Abstract
Purpose
As the incidence of thyroid cancer has increased, hypocalcemia, a common complication of thyroid surgery, has become a serious problem. However, no definite predictor of postoperative hypocalcemia is known. In this study, our purpose was to investigate the potential role of vitamin D as a predictor of postoperative hypocalcemia.
Methods
A prospective observational study was performed on patients who underwent total thyroidectomy for thyroid cancer performed by a single experienced surgeon between October 2013 and September 2014.
Measurements
Their serum 25-OH vitamin D levels were measured preoperatively. On the day after surgery, serum calcium and intact parathyroid hormone levels were measured, and symptoms of hypocalcemia were recorded.
Results
Of the 134 patients, laboratory and symptomatic hypocalcemia developed in 52 patients (39 %) and 25 patients (19 %), on the day after surgery. The preoperative vitamin D level was 16.5 ± 9.2 ng/mL, and this value did not differ according to laboratory or symptomatic hypocalcemia (p = 0.94). The incidence of laboratory or symptomatic hypocalcemia did not differ according to vitamin D deficiency. Only incidental parathyroidectomy was associated with symptomatic hypocalcemia (p = 0.03).
Conclusions
Vitamin D level is not a predictor of hypocalcemia after total thyroidectomy for thyroid cancer. Thus, routine preoperative screening for vitamin D is not recommended.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
As the incidence of thyroid cancer has increased, the number of thyroid surgeries performed has also increased [1]. The most common complications of thyroid surgery are hypoparathyroidism and recurrent laryngeal nerve injury. The incidence of postoperative hypocalcemia has been reported to range from 1 to 50 % [2–4]. Hypocalcemia can be asymptomatic but cause perioral or distal acral paresthesia, severe cramps, tetany, and convulsion. Although most patients with hypocalcemia recover within a few months [3], symptomatic hypocalcemia is of concern because it leads to prolonged hospitalization or readmission.
Several studies have tried to identify a risk factor for hypocalcemia after thyroid surgery. Some studies reported an association with early postoperative calcium level [5–7] or intraoperative parathyroid hormone (PTH) level (<10 pg/mL) [8], but they did not provide a definitive prediction of hypocalcemia. Some researchers propose routine oral calcium supplements with or without vitamin D to prevent postoperative hypocalcemia [9–13]. This may reduce symptomatic hypocalcemia and shorten hospital stay.
Recently, vitamin D has been suggested as a risk factor for postoperative hypocalcemia [14–16]. Vitamin D deficiency can decrease intestinal calcium absorption and stimulate PTH synthesis and secretion to maintain normal calcium levels [17]. Vitamin D deficiency is also reported to be associated with hyperparathyroidism [18, 19]. It has been hypothesized that temporary hypoparathyroidism after thyroid surgery may fail to compensate vitamin D deficiency and lead to postoperative hypocalcemia. Some studies showed the association between vitamin D deficiency and postoperative hypocalcemia or a longer hospital stay [14–16]; however, some did not [20–23], and Nhan et al. reported that vitamin D deficiency even had a tendency to decrease a risk of postoperative hypocalcemia [23].
Controversies remain regarding vitamin D deficiency as a predictor of postoperative hypocalcemia. Therefore, in this study, we investigated the association between vitamin D and postoperative hypocalcemia prospectively in patients undergoing total thyroidectomy for thyroid cancer.
Material and methods
Patients who underwent total thyroidectomy for thyroid cancer by a single surgeon in the Korea Cancer Center Hospital between October 2013 and September 2014 were enrolled prospectively. In accordance with the American Thyroid Association guidelines, total thyroidectomy was performed if there were big, multiple, or bilateral thyroid cancers with or without extrathyroid extensions and lymph node metastases. Patients who had had previous thyroid surgery or irradiation, concomitant parathyroid disease, or took either calcium or vitamin D supplements were excluded. Patients with abnormal renal function (glomerular filtration rate (GFR) <60 mL/min/1.73 m2) were also excluded. Informed consent was obtained from all eligible patients. During study period, 138 patients underwent total thyroidectomy for thyroid cancer, and four patients were excluded because of previous thyroid irradiation (n = 1), concomitant hyperparathyroidism (n = 1), consent withdrawal (n = 1), or loss to follow-up (n = 1). Finally, 134 patients were included and analyzed in this study. The study protocol was approved by the institutional review board of Korea Cancer Center Hospital (IRB No. K-1401-002-036).
All patients underwent preoperative ultrasonography and fine-needle aspiration. The results of cytology were papillary thyroid carcinoma (PTC), suspicious PTC, or medullary thyroid carcinoma (MTC). All patients underwent total thyroidectomy with central compartment neck dissection (level VI) with or without selective neck dissection (level IIa, III, IV, and Vb) performed by an experienced senior thyroid surgeon. For total thyroidectomy, a capsular dissection technique was used with routine identification and preservation of the recurrent laryngeal nerves and parathyroid glands. The parathyroid glands were identified and preserved on their vascular pedicle whenever possible. Incidentally removed or devascularized glands were autotransplanted in a standard fashion into the sternocleidomastoid muscle. The surgical specimens were carefully checked for parathyroid glands.
Serum 25-OH vitamin D level was measured preoperatively by using a radioimmunoassay (Diasorin, Stillwater, MN, USA). Serum calcium, ionized calcium, and intact PTH levels were measured preoperatively, 1 day after surgery and 3 weeks after surgery. Intact PTH level was measured using an autoanalyzer (the ADVIA Centaur immunoassay, NY, USA). The reference range of PTH is 14–72 pg/mL. Laboratory hypocalcemia was defined as total calcium concentration less than 8.0 mg/dL, and symptomatic hypocalcemia was defined as subjective or objective symptoms such as tingling, numbness, or carpopedal spasm with laboratory hypocalcemia. When symptomatic hypocalcemia developed during hospital stay, calcium and vitamin D were administered orally. If the symptoms continued to persist, calcium gluconate was administered intravenously. The length of hospital stay was recorded for all patients.
We divided all patients into three groups according to the laboratory or symptomatic hypocalcemia. Age, sex, body mass index (BMI), laboratory findings, and incidental parathyroidectomy were compared among groups. The data were also analyzed by dividing the patients into two groups depending on vitamin D deficiency. Vitamin D deficiency was defined as vitamin D level <10 or 20 ng/mL.
Sample size calculation and statistical analyses
Based on previous studies [15, 16], we hypothesized that hypocalcemia developed in 25 % of patients without vitamin D deficiency, and the sample size of the study was calculated to detect a difference of 15 % in hypocalcemia using Flemming’s model with a type 1 error (α) of 0.05 and a power (β) of 80 %, resulting in 57 subjects in each group (group with vitamin D deficiency and group without vitamin D deficiency).
All data are expressed as mean ± standard deviation. Categorical variables (sex, incidental parathyroidectomy, and the presence of hypocalcemia) were analyzed using the χ 2 test, and continuous variables (age, BMI, calcium, PTH, and vitamin D) were compared using the Student’s t test or one-way ANOVA. To identify predictor of postoperative hypocalcemia, logistic regression analysis was performed. All analyses were performed using SPSS 14.0 for Windows (SPSS Inc., Chicago, IL, USA), and a p < 0.05 was considered statistically significant.
Results
A total of 134 patients were included in this analysis. The mean age at surgery was 50 years (range, 24–77 years), and there were 21 men and 113 women. The patient characteristics are summarized in Table 1.
All patients underwent a total thyroidectomy with central compartment neck dissection. Among them, 20 (15 %) patients underwent additional selective neck dissection. The final pathological diagnoses were PTC (n = 132) and MTC (n = 2). The mean size of the tumor was 1.2 ± 0.9 cm, and lymph node metastasis was observed in 83 (62 %) patients. During surgery, surgeon tried to preserve parathyroid glands, and parathyroid gland autotransplantations were performed in 19 (14 %) patients. Nevertheless, regarding surgical specimens, one parathyroid gland was removed incidentally in 22 patients, and two parathyroid glands were removed in one patient. Additional selective neck dissection did not increase the risk of incidental parathyroidectomy (p = 0.75).
The mean preoperative calcium and PTH levels were 9.3 ± 0.4 mg/dL and 50 ± 18 pg/mL, respectively. On the day after surgery, serum calcium and PTH levels were 8.1 ± 0.5 mg/dL and 26 ± 20 pg/mL, respectively. Laboratory hypocalcemia developed in 52 (39 %) patients. Symptomatic hypocalcemia developed in 25 (19 %) patients, and calcium and vitamin D supplements were started.
There was no difference in age, sex, BMI, preoperative calcium or PTH levels, or selective neck dissection between patients with or without laboratory or symptomatic hypocalcemia on the day after surgery (Table 2). The length of hospital stay also did not differ between patients with or without symptomatic hypocalcemia (7.5 ± 1.9 days vs. 7.9 ± 3.1 days, p = 0.57). The mean preoperative vitamin D level was 16.5 ± 9.2 ng/mL and was not significantly different among groups. The parathyroid glands removed incidentally during surgery were more frequently found in patients with symptomatic hypocalcemia (p = 0.04; Table 2). In logistic regression analysis, incidental parathyroidectomy was significantly associated with an increased risk of symptomatic hypocalcemia (p = 0.03; Table 3).
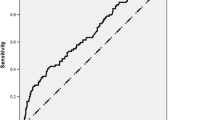
We examined the association between preoperative vitamin D level and postoperative calcium level. Postoperative calcium level did not correlate with preoperative vitamin D level (p = 0.49; Fig. 1). Vitamin D deficiency is generally defined as a vitamin D level <20 ng/mL [24], and 90 (69 %) patients had vitamin D deficiency (<20 ng/mL). The incidence of laboratory hypocalcemia (38 vs. 42 %, p = 0.70) or symptomatic hypocalcemia (18 vs. 20 %, p = 1.00) was not different between patients with and without vitamin D deficiency. Next, we used a stricter cutoff value of 10 ng/mL. Vitamin D deficiency (<10 ng/mL) was found in 41 (31 %) patients. Postoperative calcium levels in patients with vitamin D deficiency were not different from those in patients without vitamin D deficiency (Table 4). The percentage of laboratory or symptomatic hypocalcemia did not differ according to vitamin D deficiency (Table 4).
At 3 weeks after surgery, laboratory and symptomatic hypocalcemia had developed in five additional patients. In all, laboratory hypocalcemia was noted in 57 (43 %) patients, while calcium and vitamin D supplements were administrated in 30 (22 %) patients. At the 6-month follow-up, calcium and vitamin D supplements were discontinued in 24 of the 30 patients and it was maintained in only six patients. Among them, five patients took below 500 mg of elemental calcium per day, and 1000 mg of elemental calcium per day was taken in one patient, which did not have vitamin D deficiency preoperatively.
Discussion
Vitamin D plays an important role in calcium homeostasis. Therefore, serum vitamin D level is expected to be associated with hypocalcemia after thyroidectomy. However, this hypothesis remains controversial [14–16, 20–22], and previous studies had some limitations such as retrospective design, differences in underlying disease, surgical extent, and surgeon. The surgical extent, surgeon’s experience, and underlying disease such as hyperthyroidism affect the risk of hypocalcemia [25]. To cope with these limitations, we used a prospective design that included a similar population, a similar pathology, the same operation, and the same surgeon. In this study, preoperative serum vitamin D level was not associated with postoperative hypocalcemia. Only incidental parathyroidectomy showed an association with postoperative hypocalcemia. Because incidental parathyroidectomy significantly attributed to symptomatic hypocalcemia, we analyzed the group in which no parathyroid glands were removed incidentally (n = 111). However, even excluding the patients whose parathyroid glands were removed incidentally, vitamin D level did not differ between patients with or without laboratory or symptomatic hypocalcemia (data not shown).
The causes of hypocalcemia and hypoparathyroidism are multifactorial and include hemodilution, surgical injury such as devascularization, and incidental resection of the parathyroid gland. The incidence of incidental parathyroidectomy ranges from 5 to 20 % even for experienced surgeons [25, 26]. Because a large number of parathyroid glands are located within the thyroid gland, incidental parathyroidectomy is difficult to avoid. However, the clinical relevance of incidental parathyroidectomy, i.e., whether it is associated with postoperative hypocalcemia, is unclear [3, 25–27]. The question of how many parathyroid glands must be preserved to avoid hypocalcemia remains unresolved. Some believe that a single intact parathyroid gland is enough, and others believe that at least three parathyroid glands are necessary [3]. In this study, incidental parathyroidectomy increased the risk of postoperative hypocalcemia, suggesting the importance of identifying and preserving as many parathyroid glands as possible during surgery.
Vitamin D deficiency is common in Korea, the USA, and Europe alike [28, 29]. In this study, the incidence of vitamin D deficiency was fairly high. However, vitamin D deficiency did not show an association with postoperative hypocalcemia. Currently, the role of vitamin D is being studied in several thyroid-related researches, in addition to its potential role in postoperative hypocalcemia. Vitamin D level has been reported to be associated with autoimmune thyroid disease or the stage of thyroid cancer [30, 31]. Therefore, there is a possibility that vitamin D level is not a predictor of postoperative hypocalcemia but a marker for disease severity, because for underlying disease with greater severities, a wider surgical extent is required, thus increasing the chances of hypocalcemia.
In this study, symptomatic hypocalcemia was finally noted in 22 % of all the patients although all operations were performed by an experienced surgeon. This result is in accordance with that of a previous report [4]. Since postoperative hypocalcemia is affected by the surgical procedure, it is difficult to predict. Moreover, hypocalcemia can develop a few days after thyroid surgery. Previous studies have reported that the time to reach the nadir of serum calcium level is generally 2 or 4 days after surgery [3, 32]. Unfortunately, we planned to measure serum calcium concentration only on 1 day after surgery, and serum calcium concentration on 2 or 3 days after surgery was measured only in 62 (46 %) patients. Among them, laboratory hypocalcemia on day 2 or 3 was newly developed in four patients. Some symptomatic hypocalcemia (17 %) also developed a few days after surgery. Therefore, if length of hospital stay is more than 4 days, the development of hypocalcemia can be observed without pre-medication. However, in case of outpatient-based thyroid surgery or early discharge after surgery, preoperative routine oral calcium and vitamin D supplementation can be considered [10, 13].
The method of vitamin D level measurement and the definition of vitamin D deficiency used here can be considered as the limitations of this study. High-performance liquid chromatography is the gold standard for vitamin D measurement, but we measured vitamin D level using a commercialized radioimmunoassay. The definition of vitamin D deficiency is controversial. We used two cutoff values of 10 and 20 ng/mL, and the incidence of postoperative hypocalcemia was not different between patients with and without vitamin D deficiency even if using any cutoff values. When patients were divided into quartiles according to the vitamin D level, there was no association between vitamin D level and postoperative hypocalcemia (data not shown). In addition, this study has a relatively small sample size. This study was terminated because an interim analysis revealed that the vitamin D deficiency group showed no tendency toward increased postoperative hypocalcemia.
Conclusion
In this study, we demonstrated that serum vitamin D level is not a predictor of hypocalcemia after total thyroidectomy for thyroid cancer. Thus, routine preoperative screening for vitamin D is not recommended.
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Al-Suliman NN, Ryttov NF, Qvist N et al (1997) Experience in a specialist thyroid surgery unit: a demographic study, surgical complications, and outcome. Eur J Surg 163:13–20
Pattou F, Combemale F, Fabre S et al (1998) Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg 22:718–724
Reeve T, Thompson NW (2000) Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg 24:971–975
Adams J, Andersen P, Everts E et al (1998) Early postoperative calcium levels as predictors of hypocalcemia. Laryngoscope 108:1829–1831
Bentrem DJ, Rademaker A, Angelos P (2001) Evaluation of serum calcium levels in predicting hypoparathyroidism after total/near-total thyroidectomy or parathyroidectomy. Am Surg 67:249–251, discussion 251–242
Moore C, Lampe H, Agrawal S (2001) Predictability of hypocalcemia using early postoperative serum calcium levels. J Otolaryngol 30:266–270
Quiros RM, Pesce CE, Wilhelm SM et al (2005) Intraoperative parathyroid hormone levels in thyroid surgery are predictive of postoperative hypoparathyroidism and need for vitamin D supplementation. Am J Surg 189:306–309
Moore FD Jr (1994) Oral calcium supplements to enhance early hospital discharge after bilateral surgical treatment of the thyroid gland or exploration of the parathyroid glands. J Am Coll Surg 178:11–16
Bellantone R, Lombardi CP, Raffaelli M et al (2002) Is routine supplementation therapy (calcium and vitamin D) useful after total thyroidectomy? Surgery 132:1109–1112, discussion 1112–1103
Kurukahvecioglu O, Karamercan A, Akin M et al (2007) Potential benefit of oral calcium/vitamin D administration for prevention of symptomatic hypocalcemia after total thyroidectomy. Endocr Regul 41:35–39
Roh JL, Park CI (2006) Routine oral calcium and vitamin D supplements for prevention of hypocalcemia after total thyroidectomy. Am J Surg 192:675–678
Roh JL, Park JY, Park CI (2009) Prevention of postoperative hypocalcemia with routine oral calcium and vitamin D supplements in patients with differentiated papillary thyroid carcinoma undergoing total thyroidectomy plus central neck dissection. Cancer 115:251–258
Yamashita H, Noguchi S, Murakami T et al (2001) Predictive risk factors for postoperative tetany in female patients with Graves' disease. J Am Coll Surg 192:465–468
Erbil Y, Barbaros U, Temel B et al (2009) The impact of age, vitamin D(3) level, and incidental parathyroidectomy on postoperative hypocalcemia after total or near total thyroidectomy. Am J Surg 197:439–446
Kirkby-Bott J, Markogiannakis H, Skandarajah A et al (2011) Preoperative vitamin D deficiency predicts postoperative hypocalcemia after total thyroidectomy. World J Surg 35:324–330
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Valcour A, Blocki F, Hawkins DM et al (2012) Effects of age and serum 25-OH-vitamin D on serum parathyroid hormone levels. J Clin Endocrinol Metab 97:3989–3995
Garg MK, Tandon N, Marwaha RK et al (2014) The relationship between serum 25-hydroxy vitamin D, parathormone and bone mineral density in Indian population. Clin Endocrinol (Oxf) 80:41–46
Lin Y, Ross HL, Raeburn CD et al (2012) Vitamin D deficiency does not increase the rate of postoperative hypocalcemia after thyroidectomy. Am J Surg 204:888–893, discussion 893–894
Lang BH, Wong KP, Cheung CY et al (2013) Does preoperative 25-hydroxyvitamin D status significantly affect the calcium kinetics after total thyroidectomy? World J Surg 37:1592–1598
Griffin TP, Murphy MS, Sheahan P (2014) Vitamin D and risk of postoperative hypocalcemia after total thyroidectomy. JAMA Otolaryngol Head Neck Surg 140:346–351
Nhan C, Dolev Y, Mijovic T et al (2012) Vitamin D deficiency and the risk of hypocalcemia following total thyroidectomy. J Otolaryngol Head Neck Surg 41:401–406
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Thomusch O, Machens A, Sekulla C et al (2000) Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 24:1335–1341
Gourgiotis S, Moustafellos P, Dimopoulos N et al (2006) Inadvertent parathyroidectomy during thyroid surgery: the incidence of a complication of thyroidectomy. Langenbecks Arch Surg 391:557–560
Abboud B, Sargi Z, Akkam M et al (2002) Risk factors for postthyroidectomy hypocalcemia. J Am Coll Surg 195:456–461
Choi HS, Oh HJ, Choi H et al (2011) Vitamin D insufficiency in Korea—a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 96:643–651
Choi HS (2013) Vitamin D status in Korea. Endocrinol Metab (Seoul) 28:12–16
Choi YM, Kim WG, Kim TY et al (2014) Low levels of serum vitamin D3 are associated with autoimmune thyroid disease in pre-menopausal women. Thyroid 24:655–661
Kim JR, Kim BH, Kim SM, et al. (2014) Low serum 25 hydroxyvitamin D is associated with poor clinicopathologic characteristics in female patients with papillary thyroid cancer. Thyroid 24(11):1618–1624
Roh JL, Park JY, Park CI (2007) Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 245:604–610
Acknowledgments
This study was supported by a grant of the KCCH Research Competence Promotion (KRP), Korea Institute of Radiological and Medical Sciences (50246–2014).
Conflicts of interest
The authors declare that they have no conflict of interest.
Authors’ contribution
G. H. L. and M. J. K. contributed to the study conception and design, analysis and interpretation of data, and drafting of the manuscript. G. H. L. and M. L. collected the data. Y. H. K. and H. I. K. participated in the drafting and critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, G.H., Ku, Y.H., Kim, H.I. et al. Vitamin D level is not a predictor of hypocalcemia after total thyroidectomy. Langenbecks Arch Surg 400, 617–622 (2015). https://doi.org/10.1007/s00423-015-1311-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1311-1