Abstract
Background
The interactions between non-obstructive coronary atherosclerosis (<50% stenosis) and myocardial perfusion and functional parameters on myocardial perfusion imaging (MPI) have never been evaluated.
Methods and Results
One-hundred and ninety-five patients were submitted to stress-rest MPI and invasive coronary angiography. The presence of obstructive coronary lesions (>50% stenosis) was excluded. The summed stress score (SSS) was calculated in every patient. Moreover, the left ventricular (LV) ejection fraction (EF) and peak filling rate (PFR) were computed from gated MPI images as measures of systolic and diastolic functions. Sixty/195 patients (31%) showed the presence of non-obstructive atherosclerosis (>20% and <50% diameter reduction). Interestingly, they presented a higher SSS than those with normal coronary arteries (P < 0.001) despite a similar myocardial scar burden. If compared to patients with normal coronary arteries, those with non-obstructive atherosclerosis showed more abnormal post-stress PFR values (2.5 ± 0.9 vs 2.9 ± 0.8, P = 0.004), despite a similar EF. On multivariate analysis, the presence non-obstructive atherosclerosis was the only significant predictor (P = 0.026) of post-stress LV diastolic impairment, independently from perfusion parameters.
Conclusions
In patients without anatomically significant coronary lesions, the development of post-stress LV diastolic dysfunction on MPI associates with the presence of non-obstructive atherosclerosis on coronary angiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the western world, ischemic heart disease (IHD) still represents a major cause of overall morbidity and mortality, and a major determinant of cardiac-related health expenditures.1 Therefore, in order to increase the effectiveness of cardiac therapies and to contain long-term sanitary costs, an early diagnosis of the presence of IHD seems of paramount importance. In this respect, while it is now accepted that the development of myocardial ischemia has generally a multifactorial nature,1-3 IHD has been classically associated with the presence of anatomically obstructive (i.e., >50% stenosis) epicardial coronary artery disease (CAD).4 Nevertheless, evidence has been accumulating on the role of diffuse, non-obstructive (<50% of lumen reduction), atherosclerosis in the genesis of myocardial ischemia, showing that relevant alterations of myocardial perfusion may develop even in the absence of apparently critical coronary lesions.2,3,5-7
Cardiac imaging plays a central role in the evaluation of the presence of myocardial ischemia, offering the chance to assess and quantitate its effects on myocardial structure and/or function. In particular, myocardial perfusion imaging (MPI) by single-photon emission computed-tomography (SPECT) still represents the backbone of the non-invasive evaluation of myocardial perfusion, allowing to evaluate the functional effects of a given coronary stenosis on regional myocardial perfusion.8,9
Moreover, SPECT-MPI gives the possibility to obtain reproducible measures of left ventricular (LV) systolic and diastolic functions that may help in the functional evaluation of CAD.10,11
Accordingly, it has been recently reported how the development of alterations of LV diastolic function during stress may represent an early marker of the presence myocardial ischemia, theoretically allowing a more precocious diagnosis of CAD.12 Nevertheless, while the evaluation of post-stress LV diastolic function has been shown to be able to detect the presence of obstructive coronary stenosis,13,14 the possible diagnostic power of stress-induced diastolic impairment in unmasking the presence of non-obstructive atherosclerosis has never been reported.
Interestingly, the recent introduction of dedicated cardiac cameras equipped with stationary cadmium-zinc-telluride detectors allows to perform an ultra-rapid imaging protocol with the stress acquisition consistently nearer than before to the end of the stressor (i.e., <15 minutes from the end of the stressor to the end of the acquisition),15,16 possibly giving the chance to assess better the presence of transient ischemia-related alteration of LV diastolic function.
With these considerations in mind, we sought to evaluate the relationships between non-obstructive coronary atherosclerosis, and myocardial perfusion, and functional parameters in patients with anginal chest pain, and suspected IHD and to assess the accuracy of stress-induced LV diastolic dysfunction in detecting the presence of anatomically non-obstructive coronary lesions.
Materials and Methods
Patient Population
All the consecutive subjects with cardiac chest pain and suspected IHD that, between January 2010 and June 2015, underwent a scintigraphic evaluation of myocardial perfusion with a CZT camera followed by invasive coronary angiography within 3 months were considered. The exclusion criteria were anatomically obstructive (>50% of diameter reduction) stenosis in any epicardial coronary vessel, recent (<6 months) acute coronary syndrome, hemodynamic instability, severely symptomatic heart failure, more than moderate valvular disease, and/or in the case of assessment of treatment efficacy. Therefore, a final population of 195 consecutive patients was included in the present analysis. The study was approved by the Local Ethical Committee and conformed to the Declaration of Helsinki on human research. Written informed consent was obtained from every patient.
Patient Preparation and Stress Protocols
According to our clinical practice, patients were asked to discontinue beta-blockers, calcium-antagonists, and long-acting nitrates for 24 to 48 hours before testing,17 while short-acting nitrates were allowed in case of angina. One-hundred and twenty-three patients (63%) underwent exercise while seventy-two patients (37%) dipyridamole stress testing. Bicycle exercise stress test (stepwise increments of 25 W every 2 minutes) or dipyridamole (0.56 mg/kg IV over 4 minutes) were chosen on the basis of the patient’s ability to exercise and to reach ≥85% of the maximal age-predicted heart rate. The stress protocol was completed in each patient without adverse events.
Acquisition Protocol
Patients underwent stress-rest CZT imaging with a single-day protocol (185-222 MBq of 99mTc-tetrofosmin during stress and 370-444 MBq at rest). In all patients, stress and rest CZT imaging were acquired as previously described.11,18 Stress-CZT imaging was performed 10-15 minutes after injection of the radiopharmaceutical with an acquisition time of 7 minutes. Patients were injected at rest 30 minutes after the end of the first acquisition and then, after an interval of 30-45 minutes, a second acquisition was carried out for 6 minutes.11,12 Patients were imaged in the supine position with arms placed over their head without any detector or collimator motion. All images were acquired with a 32 × 32 matrix and a 20% energy window centered at the 140 keV photopeak of 99mTc. List mode files were acquired and stored. Images were reconstructed on a standard workstation (Xeleris II; GE Healthcare, Haifa, Israel) using a dedicated iterative algorithm.17,18 All studies were reconstructed using a standard iterative algorithm with ordered-subset expectation maximization with 50 iterations, without resolution recovery or attenuation correction. A Butterworth post-processing filter (frequency 0.37, order 7) was applied to the reconstructed slices. The tomographic studies were also re-projected into 60 planar projections to emulate a standard SPECT layout.
Semiquantitative Analysis of Perfusion Images
Stress and rest images were semiquantitatively scored according to the 17-segment LV model and a five-point scale (0: normal, 1: equivocal, 2: moderate, and 3: severe reduction in radioisotope uptake, and 4: absence of detectable tracer uptake) by two experienced nuclear cardiologists (AG and PM), and consensus was reached in case of disagreement by re-evaluation of individual cases.12,17,18 Accordingly, the summed rest score (SRS) and stress score (SSS) were calculated. The SSS was considered pathological if >4.
Analysis of Gated Images
LV function analysis was performed from 16-frames reformatted images using a commercially available software (Corridor4DM, Invia, Ann Arbor, MI). In patients with inadequate border detection, manual editing was performed. End-diastolic volume (EDV), end-systolic volume (ESV), and ejection fraction (EF) were automatically calculated.10,11 Moreover, the same software automatically fits the left ventricular volume curve with a fourth-order harmonic function in order to derive the PFR (EDV*sec−1) as indicator of LV diastolic function.10,11,19 All functional measurements were obtained from rest and stress-gated 99mTc-tetrofosmin images.
In the absence of an accepted cut-off value of PFR, the presence of an abnormal post-stress LV diastolic function was defined when the PFR was ≤2.00 EDV*sec−1, corresponding to less than 2 standard deviations (SD) below the mean value in patients without CAD and no cardiovascular risk factors.
Invasive and CT Coronary Angiography
Invasive coronary angiography was performed using standard techniques and multiple projections. Coronary angiograms were quantified with a dedicated computer software (Advanced Vessel Analysis, Innova 3DXR for Advanced Workstations; GE Healthcare) using an automatic edge-contour detection algorithm to compute stenosis severity. In vessels showing multiple stenoses in series, only the most severe was considered. For the purpose of the present study, coronary vessels were categorized as follows: normal (absence of any CAD), minimal non-obstructive CAD (<20% of coronary luminal narrowing), and moderate non-obstructive CAD (>20% and <50% of coronary luminal narrowing).
Statistical Analysis
Continuous variables were expressed as mean ± SD in case of normal distribution or median ± interquartile range (IQR) if non-normally distributed, and categorical variables as percentages. Groups were compared for categorical data using Fisher’s exact test and for continuous variables using analysis of variance followed by Fisher’s protected least significant difference for multiple comparisons. In case of non-normal data distributions, the pertinent non-parametric test (i.e., The Kruskall-Wallis rank test) was used. All tests were 2-sided; a P < 0.05 was considered to be significant. The major predictors of the presence of non-obstructive CAD, among cardiovascular risk factors, myocardial perfusion, and LV functional parameters were assessed at multivariate logistic regression analysis. Finally, the accuracy of CZT-derived PFR in unmasking the presence of non-obstructive CAD was assessed by the receiving operating characteristic (ROC) analysis, and the most accurate diagnostic cut-off individuated. Statistical analyses were performed using JMP statistical software (SAS Institute Inc, version 4.0.0) and Stata software (Stata Statistical Software: Release 10, StataCorp. 2007, College Station, TX).
Results
Characterization of the Study Population
Table 1 shows the demographical and clinical characteristics of the whole patients’ population. As shown, the mean age of the study population was 69 ± 11 years with a significant predominance of male patients (65%). The majority of the study subjects were submitted to exercise stress MPI (63%), while 37% underwent pharmacological stress test, mainly due to the development of early effort dyspnea (61%). On coronary angiography, 60/195 (30%) of the patients showed moderate non-obstructive CAD (>20% and <50% stenosis), while the remainders presented either minimal CAD (<20% narrowing) (64%) or completely flat coronary arteries (6%). Accordingly, considering the limited number of patients with completely normal coronary arteries and the similar clinical characteristics with patients with minimal CAD, those subjects were conveniently grouped together for subsequent analyses.
Coronary Atherosclerosis and Myocardial Perfusion and Functional Data
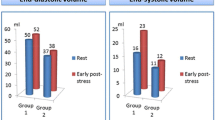
Of the 60 patients with angiographic evidence of moderate non-obstructive CAD (>20% and <50% stenosis), 37 presented a single coronary vessel involvement, while 23 a multi-vessel disease. On CZT-MPI, those patients presented more abnormal measures of stress-induced myocardial perfusion heterogeneity than subjects with normal coronary arteries or minimal CAD, despite a similar scar burden (Table 2). When LV functional parameters were considered, the presence of non-obstructive coronary atherosclerosis was associated with significantly impaired measures of LV diastolic function, as expressed by the post-stress PFR (P = 0.004), despite the absence of relevant reduction of post-stress LV ejection fraction (P = 0.240) (Table 2). In the whole patients’ population a significant, albeit modest, correlation between post-stress myocardial perfusion heterogeneity on MPI (SSS) and post-stress PFR was shown (Figure 1A). These findings were maintained both in patients submitted to exercise and to pharmacological stress test that presented overall similar CZT perfusion and LV diastolic functional parameters (PFR: 2.8 ± 0.8 vs 2.6 ± 0.9, respectively, P = 0.096).
Predictors of LV Diastolic Function Impairment
The relationships between coronary atherosclerotic burden and LV perfusion and functional variables were better investigated. In the whole population, an increasing extent of non-obstructive coronary atherosclerosis, as indicated by an increasing number of diseased coronary vessels, was associated with more abnormal measures of post-stress myocardial perfusion (Figure 1B) and LV diastolic function (Figure 2), despite similar scar burden (i.e., SRS; P = 0.669) and LV EF values (P = 0.213). Seventeen/sixty (28%) of the patients with moderate non-obstructive CAD (>20% and <50% stenosis) presented a significantly abnormal post-stress PFR (≤2.00 EDV*sec−1), while it was abnormal only in 13% of the patients with normal coronary arteries or minimal CAD (P = 0.007). Similarly, the development of an impaired post-stress PFR was significantly associated with higher SSS values, as a measure of stress-induced myocardial perfusion heterogeneity (Table 3). On multivariate regression analysis, after correction for demographic, perfusion, and angiographic parameters, the presence of moderate non-obstructive CAD (>20% and <50% stenosis) resulted the only independent predictor of stress-induced LV diastolic dysfunction (Table 4). Non-obstructive CAD remained the only predictor of PFR even after accounting for the type of the stressor performed during CZT-MPI (i.e., exercise vs pharmacological) (OR: 2.60, 95% CI 1.06-6.35; P = 0.036).
Discussion
The present study shows that in patients with chest pain without obstructive (>50% of lumen diameter stenosis) CAD, the development of stress-induced alterations of LV diastolic function could predict independently the presence of non-obstructive coronary lesions on coronary angiography. In those patients, the magnitude of post-stress impairment of LV diastolic function correlates with the extent of myocardial perfusion abnormalities on MPI and may represent an early functional marker of myocardial ischemia.
LV Diastolic Dysfunction and IHD
It is now accepted that the evaluation of symptomatic patients with suspected IHD should include the execution of a cardiac stress test, in order to define the specific location and overall extent of regional myocardial ischemia.1 Accordingly, each myocardial imaging modality is considered almost equivalent for the non-invasive evaluation of patients with suspected or known CAD, offering the chance to depict the functional effects of the presence of a given coronary lesion.1,8,20
In this respect, MPI by SPECT imaging still represents one of the most widely used methods for the assessment of the presence of cardiac perfusion abnormalities.9 At the same time, SPECT imaging is also capable to compute measures of LV systolic and diastolic functions, integrating the evaluation of regional myocardial perfusion with indexes of LV global and regional function.10,11,19
Specifically, while the occurrence of post-stress LV systolic stunning may be an index of the presence of diffuse significant CAD,21 different reports have suggested that the evaluation of LV diastolic function under stress conditions may give the chance to obtain more precocious markers of the presence of myocardial ischemia, theoretically offering the possibility to detect the presence of CAD at an early phase.12-14
Our results showed that in anginal patients submitted to MPI on a dedicated cardiac camera equipped with CZT detectors, the development of stress-induced alterations of LV diastolic function associate with the presence of non-obstructive atherosclerosis, and predict the presence of coronary lesions that reduce the luminal diameter of less than 50%.
In these patients, the occurrence of post-stress LV diastolic dysfunction was correlated with the presence of early signs of myocardial ischemia, as expressed by relatively limited myocardial perfusion abnormalities on CZT-MPI, suggesting how a combined assessment of myocardial perfusion and function may better detect patients at a more precocious stage of IHD.
In this respect, while myocardial perfusion abnormalities may result in LV diastolic impairment as an early functional sign of ischemia, the opposite relationship may also be true, since conditions specifically characterized by diastolic disfunction (i.e., LV hypertrophy) may hesitate in myocardial ischemia as an effect of increased LV intracavitary pressures.22
Relationships Between Myocardial Ischemia and Non-obstructive Atherosclerosis
The existence of a relationship between the anatomical severity of a coronary stenosis and alterations of downstream myocardial perfusion has been classically reported, and a cut-off of 50% of coronary luminal diameter reduction is generally believed as indicative of the presence of significant CAD.4 Nevertheless, myocardial ischemia may frequently develop in the absence of anatomically significant coronary lesions or even in the absence of appreciable CAD, still significantly predicting adverse prognosis.2,5
Different reports have demonstrated consistently that the haemodynamic relevance of a given coronary lesion, as evaluated both non-invasively and invasively (i.e., through invasive fractional flow reserve),5,6,23,24 may not be accurately predicted by its anatomic relevance, suggesting that the evaluation of the presence of functional measures of myocardial ischemia should be a mandatory step in the assessment of patients with any degree of CAD.1
In line with these reports, evidence has been accumulating on the possible role of diffuse, anatomically non-obstructive (<50% of coronary luminal reduction), atherosclerosis in impairing myocardial perfusion, also in the absence of discrete critical coronary lesions.6,7
Our study showed that, in patients with anginal chest pain without anatomically obstructive coronary lesions on coronary angiography, the presence of non-obstructive atherosclerosis associates independently with the development of post-stress alterations of LV diastolic function, as a functional measure of stress-induced myocardial ischemia. Interestingly, only the magnitude of post-stress PFR impairment was significantly correlated with myocardial ischemic burden, confirming its better diagnostic accuracy in detecting early CAD than LV systolic stunning.
In patients without anatomically obstructive coronary stenosis, the evidence of myocardial perfusion abnormalities by SPECT is generally considered as a false-positive finding, possibly as a result of an acquisition artifact. In this respect, present and previous5-7 results further suggest that non-obstructive coronary lesions may impair significantly regional myocardial perfusion and produce marked functional and clinical manifestations of IHD. This is in line with the recent ESC guidelines on stable angina that started to introduce “non conventional” mechanisms of myocardial ischemia (i.e., coronary microvascular dysfunction and coronary spasm) as frequent causes of anginal chest pain in patients without anatomically significant CAD.1
Limitations
The retrospective nature of the study prevented the selection of a homogeneous population of patients. Moreover, as consecutive patients submitted to MPI and coronary angiography by the referring physician were selected, the presence of some degrees of referral bias cannot be excluded.
The fact that, in patients with a history of myocardial infarction, sublingual nitrates were given prior to the rest scan might have impacted the evaluation of myocardial perfusion. However, in those patients the pre-treatment with nitrates allows a significantly more precise evaluation of residual myocardial viability on MPI. Furthermore, since the post-stress acquisition was performed 15 minutes after the completion of the dipyridamole infusion or of the exercise test, the evaluation of the magnitude of post-stress PFR functional abnormalities could have been impaired. Nevertheless, considering the timing of the employed imaging protocol, a more precocious assessment of LV function seems unrealistic.
Moreover, the radiotracer’s dose and the stress-to-rest dose ratio and the acquisition times used in the present study are relatively low if compared to those generally used with traditional SPECT devices. However, those parameters were already validated in different patients’ population studied with a CZT camera, allowing an excellent image quality despite a reduced radiation burden.11,12,17-19 In the present study, attenuation correction of CZT images was not performed mainly for technical reasons, and specifically because of the logistic difficulty to make every patient undergo a low-dose chest CT in the absence of a hybrid CZT-CT scanner. Nevertheless, previous reports have suggested that the actual additive diagnostic value of attenuation correction might be limited.25
Finally, in the present study, the few patients with completely flat coronary arteries and those with minimal CAD (< 20% coronary narrowings) were grouped together. Accordingly, while the relationships between extremely limited atherosclerosis and myocardial ischemia could not be conclusively explored, previous reports have shown how its specific effect on myocardial perfusion should be limited.4
Conclusions
In patients with chest pain despite the absence of anatomically obstructive (>50% of coronary luminal diameter reduction) CAD, the reduction of post-stress LV diastolic function on CZT-MPI associates with the presence of non-obstructive atherosclerosis on coronary angiography. In those subjects, the degree of post-stress LV diastolic impairment correlates with myocardial perfusion abnormalities on MPI, suggesting how a combined evaluation of myocardial perfusion and diastolic function may better detect the presence of early stages of CAD. However, due to the rather consistent overlap of PFR values between patients’ categories and the relatively low number of enrolled patients, the present study remains a proof-of-concept investigation, and larger studies are needed to define conclusively the causal relationships between myocardial ischemia and non-obstructive atherosclerosis.
New Knowledge Gained
The evidence of myocardial perfusion abnormalities in the absence of anatomically obstructive CAD is frequently believed to be a benign finding secondary to imaging artifacts. Present results suggest that myocardial ischemia may develop even in the presence of non-obstructive coronary lesions and result in alterations of post-stress LV diastolic function. Accordingly, the results of our proof-of-concept study suggest that impaired measures of post-stress LV diastolic function may represent additive markers in the clinical management of patients with suspected IHD and may represent early signs of the presence of non-obstructive coronary atherosclerosis.
Abbreviations
- CZT:
-
Cadmium-zinc-telluride
- CAD:
-
Coronary artery disease
- IHD:
-
Ischemic heart disease
- SRS:
-
Summed rest score
- SSS:
-
Summed stress score
- PFR:
-
Peak filling rate
References
Task Force Members. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830-40.
Liga R, Marini C, Coceani M, Filidei E, Schlueter M, Bianchi M, et al. Structural abnormalities of the coronary arterial wall-in addition to luminal narrowing-affect myocardial blood flow reserve. J Nucl Med 2011;52:1704-12.
Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 1994;330:1782-8.
Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc Imaging 2012;5:193-202.
De Bruyne B, Hersbach F, Pijls NH, Bartunek J, Bech JW, Heyndrickx GR, et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “Normal” coronary angiography. Circulation 2001;104:2401-6.
Gould KL, Nakagawa Y, Nakagawa K, Sdringola S, Hess MJ, Haynie M, et al. Frequency and clinical implications of fluid dynamically significant diffuse coronary artery disease manifest as graded, longitudinal, base-to-apex myocardial perfusion abnormalities by noninvasive positron emission tomography. Circulation 2000;101:1931-9.
Parker MW, Iskandar A, Limone B, Perugini A, Kim H, Jones C, et al. Diagnostic accuracy of cardiac positron emission tomography versus single photon emission computed tomography for coronary artery disease: A bivariate meta-analysis. Circ Cardiovasc Imaging 2012;5:700-7.
Hesse B, Tägil K, Cuocolo A, Anagnostopoulos C, Bardiés M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855-97.
Giorgetti A, Masci PG, Marras G, Rustamova YK, Gimelli A, Genovesi D, et al. Gated SPECT evaluation of left ventricular function using a CZT camera and a fast low-dose clinical protocol: Comparison to cardiac magnetic resonance imaging. Eur J Nucl Med Mol Imaging 2013;40:1869-75.
Gimelli A, Liga R, Pasanisi EM, Giorgetti A, Marras G, Favilli B, et al. Evaluation of left ventricular diastolic function with a dedicated cadmium-zinc-telluride cardiac camera: Comparison with Doppler echocardiography. Eur Heart J Cardiovasc Imaging 2014;15:972-9.
Gimelli A, Liga R, Bottai M, Pasanisi EM, Giorgetti A, Fucci S, et al. Diastolic dysfunction assessed by ultra-fast cadmium-zinc-telluride cardiac imaging: Impact on the evaluation of ischaemia. Eur Heart J Cardiovasc Imaging 2015;16:68-73.
Detry JMR. The pathophysiology of myocardial ischemia. Eur Heart J 1996;17:48-52.
Ishii K, Imai M, Suyama T, Maenaka M, Nagai T, Kawanami M, et al. Exercise-induced postischemic left ventricular delayed relaxation or diastolic stunning: Is it a reliable marker in detect in coronary artery disease? J Am Coll Cardiol 2009;53:698-705.
Gimelli A, Bottai M, Giorgetti A, Genovesi D, Kusch A, Ripoli A, et al. Comparison between ultrafast and standard single-photon emission CT in patients with coronary artery disease: A pilot study. Circ Cardiovasc Imaging 2011;4:51-8.
Herzog BA, Buechel RR, Katz R, Brueckner M, Husmann L, Burger IA, et al. Nuclear myocardial perfusion imaging with a cadmium-zinc-telluride detector technique: Optimized protocol for scan time reduction. J Nucl Med 2010;51:46-51.
Gimelli A, Liga R, Coceani M, Quaranta A, Emdin M, Marzullo P. Chronotropic response to vasodilator-stress in patients submitted to myocardial perfusion imaging: Impact on the accuracy in detecting coronary stenosis. Eur J Nucl Med Mol Imaging 2015;42:1903-11.
Gimelli A, Liga R, Pasanisi EM, Casagranda M, Coceani M, Marzullo P. Influence of cardiac stress protocol on myocardial perfusion imaging accuracy: The role of exercise level on the evaluation of ischemic burden. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0101-z.
Gimelli A, Liga R, Giorgetti A, Kusch A, Pasanisi EM, Marzullo P. Relationships between myocardial perfusion abnormalities and poststress left ventricular functional impairment on cadmium-zinc-telluride imaging. Eur J Nucl Med Mol Imaging 2015;42:94-1003.
Sicari R, Nihoyannopoulos P, Evangelista A, Kasprzak J, Lancellotti P, Poldermans D, et al. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 2008;9:415-37.
Abidov A, Bax JJ, Hayes SW, Cohen I, Nishina H, Yoda S, et al. Integration of automatically measured transient ischemic dilation ratio into interpretation of adenosine stress myocardial perfusion SPECT for detection of severe and extensive CAD. J Nucl Med 2004;45:1999-2007.
Cannon RO 3rd, Rosing DR, Maron BJ, Leon MB, Bonow RO, Watson RM, et al. Myocardial ischemia in patients with hypertrophic cardiomyopathy: Contribution of inadequate vasodilator reserve and elevated left ventricular fulling pressures. Circulation 1985;71:234-43.
Takx RA, Blomberg BA, El Aidi H, Habets J, de Jong PA, Nagel E, et al. Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging 2015;8:e002666. doi:10.1161/CIRCIMAGING.114.002666.
Neglia D, Rovai D, Caselli C, Pietila M, Teresinska A, Aguadé-Bruix S, et al. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging 2015;8:e002179. doi:10.1161/CIRCIMAGING.114.002179.
Genovesi D, Giorgetti A, Gimelli A, Kusch A, D’Aragona Tagliavia I, Casagranda M, et al. Impact of attenuation correction and gated acquisition in SPECT myocardial perfusion imaging: Results of the multicentre SPAG (SPECT Attenuation Correction vs Gated) study. Eur J Nucl Med Mol Imaging 2011;38:1890-8.
Disclosure
Alessia Gimelli, Riccardo Liga, Emilio Maria Pasanisi, Mirta Casagranda, and Paolo Marzullo have no conflict of interest or relationship with industries to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0486-3.
Alessia Gimelli and Riccardo Liga share the first co-authorship.
Rights and permissions
About this article
Cite this article
Gimelli, A., Liga, R., Pasanisi, E.M. et al. Myocardial ischemia in the absence of obstructive coronary lesion: The role of post-stress diastolic dysfunction in detecting early coronary atherosclerosis. J. Nucl. Cardiol. 24, 1542–1550 (2017). https://doi.org/10.1007/s12350-016-0456-9
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0456-9