Abstract
Background
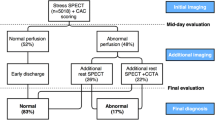
We conducted an exploratory analysis to test whether the addition of a CAC scan can increase the applicability of stress-only SPECT-MPI.
Methods
We studied 162 patients referred for rest/stress SPECT-MPI who underwent a CAC scan. Each scan was interpreted by two readers in stepwise fashion: stress-only images; addition of clinical data; and addition of CAC data. At each step, the reader was asked if rest SPECT-MPI was necessary.
Results
Stress-only images were interpreted as normal in 62, probably normal in 42, equivocal in 15, probably abnormal in 5, and definitely abnormal in 38 patients. Rest SPECT-MPI imaging was considered necessary, in 0% of normal studies, but in 88% of probably normal studies, and 100% of those with equivocal/abnormal studies. Addition of the clinical data did not materially change this decision. Additional consideration of the CAC scan results did not influence the deemed lack of need for a rest SPECT-MPI with normal SPECT-MPI or the necessity of rest SPECT-MPI with abnormal SPECT-MPI. However, the CAC scan reduced the deemed need for a rest SPECT-MPI in 72% with a probably normal, 47% with an equivocal, and 40% of those with a probably abnormal SPECT-MPI.
Conclusions
Our exploratory analysis indicates that addition of a CAC scan to stress SPECT-MPI tends to diminish experienced readers’ deemed need to perform rest SPECT-MPI studies among patients with probably normal or borderline stress-only SPECT-MPI studies. Thus, further study appears warranted to assess the utility of using CAC scanning as a means for increasing the percent of SPECT-MPI studies that can be performed as stress-only studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress single-photon emission-computed tomography (SPECT) myocardial perfusion imaging (MPI) is most commonly performed as a rest/stress sequence, requiring two sets of images on the same day or over 2 days in selected patients. In recent years, increasing emphasis has been placed on using a stress-only SPECT-MPI protocol in selected diagnostic patients. Patients with a normal stress-only MPI have a comparable risk vs those patients with a normal rest/stress SPECT-MPI.1-3 However, wide adoption of a stress-only protocol has been limited for several reasons including its application to primarily low likelihood cohorts, the requirement to have a completely normal study in order to obviate a resting study,4 and the reliance on either attenuation correction software5 or supine-prone imaging6 to reduce the percentage of patients needing resting studies. A significant advantage would be accrued if we were able to broaden the adaptation of a stress-only SPECT-MPI protocol, as this protocol reduces testing time and can be performed with lower radiation exposure to patients.
Potentially combining the stress-only SPECT-MPI study with a coronary artery calcium (CAC) scan could represent a new approach for reducing the need for resting SPECT-MPI images in a larger percentage of patients. A normal CAC scan could increase reader confidence concerning the interpretation of minimal scan abnormalities, whereas in the face of an abnormal CAC scan, concern as to the significance of minimal defects might also be reduced, given that the diagnosis of coronary artery disease (CAD) would be apparent from the CAC scan. Currently, however, there are no guidelines to inform us as to how to combine a stress-only SPECT-MPI study and CAC scan together. Accordingly, we performed an exploratory analysis to determine the frequency with which the deemed need for a rest SPECT-MPI study was reduced by adding the results of a CAC scan to the interpretation of a stress-only SPECT-MPI study.
Methods
An add-on CAC scan is performed among diagnostic patients referred for SPECT-MPI at our institution at the discretion of referring physicians at no added charge. This study included 162 randomly selected patients (46 ± 26 years, 44% males) who underwent a rest/stress SPECT-MPI study and add-on CAC scan on the same day. Clinical and demographic data including age, gender, race, height, weight, presence of CAD risk factors, medications, and the presence and type of chest pain were collected prior to stress testing. This study was approved by the Institutional Review Board of St. Luke’s-Roosevelt Hospitals.
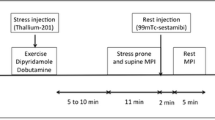
Rest-Stress 99mTc-Sestamibi Imaging
All patients underwent rest/stress SPECT-MPI with 99mTc-sestamibi. Patients were asked to withhold beta-blocker 24 hour prior to testing. All SPECT studies were acquired on a commercially available camera and computer using a 180° arc, high-resolution parallel-hole collimator; and 64 stops with 20 seconds per stop for a total imaging time of 25 minutes. For resting studies, patents were injected with 5-7mCi of 99mTc-sestamibi and SPECT-MPI were acquired 30-45 minutes after resting injection. All images were acquired using a 64 × 64 image matrix. Patients who were able to exercise underwent symptom limited treadmill exercise testing using the Bruce protocol and continuous 12-lead ECG monitoring. At peak heart rate (85% maximal predicted heart rate), 12-15mCi of 99mTc-sestamibi (dose was weight based) was injected. For patients who were unable to exercise, stress was performed using 140 mg/kg dipyridamole injection over 4 minutes or regadenoson 0.4 mg injection over 20 seconds followed by injection of 12-15mCi of 99mTc-sestamibi (dose was weight based) injected at 7 minutes. All patients then underwent post-stress SPECT image acquisition that included post-stress gated images to assess left ventricular function. SPECT-MPI studies were reconstructed using wide beam reconstruction (UltraSPECT Inc., Auburndale, MA, USA). Gated SPECT images were acquired eight frames per cardiac cycle. Two sets of SPECT-MPI were processed in each patient: a stress-only image set and a standard rest stress image set.
CAC Scans
All CAC scans were performed on a commercially available CT scanner (Siemens Somatoform Sensation 64-detector, Siemens Medical Solutions USA, Malvern, PA, USA). Each patient’s CAC scan consisted of 40 to 60 slices of 3.0-mm slice thickness, with ECG-triggering and acquisition at 65% of the cardiac cycle. Foci of CAC were identified by an experienced radiologist and scored using semi-automatic commercial software (Vitrea, Vital Images, Toshiba Medical Systems, Minnetonka, MN, USA).
SPECT-MPI Interpretation
Two experienced readers interpreted each SPECT-MPI study in a consensus manner. Each SPECT-MPI study was interpreted as a stress SPECT only study with the reader blinded to the resting SPECT-MPI study (as described below) and as clinical rest/stress SPECT-MPI study. All SPECT-MPI images were interpreted as either normal, probably normal, equivocal, probably abnormal, and abnormal based on semi-quantitative visual assessment using the 5-point scale as recommended by the ASNC.7 In general, normal = SSS of 0, probably normal was a SSS 1 or 2 with each myocardial segment having a score of 0 or 1, equivocal was a SSS of 3-4 with each myocardial segment having a score of 0 or 1, and probably abnormal a SSS 3-4 with only one segment with a score >1, definitely abnormal had a SSS >4. The gated SPECT images were interpreted as normal wall motion, regional wall motion abnormalities, or global hypokinesis.
In order to determine the effect of the CAC score on the need for a rest SPECT-MPI study and clinical management of the patient, the readers interpreted the stress SPECT-MPI images only. Subsequent to interpreting the stress-only images, the blinded readers were asked to assess the need for a rest study for a definitive interpretation of the SPECT study in the following sequence: (1) after interpreting the stress SPECT-MPI only; (2) after addition of the clinical and stress ECG data in addition to the stress SPECT-MPI, and (3) after the further addition of the CAC score. In addition, each SPECT-MPI study was blindly interpreted in the standard rest/stress SPECT-MPI format on a separate occasion at least 1 month apart from the stress-only SPECT-MPI readings.
Statistical Analysis
All continuous variables are expressed as means ± SD and categorical variables are presented as number and percentage. All statistical analysis was performed using SPSS version 16 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA).
Results
Baseline clinical characteristics are listed in Table 1. The population was relatively young but included patients with a high concentration of CAD risk factors, including hypertension in nearly four-fifths of patients and diabetes in 45% of patients. Over half of patients were obese (BMI ≥30 kg/m2). There was a wide distribution of chest pain symptoms. Nearly three-fifths of our patients required pharmacological stress testing. The CAC scores were widely distributed, with 38% having a zero CAC score and 19% having CAC scores >400.
With initial blinded interpretation of the stress SPECT-MPI only, 62 (38%) of the stress SPECT-MPI only studies were considered normal, 43 (27%) were considered probably normal, 15 (9%) were considered equivocal, 5 (3%) were considered probably abnormal, and 37 (23%) were considered definitely abnormal. Among the studies considered normal, a rest SPECT-MPI study was deemed unnecessary in all 62 patients and this did not change with the addition of the clinical data, stress ECG results, or the CAC scan (Table 2). Among the definitely abnormal stress-only SPECT-MPI studies, a rest SPECT-MPI study was deemed necessary and this did not change with the addition of the clinical data, stress ECG results, or the CAC score. Among the stress-only studies considered within a borderline range—i.e., as having probably normal, equivocal, or probably abnormal (n = 63) studies—a rest study was deemed necessary in 58 (92%) patients. The addition of the clinical data and ECG results had virtually no impact on the need for a rest SPECT-MPI study in this borderline group of patients (reduced from 58 to only 57 patients). However, the addition of the CAC score decreased the deemed need for a rest study by 64% (from 57 to 22 patients) within the borderline group.
Impact on Interpretation According to Presence or Absence of CAC Abnormality and the CAC Score
Table 3 subdivides the deemed need to perform a rest SPECT-MPI study according to whether the CAC scan was normal (score = 0) or abnormal (score >0) in the patients with probably normal, equivocal, or probably abnormal SPECT-MPI studies. (As aforementioned, the CAC scan results did not influence the deemed need for a rest SPECT-MPI study in patients with definitely normal or definitely abnormal studies). Overall, within these three SPECT-MPI interpretation groups, the need for a rest SPECT-MPI study was reduced by 57% of the patients if the CAC score was 0, but also by 64% of the patients if the CAC scan was abnormal.
Figure 1 further analyzes the relationship between SPECT-MPI abnormality, CAC abnormality, and physician determination for the need for a rest SPECT-MPI study according to patients summed stress score. For those with a SSS score of 1-3, a rest SPECT-MPI study was deemed necessary in relatively few patients given the knowledge of patients’ CAC score. The deemed need for a rest SPECT-MPI study was low regardless of whether CAC abnormality was present or absent. In the presence of a SSS of 4-7, a rest SPECT-MPI was more likely to be deemed necessary if the CAC study was abnormal.
Table 4 shows the impact of the CAC score on the deemed need for a rest SPECT-MPI study among patients with a probably normal, equivocal, and probably abnormal stress-only SPECT-MPI studies. Among the patients with CAC abnormality, there was a decreasing tendency to forego a rest SPECT-MPI study with increasing CAC abnormality. This was more marked among the patients with CAC scores ≥400.
Comparison of Findings to the Rest/Stress SPECT MPI Interpretation
Table 4 shows the independent interpretation of the stress-only SPECT-MPI vs the rest/stress SPECT-MPI, further stratified according to the presence or absence of CAC abnormality. Among the patients who had either a normal or probably normal SPECT-MPI study (n = 105), a two grade interpretation change toward abnormality (e.g., going from a normal to an equivocal study or probably normal to probably abnormal study) on rest SPECT-MPI was only observed in 3 (3%) patients, all of which had the presence of CAC. By contrast, among the 37 patients with abnormal scans, 12 (32%) had a two grade change toward a normal/equivocal interpretation on combined rest/stress SPECT-MPI. Among these 12 patients, the rest/stress defects were all fixed defects, with normal wall motion in nine and abnormal wall motion in three.
Figures 2 and 3 show representative examples of patients in whom a rest SPECT-MPI study was deemed unnecessary after considering the combination of the stress-only SPECT-MPI study and CAC scan results.
A 55-year-old female with hypertension and dyslipidemia who presented with atypical chest pain. Perfusion images reveal an equivocal anterior wall defect. Gated SPECT images demonstrated normal wall motion and ejection fraction. Based on the stress-only SPECT-MPI alone, a rest SPECT study was deemed necessary. After considering that the patient’s CAC score was zero, a resting SPECT-MPI study was deemed unnecessary. MPI, Myocardial perfusion imaging; SPECT, single-photon emission-computed tomography
A 66-year-old female with diabetes who presented with atypical chest pain. (Left panel) Stress-only perfusion images revealed a mild inferior wall defect. The gated SPECT images demonstrated normal wall motion and ejection fraction. Based on the stress-only SPECT-MPI, a rest SPECT-MPI study was deemed necessary. After considering the CAC score of 146 (right panel), a rest SPECT-MPI study was deemed unnecessary. MPI, Myocardial perfusion imaging; SPECT, Single-photon emission-computed tomography
Discussion
A stress-only SPECT MPI study has been advocated for patients with a relatively low intermediate likelihood of CAD, with careful attention to measures designed to reduce the frequency of mild abnormalities, such as the use of attenuation correction, combining supine and prone imaging, and the combined reliance on visual and quantitative analysis of myocardial scintigrams. In this study, we assessed whether combining a stress-only SPECT-MPI study with a CAC scan could serve as a new means to further decrease the deemed need for rest SPECT-MPI. Of note, our study was exploratory, with no specific guidelines. Rather, we sought to determine what patterns of stress-only SPECT-MPI and CAC findings might serve to reduce the frequency of rest SPECT-MPI in the estimation of experienced nuclear readers.
A number of interpretative patterns were evident from our data. When considering the stress-only SPECT-MPI studies, without knowledge of the clinical history or CAC result, a rest SPECT-MPI study was deemed unnecessary in all 62 patients with a definitely normal stress-only SPECT-MPI study. By contrast, 88% of the probably normal scan patients and all patients with an equivocal or abnormal stress-only scan were deemed to need a resting scan before the consideration of any clinical data. The addition of the clinical history had virtually no impact on this ascertainment. When the CAC scan result was also considered, three interpretative patterns emerged. Among those with normal stress-only SPECT-MPI, none were considered as candidates for a rest SPECT-MPI study based on the CAC score. Similarly, the consideration of the CAC scan had no impact upon those patients who had a definitely abnormal stress-only SPECT-MPI. All these patients were still considered to need a rest SPECT-MPI study despite knowledge of their CAC score. By contrast, the CAC scan results had a large impact upon the deemed need for rest SPECT-MPI study among the patients with mild perfusion abnormalities, including the patients with a probably normal, equivocal, or probably abnormal scans. Specifically, nearly three quarters of the patients with a probably normal scan, nearly one half of patients with an equivocal scan, and 40% of the patients with a probably abnormal scan based on the stress-only SPECT-MPI study were not considered to need a rest SPECT-MPI study following the consideration of the CAC score in these patients.
We further assessed how the presence or absence of CAC abnormality influenced the decision to perform a rest SPECT-MPI study among the patients with a probably normal, equivocal, or probably abnormal scans. Both when the CAC score was 0 and when it was >0, there was a similarly large reduction in the deemed need for rest SPECT-MPI study in this subgroup of patients: by 70% if the CAC score was normal and by 64% if the CAC score was abnormal.
There are a number of potential mechanisms by which a normal and abnormal CAC scan could serve to reduce the need for a rest SPECT-MPI study. The presence of a normal CAC scan could serve to increase reader confidence in interpreting minor scan abnormalities as normal. When the CAC score is zero, the likelihood of having non-calcified plaque is reduced to only ~10%,8 the likelihood of angiographically significant coronary stenosis (>50%) stenosis becomes rare,9 the 10 year event rate for CAD events falls to approximately 0.1% per year,10 and the frequency of inducible myocardial ischemia is rare.11,12 For these reasons, readers are more likely to interpret subtle findings as normal variants in the presence of a normal CAC scan. An abnormal CAC scan could serve to decrease the need for a rest SPECT-MPI study through a couple of potential mechanism. First, in the presence of only a very low CAC score, readers may also be inclined to read minor SPECT-MPI findings as normal variants, given the very low frequency of inducible myocardial ischemia when CAC scores are only mildly elevated (e.g., in the range of 1-99). Second, since the presence of CAC is very specific for diagnosing the presence of CAD, when such abnormality is present, it may no longer be crucial to distinguish between a normal and probably normal or equivocal SPECT-MPI study for diagnostic purposes. The CAC scan has served in such cases to establish the presence of CAD. Rather, in such cases, the SPECT-MPI study could be viewed as converting into a prognostic study, where the deciding issue relative to outcomes is the degree of inducible myocardial ischemia. Since very minor SPECT-MPI abnormalities in the presence of CAD do not substantially elevate patient risk to the point of considering a myocardial revascularization procedure,13 it may be that the added performance of a rest SPECT-MPI study would not change medical management once a CAC scan has established that CAD is present and the SPECT-MPI study has established no major defect is present. Furthermore, we found that there was a decreasing tendency to forego a rest SPECT-MPI study with increasing CAC abnormality. This was more marked among the patients with CAC scores >400. One possible reason that a CAC score ≥400 resulted in little decrease in the perceived need for a rest SPECT is likely based on the literature showing a significant increase in ischemia among patients with a CAC ≥400.11
Comparison of Stress-Only and Stress-Rest SPECT-MPI in Patients with Normal and Abnormal CAC Studies
Among the patients with normal or probably normal stress-only SPECT-MPI studies, the rest SPECT-MPI were concordantly normal or probably normal in 91% of the patients on rest SPECT-MPI. By contrast, over one-third of patients with definitely abnormal SPECT-MPI studies were re-classified as either an equivocal or normal/probably normal study after consideration of the rest SPECT-MPI study. This difference is logical. In the presence of a definite defect on stress-only SPECT-MPI, the interpreter has no way of knowing whether the defect will reverse or not on rest SPECT-MPI. The gated SPECT images are not helpful in that case either, because normal wall motion will not differentiate between ischemia or a fixed defect that is present as an attenuation artifact. In fact, in all 12 patients with definite defects which were reclassified as normal/equivocal after the consideration of the rest/stress SPECT-MPI that identified these fixed defects as primarily due to attenuation (fixed defects with normal wall motion). As all patients with definite defects were deemed as needing rest SPECT-MPI studies, regardless of the CAC score, on a practical basis the CAC scan would not have led to a missed identification of ischemia in our patient population based on our exploratory analysis.
Comparison to the Literature
Both interest in performing stress-only imaging and combining SPECT-MPI with a CAC scan have been increasing. Studies demonstrate that a definitely normal stress-only SPECT-MPI study conveys a low short-term risk for cardiac events, comparable to that seen with a normal rest/stress SPECT-MPI study.3 As shown by Chang et al,3 the addition of a CAC scan adds prognostic information to the results of SPECT-MPI, with high CAC scores increasing risk both among patients with normal and abnormal scan SPECT-MPI. Of note, CAC abnormality is highly common among patients with a normal SPECT-MPI studies, occurring in 84% of the patients with a normal SPECT-MPI study in a large series that was reported by Berman et al.11 To date, however, there has been little study regarding how a CAC scan might influence the actual interpretation of SPECT-MPI studies. In one recent study, Mouden et al14 performed an interpretation of rest/stress SPECT-MPI before and after knowledge of concomitant CAC scan results. They found that the overall interpretation changed in 37% of 151 patients, including a reduction in equivocal interpretations (from 21% to 9%). Our exploratory analysis is the first to assess how a CAC scan might aid the interpretation of stress-only SPECT-MPI studies.
Limitations
Our study contains a number of important limitations. Our patient population was relatively small, thus not permitting potentially important sub-analyses. For instance, after dividing patients both by interpretative scan category and presence or absence of CAC abnormality, there were not sufficient patients to further analyze our results according to the degree of CAC abnormality. Second, we did not have the option of applying attenuation correction to our data, which has been a standard in most studies that have assessed the utility of stress-only SPECT-MPI studies. Still, only a minority of nuclear labs, in fact, have been applying attenuation correction to SPECT-MPI.15 Thus, our findings are likely to be relevant to the experience of many current Nuclear Cardiology laboratories. Similarly, we did not apply quantitative analysis to our SPECT-MPI images or supine-prone imaging which can also reduce the frequency of scan abnormalities.16 In retrospect, within our exploratory analysis, we did not collect the reasons as to why our experienced readers deemed a rest SPECT-MPI study not to be necessary according to CAC findings. Such analysis would be important in further study, to gather a consensus understanding as to how a CAC scan increases reader confidence and influences decision-making following a stress-only SPECT-MPI study. Furthermore, given the small sample size of this study, we must be cautious in drawing conclusions regarding how the degree of CAC abnormality influenced readers deemed need to for a rest study.
Clinical Implications
Two principle limitations of rest/stress SPECT-MPI are that the test is relatively inconvenient, taking up to nearly one half of a patient’s day (3-4 hours), and that the test cannot detect sub-clinical atherosclerosis. Furthermore, rest/stress SPECT-MPI protocols expose patients to higher amounts of radiation than does stress SPECT only protocols. Given recent improvements in hardware and software, wide use of stress SPECT-MPI only protocols could result in significant decreases in radiation exposure to a large population of patients. In our study, all patients underwent a rest/stress protocol using dose reduction strategies (wide beam reconstruction) exposing patients to an average of ~8 mSv of radiation. If, one was to combine the radiation exposure of a CAC scan (~1 mSv) with a stress SPECT-MPI study on a conventional camera using software improvements, a significant reduction in radiation exposure would result. In our study, the total radiation exposure to 162 patients was ~1,944 mSv. Our interpreters felt that the addition of the CAC scan made the rest study unnecessary in 104 patients. Assuming a low dose stress (~3 mSv) protocol is used, we would see a 40% reduction in radiation exposure [(104 stress-only × 3 mSv) + (58 stress/rest × 12mSv) + (162 CAC scans × 1mSV) = 1,171 mSv].
Pending further prospective study, our findings suggest that the combination of stress-only SPECT-MPI and a CAC scan could help to substantially widen the spectrum of patients in which a stress-only SPECT-MPI study could be performed. Concomitant analysis of CAC in such patients could increase the potential diagnostic and prognostic information provided by SPECT-MPI. Our analysis suggests that the greatest benefit might be derived among those patients who have probably normal and equivocal stress-only SPECT-MPI studies. This potential benefit may have assumed more importance in our era, where there has been a marked temporal decline in the frequency of abnormal SPECT-MPI studies,12 but with a high residual frequency of underlying atherosclerosis, often of a significant degree, as identified by CAC scanning, in those patients who have normal SPECT-MPI studies.3,11,17 Thus, more prospective study appears indicated to evaluate the clinical utility of a combined stress-only SPECT-MPI and CAC scan for the work-up of patients with suspected CAD.
New Knowledge Gained
The addition of a CAC scan to a stress-only SPECT-MPI has the potential for the expansion of stress-only SPECT-MPI protocols to patients with significant CAD risk factor burden, undergoing pharmacologic stress studies, and who are overweight. These findings can have significant implication for patient radiation exposure and cost.
References
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol 2002;39:999-1004.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221-30.
Mahmarian JJ. Stress only myocardial perfusion imaging: Is it time for a change? J Nucl Cardiol 2010;17:529-35.
Heller GV, Bateman TM, Johnson LL, Cullom SJ, Case JA, Galt JR, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol 2004;11:273-81.
Des Prez RD, Dahlberg ST, Einstein AJ, Grossman GB, Henzlova MJ, Mahenthiran J, et al. Stress-only myocardial perfusion imaging. J Nucl Cardiol 2009;16:255-76.
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol 2010;17:941-73.
Uretsky S, Rozanski A, Singh P, Supariwala A, Atluri P, Bangalore S, et al. The presence, characterization and prognosis of coronary plaques among patients with zero coronary calcium scores. Int J Cardiovasc Imaging 2011;27:805-12.
Villines TC, Hulten EA, Shaw LJ, Goyal M, Dunning A, Achenbach S, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: Results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol 2011;58:2533-40.
Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA, Kondos GT, et al. Cardiovascular events with absent or minimal coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J 2009;158:554-61.
Berman DS, Wong ND, Gransar H, Miranda-Peats R, Dahlbeck J, Hayes SW, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol 2004;44:923-30.
Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE, et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 2013;61:1054-65.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900-7.
Mouden M, Ottervanger JP, Timmer JR, Reiffers S, Oostdijk AH, Knollema S, et al. The influence of coronary calcium score on the interpretation of myocardial perfusion imaging. J Nucl Cardiol 2014;21:368-74.
Germano G, Slomka PJ, Berman DS. Attenuation correction in cardiac SPECT: The boy who cried wolf? J Nucl Cardiol 2007;14:25-35.
Hayes SW, De Lorenzo A, Hachamovitch R, Dhar SC, Hsu P, Cohen I, et al. Prognostic implications of combined prone and supine acquisitions in patients with equivocal or abnormal supine myocardial perfusion SPECT. J Nucl Med 2003;44:1633-40.
Bybee KA, Lee J, Markiewicz R, Longmore R, McGhie AI, O’Keefe JH, et al. Diagnostic and clinical benefit of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial perfusion stress imaging. J Nucl Cardiol 2010;17:188-96.
Disclosure
The authors have no relevant financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uretsky, S., Cohen, R., Argulian, E. et al. Combining stress-only myocardial perfusion imaging with coronary calcium scanning as a new paradigm for initial patient work-up: An exploratory analysis. J. Nucl. Cardiol. 22, 89–97 (2015). https://doi.org/10.1007/s12350-014-9958-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-9958-5