Abstract
Purpose
Transient hypocalcaemia after thyroid surgery and its possible predictors have not been extensively described in the elderly. This study aimed to establish the frequency of postsurgical transient hypocalcaemia according to the extent of thyroid surgery in older adults and to assess mineral metabolism biochemical parameters as its predictors.
Methods
All patients ≥60 years undergoing thyroid surgery were prospectively included. Type of surgery (hemithyroidectomy(HT) or total thyroidectomy(TT)); and preoperative 25OH Vitamin D (25OHD) and pre and 6 (only TT), 24 h and 6 months postsurgical serum levels of calcium, magnesium, phosphate and parathormone (PTH) were considered. Postsurgical hypoparathyroidism (hPTpost) was defined at PTH levels ≤11 pg/mL.
Results
Out of 46 patients (87% female), age (mean ± SD) 70.1 ± 6.2 years, 24 h postsurgical hypocalcaemia was found in ten patients (22%). In 25 (54%) TT patients, 36% and 16% had postsurgical hypocalcaemia at 6 and 24 h respectively; 28% hPTpost but no definitive hPT was recorded and 44% had 25OHD deficiency. Lower 24 h magnesium levels were found in those TT patients with 24 h hypocalcaemia (1.6 ± 0.1 vs 1.9 ± 0.1 mg/dL (p = 0.005)). Among 21 (46%) HT patients, 28.6% had 24 h postsurgical hypocalcaemia; 9.5% had hPTpost. A positive correlation was observed between preoperative 25OHD and 24 h calcaemia (r:0.51,p = 0.02). 43% of the patients were 25OHD deficient, in whom 55% had 24 h hypocalcaemia vs only 9% in the 25OHD sufficient group (p = 0.049).
Conclusion
Postsurgical hypocalcaemia was common in elderly thyroidectomized patients. After TT, lower magnesium levels were found in those patients with 24 h hypocalcaemia. In the HT group, preoperative 25OHD deficiency predicted lower postsurgical calcium levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A normal serum calcium level is critical for many vital cellular functions, including hormonal secretion, blood clotting, neurotransmission, skeletal and cardiac muscle contraction [1]. Acute hypocalcemia is well known for its effects on cardiac conduction and is manifested on the electrocardiogram as prolongation of the QTc interval, which can trigger life-threatening arrhythmias, requiring urgent treatment [1]. It is of particular interest that the most common cause of acute symptomatic hypocalcaemia in hospital practice is the alteration of the parathyroid glands secondary to thyroid surgery [2].
It is well known that either hemithyroidectomy (HT) or total thyroidectomy (TT) are amongst the treatments of choice both for benign nodular goiter and thyroid cancer. Despite being safe procedures, patients undergoing thyroid surgery can still present postsurgical complications, such as transient hypocalcaemia and hypoparathyroidism [3]. In fact, the incidence of transient hypocalcaemia in the immediate postoperative period of thyroid surgery varies widely (1.6–68%), reflecting the considerable heterogeneity among the different studies [3].
Direct injury or devascularization of the parathyroid glands is generally accepted as the most common cause of post-thyroidectomy hypocalcaemia [4]. However, several studies have been developed to investigate predictors of postoperative hypocalcaemia. These predictors include type of thyroid disease, extent of surgery, need for reoperation and parathyroid autologous transplantation as well as biochemical factors such as perioperative levels of calcaemia, magnesemia, phospatemia, parathormone (PTH) and 25OH vitamin D (25OHD) [4]. Moreover according to Dip et al. [5], near-infrared light autofluorescence used intraoperatively for parathyroid gland identification decreases the incidence of postoperative hypocalcaemia.
Recently, it was described that elderly patients are increasingly referred to head and neck surgery. Furthermore, postoperative complications were reported significantly higher compared to younger patients [6].
In this context advanced age, together with the extent of the thyroid nodular disease, are all variables to be considered on planning the best surgical strategy. It has been proposed that low-risk thyroid cancer be managed with more conservative surgery such as HT [7]. It is also worth noting that in benign nodular disease, HT may also be resolutive, particularly in older patients with comorbidities in whom invasive surgery strategies should be avoided [8]. Furthermore, older age at surgery has proved an independent risk factor for a lower rate of nodule recurrence after HT for benign nodular disease [9].
Among the possible complications of thyroid surgery, one of the most frequent is transient hypocalcaemia. Contrary to what would be expected with TT, in HT, postsurgical alterations in mineral metabolism have not been extensively reported and little headway has been made to explore treatment outcomes among elderly patients undergoing different thyroid surgery strategies. One of the risk factors for mineral alterations in this setting is low 25OHD serum levels. In fact, hypovitaminosis D, a highly prevalent condition [10], could favor the development of transient hypocalcaemia in the immediate postoperative period of nodular thyroid disease in older adults.
Magnesium levels have indeed been shown to modulate calcium levels through PTH secretion and low magnesium serum levels could also play a role in the occurrence of postsurgical hypocalcaemia in aged patients [11].
The aim of this study has been to establish the frequency of transient hypocalcaemia in the postoperative period of thyroid surgery in older adults according to the extent of surgery and to assess if 25OHD deficiency and lower magnesium serum levels are possible predictors of transient hypocalcaemia.
Materials and methods
Study design
A prospective, consecutive, and longitudinal study was designed in which all patients above 60 years of age referred to surgery from June 2014 to November 2017 at Dr. Cesar Milstein Care Unit for both benign and malignant thyroid pathology were included. Surgical indication in those patients with benign tumors was based on size of tumor and compressive symptoms, while in those malignant tumors the decision was taken upon an indeterminate, suspicious for malignancy, or malignant cytological report.
The type of surgery either HT or TT was decided prior to surgery by an interdisciplinary medical team taking into consideration the presence of 1 or more nodule, the size and extension of the lesion, age, and comorbidities of each patient. The same two surgeons were in charge of all these patients.
In all patients a preoperative biochemical assay including calcaemia, 25OHD and PTH, magnesium, phosphate, and albumin was performed in fasting conditions on the same day of the thyroid surgery. Calcaemia was determined at 6 h only in patients undergoing TT and, 24 h after the surgical procedure, either HT or TT, in all patients together with PTH, magnesium, phosphate and albumin levels.
After surgery, periodic clinical evaluations of the patients were carried out, focusing on signs and/or symptoms compatible with hypocalcaemia (paresthesias, Chvostek, and Trousseau signs).
Six months after surgery, calcaemia and PTH values were measured to assess the presence of definitive hypoparathyroidism.
Patients with incomplete data, previous hypoparathyroidism, indication for parathyroid surgery, hyperthyroidism, previous neck surgeries, chronic renal failure, and patient refusal to participate in the study were excluded.
Ethical compliance
The protocol was approved by the Ethics Committee for human studies of Dr. Cesar Milstein Care Unit, Buenos Aires. All participants gave a written voluntary consent to participate.
Biochemical determinations
In all cases blood sampling was obtained by venopuncture, thus obtaining two tubes, one with lithium heparin for the determination of calcium, phosphate, magnesium, and albumin in serum which were processed 1 h after the extraction; and a second dry tube for serum determination of Vitamin D and PTH. This second tube was centrifuged, serum was aliquoted and frozen at −20 °C until 7 days later where it was processed.
The methodologies used for the different assays were: intact PTH: two-site solid-phase chemiluminescent immunometric automated assay system (Reference value (RV) 11–67 pg/mL, coefficient of variation (CV) 9.85%) (Immulite1000, Siemens Healthcare Diagnostics, Llanberis, UK); for 25OHD chemiluminescent immunometric automated assay system (RV: deficiency < 20, insufficiency: 20–30 and normal values > 30 ng/mL, CV 6.75%) (Advia Centaur XP, Siemens Healthcare Diagnostics, Llanberis, UK), albumin (RV: 3.5–5.2 g/dL VC 2.19%); calcaemia (RV 8.5–10.2 mg/dL CV 3.21%), phosphatemia (RV 2.7–4.5 mg/dL CV 1.62%) and magnesemia (RV 1.6–2.6 mg/dL CV 2.94%) were analyzed with automated colorimetric method (Cobas C311 Chemistry analyzer, Roche, Switzerland).
The serum calcium result was corrected for albumin levels [corrected calcium = serum calcium + (4–serum albumin) × 0.8 [1]. Hypocalcaemia was considered a value ≤ 8.5 mg/dL, severe hypocalcaemia a value ≤ 7.5 mg/dL, and postsurgical hypoparathyroidism (hPTpost) PTH ≤ 11 pg/mL (according to laboratory rank). As mentioned, 25OHD insufficiency was defined at values between 20 and 30 ng/mL and deficiency < 20 ng/mL [12].
Reposition protocol
The same postsurgical replacement protocol was used for calcium replacement in the entire population, approved and authorized by our institution. Those patients with albumin-corrected serum calcium values between 7.5 and 7.9 mg/dL and between 8 and 8.5 mg/dL, received 4 and 2 tablets of calcium carbonate respectively (500 mg of elemental calcium each tablet) away from meals, plus 2 tablets of active vitamin D [1,25- (OH) 2D3)] of 0.25 mcg each, subsequently adjusting the doses according to periodic evaluations.
Severe hypocalcaemia with serum calcium ≤7.5 mg/dL or presence of clinical manifestations of hypocalcaemia were treated with intravenous calcium gluconate (90 mg ampoules), with periodic laboratory follow-up, until improvement of symptoms and calcium levels in normal range and then switched to the oral route.
Patients who presented hypocalcaemia, once a serum calcium value > 8 mg/dL had been attained, were discharged and continued with oral replacement of calcium and active vitamin D until the next evaluation.
Patients follow-up
The patients were summoned 1 week after surgery for control and if calcium serum values were normal, calcium and active vitamin D oral administration were discontinued. Six months after surgery, calcaemia and PTH were requested to detect those patients with definitive hypoparathyroidism.
Pathology report
The terms benign and malignant were used according to the definitive histological report, and the classification according to the WHO 4th edition, published in 2017 was applied. Follicular adenoma, colloid goiter, nodular hyperplasia, multinodular goiter, and lymphocytic thyroiditis were included in benign pathology. Among the malignant pathologies, noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP), classic variant and follicular variant papillary carcinoma, follicular carcinoma, Hürthle cell carcinoma, poorly differentiated, medullary and anaplastic carcinoma were all contemplated [13].
Statistical analysis
Variables were considered as continuous or categorical. According to data distribution, Pearson or Spearman correlation tests were used. Continuous variables were compared by Student t test or Mann–Whitney U test for normally or skewed distributed variables, respectively and categorical variables were compared by Fisher´s exact test. A p ≤ 0.05 was deemed as being indicative of statistical significance.
Statistical analyses were performed using SPSS 17.0 statistical software (IBM, Chicago, Ill, USA).
Results
Seventy-seven thyroid-operated patients were evaluated consecutively, of which 31 had exclusion criteria. In the present study, 46 patients were analyzed, predominantly women (87%) whose age (mean ± SD) was 70.1 ± 6.2 years.
In the analysis of the studied population, there were 20 patients with malignant (largest diameter of the dominant nodule, mean ± SD: 21.4 ± 11 mm) and 26 benign (largest diameter of the dominant nodule, mean ± SD: 37.2 ± 17 mm) thyroid tumors. No patient with thyroid malignancy underwent neck dissection; presented medullary or anaplastic carcinoma. In the whole group 43% (n = 20) were 25OHD deficient and 24% (n = 11) insufficient while only 33% (n = 15) exhibited normal 25OHD serum values as assessed at the date of surgery.
Twenty-one patients (45%) underwent HT while 25 patients (55%) TT. The characteristics and preoperative biochemical determinations of the whole population according to the type of surgery is described in Table 1.
Within the HT group of patients, the vast majority, 86% (n = 18) were benign thyroid tumors, with follicular adenoma, multinodular goiter and colloid goiter being the most prevalent pathologies. Only three patients (14%) had malignant thyroid tumors. Two patients had papillary thyroid carcinoma and one follicular carcinoma (Supplementary Table 1).
In the TT group, only 32% (n = 8) presented benign thyroid tumors while 68% (n = 17) harbored thyroid cancer, being papillary thyroid carcinoma the most prevalent type of malignancy (Supplementary Table 1).
Postsurgical biochemical determinations
Considering the whole group, there was 22% of patients with 24 h postsurgical hypocalcaemia. Six months after surgery calcaemia was 9.4 ± 0.67 mg/dL and PTH 42.6 ± 21 pg/mL (Table 2).
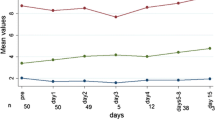
In the TT group at 6 h postoperatively, the proportion of hypocalcaemia was 36% (n = 9), with two cases of severe hypocalcaemia (7.0 and 7.5 mg/dL), without frank symptoms and only one persistent after 24 h. After 24 h, the rate of hypocalcaemia in the TT group was 16% (n = 4), despite having received reposition of calcium when hypocalcaemic at 6 h after surgery. After TT, 24 h postsurgical PTH levels were significantly lower in those patients with 6 h postsurgical hypocalcaemia than in patients with normal calcium values (11.7 ± 9.3 pg/mL vs 31 ± 18 pg/mL, p = 0.02) and a positive correlation between the 6 h calcaemia and 24 h PTH was also observed (r: 0.647, p = 0.003). Regarding magnesium concentrations in patients with TT, magnesium measured at 24 h was significantly lower in 24 h hypocalcaemic patients than in those who were normocalcaemic, 1.6 ± 0.12 vs 1.9 ± 0.16 mg/dL (p = 0.005). Indeed, presurgical magnesium levels in patients who developed hypocalcaemia were also lower than in normocalcaemic patients 1.9 ± 0.07 vs 2.09 ± 0.18 mg/dL (p = 0.03). Regarding postsurgical PTH, in the group of TT there were seven patients with hPT; however, none evolved to definitive hPT, when they were re-evaluated 6 months after surgery.
Regarding 25OHD levels, 44% (n = 11) of TT patients exhibited 25OHD deficiency but only two of them (15%) showed hypocalcaemia at 24 h. No observed correlation between calcaemia and 25OHD levels was either observed.
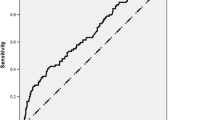
In the HT group, 24 h postsurgical hypocalcaemia occurred in 28.6% (n = 6) of the patients, none within the range of severe hypocalcaemia. There were two cases of hPT in the HT group that evolved to normal PTH values at 6 months. Fourty-three percent (n = 9) of the patients had 25OHD deficiency and five of them (55%) presented hypocalcaemia at 24 h. This proportion was significantly higher than in patients with normal vitamin D values (1 hypocalcaemia out of 11 patients) (p = 0.049) (Fig. 1). Moreover, the correlation between preoperative 25OHD and 24 h calcaemia was positive (r: 0.516, p = 0.02) (Fig. 2). Unlike what was observed in TT, the comparison of the mean Mg concentrations at 24 h of patients with HT who presented hypocalcaemia at 24 h was not different in hypocalcaemic and normocalcaemic patients.
Discussion
One of the main findings of this study is the large amount of transient hypocalcaemia observed in older adults. It is also worth noting that this observation is also valid for a less invasive surgical approach than TT. Moreover, in hemithyroidectomized patients, preoperative 25OHD deficiency was related to lower calcium serum values 24 h after surgery.
Until the present moment there have been several reports of transient postsurgical hypocalcaemia and of its possible predictors. However, most of these studies focused in patients with TT [14]. Plausible mechanisms that can link hypocalcaemia to TT include the inadvertent damage of parathyroid glands [2], although the presence of hypomagnesemia impairing PTH secretion in the context of hypocalcaemia should also be considered [11].
The rate of hypocalcaemia and hPT in the published literature [3, 4], varies according to different cut-off values used for definitions [15]. Furthermore, prophylaxis with calcium and vitamin D supplements, before and after surgery, may also lead to misinterpretations [16].
Several studies have been designed to investigate predictors of postoperative hypocalcaemia [17]. Calcaemia < 8 mg/dl combined with PTH < 10–15 pg/ml, indicate the highest risk of transient and permanent hPT, regardless of the extent of the resection and the type of disease [17]. In a recent meta-analysis, it was found that PTH levels either intra or immediately postsurgery (TT) can predict low calcium serum levels over other possible variables such as age or preoperative 25OHD levels [14]. Conversely, there is paucity of data with regards to predictors of transient hypocalcaemia after HT, probably due to the idea that as the contralateral parathyroid glands are preserved from potential damage, no need for postsurgical calcium assessment is deemed important.
In this study, it was found that the proportion of postoperative hypocalcaemia at 24 h was similar both in patients with HT and TT. However, it should be stated that TT patients also had 6 h postoperative assessement and received oral calcium reposition as per protocol when hypocalcaemia was detected. Severe hypocalcaemia was infrequent, occurring only in two patients post TT who were hypocalcaemic both at 6 and 24 h postsurgery.
As regards to the biochemical predictors of hypocalcaemia in TT patients, 24 h PTH levels were significantly associated with 6 h calcium values after surgery. It is also worth noting that at 24 h lower magnesemia was detected in hypocalcaemic compared to normocalcaemic patients. As previously mentioned, severe hypomagnesemia as described in primary hypomagnesemia, is well known for its interference with PTH secretion [18]. In line with our results, mild, even in the normal low range of magnesium serum concentrations early post thyroidectomy were associated with postsurgical hypocalcemia in two retrospective studies [19, 20].
The lack of an association between 25OHD deficiency and hypocalcaemia in TT patients is rather intriguing. However, an important aspect to be considered is that the risk of parathyroid gland injury is higher in TT and may obscure the role of lower 25OHD status in postsurgical hypocalcaemia [3, 21]. Furthermore, lower preoperative vitamin D levels have been associated with transient hypocalcaemia in TT patients in some publications [22, 23], while this correlation has not been found in other reports [24, 25].
In contrast to what was observed in TT patients, 25OHD deficiency was associated with 24 h hypocalcaemia in the group of HT patients. Given that vitamin D insufficiency and deficiency are highly prevalent in elderly people, ranging from 52 to 87% [26], our findings illustrate the importance of including 25OHD in the preoperative assessment of older adults. In support of this idea, Tripathi et al. [27] reported that preoperative 25OHD deficiency was the single most important factor in predicting postoperative hypocalcaemia in a young group of patients undergoing HT. The American Thyroid Association (ATA) clinical practice guideline on postsurgical hypoparathyroidism, recommends treating vitamin D deficiency before surgery [28]. Yet there is no recommendation in regards to HT or the age of the patient.
It is worth noting that thyroid cancer has increased about three times in the last decades [29], but in contrast there is currently a tendency to carry out more conservative surgical treatments [30] such as HT in exchange for lower treatment-related risks [31]. This change of thyroid cancer surgical management [32,33,34,35,36] has proved that survival is similar when comparing TT vs HT in selected patients with thyroid cancer. According to our findings, in the future, the preoperative evaluation of 25OHD deficiency should become a mandatory step in the workup of patients referred to HT.
As regards benign nodular disease, Erbil et al. [37] also described preoperative 25OHD deficiency together with older age (specifically older than 50 y) and postsurgical PTH, as independent predictors of transient hypocalcaemia in patients undergoing TT. The present study extends these findings to an elderly cohort in whom several patients with benign disease, including multinodular goiter were managed successfully with a more conservative strategy such as HT.
One of the limitations of this study remains the lack of intervention with preoperative administration of Vitamin D to assess its effects on hypocalcaemia. Considering that hypocalcaemia is a main discharge-limiting factor following thyroid surgery, future research should pinpoint the exact role of preoperative Vitamin D supplementation. Another limitation is the lack of information collected in the preoperative file regarding drugs that may alter calcium-phosphoric metabolism.
In other terms, this study has targeted a different age segment not yet explored in previous studies and its findings underscore 25OHD deficiency as a potential risk factor for the development of postoperative complications. Intervention trials showing the benefit of 25OHD repletion are needed.
In conclusion, about a quarter of this aged population, presented transient hypocalcaemia after surgery, with severe hypocalcaemia being an infrequent form. In the TT group postsurgical Mg concentrations seem to have a role in hypocalcaemia while in the HT group, an association between preoperative 25OHD deficiency and 24 h postoperative hypocalcemia was demonstrated.
Data availability
All data and material was collected at Dr. Cesar Milstein Care Unit, Buenos Aires.
Change history
26 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s12020-021-02943-3
References
A.L. Schafer, D. Shoback, Hypocalcemia: Definition, Etiology, Pathogenesis, Diagnosis, and Management. In: Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 9th edn. ed. by J.P. Bilezikian, (American Society for Bone and Mineral Research, John Wiley & Sons, Inc., 2019), p. 646–653.
J. Turner, N. Gittoes, P. Selby, __. Society for endocrinology endocrine emergency guidance: emergency management of acute hypocalcaemia in adult patients. Endocr. Connect. (2016). https://doi.org/10.1530/EC-16-0056
E.B.Y. Filho, R.V. Machry, R. Mesquita, R.S. Scheffel, A.L. Maia, The timing of parathyroid hormone measurement defines the cut-off values to accurately predict postoperative hypocalcemia: a prospective study. Endocrine. (2018). https://doi.org/10.1007/s12020-018-1601-9
O. Edafe, R. Antakia, N. Laskar, L. Uttley, S.P. Balasubramanian, Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br. J. Surg. (2014). https://doi.org/10.1002/bjs.9384
F. Dip, J. Falco, S. Verna, et al. Randomized Controlled Trial Comparing White Light with Near-Infrared Autofluorescence for Parathyroid Gland Identification During Total Thyroidectomy. J. Am. Colleg. Surg. (2019). https://doi.org/10.1016/j.jamcollsurg.2018.12.044
Z. Al-Qurayshi, C.B. Sullivan, A. Schwalje, et al. Presentation and Outcomes of Elderly Patients Undergoing Head and Neck Surgeries: a National Perspective. Otolaryngol. Head Neck Surg. (2020). https://doi.org/10.1177/0194599820911727
V.D. Tarasova, R.M. Tuttle. Current Management of Low Risk Differentiated Thyroid Cancer and Papillary Microcarcinoma. Clin. Oncol. (2017). https://doi.org/10.1016/j.clon.2016.12.009
Z. Wang, C.M. Vyas, O. Van Benschoten, et al. Quantitative Analysis of the Benefits and Risk of Thyroid Nodule Evaluation in Patients ≥70 Years Old. Thyroid. (2018). https://doi.org/10.1089/thy.2017.0655
M.C. Zatelli, L. Lamartina, D. Meringolo, et al. Thyroid nodule recurrence following lobo-isthmectomy: incidence, patient’s characteristics, and risk factors. J. Endocrinol. Investig. (2018). https://doi.org/10.1007/s40618-018-0946-5
M.F. Holick. Vitamin D Deficiency. N. Engl J. Med. (2007). https://doi.org/10.1056/NEJMra070553
C.S. Anast, J.M. Mohs, S.L. Kaplan, T.W. Burns. Evidence for Parathyroid Failure in Magnesium Deficiency. Science. (1972). https://doi.org/10.1126/science.177.4049.606
M.F. Holick, N.C. Binkley, H.A. Bischoff-Ferrari, et al., Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 96(7), 1911–1930 (2011). https://doi.org/10.1210/jc.2011-0385
R.V. Lloyd, R.Y. Osamura, G. Klöppel, J. Rosai, WHO Classification of Tumours of Endocrine Organs, 4th edn. (IARC print publications. WHO Press, World Health Organization, Switzerland, 2017).
A.E.L. McMurran, R. Blundell, V. Kim, Predictors of post-thyroidectomy hypocalcaemia: a systematic and narrative review. J. Laryngol. Otol. 134(6), 541–552 (2020). https://doi.org/10.1017/S0022215120001024
H.M. Mehanna, A. Jain, H. Randeva, J. Watkinson, A. Shaha, Postoperative hypocalcemia-The difference a definition makes. Head Neck. Published online 2009:NA-NA. https://doi.org/10.1002/hed.21175
D.R. Chadwick, Hypocalcaemia and permanent hypoparathyroidism after total/bilateral thyroidectomy in the BAETS Registry. Gland Surg. (2017) https://doi.org/10.21037/gs.2017.09.14
D.M. Shoback, J.P. Bilezikian, A.G. Costa, et al. Presentation of Hypoparathyroidism: Etiologies and Clinical Features. J. Clin. Endocrinol. Metab. (2016) https://doi.org/10.1210/jc.2015-3909
S.M. Suh, A.H. Tashjian, N. Matsuo, D.K. Parkinson, D. Fraser, Pathogenesis of Hypocalcemia in Primary Hypomagnesemia: Normal End-Organ Responsiveness to Parathyroid Hormone, Impaired Parathyroid Gland Function. J. Clin. Investig. (1973) https://doi.org/10.1172/JCI107159
A. Garrahy, M.S. Murphy, P. Sheahan, Impact of postoperative magnesium levels on early hypocalcemia and permanent hypoparathyroidism after thyroidectomy: Magnesium Levels and Postthyroidectomy Hypocalcemia. Head Neck. (2016) https://doi.org/10.1002/hed.23937
W. Wang, C. Meng, Q. Ouyang, J. Xie, X. Li, Magnesemia: an independent risk factor of hypocalcemia after thyroidectomy. CMAR. (2019) https://doi.org/10.2147/CMAR.S218179
C.S.P. Soares, J.V. Tagliarini, G.M.F.S. Mazeto, Preoperative vitamin D level as a post-total thyroidectomy hypocalcemia predictor: a prospective study. Braz. J. Otorhinolaryngol. (2021) https://doi.org/10.1016/j.bjorl.2019.07.001
Y. Erbil, U. Barbaros, B. Temel, et al. The impact of age, vitamin D3 level, and incidental parathyroidectomy on postoperative hypocalcemia after total or near total thyroidectomy. Am. J. Surg. (2009) https://doi.org/10.1016/j.amjsurg.2008.01.032
T. Al-Khatib, A.M. Althubaiti, A. Althubaiti, H.H. Mosli, R.O. Alwasiah, L.M. Badawood, Severe Vitamin D Deficiency: A Significant Predictor of Early Hypocalcemia after Total Thyroidectomy. Otolaryngol. Head Neck Surg. (2015) https://doi.org/10.1177/0194599814561209
Y. Lin, H.L. Ross, C.D. Raeburn, et al. Vitamin D deficiency does not increase the rate of postoperative hypocalcemia after thyroidectomy. Am. J. Surg. (2012) https://doi.org/10.1016/j.amjsurg.2012.10.001
G. Manzini, F. Malhofer, T. Weber, Can preoperative vitamin D deficiency predict postoperative hypoparathyroidism following thyroid surgery? Langenbecks Arch. Surg. (2019) https://doi.org/10.1007/s00423-019-01748-3
B. Oliveri, L. Plantalech, A. Bagur, et al. High prevalence of vitamin D insufficiency in healthy elderly people living at home in Argentina. Eur. J. Clin. Nutr. (2004). https://doi.org/10.1038/sj.ejcn.1601786
M. Tripathi, R. Karwasra, S. Parshad, Effect of preoperative vitamin D deficiency on postoperative hypocalcemia after thyroid surgery. Thyroid Res. (2014). https://doi.org/10.1186/1756-6614-7-8
L.A. Orloff, S.M. Wiseman, V.J. Bernet, et al. American Thyroid Association Statement on Postoperative Hypoparathyroidism: Diagnosis, Prevention, and Management in Adults. Thyroid. (2018) https://doi.org/10.1089/thy.2017.0309
L. Davies, L.G.T. Morris, M. Haymart, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: the Increasing Incidence of Thyroid Cancer. Endocr. Pract. (2015) https://doi.org/10.4158/EP14466.DSCR
J.J. Díez, A. Oleaga, C. Álvarez-Escolá, T. Martín, J.C. Galofré, Guía clínica para el manejo de pacientes con carcinoma diferenciado de tiroides de bajo riesgo. Endocrinología y Nutrición. (2015) https://doi.org/10.1016/j.endonu.2015.02.006
S. Ahmadi, J.M. Gonzalez, M. Talbott, et al. Patient Preferences Around Extent of Surgery in Low-Risk Thyroid Cancer: a Discrete Choice Experiment. Thyroid. (2020) https://doi.org/10.1089/thy.2019.0590
K. Matsuzu, K. Sugino, K. Masudo, et al. Thyroid Lobectomy for Papillary Thyroid Cancer: long-term Follow-up Study of 1088 Cases. World J. Surg. (2014) https://doi.org/10.1007/s00268-013-2224-1
B.M. Barney, Y.J. Hitchcock, P. Sharma, D.C. Shrieve, J.D. Tward, Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck. (2011) https://doi.org/10.1002/hed.21504
A.H. Mendelsohn, D.A. Elashoff, E. Abemayor, M.A. St John, Surgery for Papillary Thyroid Carcinoma: Is Lobectomy Enough? Arch. Otolaryngol. Head Neck Surg. (2010) https://doi.org/10.1001/archoto.2010.181
I.J. Nixon, I. Ganly, S.G. Patel, et al. Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery. (2012) https://doi.org/10.1016/j.surg.2011.08.016
M.A. Adam, J. Pura, L. Gu, et al. Extent of Surgery for Papillary Thyroid Cancer Is Not Associated With Survival: an Analysis of 61,775 Patients. Ann. Surg. (2014) https://doi.org/10.1097/SLA.0000000000000925
Y. Erbil, Predictive Value of Age and Serum Parathormone and Vitamin D3 Levels for Postoperative Hypocalcemia After Total Thyroidectomy for Nontoxic Multinodular Goiter. Arch. Surg. (2007) https://doi.org/10.1001/archsurg.142.12.1182
Acknowledgements
We would like to thank the Endocrine and Surgery residents of Dr. Cesar Milstein Unit Care for their support in the follow-up of patients and collection of data.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [B.M.P., S.N., M.A.Y., L.M., S.L., S.C., M.T., F.C., F.M.P. and B.G.]. The first draft of the paper was written by [B.M.P., M.E., S.C. and B.G.] and all authors commented on previous versions of the paper. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent to participate
All participants gave a written voluntary consent to participate.
Consent for publication
Yes.
Ethical approval
The protocol was approved by the Ethics Committee for human studies of Dr. Cesar Milstein Care Unit, Buenos Aires.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Barbier, M.P., Mingote, E., Sforza, N. et al. Incidence and predictive factors of postoperative hypocalcaemia according to type of thyroid surgery in older adults. Endocrine 75, 276–283 (2022). https://doi.org/10.1007/s12020-021-02840-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02840-9