Abstract
Background
The relationship between obesity and prognosis of early breast cancer is complex. Increased levels of aromatase present in adipose tissue of obese postmenopausal women may lead to suboptimal suppression of systemic estrogens. However, studies have been mixed with respect to the association between use of aromatase inhibitors (AIs) and clinical outcomes in obese women with early breast cancer.
Methods
We conducted a systematic literature review following PRISMA guidelines to examine the impact of obesity on the efficacy of AIs in early-stage hormone receptor-positive breast cancer. Primary outcome measures included disease-free survival, relapse-free survival, distant recurrence-free survival, breast cancer-free survival, and overall survival.
Results
Of 491 studies identified, eight studies met criteria for inclusion: three retrospective cohort studies, one prospective cohort study and four randomized controlled trials. Four studies limited eligibility to postmenopausal women. Percentage of obese patients in studies ranged from 10 to 30%. Two studies examined use of AIs alone while the remainder included patients treated with either AIs or tamoxifen. Five out of seven studies suggested a negative impact of obesity on AI efficacy.
Conclusions
The results of our systematic review highlight a need for further research exploring the optimal endocrine therapies for obese women. There is insufficient evidence at present to recommend tailoring adjuvant endocrine therapy with use of specific AIs or for dosing modifications of AIs in this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity, defined as a body mass index (BMI) greater than or equal to 30 kg/m2, according to the WHO classification, is associated with an increased risk of breast cancer [1, 2]. In a large prospectively studied cohort of U.S. adults, obesity was associated with increased mortality from a number of solid tumors, including breast cancer [3, 4]. While there are many possible underlying reasons for a worsened prognosis including the negative impact of increased body mass on tumor biology [5,6,7,8,9], the type of adjuvant endocrine therapy used in obese breast cancer patients may play an important role [10, 11]
Both tamoxifen and AIs are commonly used adjuvant endocrine therapies in breast cancer [12, 13]. AIs are often the preferred treatment for postmenopausal women and are combined with ovarian suppression in premenopausal women. However, there is a lack of large prospective randomized studies examining the impact of the type of endocrine therapy on clinical outcomes for obese breast cancer patients. Although endocrine therapies such as AIs and tamoxifen are not dosed according to BMI, standard treatment doses may not be sufficient to antagonize circulating estrogens in obese women [14]. This is possibly due to the higher levels of aromatase in peripheral fatty tissue of obese women [15, 16]. Since obesity is associated with increased adipose tissue and aromatase activity (the target of AIs), there is concern that these agents may be less effective in women who are overweight or obese [10]. However, the literature is mixed on this association [17,18,19,20,21,22,23,24] and there are no specific recommendations regarding use of adjuvant AIs in this patient population. Therefore, we performed a systematic review of observational cohort studies and interventional clinical trials to examine the impact of obesity on clinical outcomes for women treated with adjuvant aromatase inhibitors versus tamoxifen for early breast cancer.
Materials and methods
Data sources
A systematic review was conducted based on the guidelines outlined in The PRISMA Statement [25], using the databases Medline (January 1946–July 2019), EMBASE (January 1947–2019 Week 29), and the Cochrane Central Database on Controlled Trials (June 2019). The following Search terms were used: breast neoplasms; obesity; estrogens; receptor, estrogens; neoplasm recurrence, local. Subject headings and keywords were modified for each database according to its unique indexing terms. The search (Supplementary Tables 1–3) was conducted by a medical information specialist and limited to humans, without language restrictions. Reference lists of retrieved articles were also screened for additional relevant studies.
Study selection
The aim of this systematic review was to examine clinical outcomes for obese patients treated with AIs for early breast cancer. Inclusion criteria included women with hormone receptor-positive (HR +) breast cancer on treatment with AIs in which BMI was recorded. Primary outcome measures included disease-free survival (DFS), relapse-free survival (RFS), distant recurrence-free survival (DFRS), breast cancer-free survival (BCFS), and overall survival (OS). Secondary outcome measures were not included in selection of studies. Studies were excluded if the patient population did not include early breast cancer patients; if trials were evaluating systemic therapies other than endocrine therapies; if trials did not report clinical outcomes for obese breast cancer patients on adjuvant AIs or if duplicate data were reported. Only studies in English language were included. Included publication types were published and unpublished studies including peer-reviewed publications and conference abstracts in which full study results could be obtained. When full articles were not available, the authors were contacted and full-study publications requested. If full publication could not be obtained, the conference abstract was excluded. Editorials, letters, commentaries, reviews, case series, case reports and case–control studies were excluded.
One reviewer (MS) selected potentially eligible studies by independently screening titles and abstracts of identified studies following literature searches on the three chosen databases. A second reviewer (RCP) confirmed the selection of eligible studies. Full texts of the studies identified were subsequently retrieved and independently assessed for eligibility by two reviewers (MS and RCP).
Data extraction
Data from selected studies were then independently extracted by the two study authors (MS and RCP) using duplicate Excel spreadsheets. The data extracted included information on study author, date of publication, article title, type of publication, study design, inclusion/exclusion criteria, age, gender, disease characteristics, number of participants enrolled on each study arm, measurement tool or methods used, setting, intervention and control, description of interventions, analysis units, statistical tests used, pre-specified outcomes, length of follow-up, summary of outcomes data and additional outcomes of the included studies for the purposes of this systematic review.
Risk of bias assessment
The Cochrane Risk of Bias Tool for Randomized Controlled Trials 2.0 (RoB 2.0) was used to assess the quality of included studies. In this checklist tool, domains pertaining to randomized studies only were indicated as “not applicable” for the analysis of the four cohort studies. The RoB 2.0 rates studies as “low risk”, “unclear risk” or “high risk” of bias using pre-established criteria to evaluate both study design and applicability. Risk of bias was determined by a single reviewer (RCP).
Results
Our search yielded a total of 491 publications of which 40 were duplications. 419 studies were excluded with reasons after reviewing the abstracts and titles. For the remaining 32 studies, full manuscripts were retrieved and assessed for eligibility of which 24 were excluded with reasons and 8 articles met inclusion criteria (Fig. 1 PRISMA flow diagram). Study characteristics are summarized in Table 1. Comparison of study outcomes based on treatment are shown in Table 2. Included studies were deemed to have a low risk of bias (Supplementary Data Fig. 1).
Three studies focused on treatment with anastrozole specifically and reported a difference in efficacy of anastrozole according to BMI. Pfeiler et al. [26] retrospectively analyzed premenopausal patients from ABCSG-12 trial to investigate the influence of BMI on the efficacy of adjuvant endocrine therapy. ABCSG-12 examined the efficacy of goserelin in combination with anastrozole or tamoxifen with or without zoledronic acid in premenopausal women with HR + breast cancer. They compared overweight and obese patients (BMI ≥ 25 kg/m2) with normal weight patients (BMI 18.5–24.9 kg/m2) and found that overweight patients treated with anastrozole had a 60% increase in the risk of disease recurrence (HR 1.60; 95% CI 1.06–2.41; P = 0.02) and more than a doubling in the risk of death (HR 2.14; 95% CI 1.17–3.92; P = 0.01) compared with normal weight patients treated with anastrozole. In contrast, BMI showed no prognostic impact in patients treated with tamoxifen. In tamoxifen-treated patients, DFS (HR 0.94; 95% CI 0.60–1.64; P = 0.76) and OS (HR 0.83; 95% CI 0.35–1.93; P = 0.65) were not significantly different between normal weight patients and overweight patients.
Sestak et al. [21] retrospectively analyzed data from the ATAC trial, which randomized women HR + early breast cancer to either anastrozole or tamoxifen, to investigate the effect of BMI on treatment efficacy. They found that anastrozole was more effective than tamoxifen across all BMI groups. Recurrence rate in the anastrozole group was significantly lower than the tamoxifen-treated group. However, this benefit was non-significantly greater in thinner women (BMI < 23 kg/m2) for all recurrences compared to obese women (BMI ≥ 30 kg/m2) (HR 0.64, 95% CI 0.45–0.91). Anastrozole was significantly less effective in postmenopausal women with a BMI higher than 30 kg/m2 compared to those women with a BMI lower than 28 kg/m2 (P = 0.01), while the efficacy of tamoxifen was comparable across all BMI groups (P = 0.54). Moreover, women with a high BMI (BMI ≥ 35 kg/m2) had a significantly higher rate of breast cancer recurrences compared to those women with a low BMI (HR 1.39; 95% CI 1.06–1.82).
Gnant et al. [23] retrospectively investigated the impact of BMI on disease outcome from the ABCSG-6a trial, in which postmenopausal HR + early breast cancer patients were randomly assigned to receive either 3 years of anastrozole or no further treatment. DFS and OS were compared in obese and overweight patients (BMI ≥ 25 kg/m2) versus normal weight and underweight patients (BMI < 25 kg/m2). No difference was found in DFS (HR 1.05; 95% CI 0.75–1.49, P = 0.76) and OS (HR 1.05; 95% CI 0.67–1.64, P = 0.83) between these BMI groups. The two BMI groups were also compared according to treatment arm. In the control group, no difference was observed between the two BMI groups with regards to DFS (HR 0.79; 95% CI 0.52–1.23, P = 0.3) and OS (HR 0.81; 95% CI 0.47–1.4, P = 0.45). However, in the group treated with additional anastrozole, overweight and obese patients had a non-significant worse DFS compared with normal weight patients (HR 1.55; 95% CI 0.87–2.77, P = 0.14), and a non-significant worse OS (HR 1.58; 95% CI 0.72–3.49, P = 0.25).
In contrast, two studies that focused on postmenopausal women treated with letrozole reported no difference in efficacy of this drug between obese and non-obese patients. In a retrospective cohort study, Sendur et al. [27] compared the efficacy of anastrozole or letrozole in overweight and obese (BMI ≥ 25 kg/m2) versus normal weight (BMI < 25 kg/m2) postmenopausal women with HR + breast cancer, and found no difference in DFS. Both letrozole- and anastrozole-treated patients had similar DFS and OS rates in normal weight patients, overweight and obese patients. Analysis of DFS according to BMI also revealed a non-significant difference between BMI < 25 kg/m2 and BMI ≥ 25 kg/m2 patients (P = 0.08).
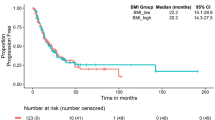
Ewertz et al. [22] performed a sub-analysis of the BIG 1–98 trial in which 4760 postmenopausal women with HR + early breast cancer were randomly assigned to receive 5 years of monotherapy with either letrozole or tamoxifen. They compared DFS and OS outcomes for obese patients (BMI ≥ 30 kg/m2) versus normal weight patients (BMI < 25 kg/m2) and efficacy of endocrine therapy. OS was worse for obese patients (HR 1.19; 95% CI 0.99–1.44) compared to normal weight patients, but there was no significant difference in DFS between these two groups. Analysis by treatment showed no significant difference between obese and normal weight patients in OS (P = 0.74) and DFS (P = 0.89) for both the letrozole- and tamoxifen-treated groups.
Three studies assessed efficacy of AI (type not specified) versus tamoxifen, two of which found an inferior AI efficacy in patients with higher BMI. Similarly, in a prospective cohort study, Wisse et al. [28] analyzed 1640 patients with primary breast cancer to investigate the impact of preoperative BMI on breast cancer-free interval and OS. They found that patients ≥ 50 years with ER + tumors and BMI ≥ 25 kg/m2 had a shorter breast cancer-free interval when treated with tamoxifen (HR 1.72; 95% CI 1.00–2.95; P = 0.032) or an AI (HR 1.71; 95% CI 0.91–3.20; P = 0.055) compared to patients with a lower BMI. These patients also had a shorter OS when treated with tamoxifen (HR 2.28; 95% CI 1.29–4.03; P = 0.001) or AIs (HR 1.75; 95% CI 0.92–3.30; P = 0.019) compared to patients with lower BMI.
Similarly, in a retrospective analysis, Wolters et al. [29] compared efficacy of AI and tamoxifen based on BMI without specifying the type of AI used. They examined 4636 patients with primary breast cancer, 74.6% of which were postmenopausal and 84% of whom had HR + tumors. RFS and efficacy of endocrine therapy was compared in obese (BMI ≥ 30 kg/m2) and non-obese (BMI < 30 kg/m2) patients. They found that in contrast to tamoxifen, AI efficacy was dependent on BMI. A non-significant RFS benefit was observed for AI versus tamoxifen in the non-obese patients (HR 1.29, 95% CI 0.63–2.62); whereas there was an RFS benefit for tamoxifen versus AI in the obese group (HR 0.65, 95% CI 0.29–1.45).
In contrast, Jiralerspong et al. [30] assessed outcomes for 6342 breast cancer patients with a median follow-up of 5.4 years and found that overweight and obese groups (BMI > 25 kg/m2) had significantly worse RFS (P = 0.01) and OS (P = 0.004) in patients treated with tamoxifen, but not in patients treated with AI (RFS P = 0.74, OS P = 0.58).
Discussion
Five out of eight included studies suggest a positive association between high BMI and inferior breast cancer outcomes in patients treated with AIs. Most studies only included postmenopausal patients, but a single study focused on premenopausal women and also found a positive association between higher BMI and decreased AI efficacy.
Obesity is associated with poor breast cancer prognosis in both premenopausal and postmenopausal women [31,32,33]. In ER + breast cancer patients, the outcome can be improved through inhibition of the estrogen receptor with drugs such as tamoxifen or through decreasing estrogen production with AIs. AIs have been shown to be more effective than tamoxifen in improving the disease-free (or recurrence-free) outcomes in postmenopausal early breast cancer patients [13]. In obese postmenopausal women, increased production of estrogen by aromatase in excess adipose tissue is associated with higher estrogen levels. These patients may require higher doses of AIs for sufficient estrogen suppression. However, AIs are currently not dosed according to body weight and the same dose of a particular AI is prescribed for all patients [19]. Evidence suggests that AIs (particularly letrozole) may be more beneficial than tamoxifen in postmenopausal women regardless of BMI, although this benefit may be smaller in overweight and obese women [34]. Our results provide further support for these findings with an overall trend toward a negative impact of obesity on clinical outcomes with anastrozole but not with letrozole treatment.
The impact of obesity on AI efficacy in early breast cancer deserves further investigation as there were only a handful of studies that we were able to identify that specifically focused on this question. Furthermore, it is important to investigate whether the impact of obesity on AI efficacy is specific to the AI used for treatment. Analyses of the ABCSG-12 [26], ATAC [21], and ABCSG-6a [24] trials by BMI, found a significant decrease in efficacy of anastrozole in patients with higher BMI. In contrast, the studies by Sendur et al. [27] and Ewertz et al. [22], which investigated use of letrozole, found no difference in outcomes across BMI groups. These findings have led to the notion that the impact of BMI on AI efficacy may be drug dependent. Indeed, third-generation AIs (letrozole, anastrozole, and exemestane) are not equipotent. It has been found that letrozole is 10–30 times more potent than anastrozole in its ability to inhibit intracellular aromatase and is also used at a 2.5-fold higher dose [35, 36]. Letrozole is in fact a more potent estrogen suppressor than either anastrozole or exemestane [37]. This could account for the studies with letrozole as the AI showing little or no difference in outcomes compared to studies using anastrozole.
There are a few limitations to note in our systematic review. Significant variability in study factors limit our ability to combine the study results in a meta-analysis to draw generalized conclusions. The definition of obesity and the comparison groups varied significantly amongst the included studies. In our opinion, obesity should be defined as per the World Health Organization (WHO) guidelines, in which obesity is defined as a BMI of 30 kg/m2 or higher. While the majority of studies followed the WHO classification of BMI to compare obese (BMI ≥ 30 kg/m2) patients to normal weight (BMI 18.5–24.9 kg/m2) patients [22, 26, 30], one study compared obese (BMI ≥ 30 kg/m2) versus non-obese (BMI < 30 kg/m2) patients [29]. Some studies included overweight and obese patients together in one group (BMI ≥ 25 kg/m2) and compared them to normal weight (BMI 18.5–24.9 kg/m2) patients [24, 27, 28]. The study by Sestak et al.[21] followed a different classification and compared women with a ‘low’ BMI (BMI < 23 kg/m2) with either morbidly obese (BMI ≥ 35 kg/m2) or obese (BMI 30–35 kg/m2) women.
Differences in patient populations included further impact on the clinical outcome data and limited the ability to pool study results. Included studies differed in terms of menopausal status, presence of comorbidities, and the treatment regimens used. While majority of the studies included both premenopausal and postmenopausal women, four studies only included postmenopausal patients [21, 22, 24, 27], and one study [26] only included premenopausal women. Whether there may be a differential impact of obesity in postmenopausal women on AI alone versus premenopausal women on the combination of AI and ovarian suppression is unknown.
Use of adjuvant chemotherapy also differed significantly among the studies and may further account for the observed differences in clinical outcomes in the studies. Perhaps differential dosing of chemotherapy in obese versus non-obese patients may have played an important role in the variability of survival outcomes across studies.
In conclusion, despite the observed poorer survival outcomes in obese versus non-obese women noted in our review, there is not sufficient evidence at present to suggest that obese women have inferior outcomes on AIs versus tamoxifen. Selection of optimal adjuvant endocrine therapies must also take into account the risk–benefit ratio. The risk of common AI toxicities such as joint symptoms [38] and cardiovascular effects [39] may be higher in obese compared to normal weight women. This may result in lower compliance to AI in obese women, and therefore, potentially translate to poorer clinical outcomes in this population. Future prospective studies are needed to better understand the efficacy and toxicities of AIs in obese women and to determine whether specific AIs or altered dosage of these drugs would benefit obese patients.
Abbreviations
- AI:
-
Aromatase inhibitor
- BMI:
-
Body mass index
- DFS:
-
Disease-free survival
- RFS:
-
Relapse-free survival
- DFRS:
-
Distant recurrence-free survival
- BCFS:
-
Breast cancer-free survival
- OS:
-
Overall survival
- ER:
-
Estrogen receptor
- HR:
-
Hormone receptor
References
Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet. 2008;371:10.
Cleary MP, Grossmann ME. Obesity and breast cancer: the estrogen connection. Endocrinology. 2009;150:2537–42. https://doi.org/10.1210/en.2009-0070.
Petrelli JM, Calle EE, Rodriguez C, Thun MJ. Body mass index, height, and postmenopausal breast cancer mortality in a prospective cohort of US women. Cancer Causes Control. 2002;13(4):325–332. https://doi.org/10.1023/a:1015288615472.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–1638. https://doi.org/10.1056/NEJMoa021423.
Niraula S, Ocana A, Ennis M, Goodwin PJ. Body size and breast cancer prognosis in relation to hormone receptor and menopausal status: a meta-analysis. Breast Cancer Res Treat. 2012;134:769–81. https://doi.org/10.1007/s10549-012-2073-x.
Daling JR, Malone KE, Doody DR, Johnson LG, Gralow JR, Porter PL. Relation of body mass index to tumor markers and survival among young women with invasive ductal breast carcinoma. Cancer. 2001;92(4):720–729. https://doi.org/10.1002/1097-0142(20010815)92:4<720::aid-cncr1375>3.0.co;2-t.
Loi S. Obesity and outcomes in premenopausal and postmenopausal breast cancer. Cancer Epidemiol Biomark Prev. 2005;14:1686–91. https://doi.org/10.1158/1055-9965.EPI-05-0042.
Whiteman MK. Body mass and mortality after breast cancer diagnosis. Cancer Epidemiol Biomark Prev. 2005;14:2009–14. https://doi.org/10.1158/1055-9965.EPI-05-0106.
Abrahamson PE, Gammon MD, Lund MJ, et al. General and abdominal obesity and survival among young women with breast cancer. Cancer Epidemiol Biomark Prev. 2006;15:1871–7. https://doi.org/10.1158/1055-9965.EPI-06-0356.
Azrad M, Demark-Wahnefried W. The association between adiposity and breast cancer recurrence and survival: a review of the recent literature. Curr Nutr Rep. 2014;3:9–15. https://doi.org/10.1007/s13668-013-0068-9.
Ioannides SJ, Barlow PL, Elwood JM, Porter D. Effect of obesity on aromatase inhibitor efficacy in postmenopausal, hormone receptor-positive breast cancer: a systematic review. Breast Cancer Res Treat. 2014;147:237–48. https://doi.org/10.1007/s10549-014-3091-7.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. The Lancet. 2011;378:771–84. https://doi.org/10.1016/S0140-6736(11)60993-8.
Dowsett M, Coombes RC. Second generation aromatase inhibitor ? 4-hydroxyandrostenedione. Breast Cancer Res Treat. 1994;30:81–7. https://doi.org/10.1007/BF00682742.
Lønning PE, Haynes BP, Dowsett M. Relationship of body mass index with aromatisation and plasma and tissue oestrogen levels in postmenopausal breast cancer patients treated with aromatase inhibitors. Eur J Cancer. 2014;50:1055–64. https://doi.org/10.1016/j.ejca.2014.01.007.
Morris PG, Hudis CA, Giri D, et al. Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev Res. 2011;4:1021–9. https://doi.org/10.1158/1940-6207.CAPR-11-0110.
Subbaramaiah K, Howe LR, Bhardwaj P, et al. Obesity Is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res. 2011;4:329–46. https://doi.org/10.1158/1940-6207.CAPR-10-0381.
Gérard C, Brown KA. Obesity and breast cancer—role of estrogens and the molecular underpinnings of aromatase regulation in breast adipose tissue. Mol Cell Endocrinol. 2018;466:15–30. https://doi.org/10.1016/j.mce.2017.09.014.
Goodwin PJ. Obesity and breast cancer—what’s new? Expert Rev Endocrinol Metab. 2017;12:35–43. https://doi.org/10.1080/17446651.2017.1253470.
Goodwin PJ, Pritchard KI. Obesity and hormone therapy in breast cancer: an unfinished puzzle. JCO. 2010;28:3405–7. https://doi.org/10.1200/JCO.2010.29.5113.
Lohmann AE, Goodwin PJ. Moving forward with obesity research in breast cancer. The Breast. 2017;32:225–6. https://doi.org/10.1016/j.breast.2016.11.004.
Sestak I, Distler W, Forbes JF, et al. Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. JCO. 2010;28:3411–5. https://doi.org/10.1200/JCO.2009.27.2021.
Ewertz M, Gray KP, Regan MM, et al. Obesity and risk of recurrence or death after adjuvant endocrine therapy with letrozole or tamoxifen in the breast international group 1–98 trial. JCO. 2012;30:3967–75. https://doi.org/10.1200/JCO.2011.40.8666.
Gnant M, Mlineritsch B, Stoeger H, et al. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol. 2011;12:631–41. https://doi.org/10.1016/S1470-2045(11)70122-X.
Gnant M, Pfeiler G, Stöger H, et al. The predictive impact of body mass index on the efficacy of extended adjuvant endocrine treatment with anastrozole in postmenopausal patients with breast cancer: an analysis of the randomised ABCSG-6a trial. Br J Cancer. 2013;109:589–96. https://doi.org/10.1038/bjc.2013.367.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467. https://doi.org/10.7326/M18-0850.
Pfeiler G, Königsberg R, Fesl C, et al. Impact of body mass index on the efficacy of endocrine therapy in premenopausal patients with breast cancer: an analysis of the prospective ABCSG-12 trial. JCO. 2011;29:2653–9. https://doi.org/10.1200/JCO.2010.33.2585.
Sendur MAN, Aksoy S, Zengin N, Altundag K. Efficacy of adjuvant aromatase inhibitor in hormone receptor-positive postmenopausal breast cancer patients according to the body mass index. Br J Cancer. 2012;107:1815–9. https://doi.org/10.1038/bjc.2012.473.
Wisse A, Tryggvadottir H, Simonsson M, et al. Increasing preoperative body size in breast cancer patients between 2002 and 2016: implications for prognosis. Cancer Causes Control. 2018;29:643–56. https://doi.org/10.1007/s10552-018-1042-z.
Wolters R, Schwentner L, Regierer A, et al. Endocrine therapy in obese patients with primary breast cancer: another piece of evidence in an unfinished puzzle. Breast Cancer Res Treat. 2012;131:925–31. https://doi.org/10.1007/s10549-011-1874-7.
Jiralerspong S, Kim ES, Dong W, et al. Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol. 2013;24:2506–14. https://doi.org/10.1093/annonc/mdt224.
Majed B, Moreau T, Senouci K, et al. Is obesity an independent prognosis factor in woman breast cancer? Breast Cancer Res Treat. 2008;111:329–42. https://doi.org/10.1007/s10549-007-9785-3.
Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–35. https://doi.org/10.1007/s10549-010-0990-0.
Ayoub NM, Yaghan RJ, Abdo NM, et al. Impact of obesity on clinicopathologic characteristics and disease prognosis in pre- and postmenopausal breast cancer patients: a retrospective institutional study. Journal of Obesity. 2019;2019:1–11. https://doi.org/10.1155/2019/3820759.
Goodwin PJ. Obesity and endocrine therapy: Host factors and breast cancer outcome. The Breast. 2013;22:S44–7. https://doi.org/10.1016/j.breast.2013.07.008.
Bhatnagar AS, Brodie AMH, Long BJ, et al. Intracellular aromatase and its relevance to the pharmacological efficacy of aromatase inhibitors. J Steroid Biochem Mol Biol. 2001;76:199–202. https://doi.org/10.1016/S0960-0760(01)00050-4.
Folkerd EJ, Dixon JM, Renshaw L, et al. Suppression of plasma estrogen levels by letrozole and anastrozole is related to body mass index in patients with breast cancer. JCO. 2012;30:2977–80. https://doi.org/10.1200/JCO.2012.42.0273.
Geisler J, Haynes B, Anker G, Dowsett M, Lønning PE. Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. J Clin Oncol. 2002;20(3):751–757. https://doi.org/10.1200/JCO.2002.20.3.751.
Sestak I, Cuzick J, Sapunar F, et al. Risk factors for joint symptoms in patients enrolled in the ATAC trial: a retrospective, exploratory analysis. Lancet Oncol. 2008;9:866–72. https://doi.org/10.1016/S1470-2045(08)70182-7.
Amir E, Seruga B, Niraula S, et al. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2011;103:1299–309. https://doi.org/10.1093/jnci/djr242.
Funding
No external funding received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RCP reports receipt of speaker honoraria from Pfizer and Novartis, research funding from Merck and serves on advisory boards for Astra Zeneca, Exact Sciences, Myriad Genetics, Lilly, Pfizer and Novartis, all outside the submitted work. MS reports no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

About this article
Cite this article
Shirdarreh, M., Pezo, R.C. Impact of obesity on clinical outcomes in hormone receptor-positive breast cancer: a systematic review. Breast Cancer 28, 755–764 (2021). https://doi.org/10.1007/s12282-020-01213-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-020-01213-w