Abstract
The neuropsychological characteristics of the cerebellar cognitive affective syndrome (CCAS) in congenital, non-progressive malformations of the cerebellum have been scarcely investigated, and even less is known for Joubert syndrome (JS), an inherited, non-progressive cerebellar ataxia characterized by the so-called molar tooth sign. The few studies on this topic reported inconsistent results about intellectual functioning and specific neuropsychological impairments. The aim of this research is to examine the neuropsychological profile of JS compared to other congenital cerebellar malformations (CM), considering individual variability of intellectual quotient (IQ) in the two groups. Fourteen patients with JS and 15 patients with CM aged 6-25 years were tested through a comprehensive, standardized neuropsychological battery. Their scores in the neuropsychological domains were inspected through descriptive analysis and compared by mean of MANOVA and ANOVA models, then replicated inserting IQ as covariate. The two groups showed a largely overlapping neuropsychological profile, consistent with CCAS. However, the JS group showed worse performance in visual-spatial memory compared to CM patients, although this difference was mitigated when considering IQ. These findings highlight a divergence between JS and other CM in visual-spatial memory, which might suggest a critical role of the cerebellum in recalling task-relevant memories and might inform rehabilitative interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beyond its classical role in sensorimotor control, the cerebellum is critically involved in many cognitive and affective functions [1,2,3]. The anatomical uniformity of cerebellar organization and the parallel and partially segregated connections with motor and associative cerebral areas [4] have sustained the hypothesis of a universal cerebellar computation based on prediction and error-signaling. Accordingly, Schmahmann proposed that cerebellar alterations could influence cognitive functioning in the same way as they influence motor control, resulting in what he called dysmetria of thought [5]. A complex constellation of symptoms encompassing deficits in cognitive functions, affect, and behavior regulation, characterized by an abnormal response to external stimuli, was thus described in 1998 as cerebellar cognitive affective syndrome (CCAS) [6], and documented also in developmental age [7].
More specifically, CCAS includes cognitive impairments in attention and executive functions, visuospatial processing, and language, in addition to deficits in the sensorimotor domain [8]. The neuropsychological profile of CCAS has been investigated and confirmed in populations with acquired cerebellar damage due to stroke [9] or brain tumor [10], especially when affecting the posterior lobe [4], as well as in progressive, hereditary ataxias [11, 12].
Few studies have investigated these specific deficits in congenital, non-progressive malformations of the cerebellum [13]. These conditions might disrupt the emerging connections between the cerebellum and other cortical and subcortical areas [14], thus resulting in a developmental form of CCAS [15]. The seminal work of Steinlin and colleagues [16] investigated cognitive impairments in 11 patients with congenital malformations of the cerebellum through Wechsler’s intelligence scales, reporting better verbal than non-verbal performance. In a similar vein, Tavano and colleagues [17] documented CCAS cognitive impairments in children and young adults with congenital, non-progressive malformations of the cerebellum, with greater deficits in attentional and visuospatial skills, while language abilities were more preserved. However, these studies excluded patients with Joubert syndrome (JS).
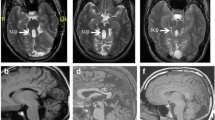
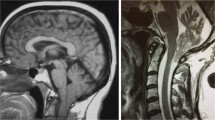
JS is an inherited, non-progressive cerebellar ataxia that usually presents with hypotonia, developmental delay, abnormal ocular movements, and distinctive facies. Advances in molecular genetics and neuroimaging techniques led to identification of a spectrum of JS-related disorders [18, 19]. Still, the main hallmark remains the so-called molar tooth sign, a set of malformations characterized by cerebellar vermis hypoplasia, deepened interpeduncular fossa, and elongated superior cerebellar peduncles, easily recognizable through magnetic resonance imaging (MRI) [20, 21]. A recent study on a wide Italian sample reported a higher prevalence in male than female individuals [22], even though sex differences were not associated with neurodevelopmental outcomes in congenital cerebellar malformations [23]. General cognitive functioning in JS has been reported to be largely variable, spanning from severe intellectual disability to borderline and even (high) average intellectual functioning [24,25,26]. The frequent presence of limb and oculomotor difficulties and speech disorders can affect cognitive evaluation in JS. Despite this, Bulgheroni and colleagues [27] reported reliable evidence of such a great variability in intellectual functioning in a sample of 49 individuals with JS, with intelligent quotient (IQ) ranging from 32 to 129. These studies, however, mainly focused on the assessment of developmental delay and intellectual disabilities, rather than characterizing the neuropsychological profile of JS patients.
A previous study [28] investigated differences in the neuropsychological profile associated with CCAS presented by eight children with JS compared to individuals with other congenital cerebellar malformations (CM). Results not only confirmed common presence of cognitive and linguistic impairments overlapping with CCAS, but also highlighted group-specific strengths and weaknesses, with CM participants showing a greater impairment of affective and executive functions and JS showing a greater impairment of verbal performance. A wide variability, however, was observed in both groups, thus requiring further examination. More recently, Hickey and colleagues [29] assessed the neuropsychological profile of three adult brothers with JS, reporting general intellectual disability, but most evident deficits of executive functions, language, and behavioral regulation. Summers and colleagues [30] investigated the neuropsychological phenotypes of 76 individuals with JS through administration of the age-appropriate Wechsler Intelligence Scales and the Vineland Adaptive Behavior Scales for participants under 2 years and 6 months of age. Unlike previous studies, the authors reported verbal comprehension and receptive language as relative strengths of the profile, while processing speed was the most affected index. Still, although reporting interesting correlations between IQ and other clinical features such as abnormal EEG and taking psychiatric medication, this study did not consider any specific neuropsychological domains other than those investigated by the Wechsler scales.
Even less is known about social perception in JS, with few studies suggesting that malformations affecting the cerebellar vermis might be associated with social disorders and autism-like behavior [17, 31, 32]. On the other hand, recent literature has documented that cerebellar alterations could affect multiple levels of social processing, from facial affect recognition to theory of mind abilities [33,34,35]. Investigating social perception abilities in the broad context of the neuropsychological profile would thus provide new insights into whether the social domain can be considered relatively more spared or impaired in JS than in other CM.
To shed further light on these issues, in this study, we compared the neuropsychological profile of children, adolescents, and young adults with JS and with other forms of CM. All participants were administered selected subtests of the NEPSY-II battery assessing attention and executive functions, memory and learning, visuospatial, sensorimotor, and social perception domains. The choice of a single, co-normed battery allowed us to overcome the issue of adopting tests from multiple batteries to evaluate different neuropsychological domains [27]. The individual IQ was also considered to control for effects of general cognitive functioning on the examined domains. Overall, the aim of this study was to compare the neuropsychological profile of JS to other CM taking into account individual variability of IQ in the two groups. Based on previous evidence of cerebellar neuropsychological impairments [6, 7], we expected to find impairments in several cognitive domains in both groups. Furthermore, based on studies of specific JS and CM neuropsychological profile [28, 29], we expected to find relatively greater attentional deficits in CM and greater verbal and visuospatial deficits in JS.
Materials and Methods
Participants
Twenty-nine patients (19 males), aged 6-25 years, were recruited at the Child Neuropsychiatry and Neurorehabilitation Unit of the Scientific Institute, IRCCS E. Medea. All participants presented with congenital malformations of the cerebellum as revealed by T1-weighted and T2-weighted images obtained through MRI. Exclusion criteria were (i) primary acquired brain lesions and (ii) severe sensorial, motor, and phono-articulatory deficits that could interfere with the neuropsychological assessment administration. For each participant, the full-scale intelligence quotient (FSIQ) derived from the age-corresponding Wechsler Intelligence Scale [36] was assessed as a routine clinical procedure during the same hospital stay in which the patients were enrolled in this study. Based on clinical evaluation of neuroimaging findings by an expert pediatric neuropsychiatrist (RR), 14 patients were classified as JS and 15 patients as CM. A resume of demographic and clinical features of the two groups is reported in Table 1 (see Supplementary material for a detailed description).
All participants and their parents were informed about study aims and provided verbal assent to participate to the study. Parents of underage children signed a written informed consent, while for participants aged 18 or over, written informed consent was obtained from them or their parents according to their legal status. The procedures were approved by the local Ethics Committee of the Scientific Institute (IRCCS) E. Medea (Prot. N.34/18 – CE) and were in accordance with the Helsinki Declaration guidelines.
Neuropsychological Assessment
All participants were assessed by a trained psychologist (EF or NB) with eight selected subtests of the Italian NEPSY–II version [37, 38]. These subtests were selected to assess six cognitive domains (attention and executive functions, memory and learning, visuospatial processing, sensorimotor functioning, and social perception) and to be administered to children of different ages and cognitive levels. In a silent room, patients were tested individually in two separate sessions, each lasting approximately 45 min. Sessions were administered in two different days at intervals of less than 10 days.
A short description of the selected NEPSY-II subtests divided by each neuropsychological domain is provided below (for further details please see [37]).
Attention and Executive Functions
Visual Attention (VA)
This task is a paper-pencil cancelation test. Children are asked to point at only figures that match the target item on an A3 sheet containing both distractors and targets. Children have 180 s to complete the task. The subtest score is calculated by subtracting the number of false alarms from the number of hits. This visual search test measures selective visual attention and the ability to inhibit distractor information.
Language
Comprehension of Instructions (CI)
This task is an auditory comprehension test. Children are required to point at pictures on a sheet according to the examiner’s commands, which have increasing length and syntactic complexity. The subtest score is the sum of the correct answers.
Memory and Learning
Memory for Designs (MD)
The examiner shows to the child a sheet depicting a 4 × 4 grid containing colored abstract drawings. The child is required to memorize the drawings and their location on the grid. After 10 s, the examiner hides the grid and gives to the child several cards depicting the previously seen drawings and other similar distractors. The child is asked to recall the position of the previously seen designs by putting the corresponding cards on a two-dimensional grid. In each trial, the number of presented drawings increases to a maximum of ten (in addition to the same number of distractor cards), while each drawing maintains the same spatial location across trials. The sum of target designs recalled correctly by the child provides a score referred to as memory for design content, while the sum of cards put in the right location on the two-dimensional grid is considered the memory for design spatial score. The two scores are averaged in a composite score that assesses visual-spatial memory and learning.
Visuospatial Processing
Geometrical Puzzles (GP)
In this task, the child looks at a sheet depicting several geometrical shapes inside and outside of a grid. The child identifies the two geometrical shapes inside the grid that match two figures outside the grid, which may be rotated. The subtest score is the sum of the correct answers. This subtest measures visual-spatial processing and mental rotation abilities.
Sensorimotor Functioning
Imitating Hand Positions
In this task, the child copies meaningful or meaningless hand and finger postures demonstrated by the examiner, with either the dominant or the non-dominant hand. The subtest score is the number of positions correctly copied with each hand. This test measures fine motor programming.
Manual Motor Sequences
In this task, the child imitates and repeats for five times a sequence of unimanual or bimanual gestures demonstrated by the examiner. The subtest score is the sum of the number of times in which the child correctly imitates each sequence. This test measures manual motor programming.
Social Perception
Affect Recognition
In this task, the child discriminates facial affect expressions. In the first part of the test, the child is required to select one of the four photographs that depicts similar affect as a target photograph at the top of the page. In the second part, the child memorizes a target emotional face shown for 5 s, and then selects, from a sample of six photographs, two pictures with similar affect as the face previously shown. The subtest score is the sum of correct responses.
Theory of Mind
This subtest consists of two parts that investigate verbal and non-verbal social abilities, respectively. During the verbal part, the child is provided with short stories or illustrations of some social situations and is then asked questions that require knowledge of another individual’s point of view to solve the task. In the contextual, non-verbal part, the child is shown an illustration depicting a social context in which the protagonist’s face is hidden. Out of four photographs showing different protagonist’s face expressions, the child must select the one that depicts the appropriate emotion of the protagonist in the illustrated social context. The sum of correct responses in each part is then aggregated in a total score.
Data Handling and Statistical Analysis
Gender distribution in the two clinical groups was compared using the chi square statistics. Their age and FSIQ were compared with Student’s T-tests (two tailed) applying Welch’s correction for unequal variance (Table 1).
Raw scores on the NEPSY-II subtests were transformed into standard scores (M =10, SD = 3) according to the mean and SD for the corresponding chronological age reported in the Italian standardization manual [38]. This transformation avoided the approximation at the low and high extremes that is inherent to the use of normative standardization tables. For each subtest, we computed descriptive statistics and we estimated the percentage of participants showing a defective performance (standard score < 4). Neuropsychological outcome measures were the standard scores obtained at the single subtests for each of the following neuropsychological domains: VA for attention and executive functions; CI for language; MD for memory and learning; and GP for visuospatial processing. Even though they assessed different components, content and spatial scores of MD were not considered separately as they were highly correlated (r(26) = 0.83, p < 0.001). In a similar vein, to reduce data dimensionality, we collapsed the standard scores obtained on the different subtests administered within the same cognitive domain. This way, the scores obtained at the imitating hand position and manual motor sequence subtests were averaged into a sensorimotor domain (SM) index, and the scores obtained at the affect recognition and theory of mind subtests were averaged into a social perception domain (SP) index. For theory of mind, please note that the scores obtained at the verbal and contextual part did not differ significantly either in the whole sample or in the two groups (all t < .056, all p > 0.58). A resume of all subtests, the corresponding examined domain and the adopted abbreviation for each neuropsychological outcome, is reported in Table 2.
The six neuropsychological outcomes (VA, CI, MD, GP, SM, and SP) were first entered into a multivariate analysis of variance (MANOVA) with diagnostic group (JS vs. CM) as a between-subject factor. The aim of this analysis was to examine whether the two clinical populations differed overall in relation to the selected outcome measures. The advantage of performing a MANOVA is that it combines multiple dependent variables into a single value that maximizes difference across group, while controlling for the inter-correlations among them [39]. The same differences were tested adding IQ scores as a covariate into a MANCOVA design, since group difference for IQ may be a potential explanation for group differences on the neuropsychological outcomes. In fact, the potential impact of IQ cannot be ruled out through statistical adjustment, regardless of whether IQ is a significant covariate or whether the differences on the dependent variables are significant [40]. Nevertheless, according to statistical considerations [41], the investigation of IQ as covariate appeared appropriate in the context of the present study, as this index is related to the dependent variables, but this relation is of no theoretical interest in terms of the investigated question, namely the identification of specificities in the neuropsychological profiles of the two clinical populations. As the difference in IQ among groups was not statistically significant in our sample (Table 1), IQ was considered here a source of variation not inherently linked to the diagnosis, which, if controlled, would allow for a more powerful test of the effects of the diagnostic group.
Second, a series of univariate ANOVAs were performed on each neuropsychological outcome separately, with diagnostic group (JS vs. CM) as a between-subject factor, to test for between-group differences in each neuropsychological domain. As with the multivariate analysis, these differences were also tested adding IQ as a covariate.
Statistical significance was obtained by a type III of sums of squares. The level of statistical significance in all tests was set at p < 0.05. The R software (version 4.0.3; R Foundation for Statistical Computing) was used to perform all the statistical analyses.
Results
Descriptive statistics for each subtest of the NEPSY-II and percentage of participants in each group showing a defective performance are reported in Table 3.
The MANOVA on the neuropsychological outcomes yielded a non-significant effect of diagnostic group (F6,22 = 0.91, p = 0.51, ηp2 = 0.19), suggesting that the two groups had similar overall neuropsychological performance. The MANCOVA with IQ as a covariate confirmed the non-significant effect of the diagnostic group (F6,22 = 0.65, p = 0.69, ηp2 = 0.16) and yielded a significant effect of IQ (F6,22 = 5.76, p = 0.001, ηp2 = 0.62), with better neuropsychological outcome in individuals with higher IQ (Pearson correlations between IQ and NEPSY subtests: VA r(27) = 0.35, p = 0.07; CI r(27) = 0.75, p < 0.001; MD r(27) = 0.48, p = 0.01; GP r(27) = 0.47, p = 0.01; SM r(27) = 0.56, p = 0.002; SP r(27) = 0.39, p = 0.04).
Regarding the univariate ANOVAs, a significant effect of diagnostic group emerged in MD (F1,27 = 5.62, p = 0.03, η2 = 0.17). This result indicated that the memory outcomes differed between groups, with JS patients showing poorer performance as compared to CM (JS: M = −8.4, SEM = 3.7; CM: M = 1.0, SEM = 1.7). Non-significant effects of diagnostic group were found in the following cognitive outcomes: VA (F1,27 = 0.41, p = 0.53, η2 = 0.01); CI (F1,27 = 1.15, p = 0.29, η2 = 0.04); GP (F1,27 = 0.59, p = 0.45, η2 = 0.02); SM (F1,27 = 0.1, p = 0.79, η2 = 0.003); and SP (F1,27 = 0.36, p = 0.55, η2 = 0.01). The ANCOVA with IQ as a covariate yielded only a trend of significance in MD (F1,27 = 3.34, p = 0.08, η2p = 0.11) and confirmed the non-significant effect of diagnostic group in VA, CI, GP, SM, and SP (all p > 0.5). Figure 1 depicts cognitive outcome distributions among diagnostic groups.
Boxplot of cognitive outcome scores by group (JS vs. CM). * indicates p < 0.05. The boxes represent the middle 50% of the data for each subtest. The upper and lower whiskers represent scores outside the middle 50% (i.e., the lower 25% of scores and the upper 25% of scores). The horizontal line within each box represents the median score. The score of 10, signaled by the dashed line, represents the normative mean
Discussion
The aim of the present study was to investigate differences in the neuropsychological profile of patients with JS and with other CM, also considering variability in general intellectual functioning. Results documented a largely overlapping profile, although the JS group showed worse performance in visual-spatial memory compared to CM patients. The covariate IQ mitigated this effect and was significant in all the examined domains, as individuals with higher IQ showed better neuropsychological outcomes. Interestingly, a strong correlation was found between IQ and verbal comprehension, whereas for the other neuropsychological outcomes, only small to moderate correlations were found. While confirming CCAS-compatible neuropsychological impairments in patients with congenital cerebellar malformations, these findings highlighted a discrepancy between JS and other CM in visual-spatial memory. This might suggest a critical role of the cerebellum in recalling task-relevant memories and might inform rehabilitative interventions.
Since its first description by Schmahmann and Sherman (1998), most of the studies documented CCAS and related cognitive impairments in adults with acquired cerebellar damage (for a meta-analysis see [8]). Here, we confirmed and integrated previous contributions in showing that non-progressive, pediatric ataxia due to either JS or other congenital CM could result in neuropsychological deficits consistent with CCAS [16, 17, 27]. Even though the profiles of the two groups were similar, displaying poor performance across all the examined cognitive domains, the patients with JS performed worse than patients with other CM in visual-spatial memory. This difference was still at least partially detectable after random-noise-variability reduction achieved by the use of IQ as a covariate. These findings could not be attributed to a higher prevalence of visual deficits in JS compared to CM patients, since both groups were similarly impaired in visuospatial processing and visual attention. Neither could they be due to the adoption of tests from different batteries as, unlike previous studies [17, 28], all the administered subtests were standardized on the same sample. Thus, our results provide evidence that a significant impairment of visual-spatial memory is inherently characteristic of the cognitive profile of JS. This is in keeping with previous literature documenting worse performance of JS individuals in tasks requiring temporary storage and manipulation of visual information [27, 28].
A cerebellar contribution to visual-spatial memory has been widely considered in previous studies [42, 43]. In detail, it has been proposed that, through its connections with basal ganglia and prefrontal cortex, the cerebellum might modulate filtering processes of incoming information in memory [44, 45]. Moreover, the cerebellum would contribute to a cerebellar-frontal-parietal network in maintaining stimulus-specific representations of working memory items [46, 47]. These studies pointed to lobules VIIb and VIIIa in representing visual-spatial stimuli, with the pyramid of the vermis critically involved in filtering irrelevant information [44]. Accordingly, we could speculate that the absence or hypoplasia of the cerebellar vermis, which is characteristic of the molar tooth sign [18, 20], might result into a more pronounced deficit of visual-spatial memory in JS through an enhanced susceptibility to distracting stimuli. However, it is to note that both groups were similarly impaired in the visual attention task. This suggests that vermis malformations associated with JS might hinder the specific filtering function exerted during the recalling of task-relevant memories more than when distinguishing target stimuli from distractors. Indeed, distinct cortico-cerebellar loops for visual attention and visual memory have been reported [47]. During memory tasks, the proposed computational mode of the cerebellum, consisting of forward-modeling and error estimation [48] (but see also [49]), would prioritize items matching the content of the internal predictive models and facilitate supervised learning trials after trials [50]. Nevertheless, the complex picture of malformations presented by our sample, affecting the cerebellum as well as other infratentorial and supratentorial areas, prevented us from disentangling the contribution of specific cerebellar areas. Furthermore, it is to note that also many CM participants presented abnormalities of the vermis. Thus, the hypothesis of a link between vermis malformations in JS and their visual-spatial memory deficits should be investigated and confirmed in future research adopting functional neuroimaging techniques.
Although higher IQ scores were associated with better performance in all the examined domains, verbal comprehension showed the highest correlation with IQ in the whole sample. This result may reflect the importance of understanding instructions in almost all tasks [51]. Furthermore, it could help to shed light on previous controversial evidence about verbal comprehension in JS. This ability was indeed indicated to be a weak point of verbal functioning in the study of Bulgheroni and colleagues [27], while it was reported to be more preserved by Tavano and Borgatti [28] and Summers and colleagues [30]. In light of the strong association between verbal comprehension and IQ reported here, these inconsistent results might depend on the large IQ variability within and across the samples investigated in these two previous studies. As suggested by Hickey and colleagues [29], patients with JS often show speech disorders mainly in expressive language due to difficulties with articulation, while other linguistic skills, such as verbal comprehension, might be in line with their intellectual functioning, with greater impairments in individuals with lower IQ.
All the other neuropsychological outcomes showed low to moderate (r < 0.6) correlations with IQ, mostly in line with the values reported in the Italian manual for the standardization sample [38]. On one hand, these findings confirm the reliability of the NEPSY-II battery for the assessment of neuropsychological profile in neurodevelopmental disorders [52,53,54]; on the other hand, they suggest that the classical IQ scales may not capture all dimensions of neuropsychological functioning. A detailed, individual assessment of neuropsychological functions should be thus included in the cognitive evaluation of cerebellar patients.
The differences in the profile of JS compared to other CM, and particularly the visual-spatial memory deficits shown by patients with JS, should be considered in identifying potential targets of rehabilitation. To date, only few studies have proposed interventions for CCAS-related cognitive impairments [55,56,57], and only a single-case study addressed these deficits in JS [58]. Interestingly, the authors reported that an intensive training focused on visual perceptual and sequencing skills was effective in improving visual-spatial memory, possibly because of more efficient strategies in manipulating visual and sequential information. A recent task-force paper [15] suggested that making cerebellar patients aware of their deficits and providing them with explicit strategies could compensate deficits in implicit, automatic cerebellar functions.
In line with the hypothesis of a predictive contribution of the cerebellum to working memory [50], the cerebellar functions of maintaining internal models and signaling mismatches between the expected and the incoming information might be targeted by interventions aiming to boost filtering of irrelevant information and enhance learning. Accordingly, previous studies proposed the cerebellar functions of predictive coding and error-signaling could be directly targeted with interventions addressing motor impairments [59] and social cognition deficits [60, 61].
Limitations should be acknowledged in interpreting the present findings. The small sample size asks for caution in generalizing the results presented here, even though the number of participants recruited is in line with or larger than previous studies on this topic [16, 28, 29]. The exclusion of participants with severe sensorial, motor, and phono-articulatory deficits was chosen in order to obtain reliable data from the neuropsychological tests; however, we cannot rule out that JS and CM patients with these features might present a rather different profile. Moreover, CCAS includes not only cognitive impairments but also affective and behavioral abnormalities, which were not assessed in the present study. Future research should consider extending psychological evaluations to detect both neuropsychological deficits and emotional-behavioral disorders [12, 30]. Despite the choice of the subtests arbitrarily based on their sensitivity to detect CCAS deficits, the adoption of the NEPSY-II allowed us to assess specific cognitive domains and to obtain standardized scores for each subtest. Finally, the specific neural bases of the reported impairments should be addressed by future research combining behavioral tasks and precise cerebellar structure and functioning measures.
Conclusions
In this study, we investigated the neuropsychological profile of JS compared to other congenital CM, also considering the individual variability of IQ in the two groups. Our results indicated that both groups presented similar impairments across multiple domains, consistent with the CCAS. However, the JS group showed worse performance in visual-spatial memory compared to CM patients. A significant effect of the covariate IQ was also found, particularly indicating a strong correlation with verbal comprehension. Overall, these findings highlight that a significant impairment of visual-spatial memory should be considered characteristic of the neuropsychological profile of JS, and they help in clarifying previous inconsistent results about relatively spared or impaired domains in this syndrome. Moreover, these results suggest a critical role of the cerebellum in recalling task-relevant memories, which could be targeted by specific rehabilitative interventions for JS.
Data Availability
The anonymized datasets generated for this study are publicly available at this link: https://zenodo.org/record/7852234#.ZFonU3bMK5c.
References
Leiner HC, Leiner AL, Dow RS. Does the cerebellum contribute to mental skills? Behav Neurosci. 1986;100(4):443–54.
Leiner HC, Leiner AL, Dow RS. Cognitive and language functions of the human cerebellum. Trends Neurosci. 1993;16(11):444–7.
Strick PL, Dum RP, Fiez JA. Cerebellum and nonmotor function. Annu Rev Neurosci. 2009;32:413–34. Available from: http://www.annualreviews.org/doi/10.1146/annurev.neuro.31.060407.125606.
Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex. 2010;46:831–44. https://doi.org/10.1016/j.cortex.2009.11.008.
Schmahmann JD. From movement to thought: anatomic substrates of the cerebellar contribution to cognitive processing. Hum Brain Mapp. 1996;4(3):174–98.
Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121(Pt 4):561–79.
Levisohn L, Cronin-Golomb A, Schmahmann JD. Neuropsychological consequences of cerebellar tumour resection in children. Cerebellar cognitive affective syndrome in a paediatric population. Brain. 2000;123(Pt 5):1041–50.
Ahmadian N, van Baarsen K, van Zandvoort M, Robe PA. The cerebellar cognitive affective syndrome—a meta-analysis. Cerebellum. 2019;18(5):941–50.
Chirino-Pérez A, Marrufo-Meléndez OR, Muñoz-López JI, Hernandez-Castillo CR, Ramirez-Garcia G, Díaz R, et al. Mapping the cerebellar cognitive affective syndrome in patients with chronic cerebellar strokes. Cerebellum. 2021:1–11. Available from: https://springerlink.bibliotecabuap.elogim.com/article/10.1007/s12311-021-01290-3.
Schmahmann JD. Pediatric post-operative cerebellar mutism syndrome, cerebellar cognitive affective syndrome, and posterior fossa syndrome: historical review and proposed resolution to guide future study. Childs Nerv Syst. 2020;36(6):1205–14.
Giocondo F, Curcio G. Spinocerebellar ataxia: a critical review of cognitive and socio-cognitive deficits. Int J Neurosci. 2018;128:182–91. Available from: https://www.tandfonline.com/doi/full/10.1080/00207454.2017.1377198.
Maas RPPWM, Killaars S, van de Warrenburg BPC, Schutter DJLG. The cerebellar cognitive affective syndrome scale reveals early neuropsychological deficits in SCA3 patients. J Neurol. 2021;268:3456–66. https://doi.org/10.1007/s00415-021-10516-7.
Poretti A, Boltshauser E. Overview of ataxias in children. Springer International Publishing Switzerland; 2016.
Stoodley CJ, Limperopoulos C. Structure–function relationships in the developing cerebellum: Evidence from early-life cerebellar injury and neurodevelopmental disorders. Semin Fetal Neonatal Med 2016;21:356–64. Available from: https://doi.org/10.1016/j.siny.2016.04.010.
Argyropoulos GPD, van Dun K, Adamaszek M, Leggio M, Manto M, Masciullo M, et al. The cerebellar cognitive affective/Schmahmann syndrome: a task force paper. Cerebellum. 2020;19(1):102–25.
Steinlin M, Styger M, Boltshauser E. Cognitive impairments in patients with congenital nonprogressive cerebellar ataxia. Neurology. 1999;53:966–73. Available from: https://n.neurology.org/content/53/5/966.
Tavano A, Grasso R, Gagliardi C, Triulzi F, Bresolin N, Fabbro F, et al. Disorders of cognitive and affective development in cerebellar malformations. Brain. 2007;130(Pt 10):2646–60.
Romani M, Micalizzi A, Valente EM. Joubert syndrome: congenital cerebellar ataxia with the molar tooth. Lancet Neurol. 2013;12:894–905. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1474442213701364.
Arrigoni F, Romaniello R, Peruzzo D, De Luca AD, Parazzini C, Valente EM, et al. Anterior mesencephalic cap dysplasia: novel brain stem malformative features associated with joubert syndrome. AJNR Am J Neuroradiol. 2017;38(12):2385–90.
Maria BL, Hoang KBN, Tusa RJ, Mancuso AA, Hamed LM, Quisling RG, et al. “Joubert syndrome” revisited: key ocular motor signs with magnetic resonance imaging correlation. J Child Neurol. 1997;12:423–30. Available from: https://journals.sagepub.com/doi/abs/10.1177/088307389701200703.
Poretti A, Boltshauser E, Valente EM. The molar tooth sign is pathognomonic for Joubert syndrome! Pediatr Neurol. 2014;50:e15–6. Available from: http://www.pedneur.com/article/S0887899413006668/fulltext.
Nuovo S, Bacigalupo I, Ginevrino M, Battini R, Bertini E, Borgatti R, et al. Age and sex prevalence estimate of Joubert syndrome in Italy. Neurology. 2020;94:e797–801. Available from: https://n.neurology.org/content/94/8/e797.
Pinchefsky EF, Accogli A, Shevell MI, Saint-Martin C, Srour M. Developmental outcomes in children with congenital cerebellar malformations. Dev Med Child Neurol. 2019;61:350–8. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/dmcn.14059.
Fennell EB, Gitten JC, Dede DE, Maria BL. Cognition, behavior, and development in Joubert syndrome. J Child Neurol. 1999;14:592–6. Available from: https://journals.sagepub.com/doi/abs/10.1177/088307389901400907.
Poretti A, Dietrich Alber F, Brancati F, Dallapiccola B, Valente EM, Boltshauser E. Normal cognitive functions in Joubert syndrome. Neuropediatrics. 2009;40:287–90. Available from: http://www.thieme-connect.com/products/ejournals/html/10.1055/s-0030-1249630.
Steinlin M, Schmid M, Landau K, Boltshauser E. Follow-up in children with Joubert syndrome. Neuropediatrics. 1997;28:204–11. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/s-2007-973701.
Bulgheroni S, D’Arrigo S, Signorini S, Briguglio M, Di Sabato ML, Casarano M, et al. Cognitive, adaptive, and behavioral features in Joubert syndrome. Am J Med Genet Part A. 2016;170:3115–24. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/ajmg.a.37938.
Tavano A, Borgatti R. Evidence for a link among cognition, language and emotion in cerebellar malformations. Cortex. 2010;46:907–18. https://doi.org/10.1016/j.cortex.2009.07.017.
Hickey CL, Sherman JC, Goldenberg P, Kritzer A, Caruso P, Schmahmann JD, et al. Cerebellar cognitive affective syndrome: insights from Joubert syndrome. Cerebellum and Ataxias. 2018;5:1–8. Available from: https://springerlink.bibliotecabuap.elogim.com/articles/10.1186/s40673-018-0085-y.
Summers AC, Snow J, Wiggs E, Liu AG, Toro C, Poretti A, et al. Neuropsychological phenotypes of 76 individuals with Joubert syndrome evaluated at a single center. Am J Med Genet Part A. 2017;173:1796–812. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ajmg.a.38272.
Holroyd S, Reiss AL, Bryan RN. Autistic features in Joubert syndrome: a genetic disorder with agenesis of the cerebellar vermis. Biol Psychiatry. 1991;29:287–94. Available from: https://linkinghub.elsevier.com/retrieve/pii/000632239191291X.
Ozonoff S, Williams BJ, Gale S, Miller JN. Autism and autistic behavior in Joubert syndrome. J Child Neurol. 1999;14:636–41. Available from: https://pubmed.ncbi.nlm.nih.gov/10511335/.
Clausi S, Olivito G, Lupo M, Siciliano L, Bozzali M, Leggio M. The cerebellar predictions for social interactions: theory of mind abilities in patients with degenerative cerebellar atrophy. Front Cell Neurosci. 2019;12:510.
Butti N, Corti C, Finisguerra A, Bardoni A, Borgatti R, Poggi G, et al. Cerebellar damage affects contextual priors for action prediction in patients with childhood brain tumor. Cerebellum. 2020;19(6):799–811.
Van Overwalle F, Manto M, Cattaneo Z, Clausi S, Ferrari C, Gabrieli JDE, et al. Consensus paper: cerebellum and social cognition. The Cerebellum [Internet]. Cerebellum. 2020;19:833–68. Available from: https://springerlink.bibliotecabuap.elogim.com/10.1007/s12311-020-01155-1.
Wechsler D. Wechsler intelligence scale for children – Fourth edition (WISC-IV) administration and scoring manual. San Antonio, TX: The Psychological Corporation; 2003.
Korkman M, Kirk U, Kemp S. NEPSY—Second Edition (NEPSY-II). San Antonio, TX: Harcourt Assessment; 2007.
Urgesi C, Campanella F, Fabbro F. NEPSY-II, Contributo alla Taratura Italiana. Firenze: Giunti OS; 2011.
Bray J, Maxwell S. Multivariate analysis of variance. Multivar. Anal Var. 2455 Teller Road, Newbury Park California 91320 United States of America: SAGE Publications, Inc.; 1985 [cited 2022 Feb 14]. Available from: http://methods.sagepub.com/book/multivariate-analysis-of-variance.
Dennis M, Francis DJ, Cirino PT, Schachar R, Barnes MA, JMJM F. Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. J Int Neuropsychol Soc. 2009;15:331–43. Available from: https://www.cambridge.org/core/journals/journal-of-the-international-neuropsychological-society/article/abs/why-iq-is-not-a-covariate-in-cognitive-studies-of-neurodevelopmental-disorders/2327A3514AFC09E32B736071B9399972.
Huitema BE. The analysis of covariance and alternatives: statistical methods for experiments, quasi-experiments, and single-case studies: second edition [Internet]. Anal. Covariance Altern. Stat. Methods Exp. Quasi-Experiments, Single-Case Stud. Second Ed. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2011 [cited 2022 Feb 11]. Available from: https://books.google.it/books?hl=it&lr=&id=6dxwep5_ZxAC&oi=fnd&pg=PT15&dq=Huitema+BE.+The+analysis+of+covariance+and+alternatives.+&ots=gyzO1pDd0j&sig=Z-sCt8TtcHaZT86FKJDaBvnXhsc&redir_esc=y#v=onepage&q=Huitema BE. The analysis of covariance and alternative.
Desmond JE, Fiez JA. Neuroimaging studies of the cerebellum: language, learning and memory. Trends Cogn Sci. 1998;2:355–62.
Guell X, Gabrieli JDE, Schmahmann JD. Triple representation of language, working memory, social and emotion processing in the cerebellum: convergent evidence from task and seed-based resting-state fMRI analyses in a single large cohort. Neuroimage. 2018;172:437–49. Available from: https://linkinghub.elsevier.com/retrieve/pii/S105381191830082X.
Baier B, Müller NG, Dieterich M. What part of the cerebellum contributes to a visuospatial working memory task? Ann Neurol. 2014;76:754–7. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/ana.24272.
Baier B, Karnath HO, Dieterich M, Birklein F, Heinze C, Müller NG. Keeping memory clear and stable—the contribution of human basal ganglia and prefrontal cortex to working memory. J Neurosci. 2010;30:9788–92. Available from: https://www.jneurosci.org/content/30/29/9788.
Brissenden JA, Tobyne SM, Halko MA, Somers DC. Stimulus-specific visual working memory representations in human cerebellar lobule VIIb/VIIIa. J Neurosci. 2021;41:1033–45. Available from: https://www.jneurosci.org/content/41/5/1033.
Brissenden JA, Somers DC. Cortico–cerebellar networks for visual attention and working memory. Curr Opin Psychol. 2019;29:239–47.
Schmahmann JD. The role of the cerebellum in cognition and emotion: personal reflections since 1982 on the dysmetria of thought hypothesis, and its historical evolution from theory to therapy. Neuropsychol Rev. 2010;20(3):236–60.
Diedrichsen J, King M, Hernandez-Castillo C, Sereno M, Ivry RB. Universal transform or multiple functionality? Understanding the contribution of the human cerebellum across task domains. Neuron. 2019;102:918–28. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0896627319303782.
Stein H. Why does the neocortex need the cerebellum for working memory? J Neurosci. 2021;41:6368–70. Available from: /pmc/articles/PMC8318082/.
Braaten EB, Norman D. Intelligence (IQ) testing. Pediatr Rev. 2006;27:403–8. Available from: /pediatricsinreview/article/27/11/403/34094/Intelligence-IQ-Testing.
Ferrari E, Butti N, Gagliardi C, Romaniello R, Borgatti R, Urgesi C. Cognitive predictors of Social processing in congenital atypical development. J Autism Dev Disord. 2022; Available from: https://springerlink.bibliotecabuap.elogim.com/10.1007/s10803-022-05630-y.
Narzisi A, Muratori F, Calderoni S, Fabbro F, Urgesi C. Neuropsychological profile in high functioning autism spectrum disorders. J Autism Dev Disord. 2013;43(8):1895–909.
Di Lieto MC, Brovedani P, Pecini C, Chilosi AM, Belmonti V, Fabbro F, et al. Spastic diplegia in preterm-born children: executive function impairment and neuroanatomical correlates. Res Dev Disabil. 2017;61:116–26.
Ito T, Osawa A, Maeshima S, Kikuchi Y, Kigawa H. Rehabilitation approach for the patient with cerebellar cognitive affective syndrome. Int J Stroke. 2010;5:291. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L70335673%5Cn. https://doi.org/10.1111/j.1747-4949.2010.00480.x.
Ruffieux N, Colombo F, Gentaz E, Annoni JM, Chouiter L, Roulin Hefti S, et al. Successful neuropsychological rehabilitation in a patient with cerebellar cognitive affective syndrome. Appl Neuropsychol Child. 2017;6:180–8. https://doi.org/10.1080/21622965.2015.1092087.
Maeshima S, Osawa A. Stroke rehabilitation in a patient with cerebellar cognitive affective syndrome. Brain Inj. 2007;21:877–83.
Gagliardi C, Brenna V, Romaniello R, Arrigoni F, Tavano A, Romani M, et al. Cognitive rehabilitation in a child with Joubert Syndrome: developmental trends and adaptive changes in a single case report. Res Dev Disabil. 2015;47:375–84. https://doi.org/10.1016/j.ridd.2015.09.013.
Bhanpuri NH, Okamura AM, Bastian AJ. Predicting and correcting ataxia using a model of cerebellar function. Brain. 2014;137:1931–44.
Butti N, Biffi E, Genova C, Romaniello R, Redaelli DF, Reni G, et al. Virtual reality social prediction improvement and rehabilitation intensive training (VR-SPIRIT) for paediatric patients with congenital cerebellar diseases: study protocol of a randomised controlled trial. Trials. 2020;21(1):82.
Urgesi C, Butti N, Finisguerra A, Biffi E, Valente EM, Romaniello R, et al. Social prediction in pediatric patients with congenital, non-progressive malformations of the cerebellum: from deficits in predicting movements to rehabilitation in virtual reality. Cortex. 2021;144:82–98. Available from: http://www.ncbi.nlm.nih.gov/pubmed/34662720.
Acknowledgements
We would thank all children and their parents for taking part into the study.
Funding
This study was funded by the Italian Ministry of Health (Ricerca Finalizzata 2013: NET-2013-02356160-4, to RB; Ricerca Finalizzata 2016: GR-2016-02363640 to CU; Ricerca Corrente 2021-2022-2023).
Author information
Authors and Affiliations
Contributions
Niccolò Butti, Cosimo Urgesi, Romina Romaniello, Chiara Gagliardi, and Renato Borgatti conceived the study design. Material preparation, data collection, and analysis were performed by Niccolò Butti, Elisabetta Ferrari, and Viola Oldrati. Niccolò Butti, Elisabetta Ferrari, and Viola Oldrati wrote and revised the first draft and all authors commented on previous versions of the manuscript. All authors critically read, improved, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Ethics Committee of the Scientific Institute IRCCS E. Medea (Prot. N.34/18 – CE) and procedures were in accordance to the 1964 Declaration of Helsinki and its later amendments.
Consent to Participate
Before starting the experiment, all participants and their parents were informed about aims and methods of the study and asked to sign informed consent.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 53 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Butti, N., Oldrati, V., Ferrari, E. et al. New Insights into the Neuropsychological Profile and Intellectual Quotient Variability in Joubert Syndrome Compared to Other Congenital Cerebellar Malformations. Cerebellum 23, 579–588 (2024). https://doi.org/10.1007/s12311-023-01580-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-023-01580-y