Abstract
The military’s primary mission is to prevent, fight, and win wars. A critical key to its success is the military’s dual mission of force health protection that translates to preventing and treating the physical and psychological wounds of war in order to preserve the fighting force. To accomplish both missions, the military relies extensively on documenting its lessons learned to build upon its successes and prevent avoidable disasters caused by repeating its failures. The military’s commitment to learning battlefield lessons are directly responsible for unparalleled technological and medical, life-saving advances that greatly benefit both military and private sectors. However, the evolution of modern industrialized warfare’s capacity to kill, maim, and terrorize has exceeded the limits of human endurance whereby psychiatric casualties have outnumbered the total of combatants, both wounded- and killed-in-action, since the Second World War. Psychiatric attrition and skyrocketing costs associated with psychiatric treatment and disability compensation threaten the military’s capacity to accomplish its primary mission as well as risk straining the finances of society, thereby presenting a significant mental health dilemma. Central to the military’s mental health dilemma are two competing alternatives: (1) to fulfill its moral, ethical, and legal obligation of preventing and treating war stress injuries by learning from its documented lessons learned, or (2) develop strategies to avoid learning its war trauma lessons in order to avoid psychiatric attrition, treatment, and pensions. The first option conjures deep-seated fears of mass evacuation syndromes should the military treat mental wounds similar to physical injuries. Consequently, the military has embraced the second option that inevitably has been harmful to veterans, their families, and society, in what we refer to as the darker side of military mental healthcare. In this, the first of a three-part review, we examine the contextual factors framing the military’s dilemma and 10 strategies utilized to avoid learning its war trauma lessons, which will be explored in-depth in parts two and three. While disturbing, these signs of failures are readily ignored and dismissed by a war wary republic. To our knowledge, such an analysis has never been undertaken before or publicly disclosed. When considered as parts of the whole, the findings point to a critical need for improvement in treating military psychological injuries in the war theater.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The next most important lesson is that of preparing, in advance of an urgent need, a comprehensive plan for establishing special military hospitals and using existing civil facilities for treating mental disease in a manner that will serve the army effectively and at the same time safeguard the interests of the soldiers, of the government and of the community (Salmon, 1917, p. 28).
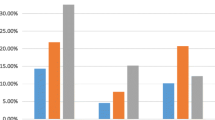
Since the dawn of the twentieth century, wars have become exponentially more expensive. Institutions of military, government, and healthcare have struggled with skyrocketing prevalence and costs associated with escalating numbers of veterans developing war stress injuries. In fact, since the First World War (WWI, 1914–1918), a trend started whereby more U.S. military personnel returned from war as psychiatrically disabled than the total combatants killed-in-action (KIA; see Fig. 1). Specifically, by 1919, 77,000 U.S. veterans were discharged from the military as “nervously handicapped” compared to 53,000 KIA (Salmon & Fenton, 1929). Perhaps most startling is that the casualty numbers reflect only 5 months of trench warfare, given America’s late entry into WWI. In this series of three articles, we cite from historical records that clearly reveal that the military’s positive approaches toward mentally wounded combatants has been exceptionally brief and incomplete at best (see Russell & Figley, 2017a, b, c) in comparison with its reliance upon darker, less humane approaches that we will be discussing throughout. By documenting this darker side, we hope to help improve current and future military mental health within the military and beyond.
Comparing U.S. military neuropsychiatric and non-psychiatric casualties rates. Sources. Data on KIA and WIA (CRS, 2010) except Global War on Terrorism (GWOT) (http://www.defense.gov/news/casualty.pdf). Data on neuropsychiatric (NP) rates for WWI (Department of Veterans Affairs (VA), 1959)—NP disability pensions only; WWII (Brill, 1966; Chermol, 1985; per VA (1947)—greatest number of NP disability pensions for WWII veterans is 474,395; Korean War (VA, 1959)—NP disability pensions only; Vietnam War (Veterans Benefits Administration (VBA), 2015)—PTSD disability pensions only; Persian Gulf War (VBA, 2015)—PTSD disability pensions only; GWOT (VA, 2015)—total veterans who received VA mental healthcare; 300,108 GWOT veterans are receiving PTSD disability pensions (VBA, 2015)
Casualty Trends of Modern Warfare
Moreover, from the Second World War (WWII, 1939–1945) up to the twenty-first century, global war on terror, psychiatric casualties have eclipsed the combined numbers of personnel KIA and medically wounded-in-action (WIA; see Fig. 1). For instance, during WWII a total of 1,076,245 U.S. personnel were either KIA (405,399) or WIA (670,846; Congressional Research Service, 2010), whereas 1,253,000 American service members were admitted to hospitals for war stress injury (1,103,000—Army; Brill, 1966; and 150,000—Navy/Marine Corps; Chermol, 1985). What makes the WWII trend even more alarming is the fact the U.S. War Department (now called the Department of Defense) psychiatrically screened and rejected over 1.6 million purportedly predisposed war “neurotics” from entering the military and another 1 million from deploying to warzones (e.g., Glass, 1966b).
Fast forward to the twenty-first century, the trend is ever more apparent, with 936,283 military personnel (Congressional Research Services (CRS), 2013) and 685,540 veterans treated for psychiatric conditions by the Department of Veterans’ Affairs (VA) respectively (e.g., VA, 2015) who served during Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND), far exceeding the combined total of 57,651 U.S. military personnel either KIA (5353) or WIA (52,298; U.S. military casualty statistics retrieved on 4 June 2015 at www.defense.gov/news/casualty.pdf). Bearing in mind that the epidemiology of war stress injuries, such as 364,894 OIF/OEF/OND veterans diagnosed by the VAFootnote 1 (2015) with PTSD, inherently underestimates the actual prevalence of conditions like PTSD due to the absence of a centralized database or organization responsible for tracking mental health needs across government agencies and the private sector (e.g., Russell & Figley, 2015a) as well as the fact many veterans suffer silently and do not utilize the VA (e.g., VA, 2015) nor seek mental health treatment for fear of stigma and reprisal (e.g., Acosta et al., 2014; Hoge et al., 2004).
In addition, psychiatric diagnostic statistics inadequately describe the full harmful impact of wartime behavioral health crises in terms of the short-and-long-term suffering that individual veterans and their families must endure, such as the undesired loss of a military career, unemployment, homelessness, medically unexplained physical conditions, moral injury, domestic violence, legal prosecution, stigma, substance abuse, divorce, incarceration, vicarious traumatization, and premature death (including suicide) that has affected more than 5383 families of OEF/OIF/OND veterans (e.g., Russell & Figley, 2015a; Russell, Butkus, & Figley, 2016a)—a disturbing trend that many believe started after the Vietnam War, while being clearly evident in the wake of the Persian Gulf War (see Russell & Figley, 2015b).
Overview of Veteran Mental Disability Compensation and Controversy
Veterans have been compensated for wounds and injury since 1636 when the Pilgrims at Plymouth passed the first pension law in American: “that any man who should be sent forth as a soldier and return maimed should be maintained competently by the colony during his life” (Burke, 1899; cited in the Institute of Medicine (IOM, 2007), p. 29). However, the primary motive for veteran compensation has always been military recruitment and prevention of mass desertion (IOM, 2007). For instance, during the Revolutionary War the Continental Congress was compelled to enact the first veterans’ national disability-compensation laws because “Officers in the field warned the Congress that if it did ‘not give better encouragement to the privates than at present is held forth to them, you will have no winter army’” (Bodenger, 1971 cited by IOM, 2007, p. 30) with identical rationale stated for the 1861 Civil War Pension law (IOM, 2007).
Provision for caring of citizens with mental health disabilities was established in a 1751 Pennsylvania law (Braddock & Parish, 2001) that was extended to war veterans in the Military Pension Law of 1776 (IOM, 2007). Per the IOM (2007): “The promise of monetary compensation for war-related disability served not only to attract enlistments in the Colonies—where popular support for the war was far from unanimous (Bradley Commission, 1956)—but also to prevent desertions from an Army fighting in conditions that were abjectly cruel” (p. 30). Attention to veterans’ mental health disability pensions intensified after the U.S. Civil War, especially delayed claims submitted after the war for less tangible war wounds. For instance, a report by the Commission of Pensions indicated that between 1862 and mid-1888 a greater number of awards were granted for delayed-onset diseases than for service-incurred injuries, including 5320 pensions for “nervous prostration,” 1098 pensions for “disease of the brain” such as “insanity,” and 25,994 cases of “diseases of the heart” such as “irritable heart” (IOM, 2007).
Government Concerns over Costs of War Stress Injury
Government concerns over the financial costs of war stress injury are primarily focused on disability pensions and treatment, as well as fears over malingering, all of which can threaten the government’s ability to recruit and retain a fighting force as well as jeopardize its economic standing (IOM, 2007). As the volume and costs of disability pensions increased for psychological conditions, so too did government scrutiny and efforts to tighten regulations. For instance, after WWI, 72,000 veterans were discharged for neuropsychiatric conditions despite psychiatric screenings at enlistment and 40,000 sought disability benefits (IOM, 2007). Consequently, government and military officials attributed much of the neuropsychiatric problem to predisposition and fraud, resulting in the 1921 amendment of the War Risk Insurance Act that excluded conditions believed to have preexisted prior to military service (IOM, 2007). In other words, prior to 1921, the overriding presumption in military pension laws was that any injury or condition incurred on active duty was compensable (e.g., IOM, 2007).
During WWII, the IOM (2007) reports an estimated 1.3 million service members were treated for a neuropsychiatric condition and over 500,000 U.S. Army soldiers were discharged for psychiatric disability in spite of extensive psychiatric screenings at enlistment. Consequently, per the IOM (2007): “policy makers were also concerned with preventing the national economy from slumping into a postwar recession or even depression” (p. 45). In 1956, the Bradley Commission reported that after the Korean War in 1955, a total of 3.7 million out of 22 million living veterans, including survivors from the Spanish-American War (April 1898–August 1898), were receiving a service-connected disability pension,Footnote 2 totaling around $1.9 billion.
Heightened government concerns over exploding disability claims for war stress injury were reignited following the Vietnam War. According to the U.S. military: “The incidence of neuropsychiatric illness in U.S. Army troops in Vietnam is lower than any recorded in previous conflicts” (Ayers, 1969), with only 2–5% of total casualties identified in the warzone as neuropsychiatric (e.g., Jones, 1995a). However, such minimization was contradicted in the post-war psychiatric landscape, whereby an estimated 250,000 (Wilson, 1978) to 2 million (Egendorf, 1982) Vietnam veterans suffering from PTSD overwhelmed the VA, and an additional 9000 to 150,000 reportedly committed suicide (Russell & Figley, 2015b).
In light of the discordant reports of Vietnam veterans’ mental health needs, Congress mandated the National Vietnam Veterans Readjustment Study (NVVRS) in 1983 by enacting Public Law 98-160 to “establish the prevalence and incidence of PTSD and other psychological problems in readjusting to civilian life” (Kulka et al., 1990, p. xxiii). In 1988, the NVVRS reported 479,000 (15.2%) male and 7166 (8.5%) female veterans currently met criteria for PTSD, with a lifetime prevalence of 30.6% or 960,000 male veterans and 26.9% or 1900 female veterans (Kulka et al., 1990), which has subsequently been reanalyzed (Dohrenwend et al., 2006). Regardless, the NVVRS results served to intensify the so-called PTSD debate about the veracity of the diagnosis itself (e.g., Shepard, 2001).
Estimated Costs of War Stress Injury Disability and Treatment
Bilmes (2011) estimated an overall $1 trillion price tag for the American government in regards to disability compensation and VA treatment for OEF/OIFOND veterans. The equivalent costs for veterans of previous wars are not included in this total.
Disability Pension Compensations Footnote 3
In the twenty-first century wars in Afghanistan and Iraq, government concerns regarding skyrocketing rates of PTSD disability compensation claims resurrected the unresolved debates about legitimacy of war stress injury. For instance, a 2005 investigation by the VA Office of the Inspector General reported the number of beneficiaries receiving compensation for PTSD increased by 79.5% from 120,265 to 215,871 from 1999 to 2004, and PTSD disability compensation increased 148.8% from $1.72 billion to $4.28 billion while compensation for all other disability categories only increased by 41.7%. Government concerns led the VA to commission the IOM because:
In particular, compensation claims for PTSD have attracted attention because of the increasing numbers of claims in recent years and because diagnosing PTSD is more subjective than is the case with many of the other disorders that VA administers benefits for (IOM, 2007, p. 20).
In short, the IOM (2006) was charged to review whether the diagnostic construct of PTSD was evidence-based and to advise on more stringent criteria and procedures for accurately diagnosing PTSD. The IOM (2015) report is still dealing with similar issues, this time in the area of social security.
The Congressional Budget Office (CBO, 2014) reported that in 2013, some 3.5 million out of 22 million living U.S. veterans received disability compensation for medical and mental health conditions. Spending on veteran’s disability benefits nearly tripled since fiscal year 2000, from $20 billion in 2000 to $54 billion in 2013, with a forecasted total $64 billion in 2015 (CBO, 2014). The most common disability categories are musculoskeletal (36%), hearing-related (13%), and skin-related (11%), with PTSD accounting for 4% of pensions granted for compensation of an injury. However, over the next 40 years, PTSD disability pension costs will likely increase from $355 to $534 billion depending on the duration and intensity of U.S. military deployments (Bilmes, 2011).
Table 1 reflects the CBO’s (2012) cost estimate for VA treatment of OEF/OIF/OND veterans (from only 2004 to 2009) diagnosed with PTSD and TBI.Footnote 4 The combined total cost for veterans diagnosed with PTSD, TBI, or both is estimated to be $2220 million in comparison to $1450 million for veterans seeking VA treatment without PTSD or TBI (CBO, 2012). The CBO (2012) estimates the average annual cost of VA treatment for mental health conditions other than PTSD or TBI is $4300 per veteran. During FY2004–2009, the VA spent $3.7 billion on the first 4 years of mental health treatment in general, 60% of which ($2.2 billion) was spent only for veterans diagnosed with PTSD and/or TBI (CBO, 2012).
Looking at more recent VA (2015) utilization data, the VA reported 662,722, or 57.2% of all OEF/OIF/OND veterans receiving VA treatment benefits, was for a mental health diagnosis. Using the CBO’s (2012) cost estimates, the VA spent about $12.8 million to treat 297,828 OEF/OIF/OND veterans for a non-PTSD mental health condition (VA, 2015) and an additional $30.2 million to treat 364,894 veterans diagnosed with PTSD (VA, 2015) for a combined total of $43 million. Per Bilmes (2011):
Veterans from Iraq and Afghanistan are utilizing VA medical services and applying for disability benefits at much higher rates than in previous wars. This is because of soldiers: (a) better survival rates for seriously wounded soldiers; (b) more diagnoses of PTSD and other mental health conditions; (c) more veterans who are willing to undergo therapy and apply for disability compensation for mental health difficulties and; (d) better medical benefits, more conditions to which they apply, and higher benefits for some conditions (p. 5).Footnote 5
Moreover, the long-term ripple effect of societal costs from war stress injury typically expands three to four decades after war ends (Bilmes, 2011). The aforementioned crude estimates of disability pension and treatment costs ensure that the trend in Fig. 2 will continue, whereby healthcare costs after war far exceeds the cost of the war itself. Some might hold out hope that eventually the fiscal imbalance will prevent future wars. However, there is no evidence of a global rise in efforts to mitigate war and oversee deployment. Instead, it is more likely that veterans and their families will bear the burden as the military and its government struggle to deal with its fiscal realities.
Cost of war compared to cost of post-war veteran’s benefits. Source: Bradley Commission (1956), p. 113)
Explaining the Psychiatric Casualty Trend of Modern Warfare
Since WWI, the world’s greatest military powers engaged in rigorous, impassioned debates on explaining and more importantly how to end a deplorable psychiatric casualty trend that existentially threatened the military’s capacity to fulfill its mission to fight and win wars, as well as posing a risk of financial burden at home. These so-called trauma-pension debates have been written about extensively and initially emerged out of controversy regarding liability torts from railroad and other industry accidents (e.g., Jones & Wessely, 2005). The majority of military and government leaders, as well as military historians, blame the unmanly military trend on the morally corrosive cultural influence of psychiatry that pathologies normal combat stress reactions with diagnoses like shell shock and traumatic neuroses, as well as the generally weakening influence of modern culture of trauma, which emphasizes victimhood over the customary stiff upper lip resilience (e.g., Shepard, 2001).
On the other hand, military leaders who dealt first hand with war stress injury provide an alternative viewpoint: “Each moment of combat imposes a strain so great that men will break down in direct relation to the intensity and duration of their exposure. Thus psychiatric casualties are as inevitable as gunshot and shrapnel wounds in warfare” (Appel & Beebe, 1946, p. 185), and “Undoubtedly, the most important lesson learned by psychiatry in World War II was the failure of responsible military authorities, during mobilization and early phases of hostilities, to appreciate the inevitability of large-scale psychiatric disorders under conditions of modern warfare” (Glass, 1966b, p. 736). That is, earlier military leaders attributed primary etiology of war stress injuries to exposure to toxic war stress, and assigned responsibility to the military to properly plan and prepare for these equally legitimate and predictable wounds of war.
The Generational Cycle of Preventable Wartime Behavioral Health Crises
Each of the military medical departments (Air Force, Army, and Navy/Marine Corps) are responsible for provision of mental health services to their respective service personnel and family members during times of peace and war (IOM, 2013). The task is complex and can be helped by learning from past efforts. Military medicine acknowledges the value of knowing the history of war stress injuries in that “the past can enable mental health professionals to avoid mistakes made earlier and to devise new ways to deal with modern stress” (Jones, 1995a, p. 6). The underlying causes of wartime mental health crises are inherently complex and multifactorial, and could be mitigated by referring to past strategies. Evidence of learning war trauma lessons is relatively straightforward. The many psychiatric lessons of war are available through numerous retrospective analyses and official reports conducted by the military, historians, commissioned investigations, and by military leaders in memoirs (Russell & Figley, 2015a). The clearest proof of actual lessons learned is the absence of forgetting or ignoring basic tenets for meeting wartime mental health needs and preventing crisis. Preliminary investigations into present and past wartime behavioral health crises reveal a clear pattern of self-inflicted and largely preventable crises caused primarily by the military’s repetitive neglect and failure to learn from its own documented lessons of war trauma (Jones, 1995a; Russell & Figley, 2015a, b).
Ten Foundational Lessons of War Trauma
An extensive review of the military’s lessons learned literature has identified 10 inter-related foundational war trauma lessons that each war generation has either implied or explicitly stated as essential for meeting basic wartime mental health and social reintegration needs (Russell, Figley, & Robertson, 2015). Those foundational lessons are:
-
1.
War inevitably causes a legitimate spectrum of war stress injury.
-
2.
Adequate research, planning, and preparation are indispensable during war and peace.
-
3.
A large cadre of well-trained mental health specialists is compulsory during peace and war.
-
4.
A holistic public health approach to war stress injuries necessitates close collaboration with the private sector along with full parity between medical and mental health services.
-
5.
Effective mental health services demand empowered leadership of an independent, unified, organizational structure (e.g., “Behavioral Health Corps”) providing integrated, well-coordinated continuity of care equal to medical services.
-
6.
Elimination of mental health stigma, barriers of care, and disparity is a priority leadership issue at all levels directly impacting individual, family, and military readiness.
-
7.
Ensure ready access to high quality mental health services including definitive care prior to military separation or discharge.
-
8.
Families must receive adequate mental health and social support during and after military service.
-
9.
Accurate, regular monitoring and reporting are crucial for timely, effective management of mental health needs.
-
10.
Robust dedicated mental health “lessons learned” policy and programs are integral to meeting present and future needs and prevent crisis.
What Is Meant by Preventable Crisis?
War stress injuries cannot be fully prevented any more than the deaths and maiming of those exposed to warzones. That said, until the twentieth century, significantly more combatants died from disease and infection than killed in actual battle (Gabriel, 2013). Thus, learning medical lessons of war (e.g., sterilization of surgical equipment, ensuring adequate supply of well-trained medical specialists, mandatory annual medical examinations) has prevented millions of veterans from unnecessary suffering and premature death. The overall success from the military’s investment in learning from post-war medical analyses and research is best exemplified by the stunning evolution of survivability rates whereby 97% of severely wounded twenty-first-century combatants survive in contrast to 3% in the armies of Alexander (Gabriel, 2013).
We posit that wartime mental health crises, just as epidemics of avoidable medical disease and infection, are preventable or at least can be greatly mitigated by actual learning basic war trauma lessons (Russell & Figley, 2015a). Conversely, a preventable mental health crisis is one caused or exacerbated by the intentional or unintentional ignoring of psychiatric lessons (Russell & Figley, 2015a, b) as WWII hero General Eisenhower aptly concluded:
In seeking the many causes of psychiatric disability in order to correct them, we must put first the absence of prewar planning to prevent and to treat them. This blunder was made by the War Department and the technical service of the Medical Department and was ignored by the profession of psychiatry (U.S. Army Chief of Staff General Dwight D. Eisenhower cited in Menninger, 1948, p. 532).
For example, the introductory chapter in the U.S. Army’s Textbook of Military Medicine: War Psychiatry on The Psychiatric Lessons of War (Jones, 1995a) candidly summarizes the entire history of war stress management under the twin headers of “Lessons Learned/Relearned” and “Lessons Available but Not Learned” (p. 5).
Evidence of Preventable Wartime Mental Health Crisis in the Twenty-First Century
Through its review, the committee found that PTSD management in DoD appear to be local, ad hoc, incremental, and crisis-driven with little planning devoted to the development of a long-range, population-based approach for this disorder by either the office of the Assistant Secretary of Defense for Health Affairs (OASDHA) or any of the service branches (Institute of Medicine (IOM), 2014; p. 216).
The above quote is a worrisome judgment on the current status of military mental healthcare and its compromised organizational and leadership structure after 14 years of war in the cited theaters. The consistent narrative in the twenty-first century along these lines is reflected by the 2007 Washington Post report, “System Ill Equipped for PTSD Troops Returning with Psychological Wounds Confront Bureaucracy, Stigma” (Priest & Hull, 2007) and the 2011 USA Today headline, “Lag in Mental Health Care Found at a Third of VA Hospitals” (Zoroya & Monies, 2011). From the outset of OIF (2003–2004), public concerns about the mental healthcare systems’ capacity to meet wartime needs spurred government intervention, albeit with the problems indicated.
Despite Herculean individual efforts of dedicated professionals working both within, and in collaboration with, the DoD and VA, as well as many notable adjustments made by DoD/VA over recent years (Ritchie, 2013), the crisis in mental healthcare of veterans appears to have intensified as mental health demand escalated. In response, an unprecedented flurry of corrective oversight ensued including presidential commissioned studies (President’s Commission on Care for America’s Returning Wounded Warriors, 2007) and multiple executive orders (e.g., Executive Order 13518. 9 November 2009, Employment of Veterans in the Federal Government; Executive Order, 2012. 31 August 2012, Improving Access to Mental Health Services for Veterans, Service Members, and Military Families), and an incalculable number of congressional actions including frequent hearings (e.g., US Congress, Committee of Conference, 2005; US Congress, Senate Committee on Veterans’ Affairs, 2011a, b; US Congress, House Committee of Veteran’s Affairs, 2011), mandated investigations (e.g., DoD Task Force , 2007, 2010; GAO, 2011, 2010, 2016; IOM 2010, 2012, 2013, 2014; VA Office of Inspector General, 2009, 2012), and new legislation (e.g., Joshua Omvig Veterans Suicide Prevention Act 2007: P.L. 110-110; Women Veterans and Other Health Care Improvements Act of, 2018)—all intended to correct systemic mental health deficiencies during time of war. Russell and Figley (2015b) identified a similar pattern of government reactions to past self-inflicted wartime mental health crises. The clearest declaration of poor planning and insufficient capacity in dealing with military mental health comes from the military itself 6 years into a shooting war:
A single finding underpinning all others: The Military Health SystemFootnote 6 lacks the fiscal resources and the fully trained personnel to fulfill its mission to support psychological health in PEACETIME or fulfill the enhanced requirements imposed during times of conflict (DoD Task Force, 2007, p. ES.2).
Chronic, severe systemic deficiencies were identified by the congressionally mandated task force in staffing levels, training, stigma, monitoring, assessment and diagnosis, familial support, access to quality treatment, organizational fragmentation, social reintegration, and collaboration with external agencies (DoD Task Force, 2007). Regarding military families, the DoD Task Force (2007) reported:
A consistent theme that emerged during Task Force site visits was that families perceive, and care providers confirm, that family members have difficulty obtaining mental health services in the existing system… Specialized mental health care for children and adolescents appears to be in particularly short supply… Few data are available to address the long-term mental health needs of the survivors of deceased service members (p. 39).
In short, the aforementioned DoD Task Force (2007) findings—including those like: “The number of active duty mental health professionals is insufficient and likely to decrease without substantial intervention” (p. ES-3) and “90% of the providers indicated they had received no training or supervision in clinical practice guidelines for PTSD (Russell, 2006a, 6b)” (p. 20), and “There are not sufficient mechanisms in place to assure the use of evidence-based treatments or the monitoring of treatment effectiveness” (p. ES-3)—offer a troubling picture of the military’s inadequate planning, preparation, and responsiveness to meeting predictable wartime mental health demands, requiring presidential and congressional corrective action. Recent reviews have summarized corrective findings from multiple national commissioned investigations into all aspects of the military’s mental health services, including a deeply fragmented and unaccountable organizational and leadership structure (e.g., IOM, 2014; Russell et al., 2016a; Russell, Butkus, & Figley, 2016b). The notion of crisis is aptly expressed in the IOM’s (2012) review of military substance abuse programs asserting: “Yet alcohol and other drug use in the armed forces remain unacceptably high, constituting a public health crisis, and both are detrimental to force.” (p. 248).
Legal Precedents of Preventable Wartime Behavioral Health Crises
The time for action is now. The human and financial costs of un-addressed problems will rise dramatically over time. Our nation learned this lesson, at a tragic cost, in the years following the Vietnam War. Fully investing in prevention, early intervention, and effective treatment are responsibilities incumbent upon us as we endeavor to fulfill our obligation to our military service members (DoD Task Force, 2007, p. 63).
The above plea is genuine and accurate, except for the part about: “Our nation learned this lesson, at a tragic cost, in the years following the Vietnam War” (p. 63). Russell and Figley (2015a) argued that the military and its government have failed this generation of warfighters by neglecting its war trauma lessons, a pattern the military itself acknowledges after each successive war since WWI (Russell & Figley, 2015b). Earlier we highlighted the psychological toll on veterans and their families, including suicide, as well as some of the financial costs associated with war stress injury. How much suffering, premature death, and related costs could have been avoided if the military had actually learned from its well-documented psychiatric foundational lessons of war is of course unknowable, but likely significant. By implication, the status quo can only be described as a clear example of inappropriate negligence (Russell, Zinn, & Figley, 2016).
A recent legal analysis examined historical precedents for class action to compel the military to learn from the psychological realities of war (Russell et al., 2016). For instance, unbeknownst to most Americans, a landmark legal case in 2003 was adjudicated by the British High Court of England and Wales whereby over 2000 British combat veterans sued the Ministry of Defense (MoD)—akin to American Department of Defense (DoD)—for its failure to utilize proper measures in preventing, detecting, and treating predictable long-term adverse effects of war like post-traumatic stress disorder (PTSD; McGeorge, Hughes, & Wessely, 2006). Ultimately, a handful of successful tort claims resulted in the MoD making substantial and meaningful changes by implementing its documented lessons learned including adopting policies that strictly limit level of combat exposure, ensuring ready access to evidence-based treatment on active duty, and granting all war veterans access to their VA services when they leave the military (see Russell et al., 2016).
Despite obvious parallels of Multiple Claimants v. MoD, no similar class actions have ever been filed against the American military due largely to litigation protection (Russell et al., 2016). However, the IOM’s (2014) most recent criticism of the military’s problematic mental healthcare system clearly indicates that the past decade of executive and congressional actions with an estimated $1 trillion price tag (e.g., Bilmes, 2011) has not achieved their objective. The status quo creates an inertia toward extending the pattern of avertible wartime crises marking American society since the WWI (Russell & Figley, 2015a; Russell & Figley, 2015b). Therefore, if not for the contemporary American cohort, eventually, one can reasonably expect legal challenges to the DoD will be forthcoming. In short, it would be helpful if the DoD and U.S. government recognize the potential legal liabilities, and their moral obligations, by addressing the root causes of these self-inflicted crises in the military’s approach to mental health issues.
The Military’s Mental Health Dilemma
Origins of the word dilemma can be traced to the 1520s, from Late Latin and Greek dilemma or “double proposition,” a technical term in rhetoric referring to situations in which someone is forced to choose between two unfavorable alternatives (Harper, 2017). From the military’s perspective, the dilemma involving military mental health can essentially be boiled down to two undesirable propositions: (1) openly acknowledge and commit to learning from the psychiatric realities of war—thus running the risk of catastrophic failure to fulfill its warfighting mission (e.g., mass evacuation syndromes) and potential financial strain, or (2) actively ignore and avoid fully learning the psychiatric lessons of war to sustain the immediate ability to fight and win wars—thus perpetuating a generational cycle of preventable wartime behavioral health crises harming millions of veterans and their families, as well as society (e.g., Russell & Figley, 2015a).
At the heart of the mental health dilemma is the competing demands and responsibilities placed on military commanders to look out for the welfare of individual service members and their families, while maintaining unit morale and readiness in order to accomplish mission priority one, to fight and win wars. During war, individual physical safety and mental wellbeing regularly take a backseat to the unit and mission. For example, during WWI, 22-year-old Army Private McCubin was diagnosed with “shell shock” after exposure to 26 days of continuous shelling but now faced the death penalty after his Courts-Martial conviction for cowardice (Holden, 1998). The Private appealed for leniency and even his company commander recommended mercy, but the Commanding General rejected the appeal citing: “If toleration be shown to private soldiers who deliberately decline to face danger, all the qualities which we desire will become debased and degraded” (Cited in Holden, 1998, p. 84). Private McCubin was executed at dawn. By most measures, the General’s insensitive response was cruel and unjust; would he have executed a disabled soldier suffering from a shrapnel or gunshot wound? However, what if the General was correct and leniency results in entire units refusing to fight (aka “evacuation syndrome”); such mass attrition may cause greater casualties from losing a war. Those in the military do not have the luxury of debating and claiming the moral high ground.
Genesis of the Military’s Mental Health Dilemma
During WWI, all major European armies witnessed unprecedented, some would say epidemic, numbers of neuropsychiatric casualties (e.g., Russell & Figley, 2015b). At the outset of the war, mental wounds were treated on par with physical wounding, typically invoking evacuation to rear hospitals for compassionate treatment. In some cases, such as the British, the awarding of Red Stripes, that is equivalent to the U.S. military’s Purple Heart (Holden, 1998), reflected the predominant European medico-legal paradigm, which only held sway after heated trauma-pension debates regarding post-traumatic stress conditions such as railway spine, accident neuroses, and traumatic neuroses as legitimate injuries to the central nervous system—thus equally compensable as physical wounds suffered in railway and industrial accidents (e.g., Lerner, 2003). However, the military’s early compassionate treatment of psychiatrically disabled soldiers was far from universal. Historically, the military has used many stern methods of dealing with what they deem cowardice regardless of reason, especially during wartime (which we will review shortly).
In those early months of WWI, access to mental health treatment was nearly non-existent for many reasons including (a) many believed the war would be over by Christmas or shortly thereafter, (b) the military has long-standing procedures for dealing with cowardice and disposing of the few mental invalids, (c) the fields of applied mental health were untested in terms of their value to society and the military, and perhaps most importantly (d) the mere idea of mass psychiatric attrition within the military ran counter-intuitive to centuries of warrior ethos, military training, and discipline. Thus, it is understandable that war planners in WWI might dismiss existing documentation of unprecedented emotional breakdown from earlier industrialized wars (e.g., Da Costa, 1871).
Consequently, in the early months of WWI, military personnel experiencing emotional breakdown were unable to return to duty (RTD) due to an identified central nervous system injury or functional neurological condition (e.g., Disordered Action of the Heart, Shell Shock, Traumatic Neuroses). Unlike for a diagnosis or label of cowardice, military personnel were routinely evacuated to hospitals back home, but they were completely unprepared to treat traumatic stress injuries. Hence, the majority of medical evacuees were honorably discharged and awarded disability compensation. In other words, discharged soldiers diagnosed with war stress injury (e.g., traumatic neuroses, shell shock) were initially entitled to essentially the same treatment as those physically wounded and missing limbs.
However, the volume of war stress casualties dramatically escalated as trench warfare persisted along with technological advancements in delivering progressively lethal and terrorizing threats (e.g.., airplanes, tanks, gas, submarines). By mid-1914, every major warring power witnessed an unprecedented number of evacuations due to psychiatric breakdown (Jones & Wessely, 2005). Hundreds of thousands of military officers and enlisted members alike were being discharged, sent home, and given disability pensions for afflictions like shell shock and traumatic neuroses (e.g., Holden, 1998). European governments and their military departments became increasingly alarmed by the epidemic of war stress casualties that existentially endangered the military’s capacity to fight and win wars, as well producing skyrocketing disability pension costs threatening to bankrupt economies (e.g., Jones & Wessely, 2007; Lerner, 2003; Shepard, 2001).
Evacuation Syndrome
Per the U.S. Army’s Textbook on War Psychiatry, an evacuation syndrome “develops in combat or in field training exercises when through accident or ignorance an evacuation route, usually through medical channels, opens to the rear for soldiers displaying certain constellation of symptoms and signs” (Jones, 1995a, p. 10). The Army authors elaborated on WWI evacuation syndromes: “An initial trickle of soldiers turned into a flood, and very soon this inappropriate evacuation of men—for symptoms only—turned into a significant source of manpower loss” (Jones, 1995a, p. 10). The military’s causal explanation for evacuation syndromes offers invaluable insight into its ambivalence toward mental health:
It is important to remember that most psychiatric casualties are soldiers who, because of the influence of negative psychological, social, and physiological factors, unconsciously seek a medical exit from combat. Most cases, therefore, will mimic features of other medical disorders that would be ‘legitimate’ forms of escape from combat, thus becoming ‘evacuation syndromes’. Improperly treated through evacuation, the symptoms may persist or worsen, developing characteristics of traumatic neurosis (chronic post-traumatic stress disorder) (Jones, 1995b, pp. 37–38).
The Military’s Trauma-Pension Debate
Toward the end of the first year of WWI, European militaries and their governments hotly debated the legitimacy of war stress injuries and their compensation, as well as how best to deal with the societal threats posed by mass psychiatric attrition. During the 1914 Berlin Society of Psychiatry and Nervous Illness meeting, famed German neurologist Hermann Oppenheim, a staunch proponent of the legitimacy of traumatic neuroses, argued:
The war has taught us and will continue to teach us (1) that just as before there are traumatic neuroses; (2) that they are not always covered by the concept of hysteria; and (3) that they are really the product of trauma and not goal-oriented, well cultivated pseudo illness (cited in Lerner, 2003, p. 67).
In response, German Army psychiatrist Robert Gaupp (1911) declared: “the most important duty of the neurologist and psychiatrist is to protect the Reich from proliferations of mental invalids and war pension recipients” (Lerner, 2003, p. 64) in reference to the new diagnosis of pension-seeking neuroses believed to harm veterans (e.g., Shepard, 2001).
The military’s innovative response to evacuation syndromes during and since WWI included preventing psychiatric evacuations by deploying mental health specialists to implement what is today referred to as the combat and operational stress control (COSC) doctrine (Russell & Figley, 2017a). The military’s COSC policy entails providing brief respite and restorative interventions with the explicit expectation that 95% of psychiatric casualties will be RTD to their frontline units until either they complete their deployment or their mental health deteriorates resulting in gross incapacitation (e.g., psychosis) or imminent danger to self or others (e.g., Russell & Figley, 2017a). A comprehensive review of the military’s frontline psychiatry (COSC) policies demonstrates its unquestionable effectiveness in preventing psychiatric evacuations (Russell & Figley, 2017b). However, a recent review of the long-term effects of the military’s unchallenged 100-year policy offers stark contradiction to official military narratives promoting the health benefits for service members and their families (Russell & Figley, 2017c). Later we will further examine this particular stratagem in dealing with the mental health dilemma.
1916-Military Replacement of the Paradigm of Traumatic (War) Stress Injury
As WWI battles of 1916 intensified (i.e., The Somme), unmatched numbers of war neuroses occurred, elevating the trauma-pension debate into a German state of emergency (e.g., Brunner, 2003). Consequently, the military on both sides found itself in a classic double-bind whereby if they openly acknowledge the psychological toll from modern warfare as a legitimate outcome akin to physical sacrifices, then this would inevitably lead to mass evacuation syndromes and possible bankruptcy—thus resulting in systemic failure to sustain warfighting, let alone win the war. At a September 1916 Munich War Congress of the German Association for Psychiatry and Neurological Association, medical history was made. European powers replaced the holistic, authentic post-traumatic stress paradigm (e.g., traumatic neuroses) espoused by Oppenheim and others, with an emasculated paradigm of war hysteria, a pseudo illness caused primarily by predisposed individual weakness, cowardice, malingering, and pension-seeking (e.g., Lerner, 2003). The impact of the military’s 1916 paradigmatic change cannot be overstated, as recently acknowledged by the Department of Navy and U.S. Marine Corps (2010):
After 1916, the medical model of combat stress was replaced by the idea of shell shock. Shell shock was considered a temporary and reversible response to stress that would always resolve with no more than a little rest and encouragement. It was then believed to be caused not by literal damage to the brain, but by a weakness of character brought out by the dangers and hardships of war (p. 1–3).
Consequently, after 1916, a uniformed frontline mental health doctrine emerged with strict prohibition against psychiatric labeling, evacuation, discharge, and pensioning (e.g., Jones & Wessely, 2007). In addition, aggressive methods replaced ineffectual gentle approaches in treating war hysteria, such as increasing battlefield executions, legal prosecution, public shaming, faradization (electric shock), and the Kauffman Cure (severe electric shocks) to reduce incidence of cowardice, resulting in claims of 90% RTD to the frontlines (e.g., Holden, 1998; Russell & Figley, 2017a). The Allied powers took similar concerted actions to end the perceived existential threats to their military and society caused by evacuation syndromes. For example, in 1916, the British Army Council issued a directive replacing shell shock diagnosis with a Not Yet Diagnosed (NYD) (Nervous) classification due to concerns about rampant attrition and pensions for malingerers (e.g., Holden, 1998). Efforts to increase social pressure on combatants to avoid seeking psychiatric care included the intentional weaponization of stigma with labels of cowardice, followed by intensifying use of proven strategies to deal with weakness, as well as full implementation of frontline psychiatry doctrine. By the time the U.S. military entered WWI in 1918, it was prepared to manage its mental health dilemma by adopting the European frontline psychiatry doctrine (e.g., Russell & Figley, 2017a). Justification for the new NYDN classification scheme is apparent in the U.S. Army’s summary of its “lessons learned.”
Soldiers in WWI who were called “shell shocked” indeed acted as though they had sustained a “shock to the central nervous system” and the diagnosis of “war neurosis” conveyed chronic or severe mental illnesses. This problem was remedied when medical personnel were instructed to tag such casualties as NYD (nervous) which gave soldiers nothing definite to cling to and no suggestion had been made to help them in formulating their disorder into something that was generally recognized as incapacitating and requiring hospital treatment, thus honorably releasing them from combat duty (Jones, 1995a, p.10). Naturally, stigma associated with war stress injuries greatly intensified and has served as an invaluable tool in managing the military’s mental health dilemma, as we discuss later.
Toleration of Psychiatry in WWI to Reduce Attrition and Pensions
When WWI began, the mental health fields of psychiatry (1808) and psychology (1879) were still in their infancy and desperate for external validation in academic and medical circles. Epidemic numbers of psychiatric casualties, as well as negative publicity regarding psychiatric attrition and pension costs for returning shell-shocked veterans, created the perfect storm that forced frantic military leaders to solicit the services of so-called mental health specialists that many regarded as frauds (e.g., Lerner, 2003). Ambiguity toward mental health in both military and civilian sectors was widespread, as articulated by British Secretary of Navy and future Prime Minister Winston Churchill (1942): “I am sure it would be sensible to restrict as much as possible the work of these gentlemen, who are capable of doing an immense amount of harm with what may very easily degenerate into charlatanry” (cited in Holden, 1998, p. 94). The military’s distrust and antipathy toward psychiatry was clearly demonstrated when WWI ended. Most warring powers, including the U.S., expeditiously purged their mental health programs and specialists from the military (e.g., Russell & Figley, 2017a). Begrudgingly, the same warring powers were compelled to reconstitute its mental health services to deal with WWII evacuation syndromes.
Attempted Solutions to Resolve the Military’s Mental Health Dilemma
From the military’s perspective, one might argue that early attempts at treating mental injuries humanely on par with physical wounds at the outset of WWI were directly responsible for intolerable evacuation syndromes. Consequently, alternatives strategies for dealing with its mental health dilemma are not only justified, but constitute the best viable answer to a perplexing problem. However, the historical record clearly reveals the military’s episodic flirtation with more “positive” or enlightened approaches toward mentally wounded combatants has been exceptionally brief and incomplete at best (see Russell & Figley, 2017a, b, c) in comparison with its reliance upon “darker,” less humane approaches that we will be discussing.
Societal Benefits from Military Medicine’s Remarkable Achievements
Before delving into the dark side of military mental healthcare, we must express our deepest appreciation for the contributions of many military and civilian leaders who have been staunch mental health advocates, as well as acknowledging the herculean efforts by the majority of past, current, and future healers. For mental health as much as any area, much of the life-saving advances in modern medicine arise from the destructive effects of war necessitating innovative treatments. Centuries of trial and error have led to progressive evolutions in our understanding, prevention, diagnosis, and treatment of physical disease, wounds, and injuries. Gabriel’s (2013) Between Flesh and Steel traces the historical linkage of advances in the medical sciences to the lessons learned from military medicine. Breakthroughs such as triage, ambulances, surgical sterilization, burn care, tourniquets, blood transfusion, amputations, x-ray, inoculations, and disease prevention are all either innovations or refinements that have saved countless lives both within and outside of military circles. Disciplines such as neurology and nursing emerged during the U.S. Civil War. Indeed, one can reasonably argue that the credibility of physicians and the field of medicine as a whole have been enhanced through the trials of military medicine (e.g., Gabriel, 2013).
As Goes the Military, So Goes Mental Healthcare
Similarly, no other institution has been as instrumental as the military in promulgating the fields of applied mental health sciences. For instance, the world’s first-ever clinical trial for treating traumatic stress injury (Irritable Heart) was undertaken by the Union Army during the U.S. Civil War (e.g., Da Costa, 1871). Prior to WWI, psychiatry was still in its infancy with alienists as they were called relegated to custodial care in insane asylums. It was not until Charcot and other physicians of his time began treating male hysteria in combat veterans from wars such as the Franco-Prussian War that the field of psychiatry began to be taken seriously in Europe.
Consequently, in 1884 medical and psychiatric military experts from Germany, Great Britain, France, Russia, and the United States all converged in growing recognition of the psychological impact of trauma caused by modern warfare. Rampant psychiatric attrition in traumatized European armies of WWI led to the official acceptance of the emerging fields of psychiatry and psychology by the military, and thus enhancing their professional standing in broader society. Psychological testing became a national priority for the fledgling psychology discipline during WWI with expanded investments in measures of personality, ability, and vocation arising from WWII. During and after WWII, acute shortages of psychiatrists led the Veteran’s Administration (VA) to create the first clinical internships for training psychologists and the discipline of clinical social work emerged (Baker & Pickren, 2007). By 1946, psychiatry, psychology, and social work were given permanent status in the U.S. military, thus raising the credibility and growth potential of mental healthcare. The U.S. Army’s WWII psychiatric diagnostic classification system was adopted by the American Psychiatric Association (APA) in the first Diagnostic Statistical Manual (DSM; APA, 1952).
Those and many other hard-won lessons from the two world wars promised changes in societal paradigms of incurable insanity to mental “illness” that most can recover with proper treatment resulting in more humane treatment outside of asylums. Treatment of mental illness with psychopharmacology and psychotherapy of individuals, groups, and families all have their roots in the lessons of war. Efforts were also made to translate the psychiatric lessons from WWII by establishing the National Institute of Mental Health to destigmatize mental illness and symbolize parity with physical medicine (e.g., Russell & Figley, 2014). Indeed, if not for military mental healthcare, one might ponder whether alienists would still be relegated to custodial care in the nation’s asylums and psychologists confined largely to academic laboratories.
The Darker Side of Military Mental Healthcare
As a whole, the nation deserves great credit in the positive ways it has demonstrated support to its current warrior class, especially those bearing tangible evidence of their sacrifice. As a country, we honor our heroes. However, there is a profound, unrecognized chasm in the level and type of institutional and public sustenance for the millions of veterans and family members in this, and every previous American war suffering from less-visible wounding. As previously asserted, a debt of gratitude is owed to military mental healthcare from its direct beneficiaries, mental health professions, as well as broader society. Yet, a full understanding of the mental health narrative requires us to also acknowledge a darker and generally unspoken aspect of the military’s struggle to resolve its mental health dilemma, which continues to present day.
Ten Military Strategies to Manage its Mental Health Dilemma
After an extensive review of the literature on war stress, we have identified ten overarching strategies or approaches the military has implemented in order to eliminate, minimize, or conceal its mental health problem: (1) Cruel and Inhumane Handling; (2) Legal Prosecution, Incarceration, and Executions; (3) Weaponizing Stigma to Humiliate, Ridicule, and Shame into Submission; (4) Denying the Psychological Realities of War; (5) Screening and Preventing Weakness; (6) Delay, Deception, and Watchful Waiting; (7) Bad Paper Discharges; (8) Diffusion of Responsibility and Accountability; (9) Inadequate, Experimental, and Harmful Treatments; and (10) Perpetuating Neglect and Self-Inflicted Crises.
Conclusion
This first paper in a three-part series provided the foundation for appreciating the “dark side” of military mental health—instead of avoiding the mental health decline of our fighting force the 10 indicated strategies were used along with other implicit and explicit policies to put our nation as well as our fighting force at risk. The intention of our analysis is not to criticize or take cheap shots at the military, but to help our military and civilian leaders, mental health advocates, and military populations to come to a general mutual understanding of what our country has been through and may likely continue to replicate absent improved policies. In articles two and three of our analysis, we will examine the evidence and implications of the military’s 10 strategies used to avoid learning the psychological realities of war. We describe and document the ten avoidance strategies used by the U.S. military to plan and fight in wars without seriously considering the predicted the harmful mental health consequences of the fighting force. Collectively, we hope this series will have a tangible and positive impact on DoD planning for troop deployments that provides clear and measurable increases in mental health resilience as a result of its policies, procedures, and programs based on science and data.
Notes
The VA’s diagnosis of PTSD in the VA can be determined by not only MDs and PCMs, but also providers who are not sufficiently trained and certified.
The VA considers all disability pensions as disability compensations for the servicemembers’ loss.
The term “service-connected disability” or “VA disability” should be followed by “compensation” v. “pension” because we are not talking about pensions related to veteran’s age or non-service-connected disabilities. So we will need to change that…and in the section where we review the “trauma-pension debates,” we may want to mention that the term “pension” is defined by the VA as a compensation for service-connected injury.
It is common knowledge that the VBA does not support evidenced-based C&P examinations. Some examinations are 1 h long; other examinations may take up to 4 h. There is rarely any psychological testing and there is no training on understanding/reviewing military records.
It was told to the authors that the Veteran Service Organizations today are urging veterans they see to “claim everything” and to assert that it was linked to being deployed.
It was reported to the authors that currently, for example, the U.S. Army is significantly understaffed with approximately 150–200 active-duty psychologists for about 1 million soldiers.
References
Acosta, J. D., Becker, A., Cerully, J. L., Fisher, M. P., Martin, L. T., Vardavas, R., Slaughter, M. E., & Schell, T. L. (2014). Mental health stigma in the military. Prepared for the Office of the Secretary of Defense Center for Military Health Policy Research. Santa Monica: RAND.
American Psychiatric Association. (1952). Diagnostic and statistical manual of mental disorders—first edition. Washington, DC: Author.
Appel, J., & Beebe, G. (1946). Preventive psychiatry; an epidemiologic approach. Journal of the American Medical Association, 131(18), 1469–1475.
Ayers, B. D. (1969). Combat fatigue in Vietnam rare: facilities at front, almost eliminate it doctors say. The New York Times, 7.
Baker, R. R., & Pickren, W. E. (2007). Psychology and the Department of Veterans Affairs: a historical analysis of training, research, practice, and advocacy. Washington, DC: American Psychological Association.
Bilmes, L. J. (2011). Current and projected future costs of caring for veterans of the Iraq and Afghanistan wars. Unpublished manuscript, Department of Economics, Harvard University, Massachusetts, USA. Retrieved from: http://costsofwar.org/sites/default/files/articles/52/attachments/BilmesVeteransCosts.pdf.
Bodenger, R. G. (1971). Soldiers’ bonuses: a history of veterans’ benefits in the United States, 1776–1967. (Doctoral dissertation, Pennsylvania State University).
Braddock, D. L., & Parish, S. L. (2001). An institutional history of disability. In K. D. Seelmann, G. L. Albrecht, & M. Bury (Eds.), Handbook of disability studies (pp. 11–68). Thousand Oaks: Sage Publications.
Bradley Commission. (1956). The President’s commission on veterans’ pensions: a report to the president, veterans’ benefits in the United States. 84th congress, 2nd session, House Committee print no. 236. Washington, DC: U.S. Government Printing Office.
Brill, N. Q. (1966). Hospitalization and disposition. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army: Neuropsychiatry in World War II (Vol. I) (pp. 195–253). Washington, DC: Office of the Surgeon General, Department of the Army.
Brunner, J. (2003). Trauma in court: medico-legal dialectics in the late nineteenth-century German discourse on nervous injuries. Theoretical Inquiries in Law, 4(2), 697–727.
Burke, W. M. (1899). History and functions of central labor unions. New York: MacMillan.
Chermol, B. H. (1985). Wounds without scars: treatment of battle fatigue in the U.S. Armed Forces in the Second World War. Military Affairs, 49, 9–12.
Civic Impulse. (2018). H.R. 958 — 113th congress: Women veterans and other health care improvements act of 2013. Retrieved from: https://www.govtrack.us/congress/bills/113/hr958.
Congressional Budget Office. (2012). The Veterans Health Administration’s treatment of PTSD and traumatic brain injury among recent combat veterans. The Congress of the United States. Washington, DC: Congressional Budget Office.
Congressional Budget Office. (2014). Veterans’ disability compensation: trends and policy options. Washington, DC: Congressional Budget Office.
Congressional Research Service. (2010). American war and military operations casualties: lists and statistics. Retrieved from http://fas.org/sgp/crs/natsec/RL32492.pdf.
Congressional Research Service. (2013). Post-traumatic stress disorder and other mental health problems in the military: oversight issues for the Congress. 7-5700: R43175. Prepared by K. Blakeley and D. J. Jansen, August 8, 2013, www.crs.gov.
Da Costa, J. M. (1871). On irritable heart: a clinical study of a form of functional cardiac disorder and its consequences. American Journal of Medicine, 61, 17–52.
Department of Defense Task Force on Mental Health. (2007). An achievable vision: report of the Department of Defense Task Force on Mental Health. Falls Church: Defense Health Board.
Department of Defense Task Force on the Prevention of Suicide by Members of the Armed Forces. (2010). The challenge and the promise: strengthening the force, preventing suicide, and saving lives. Falls Church: Defense Health Board Retrieved from: www.health.mil/dhb/subcommittees-tfpsmaf.cfm
Department of Navy & U.S. Marine Corps. (2010). Combat and operational stress control. U.S. Navy, NTTP 1-15M; U.S. Marine Corps, MCRP 6-11C. Washington, DC: Pentagon
Department of Veterans Affairs. (2015). Analysis of VA health care utilization among Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn veterans, from 1st Qtr FY 2002 through 1st Qtr FY 2015. Washington, DC: Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration Author. Retrieved from: www.publichealth.va.gov/epidemiology
Dohrenwend, B. P., Turner, J. B., Turse, N. A., Adams, B. G., Koenen, K., & Marshall, R. (2006). The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science, 18(313), 979–982.
Egendorf, A. (1982). The postwar healing of Vietnam veterans: recent research. Hospital and Community Psychiatry, 33(11), 901–908.
Gabriel, R. A. (2013). Between flesh and steel: a history of military medicine from the Middle Ages to the war in Afghanistan. Washington, DC: Potomac Books.
Gaupp, R. (1911). Uber den Begriff der hysterie. ZgNP, 5, 457–466.
Glass, A. J. (1966b). Lessons learned. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II, volume I: zone of interior (pp. 735–759). Washington DC: Office of the Surgeon General, Department of the Army.
Government Accountability Office. (2010). Defense health care: status of efforts to direct lack of compliance with personality disorder separation requirements (GAO-10-1013T). Washington, DC: Author.
Government Accountability Office. (2011). VA mental health number of veterans receiving care, barriers faced, and efforts to increase access (GAO-12-12). Washington, DC: Author.
Government Accountability Office. (2016). Human capital: additional actions needed to enhance DoD’s efforts to address mental health care stigma (GAO-16-404). Washington, DC: Author.
Harper, D. (2017). Online etymology dictionary. Retrieved from: www.etymonline.com/index.php?term=dilemma.
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22.
Holden, W. (1998). Shell shock: the psychological impact of war. London: Macmillan.
Institute of Medicine. (2006). Posttraumatic stress disorder: diagnosis and assessment. Washington, DC: The National Academies Press.
Institute of Medicine. (2007). PTSD compensation and military service. Committee on veteran’s compensation for posttraumatic stress disorder, National Research Council. Washington, DC: The National Academies Press.
Institute of Medicine. (2010). Preliminary assessment of readjustment needs ofvVeterans, service members, and their families. Washington, DC: The National Academies Press.
Institute of Medicine. (2012). Substance use disorders in the U.S. Armed Forces. Report brief. Washington, DC: The National Academies Press.
Institute of Medicine. (2013). Returning home from Iraq and Afghanistan: assessment of readjustment needs of veterans, service members, and their families. Washington, DC: The National Academies Press.
Institute of Medicine. (2014). Treatment for posttraumatic stress disorder in military and veteran populations: final assessment. Washington, DC: The National Academies Press.
Institute of Medicine. (2015). Psychological testing in the service of disability determination. Washington, DC: National Academic Press.
Jones, E., & Wessely, S. (2005). Shell shock to PTSD: military psychiatry from 1900 to the Gulf War. Hove: Psychology Press.
Jones, E., & Wessely, S. (2007). A paradigm shift in the conceptualization of psychological trauma in the 20th century. Journal of Anxiety Disorders, 21, 164–175.
Jones, F. D. (1995a). Psychiatric lessons of war. In F. D. Jones, L. R. Sparacino, V. L. Wilcox, J. M. Rothberg, & J. W. Stokes (Eds.), Textbook of military medicine: war psychiatry (pp. 1–34). Washington, DC: Office of the Surgeon General, U. S. Department of the Army and Borden Institute.
Jones, F. D. (1995b). Disorders of frustration and loneliness. In F. D. Jones, L. R. Sparacino, V. L. Wilcox, J. M. Rothberg, & J. W. Stokes (Eds.), Textbook of military medicine: war psychiatry (pp. 63–83). Washington, DC: Office of the Surgeon General, U. S. Department of the Army and Borden Institute.
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R., Weiss, D. S., & Grady, D. A. (1990). Trauma and the Vietnam war generation: report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel.
Lerner, P. (2003). Hysterical men: war, psychiatry, and the politics of trauma in Germany, 1890–1930. Ithaca: Cornell University Press.
McGeorge, T., Hughes, J. H., & Wessely, S. (2006). The MoD PTSD decision: a psychiatric perspective. Occupational Health Review, 122, 21–28.
Menninger, W. C. (1948). Reactions to combat. Psychiatry in a troubled world. New York: MacMillan.
President’s Commission on Care for America’s Wounded Warriors, Serve, Support, Simplify, Washington, DC: President’s Commission on Care for America’s Wounded Warriors. (2007). Retrieved from: www.veteransforamerica.org/wp-content/uploads/2008/12/presidents-commission-on-care-for-americasreturning-wounded-warriors-report-july-2007.pdf. What is the author or title here?
Priest, D., & Hull, A. (2007). System ill equipped for PTSD: troops returning with psychological wounds confront bureaucracy, stigma. The Washington Post. Retrieved from: www.msnbc.msn.com/id/19267926/from/ET/print/1/displaymode/1098/.
Ritchie, E. C. (2013). Military mental health’s wins and losses since the Iraq invasion U.S. Time. Retrieved from http://nation.time.com/2013/03/19/military-mental-healths-wins-andlosses-since-the-iraq-invasion/.
Russell, M. (2006a). Mental health crisis in the Department of Defense: DoD Inspector General Hotline Investigation #98829 submitted by Commander Mark Russell, USN on 05JAN2006. Available upon request via Freedom of Information Act (FOIA) at Department of Defense; Office of Freedom of Information, 1155 Defense Pentagon; Washington, DC 20301–1155.
Russell, M. (2006b). The future of mental health care in the Department of Defense. Invited testimony before the Congressionally-mandated Department of Defense Task Force on Mental Health, on 19–20 October 2006, San Diego, CA. Transcript available on Defense Health Board (www.ha.osd.mil/DHB/mhtf/meeting/2006oct.cfm).
Russell, M. C., Butkus, S., & Figley, C. R. (2016a). Contribution of military organization and leadership factors in perpetuating generational cycle of preventable wartime mental health crises: part one. Psychological Injury and Law, 9(1), 55–72.
Russell, M. C., Butkus, S., & Figley, C. R. (2016b). Ending the generational cycle of preventable wartime mental health crises: part two: establishing a behavioral health corps and other constructive solutions. Psychological Injury and Law, 9(1), 73–86.
Russell, M. C., & Figley, C. R. (2014). Overview of the Affordable Care Act’s impact on military and veteran mental health services: nine implications for significant improvements in care. Journal of Social Work in Disability & Rehabilitation, 13(1–2), 162–196.
Russell, M. C., & Figley, C. R. (2015a). Investigating recurrent generational wartime behavioral health crises: part one of a preliminary analysis. Psychological Injury and Law, 8(1), 106–131.
Russell, M. C., & Figley, C. R. (2015b). Generational wartime behavioral health crises: part two of a preliminary analysis. Psychological Injury and Law, 8(1), 132–152.
Russell, M. C., & Figley, C. R. (2017a). Do the military’s frontline psychiatry/combat and operational stress control doctrine help or harm veterans? Part one: framing the issue. Psychological Injury and Law, 10, 1–23.
Russell, M. C., & Figley, C. R. (2017b). Do the military’s frontline psychiatry/combat operational stress control programs benefit veterans? Part two: systematic review of the evidence. Psychological Injury and Law, 10, 24–71.
Russell, M. C., & Figley, C. R. (2017c). Is the military’s century-old frontline psychiatry policy harmful to veterans and their families? Part three of a systematic review. Psychological Injury and Law, 10, 72–95.
Russell, M. C., Figley, C. R., & Robertson, K. R. (2015). Investigating the psychiatric lessons of war and pattern of preventable wartime behavioral health crises. Journal of Psychology and Behavioral Science, 3(1), 1–16.
Russell, M. C., Zinn, B., & Figley, C. R. (2016). Exploring options including class action to transform military mental healthcare and ends the generational cycle of preventable wartime behavioral health crises. Psychological Injury and Law, 9, 166–197.
Salmon, T. W. (1917). Recommendations for the treatment of mental and nervous diseases in the United States Army. New York: National Committee for Mental Hygiene.
Salmon, T. W., & Fenton, N. (1929). Neuropsychiatry in the American expeditionary forces. In P. Bailey, F. E. Williams, P. A. Komora, T. W. Salmon, & N. Fenton (Eds.), Neuropsychiatry: the Medical Department of the United States Army in the world war (Vol. 10) (pp. 271–474). Washington, DC: Office of the Surgeon General, US Army.
Shepard, B. (2001). A war of nerves: soldiers and psychiatrists in the twentieth century. Cambridge: Harvard University Press.
U.S. Congress, Committee of Conference. (2005). Making appropriations for military quality of life functions of the Department of Defense, Military Construction, the Department of Veterans Affairs, and Related Agencies for the Fiscal Year Ending September 30, 2006, and for Other Purposes, report to accompany H.R. 2528, 109th Congress, 1st session November 18, 2005, H. Rept. 109–305 (Washington: GPO, 2006).
U.S. Congress, House Committee on Veterans’ Affairs. (2011). Subcommittee on Health, Understanding and Preventing Veteran Suicide. 112th Congress, 1st session, hearing held on December 2, 2011.
U.S. Congress, Senate Committee on Veterans’ Affairs. (2011a). VA Mental Health Care: closing the gaps. 112th Congress, 1st session, hearing held on July 14, 2011.
U.S. Congress, Senate Committee on Veterans’ Affairs. (2011b). VA Mental Health Care: addressing wait times and access to care. 112th Congress, 1st session, hearing held on November 30, 2011. Congressional Research Service. (2010). American war and military operations casualties: Lists and statistics. (CRS Publication No. 7–5700: RL32492).
Veterans Administration. (1947). Annual report of the director of Veterans Affairs—1947. Washington, DC: U.S. Government Printing Office.
Veterans Administration. (1959). Annual report of the director of Veterans Affairs—1959. Washington, DC: U.S. Government Printing Office.
Veterans Administration, Office of Inspector General. (2009). Healthcare inspection: evaluation of suicide prevention program implementation in VHA Facilities, January–June 2009, Report No. 09-00326-223, Washington, DC, September 22, 2009. Retrieved from: www.va.gov/oig/54/reports/VAOIG-09-00326-223.pdf.
Veterans Administration, Office of Inspector General. (2012). Veterans Health Administration review of veterans’ access to mental health care. Retrieved from: www.va.gov/oig/publications/reports-list.asp.
Veterans Benefits Administration. (2015). Annual benefits report FY2015. Washington, DC: U.S. Department of Veterans’ Affairs.
Wilson, J. P. (1978). Identity, ideology, and crisis: the Vietnam veteran in transition (vol. 2). Washington, DC: Disabled American Veterans.
Zoroya, G., & Monies, P. (2011). Lag in Mental Health Care Found at a Third of VA Hospitals. USA Today. Retrieved from: https://usatoday30.usatoday.com/news/military/story/2011-11-09/veterans-mental-health-care/51143216/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
This study was unfunded and there are no conflicts of interests involving the authors.
Rights and permissions
About this article
Cite this article
Russell, M.C., Schaubel, S.R. & Figley, C.R. The Darker Side of Military Mental Healthcare Part One: Understanding the Military’s Mental Health Dilemma. Psychol. Inj. and Law 11, 22–36 (2018). https://doi.org/10.1007/s12207-018-9313-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12207-018-9313-2