Abstract
To determine whether there is higher degree of platelet and/ or coagulation activation in sickle cell anaemia (SS) patients in complications and with clinical risk factors. A cross sectional study was conducted at a tertiary health care centre in central India with study groups: sickle cell disease (SCD): sickle cell anaemia (SS) and sickle cell trait (AS) consisting of 100 subjects each and controls (AA) with 40 subjects. Platelet aggregation (PA) with ADP, collagen and epinephrine, PT and aPTT were performed in all subjects and PA with ristocetin in ten candidates of each group. ANOVA and student’s unpaired t test were used to compare PA and coagulation profile of the three groups with respect to age groups, gender, present diagnosis, history of complications, frequency of hospital admissions (high ≥ 3/year) and frequency of blood transfusion (high > 2/year). The max PA% with ADP was significantly less in SS patients in steady state, which was even lesser in those having symptoms, complications in past/ present, high-frequency hospital admission and > 2 blood transfusions per year subgroups, as compared to all other groups and subgroups, but not consistently with collagen and epinephrine. The max PA % with ristocetin was least in SS with complications. No statistically significant difference in PT and aPTT values among the various clinical risk subgroups and groups was found. SCD patients can be monitored by using PA with ADP for their timely and better management. PA with ADP, PT and aPTT should be added to the workup of these patients for improved prognostication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current opinion regarding the pathophysiology of sickle cell disease (SCD), a relatively common hemoglobinopathy in central India, favors multiple interactions between red blood cells (RBCs), platelets, white blood cells (WBCs), plasma proteins and the blood vessel wall; and is not just limited to the sickled RBCs [1]. The role of platelets is supported by findings of the presence of platelet activation in these patients [2, 3].
There are varied phenotypic clinical presentations seen in SCD. This depends on and vice versa causes multiple clinical and hematological parameters to act as risk factors. The well-established clinical risk factors including high pain rate (> 3 per year), high frequency of emergency department (ED) utilizers (> 3 per year), high requirement of blood transfusion (> 2 per year) and present/ previous history of complications of SCD such as vasooclusive crisis (VOC), acute chest syndrome, stroke, priapism may predict poor prognosis/outcome [4]. The hematological values established as risk factors include high HbS %, decreased HbF and highly raised total leukocyte count prominently [4,5,6,7]. The platelet and coagulation activation has been reported to be increased in the steady state of SCD and much more increased in the crisis phase [2, 8,9,10]. Other than the present symptomatic stage, these platelet and coagulation parameters have not been studied in relation to the other clinical risk factors.
Thus, we sought to determine whether the degree of platelet and coagulation activation varies in Sickle cell anaemia (SCA) and Sickle cell trait (SCT) patients in crisis and/ or with other clinical risk factors as frequent hospital admissions, from those in steady state and controls; by measuring maximum Platelet Aggregation (PA) with Adenosine diphosphate (ADP), Collagen, Epinephrine & Ristocetin, and Prothrombin time (PT) and aPTT (activated partial thrombin time).
Material and Method
The present cross-sectional study was carried out in the Department of Pathology, at a tertiary health care center after obtaining the ethical committee approval, over a period of two years. The hospital of this institute caters to the population residing in the adjoining districts in Central India.
The sickle cell anemia and trait subjects attending the various outpatient departments and admitted in various wards were enrolled in the study after obtaining written informed consent from them. They were divided into two study groups: A. Sickle cell anaemia—SCA, i.e. SS patients (HbSS pattern on hemoglobin (Hb) electrophoresis and HbSS homozygous proved by HPLC as well) and B. Sickle cell trait patients: AS (HbAS pattern on Hb electrophoresis). Also, a control group: C. AA, constituted of healthy participants without any clinical complaints (HbAA pattern on Hb electrophoresis) was included. None of the patients or controls had received transfusions during four weeks prior to their blood draws, or therapy with aspirin or other non-steroidal anti-inflammatory drugs during the previous week, nor were they on hydroxyurea in past six months and or receiving routine blood transfusion therapy. Also, cases of double heterozygosity with HbS and beta-thalassemia, confirmed from family studies also were excluded.
History including age, gender, hemoglobin electrophoresis pattern, the presentation of the patients – symptomatic or not, in complication or steady state (no complications in past six months); complication as present diagnosis or past history; hospital admissions per year—high frequency (≥ 3 admissions per year) or low frequency, history of number of crises or pain episodes per year, frequency of blood transfusion < 2 or ≥ 2 per year, and history of hydroxyurea treatment was recorded in the case record forms.
Blood samples were obtained for performing platelet aggregation studies (PA), prothombin time (PT) and activated partial thromboplastin time (aPTT) in citrate bulbs before pricking the patient for other test samples or administration of intravenous fluids or medicines; as well as before any medicine was administered in casualty or ward. A whole blood sample was anticoagulated with 3.2 g% of sodium citrate (sodium citrate/whole blood ratio, 1:10) by collecting 4.5 ml of blood into a plastic polypropylene tube containing 0.5 ml of anticoagulant, followed by mixing it gently by tilting action. Collection, transport and centrifugation of samples were performed at room temperature. Hemolysed or lipemic samples were not processed to avoid interference with the light transmission on the platelet aggregometer, and those subjects were excluded from the study.
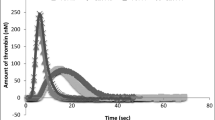
Platelet-rich plasma (PRP) was obtained by centrifuging the anticoagulated sample at 180 g for 10 min at room temperature while platelet-poor plasma (PPP) by centrifuging the remaining blood specimen for 20 min at 1200 g. PRP and PPP were carefully removed without disturbing the WBC and RBC cell layers and placed into clean polypropylene tubes with caps. PA was performed using instrument APACT 4004—four channel thrombocyte function aggregometer of LABITec Labor Biomedical Technique Gmbh with reagents adenosine diphosphate (ADP), Collagen, Epinephrine and Ristocetin of Hart Biologicals Platelet Aggregation Reagents as per the standard procedures [11]. The PT and aPTT were performed on a semi-automated coagulation analyzer.
Platelet aggregation (PA) studies with adenosine (ADP), collagen and epinephrine, PT and aPTT were performed in all subjects. Platelet aggregation with ristocetin was done in only ten patients of SS, AS and AA each. All the tests including PA were completed within 3 h after blood collection.
Statistical Analysis
The results of PA with ADP, collagen and epinephrine, PT and aPTT of the three groups were compared with respect to age groups, gender, present diagnosis, history of complications, high and low frequency of hospital admissions, frequency of blood transfusion and high-risk group.
Statistical analysis was done using statistical software STATA version 10.0 2009, using ANOVA and student’s unpaired t-test. A probability value of p < 0.05 was considered significant while p < 0.01 was taken as highly significant.
Results
There were 100 SS and AS patients; and 40 AA (control). Group A: SS, comprised 49 (49%) children and 21 (21%) adults, with age range between two and 42 years.(Fig. 1A) Slight female preponderance with 53 (53%) females and 47 (47%) males was seen.(Fig. 1B) Forty-five subjects were symptomatic at presentation and 40 had a high frequency of hospital admissions. (Fig. 2) One of the symptomatic patients of SS had the reading of max PA% with all the agonists being displayed as ‘HIGH NOISE’, thus was excluded from the analysis, resulting in 44 patients remaining in symptomatic subgroup. Most SS patients presenting with symptoms were diagnosed with VOC (painful crisis) (six), anemia (two), or infections (three patients). (Table 1).
In Group B: AS, 13 subjects were symptomatic at presentation and five had a high frequency of hospital admissions. (Table 2).
In the control group, the max PA% with ADP, collagen, epinephrine, and ristocetin was 93.17 ± 6.07%, 90.89 ± 5.24%, 87.48 ± 5.78% and 92.50 ± 11.0% respectively(Table 2).
The max PA% with ADP was less in SS patients in steady state, which was even lesser in those having symptoms, complications in past or present, high-frequency hospital admission and > 2 blood transfusions per year subgroups, as compared to all others in group and subgroup analyses. This reduction was statistically highly significant as well (p < 0.001). With Collagen and Epinephrine similar significant difference was found in SS patients with clinical risk factors but not in AS with clinical risk factors. Also, the max PA% with ristocetin was least in SS (36.833 ± 39.825%) as compared to AS (78.666 ± 26.097%) and AA (92.498 ± 10.999%). There was a significant reduction in the PA with ADP (p value < 0.05) and Ristocetin in SS patients with complications as compared with steady state patients. (Table 2).
There was no consistent statistically significant difference in PT and aPTT values of the three groups as well as among the various subgroups of SS and AS groups. The mean values of PT were prolonged in SS and AS patients. However, mean values of PT and aPTT did not show significant differences or prolongation in SS and AS patients with complication or with other clinical risk factors than rest subgroups. (Table 3).
In the SS patients presenting with joint pain (36) the PA ADP ranged from 5.98% to 131.90%, with more number of patients in > 70% (12), 41–60% (14) and < 30% (eight) ranges. (Fig. 3).
Discussion
Large interest has been generated in the possible role of platelets and clotting factors in the pathogenesis of complications of SCD with conflicting reports in most works, possibly owing to the different settings in which they were done.
Platelet Aggregation Studies
The max PA% in steady state SS has been found to be normal, values similar to that of control (AA) patients, concordant to previous works [2] and in contrast to others [3, 8, 12]. Decreased PA in SS during the complication phase as compared to steady state is concordant to many previous works [9]. It has been suggested that there is increased in vivo platelet activation and secretion during complications, as indicated by these findings, leading to depletion of platelet granule stores, thus in turn causing reduced responsiveness to platelet aggregating agents in vitro [8]. However, few researchers have found no significant difference in max PA% in these two phases [8].
Also, statistically significant lower values of PA are present in SS patients with clinical risk factors: presence of complications in the present/past and requiring > 3 hospital admission/ year. This difference is present with all the agonists including ADP, collagen, epinephrine and Ristocetin. In contrast, AS patients with these clinical risk factors have significantly lower values of PA with only ADP, and not with collagen and epinephrine. This might be explained as:
Adenosine diphosphate (ADP), an intermediate platelet agonist (agonist: chemical stimulus whose exposure is rapidly followed by platelet activation), requires granule secretion for full irreversible aggregation. The sources of ADP are multiple: platelet-dense granules upon platelet activation and from red blood cells and damaged endothelial cells; probably resulting in the consistent finding of decreased PA with ADP in almost all studies on this topic, including ours and in SS as well as AS patients with various clinical risk factors also [13].
Collagen, a strong agonist, can produce aggregation independent of platelet granule secretion, rather resulting from endothelial damage exposing the extracellular matrix protein collagen [14]. In SS patients there might be endothelial damage exposing collagen due to the greater severity of complications as compared to AS patients in addition to platelets activation degranulation and ADP secretion. This might lead to no significant difference in PA with collagen in AS patients with and without clinical risk factors, in contrast to the SS ones.
Epinephrine is effective only at supraphysiological concentrations as it is a weak agonist and requires other agonists to induce full platelet aggregation [15]. The platelet aggregation thus might not have shown a significant decrease again in the AS patients with clinical risk factors.
The preliminary result of Ristocetin-induced platelet aggregation (RIPA) is decreased RIPA in SS patients with complications. The earlier studies were done only in SCA patients in steady state, with the RIPA being absent to reduced [13, 16, 17]. One of these studies had this finding confirmed in the black patients [17], while the other two were not mentioning or correlating the findings with race and ethnicity [13, 16]. According to all of them, rather the differences in RIPA could not be explained by age, gender, presence of sickle haemoglobin, or medications. The possibility of the presence of a plasma inhibitor of RIPA [16], or some component competing for available Ristocetin [13], was suggested on the basis of the mixing studies done by them. As the ethnicity of subjects is different in the present work and the sample size for RIPA is too small, it should be worked on with larger number of patients.
PT and aPTT
The mean values of PT and aPTT were not showing significant differences or prolongation in SS and AS patients with complications at presentation when compared with those in steady state at present. Also, these parameters were in the normal range in all the clinical subgroups. This is in contrast to the conflicting reports present on the coagulation profile changes in SCA patients [8,9,10, 18, 19]. Heterogeneity of the age of the subjects of the present work along with the clinical features and diagnosis may be few reasons as other works were done in either children or adults with VOC. Many have documented prolonged PT in a steady state, which has been proposed to be the result of chronic consumption of coagulation factors from the enhanced procoagulant activity and liver dysfunction from various causes resulting in decreased synthesis of these factors [20]. Whereas, the shorter values in others may be caused due to activated coagulation factors along with ongoing subclinical vaso-occlusion with attendant thrombosis at the microvascular level, leading to a vicious cycle of coagulation [2, 21]. The shorter value of aPTT was proposed as the possible explanation for the hypercoagulable nature of SCD [9, 19]. The subclinical ischemic episodes resulting from the continuous cycle of micro-vaso occlusion were suggested to cause a decrease in aPTT [19].
PA ADP in Joint Pain
In a previous work lower max PA% in the SS patients presenting in acute phase of VOC was found than the convalescence phase and steady state SS patients [3]. The max PA % of the convalescence phase and steady state SS patients was lesser than AA [3]. In present work, the max PA% in SS patients with joint pain is showing clustering of values in much lower range in some cases when compared to others [ranges: 41–60% (14 patients) and < 10–30% (8 patients)], which may in be taken as indicative of VOC rather than other causes of pain if the concurrence is drawn with above mentioned study. This in turn may help in better and timely management of the needy patients (with PA ADP < 60%). However, this hypothesis should be validated with a follow up study in such patients as all the joint pain patients were in acute phase in current work and/ or by confirming VOC diagnosis in them with help of other investigations.
Complications in Past or Present
The comparison subgroup for the SS and AS patients with complications (past/ present) was sickle cell patients without any complications ever. The values of various parameters of the second subgroup (SS and AS patients without any complications ever) may become baseline/ reference for comparison of all others and for the treatment goals. The difference in these two subgroups shows significantly lesser value of max PA with ADP in complication (past/ present) subgroup of SS and AS groups both, which may suggest chronic platelet activation secondary to long term/ constant increased concentration of ADP in blood in them.
Scope of Antiplatelet Drugs
Most of the trials did not correlate the in vivo effect of the drugs on platelet activation with clinical endpoints, with noteworthy drugs studied being eptifibatide and prasugrel [22,23,24,25,26]. The trials of prasugrel (platelet P2Y12 ADP antagonist) showed non-significant reduction in the rate and intensity of pain [27] and no significant difference in the rate of the VOC, again indicating the role of other agonists and mechanisms causing platelet activation.
Scope of Drugs Inhibiting Coagulation Factors
Various animal studies with blockade of factor Xa or thrombin suggest that diminution of coagulation activation in SCD significantly reduces coagulation activation, thrombin-antithrombin complexes (TAT), local tissue inflammation as well as systemic and vascular injury; in turn, decreasing end-organ damage [28,29,30].
Limitations of Present Work
In spite of the considerable sample size, the findings of the present study are only suggestive of possibilities, owing to its design of being a cross-sectional study, which need to be confirmed with follow-up studies.
Conclusion
The consistent statistically significant decrease in PA with ADP found in SS and AS patients with complications and other clinical risk factors, which was not seen with collagen and epinephrine, may indicate that SCD patients can be monitored by using PA with ADP alone for their timely and better management. Thus, PA with ADP if added to the workup will improve prognostication of these patients. The virtually absent RIPA in SS patients with clinical risk factors indicates presence of some inhibitor of RIPA in plasma, the determination of which may be useful in predicting the worse outcome. The values of various parameters of the SS and AS patients without any clinical risk factors found in this study may act as a reference range for the treatment goals, as there are almost no works mentioning such data from this region.
References
Villagra J, Shiva S, Hunter LA, Machado RF, Gladwin MT, Kato GJ (2007) Platelet activation in patients with sickle disease, hemolysis-associated pulmonary hypertension and nitric oxide scavenging by cell-free hemoglobin. Blood 110:2166–2172. https://doi.org/10.1182/blood-2006-12-061697
Alhawiti NM (2021) Hemostatic alteration in sickle cell disease: pathophysiology of the hypercoagulable state. King Khalid Univ J Health Sci 6:1–5
Mehta P, Mehta J (1980) Abnormalities of platelet aggregation in sickle cell disease. J Pediatr 96(2):209–213. https://doi.org/10.1016/s0022-3476(80)80804
Platt OS, Thorington BD, Brambilla DJ, Milner PF, Rosse WF, Vichinsky E et al (1991) Pain in sickle cell disease. N Engl J Med 325:11–16. https://doi.org/10.1056/NEJM199107043250103
Wang WC, Lukens JN (1998) Sickle cell anemia and other sickling syndromes. In: Lee R, Lukens J, Greer JP, Rodgers GM, Paraskevas F, Foerster J (eds) Wintrobe’s clinical hematology. Williams & Wilkins, pp 1346–1397
Miller ST, Sleeper LA, Pegelow CH, Enos LE, Wang WC, Weiner SJ et al (2000) Predicting adverse outcomes in children with sickle cell disease: a report from the cooperative study (CSSCD). N Engl J Med 342:83–89. https://doi.org/10.1056/NEJM200001133420203
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, Klug PP (1994) Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med 330:1639–1644. https://doi.org/10.1056/NEJM199406093302303
Bashawri LA, Al-Mulhim AA, Ahmed MA, Bahnassi AA (2007) Platelet aggregation and physiological anticoagulants in sickle-cell disease. East Mediterr Health J 13(2):266–272 (PMID: 17684847)
Gupta GK, Sarkar PD, Manyal R, Rajput MS (2022) Sickle cell disease: Assessment of hemostasis parameters in steady-state patients at tertiary care hospital, Indore. India Biomed Biotechnol Res J 6:81–85. https://doi.org/10.4103/bbrj.bbrj_162_21
Chinawa JM, Emodi IJ, Ikefuna AN, Ocheni S (2013) Coagulation profile of children with sickle cell anemia in steady state and crisis attending the university of Nigeria teaching hospital, Ituku-Ozalla, Enugu. Niger J Clin Pract 16:159–163. https://doi.org/10.4103/1119-3077.110132
Dacie JV, Lewis SM (1994) Practical hematology, 8th edn. Churchill Livingstone, Edinburg, pp 320–325
Sarji KE, Eurenius K, Fullwood CO, Schraibman HB, Colwell JA (1979) Abnormalities of platelet aggregation in sickle cell anemia. Presence of a plasma factor inhibiting aggregation by ristocetin. Thromb Res 14(2–3):283–297. https://doi.org/10.1016/0049-3848(79)90238-x
Woulfe D, Yang J, Brass L (2001) ADP and platelets: the end of the beginning. J Clin Invest 107(12):1503–1505. https://doi.org/10.1172/JCI13361
Sixma JJ, van Zanten GH, Huizinga EG, van der Plas RM, Verkley M, Wu YP et al (1997) Platelet adhesion to collagen: an update. Thromb Haemost 78:434–438 (PMID: 9198192)
Lanza F, Beretz A, Stierlé A, Hanau D, Kubina M, Cazenave JP (1988) Epinephrine potentiates human platelet activation but is not an aggregating agent. Am J Physiol 255(6):H1276–H1288. https://doi.org/10.1152/ajpheart.1988.255.6.H1276
Leichtman DA, Brewer GJ (1977) A plasma inhibitor of ristocetin-induced platelet aggregation in patients with sickle hemoglobinopathies. Am J Hematol 2(3):251–258. https://doi.org/10.1002/ajh.2830020307
Buchanan GR, Holtkamp CA, Levy EN (1981) Racial differences in ristocetin-induced platelet aggregation. Br J Haematol 49(3):455–464. https://doi.org/10.1111/j.13652141.1981.tb07249.x
Raffini LJ, Niebanck AE, Hrusovsky J, Stevens A, Blackwood-Chirchir A, Ohene-Frempong K et al (2006) Prolongation of the prothrombin time and activated partial thromboplastin time in children with sickle cell disease. Pediatr Blood Cancer 47:589–593. https://doi.org/10.1002/pnc.20579
Kusfa IU, Aminu SM, Mamman AI, Hassan A, Babadoko AA, Mohammed MH et al (2018) Basic hemostatic parameters in adults with sickle cell anemia at Ahmadu Bello University Teaching Hospital. Zaria Nigeria Sahel Med J 21:157–161. https://doi.org/10.4103/smj.smj_2_17
Kotila T, Adedapo K, Adedapo A, Oluwasola O, Fakunle E, Brown B (2005) Liver dysfunction in steady state sickle cell disease. Ann Hepatol 4:261–263 (PMID: 16432491)
Stathakis NE, Papayannis AG, Papayotas H, Scliros P, Gardakis C (1975) Hypercoagulability and hypofibrinolysis in sickle cell disease. Ann Hematol 31:355–364. https://doi.org/10.1007/BF01634001
Heeney MM, Hoppe CC, Abboud MR, Inusa B, Kanter J, Ogutu B et al (2016) A multinational trial of prasugrel for sickle cell vaso-occlusive events. N Engl J Med 374:625–635. https://doi.org/10.1056/NEJMoa1512021
Wun T, Soulieres D, Frelinger AL, Krishnamurti L, Novelli EM, Kutlar A et al (2013) A double-blind, randomized, multicenter phase 2 study of prasugrel versus placebo in adult patients with sickle cell disease. J Hematol Oncol 6:17. https://doi.org/10.1186/1756-8722-6-17
Desai PC, Brittain JE, Jones SK, McDonald A, Wilson DR, Dominik R et al (2013) A pilot study of eptifibatide for treatment of acute pain episodes in sickle cell disease. Thromb Res 132:341–345. https://doi.org/10.1016/jthromres.2013.08.002
Semple MJ, Al-Hasani SF, Kioy P, Savidge GF (1984) A double-blind trial of ticlopidine in sickle cell disease. Thromb Haemost 51:303–306 (PMID: 6388012)
Zago MA, Costa FF, Ismael SJ, Tone LG, Bottura C (1984) Treatment of sickle cell diseases with aspirin. Acta Haematol 72:61–64. https://doi.org/10.1159/000206360
Noubouossie D, Key NS, Ataga KI (2016) Coagulation abnormalities of sickle cell disease: relationship with clinical outcomes and the effect of disease modifying therapies. Blood Rev 30(4):245–256. https://doi.org/10.1016/j.blre.2015.12.003
Sparkenbaugh EM, Chantrathammachart P, Mickelson J, van Ryn J, Hebbel RP, Monroe DM et al (2014) Differential contribution of FXa and thrombin to vascular inflammation in a mouse model of sickle cell disease. Blood 123:1747–1756. https://doi.org/10.1182/blood-2013-08-523936
Sparkenbaugh E, Pawlinski R (2013) Interplay between coagulation and vascular inflammation in sickle cell disease. Br J Haematol 162:3–14. https://doi.org/10.1111/bjh.12336
Arumugam PI, Mullins ES, Shanmukhappa SK, Monia BP, Loberg A, Shaw MA et al (2015) Genetic diminution of circulating prothrombin ameliorates multiorgan pathologies in sickle cell disease mice. Blood 126:1844–1855. https://doi.org/10.1182/blood-2015-01-625707
Acknowledgements
We are greatful to Dr W. K. Raut, ex Professor and Head of Department of Pathology, GMCH, Nagpur for his unrelenting support and guidance for this work.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by VBN, PMK and SSR. The first draft of the manuscript was written by VBN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical Approval
The study was approved by the institutional ethics committee (Government medical college, Nagpur). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments comparable ethical standards.
Informed Consent
A written informed consent to participate in the study was obtained from all the participants or their parent or legal guardian in the case of children under 16 years of age.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagose, V.B., Kodate, P.M., Kumbhalkar, D.T. et al. Platelet Aggregation Studies and Coagulation Profile in Sickle Cell Disease in Symptomatic and Steady State Patients. Indian J Hematol Blood Transfus 40, 281–288 (2024). https://doi.org/10.1007/s12288-023-01703-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-023-01703-9