Abstract
Background
The diagnosis of infective endocarditis (IE), especially the diagnosis of prosthetic valve endocarditis (PVE) is challenging since echocardiographic findings are often scarce in the early phase of the disease. We studied the use of 2-[18F]fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) in IE.
Methods
Sixteen patients with suspected PVE and 7 patients with NVE underwent visual evaluation of 18F-FDG-PET/CT. 18F-FDG uptake was measured also semiquantitatively as maximum standardized uptake value (SUVmax) and target-to-background ratio (TBR). The modified Duke criteria were used as a reference.
Results
There was strong, focal 18F-FDG uptake in the area of the affected valve in all 6 cases of definite PVE, in 3 of 5 possible PVE cases, and in 2 of 5 rejected cases. In all patients with definite PVE, SUVmax of the affected valve was higher than 4 and TBR higher than 1.8. In contrast to PVE, only 1 of 7 patients with NVE had uptake of 18F-FDG by PET/CT in the valve area. Embolic infectious foci were detected in 58% of the patients with definite IE.
Conclusions
18F-FDG-PET/CT appears to be a sensitive method for the detection of paravalvular infection associated with PVE. Instead, the sensitivity of PET/CT is limited in NVE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE) is a life-threatening disease.1-5 Despite developments in both imaging and microbiological techniques, the diagnosis of IE is challenging, especially the diagnosis of prosthetic valve endocarditis (PVE). The current standard of clinical assessment is the modified Duke criteria.6 , 7 According to the modified Duke criteria, definite diagnosis of IE is mainly based on positive blood cultures with a typical micro-organism and/or evidence of IE by echocardiography. Sensitivity of transthoracic echocardiography (TTE) for endocarditis ranges from 20% to 65% and that of transesophageal echocardiography (TEE) from 70% to 90%.8-10 Sensitivity can be improved by doing repeated examinations.8,11 However, identification of IE vegetation in the presence of pre-existing valve lesions and differential diagnosis between IE vegetation and other pathologies, such as thrombosis can be difficult.12 Furthermore, the sensitivity of echocardiography for diagnosing PVE is lower compared to diagnosing native valve infective endocarditis (NVE).8,13 Rapid diagnosis of IE is important as early initiation of effective antimicrobial treatment prevents complications requiring valve surgery.7 Therefore, new more sensitive methods to detect IE are needed.
Positron emission tomography (PET) with the glucose analogue 2-[18F]fluoro-2-deoxy-D-glucose (18F-FDG) has been used to detect inflammation and infection based on high glucose uptake of leukocytes. Recent studies have indicated that 18F-FDG-PET/CT may be useful in IE, especially in the detection of extracardiac infectious foci.14-16 However, less is known about the ability of 18F-FDG-PET/CT to visualize directly heart valve infection in NVE or PVE. Therefore, we wanted to study the diagnostic value of 18F-FDG-PET/CT imaging of valvular infection in patients with suspected PVE or NVE.
Methods
Patients
This prospective study evaluated 23 consecutive patients admitted to Turku University Hospital, Turku, Finland between September 2011 and September 2014 due to suspected NVE or PVE. Patients with hemodynamic instability or need for urgent surgery were excluded. The hospital is a tertiary-care center for the south-west part of the country. Seven of the patients had suspected NVE and 16 of the patients had suspected PVE. The study was approved by the institutional ethical review board, and all participants signed an informed consent.
On admission and during hospital stay, clinical history and findings as well as data on blood culture findings and serum markers of inflammation (C-reactive protein and procalcitonin) were collected. Times from the onset of symptoms, onset of antimicrobial treatment, and valvular surgery to PET/CT were recorded. TEE was done in all except one patient who had tricuspid valve vegetation visible on TTE. Histological and microbiological findings of the tissue specimens taken during the operation were evaluated when available. Follow-up after hospital discharge was conducted for a mean of 19 months (range 2-33 months).
The clinical diagnosis of IE was done by expert team according to the modified Duke criteria7 and based on all available clinical and microbiological data, but excluding PET/CT findings. The modified Duke criteria were determined after the follow-up.
18F-FDG-PET/CT
A whole-body or cardiac 18F-FDG-PET/CT scan (Discovery VCT, General Electric Medical Systems, Milwaukee, WI, USA) was performed in all patients. Mean time from hospital admission to PET/CT was 5 days in NVE and 13 in PVE. In order to reduce physiological glucose uptake of the myocardium, patients were on low-carbohydrate diet for 24 hours before the PET-scan and fasted at least 10 hours before the study.17 Mean injected dose of 18F-FDG was 280 MBq (range 147-371 MBq). An average of 72 minutes (range 52-98 minutes) later a whole-body PET acquisition (3 minutes per bed position) was performed following CT scan for anatomical reference and attenuation correction. One patient had only cardiac PET/CT.
Blood glucose levels were <10 mmol∙L−1 prior to injection of the tracer in all patients. PET images were reconstructed with 128 × 128 matrix size in full 3D mode using maximum-likelihood reconstruction with ordered-subsets expectation maximization algorithm (VUE Point, GE Healthcare).
Visual analysis of the images was performed by an experienced nuclear medicine specialist and results were re-evaluated by the research team for consensus. All image analyses were done blinded with respect to patient’s clinical details. A positive finding was defined as an increase in 18F-FDG accumulation in the valve or valve prosthesis area. The presence of visual FDG uptake in attenuation corrected images was confirmed in non-attenuation corrected images when appropriate. In addition to the valves, the images were evaluated for the presence of abnormal 18 F-FDG accumulation elsewhere in the body.
18F-FDG uptake was also measured semiquantitatively as maximum standardized uptake value (SUVmax) which was obtained by normalizing the tissue concentration of FDG activity and the patient’s weight and as target-to-background ratio (TBR). The SUVmax was measured in a volume of interest covering the valve or prosthesis area based on co-registered CT images. Mean volume size was 14.6 cm3 in the aortic and 13.1 cm3 in the mitral position. The mean background radioactivity in the blood was measured in the ascending aorta excluding the vessel wall (mean radioactivity in a volume of interest of 6.8 cm3) to calculate TBR.
Statistical Analysis
Values are shown as medians or means with range of values. 18F-FDG uptake in the affected valve and another valve of the same patient were compared using Wilcoxon signed rank test and in the valves of patients with definitive, possible, or rejected PVE by Kruskall-Wallis test. A value of P < .05 was considered significant. Statistical analyses were performed using SAS for Windows, version 9.4 (SAS Institute Inc., Cary, NC).
Results
Clinical characteristics, TEE findings, microbiological findings, and diagnostic classification based on the modified Duke criteria of the patients are presented in Table 1.
Clinical Characteristics in Suspected NVE
Seven patients had suspected NVE. The mean age of these patients was 53 years and 6 were males. Time from the onset of symptoms to PET/CT was on average 48 days (range 5-150 days) and from the onset of antimicrobial treatment 5 days (range 3-7 days). Surgery was performed in 4 cases with definite IE and histological examination confirmed the diagnosis. The patient with the paravalvular abscess died after surgery.
Clinical Characteristics in Suspected PVE
There were 16 patients with suspected PVE. Mean age was 67 years and 14 were males. Time from surgery to PET/CT varied from 4 weeks to 28 years (Table 3). Times from the onset of symptoms and from commencement of antimicrobial treatment to PET/CT were on average 16 days (range 5-62 days) and 13 days (range 0-59 days), respectively. Surgery was performed in 2 cases (Patient #12 and #20 in Table 1). Histology and microbiological tests confirmed the diagnosis in the case with definitive IE whereas, in the other case with possible PVE histology showed no signs of IE. During follow-up, 4 patients (25%) died due to IE, heart failure, chronic obstructive pulmonary disease, or colon cancer.
18F-FDG-PET/CT Findings in Suspected NVE
Of the seven patients with NVE, visual analysis of 18F-FDG-PET/CT images showed increased tracer uptake in the aortic valve region in only one patient who also had a paravalvular abscess (Table 2; Figure 1). In the remaining six cases with NVE, the visual analysis was negative even in the presence of large vegetations on TEE (Figure 1). Median SUVmax of the affected valves was 2.7 (range 2.4-8.3) and TBR 1.3 (range 1.0-2.9) that were comparable with the non-affected valves (2.5 (range 1.4-3.5) and 1.2 (range 1.0-1.9), P = .813 and P = .813, respectively). Thus, PET/CT was positive only in 1 of the 6 definite cases of NVE, indicating that the sensitivity for the detection of infection in the native valves is low.
Examples of 18F-FDG-PET/CT (panels A-C and D-F) and transesophageal echocardiography (TEE, panels G, H and I, J) images of two patients with native valve endocarditis (NVE). The upper row shows no 18F-FDG uptake at the site of aortic valve (arrows in panels A-C) despite large vegetation on TEE (panels G, H). Note some physiological 18F-FDG uptake in the myocardium. The lower row shows increased 18F-FDG uptake at the site of aortic valve (arrow in panels D-F) in a patient with a paravalvular abscess on TEE (panels I, J)
18F-FDG-PET/CT Findings in Suspected PVE
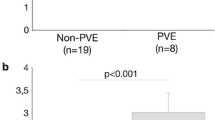
In definite PVE, visual analysis of PET/CT images showed 18F-FDG uptake of the prosthetic valve area in all 6 cases. The SUVmax of 4 was identified as a cut-off point differentiating visually PET positive and negative cases. In all patients with definite PVE, SUVmax of the affected valve was higher than 4 and TBR higher than 1.8. Median SUVmax and TBR of the affected valve were significantly higher compared with the SUVmax and TBR of the native valve of these patients (5.8 (range 4.1-9.0) and 2.3 (range 1.9-3.8) vs 2.5 (range 1.9-3.4), and 1.1 (range 1.0-1.2), P = .031 and .031).
In possible PVE, 18F-FDG uptake of the prosthetic valve area was visually detected in 3 of 5 patients. SUVmax was higher than 4 in all of these 3 cases. In the group of possible PVE, median SUVmax and TBR of the prosthetic valves were 5.2 (range 3.4-8.4) and 2.0 (range 1.5-3.0), and 3.0 (range 2.8-3.3) and 1.3 (range 1.0-1.7) in the native valves of the same patients. In the 3 patients with possible PVE and positive 18F-FDG finding, positive blood culture and clinical data, including positive response to antimicrobial therapy, supported the diagnosis of PVE despite negative TEE findings. In addition one of these patients (Patient #14 in Table 3) had biological aortic and mitral prostheses, but 18F-FDG uptake only at the aortic valve prosthesis area (Figure 2). In 2 patients with possible PVE and negative 18F-FDG finding of the prosthetic valve, an alternative diagnostic finding was detected in PET/CT: pneumonia in one and colon tumor and metastasis in the other.
Examples of 18F-FDG-PET/CT images of a patient with prosthetic valve endocarditis (PVE). The upper row shows increased 18F-FDG uptake at the site of the aortic valve prosthesis (arrows in panels A-C) and the lower row shows no 18F-FDG uptake at the site of mitral valve prosthesis in the same patient (arrows in panels E-G). The whole-body 18F-FDG-PET/CT image shows focal tracer uptake at the site of aortic valve (arrow in panel D)
Median SUVmax and TBR of the prosthetic valve of the rejected group were 4.8 (range 2.9-7.8) and 2.2 (range 1.3-3.3), and 2.5 (range 2.1-3.3) and 1.2 (range 0.9-1.6) in the native valves. Four patients in this group had prolonged fever of unknown cause after recent (4-14 weeks) valve surgery. They all received anti-inflammatory treatment for suspected post-pericardiotomy syndrome and had an uncomplicated clinical course. In 3 of these 4 patients, PET/CT did not show valvular 18F-FDG uptake. One of these PET/CT negative patients (Patient #19 Table 1) had suspected vegetation on TEE, but that was most likely a remnant of the native valve as there was no progression during 1 year follow-up. However, one patient (Patient #23 Table 3) showed 18F-FDG uptake of the aortic valve prosthesis, which was later classified false positive. In addition, the rejected group included one patient with positive valvular 18F-FDG uptake (Patient #20 Table 3) and echocardiographic suspicion of IE. This patient was operated due to aneurysm of sinus valsalva, the microbiological tests obtained from the valve were negative and histology showed a foreign body reaction around the valve instead of endocarditis.
When comparing the SUVmax and TBR values of the prosthetic valves in patients with definitive, possible or rejected PVE, no significant difference was found between the groups ( P = 0.301 and 0.264).
In summary, visual 18F-FDG uptake and SUVmax > 4.0 was detected in all 6 patients with definite PVE (sensitivity 100%, 95% CI 54.1-100.0%). However, specificity of 18F-FDG-PET/CT was only 60% (95% CI 14.7-94.7%). By using the cut-off value of SUVmax of 4.0 as a criterion for definite PVE, 3 of the 5 cases with possible PVE and 2 of the 5 cases of rejected PVE would be defined as definite PVE.
Embolic Foci
Embolic and/or metastatic infectious foci were detected in 7 of 12 (58%) patients with definitive IE (4 NVE and 3 PVE). All of the NVE patients had peripheral infectious emboli in the limbs. Besides that, 1 had pulmonary infection foci and 1 had embolic infarction of spleen and kidney. The patient with splenic and kidney infarction had also an embolic finding in retina, which was not detected by PET/CT. PET/CT showed spondylodiscitis in 2 definite and 1 possible PVE patient. In 1 definite PVE patient, PET/CT showed peripheral infectious emboli in lower limbs. Pulmonary infection as well as splenic and kidney infarctions were confirmed by CT findings and spondylodiscitis by magnetic resonance imaging.
Other Findings
In addition to the case with apparent malignant colon tumor and metastasis detected in 1 case, PET/CT showed high 18F-FDG uptake in the colon in another case (Patient #20 in Table 3) in whom colitis ulcerosa was later diagnosed. Pericardial uptake of 18F-FDG confirmed the diagnosis of postpericardiotomy syndrome in 1 case. In addition, Paget’s disease was later confirmed in 1 patient with high uptake of 18F-FDG in iliac bone and femur.
Discussion
The main findings of the present study are that the sensitivity of 18F-FDG-PET/CT for detecting valvular infection in NVE was low in the absence of paravalvular involvement. In contrast, 18F-FDG uptake in the valve region was a consistent finding in definite PVE. These results in this small patient cohort suggest that 18F-FDG-PET/CT is a sensitive method for detecting paravalvular infection in IE.
Case reports have shown 18F-FDG accumulation in the infected valve in patients with NVE,18-20 but this has been rare in larger series of patients with NVE.14-16,21,22 Our study is one of the few series of patients with definite NVE according to the Duke criteria. In line with the studies of Ricciardi et al21 and Kestler et al22 our results show that even in the presence of a large vegetation on TEE, 18F-FDG uptake was not detectable in the infected valves. The possible explanation to this is that small size and continuous movement of vegetation may reduce sensitivity of PET. In addition, patients with NVE tend to develop more frequently vegetations than abscesses and vegetations contain less activated inflammatory cells than peri-valvular abscesses. Antimicrobial therapy before 18F-FDG-PET/CT may have also reduced tracer uptake and inflammatory activity in these lesions. Still, as the diagnostic performance of TEE is better in patients with a suspicion of NVE, the need for a new diagnostic method and interest of FDG-PET imaging is less obvious in NVE than in PVE.
Interestingly,18F-FDG-PET/CT was positive in 1 patient with NVE who also had large para-aortic abscess on TEE that was confirmed during surgery. Early detection of paravalvular complications is often challenging.13 Based on our finding and some case reports18,19 further studies seem warranted on the value of 18F-FDG-PET/CT in the detection of paravalvular complications of NVE.
Two recent clinical studies indicate that valvular 18F-FDG uptake is common in PVE and 18F-FDG-PET/CT may even improve sensitivity of detection of PVE as compared with the conventional clinical work-up.21,23 Our results are in line with those, since 18F-FDG-PET/CT was positive in all cases with definite PVE. We found SUVmax of 4.0 or higher in all cases with definitive PVE indicating that it could be used as a cut-off value for objective assessment of scans. However, further studies with larger patient populations are needed to study whether any cut-off point of SUVmax can be used in clinical practise. Paravalvular extension is a typical feature of PVE. However, sensitivity of TEE for the detection of paravalvular leak or abscess is limited and therefore, new diagnostic tools are needed. Our results indicate that 18F-FDG-PET/CT has potential for the early detection of paravalvular infection. However, it is important to notice that in previous studies 18F-FDG accumulation has been absent in many patients with definite or possible PVE14,15,21-23 and therefore, more studies are needed to confirm its diagnostic value in PVE.
Regarding specificity of 18F-FDG-PET/CT, one must bear in mind that distinction between infection and inflammation is not possible. This was highlighted by the two false positive cases in whom 18F-FDG uptake associated with foreign body reaction in 1 patient and with recent valve surgery in another patient. Within the first weeks after surgery, the natural wound healing process may explain the 18F-FDG uptake. This may be of clinical relevance since the risk of PVE is highest in the first 3 months after surgery.24 Our study included 6 patients who underwent PET/CT 4-18 weeks after valve operation. In 2 of them, a positive 18F-FDG-PET/CT study was associated with possible or definite PVE. In the patient with possible PVE, only 1 of the 2 valve prosthesis was positive supporting the diagnosis of IE. It is of interest that in one patient 18F-FDG uptake was found in the pericardium supporting the diagnosis of postpericardiotomy syndrome (Patient #22).25 Further studies are warranted to study the accuracy of 18F-FDG-PET/CT in the early postoperative period.
In our study, image quality of 18F-FDG-PET/CT was considered diagnostic in all patients. Diet intervention efficiently reduced physiological uptake of 18F-FDG in the myocardium that is probably essential for good image quality.
In several patients, there were extracardiac findings in the 18F-FDG-PET/CT study that can provide valuable additional diagnostic information. Embolic and/or metastatic infectious foci were detected in 58% of the patients with definite IE. This supports previous studies on PET/CT and IE showing embolic foci in 44-57% of the patients with definite IE.15,16,22,26
Limitations
Our study is limited by the small number of the patients. As a result no firm conclusions can be driven based on our results. Also the time interval between admission and PET/CT varied from 1 to 59 days. One of the general limitations of all studies of suspected IE is the lack of a gold standard for IE diagnosis, which could be applied in all patients. The Duke criteria are based on current understanding of the various tests and are subject to revisions according to the new clinical evidence. The cut-off values for SUVmax and TBR in the present study should be tested prospectively in another patient cohort. Furthermore, the optimal imaging and analysis protocols for quantification of valvular FDG uptake remain to be determined in future studies.27
New Knowledge Gained
18F-FDG-PET/CT appears to be a sensitive method for the detection of paravalvular infection associated with PVE. Instead, the sensitivity of PET/CT was limited in NVE.
Conclusions
18F-FDG-PET/CT appears to detect paravalvular infection in IE and may provide additional information over echocardiography in the evaluation of suspected PVE. However, the sensitivity of 18F-FDG-PET/CT for detecting NVE in the absence of paravalvular involvement is low. More studies with larger patient groups are warranted to study the value of 18F-FDG-PET/CT in the diagnostic workup of PVE.
Abbreviations
- IE:
-
Infective endocarditis
- PVE:
-
Prosthetic valve endocarditis
- NVE:
-
Native valve endocarditis
- PET/CT:
-
Positron emission tomography/computed tomography
- 18F-FDG:
-
2[18F]fluoro-2-deoxy-D-glucose
- SUVmax :
-
Maximum standardized uptake value
- TBR:
-
Target-to-background ratio
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
References
Tleyjeh IM, Abdel-Latif A, Rahbi H, Scott CG, Bailey KR, Steckelberg JM, et al. A systematic review of population-based studies of infective endocarditis. Chest 2007;132:1025-35.
Heiro M, Helenius H, Hurme S, Savunen T, Engblom E, Nikoskelainen J, et al. Short-term and one-year outcome of infective endocarditis in adult patients treated in a Finnish teaching hospital during 1980–2004. BMC Infect Dis 2007;7:78.
Heiro M, Helenius H, Hurme S, Savunen T, Metsärinne K, Engblom E, et al. Long-term outcome of infective endocarditis: A study on patients surviving over one year after the initial episode treated in a Finnish teaching hospital during 25 years. BMC Infect Dis 2008;8:49.
Leitman M, Dreznik Y, Tyomkin V, Fuchs T, Krakover R, Vered Z. Vegatation size in patients with infective endocarditis. Eur Heart J Cardiovasc Imaging 2012;13:330-8.
Hill EE, Herijgers P, Claus P, Vanderschueren S, Peetermans WE, Herregods MC. Clinical and echocardiographic risk factors for embolism and mortality in infective endocarditis. Eur J Clin Microbiol Infect Dis 2008;27:1159-64.
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633-8.
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): The task force on the prevention, diagnosis, and treatment of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J 2009;30:2369-413.
Vieira ML, Grinberg M, Pomerantzeff PM, Andrade JL, Mansur AJ. Repeated echocardiographic examinations of patients with suspected infective endocarditis. Heart 2004;90:1020-4.
Habib G, Derumeaux G, Avierinos JF, Casalta JP, Jamal F, Volot F, et al. Value and limitations of the Duke criteria for the diagnosis of infective endocarditis. J Am Coll Cardiol 1999;33:2023-9.
Daniel WG, Mügge A, Grote J, Hausmann D, Nikutta P, Laas J, et al. Comparison of transthoracic and transesophageal echocardiography for detection of abnormalities of prosthetic and bioprosthetic valves in the mitral and aortic positions. Am J Cardiol 1993;71:210-5.
Sochowski RA, Chan KL. Implication of negative results on a monoplane transesophageal echocardiographic study in patients with suspected infective endocarditis. J Am Coll Cardiol 1993;21:216-21.
Rozich JD, Edwards WD, Hanna RD, Laffey DM, Johnson GH, Klarich KW. Mechanical prosthetic valve-associated strands: Pathologic correlates to transesophageal echocardiography. J Am Soc Echocardiogr 2003;16:97-100.
Hill EE, Herijgers P, Claus P, Vanderschueren S, Peetermans WE, Herregods MC. Abscess in infective endocarditis: The value of transesophageal echocardiography and outcome. Am Heart J 2007;154:923-8.
Bonfiglioli R, Nanni C, Morigi JJ, Graziosi M, Trapani F, Bartoletti M, et al. 18F-FDG PET/CT diagnosis of unexpected extracardiac septic embolisms in patients with suspected cardiac endocarditis. Eur J Nucl Med Mol Imaging 2013;40:1190-6.
Van Riet J, Hill EE, Gheysens O, Dymarkowski S, Herregods MC, Herijgers P, et al. (18)F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging 2010;37:1189-97.
Özcan C, Asmar A, Gill S, Thomassen A, Diederichsen AC. The value of FDG-PET/CT in the diagnostic work-up of extra cardiac infectious manifestations in infectious endocarditis. Int J Cardiovasc Imaging 2013;29:1629-37.
Williams G, Kolodny GM. Suppression of myocardial 18F-FDG uptake by preparing patients with a high-fat, low-carbohydrate diet. AJR Am J Roentgenol 2008;190:W151-6.
Vind SH, Hess S. possible role of PET/CT in infective endocarditis. J Nucl Cardiol 2010;17:516-9.
Gheysens O, Lips N, Adriaenssens T, Pans S, Maertens J, Herregods MC, et al. Septic pulmonary embolism and metastatic infections from methicillin-resistant Staphylococcus aureus endocarditis on FDG PET/CT. Eur J Nucl Med Mol Imaging 2012;39:183.
Millar BC, Prendergast BD, Alavi A, Moore JE. 18FDG-positron emission tomography (PET) has a role to play in the diagnosis and therapy of infective endocarditis and cardiac device infection. Int J Cardiol 2013;167:1724-36.
Ricciardi A, Sordillo P, Ceccarelli L, Maffongelli G, Calisti G, Di Pietro B, et al. 18-Fluoro-2-deoxyglucose positron emission tomography-computed tomography: An additional tool in the diagnosis of prosthetic valve endocarditis. Int J Infect Dis 2014;28:219-24.
Kestler M, Muñoz P, Rodríguez-Créixems M, Rotger A, Jimenez-Requena F, Mari A, et al. Role of 18F-FDG PET in patients with infectious endocarditis. J Nucl Med 2014;55:1093-8.
Saby L, Laas O, Habib G, Cammilleri S, Mancini J, Tessonnier L, et al. Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis: Increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J Am Coll Cardiol 2013;61:2374-82.
Ivert TS, Dismukes WE, Cobbs CG, Blackstone EH, Kirklin JW, Bergdahl LA. Prosthetic valve endocarditis. Circulation 1984;69:223-32.
Salomäki SP, Hohenthal U, Kemppainen J, Pirilä L, Saraste A. Visualization of pericarditis by fluorodeoxyglucose PET. Eur Hear J Cardiovasc Imaging 2014;15:291.
Asmar A, Ozcan C, Diederichsen AC, Thomassen A, Gill S. Clinical impact of 18F-PET/CT in the extra cardiac work-up of patients with infective endocarditis. Eur Heart J Cardiovasc Imaging 2014;15:1013-9.
Huet P, Burg S, Le Guludec D, Hyafil F, Buvat I. Variability and uncertainty of 18F-FDG PET imaging protocols for assessing inflammation in atherosclerosis: Suggestions for improvement. J Nucl Med 2015;56:552-9.
Acknowledgement
The study was conducted in the Finnish Centre of Excellence in Cardiovascular and Metabolic Diseases supported by the Academy of Finland, University of Turku, Turku University Hospital, and Åbo Akademi University. The study was supported by the State Research Funds of the Turku University Hospital, and Orion-Farmos Research Foundation.
Disclosure
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi: 10.1007/s12350-015-0369-z.
Rights and permissions
About this article
Cite this article
Salomäki, S.P., Saraste, A., Kemppainen, J. et al. 18F-FDG positron emission tomography/computed tomography in infective endocarditis. J. Nucl. Cardiol. 24, 195–206 (2017). https://doi.org/10.1007/s12350-015-0325-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0325-y