Abstract
Purpose
High coronary artery calcium (CAC) scores are associated with a high likelihood of ischaemia and obstructive coronary disease. Myocardial perfusion imaging (MPI) is a key investigation to determine the need for revascularization. However, the value of MPI in presence of extensive CAC has so far only been demonstrated in asymptomatic patients, whereas its value in symptomatic patients remains largely unclear. Therefore, we studied the impact of MPI in symptomatic patients with a CAC score ≥1,000.
Methods
We included 282 patients (mean age 69 ± 9 years, 63 % men) without a history of coronary disease with suspected stable angina referred for MPI and with a CAC score ≥1,000. On follow-up at 18 months invasive angiography, coronary revascularization, nonfatal myocardial infarction and death were recorded.
Results
MPI was normal in 54 %, equivocal in 10 % and abnormal in 37 % (fixed defect 9 % and ischaemia 28 %) of patients. More abnormal MPI findings were observed in men, smokers and those with even higher CAC scores. During follow-up, 1 patient (with nonischaemic MPI) died from a cardiac cause, 1 patient (with ischaemic MPI) suffered a myocardial infarction and 92 patients (33 %) underwent revascularization. Ischaemia on MPI was a strong predictor of coronary revascularization (odds ratio 13.1; 95 % CI 7.1–24.3; p < 0.001).
Conclusion
Ischaemia on MPI is observed in approximately 30 % of patients with a CAC score ≥1,000, and is a strong predictor of coronary revascularization. However, nonischaemic MPI does not exclude revascularization, and patients with persisting complaints should be considered for invasive angiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion imaging (MPI) using single photon emission computed tomography (SPECT) provides valuable diagnostic and prognostic information in patients referred for noninvasive detection of myocardial ischaemia [1, 2]. However the presence or absence of atherosclerosis remains undetected. Furthermore, the diagnostic accuracy of MPI may be impaired in patients with balanced ischaemia due to flow-limiting three-vessel coronary artery disease (CAD) or left main stenosis [3], while this group is particularly prone to adverse cardiac events [4, 5].
Coronary artery calcium (CAC) scoring is a clinical tool for the early noninvasive detection of coronary atherosclerosis [6, 7]. Higher CAC scores are generally associated with more advanced coronary sclerosis and a higher likelihood of ischaemia [8, 9] or stenotic lesions [10]. Nevertheless, according to several studies, the presence of extreme CAC scores is accompanied by a normal MPI in the majority of both asymptomatic and symptomatic patients [11, 12]. Recent studies indicate that patients with normal MPI but with high CAC scores are at increased risk of future coronary events as compared to patients with no CAC. Such patients may have obstructive CAD despite normal MPI results [9, 13, 14]. With the recent advent of hybrid SPECT/CT devices, MPI and CAC scoring can be easily combined and performed in a single session. However, the value of MPI in symptomatic patients with a very high CAC score and the resulting implications for treatment and short-term prognosis remain largely unclear.
Therefore, the aims of this study were to assess the impact of MPI patients with a low/intermediate risk of a coronary event with suspected but unconfirmed CAD who subsequently presented with a high CAC score (≥1,000) and to evaluate the resulting clinical and prognostic implications.
Materials and methods
Study population
We retrospectively evaluated all patients who presented to our hospital over a 3-year period (January 2009 to December 2011) for a clinically indicated MPI with a hybrid 64-slice SPECT/CT device. Only patients without a previous history of CAD, and a low to intermediate pretest likelihood of CAD with a very high CAC score (≥ 1,000) were included in the current analysis. All procedures were performed in accordance with the Declaration of Helsinki. The study was approved by the Committee on Research Ethics of our hospital, and written informed consent was obtained from all patients.
Clinical information
At the time of examination, all patients completed a questionnaire regarding demographic information, prior medical history, cardiac risk factors and current medication use. These data were verified and complemented with demographic and clinical information collected from medical records. Furthermore, information regarding patient age, gender, weight, height, blood pressure, heart rate and symptoms were prospectively obtained by a medical nurse. The pretest likelihood of CAD was assigned according to the criteria of Diamond and Forrester, with a risk threshold of <13.4 % for low risk, between 13.4 and 87.2 % for intermediate risk, and >87.2 % for high risk [15].
SPECT MPI data acquisition
All patients underwent a 1-day 99mTc-tetrofosmin MPI protocol. Patients were instructed to refrain from caffeine-containing beverages for at least 24 h before the test. Pharmacological stress was induced by intravenous administration of adenosine (continuous infusion at a rate of 140 μg/kg/min for 6 min). In patients with a contraindication for adenosine, stress was induced using dobutamine (starting with 10 μg/kg/min and increased at 3-min intervals to a maximum of 50 μg/kg/min until 85 % of the predicted heart rate had been reached). Whenever possible, patients performed additional low-level bicycle exercise to reduce the side effects of adenosine. ECG and blood pressure were monitored before, throughout, and following the infusion. A weight-adjusted dose of 99mTc-tetrofosmin (standard 370 MBq, 500 MBq in patients >100 kg) was injected after 3 min of adenosine infusion. Patients scheduled for rest imaging received a dose of 99mTc-tetrofosmin (standard 740 MBq, 1,000 MBq in patients >100 kg). Both stress and rest SPECT images were acquired 45–60 min after tracer injection. Patients were scanned with a hybrid 64-slice SPECT/CT device that included a conventional gamma camera (before 1 May 2010, 85 patients) or a cadmium-zinc-telluride (CZT) gamma camera (after 1 May 2010, 197 patients).
With the conventional dual-detector gamma camera (Ventri; GE Healthcare), images were acquired using a low-energy, high-resolution collimator, a 20 % symmetrical window at 140 keV, a 64 × 64 matrix, and an elliptical orbit with step-and-shoot acquisition at 6º intervals over a 180º arc (45º anterior oblique to 45º left posterior oblique) with 30 steps (30 views). All patients were imaged in the supine position with arms placed above the head. Acquisition time was 12 min for the stress images and 15 min for the rest images.
The CZT-based SPECT images were acquired using a multipinhole camera (Discovery NM/CT 570c; GE Healthcare) and 19 stationary detectors simultaneously imaging the heart. Each detector contained 32 × 32 pixelated (2.46 × 2.46 mm) CZT elements. A 20 % symmetrical energy window at 140 keV was used as previously described [16]. All patients were imaged in the supine position with arms placed above the head. The acquisition time was 5 min for the stress images and 4 min for the rest images as previously reported [16]. Gated SPECT analysis to calculate left ventricular volumes and ejection fraction, and to assess wall motion abnormalities was done in nearly all patients when feasible, usually during stress but in some cases during rest. Stress and rest SPECT studies were followed by an unenhanced low-dose CT scan during breath-hold to provide the attenuation map for attenuation correction. These scans covered the entire chest with the following scanning parameters: 5.0-mm slice thickness using a reconstruction algorithm with a 512 × 512 matrix, and 800 ms rotation times at 120 kV and 20 mA. Emission images as well as attenuation map data were entered into a dedicated reconstruction algorithm to provide 3-D volume data (available in a Xeleris workstation; GE Healthcare). These were reorientated in the standard way and displayed in the three traditional cardiac axes.
SPECT MPI analysis
Experienced nuclear cardiac readers (each with more than 10 years experience) nonblindly interpreted the images including MPI polar maps. Segments were scored by consensus of two readers using a 20-segment model for the left ventricle using the following five-point scoring system: 0 normal, 1 equivocal, 2 moderate reduction in radiotracer uptake, 3 severe reduction in radiotracer uptake, 4 no detectable tracer in a segment [17, 18].
Perfusion defects were identified on the stress images (a segment with a score ≥2 was considered to have a defect). A stress study was interpreted as normal if perfusion was assessed to be homogeneous throughout the myocardium and fewer than two segments had a stress score ≥2 [17–19]. Subsequent rest imaging was performed if the stress images did not fulfil these criteria and were therefore deemed to be either abnormal or equivocal. A reversible perfusion defect was defined as one in which a stress defect was associated with a rest score ≤1 or a stress defect score of 4 with a rest score of 2 [17, 18]. Irreversible defects were considered scar tissue when persistent despite applying CT-based attenuation correction together with abnormal wall motions in the corresponding segments [20].
Unenhanced CAC scan acquisition
All cardiac CT studies were acquired in a single session immediately after MPI using the 64-slice CT scanner of the integrated SPECT/CT device (LightSpeed VCT XT; GE Healthcare). All patients with a heart rate >70 beats/minute received oral beta-blocker therapy (50 or 100 mg metoprolol; Astra Zeneca BV, Zoetermeer, The Netherlands) prior to the CAC scan. For the CAC scans an unenhanced ECG-gated scan was performed prospectively triggered at 75 % of the RR interval using the following scan parameters: 4 × 2.5 mm, gantry rotation time 330 ms, tube voltage 120 kV, and a tube current ranging from 125 to 250 mA depending on patient size. Postprocessing of the CAC scan was performed on dedicated workstations (Advantage Windows 4.4; GE Healthcare).
Unenhanced CAC scan interpretation
The computer software for CAC scoring (Smart Score; GE Healthcare) automatically defined the presence of calcified lesions as those with radiodensity greater than 130 HU. The total calcium burden in the coronary arteries was manually depicted and allocated to the corresponding coronary artery by an experienced reader using the Agatston method for quantification of CAC [21].
Clinical follow-up
Clinical outcome data were obtained by reviewing hospital records, by telephone interviews with the patients and by contacting the patients’ general practitioners. The time between the examination date and the date of the final consultation was used to determine follow-up length. Events that were recorded during follow-up were diagnostic invasive coronary angiography (ICA), coronary revascularization, nonfatal myocardial infarction and death.
Statistical analysis
Statistical analysis to compare baseline characteristics was performed with Chi-Square and one-way analysis of variance (ANOVA) as available in SPSS software (version 18.0 for Windows; SPSS Inc., Chicago, IL). Continuous data were compared between groups using the two-sided Student’s t test. Quantitative variables are expressed as means ± SD and categorical variables as frequencies, or percentages. P values less than 0.05 were considered statistically significant.
Results
Baseline characteristics
The baseline characteristics of the patients are shown in Table 1. The mean age of the entire cohort of 282 patients was 69 ± 9 years, 63 % were men and their mean body mass index was 28 ± 5 kg/m2. In 269 patients (95 %) pharmacological stress was induced with adenosine and in 13 patients (5 %) with dobutamine. The mean CAC score for the entire cohort was 1,857 ± 862 (median 1,586, interquartile range 1,235–2,169). The mean CAC score in patients ≥70 years of age (1,959 ± 898) was higher than that in patients <70 years (1,754 ± 814, p = 0.046).
SPECT results
SPECT revealed normal perfusion in 151 patients (54 %). Stress-only imaging was performed in 73 patients (26 %) with unequivocally normal stress SPECT findings. Additional rest SPECT imaging was performed in 209 patients (74 %). The mean left ventricle ejection fraction was 62 ± 12 %. Equivocal findings were found in 27 patients (10 %), while abnormal perfusion was found in 104 patients (37 %), of whom 26 (9 %) showed fixed defects and 78 (28 %) had findings suggestive of ischaemia. Patients with abnormal findings were more likely to be men, to be a current smoker and to have an even higher CAC score (Table 2). Patients who underwent scanning with the CZT camera had fewer equivocal SPECT findings (6 % vs. 18 %, p = 0.002) and more often underwent stress-only imaging (30 % vs. 16 %, p = 0.0018).
Referral for cardiac catheterization, revascularization rates, and cardiac events
Follow-up examinations were performed in 281 patients (99 %). The minimal follow-up time was 1 year, with a mean of 24 ± 11 months (median 23 months, interquartile range 16–31 months). Overall, 132 patients (47 %) underwent ICA during follow-up, of whom 93 (33 %) were referred for early (<60 days) ICA and 39 (14 %) for late (≥60 days) ICA. ICA was chosen more commonly in patients with ischaemic SPECT findings (86 %) than in those with nonischaemic SPECT findings (32 %, p < 0.001).
Of the 204 patients with nonischaemic SPECT findings, 65 (32 %) underwent ICA because of persisting complaints, of whom 39 (19 %) were early and 26 (13 %) late referrals. Of these 65 patients, 22 had nonsignificant CAD and 43 had obstructive CAD (defined as ≥70 % luminal narrowing in a major coronary vessel, ≥50 % stenosis in the left main coronary artery or fractional flow reserve value ≤0.80). Subsequent revascularization was performed in 35 patients. Single-vessel disease was found in 16 patients, two-vessel disease in 9 and three-vessel disease in 18. Left main stem stenosis was found in two patients. Among the 78 patients with ischaemic SPECT findings, 67 (86 %) were referred for ICA, of whom 54 (69 %) underwent early and 13 (17 %) late ICA. Of these patients who underwent ICA, obstructive CAD was confirmed in 60, of whom 57 underwent revascularization. Single-vessel disease was found in 15 patients, two-vessel disease in 13 and three-vessel disease in 31. Isolated left main stem stenosis was found in one other patient, while four patients had concurrent left main involvement. Ischaemia on MPI was a very strong predictor of coronary revascularization (odds ratio 13.1, 95 % CI 7.1–24.3; p <0.001) during follow-up.
In patients with confirmed obstructive CAD the revascularization rate was higher in the group with ischaemia (95 % vs. 81 %, p = 0.048). After excluding early revascularizations, there were 13 late revascularizations in the cohort with nonischaemic SPECT findings and 10 late revascularizations in those with ischaemic SPECT findings (p = 0.077). One patient without ischaemia on MPI died of acute myocardial infarction, while one patient with ischaemia on MPI suffered an acute myocardial infarction requiring primary percutaneous intervention. Six patients died from a noncardiac cause. Analysis of event-free survival is shown in Fig. 1.
Discussion
In this single-centre observational study in symptomatic stable patients with suspected CAD and a very high CAC score, myocardial perfusion was normal in more than 50 % of the patients. Of the 32 % of patients with nonischaemic MPI who were referred for ICA, 54 % underwent subsequent revascularization. The proportion of downstream invasive testing and revascularization following a nonischaemic MPI study in this highly selected cohort was higher than in a similar population with lower CAC scores [16], again confirming the value of CAC scoring combined with MPI. Now the question is what should be the strategy in patients with normal myocardial perfusion but very high CAC score.
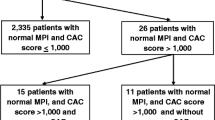
The relationship between MPI and CAC has been studied, but most of the previous studies focused mainly on asymptomatic cohorts and included only a few patients with CAC scores ≥ 1,000. In four studies that included predominantly asymptomatic subjects, the probability of myocardial ischaemia increased with higher CAC scores, but as in our study, the majority of those with a high CAC score had normal perfusion [8, 22–24]. A lower frequency (29 %) of normal MPI results among 28 asymptomatic diabetic subjects with CAC scores ≥ 1,000 was observed, probably indicating the higher-risk profile in that cohort [25]. In three large studies that included symptomatic patients, the MPI findings were normal in the majority of the patients with CAC scores ≥ 1,000 (Fig. 2) [9, 11, 12]. Summarizing all studies, the majority of patients without prior CAD but a high CAC score have normal MPI, with a higher prevalence of abnormal MPI in symptomatic patients and high-risk groups.
Several studies have assessed the prognostic value of CAC scoring over MPI alone. Patients with both a high CAC score and high-risk MPI findings show higher mortality rates than patients with only a high CAC score [24]. Similar higher long-term event rates have been found among asymptomatic individuals with normal SPECT and more extensive atherosclerosis. With regard to the short term, higher-risk patients with a CAC score ≥ 1,000 suffer more adverse events [9, 25]. Conversely, as in our study, patients with a low/intermediate risk have a low annual severe short-term event rate even in the presence of elevated CAC scores [12, 23, 24]. Time-point analysis indeed showed an initially low annual event rate in subjects with normal SPECT and a severe CAC score with separation of the survival curves for total cardiac events at 3 years and for death/myocardial infarction at 5 years after initial testing [23]. Therefore, it may be hypothesized that MPI could provide better short-term risk assessment, while CAC scoring may provide a better estimate longer-term prognosis because of its ability to detect varying degrees of coronary atherosclerosis before the development of stress-induced myocardial ischaemia [23]. Summarizing the published studies, in patients with a low/intermediate risk with a very high CAC score a normal MPI confers a benign short-term prognosis, while the long-term risk of a severe cardiac event is increased.
Potentially, CAC scoring could improve postimaging clinical management and patient behaviour. Two prior studies have investigated whether the knowledge of present coronary atherosclerotic burden affects medical treatment strategy in patients without evidence of abnormal myocardial perfusion. In consecutive patients with nonischaemic MPI findings who underwent CAC scoring in the same setting or shortly after MPI, subsequent initiation or optimization of medical therapy for CAD was more likely to occur in those found to have CAC as compared to those without CAC [26, 27]. However, whether the aggressive management of risk factors induced by CAC scores averts future adverse cardiovascular events, especially in patients with extensive CAC, is currently unclear.
The question arising from our results is why patients with extensive CAC and normal MPI findings are frequently referred for downstream invasive testing with subsequent coronary revascularization despite the lack of ischaemia. The detection of very high CAC scores is associated with a high likelihood of ischaemia and obstructive CAD [8–10]. Therefore, these patients may have a higher pretest likelihood than we defined prior to testing. As for most diagnostic tests, a normal MPI study in such patients with a high pretest probability should be interpreted with caution. This may be particularly relevant in patients with suspected three-vessel CAD or left main stenosis. Visual analysis of MPI images provides information on relative rather than absolute perfusion for each myocardial region. Therefore, global but uniform reduction in coronary vasodilator reserve may result in a homogeneous distribution of radiotracer, potentially leading to false-negative MPI results [28, 29]. In addition, the collateral circulation could maintain adequate myocardial perfusion, leading to underestimation of the angiographic severity of coronary lesions. Several other factors may contribute to false-negative MPI findings including insufficient coronary vasodilatation due to unrecognized ingestion of caffeine-containing products, attenuation and motion artifacts and plateauing of myocardial tracer uptake at high flow rates [29–36]. Although the incorporation of several nonperfusion imaging findings seems to significantly improve the detection of balanced ischaemia [37], a recent study still found obstructive CAD in 76 % of patients with extensive CAC and a normal MPI [14]. Interestingly, in less than one-third of these patients three-vessel disease was found as a possible explanation for the lack of perfusion defects. Similarly, in our study in only 42 % of patients with obstructive CAD despite nonischaemic MPI findings could the CAD be attributed to three-vessel coronary disease.
In summary, the high probability of obstructive CAD in symptomatic patients with extreme CAC scores, the possibility of false-negative MPI findings, and the recommendation for coronary revascularization for any stenosis >50 % in patients with limiting angina unresponsive to optimal medical treatment could be explanations for the high referral rate for ICA despite the absence of objective ischaemia [38]. Based on our findings, we do not believe that all symptomatic patients with a very high CAC score and a nonischaemic MPI result should routinely undergo invasive testing. However, in patients with persistent symptoms in whom clinical suspicion places them at a higher risk of significant CAD ICA should be considered.
Our study had several limitations. First, this was a retrospective study. Second, we used SPECT rather than PET imaging that may have a higher diagnostic accuracy, especially in relation to the well-known difficulty in finding balanced ischaemia. However, SPECT is more widely available and there is longer experience with its use. Further, the use of pharmacological stress and a 20-segment model for the left ventricle instead of the recommended 17-segment model could be a limitation. Furthermore, since this was a single centre study in a selected MPI referral cohort with no prior CAD at low or intermediate pretest likelihood, our findings must be read with caution before extrapolating to other populations. Patient referrals, clinical postimaging medical management and downstream utilization of invasive testing were left to the discretion of the treating physicians, which could have been a source of bias. However, the findings do reflect general cardiac patient care. Another limitation includes the definition of obstructive CAD and the determination of the need for revascularization. They were mainly based on visual assessment of the severity of coronary stenoses on ICA, as pressure-derived fractional flow reserve measurement was only used in a few patients. Finally, we also recognize that the relatively short follow-up period may have resulted in under-reporting of adverse cardiac events.
Conclusion
Approximately 50 % of the symptomatic patients with a high CAC score have normal MPI. In most of those with ischaemia on MPI, ICA confirms coronary obstructions. In patients without ischaemia on MPI but persisting complaints, the prevalence of obstructive CAD as demonstrated by ICA is also high. In all symptomatic patients with a high CAC score, the incidence of cardiac events is low, whereas the occurrence of coronary revascularization is high. However, more prospective studies are needed to assess the long-term prognostic value of severe CAC in symptomatic patients referred for MPI.
References
Shaw JL, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–85.
Marcassa C, Bax JJ, Bengel F, Hesse B, Petersen CL, Reyes E, et al. Clinical value, cost-effectiveness, and safety of myocardial perfusion scintigraphy: a position statement. Eur Heart J. 2008;29:557–63.
Chamuleau SA, Meuwissen M, Koch KT, van Eck-Smit BL, Tio RA, Tijssen JG, et al. Usefulness of fractional flow reserve for risk stratification of patients with multivessel coronary artery disease and an intermediate stenosis. Am J Cardiol. 2002;89:377–80.
Lopes NH, da Silva Paulitsch F, Gois AF, Pereira AC, Stolf NA, Dallan LO, et al. Impact of number of vessels disease on outcome of patients with stable coronary artery disease: 5-year follow-up of the Medical, Angioplasty, and bypass Surgery Study (MASS). Eur J Cardiothorac Surg. 2008;33:349–54.
Jones EL, King 3rd SB, Craver JM, Douglas JS Jr, Kaplan JA, Morgan EA, et al. The spectrum of left main coronary artery disease: variables affecting patient selection, management, and death. J Thorac Cardiovasc Surg. 1980;79:109–16.
Simons DB, Schwarz RS, Edwards WD, Sheedy PF, Breen JF, Rumberger JA. Noninvasive definition of anatomic coronary artery disease by ultrafast computed tomographic scanning: a quantitative pathologic comparison study. J Am Coll Cardiol. 1992;20:1118–26.
Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–70.
He ZX, Hedrick TD, Pratt CM, Verani MS, Aquino V, Roberts R, et al. Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia. Circulation. 2000;101:244–51.
Schenker MP, Dorbala S, Hong EC, Rybicki FJ, Hachamovitch R, Kwong RY, et al. Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease: a combined positron emission tomography/computed tomography study. Circulation. 2008;117:1693–700.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45.
Berman DS, Wong ND, Gransar H, Miranda-Peats R, Dahlbeck J, Hayes SW, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol. 2004;44:923–30.
Rozanski A, Gransar H, Wong ND, Shaw LJ, Miranda-Peats R, Polk D, et al. Clinical outcomes after both coronary calcium scanning and exercise myocardial perfusion scintigraphy. J Am Coll Cardiol. 2007;49:1352–61.
Schepis T, Gaemperli O, Koepfli P, Namdar M, Valenta I, Scheffel H, et al. Added value of coronary artery calcium scores as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediate-risk population. J Nucl Med. 2007;48:1424–30.
Ghadri JR, Pazhenkottil AP, Nkoulou RN, Goetti R, Buechel RR, Husmann L, et al. Very high coronary calcium score unmasks obstructive coronary artery disease in patients with normal SPECT MPI. Heart. 2011;97:998–1003.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–8.
Mouden M, Timmer JR, Ottervanger JP, Reiffers S, Oostdijk AH, Knollema S, et al. Impact of a new ultrafast CZT SPECT camera for myocardial perfusion imaging: fewer equivocal results and lower radiation dose. Eur J Nucl Med Mol Imaging. 2012;39:1048–55.
Berman DS, Kiat H, van Train K, Garcia E, Friedman J, Maddahi J. Technetium 99m sestamibi in the assessment of chronic coronary artery disease. Semin Nucl Med. 1991;21:190–212. Review.
Berman DS, Kiat H, Friedman JD, Wang FP, van Train K, Matzer L, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual isotope myocardial perfusion single-photon emission computed tomography: a clinical validation study. J Am Coll Cardiol. 1993;22:1455–64.
Berman DS, Hachamovitch R, Kiat H, Cohen I, Cabico JA, Wang FP, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: a basis for optimal utilization of exercise technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol. 1995;26:639–47.
Fleischmann S, Koepfli P, Namdar M, Wyss CA, Jenni R, Kaufmann PA. Gated (99m) Tc-tetrofosmin SPECT for discriminating infarct from artefact in fixed myocardial perfusion defects. J Nucl Med. 2004;45:754–9.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte Jr M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(15):827–32.
Moser KW, O’Keefe Jr JH, Bateman TM, McGhie IA. Coronary calcium screening in asymptomatic patients as a guide to risk factor modification and stress myocardial perfusion imaging. J Nucl Cardiol. 2003;10:590–8.
Chang SM, Nabi F, Xu J, Peterson LE, Achari A, Pratt CM, et al. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol. 2009;54:1872–82.
Ramakrishna G, Miller TD, Breen JF, Araoz PA, Hodge DO, Gibbons RJ. Relationship and prognostic value of coronary artery calcification by electron beam computed tomography to stress-induced ischemia by single-photon emission computed tomography. Am Heart J. 2007;153:807–14.
Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, et al. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713–21.
Thompson RC, McGhie AI, Moser KW, O’Keefe Jr JH, Stevens TL, House J, et al. Clinical utility of coronary calcium scoring after nonischemic myocardial perfusion imaging. J Nucl Cardiol. 2005;12:392–400.
Bybee KA, Lee J, Markiewicz R, Longmore R, McGhie AI, O’Keefe JH, et al. Diagnostic and clinical benefit of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial stress perfusion imaging. J Nucl Cardiol. 2010;17:188–96.
Lima RS, Watson DD, Goode AR, Siadaty MS, Ragosta M, Beller GA, et al. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol. 2003;42:64–70.
Aernoudse WH, Botman KJ, Pijls NH. False-negative myocardial scintigraphy in balanced three-vessel disease, revealed by coronary pressure measurement. Int J Cardiovasc Intervent. 2003;5:67–71.
Travin M. Is it possible for myocardial perfusion imaging to avoid missing any patients with high-risk coronary disease? J Nucl Cardiol. 2007;14:492–6.
Heller GV, Ahmed I, Tilkemeier PL, Barbour MM, Garber CE. Influence of exercise intensity on the presence, distribution, and size of thallium-201 defects. Am Heart J. 1992;123:909–16.
Iskandrian AS, Heo J, Kong B, Lyons E. Effect of exercise level on the ability of thallium-201 tomographic imaging in detecting coronary artery disease: analysis of 461 patients. J Am Coll Cardiol. 1989;14:1477–86.
Sharir T, Rabinowitz B, Livschitz S, Moalem I, Baron J, Kaplinsky E, et al. Underestimation of extent and severity of coronary artery disease by dipyridamole stress thallium-201 single-photon emission computed tomographic myocardial perfusion imaging in patients taking antianginal drugs. J Am Coll Cardiol. 1998;31:1540–6.
Smits P, Corstens FH, Aengevaeren WR, Wackers FJ, Thien T. False-negative dipyridamole thallium-201 myocardial imaging after caffeine infusion. J Nucl Med. 1991;32:1538–41.
Travin MI, Katz MS, Moulton AW, Miele NJ, Sharaf BL, Johnson LL. The accuracy of dipyridamole SPECT to identify individual coronary stenoses and multivessel disease in women versus men. J Nucl Cardiol. 2000;7:213–20.
Duvernoy CS, Ficaro EP, Karabajakian MZ, Rose PA, Corbett JR. Improved detection of left main coronary artery disease with attenuation-corrected SPECT. J Nucl Cardiol. 2000;7:639–48.
Berman DS, Kang X, Slomka PJ, Gerlach J, de Yang L, Hayes SW, et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;14:521–8.
Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, et al. Guidelines of myocardial revascularization. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2010;31:2501–55.
Conflicts of interest
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mouden, M., Ottervanger, J.P., Timmer, J.R. et al. Myocardial perfusion imaging in stable symptomatic patients with extensive coronary atherosclerosis. Eur J Nucl Med Mol Imaging 41, 136–143 (2014). https://doi.org/10.1007/s00259-013-2539-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2539-z