Abstract
As we reported in the previous two articles in this series, the U.S. military has actively attempted to deal with its mental health dilemma by utilizing 10 approaches. These strategies function to help the military avoid learning its war trauma lessons to the contrary, and it appears that their approach is to prevent or reduce mass psychiatric attrition and exorbitant costs associated with psychiatric treatment and disability pensions, to the clear detriment of its fighting force and their families denied adequate mental healthcare. In this final review, we examine the remaining five harmful approaches designed to prevent the so-called evacuation syndromes that the military worries might arise should psychiatric lessons of war ever be implemented, such as eliminating stigma and elevating mental health services on par with medical services. The five avoidance strategies we cover include (6) delay, deception, and delay; (7) faulty diagnosis and “backdoor” discharges; (8) maintaining diffusion of responsibility and unaccountability; (9) provision of inadequate, experimental, or harmful treatment; and (10) perpetuating neglect, indifference, and self-inflicted crises. We conclude our analysis by asserting that the U.S. military has tried every conceivable way to unburden itself from the psychological realities of modern warfare, with the notable exception of actually committing to learning its war trauma lessons and genuinely implementing the required policies for good.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The time for action is now. The human and financial costs of un-addressed problems will rise dramatically over time. Our nation learned this lesson, at a tragic cost, in the years following the Vietnam War. Fully investing in prevention, early intervention, and effective treatment are responsibilities incumbent upon us as we endeavor to fulfill our obligation to our military service members (Department of Defense Task Force on Mental Health, 2007, p. 63).
Introduction
It appears that the military has never genuinely learned its lesson when it comes to managing its mental health dilemma (Russell, Schaubel, & Figley, 2017a, b). Instead, military and government leaders repeatedly ignore the simplest and most basic war trauma lessons, such as the need to prepare for inevitable large numbers of psychiatric casualties, which has been the case for that every cohort since the First World War (WWI) (e.g., Russell, Figley, & Robertson, 2015). Today, the passive avoidance of learning war trauma lessons was painfully illuminated by the U.S. Army’s senior psychiatrist’s candid admission that, during the 2003 Iraq invasion planning, “Mental health was not a welcomed topic… we were not allowed to speak of the unseen wounds of war… we were not allowed to prepare for the invisible wounds” (Brigadier General Lori Sutton, U.S. Army; Sutton, 2016). One hundred years earlier, General Sutton’s WWI counterpart warned that prior to the American entry into the Great War, there is:
The next most important lesson is that of preparing, in advance of an urgent need, a comprehensive plan for establishing special military hospitals and using existing civil facilities for treating mental disease in a manner that will serve the army effectively and at the same time safeguard the interests of the soldiers, of the government and of the community (Salmon, 1917, p. 28).
Willful negligence of 100 years of lessons learned after every subsequent American war helps to explain the DoD’s Task Force on Mental Health (DoD TF-MH, 2007) conclusion: “A single finding underpinning all others: The Military Health System lacks the fiscal resources and the fully trained personnel to fulfill its mission to support psychological health in PEACETIME or fulfill the enhanced requirements imposed during times of conflict” (p. ES.2). This systematic lack has been perpetuating a generational cycle of preventable and self-inflicted wartime behavioral health crises since WWI (Russell & Figley, 2015a, b; Russell, Zinn, & Figley, 2016).
As we reported in the previous two articles in this series, the military has actively attempted to deal with its mental health problem by utilizing 10 strategies intended to avoid psychiatric attrition, treatment, and disability pensions to the detriment of millions of its soldiers (Russell et al., 2017a, b). We have already reviewed in depth the first five of the strategies in the second article of our series. In this final article, we examine the remaining five harmful approaches designed to prevent evacuation syndromes that the military worries could inevitably arise should psychiatric lessons of war ever be implemented, such as eliminating stigma and elevating mental health services on par with medical services (Russell et al., 2017a). The five avoidance strategies we will cover include (6) delay, deception, and delay; (7) faulty diagnosis and “backdoor” discharges; (8) maintaining diffusion of responsibility and unaccountability; (9) provision of inadequate, experimental, or harmful treatment; and (10) perpetuating neglect, indifference, and self-inflicted crises.
Strategy 6: Delay, Deception, and Delay
The ability of the military to accomplish its mission to fight and win wars requires not only defeating adversaries on the battlefield but also winning public support at home. Since WWI, the military has been embroiled in national controversies regarding large numbers of returning war veterans with unmet mental health needs and skyrocketing pension costs that either threaten or serve to erode public support (Russell & Figley, 2017a). Consequently, the military has been forced to develop public relations (PR) campaigns designed to manage the mental health narrative in a manner that sustains public backing long enough to win the current war. Managing or manipulating the public narrative is yet another example of an overarching strategy to avoid dealing with the psychological realities of war. The PR mission is accomplished via the avoidance strategy of delay, deceive, and delay in three, sometimes overlapping stages: (1) avoiding disclosure or recognition of wartime mental health needs or crisis via publicity blackouts; (2) public deception through narrative filters and designed to deny the existence and/or scope of a mental health crisis, typically in response to external inquiries; and (3) delaying full commitment and implementation of externally mandated changes by engaging in tactical appeasement, half-measures, or other forms of partial compliance.
Avoiding Public Disclosure of Recognition of Mental Health Needs
Transparency about the size, scope, and costs of wartime mental health needs will inevitably result in serious public questioning regarding existing policies associated with mental health issues. Therefore, it behooves for the military to maintain public ignorance about the psychological realities of war to sustain positive civic opinion. The military accomplishes this in a variety of ways, including: (a) enacting PR policies that either completely or partially prohibit verbal or written public disclosures about the extent of its mental health problem (e.g., Menninger, 1966; Russell et al., 2016); (b) restricting tracking and/or disclosure to only a handful of psychiatric diagnoses [e.g., post-traumatic stress disorder (PTSD), traumatic brain injury (TBI)] versus the full spectrum of war stress injury (e.g., Russell & Figley, 2015a, b); (c) ensuring there is no single centralized agency responsible for tracking and reporting mental health needs throughout the DoD (e.g., Russell, Butkus, & Figley, 2016a, b); (d) publishing prevalence data that is intentionally vague versus actual numbers (Russell & Figley, 2015a); and (e) avoiding to publish real-time data on mental health casualties, disability pensions, etc.
In regard to the latter point, the DoD publishes real-time casualty statistics via a centralized database maintained by the Defense Casualty Analysis System (DCAS; www.dmdc.osd.mil/dcas/pages/casualties.xhtml) that includes military and DoD-civilian personnel killed and wounded in action, as well as those who died, became ill, or were injured for noncombat reasons (e.g., accidents, illness, self-inflicted). Per DCAS (2017): “Reports are used by DoD organizations, external government agencies, both houses of Congress, the President, the news media, and the general public. The data contained in this site can be used to understand trends in casualties” (retrieved from: www.dmdc.osd.mil/dcas/pages/casualties.xhtml). However, the DCAS does not track or report prevalence of war stress injury despite the trend of psychiatric casualties outnumbering the combined totals of medically wounded and killed in action since WWII (e.g., Russell et al., 2017a).
Publicity Blackout Policies
The military use of PR blackout policies to avoid public disclosure of its mental health problem was evident during the Second World War (WWII). For example, the Director, Bureau of Public Relations, War Department, and other high-ranking officials distributed the following memorandum on 28 April 1944:
Subject: Statistical information by percentages, rates, or numbers of neuropsychiatric casualties in the armed services is classified. The release of statistical information as indicated above constitutes a violation of AR 380-5 and Article 76, Navy Regulations. The following policy will govern all Army and Navy releases for publication of information concerning neuropsychiatric casualties of the Armed Forces. All material on this subject will be checked for accuracy by the Surgeon General’s Office, U.S. Army, before final clearance by the Review Branch, War Department Bureau of Public Relations (Menninger, 1966, p. 141).
Public outrage and protests over the unexpectedly high volume of psychiatrically disabled soldiers returning from the war led to a September 23, 1944, inquiry by the Army Inspector General (IG) “concerning the handling and diagnosis of psychoneurotics within the Army” (Menninger, 1966, p. 148). The IG openly criticized the military’s blackout policy, forcing the Chairman of the Board of Declassification of Medical and Scientific Reports of the Surgeon General’s Office to issue a 1945 memorandum requiring: “Full publicity of the psychiatric problem should be given in a factual manner” (Menninger, 1966, p. 148). Yet, even as WWII ended and the country turned its attention toward helping reintegrate millions of veterans, the military’s publicity blackout was resolute:
On 29 June 1945, Joint Security Control issued a memorandum, again listing “Topics To Be Withheld From Publication.” In this memorandum, there was the specific note under miscellaneous subjects which read as follows: “Statistics (percentages, rates, numbers, names or identifiable photographs) of Neuropsychiatric Casualties” (Menninger, 1966, p. 147).
In response, the Army’s Chief Neuropsychiatry Consultant, Brigadier General Menninger issued the following rebuttal to headquarters:
The public relations and publicity policy with regard to neuropsychiatry involve a problem of great magnitude. It affects the national life. There is an urgent need for frank and extended publication in this field. By a liberal policy of public education, the War Department can give its support and aid to those veterans discharged for neuropsychiatric causes (Menninger, 1966, p. 148).
In summarizing lessons learned from WWII PR, Menninger (1966) candidly concluded:
If we are to learn any lesson, it would certainly be the importance of establishing full-time public relations officer in this field (neuropsychiatry) with the authority of the War Department to release such information as seemed indicated. Only by such methods can impending problems be attacked aggressively and the public educated, thereby avoiding the experience of this war and the common welfare of communities ignored (p. 250).
Contemporary Publicity Blackout in Afghanistan and Iraq Wars
Even in the twenty-first century, the U.S. military’s effort to avoid public disclosure of its mental health crisis is still evident, both from covert circumstantial facts as well as overt written policies. In regard to the former, the fact that the DoD does not have a single agency responsible for maintaining and reporting accurate mental health prevalence data throughout the DoD (e.g., Russell et al., 2016a), by itself, constitutes a publicity blackout. For example, the DoD’s Armed Force Health Surveillance Center and DoD Deployment Health Center (www.pdhealth.mil/clinical/psychological-health-numbers/mental-health-disorder-prevalence-among-active-duty-service) can provide only mental health data gleaned from service members seen by military medicine via its electronic health record, but do not capture workload from a number of other agencies responsible for the provision of mental health services (e.g., base community counseling centers) (Russell et al., 2016a).
The IOM (2014b) has repeatedly called on the DoD to “dedicate funding, staffing, and logistical support for data analysis and evaluation” (p. 84). Yet, comprehensive independent review after review reports, for the federal government, in particular, the DoD and the VA, in many cases, their responses do not match the extent of the problems, and “many readjustment needs are unmet or unknown” (e.g., IOM, 2013, p. 472). Consequently, since the outset of the Afghanistan and Iraq Wars, prevalence estimates for war stress injury are typically limited to a handful of psychiatric diagnoses (PTSD, depression, generalized anxiety, substance abuse, and TBI) as opposed to the full spectrum (Russell & Figley, 2015a). Moreover, the vacuum of centralized reporting in the DoD has been filled by a plethora of research studies within and outside the DoD and VA, resulting in wildly varying prevalence rates of specific post-deployment diagnosis, like PTSD ranging from 2 to 60% (e.g., Russell & Figley, 2015a). In other words, anyone and everyone is free to “cherry pick” statistics to fit their agenda or theory, resulting in chaos and controversy about the true state of mental health affairs, while conveniently providing the DoD plausible deniability. In contrast, on the medical side, there is no controversy or confusion around the number of military personnel with traumatic limb amputation, positive HIV, pregnancy, or other medical conditions, because there is only one single agency that is accountable, with a centralized database responsible for accumulating and taking care of medical needs.
Overt Attempts to Delay Recognition of Mental Health Crisis
Amid concerns over public reaction to a mental health crisis, with recurrent media reports of large numbers of untreated veterans separating from the military, suicide spikes, and other signs of social reintegration difficulty, the military ignored a foundational PR lesson from WWII calling for transparency. On May 23, 2006, the DoD published its PR policy, or Public Affairs Guidance (PAG), with the explicit purpose of “To coordinate accurate talking points and messages about the mental health of Soldiers returning from OIF/OEF for all military and VA spokespersons” (U.S. Army, 2006, p. 1).
Desired Effects
All Army spokespersons whether they are PAOs (public affairs officers), commanders, chaplains, healthcare providers, etc., will speak accurately and with one voice on the issue of mental health and deployed and returning Soldiers.
Buy-in and continuity of message with other organizations including National Guard Bureau (NGB), U.S. Army Reserve (USAR) and Department of Veterans Affairs (VA) are established and maintained.
Establish and demonstrate to the American public that even though combat affects all Soldiers mentally and physically, the majority of Soldiers returning from OIF & OEF are mentally healthy and transition home successfully. For Soldiers who may need temporary or long-term medical assistance for mental health disorders, the Army and VA are prepared to provide them the best health care possible during this time (p. 1).
The U.S. Army (2006) PR policy lists numerous “key talking points,” such as: “Unique to this war, is that military leadership is taking a proactive approach;” “The military is doing a number of things to reduce stigma and improve access to care;” “There are numerous opportunities for reserve and National Guard to receive immediate attention;” and “they (Army leaders) are proactively addressing mental health needs of Soldiers with early intervention and working to build resilience” (pp. 2–3)—all areas reported as chronically and seriously deficient by the DoD TF-MH (2007)—co-chaired by the Army Surgeon General. The military’s pre-2006 PR policy reflects a coordinated partial publicity ban intended to delay full disclosure about the actual size and scope of a mental health crisis that 1 year later is described as:
Against the backdrop of the Global War on Terror, the psychological health needs of America’s military service members, their families, and their survivors pose a daunting and growing challenge to the Department of Defense. The immediacy of these needs imparts a sense of urgency to this report. As such, the Task Force urges the Department of Defense to adopt a similar sense of urgency in rapidly developing and implementing a plan of action (DoD TF-MH, 2007, p. ES-4)
Public Deception and Usage of Propaganda
Military efforts to confuse or deceive government officials and the general public about the presence, severity, and broad scope of mental health crises can be detected by actions such as: (a) calculated decision since the Korean War to avoid collecting and/or publishing actual numbers of psychiatric casualties; (b) individual senior military officials releasing distorted, incomplete, or inaccurate statements to the media, Congress, and military populations designed to deny or minimize the crisis; and (c) issuance of written coordinated PR policies or propaganda that contain known or knowable falsehoods with the intention to deceive.
Calculated Deception in Record Keeping and Statistical Accounting
Citizens interested in the history of military mental healthcare can readily access the U.S. Army’s WWI (e.g., Bailey, 1929; Salmon & Fenton, 1929) and WWII (e.g., Glass, 1966a, b) lessons learned analyses. Each volume provides detailed statistical accounting of the psychiatric realities of war with the explicit purpose that future generations never again forget. For instance, transparent and complete data is available on the total numbers of soldiers diagnosed with specific neuropsychiatric conditions, numbers admitted to neuropsychiatric hospitals, numbers psychiatrically screened and rejected, and numbers receiving psychiatric discharges. Importantly, the same level of transparency is missing for the Navy and Marine Corps during the two world wars (e.g., Russell & Figley, 2015b). Nevertheless, after admitting culpability to a self-inflicted mental health crisis caused largely by ignoring WWI lessons (Glass, 1966a), the U.S. Army painstakingly compiled two massive data-filled volumes of WWII psychiatric lessons learned. In total, 1948 pages detailing every aspect of what is required to meet wartime mental health needs led the U.S. Army Surgeon General Heaton (1966) to sternly warn: “With this information so readily available, there can be little excuse for repetition of error in future wars, should they occur” (p. xiv).
Unfortunately, it appears that those lessons have repeatedly been ignored up to the present day (e.g., Russell & Figley, 2015a, b). It could be argued that the military appears to have made a calculated decision to avoid duplicating the transparency of the WWII cohort, opting instead for little to no recording of its psychiatric lessons and purposeful use of vague incomprehensible statistics. Consequently, individuals seeking similar detailed accounting of the psychological effects of the Korean War, Vietnam War, Persian Gulf War, and the Global War on Terror (GWOT) will be disappointed (e.g., Russell & Figley, 2015b). Statistical data on the prevalence of war stress injury are typically limited to incidence ratios of x per 1000 average troop strength for a specific month, year, or region, thus requiring researchers to locate manpower records of troop strength unique to the formula. For example, the Vietnam War cohort reported its prevalence of psychiatric casualties diagnosed with psychosis increased from 1.6 (1965) to 3.8 (1970) per 1000 average annual troop strength and psychoneurosis from 2.3 (1965) to 3.3 (1970) per 1000, but provided no data on absolute or total numbers (Neel, 1991). Surely, the military’s statistical reporting had to collect absolute numbers in order to accurately derive its ratios, but they ignored reporting this precise information instead of giving both.
Another method employed to deceive the general public and minimize the extent of a mental health crisis is by reporting inaccurate and/or incomplete prevalence data based on faulty diagnostic policies. For instance, frontline psychiatry policies have overtly restricted diagnostic labeling of psychologically injured deployed personnel until their condition deteriorates to imminent danger to self or others (Department of Army, 2009; Russell & Figley, 2017a), or covert diagnostic policies have pressured clinicians to avoid more severe and compensable diagnoses, like PTSD, in favor of minor nonservice-connected or compensable diagnoses, like personality disorder (PD), adjustment disorder, etc. (e.g., de Yoanna & Benjamin, 2009; Wilk, Herrell, Carr, West, Wise, & Hoge, 2016).
Deception by Official Authoritative Statements
Transparent acts of public deception are evident when top leaders in positions of authority provide verbal and/or written testimony on the status of military mental healthcare that are within weeks or months of being shown as inaccurate by the military itself. Military officials (civilian and active-duty) in senior leadership roles have ready access to aggregate data and reports on all aspects of mental healthcare (e.g., staffing levels, staff attrition rates, prevalence rates), and/or can cause such reporting to occur by merely asking. It is expected that senior military officials who make authoritative statements about the status of mental health services would either know or should know if those statements are factually true, beyond rare occasions of human error. For instance, readers are encouraged to review official statements by top military leaders to national news media (e.g., Zoroya, 2007a) and congressional testimony from 2004 to 2007 (e.g., Issa, 2007), and compare the factual bases of those statement with the June 2007 DoD TF-MH findings.
Case in point, at the 24 May 2007 Congressional hearing on: Invisible Casualties: The Incidence and Treatment of Mental Health Problems by the U.S. Military, many DoD officials gave testimony clearly contrary to the 16 June 2007 DoD TF-MH report of catastrophic system-wide failure in every aspect of mental healthcare (e.g., chronic, severe staffing shortages, inadequate access to timely, quality treatment), representing an urgent national public health crisis. Representative Issa’s (2007) very pointed questioning is informative. After hearing public testimony by a Deputy Secretary of Defense who oversees military medicine that: “The military health system is second to none in its ability to deliver timely, quality mental health, and behavioral care. In addition, walk-in appointments are available in virtually all military mental health clinics around the world” (Kilpatrick, 2007, p. 61), the Congressman alluded to reading a preview of the DoD TF-MH (2007) findings and retorted:
You had a lot of superlatives in your presentation, and I was a little surprised that there were quite as many of them as there were, terms like robust and touting surveillance programs, pre-deployment health assessments since 1998, mental health care in theater, the use of multi-faith chaplains, etc. It is in your testimony How do you explain the first panel? General Pollock I think did a very good job of saying, look, we make mistakes, things fall through the cracks. You didn’t do that in your testimony. I was a little surprised that, in light of what we are looking at here and some potential for falling through the cracks, that it was sort of gee, this thing says nothing is broken (p. 114).
In regard to severe staffing shortages, Representative Issa (2007) remarked: “I am going through the math and saying I bet you don’t have 400 psychiatrists and psychologists… why is it you are not asking for those kind of resources?” (p. 114) and added: “Again, I am going to go on to General Pollock, but I would really hope when you testify before Congress you come with the problems, not just the superlatives” (p. 114). However, a review of prior years of congressional testimony by military leaders reveals that the talking points are eerily similar from official to official and consistent with written public affairs narratives disseminated at the headquarters of the U.S. Army (2006) and Navy (2007). Issa’s (2007) factual questioning was made possible by a pre-reading of the DoD TF-MH (2007) report that directly contradicted the bright picture painted. Without factual data to the contrary, the military’s authoritative statements largely go unchallenged. Whether intentional or not, public statements by credible military officials have the propensity to mislead and deceive the public.
Military Propaganda and Public Deception
The Task Force arrived at a single finding underpinning all others: The Military Health System lacks the fiscal resources and the fully-trained personnel to fulfill its mission to support psychological health in PEACTIME or fulfill the enhanced requirements imposed during times of conflict (DoD TF-MH, 16 June 2007, p. ES.2).
After 6 years of public statements and sworn testimony to the contrary, on 16 June 2007, the DoD finally became transparent and reported a major public health crisis, caused principally by chronic neglect and cataclysmic institutional deficiencies (DoD TF-MH, 2007). Invisible to the public is that senior military and congressional leaders were well-informed of the mental health discrepancies and required corrective actions as early as 2004 in order to avoid a crisis that would predictably harm countless veterans and their families (e.g., Russell, 2006b). This forewarning included a widely circulated DoD IG’s grievance against military medicine in January 2006, documenting failure in staffing, training, treatment, monitoring, family support, stigma, and organization (e.g., Russell, 2006a; Zoroya, 2007b). This echoed charges by past mental health officers: “A frequent comment by frustrated and harassed psychiatrists during World War II was that responsible authorities failed to heed the lessons learned by psychiatry in World War I” (Glass, 1966b, p. 735).
However, rather than proactively addressing obvious mental health deficiencies, such as severe staffing shortages, attrition, and inadequate treatment (e.g., Russell, 2006a, b), on 23 January 2007, the U.S. Navy issued a PR policy regarding mental health in the form of written Public Affairs Guidance (PAG) with the stated purpose: “All Navy spokespersons whether they are PAOs (public affairs officers), commanders, chaplains, health care providers, etc., will speak accurately and with one voice on the issue of mental health and deployed and returning Sailors and Marines” (p. 1). Per the U.S. Navy (2007) headquarters, the reason for the PAG was “On September 22 2006, Stars and Stripes (Pacific Edition) published an article titled “Officer Sees ‘Perfect Storm’ Brewing in Military’s Mental Health Care System.” The article quoted CDR Mark Russell, a Navy psychologist stationed at U.S. Naval Hospital (NH) Yokosuka [this paper’s first author]. The USA Today article reiterates CDR Russell’s position that the military does not have enough mental health providers” (p. 1). The U.S. Navy’s (2007) PR policy mirrored the U.S. Army’s (2006) existing PAG listing “Key Messages and Talking Points” including:
Navy Medicine’s goal is to ensure that every returning Sailor and Marine receives any necessary mental health care services as early as possible—providing prevention and treatment services as early as possible is the best way to prevent the long-term effects of war.
Navy and Marine Corps leadership are committed at every level to the issue of mental health. They are proactively addressing mental health needs with early intervention and working to build resilience prior to combat deployments.
Navy Medicine has more mental health resources available at home and in theater than ever before in an attempt to provide Sailors and Marines with information about combat stress and its impact on mental and behavioral health.
Navy Medicine continuously monitors access and utilization of mental health assets and is working to increase the number of providers and portals to care where needed (p. 1).
Five months later, the DoD TF-MH (2007), co-chaired initially by the Army and then the Navy Surgeon General, contradicted the military’s official messaging. Moreover, in regard to the U.S. Navy’s (2007) claim of “working to increase the number of providers,” on 28 February 2007, the Navy headquarters issued a memorandum to eliminate its military social work billets, which was reversed only after the June 2007 DoD TF-MH findings were published:
There is an inadequate number of providers. A thorough review of available staffing data and findings from site visits to 38 military installations around the world clearly established that current mental health staff are unable to provide services to active members and their families in a timely manner; do not have sufficient resources to provide newer evidence-based interventions in the manner prescribed (p. 43)… [and] the military faces significant challenges in recruiting and retaining active duty mental health professionals. The number of active duty mental health professionals is likely to continue to decrease unless incentives change (p. 46).
However, manpower and personnel details, including mental health staffing and attrition rates, are routinely tracked and reported throughout the DoD (e.g., Russell, 2006a). Therefore, not issuing authoritative pronouncements of mental health staffing numbers and treatment access, or remaining silent about a known crisis, represent strategies that allow the military’s narrative to continue, and they possibly constitute a public deception that delays necessary remedies to help soldiers with mental health difficulties.
Silencing of Whistleblowers
Another harmful, less conspicuous component to the military’s delay and deception tactic is the silencing of mental health whistleblowers. Federal laws and government regulations provide legal protection of lawful whistleblowers against reprisal (e.g., DoD, 2007). Yet, cases of whistleblowing about military-related mental health issues have not led to legal protections and appear to be systematically overridden by a desire to punish and/or intimidate future potential whistleblowers to prevent or delay unwanted disclosure. For instance, in 2012, the Army suspended several doctors at Joint Base Lewis-McChord who unethically altered the deployment-related PTSD diagnosis of soldiers to nonservice connected psychiatric conditions, like PD, and adjustment disorder, in order to reduce pension costs (e.g., Bernton, 2012a, b). However, unknown to most, the Army suspended the retired Army psychiatrist who informed Congress and the news media about the Army’s illegal diagnostic practices (Phillips, 2013). Similarly, several Army mental health clinicians claimed they experienced retribution after informing the news media about wrongful misconduct discharge practices of deployed soldiers diagnosed with PTSD and TBI at Fort Carson, Colorado (Phillips, 2013). In addition, allegations of reprisal were made by a senior Navy psychologist after speaking out to prevent the current mental health crisis (Russell, 2007; Zoroya, 2007b), as well as two senior VA psychiatrists who publicly revealed harmful pain prescription policies (e.g., Bahorik, 2013; Gray, 2013).
In each of the above cases, mental health whistleblowers initially raised their concerns internally before going public (e.g., Zoroya, 2007a). Moreover, in each instance, the DoD and VA eventually validated the legitimate concerns of patient safety raised by lawful whistleblowers and were ordered by Congress to fix the problem (e.g., Gray, 2013; Phillips, 2013). Taken together, an alarming trend emerges that has a potential chilling effect on shedding public light on future mental health problems.
Delay Through Appeasement, Half-Measures, and Partial Compliance
When a mental health crisis can no longer be denied, the Congress and President will customarily dictate reforms through legislation (e.g., Wounded Warriors Act, 2009) and/or Executive Order (2012). The military might give the public an appearance of concern, commitment, and compliance while delaying full implementation, by engaging in half-measures or partial compliance. For instance, amid rampant reports of unmet military mental health needs and suicides, in October 2005, the Congress mandated the DoD to establish a mental health task force (Shane, 2006). It took the military until May 2006 (7 months) to establish the task force, and then another 13 months to disclose its findings (DoD TF-MH, 2007). There are other times when urgent need for a different approach or learning from past mistakes is called for, yet with little policy changes. For example, “The time for action is now. The human and financial costs of un-addressed problems will rise dramatically over time. Our nation learned this lesson, at a tragic cost, in the years following the Vietnam War” (DoD TF-MH, 2007, p. 63).
It is commonplace for compliance with externally mandated remedial actions regarding military mental healthcare to take years from time of investigation, perhaps in the hope that interest will wane (e.g., Russell et al., 2016b). For example, the Government Accountability Office (GAO, 2015) has conducted multiple investigations describing the DoD’s incremental and partial compliance with mandatory changes to its PD discharge policy, concluding:
The military services lack separation policies that address all of DOD’s eight requirements for separating service members with non-disability mental conditions; both DOD and the services also lack oversight over such separations. From fiscal years 2008 through 2012, DOD required the services to report on their compliance with DOD requirements for PD separations, one of the non-disability mental conditions. Most of the services reported by fiscal year 2012 that they were not compliant with all eight requirements and many of the 20 reports contained incomplete and inconsistent information (p. 1).
Additionally, the GAO (2010) was tasked to reassess DoD’s compliance with repeated recommendations by six separate independent commissioned studies and the DoD’s TF-MH (2007) to reduce stigma and organizational barriers to care concluding:
DOD has efforts underway to improve perceptions about mental health care for service-members and, to a comparably limited extent, deployed civilians, but has not clarified or updated certain policy provisions that may contribute to mental health care stigma. DOD officials and health care providers said that certain policies are unclear or out-of-date and limit career opportunities for individuals who have sought mental health care. A 2014 RAND Corporation report identified 203 DOD policies that may contribute to stigma. DOD is not well positioned to measure the progress of its mental health care stigma reduction efforts (p. 1).
Likewise, the IOM (2014b) has performed multiple studies on the DoD’s PTSD treatment programs, revealing a similar pattern of gradual, but limited compliance: “PTSD management in DoD appears to be local, ad hoc, incremental, and crisis-driven with little planning devoted to the development of a long range, population-based approach (p. 6).”
Basically, it appears that the purpose of the military’s delay strategies might be to avoid expending resources toward mental health problems. Perhaps the military generally does not feel responsible for these problems, does not want to spend money on them, etc. Moreover, delaying recognition and action allows the military to transfer costs of mental healthcare to the VA and private sector. It would appear that the military mindset about mental health might be that any war will be over before the military is forced by outsiders to fundamentally transform its mental health policies.
Harmful Impact of Delay Strategies
No direct empirical evidence exists to test the assertion that the military’s delaying strategies have harmed war veterans and their families, largely due to the strategies outlined thus far. However, anecdotally, an estimated 237 active-duty service members and 22 veterans a day committed suicide during the nearly 2 years it took the DoD to complete its internal review and finally admit to a national crisis of its own creation (DoD TF-MH, 2007; Ramchand, Acosta, Burns, Jaycox, & Pernin, 2011). Untreated war stress injury, such as PTSD, is a problem-multiplier associated with heightened risk of depression, substance abuse, medically unexplained physical conditions, domestic violence, child abuse, divorce, unemployment, homelessness, and criminal misconduct (e.g., Department of Army, 2006; Department of Navy and U.S. Marine Corps, 2010; DVA/DoD, 2010; Russell & Figley, 2015a, b).
However, there are strong disincentives for the military to collect, yet alone report on the true spectrum of war stress injury (e.g., Russell & Figley, 2015a) or clinical outcomes for service members receiving military mental healthcare, despite repeated recommendations from various commissioned studies (e.g., IOM, 2014a). However, one can simply look to the U.S. military subject matter experts who since WWI have cited the critical need for early identification and treatment of war stress injuries as a critical wartime “lesson learned”:
WWI
First, that it is not only in accordance with the best scientific practice to treat soldiers suffering with war neuroses as early and as effectively as possible but to do so is an important contribution toward the conservation of manpower and military morale (Salmon, 1929a, p. i).
WWII
A most pronounced characteristic of the cases seen early in their illness is the profusion with which new symptoms appear and disappear. As time goes on, without treatment, a more stabilized syndrome crystallizes (Grinker & Spiegel, 1943, pp. 7–8).
GWOT
The policy of tolerating long waits for initial mental health clinic appointments is inconsistent with the frequency and magnitude of mental health problems in the military. The stressors inherent in military life make basic mental health services as critical and time-sensitive as basic medical care. For individuals under stress, psychological health problems may quickly deteriorate. Stigma may cause active duty members to delay seeking help. As such, timely intervention is crucial (DoD TF-MH, 2007, p. 43).
The above statements represent a small sample of evidence that the military is very cognizant of the importance for early identification and treatment of war stress injuries. In fact, the military has adopted public policies mandating as such: “Clinicians should use the 2010 VA/DoD CPG for the Management of Post-Traumatic Stress in the assessment and treatment of patients presenting with symptoms of traumatic stress” (Department of Army, 2012). And yet, peeling away from the rhetoric, independent commissioned studies repeatedly reveal the true extent of the military’s commitment toward complying with its mental health policies:
DoD lacks a mechanism for the systematic collection, analysis, and dissemination of data for assessing the quality of PTSD care. Metrics of program effectiveness, quality of care, program awareness, and availability and acceptance of PTSD services are needed. There are no specific DoD policies or procedures that stipulate the use of measurement-based care for PTSD and no consistent use of standardized outcome measures, before, during, or after treatment (IOM, 2014b, p. 87).
Such contradictions between official policy pronouncements and actual actions on the ground are evidence of inconsistency and half-measures. We found analogous evidence of marginal, partial, and noncompliance with mental health regulations in every aspect of military mental healthcare, including screening, prevention, assessment, treatment, substance abuse rehabilitation, TBI screening, reintegration, family support, staffing, stigma, data management, service delivery, and training, (e.g., Russell et al., 2016b). Therefore, strategies intended to avoid implementing war trauma lessons by delay or deception are invariably harmful to veterans, their families, and society.
Strategy 7: Faulty Diagnosis and “Backdoor” Discharges
Being diagnosed with a mental health condition is the leading reason for military administrative separations (Hoge, Toboni, Messer, Bell, Amoroso, & Orman, 2005), but proper diagnosis is also required for timely access to appropriate high-quality treatment (e.g., DVA/DoD, 2010). Another tactic the military relies upon to prevent psychiatric attrition, treatment, and disability pensions is avoiding accurate psychiatric diagnosis by rendering faulty and highly stigmatizing diagnoses (e.g., PD, lacking moral fiber) and awarding diagnoses that allow for administration separations (ADSEP) that are devoid of service-connection (e.g., adjustment disorder) and eligibility for VA benefits or what is oft called “backdoor” or “bad paper” discharges.
Policies for Avoiding Diagnosing War Stress Injury
Thus, a solution was found for the excessive medical discharge of “psychoneurotic” cases, which consisted of both a change of psychiatric nomenclature and a tightening of the medical discharge process. The benefits of this hard-won lesson learned in World War II were continued during the Korean War and have become a permanent part of the policies and procedures of military psychiatry in the U.S. Armed Forces (Glass, 1966a, p. 757; U.S. Army Office of Surgeon General).
As illustrated above, the military regularly establishes policies that restrict psychiatric diagnosis of war stress injury. While some or many service members may benefit from policies that limit psychiatric diagnosis due to possible stigma, others are harmed by delaying appropriate diagnosis and treatment. Use of punitive and highly stigmatizing labels pertaining to cowardice (e.g., lacking moral fiber), desertion, malingering (e.g., gold-bricker, pension-seeking neuroses), and hysteria [e.g., Not Yet Diagnosed Neurotic (NYDN) in place of shell shock], as well as euphemisms conveying transient stress reactions expected to resolve rapidly with brief respite (e.g., combat fatigue, battle fatigue, combat exhaustion, flier’s fatigue, combat stress reaction, combat and operational stress reactions), all represent military policies for avoiding psychiatric labeling with the explicit purpose of preventing psychiatric attrition, treatment, and pensions (e.g., Russell & Figley, 2017a; Russell et al., 2017b).
Insight into the military’s pejorative view toward psychiatric diagnosis is gleaned from the U.S. Army (1944) Office of the Surgeon General’s Memorandum on Psychoneurosis (Combat Exhaustion). The diagnosis of psychoneurosis was the acceptable medical label at the time and is a precursor to modern-day diagnoses of anxiety disorders, PTSD, and somatoform disorders. However, the U.S. Army (1944) defined psychoneurosis as “a condition, not a disease, which results from an individual surrendering to an adverse situation. It manifests itself in many ways and varying degrees from a mild hypochondria to a severe anxiety neurosis” (p. 1031). In regard to etiology, the Army Surgeon General report stated: “The basic causes of psychoneurosis is insufficient courage” (p. 1031). In response to mass psychiatric attrition and disability discharges for psychoneurosis, the Surgeon General advised: “Psychoneurosis is not a problem in the Russian Army. The Russians punish cowardice with death” (p. 1033). Fortunately, other senior medical leaders pushed back against the antidiagnosis bias.
In March 1943, the U.S. Army abandoned its failed social experiment to purge weakness from its ranks via psychiatric screenings. Rather, it reinstated WWI-era frontline mental health services because “The problem of neuropsychiatric disabilities under modern battle conditions has been a serious one. Approximately 20 percent of all nonfatal casualties are psychiatric in origin” (U.S. Army, 1943, p. 11). In addition, the Army mandated changes in diagnostic classification: “Hence, the only diagnosis permitted was “exhaustion” in line with the policy established by General Bradley’s directive in II Corps on 26 April 1943” (Glass, 1966a, p. 11).
Justification for the military dictating psychiatric diagnostic practices includes concerns about the iatrogenic and stigmatizing effects of psychiatric labels, like psychoneurosis, along with self-fulfilling prophecies of treating war-stressed soldiers as psychiatric patients (e.g., Russell & Figley, 2017a, b). Additionally, reports of successfully returning 60 to 98% of acutely emotionally injured soldiers back to the frontlines after brief respite periods, coupled with anecdotal reports of significantly lower RTD rates when soldiers are medically evacuated and treated for psychiatric diagnosis, provided some face validity to the military’s policy of avoiding psychiatric diagnoses as beneficial to the health and well-being of the troops (e.g., Russell & Figley, 2017b). However, the primary impetus for the military’s change in practice in dictating psychiatric diagnoses is more straightforward: “With the high rates of medical separations threatening to decimate the Army, concern reached the highest military authorities. On 11 November 1943, the War Department reversed the previous liberal discharge policy and established a policy of salvage and maximum utilization of marginal personnel. A prompt effect of this directive was a precipitous decline of the medical discharge rate” (Glass, 1966a, p. 755). Importantly, some senior Army psychiatry leaders disagreed with a headquarter-driven diagnostic doctrine:
It has been suggested that cases of psychoneurosis should be designated by other terms in the hope of escaping the stigma attached to psychoneurosis. This office is strongly opposed to such a policy. There is ample evidence as to the unwisdom of employing euphemisms for well-established medical entities. The difficulty is not with the term, but rather with the attitude toward and understanding of the term (Colonel Menninger, 1944, cited in Menninger, 1966, p. 814).
After World War II, publication of WD Technical Bulletin 203 significantly revised diagnostic nomenclature into two categories: (1) transient personality reactions that were divided into either combat exhaustion or acute situational maladjustments; and (2) immaturity reactions that could be applied to chronic symptoms and lead to administrative separations (e.g., PD, Glass, 1966a)—essentially eliminating psychiatric diagnoses that might result in medical discharge and disability pension. Predictably, the military’s new diagnostic policies had the desired effect:
The new diagnostic categories made unnecessary the widespread usage of the term ‘psychoneurosis’ for situationally induced psychiatric disorders. As a result, the incidence of psychoneurosis, a distant cousin to PTSD, declined sharply and remained at low levels even during the Korean War (Glass, 1966a, p. 756).
Importantly, the military’s diagnostic policies meant that soldiers who were unable to RTD because of more chronic or severe stress reactions would be more susceptible to charges of cowardice, malingering, and/or predisposed weakness (e.g., PD; Lerner, 2003).
Contemporary Diagnostic Policies
Today, the military’s diagnostic policy remains essentially unchanged although the labels have evolved. For example, combat and operational stress control (COSC) personnel are required to defer making psychiatric diagnosis except under specific circumstances to preserve the soldier’s expectations of normalcy and return to duty, as well as avoiding stigma associated with psychiatric labeling in that: “It is both inappropriate and detrimental to treat Soldiers with COSR (combat and operational stress reaction) as if they are a BDP (behavioral disordered patient)” (Department of Army, 2006, p. 11-1). Amidst a plethora of negative publicity and Congressional scrutiny over the military’s use of backdoor discharges to manage its mental health problem, the Department of Army (2012) published its policy on psychological assessment and diagnosis of war stress injury:
Military healthcare providers understand that caution is required in attributing current PTSD-like symptoms to certain diagnoses that can result in harmful clinical, occupational, or administrative consequences for the SM (service member), particularly malingering, PDs, or adjustment disorders. These conditions are often perceived as judgmental or pejorative, can result in administrative separation (or Uniform Code of Military Justice action in the case of malingering), and/or can influence how other medical care providers approach or treat patients when they see one of these diagnoses in the problem list. Patient-centered care within a culture of trust requires that care providers focus on patients’ primary concerns, and these diagnoses, when inappropriately used, can damage therapeutic rapport and interfere with successful care (p. 4).
However, the DoD’s commitment to its diagnostic policy is best determined by the level of compliance and accountability of military personnel choosing to uncharacteristically disobey authority. To that end, the GAO’s (2010) reinvestigation of PD discharges shows:
Most of the services reported by fiscal year 2012 that they were not compliant with all eight requirements and many of the 20 reports contained incomplete and inconsistent information (p. 1).
Moreover, in 2016, the Secretary of Army responded to congressional calls for investigating allegations of noncompliance with its discharge policies by wrongfully awarding 22,194 OEF/OIF soldiers diagnosed with war stress injury (e.g., PTSD, TBI) an other than honorable (OTH) ADSEP for misconduct instead of considering treatment, revealing:
The Army remains confident in the administrative processes that define misconduct separation procedures. Although the Army was not always able to produce evidence that a mental health evaluation was considered by the separation authority, that finding alone does not mean the separation authority did not review it, or that the Army was non-compliant with 10 U.S.C. §1177 (Secretary of Army, 2016; p. 1).
Potential Harm from the Military’s Diagnostic Policies
While deferral of diagnosis may have merit in some or many cases, the military’s diagnostic policies can also cause harm by compounding problems and delaying access to appropriate treatment. According to the U.S. Army, “Once mental disorder symptoms emerge, the most effective strategy for ensuring recovery lies in prompt application of evidence-based treatments” (J-MHAT, 2011, p. 78). In 2004, the DVA and DoD published their joint practice guidelines for managing post-traumatic stress that included expert consensus recommendations for use of the identified evidence-based treatments (DVA/DoD, 2004). The practice guidelines were updated in 2010 and explicitly state the necessity for timely PTSD treatment: “The clinically significant symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning. The symptoms last more than 3 months after exposure to trauma. Chronic PTSD is unlikely to improve without effective treatment” (DVA/DoD, 2010, p. 24). However, the military’s RTD mandate coupled with restricting psychiatric evacuations for treatment outside war zones inevitably results in delays in accessing quality, effective treatment (e.g., Russell & Figley, 2017c). Consequently, returning veterans with unidentified and/or untreated war stress injury are at high risk of a host of post-deployment readjustment problems that could result in legal involvement, family conflict, and suicide (e.g., DVA/DoD, 2010; Russell & Figley, 2017c).
Faulty Diagnosing of War Stress Injury
A major concern for war veterans and their families is whether a potential or actual war stress injury is intentionally not diagnosed, and, instead, the service member is given a label only related to their misconduct or a pre-existing nonservice-connected condition. For instance, drug use is frequently associated with war stress injury like PTSD (e.g., DVA/DoD, 2010) but is also grounds for legal action and OTH ADSEP. Also, war veterans can be given diagnoses such as PD, adjustment disorder, or schizophrenia that are not rated as service-connected, thus subject to potential loss of VA benefits (e.g., DoD, 2017). For instance, during the Vietnam War, relatively low (2 to 5%) rates of classic “combat exhaustion” or “combat fatigue” casualties were heralded by military leaders as a victory over combat stress, attributed to a 12-month rotation and frontline psychiatry policy intended to reduce attrition (Jones, 1995). At the same time, some 300,000 Vietnam veterans were diagnosed and discharged with nonservice-connected disabilities (Ader, Cuthbert, Hoechst, Simon, Strassburger, & Wishnie, 2012) in the context of exceedingly high incidence of “character and behavior disorders,” including diagnoses such as PD, substance abuse, and “indiscipline” (akin to misconduct stress behaviors), as well as dramatic rises in “psychosis” 1.6 (1965) to 3.8 (1970) per 1000 (e.g., Russell & Figley, 2015b).
Contemporary Trends of Faulty Diagnosing
There is no evidence of a broad military conspiracy to wrongfully alter diagnosis to reduce costs of treatment and pensions. However, a string of media stories reveal that such practices do exist. For instance, an Army psychiatrist was audio-recorded disclosing to his Army patient widespread pressure exerted on mental health clinicians to avoid giving PTSD diagnosis to war veterans: “Not only myself, but all the clinicians up here are being pressured to not diagnose PTSD and diagnose Anxiety Disorder Not Otherwise Specified instead” (de Yoanna & Benjamin, 2009). A 2012 news story revealed a widely circulated Army memo from medical leaders at Joint Base Lewis-McChord, Tacoma, Washington, advising mental health providers that a PTSD diagnosis costs $1.5 million over a service member’s lifetime and warned doctors to be careful about “rubber-stamping” the diagnosis, in the interest of saving taxpayer dollars (Bernton, 2012a, b). An investigation by the Seattle Times and Washington State Senator Patty Murray revealed unethical conduct by a forensic mental health team changing the post-deployment PTSD diagnoses of 285 soldiers to nonservice-connected psychiatric conditions, like PD and adjustment disorder, leaving them potentially ineligible for medical disability compensation and VA benefits (Bernton, 2012a, c).
Moreover, a recent anonymous survey of 543 Army mental health providers reported clinical data for 399 service member patients, of whom 110 (28%) were reported to be suffering from PTSD (Wilk et al., 2016). However, an audit of the electronic health records revealed that 41% of soldiers reported to have PTSD by their mental health provider were not actually given a PTSD diagnosis (Wilk et al., 2016). Instead, they were diagnosed with administrative situations (e.g., post-deployment related encounter) or lesser psychiatric conditions, like adjustment disorder. The most common reason for not recording PTSD was reducing stigma or protecting the service. However, whatever the rationalization, rendering faulty diagnosis is considered unethical by professional mental health associations (e.g., American Psychological Association, 2002) as well as a violation of the military’s own policies. For example, per Department of Army (2012), “An adjustment disorder diagnosis should not be given if there is evidence that the individual has another specific Axis I disorder that explains the symptoms;” such as PTSD (p. 7). Such misdiagnosing of war stress injury like PTSD is problematic for a host of reasons: (a) prevents military personnel from requesting service-connected disability benefits after they leave the military, (b) can interfere with continuity of care and receiving appropriate PTSD treatment when service members change duty stations every 2–4 years, (c) underestimates mental health demand and needed resources by distorting military prevalence statistics that are based entirely on electronic health record diagnoses, and (d) working around stigma serves only to reinforce stigma in the military.
Backdoor Discharges
Diagnosis, however, was of paramount importance. On the one hand, psychoneurosis was classified as an illness for which an honorable discharge could be readily accomplished under medical auspices. On the other, a diagnosis of an inadequate or other PD which was not considered an illness would result in the return of the patient to duty for possible administrative discharge because of inadaptability or undesirable habits and traits of character. Such “Section Eight” discharges could be white (honorable) or blue (without honor) with the onus of social disapproval as well as the denial of certain veteran’s benefits (Glass, 1966a, p. 732).
One strategy used by the military for service members with war stress injuries is to administratively separate (ADSEP) said veterans, which is also called backdoor discharges (e.g., GAO, 2008). Backdoor discharges can originate through either legal or medical channels. They simultaneously send message to the remaining unit members and serve to reduce costs associated with psychiatric treatment, VA benefits, and disability pensions.
The Legal Backdoor: “Bad Paper” Discharges
Service members convicted by courts-martial or administratively adjudicated for a pattern of misconduct (e.g., repeated minor rule violations) are subject to “bad paper” discharges, including bad conduct or dishonorable discharges, or an OTH ADSEP. This results in forfeiture of military retirement pension, VA disability, and treatment benefits, as well as presenting significant barriers for future employment (see Russell et al., 2017b). Frequent reasons for bad paper discharges are substance abuse (e.g., illicit drug use, wrongful prescription drug use, repeat DUI), interpersonal violence (e.g., sexual assault, domestic violence, child abuse), absence without leave (AWOL, desertion), and patterns of misconduct (e.g., repeatedly being late to work, disrespectful conduct, minor rule violations; Bernton, 2012e; Kors, 2010; Phillips, 2013; Russell et al., 2017b). All are also common sequelae of war/traumatic stress injuries, like PTSD (e.g., DVA/DoD, 2010) and misconduct stress behaviors (e.g., Department of Army, 2006). Consequently, the majority of mentally ill or war stress-injured veterans discharged for misconduct are traditionally barred from receiving psychological health and substance abuse treatment both during and after military service (e.g., GAO, 2017).
Adverse or OTH ADSEP for patterns of misconduct or in lieu of courts-martial is often used by Commanders to expeditiously punish and get rid of problematic personnel, which is deemed necessary to maintain good order and discipline within the military (e.g., GAO, 2017; Kors, 2010; Phillips, 2013). The problem, however, is when military personnel are subject to bad paper discharges during or after deployment(s) and who otherwise have exemplary service records prior to deployment. We are not suggesting that war veterans who commit serious crimes (e.g., murder, rape) should not be held legally accountable for their actions. Most military leaders and legal personnel need to balance the legitimate circumstances of war veterans with the needs of the service and legal justice. However, some leaders may intentionally misuse their power to punish burdensome war veterans, or do so out of benign neglect, therefore, failing to consider mental health interventions prior to legal redress when appropriate (e.g., Phillips, 2013).
Concerns over Backdoor and Bad Paper Discharges
Multiple news media reports paint a tragic portrait of the military’s wrongful use of the legal backdoor to deal with veterans with war stress injury (e.g., Kors, 2010; Phillips, 2013; Murphy, 2011). During WWII, a reported 90,000 military personnel received OTH ADSEP for misconduct (Ginzberg, 1959). The military’s bad paper stratagem for dealing with its mental health dilemma intensified during the Vietnam War. For instance, some 560,000 Vietnam veterans reportedly received discharges under conditions that were less than honorable, with 260,000 of those “bad paper” discharges—either OTH (also sometimes termed undesirable), bad conduct, or dishonorable discharges, raising the specter of backdoor discharges (Izzo, 2014). Per Congressional leaders:
Many bad-paper veterans are among the 250,000 ex-combat soldiers who suffer from post-traumatic stress disorder. They have a higher incidence of unemployment, violent behavior, alcohol and drug abuse, family problems and homelessness than other veterans. Yet we won’t give them the treatment that could help them heal. They served their country and deserve treatment for their war wounds, physical and mental (Waters & Shay, 1994, p. 1).
In 2007, a high-ranking Navy doctor was on advisory to colleagues that the military is discharging Marines and Soldiers for misconduct when in fact they are merely displaying symptoms of PTSD (Carpenter, 2010). This was followed by a 2011 Stars and Stripes article describing multiple cases of previously deployed soldiers with prior clean records and diagnosed with war stress injury (e.g., PTSD, TBI, depression, substance abuse) who were reportedly pressured by their commanders to accept OTH ADSEP instead of courts-martials for relatively minor misconduct, including 10 cases of first-time drug use (Murphy, 2011). In June 2014, the Army Surgeon General launched an investigation into frequent complaints about Army mental health clinicians conspiring with Fort Carson commanders to deny PTSD diagnosis of returning war veterans in favor of OTH ADSEP for misconduct (e.g., Phillips, 2013; Secretary of Army, 2016). On 28 October 2015, the Army reportedly gave 22,194 war veterans OTH ADSEP for misconduct instead of treatment for post-deployment diagnosis of PTSD, TBI, or other psychiatric conditions (Zwerdling, 2015). Furthermore, on 4 November 2015, 12 U.S. Senators tasked the Army to investigate complaints of wrongful legal backdoor discharges (Secretary of Army, 2016).
In response, on 16 April 2016, the Secretary of Army reported an internal audit of the 22,194 ADSEPs, revealing that a total of 6364 discharged soldiers were diagnosed with a potential war stress injury, 4837 soldiers with PTSD, and 2624 with TBI (Secretary of Army, 2016). The remaining 15,830 discharged soldiers were excluded from review because of diagnoses other than PTSD/TBI, in contrast to everything known about the spectrum of stress injury (e.g., Department of Navy and U.S. Marine Corps, 2010). Rather than make a good-faith effort to investigate claims of improper backdoor discharges, the Army proceeded to further eliminate cases to be reviewed by utilizing rigid case selection criteria (e.g., only soldiers diagnosed within 2 years of deployment). Consequently, the Army’s internal audit found that “only” 3327 soldiers diagnosed with combat-related PTSD and/or TBI were ADSEP for misconduct, but 2933 of those received “honorable discharges,” with the remaining 324 soldiers receiving OTH (Secretary of Army, 2016). However, upon further scrutiny, the Army reversed itself and said that 96% of 2933 soldiers actually received General, not honorable discharges (Zwerdling, 2016), thus prohibiting certain VA benefits (see Russell et al., 2017b). The Army’s in-depth analysis of the 324 OTH discharges determined the Army complied with its regulations in 64% (293) of the cases (Secretary of Army, 2016). The Army also reported additional audits of alleged wrong doing were conducted and identified another 101 cases warranting further review. In the end, however, the Army Secretary reached the conclusion: “The Army does not routinely separate soldiers for misconduct who have been diagnosed with PTSD or TBI to save time or resources” (Secretary of Army, 2016, p. 1) Table 1.
To our knowledge, this is first time the military has publicly been held accountable to explain its discharge policies of war veterans. While it may be true that the majority of discharges have been fairly adjudicated, the Army’s response raises serious concerns, for example: (a) the lack of independent outside review, (b) selectively reviewing only the 22,128 cases identified in a news story versus a comprehensive fact-finding audit of all discharges, and (c) applying stringent administrative criteria to exclude cases from review. In addition, the policy continues to prohibit war veterans from accessing needed VA mental health treatment (e.g., Ader et al., 2012). Fortunately, under intense congressional scrutiny, the VA will now consider granting treatment access to veterans with bad paper discharges (GAO, 2017). Bad paper discharges are not only an Army problem. For example, Table 1 indicates the steady rise in Air Force misconduct ADSEP, so that is an issue across all service branches (e.g., GAO, 2017).
Recent Findings of Military Compliance with Misconduct Discharges
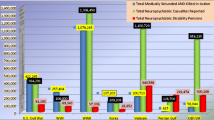
One might assume that, given the level of news media and Congressional scrutiny over its discharge policies, the military might at least temporarily abandon its use of this avoidant strategy. However, in 2017, the GAO released its most recent survey of the DoD’s compliance with legal and policy mandates to eliminate backdoor discharges. The GAO (2017) found that 57,141, or 62%, of the 91,764 service members ADSEP for misconduct from fiscal years 2011 through 2015 had been diagnosed within the 2 years prior to separation with PTSD, TBI, or other psychiatric conditions often associated with misconduct and post-deployment sequelae (e.g., Department of Army, 2009). Of the 57,141 service members, 23%, or 13,283, received an OTH characterization of service (see Fig. 1). Importantly, 6534 previously deployed personnel agreed to accept an OTH ADSEP in lieu or instead of a courts-martial (GAO, 2017). In Dave Phillips’ (2014) Pulitzer Prize series on legal backdoors, several service members featured accused the military of strong arming or threatening them with jail time, bad conduct discharge, and possible felony conviction via courts-martial if they did not or accept a quick, less than honorable exit (ADSEP).
Diagnosis status and characterization of service for service members separated for misconduct from fiscal years 2011 through 2015 (GAO, 2017). Available at https://www.gao.gov/products/GAO-17-260. Notes: The data include data for active-duty officers and enlisted service members who were separated to civilian life. Other separations such as those due to death joining officer commissioning programs or separating to the National Guard or Reserve have been excluded. We defined separations for misconduct as administrative separations for misconduct and administrative separations in lieu of trial by court-martial. We defined diagnoses of PTSD, TBI, or other certain conditions as diagnoses made within 2 years prior to a service member’s separation date. The other conditions included in our study are adjustment disorders, alcohol-related disorders, anxiety disorders, bipolar disorders, depressive disorders, and substance-related disorders. While in this figure we present data on characterization of service for service members diagnosed with PTSD, TBI, or other certain conditions, these proportions largely held true for the smaller population of service members diagnosed with PTSD or TBI. Specifically, 71% of service members diagnosed with PTSD or TBI received “general,” 23% received “other than honorable,” 4% received “honorable,” and 2% received other characterizations of service. aThis category does not include service members who were also diagnosed with PTSD or TBI. For the purpose of our analyses, we included these service members only in the “diagnosed with PTSD or TBI” category. bOther is defined as nonapplicable, uncharacterized, or unknown
Psychiatric Backdoor Discharges
There are two key ways the military can utilize improper or faulty psychiatric diagnosis and ADSEP for problematic personnel with war stress injury, weaponizing stigma, and/or reducing costs associated with psychiatric treatment, VA benefits, and pensions: (1) diagnosis of mental health conditions considered pre-existing and/or nonservice-connected and (2) diagnosis of PD.
Pre-existing Nonservice-Connected Psychiatric Conditions
Whether intentional, or through incompetence, service members with war stress injury can be misdiagnosed and ADSEP with a psychiatric condition the etiological origin of which is not directly connected to military service or being deployed to war zones (e.g., Wilk et al., 2016). During WWII, an Army Brigadier General reported “127,000 men with neuropsychiatric difficulties have been discharged on an administrative basis” (Menninger, 1966, p. 144). Today, such pre-existing or nonservice-connected conditions include, but are not limited to, ADHD, impulse control disorder, sleep-walking, specific learning disorder, adjustment disorder, or other conditions that typically originate in childhood or adolescence or are deemed “unsuitable” for further military service (DoD, 2017). Once diagnosed, service members can be ADSEP under the category of “Convenience to the Government” (DoD, 2017), typically with characterization of discharge as General under honorable, which is less than honorable (DoD, 2017). Essentially, those service members, regardless of time in service and deployment history who are given a General discharge, are typically ineligible for any VA benefits or military retirement pensions unless they are also diagnosed with a service-connected disability. They often experience difficulty obtaining certain civilian employment requiring an honorable discharge (e.g., GAO, 2011).
Military Trends
Note that psychiatric backdoor discharges are not new to the twenty-first century. For example, during WWI, a total of 6196 Army personnel was ADSEP for “character and behavior disorders, including 3,709 diagnosed as ‘constitutional psychopathic states’ (akin to PD), 455 for ‘alcoholism,’ 734 ‘bedwetting,’ 1190 for ‘drug addiction,’ and two for ‘malingering’” (Salmon & Fenton, 1929). In WWII, a total of 163,119 soldiers were ADSEP for unsuitability due to neuropsychiatric reasons, among whom were 2930 for “character and behavior disorders, which includes chronic alcoholism and drug dependence” (Glass & Bernucci, 1966). Service members ADSEP for “psychopathic personality, chronic alcoholism, or sexual perversion including homosexuality, were discharged without honor.” (Bernucci, 1966, p. 484). Prior to 1982, Vietnam War veterans diagnosed with a “pre-existing” mental health condition, such as schizophrenia or other psychotic disorder, whether accurate or not, were often medically discharged or ADSEP without VA treatment benefits. This trend of backdoor discharges was reported to have notably increased during the Korean and Vietnam Wars, but absolute numbers are not reported and thus unavailable (Glass & Jones, 2005).
PD
Although the military’s classification of PD has evolved over time, being called constitutional psychopathy (WWI, WWII), then asocial/psychopathic personalities (WWII), and then PDPD (Korean War to present day), the general policies have not. Today, a PD is defined as:
An enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, leads to clinically significant distress or impairment in social or occupational functioning and is not better explained as a manifestation or consequence of another mental disorder, or the physiological effects of a substance (e.g., drug of abuse) or another medical condition [e.g., head trauma; American Psychiatric Association, 2013, p. 645].
Given its developmental nature, a PD is considered a pre-existing (pre-military) and therefore nonservice-connected condition. From the military’s perspective, a PD diagnosis communicates an inherent difficulty adapting to social and occupational demands in adverse environments, with the potential to become a substantial burden on the command and/or a safety risk to self or others. In other words, in PD, predisposed weakness, not exposure to war stress, is the underlying cause of one’s post-deployment troubles. Therefore, service members with a PD diagnosis are routinely ADSEP for having a pre-existing condition that is incompatible and unsuitable for military service. However, by definition, a PD is not diagnosed in adulthood without substantial evidence of earlier maladjustment and only after excluding other psychiatric or physiological conditions (APA, 2013). A history of psychiatric hospitalization and legal conviction typically renders an individual as ineligible to join the military (e.g., GAO, 1998). Since WWI, the military has psychiatrically screened and rejected volunteers and draftees due to possible PD or other psychiatric risk factors as reflected in Table 2.
Once diagnosed, service members may be given an opportunity to remediate via counseling, with a formal written warning that further performance problems will result in ADSEP (DoD, 2017). However, the vast majority of personnel diagnosed with PD are recommended for ADSEP and those with a history of suicidal ideation or attempts are often subject to “expeditious” ADSEP (DoD, 2017). The senior author (mcr) has observed expeditious ADSEP occurring within a week. Individuals are ADSEP for PD under the category of Convenience to the Government (DoD, 2017), typically with characterization of discharge as General under honorable, which is less than honorable (DoD, 2017).
Military’s Wrongful Use of PD Diagnosis and Backdoor Discharge
Anyway, given the fact that both the military and the VA heard this testimony, which is very, very shocking, that there is a systematic and a policy-driven misdiagnosis of PTSD as PD to get rid of the soldier early, to prevent any expenditures in the future which are calculated in the billions of dollars, I would take that pretty seriously if I were you guys and say something about that (Hon. Bob Filner (2007), Chairman, Committee of Veterans’ Affairs; U.S. House of Representatives).
U.S. Army researchers surveyed psychiatrists deployed to Vietnam who reported that, of all possible mental health diagnoses, PD was the most frequent (27%), followed by drug dependence syndrome (15%), which is another ADSEP-qualifying condition (Camp & Carney, 1987). An estimated 300,000 Vietnam veterans received General ADSEP’s with an unknown, but large number of those subject to diagnostic abuses (e.g., Izzo, 2014), carrying stigma and adverse effects on employment.
Contemporary Trend of PD Discharges
From 2000 through 2015, a total of 99,223 active-duty service members were diagnosed with PD by military healthcare (Armed Forces Health Surveillance Center, 2016). It is unknown how many of the 81,223 service members were war veterans. In 2007, media reports surfaced alleging the Army involuntarily ADSEP over 40%, or 28,000 soldiers, for PD due to post-deployment adjustment problems (Kors, 2007; Zwerdling, 2007). On 25 July 2007, the U.S. House conducted hearings on PD backdoor discharges, prompting the committee Chairman Filner to observe:
My concern is that this country is regressing and again ignoring legitimate claims of PTSD in favor of the time and money saving diagnosis of PD. Providing veterans with the correct medical diagnosis is key for a variety of reasons ranging from receiving proper treatment to eligibility for military and veterans’ benefits. Once a service member is diagnosed with a PD, he or she has a much more difficult time receiving benefits and treatment at the VA (p. 1).
In 2008, the GAO was charged by Congress to review the DoD’s PD discharges amid widespread reports of wrongful backdoor discharges of war veterans. The GAO (2008) reported that out of a sample of 31,000 personnel ADSEP for PD, it found 2900 service members had deployed to OEF/OIF war zones. Subsequently, the Congress has enacted several laws (e.g., National Defense Authorization Act, 2010) and the DOD (2010) has modified its ADSEP policies governing the military services’ handling of PD and misconduct separations in cases involving PTSD and TBI (e.g., GAO, 2010). Consequently, Figs. 2 and 3 reveal a dramatic reduction in military PD discharges since 2007 due to external pressure. However, in 2010, the GAO found the Army, Marine Corps, and Navy remained noncompliant with the DoD’s revised PD discharge regulations, leaving open the possibility for backdoor discharges. In fact, even as recent as 2015, the GAO cited problematic PD and other nonservice-connected psychiatric discharges:
DOD and three of the four military services—Army, Navy, and Marine Corps—cannot identify the number of enlisted service-members separated for non-disability mental conditions because, for most separations, they do not use available codes to specifically designate the reason why service-members were separated.
Because the three military services are using the broad separation code “condition, not a disability” for most separations, the resulting data cannot be used to identify the number of service members separated for non-disability mental conditions. There is no other systematic way to track these separations (GAO, 2010, pp. 9–10).
Number of military personality disorder administrative separations. Note: Data from U.S. Army, Air Force, Marine Corps, Navy, National Guard, and Coast Guard (see Sidibe & Unger, 2016)
Nondisability personality and adjustment disorder separations: U.S. Air Force Only. Source: http://nlgmltf.org/military-law-library/publications/adjustment-disorder-discharge/
In reply, the Army justified its avoidance of specific separation codes needed to monitor possible backdoor discharges, citing concerns over the stigma and well-being of discharged soldiers (GAO, 2010). However, most nonservice-connected discharges are General, under honorable conditions, and it is the absence of honorable discharge that future civilian employers are more prone to discriminate against. A more plausible reason for the military’s approach is what the GAO (2010) asserts: “There is no other systematic way to track these separations” (p. 10). Case in point, Fig. 3 reveals the trend, that as the number of PD ADSEP significantly declined under the weight of immense external scrutiny, the number of other nonservice-connected psychiatric ADSEP (e.g., adjustment disorder) increased.
Specifically, since 2007–2008, the number of PD discharges across all military branches plummeted from an average of 3849 service members per year in the period 2001–2007 to only 907 in 2008–2010. However, during this same period, the number of nonservice-connected psychiatric discharges significantly increased for conditions like adjustment disorder (see Fig. 3). For example, from 2008 to 2010, the Army discharged a total of 6492 service members for adjustment disorder, with the number of deployed soldiers ADSEP for adjustment disorder increasing each year since 2008 (see Fig. 4). Furthermore, by 2010, 37% of the 2033 soldiers ADSEP by the Army for nonservice-connected adjustment disorder had been deployed to war zones (Ader et al., 2012) leaving open accusations of backdoor discharges.
U.S. Army ADSEP for adjustment disorder (Ader et al., 2012)
How Do Backdoor and Bad Paper Discharges Benefit the Military?
There are a number of ways the military benefits from awarding bad paper and backdoor discharges to war veterans versus a medical discharge for conditions like PTSD or honorable ADSEP. They include (a) avoiding increase in time and cost associated with medical boards and medical discharge, (b) avoiding rewarding personnel with a honorable discharge whom the commander does not feel deserves it because of poor performance, (c) justifying resentment toward personnel who are choosing to act-up or seeking mental health rather than persisting as should “real” soldiers, (d) constituting a means to enact long-term retribution to a soldier not liked and/or felt as unworthy of honorable discharge, (e) significant savings in cost and time to process personnel for ADSEP versus courts-martial and/or waiting for future legal violations to build a case, and (f) belief one is “doing a favor” by granting a demoralized service member’s request for expeditious ADSEP.
In regard to potential financial incentives, multiple news stories have reported military medical leaders and mental health clinicians circulating memoranda or verbally confiding of the top-down pressure to avoid million dollars associated with PTSD diagnosis and pensions (e.g., Bernton, 2012e; Carpenter, 2010; de Yoanna & Benjamin, 2009; Kors, 2007; Sidibe & Unger, 2016; Zwerdling, 2015). In fact, during the 2007 Congressional hearing on PD discharges, it was noted:
In addition, there is some indication that higher policy is leading to this or—policy made at higher levels. I have personally talked to a doctor psychiatrist who told me that his commander told him to make the diagnosis of PD rather than PTSD which would lead to further cost and obligations by this Nation to our veterans.
The doctor said, “You have the medical issues that call for a medical board, but the reason I am going to push this Chapter is because it will take care of both the needs of the Army and the needs of you. You will be able to receive all the benefits you would if you were going to go through a medical board, get out of the military, and focus on your treatment to get better. For the military, they can get a deploy-able body to fill your spot” (Hon. Bob Filner, 2007, p. 74; Chairman, Committee on Veterans’ Affairs).
To that end, it has been estimated that the DoD has saved $8 billion in disability compensation and $4.5 billion in medical care costs through its psychiatric backdoor discharges (e.g., Sidibe & Unger, 2016), but this excludes cost-savings from legal-related backdoors (e.g., OTH ADSEP for misconduct). Regardless, the status quo harkens back to German Army psychiatrist Robert Gaupp’s (1911) declaration: “The most important duty of the neurologist and psychiatrist is to protect the Reich from proliferations of mental invalids and war pension recipients” (cited in Lerner, 2003, p. 64).
Setting aside any potential financial incentives, perhaps the biggest payoff for backdoor and bad paper discharges is that it serves to maintain control of fear via intimidation and of its consequences. For instance, a deployed service member within eligibility for military retirement and lifetime pension after 20 years of active service, who is ADSEP with a bad paper discharge, forfeits her/his retirement pension and often VA benefits. In this regard, consider the GAO’s (1998) finding:
The Army and Navy have made it clear that they do not wish to reduce attrition rates by trying to rehabilitate individuals who engage in misconduct. For example, the Navy has recently made its definition of “a pattern of misconduct” less stringent, changing the number of offenses constituting “a pattern” from three or more, to two or more.” Also the Army’s Director of military personnel management has emphasized to its major commands that two of the largest areas for separations, discharges for misconduct and discharges in lieu of courts martial, are “areas that are non-negotiable” (p. 40).
In regard to the DoD’s compliance with legal and discharge policy mandates, the GAO (2017) found that two of four service branches were noncompliant with counseling provision requirement and none of the branches tracked required training and screenings. For example, 40 and 38% of deployed Army and Marine Corps personnel, respectively, given OTH ADSEP were not screened for PTSD or TBI as required! In conclusion, the GAO (2017) reported:
DOD does not routinely monitor the military services’ adherence to policies for screening servicemembers for PTSD and TBI prior to separating them for misconduct, training officers on how to identify symptoms of TBI in the deployed setting, and counseling service-members on eligibility for VA benefits and services. Without monitoring adherence to these policies, the military services cannot provide assurance that servicemembers with PTSD and TBI are receiving adequate consideration of their conditions as well as the services DOD has established for them (p. 27).
In seeking an explanation as to why the military continues to defy its legal obligations, we point to the inherent fragmentation and lack of leadership accountability in the mental health organizational structure (IOM, 2014b; Russell et al., 2016a). The military’s diffusion of responsibility represents yet another approach to avoid learning its war trauma lessons.
Strategy 8: Maintaining Diffusion of Responsibility and Unaccountability
Whether by design or accident, the U.S. military has created and sustains a mental health system that, unlike the case of military medicine and dentistry, is fragmented and unorganized without an accountable chain-of-command or leadership structure (e.g., IOM, 2014a; Russell et al., 2016a, b). Essentially, there are three major organizational components involved in providing mental health services: (a) military medicine, (b) family community counseling centers, and (c) other miscellaneous programs (Russell et al., 2016a). Each entity has its own separate chain of command, personnel, policies, record-keeping, and data-collection procedures, with widely varying levels of collaboration with other mental health entities at the installation or headquarters levels, in what is referred to as “stove piping.” Complicating matters even further is that each mental health-related entity within the four military service branches (Army, Air Force, Marine Corps, and Navy) has different policies and practices. Extensive reviews of the DoD’s organizational and leadership structure pertaining to mental healthcare, along with required changes, are available (e.g., Russell et al., 2016a, b).
Concerns over a problematic organizational structure of military mental healthcare are far from new, in that WWII-era’s Chief Army Neuropsychiatric Consultant asserted: “Certain factors within the Army-its organizations and system-further added to the difficulty for psychiatry. Each of these contributed directly to the production of psychiatric casualties. All of this could be changed so that they would be much less of a menace to mental health” (Menninger, 1948, p. 516). The General’s candid appraisal is collaborated by other senior WWII psychiatrists, who reported: “A frequent comment by frustrated and harassed psychiatrists during World War II was that responsible authorities failed to heed the lessons learned by psychiatry in World War I” (Glass, 1966b, p. 735), thus giving credence to the proposed solution: “Some clinical psychology officers believe that a separate corps within the Medical Department should have been created” (Seidenfeld, 1966, p. 586).
Current Evidence of Maintaining Diffusion and Unaccountable Leadership
Nearly 7 years after the invasion of Afghanistan, the DoD released its year-long self-assessment of mental health services as ordered by Congress. In regard to the military’s mental health organization and leadership structure, the DoD TF-MH (2007) reported:
The services exist in different authority structures and funding streams. The Task Force found various degrees of segregation for these programs and no consistent plan for collaboration in promoting psychological health of service members and their families. The services are stove-piped at the installation and Service levels. The lack of an organized system for installation-level management of psychological health is paralleled by the lack of a DOD wide or Service-level strategic plan for the delivery of services to support psychological health (p. 53).
Seven years after the DoD embarked on implementing its own list of corrective actions to address the self-reported organizational deficiencies (Russell et al., 2016a), the IOM (2014b) conducted an independent assessment of the military’s PTSD programs. According to the IOM (2014b), “Leadership accountability can help ensure that information on PTSD programs and services is collected, and that their success is measures and reported. Effective leadership extends to supporting innovation in new processes and approaches for treatment for PTSD” (p. 5). However, after extensive review of DoD’s management of its PTSD programs, IOM (2014b) concluded:
In DoD and each service branch, unit commanders and leaders at all levels of the chain of command are not consistently held accountable for implementing policies and programs to manage PTSD effectively, including those aimed at reducing stigma and overcoming barriers to accessing care. In each service branch, there is no overarching authority to establish and enforce policies for the entire spectrum of PTSD management activities. A lack of communication among mental health leaders and clinicians in DoD can lead to the use of redundant, expensive, and perhaps ineffective programs and services, while other programs, may be more effective, languish or disappear (p. 6).
The IOM (2014b) went on to state that:
In the DoD, there is no central leader who has sufficient responsibility and authority to ensure the quality and consistency of efforts to manage PTSD in all service branches or at the national level; different PTSD services and programs are the responsibility of different commands and service branches (p. 123).
Furthermore, in each service branch, there is no overarching authority to establish and enforce policies for the entire spectrum of PTSD managements activities (prevention, screening, treatment, and rehabilitation) (p. 218).
In sum, the same leadership organization that failed to adequately plan and meet wartime mental health needs at the beginning of the war (see DoD TF-MH, 2007) had been essentially left unchanged after a decade of war and a major public health crisis.
The question becomes why did such a dislocation in organization continue despite its dysfunctional signs. We will return to this question in the discussion section.
The Bystander Effect
In search of a plausible rationale, we draw upon a 1960 social psychology phenomena known as the bystander effect (Darley & Latané, 1968). Briefly, the bystander effect arises when the presence of others discourages an individual from intervening in an emergency situation. The concept was sensationalized after the infamous 1964 Kitty Genovese murder in New York City, when Genovese was repeatedly and fatally stabbed outside her apartment despite screaming for help, and having multiple bystanders observe the brutal assault, but chose to not assist or even call the police (Darley & Latané, 1968). Darley and Latané (1968) attributed the bystander effect to the perceived diffusion of responsibility (e.g., onlookers are more likely to intervene if there are few or no other witnesses) and social influence (individuals in a group monitor the behavior of those around them to determine how to act). In Genovese’s case, each onlooker concluded from their neighbors’ inaction that their own personal help was not needed. Per Darley and Latané (1968), the degree of responsibility a bystander may experience is dependent on three factors: (1) whether or not they feel the person is deserving of help, (2) the competence of the bystander to help, and (3) the relationship between the bystander and the victim.
Analysis of the Bystander Effect in Military Mental Healthcare
Building on Darley and Latané’s (1968) assertions, we examine the three factors posited as responsible for a bystander effect in relation to the military’s inertia. First, does the military believe that mentally ill or war-stressed personnel are deserving of help? If that were true, there should be ample evidence of the military’s commitment to learn war trauma lessons at the same level as battlefield medicine and war tactics, such as in ensuring ready access to high-quality treatment, and zero tolerance policy for stigma. Nothing we have seen or discussed suggests that upper echelon military leaders as a group feel that emotionally injured service members should be seriously helped while in the military. In regard to military leader competency to help, a Surgeon General would have the authority to make changes only within service branches’ medical departments; therefore, only civilian medical leaders at the DoD level could exercise authority across the different branches. However, even the Assistant Secretary of Defense for Health Affairs (head of military medicine) does not have influence over mental health agencies outside military medicine’s jurisdiction (e.g., community counseling centers, contractors; Russell et al., 2016a). Therefore, the absence of a centralized, integrated, and accountable leadership structure ensures that few military leaders will feel competent to help fix military mental healthcare. Lastly, in terms of the relationship between top military officials and those suffering war stress injury, it seems highly unlikely that senior war planners would have personal relationships with enlisted members and junior officers who do most of the warfighting. In sum, the status quo fulfills all three factors necessary for a bystander effect.
Evidence of the Effectiveness of the Military Bystander Effect
Astute observers of human behavior have long recognized that people often engage in specific behaviors because it serves to either obtain something desirable or avoid something undesirable. That said, what is the evidence of a potential payoff for the military to maintain the conditions for a bystander effect toward mental health? The service Surgeon Generals (SGs) are appointed as leaders for their respective Navy/Marine Corps, Air Force, and Army medical departments and are held accountable for medical failures. For instance, when the Army’s Walter Reed Hospital scandal broke in 2006, depicting horrid treatment conditions for medically wounded soldiers (e.g., Priest & Hull, 2007), a number of military medical leaders, including the Army Surgeon General (SG), were promptly fired. No diffusion of responsibility or bystander effect could save the Army Surgeon General.
In stark contrast, when the DoD TF-MH (2007) published their study revealing a major mental health crisis caused primarily by rampant organizational and leadership failure with an urgent appeal that: “The time for action is now. The human and financial costs of un-addressed problems will rise dramatically over time” (DoD TF-MH, 2007, p. 63), certainly someone should have been held accountable. After all, the service SGs are responsible for provision of mental health services within their respective medical department. However, military medicine’s belated admission of a mental health crisis it actively concealed did not result in customary firings or congressional fact-finding investigations (Russell et al., 2016). Indeed, the Task Force chairs, who were the Army and Navy SGs, were congratulated and not rebuked by Congress (Russell et al., 2016).
Moreover, consider the recent publication of condemnable findings from multiple independent commissions, such as:
Through its review, the committee found that PTSD management in DoD appear to be local, ad hoc, incremental, and crisis-driven with little planning devoted to the development of a long-range, population-based approach for this disorder by either the office of the Assistant Secretary of Defense for Health Affairs (OASD(HA) or any of the service branches (IOM, 2014b, p. 216)
None of these types of concerns have proven sufficient to spur any punitive actions toward military officials or congressional investigations over the military’s repeated failure (Russell et al., 2016a). In any other military issue, similar public condemnations would have actionable consequences, but the status quo persists to avoid pursuing an alternative response to the military’s mental health dilemma. Simply put, how can any military leader be held accountable for mental health problems when the IOM (2014b) findings implicate as at fault the entire system:
Each service branch has established its own prevention programs, trains its own mental health staff, and has its own programs and services for PTSD treatment. The ASD (HA) and Undersecretary of Defense for Personnel and Readiness have not developed a comprehensive plan for mental health generally or PTSD specifically” (p. 216).
Further evidence of the military’s diffusion strategy and its effectiveness in avoiding implementation of war trauma lessons, such as the need to eliminate stigma, is provided by the GAO (2016):
Finally, GAO found that responsibilities for mental health care stigma reduction are dispersed among various organizations within DOD and the services, and some information sharing is hampered. No single entity is coordinating department-wide efforts to reduce stigma. Without a clear definition for “mental healthcare stigma” with goals and measures, along with a coordinating entity to oversee program and policy efforts and data collection and analysis, DOD does not have assurance that its efforts are effective and that resources are most efficiently allocated (p. i).
In sum, the “payoff” for the military to maintain the current organizational and leadership structure is that it works to diffuse responsibility and permit military leaders to avoid issues related to mental health. But, what if the DoD adopted the recommendation of establishing a Behavioral Health Corps (BHC; Russell et al., 2016b), with an accountable chain-of-command led by Flag or General Officers similar to existing Corps (e.g., Medical, Nursing, Dental, Legal, Chaplain, Supply, Civil Engineering, Veterinary) services? A BHC makes practical sense, given the sheer level of problems and exorbitant costs associated with psychiatric casualties and attrition, as well as the degree of negative public attention to the military’s mental health problem. However, from the military’s vantage point, a unified organization with an accountable leadership that treats mental health on equal par of physical health presents quandaries.
Specifically, a unified organization for military mental health would compel the military to divert resources, personnel, and finances toward mental health and away from weapon development and procurement and other valued expenditures. The new accountability from a BHC would mean high-ranking officers could be publicly prosecuted and/or fired for dereliction should the military repeat its neglect of war trauma lessons and inadequately plan, prepare, and deliver needed mental health services. Such a public spectacle would invariably result in dragging the military establishment and its ambivalent or antithetic bias toward mental health into the open. In short, not only would immediate ranking officials be held accountable, but so too would their superiors up the chain. Indeed, the status quo provides ample diffusion of responsibility with remote chance that upper echelon leaders could be held accountable. Removal of the possibility of bystander effect by having a central mental health entity in the military would therefore be avoided by the upper chain. However, it is possible that fully committing to learning war trauma lessons and establishing a BHC with accountable leadership may, in fact, result in significant cost savings and improved military readiness (Russell et al., 2016b).
Potential Benefits of a Behavioral Health Corps
There are a multitude of potential benefits for establishing a BHC in the twenty-first century (e.g., Russell, 2006b). First, establishing a BHC would signal to the military, government, and society that mental health has the same priority, level, or urgency and needs the same resources as caring for physical wounds. Treating mental health with the equal resources and priority as medical health signifies a dramatic shift in priorities and commitment. Such a shift would take into account the lessons of war trauma, reduce stigma, and offer the best chance to end the cycle of preventable wartime behavioral crises. The second benefit would be an immediate reduction in the costs associated with redundancy, attrition, and disability. The IOM (2014a) concluded that “treatment and rehabilitation of servicemembers who are injured or ill can lead to great cost savings for DoD” (p. 107), especially given the fact that “the cost of recruiting and basic training for each servicemember average around $75,000” (p. 107). The IOM (2014a) argued convincingly about the cost benefit to the military for providing PTSD treatment: “if high value PTSD care is provided to those who need it, DoD can see savings in healthcare costs for the service member and in the larger costs of maintaining a fit and ready force” (p. 107). Moreover, standardization of policies and practices, integration of services, and the elimination of wasteful duplication and stove piping will result in considerable cost savings (Russell et al., 2016b).
The third benefit from having a BHC is that it would ensure ready access to high-quality care. Standardization of policies, training, and practices across mental health entities, along with centralized data tracking, program evaluation, and reporting, allows all beneficiaries access to high-quality integrated care regardless of location, as well as permitting licensed mental health professional to practice within the full scope of their clinical expertise. Additionally, the US Army (2006) openly acknowledged that mental healthcare is a central military readiness issue that can directly impact the capacity to fight and win wars. Early identification and treatment of mental health problems with the expectation of RTD can prevent attrition and long-term disability (e.g., DVA/DoD, 2010). This can reduce premature and unnecessary loss of manpower and enhance military readiness. The fourth reason for a BHC is to reduce and attempt to eliminate the stigma and disparity of those requiring behavioral healthcare. The DoD’s adoption of a top-down zero tolerance policy for mental health stigma and disparate treatment between mental and physical health, along with a maximum benefit reconditioning mandate (prior to military separation), would serve to improve overall military readiness and serve as a model for transforming the national mental healthcare system (Russell et al., 2016b).
Strategy 9: Provision of Inadequate, Experimental, or Harmful Treatment
Hysteria is the most epidemic of all diseases and too obvious, special facilities for treatment encourage its development (MacPhail, 1925, p. 278).
This type of post-WWI logic captures a seminal reason for the military’s steadfast avoidance of providing psychiatric treatment, despite acknowledging the necessity for early intervention to prevent chronic problems. That period did offer advice that denied the potential for hysteria epidemics: “First, that it is not only in accordance with the best scientific practice to treat soldiers suffering with war neuroses as early and as effectively as possible but to do so is an important contribution toward the conservation of manpower and military morale” (Salmon, 1929a, p. i). Despite this sage advice, it was not followed. Rather an underlying fear predominated that permitting access to specialized treatment will “encourage” its (hysteria epidemics) development. Or in other words, if you build it, it will be used even if unjustified, and so produce catastrophic evacuation syndromes.
While some war veterans of every era have benefitted from effective mental healthcare within the military, most have received either grossly inadequate or no treatment (e.g., DoD TF-MH, 2007), or possibly even harmful treatment during and after military service. In a nutshell, aside from emergent or stabilizing medical interventions, the military has traditionally been reluctant, if not aversive, toward accepting responsibility for treating traumatized personnel, opting instead to defer that responsibility to either the VA or private sector:
Before the spring of 1944, the official attitude of the Army “toward psychiatric illnesses was a mixture of fatalism and disinterest; treatment was discouraged.” In fact, AR (Army Regulations) 615-360, 26 November 1942, specifically denied definitive treatment for psychiatric patients (Quinn, 1966, p. 688).
The one notable exception to the military’s aversion toward treatment is its heralded frontline psychiatry or COSC programs (e.g., Department of Army, 2009; Russell & Figley, 2017a). Although some inaccurately refer to frontline psychiatry as a “treatment,” the military officially acknowledges the primary purpose of these brief interventions is to preserve the fighting force by avoiding psychiatric evacuations, and thus, it is not psychotherapy. Nevertheless, we summarize the military’s 100-year mental health doctrine.
Evidence of Military Avoidance of Treatment
The most straightforward proof of the military’s deliberate avoidance of providing treatment lies in explicit military policies prohibiting or severely restricting treatment access:
As late as May 1944, AR 615-360 specifically stated: “Individuals permanently unfit for Army service because of neuropsychiatric disturbances will not be retained for definitive treatment, but will be discharged and arrangements will be made for further care by the Veterans Administration if such is indicated” (Brill, 1966, p. 275).
Additionally, there is the military’s own admission of its propensity to avoid treatment:
Whereas timely screening and treatment for injuries and illnesses have always been cornerstones of physical health protection, these same activities have historically been shunned for stress-related problems occurring in operational settings for fear of drawing attention to them and fostering epidemics of stress casualties (Department of Navy and U.S. Marine Corps, 2010, pp. 1–2).
Other ways to illustrate the military’s avoidance of treatment is to give voice to credible observers from a particular era, especially the military’s own post-war lessons learned documentation. It is important to clarify that while some individual service members may receive effective treatment, including evidence-based therapies and other effective interventions, we are most concerned with evidence that such an attitude is generally not widespread, and thus, reflects an organizational avoidance to actually learn a critical war trauma lesson. There is no universally accepted definition as to what constitutes as “adequate” mental health treatment. Determination of appropriateness of certain treatments varies from historical era to era and even within a specific cohort. Rather than focus on specific modalities, we rely upon general impressions about the availability of mental health interventions of that given period by credible witnesses:
WWI
It was obvious at the outset that such patients could not be cared for in the individual American base hospitals scattered throughout France, partly because of the lack in some of them of medical officers, nurses, or enlisted personnel who had had experience in the actual care and treatment of patients suffering from acute mental disorders, but chiefly because of the absence of any special facilities for treatment (Salmon, 1929b, p. 279).
WWII
From the beginning, there was a shortage of trained psychiatrists, neurologists, psychiatric nurses, attendants, aides, social workers, psychologists, occupational therapists, and recreational therapists (Brill, 1966, p. 262).
Facilities for the care and treatment of psychiatric cases were only barely sufficient for the small peacetime Army (Glass, 1966a, pp. 17–18).
Vietnam War
In addition to providing an impetus for accurate diagnosis, the demands for treatment of large numbers of traumatized veterans spurred the development of effective treatments both for reactions that occurred on the battlefield, as well as those that occurred outside the war zone. Particularly following WWI and WWII great gains were made in diagnosing and treating stress reactions. Sad to say, many of these lessons were forgotten and had to be relearned with Vietnam veterans (Kulka, Schlenger, Fairbank, Hough, Jordan, Marmar, Weiss, & Grady, 1990, p. 286).
Military Policies Encouraging Psychiatric Treatment
The WWII cohort took great pains to document its hard-won lessons in regard to treatment provision, but that did not emerge until late in the war after President Roosevelt issued his 1944 executive order to the War Department Secretary (see Diffusion of Responsibility section). The Army’s multidisciplinary reconditioning program was established on 30 August 1944 by TB MED 80 and applied to “any patient who has even a remote chance for salvage for additional military service” (Quinn, 1966, p. 692). Per Quinn (1966), the philosophy of psychiatric reconditioning followed several basic principles: “1. Regard every case as salvageable, 2. Start treatment as early as possible, 3. Avoid the hospitalization of psychoneurotics, 4. Remove situational factors if possible and 5. An individual or group approach as indicated” (p. 693). Below is the WWII cohort’s reconditioning policy (Quinn, 1966, p. 816), as sent in a memorandum by the topic of psychoneuroses (The Assistant Chief of Staff, G-1 on 10 November 1944 to The Commanding General, Army Service Forces).
Treatment
The present policy provides for the treatment of all individuals with psychoneurosis. This is in contrast to previous policy which provided for the disposition of cases without benefit of treatment. In spite of this change in policy, however, the emphasis which can be placed on treatment depends upon the current policy regarding disposition and utilization of individuals with psychoneurosis.
-
a.
Policy
Treatment policy includes the following points:
-
1.
All cases of psychoneurosis will be treated. Those individuals to be discharged, however, will not be retained merely to receive maximum benefit of treatment except in the cases where the psychoneurosis has been incurred in combat.
-
2.
Each case will be regarded as a medical emergency requiring prompt treatment.
-
3.
Cases will be regarded as sick men needing medical treatment rather than disciplinary cases needing punishment or threats.
-
4.
Military discipline will be maintained.
-
5.
Treatment will be by or under the supervision of psychiatrists. Other personnel will be utilized including line officers, other medical officers, clinical psychologists, Red Cross, etc.
-
6.
Treatment facilities will be centralized in order to control policy and procedures and to compensate for the existing shortage of trained personnel.
-
7.
Patients will be segregated from nonpsychiatric cases in most instances.
-
8.
The majority of cases will be kept out of hospitals for treatment.
-
9.
Patients will be given a full-time program including training, education, orientation, physical reconditioning, and occupational therapy.
-
10.
Full use will be made of accepted medical treatment methods including drugs, individual and group psychotherapy, and adjuvant therapy.
-
11.
Every effort will be made to supply an incentive for recovery.
-
b.
Procedures
-
1.
Treatment in combat zones is conducted at battalion aid stations, division clearing stations, designated clearing companies known as “exhaustion centers,” and evacuation hospitals at the Army level.
-
2.
Treatment in base areas is conducted in dispensaries, training center mental hygiene clinics, hospital outpatient departments, station and general hospitals, neuropsychiatric centers, and the reconditioning programs at convalescent centers.
-
1.
-
c.
Results
-
1.
Combat cases: 40 to 60% return to full combat duty, 80 to 90% to duty of some sort.
-
2.
Base area cases: Approximately 50% return to full or limited duty.
Contemporary Evidence of Military Avoidance of Treatment Access
Despite this sage advice and practice for WWII, no military treatment policies were in effect at the start of the Afghanistan and Iraq Wars. In fact, it was not until 2012 that the Department of Army published policy guidance on treatment. Unlike previous war cohorts, this generation of military medical leaders had access to the proliferation of evidence-based therapies (EBT) shown to work. In 2004, the DVA/DoD published its first clinical practice guidelines for PTSD with expert consensus that clinicians be trained in one of four top trauma-focused EBT [exposure therapy, stress inoculation, cognitive therapy, and eye movement desensitization and reprocessing (EMDR)]. However, a military psychologist surveyed 133 uniformed mental health clinicians and found “90% of the providers indicated they had received no training or supervision in clinical practice guidelines for PTSD” (Russell & Silver, 2007; cited in DoD TF-MH, 2007, p. 20). The training survey deficits resulted in a joint DoD/VA PTSD training program, consisting of bringing national trainers to provide at no cost over 260 military therapists supervised clinical training on one of the EBT for PTSD (i.e., EMDR) (Russell, Silver, Rogers, & Darnell, 2007). Analysis of archival chart reviews from nonrandomized completed treatments was analyzed, revealing significant pre-post-PTSD and depression symptom changes after an average of four sessions in a group of 48 service members diagnosed with combat PTSD (Russell et al., 2007). These findings were repeatedly forwarded up to Surgeon Generals from 2004 to 2007 to increase compliance with DoD’s own clinical training and treatment guidance (VA/DoD, 2004), but military leaders resisted (Russell, 2006c).
Subsequently, multiple assessments have been conducted on DoD’s treatment provision, offering clear evidence of avoidance to learning any treatment lessons:
A thorough review of available staffing data and findings from site visits to 38 military installations around the world clearly established that current mental health staff are unable to provide services to active members and their families in a timely manner; do not have sufficient resources to provide newer evidence-based interventions in the manner prescribed (DoD TF-MH, 2007, p. 43).
Screening, assessment, and treatment approaches for brain injuries and psychological health problems are not always implemented between and within DoD and VA in a consistent manner or aligned with the evidence base. The committee has serious concerns about inadequate and untimely clinical follow-up and low rates of delivery of evidence-based treatments, particularly psychotherapies to treat PTSD and depression and approved pharmacotherapies for substance use disorder. Unwarranted variability in clinical practices and deviations from the evidence base are threats to high-quality patient care (IOM, 2013, p. 238).
The majority of SMs (service members) with PTSD do not receive treatment for this condition. The availability of consistent evidence-based assessment and treatment services for PTSD is a high priority for the U.S. Army Medical Department applying evidence-based clinical practice guidelines. In conjunction with the DVA, DOD has developed comprehensive evidence-based CPGs for assessment and treatment of key psychological disorders, including PTSD, depression, substance abuse and psychosis. These guidelines are not consistently implemented across the DOD and the Task Force was unable to find any mechanism that ensures their widespread use. Furthermore, providers who were interested in utilizing evidence-based approaches complained during site visits that they did not have the time to implement them (DoD TF-MH, 2007; p. 33).
After the DoD TF-MH (2007) released its findings, the military instituted a variety of clinical training and treatment programs, including establishing the DoD Centers for Excellence (IOM, 2014a). In addition, the Department of Army (2012) issued its first treatment policy in directive in DoD in 68 years (excerpts are presented in the next section).
Contemporary Military Treatment Policy
10 April 2012
MEMORANDUM FOR COMMANDERS, MEDCON REGIONAL MEDICAL COMMANDS
Subject: Policy Guidance on the Assessment and Treatment of Post-Traumatic Stress Disorder (PTSD)
-
7. Policy:
-
a.
Clinicians should use the 2010 VA/DoD CPG for the Management of Post-Traumatic Stress in the assessment and treatment of patients presenting with symptoms of traumatic stress. The assessment and treatment of PTSD must be individualized based on the clinical judgment of the treating providers.
-
b.
Treatment of PTSD should be in accordance with the 2010 VA/DoD CPG. Primary care and specialty care providers should be particularly aware of the following key treatment considerations, supported by this guideline:
-
(1)
All patients treated for PTSD should be offered an A-level treatment option (strong recommendations, benefits substantially outweigh harm). There is insufficient evidence that A-level trauma-focused psychotherapy is necessarily more effective than A-level pharmacotherapy for PTSD, and both options individually or combined are consistent with the standard of care. However, in practice, patients often have preferences for non-medications options, and may have co-existing concerns like grief, guilt, relationship problems, which lend themselves to psychotherapy approaches.
-
(2)
A-level psychotherapy for PTSD in the VA/DoD CPG is defined as “trauma-focused psychotherapy that includes components of exposure and/or cognitive restricting; or stress inoculation training: provided on an individual basis.” The components of trauma-focused PTSD psychotherapy include: (a) narration (e.g., imaginal exposure), (b) cognitive restructuring, (c) in-vivo exposure, (d) relaxation or stress modulation skills, and (e) psychoeducation.
-
(3)
The components of trauma-focused psychotherapy may be delivered using manualized packages such as Prolonged Exposure Therapy, Cognitive Processing Therapy or Eye Movement Desensitization and Reprocessing, or other strategies. Because of the complexity of PTSD and co-existing conditions, strict fidelity to treatment protocols is often challenging, and clinicians are not required to adhere to a specific treatment manual as long as they document their clinical decision-making. Selection of the approach should be based on clinical considerations, patient preferences, clinician expertise, and other factors.
Current Evidence of Inadequate Military Mental Health Treatment
The military’s genuine learning or commitment toward treatment provision can be assessed by multiple independent national inquiries (e.g., IOM, 2012a, 2014b). In 2016, the most recent study by RAND researchers defined “minimally adequate level of care” for patients entering a new treatment episode as receiving four psychotherapy visits or two evaluation and management (E&M) visits within the initial 8 weeks after being diagnosed, even though most EBT-PTSD requires 10–12 sessions (e.g., DVA/DoD, 2010). Nevertheless, researchers found that out of 14,576 military patients diagnosed with PTSD, only 34% received the low-bar minimum of four sessions, and only 24% of 30,451 military patients diagnosed with depression received the four-session minimum within 8 weeks after being diagnosed. Statistically significant variation was found across treatment and quality standards across service branches. The RAND concluded:
PTSD and depression are frequent diagnoses in active-duty service members. If not appropriately identified and treated, these conditions may cause morbidity that would represent a potentially significant threat to the readiness of the force. Assessment of the current quality of care for PTSD and depression is an important step toward future efforts to improve care. Yet little is known about the degree to which care provided by the MHS (military health system) for these conditions is consistent with guidelines (Hepner, Sloss, Roth, Krull, Paddock, Moen, Timmer, & Pincus, 2016, p. xxiii).
Nearly identical findings were reported from the IOM (2014b) 2 years earlier:
No DoD data on the use of evidence-based psychotherapy and patient outcomes were available because such data are not collected at the national or service branch level (p. 132).
In summary, there is ample evidence the military continues to avoid compliance with treatment provision lessons and its own policy directives.
Why the Military Avoids Treatment
Reasons for the military’s avoidance to take on mental health treatment are many and seem to include in one way or another, either avertly or indirectly, and either in full or in part: (a) staunch belief that war stress injury is primarily caused by personal weakness and predisposition, thus not due to military service; (b) general devaluing of mental health and its treatments; (c) belief that most war stress injury is untreatable; therefore, those who succumb must be discharged; (d) fear that treatment referrals will spark evacuation syndromes; (e) fear that treatment is too costly and will divert funding away from more important military expenditures; (f) cost inefficiency because very few need treatment so they should be discharged; (g) concerns over warehousing large numbers of psychiatrically damaged personnel unfit to deploy; and (h) belief that the military is responsible only for brief interventions while the VA is responsible for longer term treatment.
Exposure to Experimental and/or Harmful Treatments
Warfighters and nonveterans alike are always subject to the medical knowledge and technology of the day. Consequently, therapeutic techniques for war stress injury employed in earlier times (e.g., WWI-era electric shock) may appear unethical using today’s lens. However, it is also true that military populations historically are uniquely susceptible to compulsory and experimental treatments, some of which are likely or proven to be harmful. Young (1995) quoted Salmon (1917), who noted that war provides “medical scientists with thousands of natural experiments of the sort that they would rarely encounter in peacetime or more likely, would ordinarily encounter only in experimentation involving animals” (p. 84). Some of this forced approach to different therapies is captured in the following.
Leed (1981) divided early military psychiatric treatments into two broad categories: (1) disciplinary approaches emphasizing persuasion to give up psychiatric symptoms whereby being on the frontlines is viewed as less aversive and painful than being in a hospital (e.g., electric shock, seclusion, dietary restriction); and (2) analytic or psychological approaches emphasizing ventilation, uncovering, and abreaction of traumatic or emotionally laden experiences (e.g., hypnosis, narcosynthesis, brief psychodynamic therapy).
A third category of treatments can be described as physical or somatic-based, the focus of which is on correcting neurophysiological “imbalances” in the brain (e.g., drug therapy, insulin-coma therapy). Military patients could receive any one or combination of these approaches throughout the course of their treatment. Treatment method availability “reflects to a certain degree, the conception of the nature of war neuroses held by the medical office in charge” (Salmon, 1917, p. 37), which remains true today in that the DoD refuses to establish standardized mental health care services (e.g., Department of Army, 2012; IOM, 2014b) despite recommendations for such uniformed care since WWI: “And thus a uniform standard of excellence and the same general approach to problems of treatment assured in each special base hospital organized in France” (Salmon, 1917, p. 58). Below are some examples of treatments military personnel have received.
Disciplinary Treatments
Electrotherapy was prominent in the military up to the Vietnam War:
Patients are treated naked to create a crisis usually in 2–3 sessions. The current is at first feeble and then gradually increased; the poles are first applied to the affected parts and then, if necessary, to especially sensitive parts of the skin surface (ears, neck, lips, sole of the foot, perineum, scrotum (Roussy & Lhermitte, 1918, p. 168).
Although faradization had been used to treat hysteria in the private sector before WWI, the building frustration of military doctors overwhelmed with psychiatric casualties created the opportunity for some clinicians to feel emboldened to use increasingly harsh, many would say torturous, methods rationalized by a “tough love” mentality aimed to salvage the dignity of shell-shocked soldiers. The most notorious of the electro-shocking breed is represented by Yealland (1918), who described a 4-h treatment of a mute soldier whom he warned could not leave the room until he was fully “cured”:
strapped in a chair for twenty minutes at a time while strong electricity was applied to his neck and throat; lighted cigarettes had been applied to the tip of his tongue and ‘hot plates’ had been placed at the back of his mouth (pp. 7–150).
Hydrotherapy was described as: “A cold douche, either as a shower or an unbroken jet of water to obtain the crisis” (Roussy & Lhermitte, 1918, p. 169). Seclusion and prolonged sedation induced by barbiturates (2–3 days or longer) were also heavily used in WWI hospitals. Narcosis or continuous sleep treatment was extensively employed in some WWII theaters. For instance, Grinker and Spiegel (1945) reported 20 cases of war neuroses treated with continuous narcosis induced by sodium amytal given by mouth and intravenously and supplemented by paraldehyde and sodium phenobarbital. The length of sleep varied from 27 to 110 h; however, only 3 of 20 patients showed improvement (Grinker & Spiegel, 1945). Moreover, the authors noted “Some patients were made worse by the treatment,” and they were characterized as patients being “loath to awaken” as well as having prolonged periods of delirium, with patient reports of “days of nightmare-like horror alternating with periods of relief” (Grinker & Spiegel, 1945, p. 409). Today, the military has fortunately disbanded its use of disciplinary treatments since at least the Vietnam War.
Analytic Treatments
Psychodynamic approaches emphasizing abreaction have been commonplace since WWI, including at the VA. Grinker and Spiegel (1945) describe the prototypical stages of psychodynamic-oriented therapy used throughout WWII, which were quite sensitive to the patient:
-
1.
Establishing of doctor-patient relationship (transference).
-
2.
Support, and gratification of patient’s weakened and regressed ego by means of tenderness and attentive interest.
-
3.
Release and uncovering of isolated, repressed, and suppressed emotions, memories, and conflicts (abreaction).
-
4.
Direction of attention from external rationalizations toward the patient’s own inner feelings. Development of insight into relationships between psychological reactions to combat, the past behavior patterns and their derivations, and the contemporary symptoms.
-
5.
Decrease of severe superego reactions which has produced guilty feelings because of an actual, or a sense of failure, or evoked punishments for repressed hostility.
-
6.
Desensitization from the memories of the anxiety producing situations by repetitive recounting of traumatic experiences, as the therapist helps the dependent ego to discriminate between past danger and present safety, and between the world of reality and inner anxieties.
-
7.
Re-education of the ego to more effective methods of compromising between inner desires and the obstacles of reality. Encouragement of the ego in its attempts to regain mature attitudes and adult activities thereby giving it new confidence and building up of self-esteem.
-
8.
Revival of support and pressure from a strong group, and competent leadership.
-
9.
Testing emotional and intellectual insight and working through the relationship between present and past attitudes.
-
10.
Post hospital follow-up advice, and encouragement (p. 373).
Today, many contemporary talk therapies including trauma-focused evidence-based treatment for PTSD like prolonged exposure, EMDR, and cognitive processing therapy adopt a similar stage or phase approach (e.g., DVA/DoD, 2010). Individual psychotherapy was the norm until WWII.
However, group therapy modalities were adopted by the military because of acute staffing shortages, large treatment demand, and emerging evidence of curative social factors via experimentation at Northfield Military Hospital (e.g., Jones & Wessely, 2005). To expedite uncovering and working through of traumatic memories, military clinicians often relied upon hypnosis as an adjunctive technique to talk therapy, a practice that ran its course until the Vietnam War. Further, although narcosynthesis was widely employed through WWII, it faded away after the Vietnam War because of use of a quicker method to induce hypnotic states or narcosis. This was achieved by interviewing patients after slowly injecting powerful sedatives like sodium pentothal (e.g., Grinker & Spiegel, 1945). The use of hypnosis to treat war stress injury appears to have been abandoned because of its time intensiveness and questionable durability of treatment gains once patients were returned to duty.
Somatic Treatments
Massages, baths, and fever-induced treatment or pyrotherapies like malaria therapy represent a few somatic approaches used in WWI. During WWII and Korean Wars, insulin-coma therapy consisted of administering small doses of insulin to induce hypoglycemia that reportedly improved appetite and weight gain (Grinker & Spiegel, 1945). However, a modified insulin coma therapy was invented by U.S. Army psychiatrist Sargant (1942), who reported rapid improvement of anxiety and depression symptoms in 28 soldiers with war neuroses after inducing prolonged hypoglycemic coma from high doses of insulin despite the risk of permanent coma and death, prompting military observers to openly question medical ethics:
It is difficult to explain why doctors would adopt a risky treatment usually reserved for cases of schizophrenia to encourage weight gain in service men suffering from post-combat disorders. Reflecting the absence of safe and reliable methods, this intervention was driven by a determination to do something (pp. 73–74).
Today, somatic-based therapies are referred by the military as complimentary alternative medical services (CAMS) and include treatments such as yoga, acupuncture, massage (e.g., DVA/DoD, 2010).
Drug Therapy
Experimentation of drugs has been a frequent experience in the military’s treatment of war stress injury. For example, 16 WWII-era soldiers admitted as inpatients were given ergotamine tartrate, hypothetically to block sympathetic overreactivity (e.g., exaggerated startle response) despite prior knowledge that it potentially “damages the vascular endothelium, producing vascular stasis, thrombosis (blood clots), and gangrene” (Grinker & Spiegel, 1945, p. 410). The experimental study found that 13 soldiers developed toxic symptoms, notably pain in the legs and arms, three had phlebitis, and two experienced blood clots, with only two patients exhibiting improvement in tremors. The U.S. Army also experimented with hyoscine hydrobromide, which had been used for treating tremors and extrapyramidal symptoms. It was given to 50 soldiers diagnosed with war neurosis, resulting in “a very high percentage of toxic reactions consisting mainly of vertigo, fatigue, lethargy, and nausea” (Grinker & Spiegel, 1945, p. 411). In addition, during the Korean and Vietnam Wars, military “experimental psychotherapists” injected 723 soldiers with LSD. Most soldiers did not have a prior psychiatric diagnosis, although several did express war stress injury.
Overprescription of Narcotics
During the U.S. Civil War, the unlimited and unmonitored prescription of morphine, heroine, and cocaine to treat physical wounds and medically unexplained pain symptoms (e.g., functional rheumatism) was widespread. This led to unattended consequences of causing drug addiction among thousands of war veterans. There are anecdotal accounts of similar iatrogenic effects in WWI. In the twenty-first century, however, reports of rampant intentional overprescription of opioids within the VA for treating psychological problems, such as PTSD, took place and appeared in violation of medical ethics of “physician do no harm.” For instance, on 10 October 2013, the House Committee on Veterans’ Affairs heard testimony by VA physicians that narcotic prescriptions are “renewed month after month, sometimes up to two years without examination,” explaining that, “the problem is endemic in the VA because quick and cheap is rewarded over good and thorough” (Bahorik, 2013, p. 1).
Another VA physician working in a pain management clinic remarked, “I was ordered by superiors to write large amounts of schedule two narcotics inappropriately,” and the doctor goes onto to testify: “I pointed out 10–20% of opioid users become addicted… we were creating addicts… all of this fell on deaf ears, copious, large amounts of opioids inappropriately prescribed for PTSD” (Gray, 2013, p. 1). The VA physician concluded, “I do not understand how any medical institution in good conscience can perpetuate a therapy that’s harmful to the people they are supposed to serve” (Gray, 2013, p. 1). On a similarly note, overprescription of opiates and “pain killer” medications has been rampant in military populations, raising concerns by conscientious VA doctors of unethical practice(s) of knowingly causing harm by nurturing drug addiction(s) (e.g., Gray, 2013).
Psychosurgery
During WWII, American service members deemed as treatment resistant, or with “obsessional neurosis,” were sometimes recommended for prefrontal leucotomy, with a reported 80% having favorable outcomes (Sargant & Slater, 1944). Moreover, the VA’s first major clinical trial for treating war stress injury involved prefrontal lobotomies of WWII and Korean War veterans, whereby from 1949 to 1959, a total of 1500 veterans received such lobotomies (Baker & Pickren, 2007). In probably the largest clinical trial ever conducted on lobotomies in the world, 300 veterans were compared with 200 controls. Findings revealed no significant differences; in fact, the control group got better without the brain surgery (Baker & Pickren, 2007).
Iatrogenic Effects of the Military’s Frontline (Combat Stress Control) Psychiatry Programs
The explicit mission of the military’s 100-year-old frontline psychiatry doctrine is to ensure that upwards to 95% of deployed service members diagnosed with war stress injury and/or psychiatric disorder are prevented from leaving war zones until they are either grossly incapacitated or pose imminent safety risks to self or others (e.g., Department of Navy & U.S. Marine Corps, 2010). The military’s frontline psychiatry programs are referred to as forward/combat/war psychiatry, combat stress control or, more recently, combat and operational stress control. It originated in WWI as the military’s primary weapon against threats of evacuation syndromes and financial strain from skyrocketing pension costs (e.g., Shepard, 2001). The military’s sustained emphasis on RTD is based on claims that soldiers who receive psychiatric treatment and evacuation from war zones experience significantly worse long-term health and social outcomes, including developing PTSD, compared to those who are RTD (e.g., Russell & Figley, 2017b). Specifically, per the U.S. Army’s textbook on Combat and Operational Behavioral Health, “In today’s combat environment, military leaders can expect to retain and return to duty (RTD) over 95% of service members who experience COSR” (Brusher, 2011, p. 60).
In practice, the stated goal of the U.S. Army’s frontline behavioral health treatment or restoration centers in Afghanistan continues to be “to maximize the return-to-duty (RTD) rate of SMs (service members) who are temporarily impaired or incapacitated by stress related conditions” (Joint-Mental Health Advisory Team-7 (J-MHAT-7), 2011, p. 90). To that end, in 2010, the Army reported 98.7% RTD of 193 war-stressed soldiers after completing a 3–5-day behavioral health treatment program in Afghanistan, including 20% of soldiers diagnosed with an adjustment disorder and 7% diagnosed with PTSD (J-MHAT-7, 2011). The military publicly posits that the health benefits of its RTD policy include lower PTSD and other psychiatric diagnosis, lesser stigma and shame, and increased post-traumatic growth (e.g., Russell & Figley, 2017a). Consequently, “as a result of high RTD, both units and Soldiers benefit. Units benefit from continued force sustainment and Soldiers avoid the stigma linked to evacuation for a behavioral health illness” (Mental Health Advisory Team-I (MHAT-I), 2003, p. B-14). In fact, some military leaders adopt an even more strident moral stance toward frontline psychiatry policy, insisting that “when viewed objectively, inappropriate evacuation may constitute medical malpractice” (Martin & Cline, 1996, p. 164).
However, until 2017, the only review of the efficacy of the military’s century-old programs was conducted by British researchers Jones and Wessely (2003), who raised serious concerns about the legitimacy of the military’s data on RTD and relapse rates. Moreover, the U.S. military has not conducted a single clinical trial comparing the health outcomes between soldiers RTD and those receiving psychiatric evacuations and treatment (Russell & Figley, 2017b). Instead, the DoD relies upon three small longitudinal studies by the Israeli Defense Force from the 1982 Lebanon War, with the two most recent investigations revealing harmful effects of repeated combat stress reactions (see Russell & Figley, 2017c).
Subsequently, Russell and Figley (2017a, b) conducted the first-ever comprehensive review of the military’s frontline mental health policies, examining the evidence whether these policies are beneficial or harmful to veterans and their families (Russell & Figley, 2017a, b, c). Thus, they addressed unanswered clinical, moral, and legal questions. For example, in 2003, the British High Court (equivalent to the U.S. Supreme Court) heard expert testimony from the military on both sides of the issue during an unprecedented class action law suit (McGeorge, Hughes, & Wessely, 2006). The plaintiffs were Falkland Island and Persian Gulf War British soldiers, who were acting against the Ministry of Defense (MoD). The complaint was for failure to provide adequate treatment services, including CSC interventions that could have prevented their chronic PTSD. The MoD asserted, “despite the general acceptance of the principles of forward psychiatry, they have never been shown to be of therapeutic benefit to the individual” (McGeorge et al., 2006, p. 25), and it referred to the absence of scientific data that frontline interventions for acute breakdown do anything more than its intended design as expressed by American Army Medicine’s motto of “conserving the fighting strength” (Jones & Wessely, 2003).
After reviewing existing literature, the British High Court upheld the MoD’s defense ruling: “given this relative absence of reliable evidence as to their therapeutic effect there was a further question mark over whether or not it was even ethical to implement the principles of forward psychiatry at all” (McGeorge et al., 2006, p. 25). This left serious unasked questions regarding the neglected state of military research on frontline interventions despite standardized implementation since 1917 (Russell & Figley, 2017a, b, c).
After reviewing empirical studies on the health effects from cumulative exposure to war stress, previously classified reports on frontline psychiatry, prevalence and treatment of mental health conditions among deployed personnel, risk and protective factors of combat-related PTSD, and prospective deployment research on health outcomes, only one conclusion could legitimately be reached (Russell & Figley, 2017b, c). Specifically, that there is overwhelming evidence that: (1) the military has significantly benefitted by preventing psychiatric attrition, treatment, and evacuations, with average reports of 90–98% RTD and only 3–5% psychiatric evacuations (Russell & Figley, 2017b); (2) repeated exposure to war stress is significantly associated a wide variety of serious, long-term adverse medical, psychiatric, and social outcomes for individual veterans and their families (Russell & Figley, 2017c); and (3) there is clear and convincing evidence that veterans and their families are substantially more likely to be harmed than helped by the military’s century-old frontline policies and procedures (Russell & Figley, 2017c). Moreover, in 2006, the DoD reversed its century-old policy of preventing military personnel from deploying to war zones with known or suspected psychiatric diagnoses like PTSD (Assistant Secretary of Defense for Health Affairs, 2006), while maintaining its adherence to frontline psychiatry principles that actively discourage psychiatric diagnosis and treatment in war zones:
Whereas timely screening and treatment for injuries and illnesses have always been cornerstones of physical health protection, these same activities have historically been shunned for stress-related problems occurring in operational settings for fear of drawing attention to them and fostering epidemics of stress casualties (Department of Navy & U.S. Marine Corps, 2010, pp. 1–2).
In short, the military’s 100-year-old frontline psychiatry doctrine likely contributes to the generational cycle of self-inflicted wartime behavioral health crises. It remains, however, the military’s cornerstone policy for managing its mental health dilemma and thus represents a major avoidance strategy for learning from its war trauma lessons.
Strategy 10: Perpetuating Neglect, Indifference, and Self-Inflicted Crises
The final avoidance strategy the military utilizes to manage its mental health dilemma is sustained indifference and neglect that perpetuates the generational cycle of preventable or self-inflicted crises. From an organizational perspective, indifference and neglect of mental health will often be the natural by-product from adopting one or more of the avoidant strategies discussed earlier. For instance, neglect of mental health services will arise when leaders are focused on weaponizing stigma and/or adopting a punishment approach toward preventing evacuation syndromes. Similarly, maintaining a diffuse and fragmented leadership structure invites bystander effect and neglect. Obviously, attempts to purge the military of predisposed weakness and psychiatry results in neglect of mental health services, as do strategies for avoiding psychiatric diagnosis and treatment. Assuredly, efforts to avoid transparency and delay expenditure of resources are disincentives for investing in mental healthcare. The above represent organizational policies and procedures intended to prevent costly evacuation syndromes, all of which contribute to chronic indifference and neglect of learning war trauma lessons resulting in predictable crises.
However, what explains indifference and neglect at the individual level? Excluding leaders who are simply uninformed and thus, through gross ignorance and/or incompetence, are unintentionally prone to avoid learning from the lessons of war trauma, other factors help explain the perpetuation of military mental health crises, and it is not that military leaders in the twenty-first century have never heard of PTSD or do not have rudimentary knowledge of the history of war stress and popularized afflictions like shell shock. It strains credulity that any contemporary military official, especially those involved in war planning, did not have basic awareness of the reality of mass psychiatric casualties when a force is engaged in war activities.
Personal Barriers to Learning
Therefore, eliminating the minute handful of leaders who genuinely did not know that war would cause psychiatric wounds, what else may account for senior officials who, though keenly conscious of the military psychiatric realities, deliberately chose to neglect those lessons? We posit two distinct and extreme sources for personalized indifference and neglect: (1) some leaders might not care at all about the health and well-being of service members; and (2) some might favor the antipsychiatry movement, a likely much larger group of leaders; they care about their troops but they honestly believe that psychiatry (mental healthcare) is harmful to individuals and thus should be avoided. Before proceeding, we want to clarify that we believe the vast majority of leaders do not represent either of the two extremes, and genuinely do care and value the contributions of mental health, but failed to take action for any of the organizational reasons discussed earlier.
Callous, Impersonal, and Unempathic Personality Style
Frankly, it is easy to suspect that a select few military officials might literally not care. For example, “The government does not love you, you are just a number” (Guiliani, & Donahue, T. (Producer)., 2016, p. 1). History is noted for the stereotypical “bad” general who callously orders battlefield tactics that lead to indiscriminate slaughter instead of safer and more effective military strategy, or the prototypical heartless bureaucrat concerned only with the bottom-line and worker productivity, while being completely indifferent to worker health and well-being. It would be fallacy and great disservice to suggest that many military leaders fit this category, but it is also naïve to suggest none do.
Ardent Believers of the Antipsychiatry Movement
David Cooper (1967) is credited with coining the term “antipsychiatry,” but public skepticism, disbelief, and open antagonism toward the legitimacy of mental health as a profession, mental health providers, and their clientele is centuries old. Contemporary antipsychiatry movement represents a generalized condemnation of the mental health field as a pseudoscience with dubious origins, history of oppressive and harmful practices, proclivity to overpathologize, and a morally corrosive influence on society resulting in a culture of victims. However, a plethora of publications depict societies embroiled in impassioned “trauma-pension wars” since the 1800s, vigorously attacking post-traumatic stress conditions as illegitimate, fraudulent injuries exacerbated by quackery and disability pensions that harm veterans and society alike:
Just as many Great War veterans became chronic patients by the time the gleaning VA hospitals became available to treat them in 1922, so many Vietnam veterans had become irretrievably lost by the time Vet Centers were conjured upon earlier 1979 (Shepard, 2001, p. 395).
More recently, these trauma-pension debates have been greatly magnified with the 1980 DSM adoption of PTSD, spurring volumes on PTSD—debates, with both sides accusing the other of perpetuating unscientific, unethical, and harmful practices, especially those negatively impacting war veterans (McNally & Frueh, 2013). Similar to the general public watching the news, military leaders are bombarded by conflictual authoritative statements about the legitimacy of PTSD and the value of mental healthcare in general (e.g., Nasrallah, 2011). Credible sources undermining the authenticity of PTSD and/or extolling harm caused by psychiatric diagnosis, treatment, and disability compensations of war veterans have been written by military historians (e.g., Shepard, 2001), academics (e.g., Young, 1995), and medical lecturers (e.g., Summerfield, 2001), as well as Harvard and VA researchers (e.g., McNally & Frueh, 2013):
More than any other war in the twentieth century, Vietnam redefined the social role of psychiatry and society’s perception of mental health. Five years after the fall of Saigon, a new psychiatric term was devised, tailored to the needs of veterans (Shepard, 2001, p. 355).
Post-traumatic stress disorder legitimised their “victimhood,” gave them moral exculpation, and guaranteed them a disability pension because the diagnosis could be attested to by a doctor; this was a potent combination (Summerfield, 2001, p. 1).
Shame motivates righteous anger and steps to restore one’s pride. These psychological motives, plus the need to pay the rent and buy the groceries may drive many veterans to seek disability compensation as a way of meeting both kinds of needs in troubled economic times (McNally & Frueh, 2013).
In summary, a sizable, yet uncertain number of military leaders are likely influenced by antidiatribes, with some possibly believing it is their moral duty to prevent the military and its people from being harmed by the pseudoscience and cultural fiction that is mental health.
Discussion
After publishing our initial treatise identifying a generational pattern of largely self-inflicted wartime behavioral health crises (Russell & Figley, 2015a, b), we are frequently asked to explain why these problems are recurring and, more importantly, what can be done to end the tragic cycle. This three-part review marks our initial attempt to address the issue “why?”.
Since WWI, the military has been faced with a mental health dilemma that only grows larger and more costly each successive war (Russell et al., 2017a). The military’s primary mission is to fight and win wars; its secondary mission is to care for its people. At the turn of the twentieth century, every major warring power was faced for the first time with the psychiatric realities of modern technological warfare. Deep-seated fear about evacuation syndromes and financial stress that existentially threatened the military’s capacity to fulfill its primary mission led to the initial resolution of its mental health dilemma by avoiding the lessons of war trauma needed to meet basic wartime mental health needs. When earlier punitive methods to deal with its mental health problem proved inadequate to stem the tide, additional tactics evolved to intimidate, stigmatize, deny, delay, purge, and prevent psychiatric diagnoses, treatment, attrition, and disability compensation. However, the impact of avoiding to learn from war trauma lessons has resulted in progressively more expansive and costly preventable crises that has placed tremendous strain on the military, government, and society. In short, the 10 avoidant strategies we outlined show that the military has done just about everything imaginable to control its mental health problem, with one notable exception—actually learning and/or implementing foundational war trauma lessons.
While fear of evacuation syndromes will not vanish entirely, it is time that the military shifts gear and try something new in how it deals with mental health—a win-win approach. The leaders should stop avoiding lessons that could be learned and, instead, become a world leader in eradicating mental health stigma and disparity. The military self-proclaims that its vision includes “Maintaining the psychological health, enhancing the resilience, and ensuring the recovery of service members and their families are essential to maintaining a ready and fully capable military force” (DoD TF-MH, 2007, p. ES-2). Elevating mental health services to having equal priority as medical services is not inherently incompatible for achieving the military’s primary mission of warfighting. In fact, it will likely prove to enhance the ability of the military to accomplish both of its missions—a victory for the military and a victory for the warfighter.
References
Ader, M., Cuthbert, R., Hoechst, K., Simon, E. H., Strassburger, Z., & Wishnie, M. (2012). Casting troops aside: The United States military’s illegal personality disorder discharge problem. Silver Spring: Vietnam Veterans of America. Retrieved from Veterans Legal Services Clinic, Yale Law School website: https://law.yale.edu/system/files/documents/pdf/Clinics/VLSC_CastingTroopsAside.pdf.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
American Psychological Association. (2002). Ethical principles of psychologists and code of conduct. Washington, DC: Author Retrieved from: www.apa.org/ethics/code/ethics-code-2017.pdf
Armed Forces Health Surveillance Center. (2016). Mental disorders and mental health problems, active component, U.S. armed forces: 2000–2015. Medical Surveillance Monthly Reports (MSMR). Annual MSMR report. Retrieved from: www.afhsc.mil.
Assistant Secretary of Defense for Health Affairs. (2006). Policy guidance on deployment-limiting psychiatric conditions and medications. Memorandum issued by William Winkenwerder, Jr., MD., to Secretary of Army, Secretary of Navy, Secretary of Air Force, and Chairman of the Joint Chiefs of Staff. Washington, DC: Pentagon.
Bahorik, C. J. (2013). Prepared statement of Ms. Bahorik. Between peril and promise: Facing the dangers of VA’s skyrocketing use of prescription painkillers to treat veterans. Hearing before the Subcommittee on Health of the Committee on Veterans’ Affairs. U.S. House of Representatives, 113 th Congress first session on October 10, 2013. Serial No. 113-39. U.S. Government Printing Office: Washington. 66. Retrieved from: https://ia601604.us.archive.org/34/items/gov.gpo.fdsys.CHRG-113hhrg85864/CHRG-113hhrg85864.pdf.
Bailey, P. (1929). Provisions for care of mental and nervous cases. In: P. Bailey, F. E. Williams, & P. O. Komora (Eds.), The Medical Department of the United States Army in the World War: Volume X Neuropsychiatry in the United States (pp. 39–55). Prepared under the direction of Maj. Gen. M. W. Ireland, the Surgeon General. Washington, DC: U. S. Government Printing Office. Retrieved from: http://history.amedd.army.mil/booksdocs/wwi/Neuropsychiatry/default.htm.
Bailey, P., & Haber, R. (1929). Analysis of special neuropsychiatry reports. In P. Bailey, F. E. Williams, & P. O. Komora (Eds.), The Medical Department of the United States Army in the World War: Volume X Neuropsychiatry in the United States (pp. 157–269). Prepared under the direction of Maj. Gen. M. W. Ireland, the Surgeon General. Washington, DC: U. S. Government Printing Office. Retrieved from: http://history.amedd.army.mil/booksdocs/wwi/Neuropsychiatry/default.htm.
Baker, R. R., & Pickren, W. E. (2007). Psychology and the Department of Veterans Affairs: A historical analysis of training, research, practice, and advocacy (1st ed.). Washington, DC: American Psychological Association.
Bernton, H. (2012a). Madigan team reversed 285 PTSD diagnoses, Sen. Murray says. The Seattle Times. Retrieved from: http://old.seattletimes.com/text/2017692555.html.
Bernton, H. (2012b). 40% of PTSD diagnoses at Madigan were reversed. The Seattle Times. Retrieved from: www.seattletimes.com/seattle-news/40-of-ptsd-diagnoses-at-madigan-were-reversed/.
Bernton, H. (2012c). Army opens wide review of PTSD-diagnosis system. The Seattle Times. Retrieved from: www.seattletimes.com/seattle-news/army-opens-wide-review-of-ptsd-diagnosis-system/.
Bernton, H. (2012e). 20,000 misconduct discharges since 2008 saving DoD billions in war-related disability compensation. The Seattle Times. Retrieved from: https://themilitarysuicidereport.wordpress.com/2012/09/09/20000-misconduct-discharges-since-2008-saving-dod-billions-in-war-related-disability-compensation/.
Bernucci, R. J. (1966). Forensic military psychiatry. In: A. J. Glass, & R. J. Bernucci (Eds.), Medical Department United States Army: Neuropsychiatry in World War II: Zone of interior, 1(1) (pp. 475–488). Washington, DC: Office of the Surgeon General, Department of the Army.
Brill, N. Q. (1966). Hospitalization and disposition. In: A. J. Glass, & R. J. Bernucci (Eds.), Medical Department United States Army: Neuropsychiatry in World War II: Zone of interior, 1(1) (pp. 195–253). Washington, DC: Office of the Surgeon General, Department of the Army.
Brusher, E. A. (2011). Combat and operational stress control. In E. C. Ritchie (Ed.), Textbooks of military medicine: Combat and operational behavioral health (pp. 59–74). Falls Church: Office of the Surgeon General, Department of the Army.
Camp, N. M., & Carney, C. M. (1987). U.S. army psychiatry in Vietnam: Preliminary findings of a survey, II. Results and discussion. Bulletin of Menninger Clinic, 51(1), 19–47.
Carpenter, A. (2010). Military misconduct may be sign of PTSD. The Washington Times. Retrieved from: www.washingtontimes.com/news/2010/jan/12/misconduct-may-be-symptom-of-stress-disorder/.
Cooper, D. (1967). Psychiatry and anti-psychiatry. London: Tavistock Publications.
Darley, J. M., & Latané, B. (1968). Bystander intervention in emergencies: Diffusion of responsibility. Journal of Personality and Social Psychology, 8(4p1), 377–383.
de Yoanna, M., & Benjamin, M. (2009). I am under a lot of pressure to not diagnose PTSD. Salon. Retrieved from: www.salon.com/2009/04/08/tape.
Defense Casualty Analysis System. (2017). U.S. Military casualties—Operation Iraqi freedom (OIF) casualty summary by month. Department of Defense Manpower Data Center. Retrieved from: www.dmdc.osd.mil/dcas/pages/summary_data.xhtml.
Department of Defense. (2007). Department of Defense Directive Number 7050.06: Military whistleblower protection of July 23, 2007. Washington, DC: Pentagon. Retrieved from: www.dodig.mil/resources/policyreferences/Hotline/DOD%20Directive%207050.06.pdf.
Department of Defense (2010). The challenge and the promise: strengthening the force, preventing suicide, and saving lives. Department of Defense Task Force on the Prevention of Suicide by Members of the Armed Forces. Falls Church, VA: Defense Health Board. Retrieved from: www.health.mil/dhb/subcommitteestfpsmaf.cfm.
Department of Defense. (2013). Maintenance of psychological health in military operations. DoD Instruction 6490.05 of October 2, 2013. Washington, DC: Defense Logistics Agency.
Department of Defense. (2017). DoD instruction 1332.14, enlisted administrative separations of February 27, 2017. Washington, DC: Department of Defense. Retrieved from: www.dtic.mil/whs/directives/corres/pdf/133214p.pdf.
Department of Defense Task Force on Mental Health. (2007). An achievable vision: Report of the Department of Defense task force on mental health. Falls Church: Defense Health Board.
Department of the Army. (2006). Combat and operational stress control: Field manual 4-02.51 (FM 8-51). Washington, DC: Headquarters. Retrieved from: http://armypubs.army.mil/doctrine/DR_pubs/dr_a/pdf/fm4_02x51.pdf.
Department of the Army. (2009). Combat and operational stress control manual for leaders and soldiers: Field manual 6-22.5 (FM 6-22.5). Washington, DC: Headquarters, Department of the Army.
Department of the Army. (2012). Policy guidance on the assessment and treatment of post-traumatic stress disorder (PTSD). OTSG/MEDCOM Policy Memo 12-035 of 10 April 2012. Houston, TX: Headquarters, United States Army Medical Command, Fort Sam Houston, TX. Retrieved from: http://cdn.govexec.com/media/gbc/docs/pdfs_edit/042312bb1.pdf.
Department of the Navy and U.S. Marine Corps. (2010). Combat and operational stress control. U.S. Navy, NTTP1-15M; U.S. Marine Corps, MCRP 6-11C. Washington, DC: Department of the Navy. Retrieved from: www.marines.mil/Portals/59/Publications/MCRP%206-11C%20%20Combat%20and%20Operational%20Stress%20Control.pdf.
Department of Veterans Affairs & Department of Defense. (2004). VA/DoD clinical practice guideline for the management of post-traumatic stress. Office of Quality and Performance publication 10Q-CPG/PTSD-04. Washington, DC: Veterans Health Administration, Department of Veterans Affairs and Health Affairs, Department of Defense.
Department of Veterans Affairs & Department of Defense. (2010). VA/DoD clinical practice guideline for the management of post-traumatic stress. Office of Quality and Performance publication 10Q-CPG/PTSD-10. Washington, DC: Veterans Health Administration, Department of Veterans Affairs and Health Affairs, Department of Defense.
Executive Order No. 13625, Federal Register, 77(172). (2012). Improving access to mental health services for veterans, service members, and military families. Retrieved from: www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-22062.pdf.
Filner, B. (2007). Opening statement of Chairman Filner. Post-traumatic stress disorder and personality disorders: Challenges for the U.S. Department of Veterans’ Affairs. Hearing before the committee on veterans’ affairs. U.S. House of Representatives, 110 th Congress first session on July 25, 2007. Serial No. 110–37. Government Printing Office: Washington, D.C. Retrieved from: www.gpo.gov/fdsys/pkg/CHRG-110hhrg37475/pdf/CHRG-110hhrg37475.pdf.
Frizell, S. (2014). U.S. army firing more soldiers for misconduct: Number dismissed for crime or misconduct doubled between 2007 and 2013. Time. Retrieved from: http://nation.time.com/2014/02/15/u-s-army-firing-more-soldiers-for-misconduct/.
Gaupp, R. (1911). Uber den Begriff der hysterie. ZgNP, 5, 457–466. Cited in Lerner. (2003). 38.
Ginzberg, E. (1959). The lost divisions. (The ineffective soldier: Lessons for management and the nation). New York: Columbia University Press.
Glass, A. J. (1966a). Army psychiatry before World War II. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 3–23). Washington, DC: Office of the Surgeon General, Department of the Army.
Glass, A. J. (1966b). Lessons learned. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army: Neuropsychiatry in World War II volume I: Zone of interior (pp. 735–759). Washington, DC: Office of the Surgeon General, Department of the Army.
Glass, A. J., & Bernucci, R. J. (1966). Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior. Washington, DC: Office of the Surgeon General, Department of the Army.
Glass, A. J., & Jones, F. D. (2005). Psychiatry in the U.S. Army: Lessons for community psychiatry. Bethesda: Uniformed Services University of the Health Sciences.
Government Accountability Office. (1998). Military attrition: Better data, coupled with policy changes, could help the services reduce early separations (NSIAD-98-213). Washington, DC: Author.
Government Accountability Office. (2008). Defense health care: Additional efforts needed to ensure compliance with personality disorder separation requirements (GAO-09-31). Washington, DC: Author.
Government Accountability Office. (2010). Defense health care: Status of efforts to direct lack of compliance with personality disorder separation requirements (GAO-10-1013T). Washington, DC: Author.
Government Accountability Office. (2011). VA mental health number of veterans receiving care, barriers faced, and efforts to increase access (GAO-12-12). Washington, DC: General Accounting Office.
Government Accountability Office. (2015). Defense health aare: Better tracking and oversight needed of servicemember separations for non-disability mental conditions. (GAO-15-266). Washington, DC: Author. Retrieved from: http://www.gao.gov/products/GAO-15-266.s.
Government Accountability Office. (2016). Human capital: Additional actions needed to enhance DoD’s efforts to address mental health care stigma (GAO-16-404). Washington, DC: Author.
Government Accountability Office. (2017). Defense health care: Actions needed to ensure post-traumatic stress disorder and traumatic brain injury are considered in misconduct separations (GAO-17-260). Washington, DC: Author.
Gray, P. J. (2013). Prepared statement of Ms. Gray. Between peril and promise: Facing the dangers of VA’s skyrocketing use of prescription painkillers to treat veterans. Hearing before the Subcommittee on Health of the Committee on Veterans’ Affairs. U.S. House of Representatives, 113 th Congress first session on October 10, 2013. Serial No. 113-39. U.S. Government Printing Office: Washington, DC. 63. Retrieved from: https://ia601604.us.archive.org/34/items/gov.gpo.fdsys.CHRG-113hhrg85864/CHRG-113hhrg85864.pdf.
Grinker, R. R., & Spiegel, J. P. (1943). War neuroses in North Africa: the Tunisian campaign. Restricted Report prepared for The Air Surgeon, Army Air Forces. New York: JosiahMacy, Jr. Foundation.
Grinker, R. R., & Spiegel, J. P. (1945). Men under stress. Philadelphia: Blakiston.
Guiliani, R., & Donahue, T. (2016). Thank you for your service [Documentary film]. Creative Chaos: U.S.A.
Heaton, L. D. (1966). Forward. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 13–14). Washington, DC: Office of the Surgeon General, Department of the Army.
Hepner, K. A., Sloss, E. M., Roth, C. P., Krull, H., Paddock, S. M., Moen, S., Timmer, M. J., & Pincus, H. A. (2016). Quality of care for PTSD and depression in the military health system: Phase I report. RAND Health Quarterly, 6(1), 14.
Hoge, C. W., Toboni, H. E., Messer, S. C., Bell, N., Amoroso, P., & Orman, D. T. (2005). The occupational burden of mental disorders in the U.S. military: Psychiatric hospitalizations, involuntary separations, and disability. American Journal of Psychiatry, 162(3), 585–591.
Institute of Medicine. (2012a). Substance use disorders in the U. S. armed forces. Washington, DC: The National Academies Press.
Institute of Medicine. (2013). Returning home from Iraq and Afghanistan: Assessment of readjustment needs of veterans, service members, and their families. Washington, DC: The National Academies Press.
Institute of Medicine. (2014a). Preventing psychological disorders in service members and their families: An assessment of programs. Washington, DC: The National Academies Press.
Institute of Medicine. (2014b). Treatment for posttraumatic stress disorder in military and veteran populations: Final assessment. Washington, DC: The National Academies Press.
Issa, D. (2007). Statement by Chairman Daniel Issa (R) questioning Michael E. Kilpatrick, MD Deputy Director, Force Health Protection and Readiness Programs, Department of Defense. In U.S. Congress House of Representatives (2007). Invisible casualties: The incidence and treatment of mental health problems by the U.S. military (pp. 63–79). Hearing before the U.S. Congress House of Representatives Committee on Oversight and Government Reform, First Session, May 24, 2007, Serial No. 110-111. Washington, DC: U.S. Government Printing Office.
Izzo, R. (2014). In need of correction: How the army board for correction of military records is failing veterans with PTSD. The Yale Law Journal, 123(5), 1118–1625 Retrieved from: www.yalelawjournal.org/comment/in-need-of-correction-how-the-army-board-for-correction-of-military-records-is-failing-veterans-with-ptsd
Joint Mental Health Advisory Team 7 (J-MHAT-7). (2011). Operation enduring freedom 2010, chartered by the Office of the Surgeon General United States Army Medical Command. Retrieved from: http://WIN.W.armymedicine.army.mil.
Jones, F. D. (1995). Traditional warfare combat stress casualties. In R. Zatchuk & R. F. Bellamy (Eds.), Textbook of military medicine: War psychiatry (pp. 35–62). Washington, DC: Office of the Surgeon General, U. S. Army, Borden Institute.
Jones, E., & Wessely, S. (2003). Forward psychiatry in the military: Its origin and effectiveness. Journal of Traumatic Stress, 16(4), 411–419.
Jones, E., & Wessely, S. (2005). Shell shock to PTSD: Military psychiatry from 1900 to the Gulf War. Hove: Psychology Press.
Karpinos, B. D., & Glass, A. J. (1966). Disqualifications and discharges for neuropsychiatric reasons, World War I and World War II. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 13–14). Washington, DC: Office of the Surgeon General, Department of the Army.
Kilpatrick, M. E. (2007). Statement by Michael E. Kilpatrick, MD Deputy Director, Force Health Protection and Readiness Programs, Department of Defense. In U.S. Congress House of Representatives (2007). Invisible casualties: The incidence and treatment of mental health problems by the U.S. military. Hearing before the U.S. Congress House of Representatives Committee on Oversight and Government Reform, First Session, May 24, 2007, Serial No. 110-111. Washington, DC: U.S. Government Printing Office. 63–79.
Kors, J. (2007). How specialist Town lost his benefits: Wounded soldiers returning from Iraq are increasingly being wrongly diagnosed by the military, which prevents them from collecting benefits. The Nation. Retrieved from: www.thenation.com/article/how-specialist-town-lost-his-benefits/.
Kors, J. (2010). Disposable soldiers: How the pentagon is cheating wounded vets. The Nation. Retrieved from: www.thenation.com/article/disposable-soldiers.
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R., Weiss, D. S., & Grady, D. A. (1990). Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel.
Leed, E. J. (1981). No man’s land: Combat and identity in World War I. Cambridge: Cambridge University Press.
Lerner, P. (2003). Hysterical men: War, psychiatry, and the politics of trauma in Germany, 1890–1930. London: Cornell University Press.
Macphail, A. (1925). Official history of the Canadian Forces in the Great War, 1914–1919, The Medical Services. Ottawa: FA ACLAND.
Martin, J. A., & Cline, W. R. (1996). Mental health lessons from the Persian Gulf War. In J. A. Martin, L. R. Sparacino, & G. Belenky (Eds.), The Gulf War and mental health: A comprehensive guide (pp. 161–178). Westport: Praeger.
McGeorge, T., Hughes, J. H., & Wessely, S. (2006). The MoD PTSD decision: A psychiatric perspective. Occupational Health Review, 122, 21–28.
McNally, R. J., & Frueh, C. B. (2013). Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates? Journal of Anxiety Disorders, 27(5), 520–526.
Menninger, W. C. (1948). Reactions to combat. Psychiatry in a troubled world. New York: MacMillan.
Menninger, W. C. (1966). Public relations. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 129–151). Washington, DC: Office of the Surgeon General, Department of the Army.
Mental Health Advisory Team-I. (2003). MHAT operation Iraqi freedom. Washington, DC: U.S. Army Surgeon General.
Murphy, B. (2011). Critics: Fort Carson policy targeted troubled, wounded soldiers. Stars and Stripes. Retrieved from: www.stripes.com/critics-fort-carson-policy-targeted-troubled-wounded-soldiers-1.160871.
Nasrallah, H. A. (2011). The antipsychiatry movement: Who and why. Current Psychiatry, 10(12), 4–53.
National Defense Authorization Act for Fiscal Year. (2010). Pub. L. No. 111-84, § 512, 123 Stat. 2190, 2280-82 (2009) (codified, as amended, at 10 U.S.C. § 1177).
Neel, S. (1991). Vietnam studies: Medical support of the U. S. Army in Vietnam 1965–1970. Washington, DC: Department of the Army.
Phillips, D. (2013, May 19). Other than honorable: Disposable surge in discharges includes wounded soldiers. The Gazette. Retrieved from: http://cdn.csgazette.biz/soldiers/day1.html.
Priest, D., & Hull, A. (2007). System ill equipped for PTSD Troops returning with psychological wounds confront bureaucracy, stigma. The Washington Post. Retrieved from http://www.vakkur.com/psy/ptsd_art_wp_061807.htm.
Quinn, E. F. (1966). Reconditioning of psychiatric patients. In R. S. Anderson, A. J. Glass, & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 687–699). Washington, DC: Office of the Surgeon General, Department of the Army.
Ramchand, R., Acosta, J., Burns, R. M., Jaycox, L. H., & Pernin, C. G. (2011). The war within: Preventing suicide in the U.S. military (W74V8H-06-C-0002). Prepared for the Office of the Secretary of Defense Center for Military Health Policy Research. Santa Monica: RAND.
Roussy, G., & Lhermitte, J. (1918). The psychoneuroses of war. In A. Keough (Ed.), Military medical manuals. London: University of London Press.
Russell, M. (2006a). Mental health crisis in the Department of Defense: DoD Inspector General Hotline Investigation #98829 submitted by Commander Mark Russell, USN on 05JAN2006. Available upon request via Freedom of Information Act (FOIA) at Department of Defense; Office of Freedom of Information, 1155 Defense Pentagon; Washington, DC 20301-1155.
Russell, M. (2006b). The future of mental health care in the Department of Defense. Invited testimony before the Congressionally-mandated Department of Defense Task Force on Mental Health, on 19–20 October 2006. San Diego. Transcript available on Defense Health Board: www.ha.osd.mil/DHB/mhtf/meeting/2006oct.cfm.
Russell, M. (2006c). Treating combat-related stress disorders: A multiple case study utilizing eye movement desensitization and reprocessing (EMDR) with battlefield casualties from the Iraqi War. Military Psychology, 18(1), 1–18.
Russell, M. C. (2007). Reprisal complaint #104011 ICO Department of Defense (DoD) Inspector general complaint #98829 “Mental health crisis in DoD” of 5 January 2006. Official grievance filed with the DoD Inspector’s General Office on 28 May 2007, Title 10, United States Code, Section 1034, Military Whistleblower Protection Act [Available upon request via Freedom of Information Act (FOIA) at Department of Defense; Office of Freedom of Information, 1155 Defense Pentagon; Washington, DC 20301-1155].
Russell, M. C., & Figley, C. R. (2015a). Investigating recurrent generational wartime behavioral health crises: Part one of a preliminary analysis. Psychological Injury and Law, 8(1), 106–131.
Russell, M. C., & Figley, C. R. (2015b). Generational wartime behavioral health crises: Part two of a preliminary analysis. Psychological Injury and Law, 8(1), 132–152.
Russell, M. C., & Figley, C. R. (2017a). Do the military’s frontline psychiatry/combat and operational stress control doctrine help or harm veterans?—Part one: Framing the issue. Psychological Injury and Law, 10(1), 1–23.
Russell, M. C., & Figley, C. R. (2017b). Do the military’s frontline psychiatry/combat operational stress control programs benefit veterans? Part two: Systematic review of the evidence. Psychological Injury and Law, 10(1), 24–71.
Russell, M. C., & Figley, C. R. (2017c). Is the military’s century-old frontline psychiatry policy harmful to veterans and their families? Part three of a systematic review. Psychological Injury and Law, 10(1), 72–95.
Russell, M., & Silver, S. M. (2007). Training needs for the treatment of combat-related post-traumatic stress disorder: A survey of Department of Defense clinicians. Traumatology, 13(3), 4–10.
Russell, M., Silver, S., Rogers, S., & Darnell, J. (2007). Responding to an identified need: A joint DoD-DVA training program for clinicians treating trauma survivors. International Journal of Stress Management, 14(1), 61–71.
Russell, M. C., Figley, C. R., & Robertson, K. R. (2015). Investigating the psychiatric lessons of war and pattern of preventable wartime behavioral health crises. Journal of Psychology and Behavioral Science, 3(1), 1–16.
Russell, M. C., Zinn, B., & Figley, C. R. (2016). Exploring options including class action to transform military mental healthcare and ends the generational cycle of preventable wartime behavioral health crises. Psychological Injury and Law, 9(2), 166–197.
Russell, M. C., Butkus, S., & Figley, C. R. (2016a). Contribution of military organization and leadership factors in perpetuating generational cycle of preventable wartime mental health crises: Part one. Psychological Injury and Law, 9(1), 55–72.
Russell, M. C., Butkus, S., & Figley, C. R. (2016b). Ending the generational cycle of preventable wartime mental health crises: Part two: Establishing a behavioral health corps and other constructive solutions. Psychological Injury and Law, 9(1), 73–86.
Russell, M. C., Schaubel, S. R., & Figley, C. R. (2017a). The darker side of military mental healthcare—Part one: Understanding the military’s mental health dilemma. Manuscript submitted for publication.
Russell, M. C., Schaubel, S. R., & Figley, C. R. (2017b). The darker side of military mental healthcare—Part two: Five harmful strategies to manage its mental health dilemma. Manuscript submitted for publication.
Salmon, T. W. (1917). Recommendations for the treatment of mental and nervous diseases in the United States Army. New York: National Committee for Mental Hygiene.
Salmon, T. W. (1929a). Introduction. In: T. W. Salmon & N. Fenton (Eds.), The Medical Department of the United States Army in the World War: Volume X Neuropsychiatry in the American expeditionary forces (pp. i). Prepared under the direction of Maj. Gen. M. W. Ireland, the Surgeon General. Washington, DC: U. S. Government Printing Office. Retrieved from: http://history.amedd.army.mil/booksdocs/wwi/Neuropsychiatry/default.htm.
Salmon, T. W. (1929b). General view of neuropsychiatric activities. In: T. W. Salmon & N. Fenton (Eds.), The Medical Department of the United States Army in the World War: Volume X Neuropsychiatry in the American expeditionary forces (pp. 273–302). Prepared under the direction of Maj. Gen. M. W. Ireland, the Surgeon General. Washington, DC: U. S. Government Printing Office. Retrieved from: http://history.amedd.army.mil/booksdocs/wwi/Neuropsychiatry/default.htm.
Salmon, T. W., & Fenton, N. (1929). Neuropsychiatry in the American expeditionary forces. In P. Bailey, F. E. Williams, P. A. Komora, T. W. Salmon, & N. Fenton (Eds.), Neuropsychiatry: The Medical Department of the United States Army in the World War (pp. 271–474). Washington, DC: Office of The Surgeon General, US Army.
Sargant, W. (1942). Physical treatment of acute war neurosis: Some clinical observations. British Medical Journal, 2(4271), 574–576.
Sargant, W., & Slater, E. (1944). An introduction to physical methods of treatment in psychiatry. London: E. & S. Livingstone.
Secretary of the Army. (2016). Memorandum: Special review and assessment of soldiers with mental health conditions separated from active duty for misconduct of 14 April 2016. Washington, DC: Department of Army, Headquarters. Retrieved from: file:///C:/Users/desensei01/Downloads/ArmyMissedTreatmentReport%20(1).pdf.
Seidenfeld, M. A. (1966). Clinical psychology. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. Neuropsychiatry in World War II volume I: Zone of interior (pp. 567–603). Washington, DC: Office of the Surgeon General, Department of the Army.
Shane, L. (2006). Boxer: DOD slow to implement new mental health task force. Stars and Stripes. Retrieved from: https://www.stripes.com/news/boxer-dod-slow-to-implement-new-mental-health-task-force-1.48543.
Shepard, B. (2001). A war of nerves: Soldiers and psychiatrists in the twentieth century. Cambridge: Harvard University Press.
Sidibe, S., & Unger, F. (2016). Unfinished business: Correcting “bad paper” for veterans with PTSD. Retrieved from Veterans Legal Services Clinic, Yale Law School website: https://law.yale.edu/system/files/documents/pdf/unfinishedbusiness.pdf
Summerfield, D. (2001). The invention of post-traumatic stress disorder and the social usefulness of a psychiatric category. British Medical Journal, 322(7278), 95–98.
Sutton, L. (2016). In T. Donahue (producer): Thank you for your service [Documentary film]. New York: Creative Chaos.
U.S. Army. (1943). Circular letter no. 17. Neuropsychiatric treatment in the combat zone. NATOUSA: Office of Surgeon, Headquarters.
U.S. ArmyMilitary History Institute. (1944). Combat Lessons Number 5: Rank and file in combat-What they’re doing how they do it. EO-10501 Restricted Report. Classified “Unrestricted” on 5 August 1986. Washington DC: Combat Analysis Section, Operations Division, War Department.
U.S. Army. (2006). Final public affairs guidance: OEF/OIF communications plan mental health. Washington, DC: Army Medical Department.
U.S. Navy. (2007). Mental health public affairs guidance. Washington, DC: U.S. Navy Medical Department, Navy Medicine West, Bureau of Medicine and Surgery.
U.S. War Department. (1944). War department technical bulletin (TBMED)-80 convalescent treatment program for neuropsychiatric patients. Published on 30 August 1944 by Surgeon General’s Office, Washington, DC.
Waters. M., & Shay, J. (1994). Heal the ‘bad paper’ veterans. The New York Times. Retrieved from: www.nytimes.com/1994/07/30/opinion/heal-the-bad-paper-veterans.html.
Wilk, J. E., Herrell, R. K., Carr, A. L., West, J. C., Wise, J., & Hoge, C. W. (2016). Diagnosis of PTSD by army behavioral health clinicians: Are diagnoses recorded in electronic health records? Psychiatric Services, 67(8), 878–882.
Wounded Warriors Act. (2009). Retrieved from: www.congress.gov/bill/110th-congress/senate-bill/1606.
Yealland, L. R. (1918). Hysterical disorders of warfare. London: Macmillan.
Young, A. (1995). The harmony of illusions: Inventing post-traumatic stress disorder. Princeton: Princeton University Press.
Zoroya, G. (2007a). Navy psychologist: Navy faces crisis. USA Today. Retrieved from: http://usatoday30.usatoday.com/news/health/2007-01-16-ptsd-navy_x.htm.
Zoroya, G. (2007b). Officer accuses military of trying to silence him. USA Today. Retrieved from: http://usatoday30.usatoday.com/news/washington/2007-06-21-officer-accusation_N.htm.
Zwerdling, D. (2007). Army dismissals for mental health, misconduct rise. NPR. Retrieved from: www.npr.org/templates/story/story.php?storyId=16330374.
Zwerdling, D. (2015). Missed treatment: Soldiers with mental health issues dismissed for ‘misconduct’. NPR. Retrieved from: www.npr.org/2015/10/28/451146230/missed-treatment-soldiers-with-mental-health-issues-dismissed-for-misconduct.
Zwerdling, D. (2016). Senators, military specialists say army report on dismissed soldiers is troubling. NPR. Retrieved from: www.npr.org/2016/12/01/498557687/army-contests-npr-investigation-of-dismissed-soldiers-in-misleading-report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Russell, M.C., Schaubel, S.R. & Figley, C.R. The Darker Side of American Military Mental Healthcare—Part Three: Five More Harmful Strategies to Manage Its Mental Health Dilemma. Psychol. Inj. and Law 11, 69–104 (2018). https://doi.org/10.1007/s12207-018-9312-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12207-018-9312-3