Abstract
Fetal alcohol spectrum disorder (FASD) is the principal preventable cause of mental retardation in the western countries resulting from alcohol exposure during pregnancy. Ethanol-induced massive neuronal cell death occurs mainly in immature neurons during the brain growth spurt period. The cerebellum is one of the brain areas that are most sensitive to ethanol neurotoxicity. Currently, there is no effective treatment that targets the causes of these disorders and efficient treatments to counteract or reverse FASD are desirable. In this study, we investigated the effects of nicotinamide on ethanol-induced neuronal cell death in the developing cerebellum. Subcutaneous administration of ethanol in postnatal 4-day-old mice induced an over-activation of caspase-3 and PARP-1 followed by a massive neurodegeneration in the developing cerebellum. Interestingly, treatment with nicotinamide, immediately or 2 h after ethanol exposure, diminished caspase-3 and PARP-1 over-activation and reduced ethanol-induced neurodegeneration. Conversely, treatment with 3-aminobenzadine, a specific PARP-1 inhibitor, was able to completely block PARP-1 activation, but not caspase-3 activation or ethanol-induced neurodegeneration in the developing cerebellum. Our results showed that nicotinamide reduces ethanol-induced neuronal cell death and inhibits both caspase-3 and PARP-1 alcohol-induced activation in the developing cerebellum, suggesting that nicotinamide might be a promising and safe neuroprotective agent for treating FASD and other neurodegenerative disorders in the developing brain that shares similar cell death pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exposure to alcohol during brain development may cause fetal alcohol spectrum disorder (FASD) or fetal alcohol syndrome (FAS) depending on the gravity. FASD is the leading cause of mental retardation in western countries, affecting around 1% of newborn babies [1, 2]. It is well accepted that consuming numerous drink per occasion (i.e., binge drinking) is particularly detrimental to the developing brain [3]. Ethanol (EtOH) causes neuronal loss throughout the developing brain and damage varies among brain areas and during particular developmental periods. Indeed, neurons are particularly vulnerable to EtOH-induced cell death during the brain growth spurt, which, in humans, starts during the third trimester and continues for several years after birth and in rodents occurs during the first two to three postnatal weeks [4,5,6,7]. The cerebellum is one of the regions particularly susceptible to EtOH damage. Reduced cerebellar volume and altered cerebellar function, including gait and walk impairment, alterations in posture, balance, and motor coordination have been described in FASD patients [8,9,10]. In rodent models, acute EtOH injection around postnatal days (PD) 4–5 induces caspase-3 activation and massive apoptotic cell death in the developing cerebellum [11,12,13]. Alteration in cerebellar-dependent behavior has also been reported after ethanol exposure during the postnatal period including deficits on rotarod, runway, parallel bars, eyeblink conditioning, and dowel crossing [14,15,16,17,18]. Despite efforts to increase consciousness of FAS risks, consumption of alcohol during pregnancy—particularly binge drinking—is unfortunately broadly diffuse, making efficient treatments to counteract or revert FAS desirable.
Nicotinamide, an amide of vitamin B3, is the precursor for the synthesis of coenzyme β-nicotinamide adenine dinucleotide, NAD+, and the phosphorylated derivative NADP+, which are involved in several cellular functions and metabolism [19]. Nicotinamide enhances neuronal survival following a multiplicity of insults, such as free radical exposure and oxidative stress. Furthermore, it has been demonstrated that nicotinamide has neuroprotective effects in different animal models of neurodegeneration [20,21,22,23]. We have previously shown that nicotinamide prevents the neuronal cell death EtOH-induced in the hippocampus, thalamus, and cingulate cortex of PD7 mice [5]; however, it is not known whether nicotinamide is also able to inhibit the neurodegeneration induced by acute EtOH exposure in the developing cerebellum. The exact molecular mechanism(s) underlying the protective effects of nicotinamide in EtOH-induced neurodegeneration is not completely understood.
Poly (ADP-ribose) polymerase (PARP-1) is a nuclear enzyme important for DNA repair, transcription, and chromatin modification. Following activation, by binding to DNA strand breaks, PARP-1 catalyzes the covalent addition of the poly(ADP-ribose) moiety of NAD+ to nuclear proteins including histones, transcription factors and PARP-1 itself. Excessive PARP-1 activation under pathological conditions, such as ischemia-reperfusion injury, oxidative stress, glutamate excitotoxicity, and neurodegenerative diseases, consumes NAD+ and ATP resulting in cellular dysfunction and cell death [24,25,26,27,28,29,30]. It is, however, not known whether EtOH administration may induce activation of PARP-1 in postnatal cerebellum, and if nicotinamide is able to prevent this activation. Additionally, it is also not known if blocking PARP-1 activation is sufficient to prevent EtOH-induced neuronal death during cerebellum development.
The aim of this study was to investigate whether nicotinamide was able to counteract the neurotoxic effects of EtOH exposure in postnatal mice cerebellum and to assess if this effect was PARP-1-dependent.
Methods
Animals
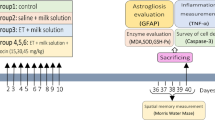
Pregnant CD1 female were purchased from Charles River Laboratories. Postnatal 4-day-old (PD4) CD1 mice were injected subcutaneously with 20% EtOH in saline solution delivering 5 g/kg body. This protocol produces blood alcohol concentrations above the toxic threshold of 200–400 mg/dl for several hours [5]. Nicotinamide (0.25, 0.5, and 1 g/kg) and 3-aminobenzadine (30 mg/kg) were administered subcutaneously immediately (0 h) or 2 h after EtOH injection. Saline injections of equal volume were used as controls for EtOH, nicotinamide, and 3-aminobenzamide (3-ABA) injections. In each litter, both male and female were used and distributed equally into the different treatment groups. Twenty-four different litters were used for all the experimental procedures. All animal procedures were approved by the Institutional Animal Care and Use Committees of Weill Cornell Medical College and were conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Histology
Mice were deeply anesthetized and transcardially perfused with 4% of paraformaldehyde in 0.1 M phosphate buffer (PB) pH 7.4 and post-fixed over night at 4 °C. The brains were cut into 40-μm-thick transverse sections on a vibratome, and sections were stored at − 20 °C in a cryoprotectant solution (30% glycerol, 30% ethylene-glycol and 40% 0.1 m PB, pH 7.4).
Western Blot
Western Blot analysis was performed as previously reported [5]. Cerebellums were lysed in boiling SDS buffer (250 mM Tris-HCl pH 6.8, 2.5% SDS), briefly sonicated and centrifuged at 14,000×g for 20 min. Protein concentration was determined using a DC Protein Assay Kit (Bio-Rad, Hercules, CA, USA). Equal amounts of proteins were loaded in a SDS-PAGE gel and transferred to a PVDF membrane (Immobilon P, Millipore, Bedford, MA, USA). Membranes were saturated with 5% nonfat milk in TBS-T and then incubated overnight at 4 °C with the following primary antibodies: anti-active caspase-3 antibody (1:1000; Cell Signalling, Beverly, MA, USA), anti-poly(ADP-ribose) (1:2000; Biomol, Hamburg, Germany), and anti-alpha-tubulin antibody (1:40,000; Sigma, St. Louis, MO, USA). Membranes were washed and incubated with the appropriate horseradish peroxidase-conjugated secondary antibodies. Peroxidase immunoreactivity bands were revealed by chemiluminescence method (Pierce, Rockford, IL, USA). Immunoreactive bands were scanned and intensity quantitated by the NIH Image software (Scion, Frederick, MD, USA).
Fluoro-Jade B Staining
Fluoro-Jade B staining was performed as previously described [5]. Briefly, sections were fixed on slides and dried over night. Slides were dipped in a solution of 1% sodium hydroxide and 80% EtOH for 5 min and then into 70% alcohol for 2 min and next washed in distilled water. Slides were immersed in 0.06% potassium permanganate solution for 10 min. Slides were rinsed in distillated water and transferred in a solution of 0.1% acetic acid and 0.0004% Fluoro-Jade B (Calbiochem, San Diego, CA, USA) for 20 min. Slides were washed three times in water, let dry at 55°C for 10 min, and mounted with Krystallon (EMD Chemicals, Gibbstown, NJ, USA).
Cell Counting
Fluoro-Jade-positive cells were counted by using a Nikon Eclipse E600 with a Nikon 40X objective as previously described [5]. Outline of the different regions was traced with a computer, and the area was calculated by the MicroBrighField Stereoinvestigator Software (MBF Bioscience, Williston, VT, USA). The relative area densities (counts/mm2) of Fluoro-Jade B positive cell profiles were estimated using the fractionator probe and systematic random sampling with a CE of 0.1–0.08. Sections were counted between 2 and 5 days after staining the sections for Fluoro-Jade B. Counting was performed in a blind manner.
Data Analysis
Statistical analyses were performed with GraphPad Prism 6 (GraphPad Software, La Jolla, CA, USA). Data are presented as mean ± standard error of the mean (SEM). Statistical analyses were performed by the analysis of variance (ANOVA) and the Dunnet’s post-hoc procedure was used for comparing time 0 group vs all the other time groups, or EtOH group vs all the other groups.
Results
Nicotinamide Blocks Ethanol-Induced Caspase-3 Activation in the Developing Cerebellum
We first assessed the time course of caspase-3 activation in the cerebellum after EtOH exposure. PD4 mice were injected with 5 g/kg of EtOH and sacrificed after 2, 4, 8, 12, and 24 hours (h). Activated caspase-3 levels were increased 4 h after EtOH treatment, reached the peak at 8 h (p < 0.001), and returned to basal levels at 24 h (Fig. 1a, b).
Nicotinamide inhibits ethanol-induced caspase-3 activation in the developing cerebellum. a, b Time course of activated caspase-3 after EtOH exposure. P4 mice were injected with 5 g/kg of EtOH and sacrificed at different time points. Representative western blot for activated caspase-3 (a) and densitometric quantification (b). One-way ANOVA (F5,18 = 5.996; p = 0.002) followed by Dunnet’s multiple comparison test; ***p < 0.001 vs 0 h. (N = four pups/group; three litters). c, d Mice were treated with different doses of nicotinamide immediately (0 h) or after EtOH exposure (2 h). Representative western blot image of activated caspase-3 measured 8 h after EtOH injection (c) and densitometric quantification (d). One-way ANOVA (F7,53 = 5.042; p = 0.0002) followed by Dunnet’s multiple comparison test; *p < 0.05; **p < 0.01; ****p < 0.0001 vs EtOH. (N = six to ten pups/group; eight litters). Sal saline, EtOH ethanol, Nic nicotinamide
We previously showed that nicotinamide reduces caspase-3 activation and EtOH-induced neurodegeneration in the forebrain at PD7 [5]. In order to assess whether nicotinamide was also able to inhibit the EtOH-induced caspase-3 activation in the cerebellum at PD4, we administered different doses of nicotinamide (0.25; 0.5; 1 g/kg) immediately after EtOH exposure (0 h), or 2 h later. Mice were then sacrificed 8 h after EtOH treatment, when the caspase-3 activation was highest. Our results showed that only 1 g/kg of nicotinamide significantly reduced the cleaved caspase-3 levels induced by EtOH (0 h p < 0.01; 2 h p < 0.05) (Fig. 1c, d).
Nicotinamide Reduces Ethanol-Induced Neurodegenaration in the Developing Cerebellum
Next we assessed whether 1 g/kg of nicotinamide was also able to inhibit EtOH-induced neurodegeneration by measuring the total amount of Fluoro-Jade-B (FJB)-positive cells in the cerebellum. We specifically counted number of FJB positive cells in the lobules III, IV, IX, and X among the most sensitive cerebellar regions to EtOH treatment [31, 32]. Twelve hours after EtOH treatment, the lobules III, IV, IX, and X showed a significantly greater number of FJB-positive cells compared with the control (p < 0.001) (Fig. 2). Remarkably, EtOH-treated mouse pups injected with nicotinamide immediately after EtOH exposure showed a significant reduction of FJB positive cells compared with EtOH treatment alone (p < 0.05) in all the lobules analyzed, while administration of nicotinamide 2 h after EtOH exposure significantly reduced the number of FJB only in the lobules IX (p < 0.001) and III (p < 0.05), indicating that the neuroprotective effect of nicotinamide was superior when administered shortly after EtOH exposure.
Nicotinamide reduces ethanol-induced neurodegeneration in the developing cerebellum. a–d Representative images of Fluoro-Jade-B staining 12 h after EtOH exposure. e–h Quantification of Fluoro-Jade-B-positive cells in the lobules X (e), IX (f), VI (g), and III (h) of cerebellum. Nicotinamide was co-administered (0 h) or post-administered (2 h) with EtOH. One-way ANOVA (e F3,19 = 15.09, p < 0.0001; f F3,19 = 6.94, p = 0.0024; g F3,19 = 16.07, p < 0.0001; and h F3,19 = 6.66; p = 0.0029) followed by Dunnet’s multiple comparison test; *p < 0.05; ***p < 0.01; ***p < 0.001; ****p < 0.0001 vs EtOH. (N = five to six pups/group; three litters). Sal saline, EtOH ethanol, Nic nicotinamide
Nicotinamide Inhibits Ethanol-Induced PARP-1 Activation in the Developing Cerebellum
Administration of nicotinamide was able to inhibit caspase-3 activation and the subsequent EtOH-induced neurodegeneration in the cerebellum. It is well known that nicotinamide may exert its neuroprotective effects also by blocking the activity of PARP-1, a DNA repair enzyme that may induce cell death when excessively activated [22, 33]. However, it is not known whether EtOH may induce activation of PARP-1 and if nicotinamide may prevent this activation in the developing cerebellum. We first assessed whether EtOH was able to induce PARP-1 activation by measuring the formation of polymers of ADP-ribose (PAR) levels at 2, 4, 8, 12, and 24 h after EtOH treatment. PAR levels started to increase at 2 h after EtOH exposure, peaked at 8-12 h (p < 0.001) and returned to baseline at 24 h (Fig. 3a, b). In order to determine whether nicotinamide was able to inhibit the EtOH-induced PARP-1 activation, PD4 mouse pups were treated with different doses of nicotinamide or with 3-aminobenzamide (3-ABA), a specific PARP-1 inhibitor, immediately after EtOH exposure or 2 h later. We found that all the doses of nicotinamide and 3-ABA were able to block PARP-1 activation when administered both immediately and 2 h after EtOH treatment (p < 0.001) (Fig. 3c, d).
Nicotinamide inhibits ethanol-induced PARP-1 activation in the developing cerebellum. a, b Time course of polymers of ADP-ribose (PAR) levels after EtOH exposure. PD4 mice were injected with 5 g/kg of EtOH and sacrificed at different time points. Representative western blot for PAR levels (a) and densitometric quantification (b). One-way ANOVA (F5,18 = 11.91; p < 0.0001) followed by Dunnet’s multiple comparison test; ***p < 0.001 vs 0 h. (N = four pups/group; three litters). c, d Mice were treated with nicotinamide or 3-aminobenzidine immediately (0 h) or after EtOH exposure (2 h). Representative western blot image for PAR levels 8 h after EtOH injection (c) and densitometric quantification (d). One-way ANOVA (F9,31 = 3.31; p < 0.0061) followed by Dunnet’s multiple comparison test; **p < 0.01 vs EtOH. (N = four to five pups/group; four litters). Sal saline, EtOH ethanol, Nic nicotinamide, 3-ABA 3-aminobenzidine
Blocking PARP-1 Activation Is Not Sufficient to Prevent Ethanol-Induced Neurodegeneration and Caspase-3 Activation in the Developing Cerebellum
Several studies have shown that inhibition of PARP-1 can prevent the neuronal death induced by excitotoxicity and oxidative stress [34,35,36]. In order to study whether blocking the activation of PARP-1 was sufficient to prevent the EtOH-induced neurodegenaration in the postnatal cerebellum, we injected subcutaneously PD4 mice with nicotinamide immediately after EtOH exposure, when the neuro-protective effect of nicotinamide was higher (Fig. 4) or with 3-ABA immediately and 2 h after EtOH exposure. Fluoro-J-B quantification revealed that only nicotinamide was able to significantly reduce the neurodegeneration induced by EtOH treatment (p < 0.05) (Fig. 4).
3-Aminobenzidine does not reduce ethanol-induced neurodegeneration in the developing cerebellum. a–d Quantification of Fluoro-Jade-B positive cells measured 12 h after EtOH treatment in the lobules X (a), IX (b), VI (c), and III (d) of cerebellum. 3-Aminobenzidine was co-administered (0 h) or post-administered (2 h) with EtOH. Nicotinamide was co-injected with EtOH. One-way ANOVA (a F4,21 = 10.18, p < 0.0001; b F4,21 = 24.48, p = 0.0024; c F4,21 = 11.76, p < 0.0001; and d F4,21 = 7.082, p = 0.0009) followed by Dunnet’s multiple comparison test; **p < 0.01; **p < 0.01; ***p < 0.001; ****p < 0.0001 vs EtOH. (N = four to six pups/group; three litters). Sal saline, EtOH ethanol, Nic nicotinamide
Although 3-ABA was able to totally block the PARP-1 over-activation, it did not prevent the EtOH-induced neurodegeneration in the cerebellum; therefore, we decided to assess the influence of 3-ABA on EtOH-induced caspase-3 activation. We administered nicotinamide immediately after EtOH exposure as a positive control. As expected, we found that nicotinamide reduces the levels of cleaved caspase-3 induced by EtOH exposure (p < 0.001), while 3-ABA was not able to decrease this caspase-3 activation (p > 0.05) (Fig. 5).
3-Aminobenzidine does not inhibit ethanol-induced caspase-3 activation in the developing cerebellum. Mice were injected with nicotinamide or 3-aminobenzidine immediately (0 h) or after EtOH exposure (2 h). Representative western blot image for activated caspase-3 levels 8 h after EtOH treatment (a) and densitometric quantification (b). One-way ANOVA (F4,30 = 10.55; p < 0.0001) followed by Dunnet’s multiple comparison test; ***p < 0.001; ****p < 0. vs EtOH. (N = seven pups/group; three litters). Sal saline, EtOH ethanol, Nic nicotinamide
These results suggest that nicotinamide exerts its neuroprotective effect against EtOH-induced neurodegeneration mainly by blocking caspase-3 activation, while solely inhibition of PARP-1 is not sufficient to prevent this neuronal cell death.
Discussion
In the present study, we have found that administration of nicotinamide prevents or reduces the activation of the cell death pathways and the consequent neurodegeneration induced by EtOH exposure in the postnatal developing cerebellum. We have demonstrated here for the first time that pharmacologically blocking EtOH-induced PARP-1 over-activation is not sufficient to prevent the cerebellar neurodegeneration induced by EtOH exposure.
Nicotinamide, a vitamin B3 amide necessary for cellular function and metabolism, can cross the blood–brain barrier reaching the brain where it is converted to NAD+ [37] preventing the neurodegeneration induced by several insults including oxidative stress [20,21,22,23]. Our results showing that nicotinamide reduces EtOH-induced neurodegeneration in 4 days old postnatal cerebellum extend our previous findings that nicotinamide was able to prevent the EtOH-induced neuronal cell death in the hippocampus, thalamus, and cingulate cortex of 7 days old mice [5]. Additionally, we have found that nicotinamide not only reduces the caspase-3 activation, as previously reported [5], but also inhibits the EtOH-induced over-activation of PARP-1. This suggests a further mechanism of action of nicotinamide against neurotoxicity triggered by EtOH exposure. Importantly, these neuroprotective effects were still evident when nicotinamide was administered 2 h after EtOH treatment.
EtOH is a well-recognized neuroteratogen factor, and its exposure during pregnancy may cause FASD. The detrimental effects of EtOH in the developing brain include reduction of neurogenesis, inhibition of differentiation, disturbance of neuron migration, alteration of cell–cell interaction, and induction of neuronal cell death [38, 39]. This provides a possible explanation for the reduced brain mass and neurobehavioral disturbances associated with the human FASD. Obviously, the most appropriate and effective method to prevent EtOH-induced neurodegeneration in the human fetal brain is to avoid alcohol exposure during pregnancy. Notably, neurons are particularly vulnerable to several different environmental toxins during the period of sensitive synaptogenesis, which occurs from the third trimester of gestation to several years after birth in humans [4]. It has been reported that anesthetic, anti-epileptic, anticancer chemotherapeutic drugs, ischemic brain injury, and Zika virus infection trigger developmental neuronal cell death by similar mechanisms as EtOH [32, 40,41,42,43,44,45], and in these circumstances, abstinence is not an option. Interestingly, there is increasing evidence that nicotinamide promotes neuroprotective effect also in some of these neurodegenerative models such as ischemic brain injury, ketamine, and anticancer chemotherapeutic drugs [43, 46, 47]. In all these models, the neuroprotective effects of nicotinamide were associated with its ability to reduce caspase-3 activation. It is tempting to speculate that nicotinamide might have a more general neuroprotective effects in the developing brain against toxic insults where activation of caspase-3 plays a key role. It would be interesting to test Nicotinamide’s neuroprotective effects in other burdening diseases such as Zika virus infection. Indeed, it was recently reported that Zika virus infection enhanced the activation of caspase-3 and that its inhibition suppressed Zika virus-induced cell death in human cortical neural progenitors [48].
Compelling evidence indicates that hyper-activation of PARP-1 leads to a new form of programmed cell death named parthanatos, which is characterized mainly by the overproduction of cytotoxic polymers of ADP-ribose and caspase-independent signaling [25, 27]. Enhancement of PARP-1 activation and accumulation of PAR has been observed in various neurodegenerative processes; different studies have reported that inhibition of PARP-1 prevents neuronal death induced by excitotoxicity, oxidative stress and neurotoxic agents [26, 28, 30, 49]. Our results, showing that EtOH administration enhanced PAR formation—a direct marker of PARP-1 activity levels—in postnatal developing cerebellum, are consistent with previous studies showing that EtOH promote DNA damage and subsequent activation of PARP-1 in cultured fetal cortical neurons [50]. Surprisingly, while the administration of 3-ABA, a specific PARP-1 inhibitor, was able to completely block the EtOH-induced PAR formation, this was not sufficient to significantly reduce the following neurodegeneration, suggesting that other cell death pathways are involved, such as the apoptotic signaling mediated by caspase-3 activation. However, it has been previously shown that in a knock-out mouse model, the absence of caspase-3 was not sufficient to inhibit the EtOH-induced neuronal death during developing brain [51]. These results suggest that EtOH induces neurodegeneration by activating at least two independent cell death pathways, parthanatos, and apoptosis and inhibiting parthanatos alone is not sufficient to reduce the neurotoxic effect produced by EtOH exposure in the developing brain. In order to better clarify the role of these two cell death pathways in the FAS mouse model of neurodegeneration, it would be interesting to assess whether 3-ABA administration would be sufficient to block the EtOH-induced neurodegeneration in the caspase-3 knock-out mice.
Given that the metabolism of ethanol by alcohol dehydrogenase requires NAD+ and that administration of nicotinamide increases the level of NAD+ [52], it might be possible to speculate that some neuroprotective effects of nicotinamide were due to an accelerating metabolism of EtOH. Yet, this is rather unlikely because we previously showed that nicotinamide administration did not change the EtOH levels, neither in the blood nor in the brain, suggesting that indeed nicotinamide does not accelerate the metabolism of EtOH [5].
A limitation of the present study is the low determination numbers for some experiments that may have somewhat limited the statistical power. We specifically assessed the efficacy of nicotinamide during the early post-natal period, a part of the brain growth spurt phase that parallels the human third trimester, using an acute binge-like alcohol exposure model. In future work, it would be very interesting to assess whether the neurotoxic effects of lower repeated EtOH exposure throughout the gestation and/or lactation will be similarly reduced by nicotinamide treatment.
In conclusion, our results clearly showed that nicotinamide blocks both caspase-3 and PARP-1 activation but its neuroprotective effect against EtOH-induced neurodegeneration appears to be mostly through its effects on caspase-3. Future pharmacological and molecular studies will be necessary to better clarify the detailed contribution of caspase-3 and PARP-1 activation in EtOH-induced cell death in developing neurons. Remarkably, nicotinamide has been used orally in a variety of clinical trials, is well tolerated and has a good safety profile [53,54,55,56,57], and there is no evidence that nicotinamide is teratogenic by itself [58]. Therefore, nicotinamide is a potential safe neuroprotective agent that promises therapeutic value in developing brain neurodegenerative related disorders, including FASD, where neuronal cell death is triggered by caspase-3 and/or PARP-1 over-activation.
Abbreviations
- FASD:
-
Fetal alcohol spectrum disorder
- FAS:
-
Fetal alcohol syndrome
- EtOH:
-
Ethanol
- PARP-1:
-
Poly (ADP-ribose) polymerase
- FJB:
-
Fluoro-Jade-B
- PAR:
-
Polymers of ADP-ribose
- NAD+:
-
Nicotinamide adenine dinucleotide
- NADP+:
-
Nicotinamide adenine dinucleotide phosphate
- PD:
-
Postnatal days
References
May PA, Gossage JP, Kalberg WO, Robinson LK, Buckley D, Manning M, et al. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Dev Disabil Res Rev. 2009;15(3):176–92. https://doi.org/10.1002/ddrr.68.
Burd L, Klug MG, Martsolf JT, Kerbeshian J. Fetal alcohol syndrome: neuropsychiatric phenomics. Neurotoxicol Teratol. 2003;25(6):697–705. https://doi.org/10.1016/j.ntt.2003.07.014.
Bonthius DJ, West JR. Alcohol-induced neuronal loss in developing rats: increased brain damage with binge exposure. Alcohol Clin Exp Res. 1990;14(1):107–18. https://doi.org/10.1111/j.1530-0277.1990.tb00455.x.
Holmes GL. Morphological and physiological maturation of the brain in the neonate and young child. J Clin Neurophysiol. 1986;3(3):209–38. https://doi.org/10.1097/00004691-198607000-00002.
Ieraci A, Herrera DG. Nicotinamide protects against ethanol-induced apoptotic neurodegeneration in the developing mouse brain. PLoS Med. 2006;3(4):e101. https://doi.org/10.1371/journal.pmed.0030101.
Ieraci A, Herrera DG. Single alcohol exposure in early life damages hippocampal stem/progenitor cells and reduces adult neurogenesis. Neurobiol Dis. 2007;26(3):597–605. https://doi.org/10.1016/j.nbd.2007.02.011.
Ikonomidou C, Bittigau P, Ishimaru MJ, Wozniak DF, Koch C, Genz K, et al. Ethanol-induced apoptotic neurodegeneration and fetal alcohol syndrome. Science. 2000;287(5455):1056–60. https://doi.org/10.1126/science.287.5455.1056.
Sowell ER, Jernigan TL, Mattson SN, Riley EP, Sobel DF, Jones KL. Abnormal development of the cerebellar vermis in children prenatally exposed to alcohol: size reduction in lobules I-V. Alcohol Clin Exp Res. 1996;20(1):31–4. https://doi.org/10.1111/j.1530-0277.1996.tb01039.x.
Lubetzky-Vilnai A, Jirikowic TL, McCoy SW. Investigation of the dynamic gait index in children: a pilot study. Pediatr Phys Ther. 2011;23(3):268–73. https://doi.org/10.1097/PEP.0b013e318227cd82.
Jirikowic TL, McCoy SW, Lubetzky-Vilnai A, Price R, Ciol MA, Kartin D, et al. Sensory control of balance: a comparison of children with fetal alcohol spectrum disorders to children with typical development. J Popul Ther Clin Pharmacol. 2013;20(3):e212–28.
Light KE, Belcher SM, Pierce DR. Time course and manner of Purkinje neuron death following a single ethanol exposure on postnatal day 4 in the developing rat. Neuroscience. 2002;114(2):327–37. https://doi.org/10.1016/S0306-4522(02)00344-5.
Siler-Marsiglio KI, Madorsky I, Pan Q, Paiva M, Neeley AW, Shaw G, et al. Effects of acute ethanol exposure on regulatory mechanisms of Bcl-2-associated apoptosis promoter, bad, in neonatal rat cerebellum: differential effects during vulnerable and resistant developmental periods. Alcohol Clin Exp Res. 2006;30(6):1031–8. https://doi.org/10.1111/j.1530-0277.2006.000126.x.
Siler-Marsiglio KI, Paiva M, Madorsky I, Pan Q, Shaw G, Heaton MB. Functional mechanisms of apoptosis-related proteins in neonatal rat cerebellum are differentially influenced by ethanol at postnatal days 4 and 7. J Neurosci Res. 2005;81(5):632–43. https://doi.org/10.1002/jnr.20591.
Bearer CF, Wellmann KA, Tang N, He M, Mooney SM. Choline ameliorates deficits in balance caused by acute neonatal ethanol exposure. Cerebellum. 2015;14(4):413–20. https://doi.org/10.1007/s12311-015-0691-7.
Cebolla AM, Cheron G, Hourez R, Bearzatto B, Dan B, Servais L. Effects of maternal alcohol consumption during breastfeeding on motor and cerebellar Purkinje cells behavior in mice. Neurosci Lett. 2009;455(1):4–7. https://doi.org/10.1016/j.neulet.2009.03.034.
Klintsova AY, Goodlett CR, Greenough WT. Therapeutic motor training ameliorates cerebellar effects of postnatal binge alcohol. Neurotoxicol Teratol. 2000;22(1):125–32. https://doi.org/10.1016/S0892-0362(99)00052-5.
Cheng DT, Jacobson SW, Jacobson JL, Molteno CD, Stanton ME, Desmond JE. Eyeblink classical conditioning in alcoholism and fetal alcohol spectrum disorders. Front Psych. 2015;6:155. https://doi.org/10.3389/fpsyt.2015.00155.
Idrus NM, McGough NNH, Spinetta MJ, Thomas JD, Riley EP. The effects of a single memantine treatment on behavioral alterations associated with binge alcohol exposure in neonatal rats. Neurotoxicol Teratol. 2011;33(4):444–50. https://doi.org/10.1016/j.ntt.2011.04.004.
Maiese K, Chong ZZ. Nicotinamide: necessary nutrient emerges as a novel cytoprotectant for the brain. Trends Pharmacol Sci. 2003;24(5):228–32. https://doi.org/10.1016/S0165-6147(03)00078-6.
Hathorn T, Snyder-Keller A, Messer A. Nicotinamide improves motor deficits and upregulates PGC-1alpha and BDNF gene expression in a mouse model of Huntington’s disease. Neurobiol Dis. 2011;41(1):43–50. https://doi.org/10.1016/j.nbd.2010.08.017.
Green KN, Steffan JS, Martinez-Coria H, Sun X, Schreiber SS, Thompson LM, et al. Nicotinamide restores cognition in Alzheimer’s disease transgenic mice via a mechanism involving sirtuin inhibition and selective reduction of Thr231-phosphotau. J Neurosci. 2008;28(45):11500–10. https://doi.org/10.1523/JNEUROSCI.3203-08.2008.
Yang J, Klaidman LK, Chang ML, Kem S, Sugawara T, Chan P, et al. Nicotinamide therapy protects against both necrosis and apoptosis in a stroke model. Pharmacol Biochem Behav. 2002;73(4):901–10. https://doi.org/10.1016/S0091-3057(02)00939-5.
Maiese K, Chong ZZ, Hou J, Shang YC. The vitamin nicotinamide: translating nutrition into clinical care. Molecules. 2009;14(9):3446–85. https://doi.org/10.3390/molecules14093446.
Alano CC, Garnier P, Ying W, Higashi Y, Kauppinen TM, Swanson RA. NAD+ depletion is necessary and sufficient for poly(ADP-ribose) polymerase-1-mediated neuronal death. J Neurosci. 2010;30(8):2967–78. https://doi.org/10.1523/JNEUROSCI.5552-09.2010.
Andrabi SA, Dawson TM, Dawson VL. Mitochondrial and nuclear cross talk in cell death: parthanatos. Ann N Y Acad Sci. 2008;1147(1):233–41. https://doi.org/10.1196/annals.1427.014.
Diaz-Hernandez JI, Moncada S, Bolanos JP, Almeida A. Poly(ADP-ribose) polymerase-1 protects neurons against apoptosis induced by oxidative stress. Cell Death Differ. 2007;14(6):1211–21. https://doi.org/10.1038/sj.cdd.4402117.
Fatokun AA, Dawson VL, Dawson TM. Parthanatos: mitochondrial-linked mechanisms and therapeutic opportunities. Br J Pharmacol. 2014;171(8):2000–16. https://doi.org/10.1111/bph.12416.
Kauppinen TM, Swanson RA. The role of poly(ADP-ribose) polymerase-1 in CNS disease. Neuroscience. 2007;145(4):1267–72. https://doi.org/10.1016/j.neuroscience.2006.09.034.
Kim MY, Zhang T, Kraus WL. Poly(ADP-ribosyl)ation by PARP-1: “PAR-laying” NAD+ into a nuclear signal. Genes Dev. 2005;19(17):1951–67. https://doi.org/10.1101/gad.1331805.
Martire S, Mosca L, D’Erme M. PARP-1 involvement in neurodegeneration: a focus on Alzheimer’s and Parkinson’s diseases. Mech Ageing Dev. 2015;146–148:53–64. https://doi.org/10.1016/j.mad.2015.04.001.
Dikranian K, Qin YQ, Labruyere J, Nemmers B, Olney JW. Ethanol-induced neuroapoptosis in the developing rodent cerebellum and related brain stem structures. Brain Res Dev Brain Res. 2005;155(1):1–13. https://doi.org/10.1016/j.devbrainres.2004.11.005.
Luo J. Mechanisms of ethanol-induced death of cerebellar granule cells. Cerebellum. 2012;11(1):145–54. https://doi.org/10.1007/s12311-010-0219-0.
Cimadamore F, Curchoe CL, Alderson N, Scott F, Salvesen G, Terskikh AV. Nicotinamide rescues human embryonic stem cell-derived neuroectoderm from parthanatic cell death. Stem Cells. 2009;27(8):1772–81. https://doi.org/10.1002/stem.107.
Yu SW, Wang H, Poitras MF, Coombs C, Bowers WJ, Federoff HJ, et al. Mediation of poly(ADP-ribose) polymerase-1-dependent cell death by apoptosis-inducing factor. Science. 2002;297(5579):259–63. https://doi.org/10.1126/science.1072221.
Outeiro TF, Grammatopoulos TN, Altmann S, Amore A, Standaert DG, Hyman BT, et al. Pharmacological inhibition of PARP-1 reduces alpha-synuclein- and MPP+-induced cytotoxicity in Parkinson’s disease in vitro models. Biochem Biophys Res Commun. 2007;357(3):596–602. https://doi.org/10.1016/j.bbrc.2007.03.163.
Yokoyama H, Kuroiwa H, Tsukada T, Uchida H, Kato H, Araki T. Poly(ADP-ribose)polymerase inhibitor can attenuate the neuronal death after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced neurotoxicity in mice. J Neurosci Res. 2010;88(7):1522–36. https://doi.org/10.1002/jnr.22310.
Bogan KL, Brenner C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu Rev Nutr. 2008;28(1):115–30. https://doi.org/10.1146/annurev.nutr.28.061807.155443.
Goodlett CR, Horn KH, Zhou FC. Alcohol teratogenesis: mechanisms of damage and strategies for intervention. Exp Biol Med. 2005;230(6):394–406. https://doi.org/10.1177/15353702-0323006-07.
Guerri C, Bazinet A, Riley EP. Foetal alcohol spectrum disorders and alterations in brain and behaviour. Alcohol Alcohol. 2009;44(2):108–14. https://doi.org/10.1093/alcalc/agn105.
Olney JW, Young C, Wozniak DF, Jevtovic-Todorovic V, Ikonomidou C. Do pediatric drugs cause developing neurons to commit suicide? Trends Pharmacol Sci. 2004;25(3):135–9. https://doi.org/10.1016/j.tips.2004.01.002.
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23(3):876–82.
Olney JW. Focus on apoptosis to decipher how alcohol and many other drugs disrupt brain development. Front Pediatr. 2014;2:81. https://doi.org/10.3389/fped.2014.00081.
Ullah N, Lee HY, Naseer MI, Ullah I, Suh JW, Kim MO. Nicotinamide inhibits alkylating agent-induced apoptotic neurodegeneration in the developing rat brain. PLoS One. 2011;6(12):e27093. https://doi.org/10.1371/journal.pone.0027093.
Hanners NW, Eitson JL, Usui N, Richardson RB, Wexler EM, Konopka G, et al. Western Zika virus in human fetal neural progenitors persists long term with partial cytopathic and limited immunogenic effects. Cell Rep. 2016;15(11):2315–22. https://doi.org/10.1016/j.celrep.2016.05.075.
Yuan F, Chen X, Liu J, Feng W, Wu X, Chen S. Up-regulation of Siah1 by ethanol triggers apoptosis in neural crest cells through p38 MAPK-mediated activation of p53 signaling pathway. Arch Toxicol. 2017;91(2):775–84. https://doi.org/10.1007/s00204-016-1746-3.
Feng Y, Paul IA, LeBlanc MH. Nicotinamide reduces hypoxic ischemic brain injury in the newborn rat. Brain Res Bull. 2006;69(2):117–22. https://doi.org/10.1016/j.brainresbull.2005.11.011.
Ullah N, Ullah I, Lee HY, Naseer MI, Seok PM, Ahmed J, et al. Protective function of nicotinamide against ketamine-induced apoptotic neurodegeneration in the infant rat brain. J Mol Neurosci. 2012;47(1):67–75. https://doi.org/10.1007/s12031-011-9685-1.
Xu M, Lee EM, Wen Z, Cheng Y, Huang WK, Qian X, et al. Identification of small-molecule inhibitors of Zika virus infection and induced neural cell death via a drug repurposing screen. Nat Med. 2016;22(10):1101–7. https://doi.org/10.1038/nm.4184.
Andrabi SA, Kang HC, Haince JF, Lee YI, Zhang J, Chi Z, et al. Iduna protects the brain from glutamate excitotoxicity and stroke by interfering with poly(ADP-ribose) polymer-induced cell death. Nat Med. 2011;17(6):692–9. https://doi.org/10.1038/nm.2387.
Cherian PP, Schenker S, Henderson GI. Ethanol-mediated DNA damage and PARP-1 apoptotic responses in cultured fetal cortical neurons. Alcohol Clin Exp Res. 2008;32(11):1884–92. https://doi.org/10.1111/j.1530-0277.2008.00769.x.
Young C, Roth KA, Klocke BJ, West T, Holtzman DM, Labruyere J, et al. Role of caspase-3 in ethanol-induced developmental neurodegeneration. Neurobiol Dis. 2005;20(2):608–14. https://doi.org/10.1016/j.nbd.2005.04.014.
Mukherjee SK, Klaidman LK, Yasharel R, Adams JD. Increased brain NAD prevents neuronal apoptosis in vivo. Eur J Pharmacol. 1997;330(1):27–34. https://doi.org/10.1016/S0014-2999(97)00171-4.
Walsh SR, Hogg D, Mydlarski PR. Bullous pemphigoid: from bench to bedside. Drugs. 2005;65(7):905–26. https://doi.org/10.2165/00003495-200565070-00002.
Libri V, Yandim C, Athanasopoulos S, Loyse N, Natisvili T, Law PP, et al. Epigenetic and neurological effects and safety of high-dose nicotinamide in patients with Friedreich’s ataxia: an exploratory, open-label, dose-escalation study. Lancet. 2014;384(9942):504–13. https://doi.org/10.1016/S0140-6736(14)60382-2.
Olmos PR, Hodgson MI, Maiz A, Manrique M, De Valdes MD, Foncea R, et al. Nicotinamide protected first-phase insulin response (FPIR) and prevented clinical disease in first-degree relatives of type-1 diabetics. Diabetes Res Clin Pract. 2006;71(3):320–33. https://doi.org/10.1016/j.diabres.2005.07.009.
Chen AC, Martin AJ, Choy B, Fernandez-Penas P, Dalziell RA, McKenzie CA, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373(17):1618–26. https://doi.org/10.1056/NEJMoa1506197.
Crino A, Schiaffini R, Manfrini S, Mesturino C, Visalli N, Beretta Anguissola G, et al. A randomized trial of nicotinamide and vitamin E in children with recent onset type 1 diabetes (IMDIAB IX). Eur J Endocrinol. 2004;150(5):719–24. https://doi.org/10.1530/eje.0.1500719.
Knip M, Douek IF, Moore WP, Gillmor HA, McLean AE, Bingley PJ, et al. Safety of high-dose nicotinamide: a review. Diabetologia. 2000;43(11):1337–45. https://doi.org/10.1007/s001250051536.
Funding
A.I. was supported by the De Witt-Reader’s Digest Fellowship, and D.G.H. was supported by grants from the National Alliance for Research on Schizophrenia and Depression and the Reader’s Digest Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal procedures were approved by the Institutional Animal Care and Use Committees of Weill Cornell Medical College and were conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ieraci, A., Herrera, D.G. Nicotinamide Inhibits Ethanol-Induced Caspase-3 and PARP-1 Over-activation and Subsequent Neurodegeneration in the Developing Mouse Cerebellum. Cerebellum 17, 326–335 (2018). https://doi.org/10.1007/s12311-017-0916-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-017-0916-z