Abstract
The role of vitamin D as a predictor of postoperative hypocalcemia after total thyroidectomy (TT) has variable reports as it is latitude and population specific. This cohort study in South India evaluated the impact of preoperative serum 25-hydroxycholecalciferol (25OHD) levels on transient and permanent hypocalcemia (> 6 months) post-TT. Consecutive patients (n = 327; median age = 34 years; man:woman = 65:262) undergoing TT for benign or malignant thyroid diseases were evaluated for serum corrected calcium, intact parathormone and 25OHD (categorized as severe deficiency < 10; deficiency = 10–19.9; insufficiency = 20–29.9; sufficiency = 30–100 ng/mL) at baseline, 48-h and 6-month post-TT. The incidence of transient and permanent hypocalcemia (calcium < 8 mg/dL) post-TT was 33.3% and 7.9%, respectively, and preoperatively 13%. Patients with 25OHD severe deficiency (n = 44), deficiency (n = 131) and insufficiency (n = 109) had 20.2, 4.4 and 4.1 times higher odds of developing transient hypocalcemia, while preoperative hypocalcemia, malignancy, hyperthyroidism, thyroiditis and transient hypoparathyroidism were other significant predictors. Major determinants of permanent hypocalcemia were severe 25OHD deficiency and permanent hypoparathyroidism (each P < 0.05). In receiver operating characteristic, 25OHD reliably predicted transient hypocalcemia with threshold of 18.4 ng/mL. Areas under curve, sensitivity and specificity were 0.661 (P = 0.001), 60% and 59.4%, respectively. Low preoperative calcium and 25-hydroxycholecalciferol levels, widely prevalent in our population, were independent risk factors for transient and permanent hypocalcemia after total thyroidectomy. The risk of post-thyroidectomy hypocalcemia escalated many-fold with decreasing 25-hydroxycholecalciferol levels including insufficient range and prophylactic therapy may facilitate day-care surgery. Trial registration: This study is retrospectively registered with Research Registry and the unique identifying number is Research Registry 5818.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative hypocalcemia is the most-frequent morbidity after total thyroidectomy (TT), often requiring frequent blood investigations, prolonged hospitalization and revisits [1]. Life-threatening hypocalcemic complications usually develop 24- to 48-h post-surgery dissuading surgeons from performing day-care surgery. Post-thyroidectomy hypocalcemia (PH) is mostly transient lasting less than 6 months with a reported incidence of 1.6–50%. Permanent hypocalcemia persisting beyond 6 months occurs in up to 12.1% [2]. Although hypoparathyroidism resulting from surgical handling, ischemia or inadvertent removal of parathyroid glands is the most attributed cause, other factors including advanced age, female gender, Graves’ disease, malignancy, concurrent neck dissection and surgeon’s inexperience have been associated with increased risk of PH [2, 3]. Vitamin D is a well-established calciotropic hormone involved in calcium homeostasis. Hence, many researchers investigated the role of preoperative vitamin D deficiency (VDD) in the development of PH, but with variable results. Some studies [4,5,6] supported the role of VDD as predictor of PH, while others refute [7, 8]. The major cause of VDD is inadequate sunlight exposure [9, 10]. During sun exposure, UVB photons (290–315 nm) convert 7-dehydrocholestrol (pro-vitamin D) present in the human skin into unstable pre-vitamin D3, which stabilizes to form cholecalciferol (vitamin D3). Cholecalciferol (either from skin or dietary supplements) on sequential hydroxylation in the liver and kidney produces 25-hydroxycholecalciferol (25OHD) and 1,25-dihydroxycholecalciferol (1,25(OH)2D). Although 1,25(OH)2D is the biologically active form, it has a limited utility in assessment of vitamin D status due to short half-life (4 h) and also expensive with limited availability. Serum 25OHD is the most reliable marker of vitamin D status as it is the major circulating form with half-life of about 2 weeks [11]. Various factors including time of the day, season and latitude affect the zenith angle at which UVB photons strike the earth’s surface and hence cutaneous vitamin D synthesis. Skin pigmentation, dietary habits and ethnicity also influence vitamin D status. Thus, the prevalence of VDD varies from region to region and is latitude and population specific. There is paucity of data regarding the prevalence of vitamin D deficiency in our South Indian population. A few studies have reported the impact of VDD on transient hypocalcemia in South India, and literature evidence with respect to permanent hypocalcemia after total thyroidectomy is still lacking [12]. Therefore, we conducted this cohort study to determine the incidence of preoperative vitamin D deficiency and evaluate the impact of serum 25OHD levels in the development of transient and permanent hypocalcemia in patients undergoing TT in our tertiary care hospital at Chennai with latitude of 13.08° N, 80.27° E.
Patients and Methods
A total of 349 consecutive patients undergoing first-time TT for benign or malignant thyroid diseases in a tertiary care teaching hospital at Chennai from July 2017 to June 2019 were enrolled in the study. Institute’s ethical committee approval (No.18092012) was obtained. The study was done in line with STROCSS criteria and registered with Research Registry (UIN: Research Registry 5818) [13]. Informed written consent was obtained from all the participants under study. The study adhered to the tenets of Declaration of Helsinki and none of the procedures involved animals. Surgical candidates were evaluated for complete haemogram, thyroid profile, liver and renal biochemistries. Indication for TT were presence of any of the following: large volume goitre, pressure symptoms, cytology suspicious/diagnostic of malignancy, indeterminate cytology, retrosternal extension, hyperthyroidism refractory to medication or radioiodine therapy and associated ophthalmopathy as well as patients opting surgery for cosmetic and logistic reasons. Exclusion criteria were revision surgery, concurrent neck dissection or comprehensive procedures, chronic medical conditions including uncontrolled diabetes, chronic renal and liver diseases, non-thyroid malignancy, immunosuppression, primary hyperparathyroidism and concurrent parathyroid procedures and patients on calcium and vitamin supplements. Conventional total thyroidectomy was performed by the same surgical team as per institutional standards, identifying and safe-guarding all the parathyroid glands, external branch of superior laryngeal and recurrent laryngeal nerves bilaterally. Postoperatively, hypocalcemic signs and symptoms including perioral or acral numbness, muscle cramps, carpopedal spam, laryngospasm, arrhythmia, seizures, positive Chvostek and Trousseau sign were monitored. Hypocalcemic patients received oral Calcium Carbonate 0.5-3 g/day ± Calcitriol (active vitamin D) 0.5–2 mcg/day. Intravenous 10% calcium gluconate at 0.5–2 mg/kg/h was administered for refractory cases. On the second postoperative day, vitamin D deficiency was treated with high-dose cholecalciferol 600,000 IU intramuscular injection and insufficiency was treated with oral doses of cholecalciferol 60,000 IU per week for 4–12 weeks tailored to clinical needs. The serum levels of corrected calcium, intact parathormone (iPTH) and 25OHD were measured at baseline, 48-h and 6-month post-TT and additional samples tailored to individual needs.
Laboratory Methods
Biochemical parameters were analyzed with automated Roche Cobas e6000 series analyzer, Switzerland. Serum calcium [8.5–10.5 mg/dL] was measured by Arsenazo III method. Serum albumin [3.4–5.4 g/dL] was measured by bromo-cresol green method. Corrected-calcium adjusted for albumin was calculated as total calcium (mg/dL) + 0.8 (4-albumin (g/dL)). Intact parathormone [15–65 pg/mL] was determined using fully automated chemiluminescent immune assay method. The intra-assay and inter-assay coefficient of variation was 5.8% and 6.4%, respectively. Serum 25OHD was analyzed on Siemens ADVIA Centaur by fully automated chemiluminescent immune assay method standardized against isotope dilution-liquid chromatography-tandem mass spectrometry reference methods as per vitamin D standardization programme. Reference range for 25OHD (measured in ng/mL) was categorized as per endocrine society practice guidelines into severe deficiency < 10; deficiency = 10–19.9; insufficiency = 20–29.9; sufficiency = 30–100 and toxicity > 150 ng/mL [11]
Definition
Transient hypocalcemia was defined as corrected calcium below 8 mg/dL and/or presence of hypocalcemic symptoms and signs lasting less than 6 months post-TT. Permanent hypocalcemia was defined as corrected calcium below reference range or the need for calcium with or without vitamin D therapy more than 6-month post-TT. Hypoparathyroidism was defined as iPTH < 10 pg/mL.
Statistical Analysis
Statistical analysis was performed with SPSS statistics, version 20.0. Armonk, NY: IBM Corp. Categorical variables were expressed as frequencies and percentage. On Kolmogorov–Smirnov normality test, continuous data was non-normal and expressed as median (interquartile range: IQR). Chi-Square test and Fischer exact test compared categorical variables. Kruskal–Wallis test compared independent samples with non-normal data. Independent variables significantly associated with dependent variable on univariate analysis were incorporated into multinomial logistic regression model for multivariate analysis. Receiver operating characteristic (ROC) curve assessed the diagnostic accuracy of 25OHD in predicting post-thyroidectomy hypocalcemia and optimal threshold was determined with Youden index. The area under the ROC curve (AUC) closer to the value of 1 implied excellent predictability, while those closer to 0.5 implied poorer predictability. Results were expressed as odds ratio (OR) with 95% confidence interval (95% CI). P < 0.05 was considered significant.
Results
Out of 349 patients undergoing TT, 327 patients with a median age of 34 years including 65 men (19.8%) and 262 women (80.1%) with a follow-up of 16.9 (5.7) months were eligible for the analysis. Patients who had concomitant central or lateral neck dissection (n = 9) and incomplete iPTH or 25OHD values (n = 13) were excluded. Histopathology comprised of colloid goitre (109, 33.3%), follicular adenoma (6, 1.8%), Hashimoto’s thyroiditis 44, 13.4%), chronic lymphocytic thyroiditis (11, 3.4%), Graves’ disease (46, 14.1%), adenomatous hyperplasia (64, 19.6%), papillary carcinoma (44, 13.4%), follicular carcinoma (1, 0.3%), medullary carcinoma (1, 0.3%) and anaplastic carcinoma (1, 0.3%). Demographics and clinical profile of patients including hyperthyroidism versus euthyroidism, benign versus malignancy and thyroiditis versus non-thyroiditis are tabulated (Table 1). Patients with Hashimoto’s thyroiditis and chronic lymphocytic thyroiditis in the histology of thyroidectomy specimen were included in the thyroiditis group. Serum corrected calcium, iPTH and 25OHD levels in each category of VDD were summarized (Table 2). Preoperative calcium, 48-h calcium and 48-h iPTH were significantly decreased in severe VDD compared to non-VDD patients.
Transient Hypocalcemia
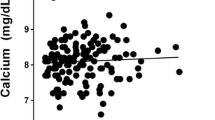
The incidence of symptomatic and asymptomatic transient postoperative hypocalcemia was 33.3% (n = 109) and 23.5% (n = 77), respectively, while preoperatively, 13.1% (n = 43) had biochemical hypocalcemia. In multivariate analysis (Table 3) adjusted for age and gender, biochemical predictors including preoperative 25OHD severe deficiency (OR = 20.2), deficiency (OR = 4.4), insufficiency (OR = 4.1), preoperative hypocalcemia (OR = 3.7) and 48-h iPTH (OR = 2.7) were independent risk factors for transient hypocalcemia in the decreasing order. Malignancy (OR = 5.9), hyperthyroidism (OR = 5.4) and thyroiditis (OR = 3.7) were also significant predictors. ROC curve was constructed to determine the diagnostic accuracy of 25OHD in predicting transient hypocalcemia. Patients with preoperative hypocalcemia (13.1%) could confound the results. Therefore, patients with preoperative normocalcemia and those with preoperative hypocalcemia were analyzed separately. In preoperative normocalcemic group, area under the ROC curve (Fig. 1) was 0.661 (95% CI: 0.60–0.72), P < 0.001 with threshold of 18.4 ng/mL indicating fair predictability. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 60%, 59.4%, 42.2% and 74.7%, respectively. In preoperative hypocalcemic group, 25OHD < 13.2 ng/mL strongly predicted transient post-thyroidectomy hypocalcemia with AUC of 0.804 (95% CI: 0.67–0.93; P = 0.001). Sensitivity and specificity were 67.9% and 66.7%, respectively.
Permanent Hypocalcemia
Permanent hypocalcemia was seen in 7.9% (n = 26) of cases. The independent risk factors (Table 3) were severe 25OHD deficiency (OR = 9.8), preoperative hypocalcemia (OR = 4.5), transient (OR = 3.2) and permanent hypoparathyroidism (OR = 4.9).
Discussion
Postoperative hypocalcemia remains the most common complication after TT and prolongs hospital stay. Many studies have recently evaluated the role of preoperative vitamin D deficiency as a predictor of PH [5, 14, 15]. However, inhomogeneity in utilization of 25OHD vs. 1,25(OH)2D for assessment of vitamin D status and variation in assay method have led to conflicting results. In particular, the “cut point” of serum 25OHD measurements for defining normal reference range and low vitamin D status varies widely. Moreover, the threshold of serum 25OHD level predicting the development of PH is not well-established. The present study addressed these issues. Based on preoperative 25OHD levels, patients were categorized into subgroups of severe VDD (n = 44; 13.5%), deficiency (n = 132; 40.3%), insufficiency (n = 109; 33.4%) and sufficiency (n = 43; 13.5%), and the development of PH in each category was assessed. Of 327 patients undergoing TT, the present study demonstrated postoperative symptomatic transient and permanent hypocalcemia in 109 (33.3%) and 26 (7.9%) patients, respectively, while 43 patients (13.1%) had hypocalcemia preoperatively. The incidence of transient hypocalcemia in subgroups with 25OHD sufficiency, insufficiency, deficiency and severe deficiency were 11.6%, 32.1%, 29.8% and 68.2%, respectively. On adjusting for age and gender, transient hypocalcemia was significantly and independently associated with low preoperative 25OHD, preoperative hypocalcemia and transient hypoparathyroidism. The odds of developing transient hypocalcemia escalated many-fold with increasing severity of preoperative vitamin D deficiency. Subgroups of patients with 25OHD insufficiency, deficiency and severe deficiency had 4.1, 4.4 and 20.2 times higher likelihood of developing transient hypocalcemia compared to 25OHD sufficient patients.
The constant blood level of calcium is maintained by the complex interaction of calciotropic hormones, namely parathormone (PTH) and vitamin D and counter-regulatory calcitonin. Any decrease in serum calcium level [Ca2+] increased the PTH secretion from parathyroid gland. PTH in turn increased Ca2+ by inducing (1) tubular reabsorption from the kidney, (2) mobilization from the bone and (3) intestinal absorption indirectly through vitamin D. However, in the presence of parathyroid injury post-TT, postoperative fall in Ca2+ is unable to increase PTH secretion from injured or ischemic parathyroid gland, and hence, vitamin D-mediated calciotropic actions become more vital to maintain constant Ca2+ level. Biological active 1,25(OH)2D enhances intestinal absorption and renal tubular reabsorption of calcium by many-fold through transcellular route. In vitamin D deficient patients, the above homeostatic mechanism to increase Ca2+ is impaired resulting in the development of hypocalcemia. Secondly, in the setting of parathyroid insufficiency, conversion of 25OHD to active 1,25(OH)2D is impaired which in-turn impairs vitamin D-mediated calcium absorption and reabsorption, further exacerbating hypocalcemia [14, 15]. In support of our observation, prior reports have shown that preoperative VDD increased the occurrence of post-thyroidectomy hypocalcemia and prolonged hospital stay [5, 16, 17]. In agreement with our findings, a recent study reported that preoperative VDD was associated with 3 times higher odds of developing symptomatic postoperative hypocalcemia. However, the study included thyroid cancer patients undergoing TT plus central compartment neck dissection, which is associated with increased risk of transient hypoparathyroidism and hence symptomatic hypocalcemia [18]. The presence of malignancy increased the risk of transient hypocalcemia after TT many-fold even in the absence of neck dissection as it is evident in our study. Moreover, the threshold of VDD was defined as less than 10 ng/mL in contrast to the standard cut-off value of < 20 ng/mL [11]. On the contrary, some investigators reported that VDD < 20 ng/mL was not a predictor of post-thyroidectomy hypocalcemia [4, 19]. Furthermore, an analysis of 366 patients undergoing bilateral thyroid surgery showed that the severe VDD < 10 ng/mL had only a trend towards transient hypocalcemia (P = 0.051) and failed to predict permanent hypoparathyroidism [20]. On the other hand, a study on 166 patients reported that the rate of transient hypocalcemia was significantly higher in severe VDD compared to VDD and non-VDD patients (32% vs. 24% vs.13%) after TT, which is in agreement with our findings [21]. However, the strength of association in terms of odds ratio or relative risk as well as the threshold of 25OHD predicting PH was not evaluated. Additionally, 25OHD (20–29.9 ng/mL) insufficient group was not evaluated separately, which was shown to have threefold increased likelihood of developing PH in our current series. Prior reports suggested that an optimal circulating 25OHD > 30 ng/mL maximized the bone health and non-skeletal benefits [11, 22]. Contradictory to our findings, a South Indian review of 150 patients reported no difference in the rate of transient post-thyroidectomy hypocalcemia between VDD and non-VDD patients (41.3% vs. 48.6%) [12]. The cut-off point of 25OHD was 20 ng/mL and hypocalcemic rate in severe deficiency and insufficient subgroup was not elucidated. It may be possible that patients with 25OHD insufficient range included in the non-VDD group could have inflated the rate of transient hypocalcemia. Moreover, the relation between preoperative 25OHD levels and permanent hypocalcemia was not elucidated. Nevertheless, our study has demonstrated that preoperative severe VDD had 9.8 times higher likelihood of developing permanent hypocalcemia compared to sufficient group. The present study has thus unravelled the impact of preoperative hypocalcemia and severe VDD on permanent post-thyroidectomy hypocalcemia in Indian subpopulation. Therefore, we emphasize that the appropriate treatment with calcium and vitamin D can improve the short-term as well as long-term outcome after TT in our population. Another Indian study reported that PTH was not a reliable predictor of post-thyroidectomy hypocalcemia in VDD patients as PTH levels may be elevated due to secondary hyperparathyroidism [23]. However, in our study neither preoperative nor postoperative median PTH levels were elevated in either 25OHD deficient or insufficient patients compared to sufficient patient group. Moreover, 48-h iPTH and 6-month iPTH independently predicted permanent hypocalcemia post-TT with an odds ratio of 3.2 (95% CI: 1.2–8.3) and 4.9 (95% CI: 1.3–18.9), respectively.
The present study demonstrated a relatively high incidence of preoperative hypocalcemia (13.1%), which may be a consequence of widely prevalent VDD in our population and was in keeping with our prior reports [24,25,26]. This was also evident from the diminishing median levels of preoperative calcium towards the spectrum of severe 25OHD deficiency and hence, subsequent PH (Table 1). Therefore, in order to determine the accuracy of predictability of preoperative 25OHD, patients who were normocalcemic and hypocalcemic preoperatively were analyzed independently. The area under the ROC curve was 0.66 (0.60–0.72), P = 0.001, which indicates that preoperative 25OHD was a significant and reliable predictor of transient hypocalcemia in normocalcemic patients undergoing TT, though with limited sensitivity and specificity. Recent evidences have shown that prophylactic calcium and vitamin D supplementation decreases the postoperative hypocalcemia rates and facilitates safe discharge [15, 27, 28]. Thus, routine analysis of preoperative calcium and 25OHD levels, stratification of vitamin D status and appropriate prophylactic therapy may allow safe same-day discharge after TT and can contemplate day-care surgery.
Limitations
In spite of latitude below 37°, VDD was widely prevalent in our population and may be related to the dark skin pigmentation due to melanin which absorbs UVB photons responsible for cutaneous vitamin D synthesis. The incidence of permanent hypocalcemia was relatively high. The delayed recovery of parathyroid gland function may be the reason and needs further evaluation beyond 1 year to allow time for the complete recovery. In order to uncover the true impact of preoperative 25OHD levels on PH, VDD was not treated until second postoperative day, which is ethically unsound.
Conclusion
Low preoperative calcium and 25-hydroxycholecalciferol levels were widely prevalent in our population and were independent risk factors for transient and permanent hypocalcemia after total thyroidectomy. The odds of developing transient hypocalcemia escalated with increasing severity of vitamin D deficiency. Patients with severe 25-hydroxycholecalciferol deficiency had 20 times increased likelihood to develop transient hypocalcemia and 9.8 times increased likelihood for permanent hypocalcemia compared to sufficient population, whereas 25OHD deficiency and insufficiency increased the likelihood to develop transient hypocalcemia by fourfold but had no impact on permanent hypocalcemia. Serum 25OHD below 18.4 ng/mL reliably predicted transient hypocalcemia in normocalcemic patients undergoing TT, though with limited sensitivity and specificity. Malignancy, hyperthyroidism, thyroiditis and postoperative hypoparathyroidism were other significant predictors of transient hypocalcemia. Thus, routine preoperative evaluation of serum calcium and 25OHD help to stratify patients at increased risk of post-thyroidectomy hypocalcemia, and appropriate calcium and vitamin D therapy can facilitate safe early discharge as well as improve long-term outcome. The feasibility of performing TT as a day-care procedure with prophylactic calcium and vitamin D merits high-level evidence with randomized controlled trials in our population.
Previous Communication to Society/Meeting
Received Best Faculty Paper Award at the 79th Annual Conference of the Association of Surgeons of India, Bhubaneswar 2019.
Data Availability
Data will be made available on reasonable request.
Code Availability
Not applicable.
References
Seo ST, Chang JW, Jin J et al (2015) Transient and permanent hypocalcemia after total thyroidectomy: early predictive factors and long-term follow-up results. Surgery (United States) 158:1492–1499. https://doi.org/10.1016/j.surg.2015.04.041
Edafe O, Antakia R, Laskar N et al (2014) Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg 101:307–320
Caglià P, Puglisi S, Buffone A et al (2017) Post-thyroidectomy hypoparathyroidism, what should we keep in mind? Ann Ital Chir 88:371–381
Wang X, Zhu J, Liu F et al (2017) Preoperative vitamin D deficiency and postoperative hypocalcemia in thyroid cancer patients undergoing total thyroidectomy plus central compartment neck dissection. Oncotarget 8:78113–78119. https://doi.org/10.18632/oncotarget.17690
Alkhalili E, Ehrhart MD, Ayoubieh H, Burge MR (2017) Does pre-operative vitamin D deficiency predict postoperative hypocalcemia after thyroidectomy? Endocr Pract 23:5–9. https://doi.org/10.4158/EP161411.OR
Vaitsi KD, Anagnostis P, Veneti S et al (2021) Preoperative vitamin D deficiency is a risk factor for postthyroidectomy hypoparathyroidism: a systematic review and meta-analysis of observational studies. J Clin Endocrinol Metab 106:1209–1224. https://doi.org/10.1210/clinem/dgab039
Lin Y, Ross HL, Raeburn CD et al (2012) Vitamin D deficiency does not increase the rate of postoperative hypocalcemia after thyroidectomy. Am J Surg 204:888–893. https://doi.org/10.1016/j.amjsurg.2012.10.001
Godazandeh G, Kashi Z, Godazandeh F et al (2015) Influence of thyroidectomy on postoperative serum calcium level regarding serum vitamin D status. A prospective study. Caspian J Intern Med 6:72–76
Holick MF, Wacker M (2013) Sunlight and vitamin D. Dermatoendocrinol 5:51–108. https://doi.org/10.4161/derm.24494
Holick M (2007) Vitamin D deficiency. N Engl J Med 357:266–281. https://doi.org/10.1056/NEJMra070553
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930. https://doi.org/10.1210/jc.2011-0385
Cherian AJ, Ponraj S, Gowri SM et al (2016) The role of vitamin D in post-thyroidectomy hypocalcemia: still an enigma. Surgery 159:532–538. https://doi.org/10.1016/j.surg.2015.08.014
Agha R, Abdall-Razak A, Crossley E et al (2019) STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int J Surg 72:156–165. https://doi.org/10.1016/j.ijsu.2019.11.002
Unsal IO, Calapkulu M, Sencar ME, et al (2020) Preoperative vitamin D levels as a predictor of transient hypocalcemia and hypoparathyroidism after parathyroidectomy. Sci Rep 10:9895-undefined. https://doi.org/10.1038/s41598-020-66889-8
Malik MZ, Mirza AA, Farooqi SA et al (2019) Role of preoperative administration of vitamin D and calcium in postoperative transient hypocalcemia after total thyroidectomy. Cureus 11(4):e4579. https://doi.org/10.7759/cureus.4579
Al-Khatib T, Althubaiti AM, Althubaiti A et al (2015) Severe vitamin D deficiency: a significant predictor of early hypocalcemia after total thyroidectomy. Otolaryngol Head Neck Surg 152:424–431. https://doi.org/10.1177/0194599814561209
Rehman M, Bhettani MK, Ahmed M et al (2019) Role of pre-operative vitamin D supplementation to reduce post-thyroidectomy hypocalcemia; cohort study. Int J Surg 71:85–90. https://doi.org/10.1016/j.ijsu.2019.08.035
Kim WW, Chung SH, Ban EJ et al (2015) Is preoperative vitamin D deficiency a risk factor for postoperative symptomatic hypocalcemia in thyroid cancer patients undergoing total thyroidectomy plus central compartment neck dissection? Thyroid 25:911–918. https://doi.org/10.1089/thy.2014.0522
Lee GH, Ku YH, Kim H, Il et al (2015) Vitamin D level is not a predictor of hypocalcemia after total thyroidectomy. Langenbecks Arch Surg 400:617–622. https://doi.org/10.1007/s00423-015-1311-1
Manzini G, Malhofer F, Weber T (2019) Can preoperative vitamin D deficiency predict postoperative hypoparathyroidism following thyroid surgery? Langenbecks Arch Surg 404:55–61. https://doi.org/10.1007/s00423-019-01748-3
Kirkby-Bott J, Markogiannakis H, Skandarajah A et al (2011) Preoperative vitamin D deficiency predicts postoperative hypocalcemia after total thyroidectomy. World J Surg 35:324–330. https://doi.org/10.1007/s00268-010-0872-y
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2012) Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab 97:1153–1158
Pradeep PV, Ramalingam K (2014) Postoperative PTH measurement is not a reliable predictor for hypocalcemia after total thyroidectomy in vitamin D deficiency: prospective study of 203 cases. World J Surg 38:564–567. https://doi.org/10.1007/s00268-013-2350-9
Karunakaran P, Maharajan C, Ramalingam S, Rachmadugu SV (2018) Is hungry bone syndrome a cause of postoperative hypocalcemia after total thyroidectomy in thyrotoxicosis? A prospective study with bone mineral density correlation. Surgery (United States) 163:367–372. https://doi.org/10.1016/j.surg.2017.09.008
Karunakaran P, Maharajan C, Mohamed KN, Rachamadugu SV (2016) Rapid restoration of bone mass after surgical management of hyperthyroidism: a prospective case control study in Southern India. Surgery 159:771–776. https://doi.org/10.1016/j.surg.2015.10.002
Karunakaran P, Abraham DT, Devadas G et al (2020) The impact of operative duration and intraoperative fluid dynamics on postoperative hypocalcemia after total thyroidectomy: a prospective non-randomized study. Langenbecks Arch Surg. https://doi.org/10.1007/s00423-020-02013-8
Sanabria A, Rojas A, Arevalo J (2019) Meta-analysis of routine calcium/vitamin D3 supplementation versus serum calcium level-based strategy to prevent postoperative hypocalcaemia after thyroidectomy. Br J Surg 106:1126–1137
Arer IM, Kus M, Akkapulu N et al (2017) Prophylactic oral calcium supplementation therapy to prevent early post thyroidectomy hypocalcemia and evaluation of postoperative parathyroid hormone levels to detect hypocalcemia: A prospective randomized study. Int J Surg 38:9–14. https://doi.org/10.1016/j.ijsu.2016.12.041
Acknowledgements
We thank Dr. Srinivasan Ramalingam PhD, Senior Technical Officer, ICMR-National Institute for Research in Tuberculosis, Chetpet, Chennai-600031, for assistance in statistical analysis and interpretation of results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, data analysis and interpretation were performed by Dr K. Poongkodi. Dr K Poongkodi drafted the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
This study was approved by the institutional Ethics committee, Madras Medical College, Chennai-3 (No.18092012). All procedures involving human participants were conducted in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and later amendments. This article does not contain any studies with animals performed by any of the authors.
Consent to Participate
Informed written consent obtained from all the individual participants included in the study.
Consent for Publication
Informed written consent obtained from all the subjects included in the study regarding participation in this research and publication of their data.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study design: Single-Centre Prospective Observational Study – Cohort study
Rights and permissions
About this article
Cite this article
Karunakaran, P., Abraham, D.T., Devadas, G. et al. Is Preoperative Vitamin D Deficiency a Predictor of Transient and Permanent Hypocalcemia After Total Thyroidectomy? A Cohort Study in a Tertiary Care Hospital. Indian J Surg (2021). https://doi.org/10.1007/s12262-021-03183-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-021-03183-5