Abstract
Biofilm formation is an important physiological process in Staphylococcus aureus (S. aureus) that can cause infections in humans. In this study, the ability of 36 methicillin-resistant S. aureus (MRSA) clinical isolates to form biofilm was studied based on genotypic and phenotypic approaches. These isolates were genotyped based on the microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) and biofilm-associated genes (icaAD) via polymerase chain reactions. Phenotyping was performed based on the determination of the strength of biofilm formation of MRSA isolates in vitro. The most prevalent MSCRAMMs and biofilm-associated genes were clfA, eno, and icaD, followed by clfB. The fnbB (38.9%) and ebpS (11.1%) occurred less frequently among the MRSA isolates, while bbp and fnbA genes were absent from all isolates. The MRSA isolates were mostly moderate to strong biofilm formers, despite the heterogeneity of the MSCRAMM profiles. MRSA isolates from different infection sources (primary, catheter-related bloodstream, or secondary infections) were capable of forming strong biofilms. However, persistent bacteraemia was observed only in 19.4% of the MRSA-infected individuals. This study suggested that persistent MRSA bacteraemia in patients might not be associated with the biofilm-forming ability of the isolates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biofilm, a polymeric matrix formed by a community of bacteria poses a major threat to human health. These sessile bacterial communities show inherent resistance to antimicrobial agents and disinfectants, thereby causing progression to chronic and persistent infections among infected individuals (Costerton et al. 1999; Francois et al. 2000; Jones et al. 2001; Lewis 2010). Recurrent infections have also been associated with biofilm-forming bacteria (Francois et al. 2000; Jones et al. 2001). Staphylococcus aureus (S. aureus) is a major target for biofilm studies as it can cause recalcitrant biofilm-associated infections such as osteomyelitis, periodontitis, peri-implantitis, chronic wound infection, chronic rhinosinusitis, endocarditis, and ocular infection (Archer et al. 2011). This organism is usually introduced into sterile sites in the body through implantation of medical devices such as orthopaedic implants, indwelling medical devices, or derived primarily from temporary bacteraemia (Costerton et al. 2005; Kiedrowski and Horswill 2011; Kwon et al. 2008).
Formation of biofilm involves four stages, i.e., initial attachment of bacteria to a substratum, interface, or each other, followed by the formation of microcolonies through cell aggregation and accumulation, biofilm formation and maturation, and lastly biofilm detachment and dispersal (Costerton et al. 1999). The S. aureus biofilm matrix often comprises of different components such as polysaccharide intercellular antigen (PIA), surface adhesion proteins, surface-associated proteins, extracellular DNA (eDNA), and host factors (Cue et al. 2012; Foster et al. 2014; Montanaro et al. 2011; O'Gara 2007). These components play an important role in establishing persistent and unresolved infections in patients infected by S. aureus.
The biofilm formers are often associated with increased antimicrobial resistance, due to the protective barrier that the extracellular matrix builds around the bacterial cells and an increased rate of horizontal gene transfer among the accumulated cells (Cascioferro et al. 2020a). Therefore, antimicrobial treatment remains an important challenge in biofilm-associated infections (Lebeaux et al. 2014). Recent research efforts have focused on developing antibiofilm treatment, which has an advantage over conventional antibiotic treatment due to its low selective pressure against bacterial cells, hence could potentially prevent the development of antimicrobial resistance (Cascioferro et al. 2020b; Parrino et al. 2019, 2020). The discovery of small organic molecules with promising in vitro and in vivo antibiofilm activity has been identified as a potential therapeutic strategy for persistent infections caused by biofilm formers, including methicillin-resistant S. aureus (MRSA) (Cascioferro et al. 2020a). These synthetic molecules could prevent biofilm formation or eradicate existing biofilm via inhibiting microbial attachment, interfering with the quorum sensing system of the bacterial cells, altering bacterial regulatory mechanisms, and direct degradation of the biofilm structure (Parrino et al. 2019). Therefore, understanding the main molecular mechanisms or cell surface proteins of biofilm-forming MRSA is essential to identify potential biomarkers for antibiofilm agents and the subsequent development of targeted therapies.
Different genotypic and phenotypic approaches have been used to study the biofilm formation in MRSA. Genetic screening for the intercellular adhesion (icaADBC) genes and microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) has been reported (Arciola et al. 2001; Tristan et al. 2003). Besides that, the screening for phenotypic characteristics of biofilm-forming S. aureus, such as slime production on Congo red agar, biofilm assay on microtitre plates, and colony morphology study using a confocal laser scanning, transmission, or scanning electron microscope, has also been employed by researchers (Archer et al. 2011; O'Toole 2011; Szczuka et al. 2013). The microbiological aspects of the MRSA biofilm have been the focus of previous studies, but little is known about the correlation between the persistence of infection with the biofilm-forming characteristics (microbiological aspects) of MRSA. Hence, this study aimed to determine the relationship between clinical characteristics and biofilm formation ability in MRSA using phenotypic and genotypic methods.
Materials and methods
Hospital setting and ethical approval
The study was conducted at the University Malaya Medical Centre (UMMC), a tertiary teaching hospital in Kuala Lumpur, Malaysia. Ethics approval was obtained from the Medical Ethics Committee of UMMC on 7th June 2014 (MEC-ID: 20145-168) and the study conformed to the principles embodied in the Declaration of Helsinki.
Bacterial isolates
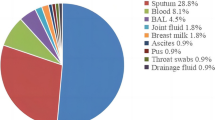
Thirty-six non-duplicated MRSA isolates were obtained from the blood samples of adult patients aged ≥ 16 years old within the 2-year study period (January 2014 to December 2015). The genotypes (agr and SCCmec typing) and phenotypes (antimicrobial susceptibility profiles) of the MRSA isolates are reported in our previous study (Niek et al. 2019).
Molecular characterization of S. aureus adhesive and surface-associated genes
Conventional polymerase chain reaction (PCR) was performed to screen for S. aureus adhesins, commonly known as microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) as described by Tristan et al. (Tristan et al. 2003). Simplex PCR was carried out to detect bbp, cna, ebpS, and eno genes. Multiplex PCR was performed to amplify fnbA, fnbB, fib, clfA, and clfB genes. The thermocycling condition included an initial denaturation at 94 °C for 5 min, followed by 25 cycles of amplification (denaturation at 94 °C for 1 min, annealing at 55 °C for 1 min, and extension at 72 °C for 1 min). The reaction was terminated at 72 °C for 10 min. PCR products were analysed by agarose gel electrophoresis. Representative amplicons were purified and sent for DNA sequencing to validate their identities. All PCRs were performed at least twice to confirm reproducibility.
MRSA isolates were screened for biofilm-associated genes, namely, icaA and icaD, based on the protocol described by Vasudevan et al. (2003). The primers pair ICAAF (CCT AAC TAA CGA AAG GTA G) and ICAAR (AAG ATA TAG CGA TAA GTG C) with an amplicon size of 1,315 bp were used to detect icaA gene; meanwhile, the primer pair ICADF (AAA CGT AAG AGA GGT GG) and ICADR (GGC AAT ATG ATC AAG ATA C) with an amplicon size of 381 bp was used to detect icaD gene in the MRSA isolates. The PCR reaction mix (25 µL) consisted of 1 × buffer, 1.25 mM MgCl2, 100 μM of each nucleotide, 0.5 μM of each primer, 0.625 U of Taq polymerase, and approximately 100 ng of bacterial DNA. The thermocycling condition included an initial denaturation at 94 °C (5 min), followed by 30 cycles of denaturation at 92 °C for 45 s, annealing at 49 °C for 45 s, and elongation at 72 °C for 1 min. The reaction was terminated at 72 °C for 7 min. Representative amplicons were sent for DNA sequencing to validate their identity.
Biofilm formation assay
Biofilm formation assay was performed on the MRSA isolates using previously described protocols (O'Toole 2011; Stepanović et al. 2007; Vasudevan et al. 2003). Briefly, the MRSA isolates were grown in trypticase soy broth (TSB) overnight at 37 °C. The cell concentration was adjusted to 0.5 McFarland standard and diluted to a 1:100 ratio in sterile TSB containing 0.25% glucose. Next, 200 µL of the diluted cell suspension was added into a sterile flat-bottom polystyrene tissue culture plate and incubated at 37 °C for 24 h. The wells were washed three times with 200 µL of phosphate-buffered saline (PBS, pH 7.4) to remove planktonic cells. Sessile bacterial cells left in the wells were heat-fixed at 60 °C for 1 h. The adhered cells were then stained with 0.1% crystal violet solution for 15 min, washed with distilled water, and air-dried in an inverted position overnight. The crystal violet dye was solubilized using absolute ethanol, and the absorbance (OD) values were determined using a spectrophotometer (570 nm). Each isolate was tested in triplicates and the assay was repeated thrice. To interpret biofilm formation in the MRSA isolates, the cutoff value (ODc) was defined as three standard deviations (SD) above the mean OD of the negative control (Stepanović et al. 2007). The absorbance values of the isolates were divided into the following categories: OD ≤ ODc = non-biofilm producer; ODc < OD ≤ 2 × ODc = weak biofilm producer; 2 × ODc < OD ≤ 4 × ODc = moderate biofilm producer; and 4 × ODc < OD = strong biofilm producer.
Clinical data extraction
Patients’ data including age, ethnicity, gender, site of acquisition of MRSA (hospital or community-acquired), and clinical characteristics (sources of bacteraemia, the persistence of bacteraemia, and recurrent infection within 6 months) were retrieved from the Medical Record Department of UMMC for correlation analysis. The source of MRSA bacteraemia was defined as primary, secondary, and catheter-related bloodstream infection (CRBSI) based on data collected from patient’s clinical note and the hospital’s Infection Control Department’s database. Persistent MRSA bacteraemia is defined as a positive blood culture taken ≥ 7 days after the initiation of glycopeptide treatment (Ok et al. 2013).
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics 27.0 software (IBM Corp., Armonk, USA). Descriptive statistics are expressed as number and percentage. Categorical variables were compared using Fisher’s exact test due to the small sample size. Univariate comparisons were made between biofilm-forming ability, MSCRAMMs and ica genes (and combinations of genes), patients’ comorbidities, in-hospital mortality, and the persistence of MRSA bacteraemia. Statistical significance is indicated by a p-value of less than or equal to 0.05.
Results
Prevalence of MSCRAMMs and ica genes in the MRSA isolates
The most prevalent MSCRAMM genes were clfA (clumping factor A) and eno (laminin-binding protein) being present in all isolates, followed by clfB (clumping factor B) in 94.4% of the isolates. More than half of the MRSA isolates were tested positive for cna (collagen-binding protein; 88.9%) and fib (fibrinogen-binding protein; 50%) genes. To a lesser extent, the MRSA isolates were detected with the presence of fnbB (fibronectin-binding protein B; 38.9%) and ebpS (elastin-binding protein; 11.1%) in their genomes. All the isolates were negative for bbp (bone sialoprotein-binding protein) and fnbA (fibronectin-binding protein A) genes. The majority of the MRSA isolates were positive for the icaA gene (77.8%) whereas the icaD gene was present in all isolates. The presence of specific biofilm-associated genes was not significantly associated with the biofilm-forming ability of the MRSA isolates (p-values > 0.05). The prevalence of the MSCRAMMs and ica genes in the different groups of MRSA biofilm formers is summarized in Table 1.
Biofilm formation ability of the MRSA isolates
All MRSA isolates tested were biofilm formers. However, the isolates varied in their ability to form a biofilm. One isolate was a weak biofilm former, two isolates were moderate biofilm formers, and 33 isolates were strong biofilm formers. The biofilm formers were grouped into nine different profiles according to different combinations of biofilm adhesion and formation genes, arbitrarily designated as M1–M9 (Table 2). For the single weak biofilm former, it was found to possess cna, eno, ebpS, fib, clfA, clfB, icaA, and icaD genes. The genotypic, phenotypic (strength of biofilm formation), and clinical characteristics (caused persistent bacteraemia or otherwise) of all MRSA isolates are compiled in Table 2 to infer the relationship among all these factors. A heterogeneous presence of biofilm-associated genes was observed among all the biofilm formers. The persistence of MRSA bacteraemia and the biofilm-forming ability of the isolates was not significantly associated with specific MSCRAMMs and ica gene profile (p-values > 0.05).
Clinical characteristics of patients with MRSA infection
The clinical characteristics of patients infected by the MRSA isolates examined in this study are summarized in Table 3. Generally, MRSA bacteraemia was relatively common among the elderly (75%), male gender (55.6%), and Malay population (41.7%). In terms of the acquisition site, most of the MRSA bacteraemia (63.9%) were acquired and developed in hospital, followed by 11 cases (30.6%) with healthcare-associated community-onset (residents in long-term care facilities such as nursing home or those undergoing frequent haemodialysis), and two cases of community-acquired MRSA in patients with no known risk factors. The MRSA infections were mostly clinically manifested as primary bacteraemia (44.4%), followed by CRBSI (30.6%), and secondary infections (25.0%). In terms of treatment outcomes, persistent infection was reported in seven patients, and four with recurrent infections within 6 months after MRSA clearance from the hospital. The observed differences between the persistent and non-persistent MRSA bacteraemia in association with the clinical, phenotypic, and genotypic characteristics were not statistically significant (p-values > 0.05).
Discussion
All MRSA isolates harboured at least four MSCRAMM genes, with one-third of the isolates (n = 12) simultaneously carrying six MSCRAMM genes in their genomes. The majority of the MRSA isolates (61%) lacked the genes encoding for fibronectin-binding proteins (FnBPs), despite all of them harboured at least two fibrinogen receptor genes. The occurrence of at least two genes encoding for fibrinogen receptor (fib, clfA, or clfB) and laminin-binding protein (eno) in all tested isolates concurred with the previous finding reported by Tristan et al. (Tristan et al. 2003), suggesting that S. aureus might harbour functionally redundant MSCRAMMs. This notion is further supported by the observation that the MRSA isolates could form strong biofilm despite their varying MSCRAMM gene profiles, some with fewer genes compared to the others. We observed the presence of icaD in all MRSA isolates within our sample pool, but only 77.8% of the isolates harboured the icaA gene. This finding is uncommon among S. aureus as the ica genes are clustered in a single operon (icaADBC), and their expressions are tightly regulated by both global and specific regulatory factors like SarA or IcaR (Cue et al. 2012). The ica operon encodes for the synthesis of the polysaccharide intercellular adhesion (PIA) protein that is the major component of S. aureus biofilm. Although infrequent, failure to detect a specific ica gene from the icaADBC operon has been documented among bovine isolates of S. aureus (Fluit 2012). Failure to detect icaA in some of the MRSA isolates despite the presence of icaD could have been attributed to gene excision events or mutation at the primer-binding site. Nonetheless, all MRSA isolates that lacked an (intact) icaA gene were strong biofilm-formers. This observation supports the previous notion that the ica operon is not essential for the formation of biofilm by MRSA (Archer et al. 2011).
Other strain-specific mechanisms that involve the use of protein A (Spa) or FnBPs (through autolysin and sigB regulation) may contribute to biofilm formation in a PIA-independent manner when ica operon is absent (Archer et al. 2011). Such mechanisms are often associated with the formation of biofilm in human MRSA isolates (McCarthy et al. 2015). However, only one-third of the biofilm-forming MRSA isolates examined in this study harboured the fnbB gene; meanwhile, fnbA was absent from all isolates. Nonetheless, previous studies have shown that each fnb gene could form strong biofilm when expressed in MRSA, even though in the absence of the other (O’Neill et al. 2008; McCourt et al. 2014). Furthermore, the high prevalence of clf, eno, and cna genes among the isolates in this study indicates that the presence of these major MSCRAMM proteins was sufficient to produce strong biofilm in MRSA. Therefore, the main molecular mechanisms leading to strong biofilm formation in local MRSA isolates could be attributable to the presence of these genes. The observation that few isolates formed moderate/weak biofilm despite sharing identical MSCRAMM gene profile with strong biofilm formers could be due to other factors such as major autolysin and extracellular DNA expression (McCarthy et al. 2015). Nonetheless, further investigation is required to test this hypothesis.
In our earlier report, we identified three agr genotypes among the MRSA isolates examined in this study (Niek et al. 2019). Most of the isolates examined in this study were of agr-type I (94.4%), followed by agr-type II (2.8%) and agr-type III (2.8%). The MRSA isolates of different agr genotypes (agr-type I, II, III) could all form biofilm and harboured a combination of multiple biofilm-associated genes. Previous studies had come to contradicting conclusions on the correlation between agr genotypes and biofilm formation capacity of the S. aureus isolates. Some studies observed a higher tendency to form biofilm among the isolates of certain agr genotype (Kawamura et al. 2011; Kwiecinski et al. 2019), while others observed no differences (Cha et al. 2013; Croes et al. 2009). The agr gene is an important modulator in the establishment and detachment process of S. aureus biofilm (Boles & Horswill 2008). The agr operon regulates the expression of multiple virulence factors in S. aureus (Arvidson & Tegmark 2001). The expression of the agr favours the production of secreted virulence factors over cell-associated factors. Conversely, the loss of function of the agr operon will induce the formation of biofilm and selects for S. aureus isolates with reduced susceptibility to vancomycin (Szabó 2009). Moreover, the expression of the SCCmec-associated β-lactamase system in MRSA has been experimentally proven to repress the transcription of agr operon (Choe et al. 2018). Therefore, it would be of great interest to investigate the differential expression of the various agr-types of the MRSA isolates in a future study to elucidate its association with the expression of the biofilm-associated genes and subsequently the strength of the biofilm formed.
Our study has shown that MRSA bacteraemia irrespective of sources (primary, CRBSI, or secondary) had a strong biofilm-forming capacity. A similar observation was made by Cha and colleagues (Cha et al. 2013), whereby primary bacteraemia and CRBSI did not show a significant difference in the prevalence of biofilm-forming MRSA, although biofilm formers were significantly associated with the presence of invasive medical devices when compared to biofilm non-formers. However, a recent study observed that the invasive S. aureus isolates from intravenous line-associated infections were particularly proficient in the formation of biofilm compared to bacteraemia without focus (Kwiecinski et al. 2019). Another earlier study has also shown a significantly higher prevalence of strong biofilm-forming MRSA in device-related orthopaedic infections compared to non-device-related infections and colonizers (Kawamura et al. 2011). Device-related MRSA infection has been associated with more severe clinical outcomes and results in a greater risk of patient mortality (Cha et al. 2013). Our study observing the similar biofilm-forming capacities of MRSA isolates from primary bacteraemia and CRBSI suggested that other factors could be affecting clinical outcomes. Other risk factors such as underlying diseases, older age, and pre-admission residences could have a greater impact on the patient’s clinical outcome compared to the MRSA’s ability to form biofilm (Eseonu et al. 2011; Yahav et al. 2016).
Our findings concurred with a recent study that reported a lack of obvious relationship between the biofilm-forming capacity of S. aureus and persistence of infection measured based on the presence of residual symptoms (Kwiecinski et al. 2019). The correlation between persistent bacteraemia and the biofilm formation ability of the MRSA isolates could not be made in this study. All MRSA isolates, with or without association with persistent bacteraemia, carried a multitude of biofilm-associated genes and formed biofilm. Nevertheless, not all isolates could form strong biofilms despite sharing similar MSCRAMMs and ica gene profiles. This observation could be due to the variable expressions of the biofilm-associated genes, controlled by other gene regulators in the MRSA genome. The absence of direct association between biofilm formation and persistent bacteraemia has led us to infer that the development of persistent MRSA bacteraemia might have been caused by other factors such as underlying host conditions, the severity of infections, and pathogenicity of the organism. Nonetheless, we should take note of the varying biofilm-forming ability of MRSA in vitro and in vivo, due to the vastly different growth environments and the involvement of host immunity factors (Archer et al. 2011).
Conclusions
In summary, our findings suggested that persistent MRSA bacteraemia in patients was not significantly associated with the biofilm-forming ability of the isolates. Furthermore, the different combinations of biofilm-associated genes and clinical characteristics of the MRSA isolates were not found associated with persistent bacteraemia. This study was limited by the low number of MRSA isolates associated with persistent bacteraemia. Nevertheless, our findings provide an insight into the low probability, if not total absence, of a correlation between biofilm-former and persistent MRSA bacteraemia.
Data availability
All data generated or analysed during this study are included in this published article.
References
Archer NK, Mazaitis MJ, Costerton JW, Leid JG, Powers ME, Shirtliff ME (2011) Staphylococcus Aureus Biofilms Virulence 2:445–459
Arciola CR, Baldassarri L, Montanaro L (2001) Presence of icaA and icaD genes and slime production in a collection of staphylococcal strains from catheter-associated infections. J Clin Microbiol 39:2151–2156
Arvidson S, Tegmark K (2001) Regulation of virulence determinants in Staphylococcus aureus. Int J Med Microbiol 291:159–170
Boles BR, Horswill AR (2008) agr-Mediated dispersal of Staphylococcus aureus biofilms. PLOS Pathog 4:e1000052
Cascioferro S, Carbone D, Parrino B, Pecoraro C, Giovannetti E, Cirrincione G, Diana P (2020a) Therapeutic strategies to counteract antibiotic resistance in MRSA biofilm-associated infections. ChemMedChem 16:65–80
Cascioferro S, Parrino B, Carbone D, Schillaci D, Giovannetti E, Cirrincione G, Diana P (2020b) Thiazoles, their benzofused systems, and thiazolidinone derivatives: Versatile and promising tools to combat antibiotic resistance. J Med Chem 63:7923–7956
Cha J-O, Yoo JI, Yoo JS, Chung H-S, Park S-H, Kim HS et al (2013) Investigation of biofilm formation and its association with the molecular and clinical characteristics of methicillin-resistant Staphylococcus aureus. Osong Public Health Res Perspect 4:225–232
Choe D, Szubin R, Dahesh S, Cho S, Nizet V, Palsson B et al (2018) Genome-scale analysis of methicillin-resistant Staphylococcus aureus USA300 reveals a tradeoff between pathogenesis and drug resistance. UK-Sci Rep 8:2215
Costerton JW, Montanaro L, Arciola CR (2005) Biofilm in implant infections: its production and regulation. Int J Artif Organs 28:1062–1068
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science (new York, NY) 284:1318–1322
Croes S, Deurenberg RH, Boumans M-LL, Beisser PS, Neef C, Stobberingh EE (2009) Staphylococcus aureus biofilm formation at the physiologic glucose concentration depends on the S. aureus lineage. BMC Microbiol 9:229.
Cue D, Lei M, Lee C (2012) Genetic regulation of the intercellular adhesion locus in staphylococci. Front Cell Infect Microbiol 2:38
Eseonu KC, Middleton SD, Eseonu CC (2011) A retrospective study of risk factors for poor outcomes in methicillin-resistant Staphylococcus aureus (MRSA) infection in surgical patients. J Orthop Surg Res 6:25
Fluit AC (2012) Livestock-associated Staphylococcus aureus. Clin Microbiol Infect 18:735–744
Foster TJ, Geoghegan JA, Ganesh VK, Höök M (2014) Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat Rev Microbiol 12:49–62
Francois P, Schrenzel J, Stoerman-Chopard C, Favre H, Herrmann M, Foster TJ et al (2000) Identification of plasma proteins adsorbed on hemodialysis tubing that promote Staphylococcus aureus adhesion. J Lab Clin Med 135:32–42
Jones SM, Morgan M, Humphrey TJ, Lappin-Scott H (2001) Effect of vancomycin and rifampicin on methicillin-resistant Staphylococcus aureus biofilms. Lancet 357:40–41
Kawamura H, Nishi J, Imuta N, Tokuda K, Miyanohara H, Hashiguchi T et al (2011) Quantitative analysis of biofilm formation of methicillin-resistant Staphylococcus aureus (MRSA) strains from patients with orthopaedic device-related infections. FEMS Immunol Med Microbiol 63:10–15
Kiedrowski MR, Horswill AR (2011) New approaches for treating staphylococcal biofilm infections. Ann NY Acad Sci 1241:104–121
Kwiecinski JM, Jacobsson G, Horswill AR, Josefsson E, Jin T (2019) Biofilm formation by Staphylococcus aureus clinical isolates correlates with the infection type. Infect Dis 51:446–451
Kwon AS, Park GC, Ryu SY, Lim DH, Lim DY, Choi CH et al (2008) Higher biofilm formation in multidrug-resistant clinical isolates of Staphylococcus aureus. Int J Antimicrob Ag 32:68–72
Lebeaux D, Ghigo J-M, Beloin C (2014) Biofilm-related infections: Bridging the gap between clinical management and fundamental aspects of recalcitrance toward antibiotics. Microbiol Mol Biol Rev 78:510–543
Lewis K (2010) Persister Cells Ann Rev Microbiol 64:357–372
McCarthy H, Rudkin JK, Black NS, Gallagher L, O’Neill E, O’Gara JP (2015) Methicillin resistance and the biofilm phenotype in Staphylococcus aureus. Front Cell Infect Microbiol 5:1
McCourt J, O’Halloran DP, McCarthy H, O’Gara JP, Geoghegan JA (2014) Fibronectin-binding proteins are required for biofilm formation by community-associated methicillin-resistant Staphylococcus aureus strain LAC. FEMS Microbiol Lett 353:157–164
Montanaro L, Poggi A, Visai L, Ravaioli S, Campoccia D, Speziale P et al (2011) Extracellular DNA in biofilms. Int J Artif Organs 34:824–831
Niek WK, Teh CSJ, Idris N, Thong KL, Ponnampalavanar S (2019) Predominance of ST22-MRSA-IV clone and emergence of clones for methicillin-resistant Staphylococcus aureus clinical isolates collected from a tertiary teaching hospital over a two-year period. Jpn J Infect Dis 72:228–236
O’Gara JP (2007) ica and beyond: Biofilm mechanisms and regulation in Staphylococcus epidermidis and Staphylococcus aureus. FEMS Microbiol Lett 270:179–188
Ok HS, Lee HS, Park MJ, Kim KH, Kim BK, Wi YM et al (2013) Predictors and clinical outcomes of persistent methicillin-resistant Staphylococcus aureus bacteremia: a prospective observational study. Korean J Intern Med 28:678–686
O’Neill E, Pozzi C, Houston P, Humphreys H, Robinson DA, Loughman A et al (2008) A novel Staphylococcus aureus biofilm phenotype mediated by the fibronectin-binding proteins, FnBPA and FnBPB. J Bacteriol 190:3835–3850
O’Toole GA (2011) Microtiter dish biofilm formation assay. J vis Exp 2011:2437
Parrino B, Carbone D, Cirrincione G, Diana P, Cascioferro S (2020) Inhibitors of antibiotic resistance mechanisms: clinical applications and future perspectives. Future Med Chem 12:357–359
Parrino B, Schillaci D, Carnevale I, Giovannetti E, Diana P, Cirrincione G, Cascioferro S (2019) Synthetic small molecules as anti-biofilm agents in the struggle against antibiotic resistance. Eur J Med Chem 161:154–178
Stepanović S, Vuković D, Hola V, Bonaventura GD, Djukić S, Ćirković I et al (2007) Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 115:891–899
Szabó J (2009) hVISA/VISA: Diagnostic and therapeutic problems. Expert Rev Anti-Infe 7:1–3
Szczuka E, Urbańska K, Pietryka M, Kaznowski A (2013) Biofilm density and detection of biofilm-producing genes in methicillin-resistant Staphylococcus aureus strains. Folia Microbiol 58:47–52
Tristan A, Ying L, Bes M, Etienne J, Vandenesch F, Lina G (2003) Use of multiplex PCR to identify Staphylococcus aureus adhesins involved in human hematogenous infections. J Clin Microbiol 41:4465–4467
Vasudevan P, Nair MKM, Annamalai T, Venkitanarayanan KS (2003) Phenotypic and genotypic characterization of bovine mastitis isolates of Staphylococcus aureus for biofilm formation. Vet Microbiol 92:179–185
Yahav D, Yassin S, Shaked H, Goldberg E, Bishara J, Paul M et al (2016) Risk factors for long-term mortality of Staphylococcus aureus bacteremia. Eur J Clin Microbiol 35:785–790
Acknowledgements
The authors would like to thank the University of Malaya for providing research facilities and Graduate Research Assistant Scheme (GRAS).
Funding
This work was supported by the Malaysian Ministry of Higher Education Fundamental Research Grant Scheme (FRGS) (Grant Number: FP016-2014B) and International Research Funding (Grant number: IF004-2020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Medical Ethics Committee of University Malaya Medical Centre (UMMC) on 7th June 2014 (MEC-ID: 20,145–168) and had conformed to the principles embodied in the Declaration of Helsinki.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niek, W.K., Teh, C.S.J., Idris, N. et al. Investigation of biofilm formation in methicillin-resistant Staphylococcus aureus associated with bacteraemia in a tertiary hospital. Folia Microbiol 66, 741–749 (2021). https://doi.org/10.1007/s12223-021-00877-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-021-00877-x