≤1 mm).
Radionuclide Scan
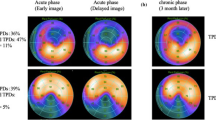
Tc99m Sestamibi (Mallinckrodt) or Tc99m Tetrofosmin (General Electric Healthcare) was injected at the peak of the exercise, and exercise continued for 1 to 2 minutes after the injection. The injected activity depended on the weight of the patient (0.05 mCi/kg, i.e., 1.85 MBq/kg). We used a Discovery NM530c (General Electric Healthcare) CZT camera, designed with 19 fixed detectors and multipinhole collimators.9 Scans were performed 10 minutes after injection, and the imaging time depended on the count rate, obtaining more than 1 million counts in the image and 1.2 million counts in the case of extra-cardiac activity on the acquisition monitoring screen (usually between 8 and 12 minutes). Scans were performed in the prone position first and then in the supine position in the case of an equivocal result. In cases of poor scan quality because of extra-cardiac activity (in the gastrointestinal tract), the scan was repeated 1 hour after injection. Iterative 3D reconstruction used 60 iterations, with a Butterworth filter (order 7, cut-off 0.37 cm−1). Left ventricular volumes and ejection fraction were calculated using Myometrix software (General Electric Healthcare). Scans were read immediately by two experienced physicians, and a third opinion was obtained when there was disagreement. A scan was considered normal when homogenous uptake of the radiotracer was observed in all myocardial segments (less than 30% count variation compared to the highest count rate with a 17 segments model) with normal left ventricular volumes (end-diastole volume less than 130 mL in males and 100 mL in females, as previously validated in our department) and ejection fraction (ejection fraction greater than 55%), as shown in Figure 2. In the case of a normal stress scan, we used a stress-only protocol and included the patient in the main analysis. When an additional resting image was needed, the scan was considered abnormal; three times the activity was injected at rest three hours later, and half-time acquisition was performed one hour after injection. The patient was subsequently excluded from the main analysis.
Follow-Up
Follow-up was performed by telephone calls to patients from March to July 2015. Patients were asked about cardiac events since MPI in 2011. Additionally, we asked about visits (hospitalization or consultation) to cardiologists or family doctors. Moreover, for patients who had medical follow-up in our hospital, detailed medical data were available. The follow-up duration was calculated as the time between the MPI date and the latest information date about the patient. In case of an event, follow-up was censored at the time of this event. We closed the follow-up time at 39 months, which was the time between the last scans (December 2011) and the first phone calls.
End-Points
The primary study end-point was the occurrence, during the follow-up period, of a cardiac event: cardiac death (defined as both documented cardiac death and unexplained sudden death), nonlethal myocardial infarction, or myocardial revascularization. The secondary end-point was the occurrence of a noncardiac death.
Statistical Analysis
The results were expressed as mean ± standard deviation with additional information about the range.
Survival analysis was performed by the Kaplan-Meier method and subgroups were compared by the log-rank method (Mantel-Cox). A multivariate Cox model regression analysis was used to detect potential additional prognostic factors after testing for statistical assumptions (linearity, normality, proportional hazards) and the absence of significant correlation between variables. Results were considered as statistically significant when p was less than .05. The statistical analysis was performed with the software SPSS Statistics v21 (IBM Corporation).
Results
Patient Characteristics
Table 1 summarizes the characteristics of the 1400 patients who were included and their indications for MPI. The mean age was 59 ± 11 years; 56% were male. The mean weight was 79 ± 16 kg. 58% of patients had dyslipidemia, 52% hypertension, and 34% diabetes. They were referred for chest pain in 44%, dyspnea in 12%, and ECG abnormalities in 18% of the cases. The remaining 25% were referred for a diagnosis of silent ischemia because of multiple vascular risk factors and/or peripheral artery disease.
Exercise Tests and Radionuclide Scans
The exercise test was performed on an ergometric bicycle (61%) or a treadmill (39%). The test was normal in 1212 patients (87%), abnormal in 71 patients (5%), and nondiagnostic in 117 patients (8%). Radionuclide scans used Sestamibi or Tetrofosmin. The mean injected activity was 145 ± 37 MBq (3.9 ± 1 mCi), and the mean acquisition duration was 10 ± 0.7 minutes (range 4 to 15 minutes). Table 2 shows the detailed results of the exercise tests and radionuclide scans.
Effective Dose Calculation (mSv)
Using the ICRP 60 correction factors, the mean effective dose was found to be 0.98 ± 0.13 mSv (range 0.66 to 1.99 mSv) with Sestamibi and 0.90 ± 0.07 mSv (range 0.68 to 1.43 mSv) with Tetrofosmin.20 With ICRP 103, the mean effective dose was 0.93 ± 0.12 mSv (range 0.63 to 1.89 mSv) with Sestamibi and 0.81 ± 0.06 mSv (range 0.62 to 1.30 mSv) with Tetrofosmin.21 These results are summarized in Table 3.
Follow-Up
1288 patients (92%) completed the follow-up, the duration of which was 1169 ± 108 days (range 550 to 1189 days). 112 patients (8%) were lost to follow-up. There were no events in 1250 patients (97%). We observed 22 cardiac events (five cardiac deaths, seven nonlethal myocardial infarctions, and ten nonurgent revascularizations — eight PTCA and two CABG) and 16 noncardiac deaths. The events are presented in Table 4. The annualized rate of cardiac events was 0.55% (0.13% for cardiac death, 0.17% for nonlethal myocardial infarction, and 0.25% for myocardial revascularization). The annualized rate for noncardiac mortality was 0.37%. The Kaplan-Meyer survival curves are shown in Figure 3.
Kaplan-Meier event-free survival curves during follow-up (months): a Overall survival, b cardiac death-free survival, c major cardiac event-free survival (i.e., without nonlethal myocardial infarction or cardiac death), d cardiac event-free survival (i.e., without major cardiac event or myocardial revascularization)
Subgroup Analysis
The only additional predictive factor for cardiac events was the number of vascular risk factors with the Cox model (P = .01) and Kaplan-Meyer analysis (P < .01). Even for the 302 patients with four or more risk factors, the annualized cardiac event rate remained low (0.9%). 478 patients were diabetic, with a cardiac event rate (0.8%) higher than in nondiabetic patients (0.4%), but the difference was not statistically significant (P = .09) in male or female patients. The exercise test was positive in 71 patients and nondiagnostic in 117 patients, with no significant difference in terms of cardiac events with the rest of the population (P = .21) or between the 71 positive and the 117 nondiagnostic patients (P = .51). However, the all-cause mortality rate varied depending on the level of exercise (P < .01). These results are presented in Figure 4.
Kaplan-Meier survival curves during follow-up (months) in subgroups: a According to the number of vascular risk factors, there is a statistically significant difference in terms of cardiac event-free survival between these subgroups (P < 0,01). b According to diabetes mellitus status, there is no statistically significant difference between the two groups (P = .09). c According to exercise level, there is a statistically significant difference in terms of overall survival between the subgroups (P < .01)
Abnormal Scans
Patients who needed an additional resting image were excluded from the main analysis. Of these 230 patients, 158 had attenuation artifacts with nonreversible abnormalities, without thickening abnormalities. Their weight was 85 ± 17 kg, which was heavier than the included patients (P < .001). Their effective dose with a one-day stress-rest protocol was 4.44 ± 0.91 mSv. Follow-up data are available in 145 of these patients (92%). We observed one cardiac death, four revascularization, and two noncardiac deaths i.e., an annualized rate of 1.4% for cardiac events (P = .047 compared with normal stress-only) and 0.56% for noncardiac mortality. The 72 remaining patients had definitively abnormal MPI. Coronary angiography data were available in 48 of them (67%). Coronary angiography was normal in eight patients and showed single-vessel disease in seven patients and multi-vessel disease in 33 patients. Follow-up data were available for 67 of the 72 abnormal patients (93%). We observed 15 early revascularizations (in the 90 days following MPI), one nonlethal myocardial infarction, six late revascularizations (>90 days after MPI), and one noncardiac death, i.e., an annualized rate of 2.9% for cardiac events (early revascularizations not included; P < .001 compared with normal stress-only patients; Figure 5).
Kaplan-Meier cardiac event-free survival curves during follow-up (months) in included normal stress-only patients (blue curve) and in excluded stress-rest patients (abnormal—red curve—or artifact—green curve-). For abnormal patients, early revascularizations are not included in cardiac events. There is a statistically significant difference between normal stress-only patients and abnormal stress-rest patients (P < .001), and also between normal stress-only patients and stress-rest patients with artifact (P = .047)
Submaximal Exercise Tests
271 patients were excluded from the main analysis because they failed to achieve 85% of MPHR (76 ± 6% of MPHR). 156 patients performed submaximal exercise because they did not discontinue cardiac drugs before the test. 97 patients stopped because of their inability to continue exercise due to poor condition. 18 patients stopped because of an abnormal exercise test. Follow-up data are available for 253 of these excluded patients (93%). We observed eight noncardiac deaths (annualized rate 1%) and seven cardiac events (two cardiac deaths, two nonlethal myocardial infarctions, and three revascularizations; annualized rate 0.9%). Compared with the included patients (maximal exercise), there was a significant statistical difference in terms of overall survival (P = .02), but not in terms of cardiac events (P = .26). No events were observed in the patients who had an abnormal submaximal exercise test.
Patients Lost to Follow-Up
We compared the 112 lost to follow-up patients with the patients remaining in the study. There were no significant differences in terms of sex, weight, risk factors (tobacco use, diabetes, dyslipidemia, hypertension, family history), and exercise test results. The only significant difference was in age with lost to follow-up patients being younger than the other patients (57.8 ± 9.7 vs 59.4 ± 10.7; P = .02).
Discussion
Ultra-low-dose protocols have been validated in the case of pathological results by comparison with conventional SPECT or with coronary angiography.11 , 12 However, the clinical value of a normal ultra-low-dose scan has not yet been validated. With conventional SPECT, the prognostic value of a normal myocardial perfusion radionuclide scan is well-established, with an annual rate of cardiac events of less than 1% per year.15 – 18 We verified here the excellent prognostic value of a normal ultra-low-dose myocardial exercise scan, with an annualized rate of cardiac events of 0.55%. This result contributes to the assessment of the validity of ultra-low-dose protocols using a CZT camera.
Patient characteristics are central in follow-up studies. In fact, the risk of a major event after a normal scan is a function of the pretest probability, based on clinical and historical factors of the tested patient.22 The characteristics of the patients included in our study are similar to those of most studies on initial testing for the diagnosis of CAD (age: 59 years; diabetes: 34%; hypertension: 52%; dyslipidemia: 58%).23 Moreover, 75% of the patients were referred for diagnosis of chest pain, dyspnea, or ECG abnormalities. The remaining 25% of the patients had several vascular risk factors or peripheral artery disease.
We only included patients who referred for exercise MPI. Current guidelines recommend exercise stress testing rather than pharmacological testing whenever possible.2 We use dipyridamole stress testing in patients unable to exercise adequately, who represent approximately 20% of patients referred to our institution. We did not include them in this study because in 2011, we still used thallium-201 for dipyridamole MPI. We know that the event rate is higher in patients referred for pharmacological stress imaging;24 thus, our results cannot be extrapolated to patients undergoing normal dipyridamole scans.
Our study concerned normal stress-only MPI. We thus excluded patients who needed an additional resting image. Among those patients, 158 were considered as having an artifact, and 72 were considered as definitely abnormal. As expected, follow-up data showed that the event rate was higher in the abnormal patients. We also observed that the event rate was higher in patients with artifacts than in normal stress-only patients, which is somewhat counter-intuitive and could suggest an over-estimation of artifacts and an under-estimation of abnormal results. In any case, in our population, 1671 on 1901 patients (88%) had a normal scan, which is a high percentage, but comparable to the high proportion of normal scans documented in recently published studies from the USA.25
Patients who did not achieve 85% of the maximal predicted heart rate were excluded from the main analysis. This would be a possible source of bias if those patients happened to be more severe. However, follow-up data showed that there was no significant difference in terms of cardiac events between this group and the study population, even when the submaximal exercise test was abnormal.
We tried to identify potential subgroups with a higher risk of cardiac events. The annualized cardiac event rate increased with the number of risk factors, but remained less than 1%, even with four or more risk factors. We observed a few more cardiac events in diabetic patients, but the difference was not significant. It is now well-established that cardiac risk is not related to diabetes, but rather to high-risk diabetes.26 Our diabetic population mixed low-risk and high-risk diabetes patients, which could explain this nonsignificant result. Among all patients, an abnormal exercise test with a normal myocardial scan was not predictive of increased cardiac events, but this could be a consequence of the small number of cardiac events and limited statistical power. Patients are often referred to MPI after a nondiagnostic exercise test because of resting ECG abnormalities, upsloping ST-segment depression, or rapid recovery of ST-segment changes. Our results confirm that a normal myocardial scan indicates a very low risk of cardiac events, despite the presence of risk factors and ECG abnormalities. On the other hand, as widely reported previously, this study confirms that the level of exercise is a good predictor of all-cause mortality, probably because it reflects the general condition of the patient.27
Radionuclide myocardial perfusion imaging has recently been enhanced by the development of cardiac CZT cameras. The count sensitivity is multiplied by a factor of six or more, allowing for an important shortening of acquisition time.10 At the same time, concerns have been raised in the cardiology community about increased radiation exposure due to medical tests. This is especially true for patients without known coronary disease referred for a screening test. In our clinical practice, these patients represent almost one-third of the patients referred for myocardial perfusion imaging. The high count efficiency of the CZT camera, combined with the use of a stress-only protocol, provides an opportunity to decrease the effective dose to these patients. We previously showed that using 2 MBq/kg of Tc99m sestamibi, 10 minutes of acquisition time with a CZT camera and an effective dose of less than 1 mSv, we could obtain higher myocardial counts and better image quality than with conventional SPECT (EANM annual congress, Birmingham, 2011). More recent papers confirm that accurate images can be obtained with an effective dose of less than 1 mSv.28,29 We calculated here the effective dose for 1400 consecutive patients undergoing stress-only imaging. The effective dose was less than 1 mSv in most patients, which is less than one year’s worth of background radiation. Moreover, we did not count the residual activity in syringes following injection and probably overestimated the injected activity and thus the effective dose by 10 to 20%.30
The 230 patients whose exercise scan was abnormal and thus needed an additional resting scan were excluded. Among them, 158 patients had attenuation artifacts. They were significantly heavier than the included patients (85 kg vs 79 kg). Obviously, the radiation dose was higher because of the additional resting study, with an average effective dose of 4 mSv. A standard 10/30 mCi rest-stress protocol provides an effective dose of 10 to 12 mSv. The use of stress-resting protocols allows the use of stress-only MPI when the stress scans are normal, which is the case for most of this low-risk population, leading to an effective dose of less than 3 mSv in most patients. The use of a CZT camera with an ultra-low-dose protocol allows the effective dose to be decreased more dramatically, down to less than 1 millisievert.
Study Limitations
Our study suffers several limitations: It was a single-center study, which targeted patients without known CAD who were referred for an exercise test, with a normal stress-only scan. In our clinical practice, these patients represent almost one-third of all patients referred for MPI. Our conclusions cannot be extrapolated to pharmacological stress imaging or to patients with known coronary artery disease, for whom further studies will be needed. The number of patients lost to follow-up, relatively high (112) by comparison with the low number of cardiac events (38), is a serious limitation. Although complete follow-up in more than 90% of the baseline cohort is one of the eligibility criteria for the quality of follow-up surveys,31 the loss of 8% of patients to follow-up is a serious limitation in a low-risk cohort with a limited number of events like our study. It is therefore possible that some events were not captured. Our population study comprises many migrant patients who sometimes move back to their native country and are thus more prone to be lost to follow-up. On the other hand, the characteristics of the patients lost to follow-up were similar to those of the other patients in the study, except that they were slightly younger, making an increased event rate in this population unlikely. The subgroup assessment has limitations because of the limited number of cardiac events, but it does not affect the main objective of the study. Lastly, our results are valid for the CZT camera that we used (General Electric), but it is likely that similar results could be obtained with other CZT cameras.
New Knowledge Gained
The high negative predictive value of a normal exercise MPI in patients referred for initial diagnosis of CAD is confirmed with a CZT camera and an ultra-low-dose protocol. The combination of ultra-low injected activity, stress-only protocol, and CZT technology leads to an effective dose of less than one millisievert. This dramatically reduced radiation dose is efficient in day-to-day practice in most patients referred for initial diagnosis of CAD.
Conclusions
Normal ultra-low-dose exercise MPI with a CZT camera in patients referred for initial diagnosis of coronary artery disease has a high negative predictive value, with an annualized rate of cardiac events equivalent to 0.55%. This coronary risk is comparable to the risk faced by the general population or by patients who have undergone normal high-dose conventional imaging. This result contributes to assessment of the validity of the ultra-low-dose protocol with a CZT camera. The effective dose was less than 1 millisievert, which is less than one year’s worth of background radiation. This study thus allays concerns about the radiation burden for these patients.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CZT:
-
Cadmium-Zinc-Telluride
- MPHR:
-
Maximal predicted heart rate
- MPI:
-
Myocardial perfusion imaging
- PTCA:
-
Percutaneous transluminal coronary angioplasty
- SPECT:
-
Single-photon emission computed tomography
References
Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008;117:1283-91.
Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, et al. 2013 ESC guidelines on the management of stable coronary artery disease. Eur Heart J 2013;34:2949-3003.
de Gonzalez Berrington. A, Kim KP, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: Projected population cancer risks from current levels of use in the United States. Circulation 2010;122:2403-10.
Einstein AJ, Weiner SD, Bernheim A, Kulon M, Bokhari S, Johnson LL, et al. Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA 2010;304:2137-44.
Cerqueira M, Allmann K, Ficaro E, Hansen CL, Nichols KJ, Thompson RC, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol 2010;17:709-18.
Dorbala S, Blankstein R, Skali H, Park MA, Fantony J, Mauceri C, et al. Approaches to reducing radiation dose from radionuclide myocardial perfusion imaging. J Nucl Med 2015;56:592-9.
Sharir T, Ben-Haim S, Merzon K, Prochorov V, Dickman D, Ben-Haim S, et al. High-speed myocardial perfusion imaging initial clinical comparison with conventional dual detector anger camera imaging. JACC Cardiovasc Imaging 2008;1:156-63.
Gambhir SS, Berman DS, Ziffer J, Nagler M, Sandler M, Patton J, et al. A novel high-sensitivity rapid-acquisition single-photon cardiac imaging camera. J Nucl Med 2009;50:635-43.
Esteves FP, Raggi P, Folks RD, Keidar Z, Askew JW, Rispler S, et al. Novel solid-state-detector dedicated cardiac camera for fast myocardial perfusion imaging: Multicenter comparison with standard dual detector cameras. J Nucl Cardiol 2009;16:927-34.
Imbert L, Poussier S, Franken PR, Songy B, Verger A, Morel O, et al. Compared performance of high-sensitivity cameras dedicated to myocardial perfusion SPECT: A comprehensive analysis of phantom and human images. J Nucl Med 2012;53:1897-903.
Duvall WL, Sweeny JM, Croft LB, Barghash MH, Kulkarni NK, Guma KA, et al. Comparison of high efficiency CZT SPECT MPI to coronary angiography. J Nucl Cardiol 2011;18:595-604.
Fiechter M, Ghadri JR, Kuest SM, Pazhenkottil AP, Wolfrum M, Nkoulou RN, et al. Nuclear myocardial perfusion imaging with a novel cadmium-zinc-telluride detector SPECT/CT device: First validation versus invasive coronary angiography. Eur J Nucl Med Mol Imaging 2011;38:2025-30.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, Croft LB, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Einstein AJ, Johnson LL, DeLuca AJ, Kontak AC, Groves DW, Stant J, et al. Radiation dose and prognosis of ultra-low-dose stress-first myocardial perfusion SPECT in patients with chest pain using a high-efficiency camera. J Nucl Med 2015;56:545-51.
Machecourt J, Longère P, Fagret D, Vanzetto G, Wolf JE, Polidori C, et al. Prognostic value of thallium-201 single-photon emission computed tomographic myocardial perfusion imaging according to extent of myocardial defect. Study in 1926 patients with follow-up at 33 months. J Am Coll Cardiol 1994;23:1096-106.
Iskandrian AS, Chae SC, Heo J, Stanberry CD, Wasserleben V. Independent and incremental prognostic value of exercise single-photon emission computed tomographic (SPECT) thallium imaging in coronary artery disease. J Am Coll Cardiol 1993;22:665-70.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535-43.
Vanzetto G, Ormezzano O, Fagret D, Comet M, Denis B, Machecourt J. Long-term additive prognostic value of thallium-201 myocardial perfusion imaging over clinical and exercise stress test in low to intermediate risk patients study in 1137 patients with 6-year follow-up. Circulation 1999;100:1521-7.
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: A scientific statement from the American Heart Association. Circulation 2013;128:873-934.
Recommendations of the International Commission on Radiological Protection. ICRP Publication 60 Elsevier Health Sciences, 1991.
Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 2007;37(2-4):1-332.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350-8.
Douglas PS, Hoffman U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291-300.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11:171-85.
Duvall WL, Henzlova MJ. Nuclear cardiology as it should look in the twenty-first century. J Nucl Cardiol 2016;23:21-3.
Acampa W, Cantoni V, Green R, Maio F, Daniele S, Nappi C, et al. Prognostic value of normal stress myocardial perfusion imaging in diabetic patients: A meta-analysis. J Nucl Cardiol 2014;21:893-902.
Bourque JM, Beller GA. Value of exercise ECG for risk stratification in suspected or known CAD in the era of advanced imaging technologies. JACC Cardiovasc Imaging 2015;8:1309-21.
Nakazato R, Berman DS, Hayes SW, Fish M, Padgett R, Xu Y, et al. Myocardial perfusion imaging with a solid-state camera: Simulation of a very low dose imaging protocol. J Nucl Med 2013;54:373-9.
Einstein AJ, Blankstein R, Andrews H, Fish M, Padgett R, Hayes SW, et al. Comparison of image quality, myocardial perfusion, and left ventricular function between standard imaging and single-injection ultra-low-dose imaging using a high-efficiency SPECT camera: The MILLISIEVERT study. J Nucl Med 2014;55:1430-7.
Reynolds SN, Kikut J. Adherence of Tc-99 Sestamibi to plastic syringes could complicate efforts in dose reduction in MPI SPECT. J Nucl Cardiol 2016;23:256-64.
Jüni P, Altman DG, Egger M. Assessing the quality of controlled clinical trials. BMJ 2001;323:42-6.
Acknowledgments
We thank Laurence Merlin, clinical research technologist, who performed the follow-up phone survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There is no financial disclosure.
Additional information
See related editorial, doi:10.1007/s12350-016-0639-4.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Songy, B., Guernou, M., Hivoux, D. et al. Prognostic value of one millisievert exercise myocardial perfusion imaging in patients without known coronary artery disease. J. Nucl. Cardiol. 25, 120–130 (2018). https://doi.org/10.1007/s12350-016-0601-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0601-5