Abstract
This is the first of a three-part systematic review of the potential benefits and harmful effects of the military’s century-old doctrine of frontline psychiatry or combat and operational stress control (COSC). Since the Second World War, psychiatric casualties have outnumbered the combined total of American service members both wounded and killed-in-action. The original, explicit purpose of frontline psychiatry programs established during the First World War was to prevent mass evacuation and attrition of military personnel experiencing acute war stress injuries by emphasizing brief, nonpsychiatric interventions resulting in return to duty (RTD). Although frontline psychiatry continues to evolve, these bedrock principles of RTD and avoiding psychiatric evacuation remain unchanged. Today, the US military explicitly predicts that over 95% of war stress casualties will be RTD with evacuation limited to those deemed either grossly impaired and/or clear safety risks to self or others. The military justifies its mental health policy by claiming that studies have demonstrated its health benefits to individual service members and their families, as well as findings that medical evacuation and subsequent psychiatric treatment are harmful. However, the only systematic review of the effectiveness of frontline psychiatry was published in 2003, warranting critical examination of the military’s claims. Specifically, the actual evidence for or against the military’s primary mental health policy has never been fully examined, so that any conclusions are tentative. The sheer complexity and national security implications underlying the military’s unchallenged 100-year doctrine required a three-part review. In this study, we frame the debate on the military’s frontline psychiatry/COSC by examining its historical origins, ethical-legal controversies, and contemporary program descriptions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The US military’s frontline psychiatry programs were formally established during WWI (WWI: 1914–1918) to eliminate epidemics of mass medical evacuations for psychiatric disability, or so-called evacuation syndromes, that threatened the capacity of armies from every European power to sustain the war effort (e.g., Jones, 1995a). Historically, this diverse set of frontline mental health policies and programs have collectively been referred to as forward, combat, preventative, and war psychiatry (Jones & Wessely, 2003), neuropsychiatric reconditioning (U.S. War Department, 1944), combat stress control (CSC; Department of the Army, 1994), operational stress control (Department of Navy, 2015), and the currently approved designator combat and operational stress control (COSC) to account for stress exposure in both combat and noncombat or operational environments [e.g., disaster relief, peace-keeping; Department of Defense (2013)].
Although technically incorrect, we use the umbrella term frontline psychiatry to convey mental health policies and interventions specifically related to war zones. Modern frontline psychiatry/COSC programs involve a variety of specialties and services well beyond psychiatry, such as clinical psychology, social work, occupational therapy, psychiatric nursing, pastoral care, primary care physicians, and enlisted peer mentors. Within war zones, frontline psychiatry consists of a comprehensive set of policies, principles, and programs implemented along a continuum of prevention, respite, and restorative interventions for military personnel experiencing acute combat and operational stress reactions (COSRs; Department of the Army, 2009). These frontline interventions emphasize immediate safety, food, rest, support, normalization, reassurance, persuasion, and possible psychotropic medication, along with unequivocal expectation of returning military members to their units within days or weeks of “breakdown” (e.g., Department of the Army, 2009). Despite its professed good intentions, an unintended consequence of the military’s frontline psychiatry policy can be summarized as one that involves repeatedly returning war stress casualties back to the frontlines and delay medical/psychiatric evacuations and treatment until war fighters are either too seriously disabled and functionally impaired, and/or present a clear and immediate danger to self or others (e.g., Department of the Army, 2006). We provide later a more detailed overview of frontline psychiatry.
Frontline Psychiatry and the UK Legal System
A class action was adjudicated by the British High Court of England and Wales in 2003, wherein 2000 British combat veterans claimed negligence by the Ministry of Defense (MoD)—akin to the US DoD—for failure to utilize proper measures in preventing, detecting, and treating predictable adverse effects of war, including posttraumatic stress disorder (PTSD; McGeorge, Hughes, & Wessely, 2006). Specifically, one of the eight charges of negligence levied against the MoD was the British military’s breach of its duty to care by failing to provide frontline psychiatric interventions for soldiers experiencing acute stress reactions who subsequently developed PTSD (Russell, Zinn, & Figley, 2016). During the adjudication of Multiple Claimants v. MoD, the High Court held the MoD’s arguments from its panel of eight international experts on military psychiatry and trauma as invalid, and asserted—“despite the general acceptance of the principles of forward psychiatry they have never been shown to be of therapeutic benefit to the individual” (McGeorge et al., 2006, p. 25). The decision referenced a lack of scientific support that the military’s frontline psychiatry programs are effective and do anything more than conserving the fighting strength. Furthermore, the British High Court concluded that, “Given this relative absence of reliable evidence as to their therapeutic effect there was a further question mark over whether or not it was even ethical to implement the principles of forward psychiatry at all” (McGeorge et al., 2006, p. 25). In other words, after systematic review of the available literature and expert testimony, the High Court ruling implies the MoD may have acted unethically toward deployed soldiers by failing to implement frontline psychiatry. The future potential for similar class action against the DoD has recently been explored, which will undoubtedly call into question the US military’s mental health policies (Russell et al., 2016).
Why Investigate the US Military’s Frontline Mental Health Policies?
Per the US military, research on frontline psychiatry/COSC has demonstrated its effectiveness in reducing rates of psychiatric disability from conditions like PTSD and in broadly improving postdeployment outcomes for service members and their families, including enhancement of posttraumatic growth (e.g., Department of Army, 2006, 2009). Despite the seemingly positive effect of the military’s frontline psychiatry doctrine, only a single review has been conducted on the matter, and it found a substantially higher level of psychiatric relapse in the military after application of frontline psychiatry than previously reported (Jones & Wessely, 2003). In this regard, consider some of the statistics involved—to what extent, if any, has the military’s frontline mental health policies helped the 936,283 service personnel diagnosed with psychiatric injury during Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF) and Operation New Dawn [OND; [Congressional Research Services (CRS), 2013], or the 685,540 OIF/OEF/OND veterans treated for psychiatric conditions by the Department of Veterans’ Affairs (DVA, 2015), as well as the more than 5383 families of OIF/OEF/OND service members who committed suicide (e.g., Russell, Butkus, & Figley, 2016a)?
We do not have the basic data required on military members treated by frontline psychiatry in the US military, for example, in terms of outcome. We need data such as this to answer basic questions, such as does frontline psychiatry genuinely benefit service members and their families when examined systematically. This type of investigation seems essential considering the doubt cast on frontline psychiatry in the UK military.
Purpose of the Research
The inherent complexity of investigating a previously neglected topic with major national defense and public health implications requires a three-part review. In this first article in the series, we frame the debate in terms of the reported benefits and detriments from the military’s frontline psychiatry doctrine, including the historical context underlying the military’s continuation of its century-old policy. We also provide a brief, contemporary description of frontline psychiatry/COSC, including a promising alternative conceptual paradigm of war stress injuries recently put forth by the Department of Navy and U.S. Marine Corps (2010). The second article in the series provides a systematic examination into the validity of the military’s claims that its frontline psychiatry doctrine is beneficial to the military mission, as well as the health and well-being of military personnel and their families (e.g., Department of Army, 2006). Lastly, the third article in our series investigates whether the military’s century-old mental health policy may be harmful instead of being helpful to military populations and contribute to the generational pattern of preventable wartime behavioral health crises (Russell & Figley, 2015a, b).
A Century of Change and Consistency in US Frontline Psychiatry Doctrine
The US military’s frontline psychiatry doctrine has continually evolved and now includes programs beyond interventions for keeping combatants in their war zones. For example, per DoD (2013) Instruction 6490.05 Maintenance of Psychological Health in Military Operations, “COSC activities include continual assessment and consultation to line, medical, and other personnel from garrison to the battlefield regarding physiologic, psychological, and organizational stressors; personnel training about combat stress; traumatic event management; and individual and unit management of COSRs” (p. 10). The explicit mission or purpose of modern frontline psychiatry includes the goal “to return Soldiers to duty expeditiously” (Bruscher, 2011, p. 60). Specifically, per the US Army’s textbook on Combat and Operational Behavioral Health “In today’s combat environment, military leaders can expect to retain and return to duty (RTD) over 95% of service members who experience COSR” (Bruscher, 2011, p. 60). In practice, the stated goal of the US Army’s frontline behavioral health treatment or restoration centers in Afghanistan continues to be “to maximize the return-to-duty (RTD) rate” of military service members who are “temporarily impaired or incapacitated by stress related conditions” [Joint-Mental Health Advisory Team-7 (J-MHAT-7), 2011, p. 90]. To that end, in 2010, the Army reported a 98.7% RTD rate of 193 war-stressed soldiers after they had completed a 3- to 5-day behavioral health treatment program in Afghanistan, including 20% of soldiers diagnosed with an adjustment disorder and 7% diagnosed with PTSD (J-MHAT-7, 2011).
Although research has shown the value of trauma-focused psychotherapy (Friedman, Keane, & Resick, 2014), the US military’s frontline psychiatric policy generally prohibits the use of evidence-based trauma-focused psychotherapies to treat acute stress injuries, such as acute stress disorder (ASD) or PTSD (e.g., DVA/DoD, 2010). This policy has been adopted ostensibly because sensitivity to the military psychiatric patient—specifically, it has been implemented to “mitigate risk that this assistance be viewed as either clinical treatment or traditional mental health care and follow up” (DoD, 2013, p. 7). Ostensibly, this prohibition derives from the frontline psychiatric principle of facilitating RTD (e.g., avoid psychiatric labeling and treatment as a patient). Stigma is associated with trauma-focused treatment, and it could be interpreted both by the service members and others as a threat to a soldier’s chance of RTD. The US military harbors concerns that to identify and treat conditions like PTSD in war zones might work against RTD, as is reflected in the US Army’s Textbook of War Psychiatry. It noted that “the application of involved treatments may only strengthen the soldier’s rationalization that he is ill physically or mentally” (Jones, 1995a, p. 10). It continued that treatments should be kept simple in order to normalize the soldier’s experience and avoid any perception of mental illness (Jones, 1995b, p. 29). In practice, this policy has led deployed personnel requiring definitive treatment for conditions like PTSD to either endure delays in accessing optimal PTSD therapies (e.g., DVA/DoD, 2010) until after their deployment(s), or face medical evacuation outside the war zone if they decompensate or become so seriously impaired as to threaten their or others’ safety (e.g., Department of Army, 2006).
Similar institutional barriers to seeking military mental health care have been well-documented, including chronic shortages of well-trained specialists and entrenched fears of stigma, aversive administrative personnel actions (e.g., loss of security clearance), and premature ending of one’s military career [e.g., Acosta et al., 2014; DoD Task Force (TF) on Mental Health (MH), 2007]. Consequently, military personnel with war stress injuries may experience inordinate and potentially harmful treatment delays resulting in the accumulation of comorbid conditions (e.g., depression, substance abuse, chronic pain, suicidal behavior, posttraumatic anger, etc.; Russell & Figley, 2015a). This pattern of repeated RTD to war zones and delayed psychiatric treatment may continue until service members either: (a) decompensate into impaired functioning, (b) voluntarily leave or retire from the military and seek VA mental healthcare, or (c) receive VA or private sector mental healthcare after being involuntarily discharged due to misconduct or personality disorder (e.g., Government Accountability Office, 2010).
Ethical Dilemmas of Frontline Psychiatry Doctrine
Military medical and behavioral health specialists whose duty is to implement the doctrine of frontline psychiatry regularly confront the need of avoiding harm to their patients (Camp, 2014). The policy of repeatedly returning war stress casualties back to war zones presents substantial risk of developing more severe and potentially debilitating chronic conditions (e.g., Institute of Medicine, 2008). Ethical concerns over the military’s frontline psychiatry doctrine have occasionally been debated considering the medical ethic of avoiding harm (e.g., Camp, 1994). For instance, during the Vietnam War, several US Army psychiatrists openly questioned the ethics of knowingly returning traumatized service members back to their units and delaying treatment, which led to harming veterans (e.g., Camp, 1994). But Camp (1994) also reported the lack of research to support such claims.
That being said, the US military maintains that properly adhering to the principles of frontline psychiatry in the war zone would avoid high psychiatric attrition and evacuation rates from war zones. There should not be a tendency to ignore, delay, or improperly utilize the principles. As noted by the US Army’s textbook of war psychiatry, “Treatment failures, when they occurred, were generally because the principles were not applied” (Jones, 1995b, p. 43). Instead of considering it ethical to protect combatants from harm by premature RTD, it has been argued that a lack of timely RTD of combatants with combat fatigue from reentering combat would “violate the soldier’s prior expectations and break an implicit promise to them,” as well as exposing other combatants to risks due to their absence (Howe & Jones, 1994, p. 119). Some military workers have even insisted that “inappropriate evacuation” could “constitute medical malpractice” (Martin & Cline, 1996, p. 164).
Furthermore, a recent review of medical evacuations out of Iraq and Afghanistan indicated that psychiatric conditions had constituted from 5 to 6% of total evacuations in 2004, but that percentage had increased to a high of 13% in 2007 (Cohen et al., 2010). Reflecting on this increase, the authors concluded that the use of preventive measures, including therapeutic interventions, could reduce any negative effect of service members’ psychiatric conditions on “military readiness” (Cohen et al., 2010, p. 301). In other words, although concerned for their service members’ psychiatric state, the ultimate concern that the military has in its frontline psychiatry policy is to conserve its fighting strength and avoid harm caused by psychiatric evacuations. Although the ethics of this policy in the military’s frontline psychiatry doctrine has been questioned (e.g., Camp, 2014), these policies remain firmly entrenched (e.g., Jones & Wessely, 2003).
Framing the Debate
Per the DoD (2013), frontline psychiatry/COSC is defined as: “Programs developed and actions taken by military leadership to prevent, identify, and manage adverse COSRs in units; enhance mission performance; increase individual and unit resilience; conserve fighting strength; prevent or minimize adverse effects of combat stress on members’ physical, psychological, behavioral, and social health; and to return the unit or Service member to duty” (p. 10). In this section, we present the underlying rationale or bases for the military’s beneficial claims about the benefits of its frontline psychiatric policies, along with the military’s arguments why frontline psychiatry that involves removal from combat and a lack of RTD may cause greater harm to military populations. Articles part II and III of our analysis present the evidence for both sides of the debate.
Arguments of the Potential Benefits from Frontline Psychiatry
Frontline psychiatry aims to provide benefits to both the military’s mission and its personnel. For example, the US Army maintains that successful treatment of service members having combat stress “prevents unnecessary evacuation” (Jones, 1995b, p. 46) and unnecessary “stigma” associated with any evacuation for a mental health condition (Mental Health Advisory Team-I (MHAT-I), 2003, p. B-14).
How Frontline Psychiatry Benefits the Military Mission
The inherent danger and stress of war predictably causes physical and psychological casualties (e.g., Department of Army, 2006). However, a depleted army cannot fight or win wars. Consequently, an evacuation policy that is too permissive risks inviting massive evacuation syndromes that can erode individuals’ and their units’ will and capacity to fight (e.g., Jones & Wessely, 2003). Therefore, policies aimed at preserving the fighting force by eliminating or significantly reducing reasons for attrition, which also serves to maintain unit identity, are conducive to the military mission. Conditions like PTSD do develop in the war zone. On the other side of the coin, they are more easily simulated or faked than physical wounds (e.g., Jones, 1995a), but that is another issue. The following review considers that claims of PTSD and the like are legitimate.
Since the Second World War (WWII) up to the present wars in Iraq and Afghanistan, the US military reports that between 60 and 98% of war stress casualties have been RTD (e.g., Martin & Cline, 1996; Cooper, Newton, & Yarvis, 2011). Conversely, during these same periods of war, only 4 to 6% of medical evacuations of US combatants have been due to psychiatric conditions (e.g., Cohen et al., 2010). These percentages appear to attest to the value of modern frontline psychiatry in war zones and its ability to preserve the fighting force. Also, these percentages stand in stark contrast to reports of 22% psychiatric evacuations prior to implementing frontline psychiatry doctrine in WWII (e.g., Jones, 1995a). Additionally, reducing psychiatric evacuations and treatment have entailed a substantial cost-savings to the military, especially if the bulk of mental health treatment is transferred to the VA after service members are discharged, which historically has been the case since WWII (e.g., Russell, Butkus, & Figley, 2016b).
Arguments Why Frontline Psychiatry Benefits Military Personnel and Their Families
With regard to the posited health benefits for individual service personnel and their families, the military’s rationale hinges mainly on avoidance of harmful premature psychiatric labeling and separation from one’s military unit. This rationale is based on the following arguments (some of which have been highlighted already in the above): (a) RTD prevents short- and long-term harm associated with stigma, guilt, and shame of being evacuated as a psychiatric casualty [e.g., “the guilt, however irrational, associated with abandoning one’s unit can be a significant contributor to ongoing personal trauma” (DoD-TF-MH, 2007, p. 24)]; (b) RTD avoids the potential harm of developing a chronic or severe psychiatric disability based from frontline units (Jones, 1995b, pp. 37–38); (c) regular access to embedded behavioral health specialists during deployment reduces the harmful effects of stigma and barriers to seeking care (e.g., Nash, 2011); (d) research shows that RTD preserves access to protective and resiliency factors such as unit morale, leadership, cohesion, and social support that otherwise is harmfully disrupted when soldiers are evacuated (Jones, 1995b, p. 28); (e) RTD reduces psychiatric morbidity by reinforcing or bolstering soldier’s psychological defenses against subsequent breakdown in combat (e.g., Camp, 1994); (f) RTD normalizes combat stress reactions as temporary and transient conditions thus instilling self-confidence and expectancy of recovery (e.g., Department of Navy & U.S. Marine Corps, 2010); (g) RTD avoids the harmful iatrogenic effects of psychiatric labeling of normal reactions as abnormal (Jones, 1995b, p. 49); (h) avoiding psychiatric evacuation prevents harm related to premature career loss due to military discharge (e.g., Cohen et al., 2010); and (i) RTD enhances individual resilience and posttraumatic growth (PTG) that otherwise would be hindered if war zone evacuation takes place (e.g., Department of Navy & U.S. Marine Corps, 2010).
Arguments Why Frontline Psychiatry Harms Military Personnel and Their Families
Despite the apparent value of RTD in frontline psychiatry in the war zone, arguments of greater individual harm than benefit from premature RTD practices can be summarized as follows: (a) empirical evidence indicates a dosage effect from cumulative exposure to war stress (see next), as reflected in the Multiple Claimants v. MoD case wherein the High Court ruled: “it was known that a linear relationship exists between the acute reaction to combat stress and the duration and intensity of combat” (McGeorge et al., 2006, p. 22); (b) systematic review and meta-analyses reveal that the single best predictor for combat-related PTSD and other war stress injury is constituted by cumulative effects of combat exposure (e.g., Dohrenwend, Yager, Wall, & Adams, 2013; Kulka et al., 1990); (c) reviews have found functional and structural changes in the brain and other body organ systems after chronic war stress exposure (e.g., Institute of Medicine, 2008); (d) the military’s own treatment guidelines, including VA/DoD (2004, 2010), recommend early identification and treatment with evidence-based therapies to prevent chronic PTSD, in that “Without early treatment, problems are more likely to become chronic and entrenched” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–6); (e) the military’s early research that RTD can be effective lacked acceptable research methodology (Jones & Wessely, 2003); (f) previously classified military reports during WWII revealed high relapse rates and low rates of restoration to full combat duty after RTD (Jones & Wessely, 2003, p. 413); (g) generally, there is a paucity of controlled and correlational research on clinical effectiveness of frontline psychiatry and its claims of individual benefit (e.g., Jones & Wessely, 2003); (h) neuropsychiatric casualties appear to have outnumbered the total number of combatants wounded-in-action (WIA) and killed-in-action (KIA) since the frontline psychiatry doctrine was formally institutionalized in WWII (e.g., Russell & Figley, 2015b); (i) there is an absence of controlled or semicontrolled research whether evacuated soldiers receiving evidence-based therapies fare worse than those RTD; (j) to the contrary, research has shown an increased risk of being WIA in Vietnam-combat Marines in war zones who RTD after being diagnosed with a psychiatric condition (e.g., Palinkas & Cohen, 1987); and (k) comparative studies from UK military researchers reveal that policies restricting exposure to war stress and provision of evidence-supported treatment can reduce PTSD prevalence rates (e.g., Fear et al., 2010).
Evidence of Possible Overselling the Benefits of Frontline Psychiatry
Prior to 9-11 and the Afghanistan War, an American Psychological Association Monitor interview quoted senior DoD medical leaders who were extolling the benefits of frontline psychiatry/COSC (see Rabasca, 2000, p. 50). However, Friedman (2004, p. 1) found only one study in support of this argument, and the results were not even statistically significant. Solomon, Shklar and Mikulincer (2005) conducted a 20-year retrospective research on Israeli combatants and found a lower but nonsignificant reduction in PTSD rates of veterans treated in the frontlines versus those evacuated out of war zones. That is, military policy had been established without proper consideration of the empirical bases. One could argue that science was used improperly, or what was selected was poor science for the question at hand and would not need any legal bar (e.g., Daubert, 1993). Lilienfeld (2005) posited nine warning signs for potential pseudoscience. Military policy regarding frontline psychiatry needs to be sufficiently buttressed by high-quality evidence-supported approaches to avoid accusations along these lines.
Understanding the Historical and Political Context of Frontline Psychiatry
An appreciation of the historical, political, and economic context of the military’s century-old frontline psychiatry doctrine is paramount in understanding the reason for its existence and future roadblocks in modifying existing policy. Numerous scholarly books and papers have been written describing the rich history of frontline psychiatry during specific wars like WWI (e.g., Myers, 1940) and across all major wars up to the Persian Gulf War (e.g., Shepard, 2001; Jones & Wessley, 2007). Rather than replicating the multitude of descriptive summaries on war psychiatry, our review focuses on the origins of the military’s messaging regarding frontline psychiatry doctrine. In doing so, five interrelated narrative themes emerge: (1) the military’s struggle in accepting the reality of the psychological impact of modern warfare and managing fear of mass psychiatric attrition, (2) a nearly exclusive focus on short-term administrative disposition (e.g., RTD rates) over long-term health outcomes, (3) changing etiological paradigms of the legitimacy and primary cause of war stress injury to align with the military’s goal of conserving the fighting force and reducing the financial burden of psychiatric disability pensions, (4) the military’s mistrust and ambiguity toward mental health professions and efforts by those professions, and (5) selective bias toward reporting favorable evidence supporting the military’s approach that frontline psychiatry as presently practiced is beneficial to service members.
Pre-Twentieth Century Origins of Frontline Psychiatry
Military efforts to prevent attrition from psychiatric “breakdown” by use of brief respite (e.g., rest, food, shelter), occupational therapy, massage, and mild electric shock while limiting evacuation to distant hospitals can be traced back to the Russian Army during the Crimean War (1853–1856; Wanke, 2005). After the Crimean War, in 1859, the Russian Chief Military-Sanitary Committee established the first military psychiatric school dedicated to training military psychiatrists and to study war stress injuries and their treatment (Wanke, 2005).
The US Civil War
The American Civil War (1861–1865) compelled the nation to recognize the emotional toll of warfare, as Civil War era physicians were ill-prepared and overwhelmed by large numbers of psychophysical maladies defying logical explanation (Dean, 1997). Union Army Surgeon General William A. Hammond adopted a progressive holistic medical paradigm of unitary mind-body that essentially equated physical wounds and psychiatric conditions like “irritable heart.” As well, in 1862, he helped establish the U.S. Army Hospital for Diseases of the Nervous System in Philadelphia (later known as Turner Lane) (Wooley, 2002). At Turner Lane, S. Weir Mitchell, the father of American neurology, developed the resting cure, whereby war stress casualties were administered seclusion, rest, ample nourishment, and mild electrical stimulation to replenish depleted “nerve force” (e.g., Lande, 2003). Emphasis was placed on the physician’s use of persuasion and appealing to a soldier’s strengths and masculinity for eventual RTD (Lande, 2003). Occupational therapy was employed for recuperating soldiers to maintain their military identity by engaging in menial labor just behind the frontlines rather than receiving automatic military discharge (Lande, 2003). In 1864, Union Army physician Jacob M. DaCosta reported that 33% of 200 soldiers diagnosed with irritable heart, a PTSD precursor, were successfully treated using Mitchell’s resting cure (DaCosta, 1871). The emerging frontline policy of appropriate attitude and convalescence utilized firm expectations of recovery and RTD, thus helping to avoid malingering and feared mass exodus (Dean, 1997; Lande, 2003). However, contemporary military mental healthcare appears to have set aside this approach to war trauma (e.g., Jones, 1995a; Russell, Figley, & Robertson, 2015). Granted, wars differ over country, generations, and locations. However, history might provide informative examples.
Industrialization and Emergence of Trauma-Pension Debates
Prior to WWI, traumatic stress injuries in Western society were considered as authentic and compensable, with impacts to the central nervous system caused primarily by exposure to extreme environmental events (e.g., Lerner, 2003; Wanke, 2005). Early posttraumatic conceptualizations, such as Erichsen’s (1866) “railway spine,” Beard’s (1869) traumatic neurasthenia, and Oppenheim’s (1889) “traumatic neuroses,” all posited legitimate brain injury caused by traumatic events. Subsequently, the British Legislative Act of 1864 and the 1889 German Imperial Insurance Office Act established the legal precedent granting traumatic or accident neuroses the status of actionable conditions, whereby responsible companies were held liable to provide compensation (e.g., Brunner, 2003).
Fearing mass fraud, industries hired physicians to discredit the authenticity of traumatic neuroses in favor of a paradigm of hysteria, pseudo-illness, predisposed weakness, and malingering (e.g., Brunner, 2003; Glynn, 1910). In 1900, the Hartmannbund Association of German Doctors for the Protection of Economic Interests was formed to combat state welfare legislation (Lerner, 2003). For example, traumatic reactions/ neuroses involving hysteria led to poor inhibition “seen in particular women, effeminate men, children, the uneducated, and those outside Western Europe” (Lerner, 2003, p. 38).
Rediscovering the Value of Frontline Psychiatry During WWI
By mid-1914, early into WWI, every major warring power witnessed an unprecedented number of evacuations due to psychiatric “breakdown.” Hundreds of thousands of military officers and enlisted members alike were being discharged, sent home, and given disability pensions for afflictions such as shell shock and traumatic neuroses (e.g., Holden, 1998). European governments and their military departments became increasingly alarmed by the epidemic of war stress casualties. These casualties existentially endangered the military’s capacity to fight and win wars, as well as producing skyrocketing disability pension costs that threatened to bankrupt economies (e.g., Jones & Wessely, 2007; Shepard, 2001). The ensuing trauma-pension debate intensified (Lerner, 2003; Shepard, 2001).
1916-Military Replacement of the Paradigm of Traumatic (War) Stress Injury
As WWI battles of 1916 intensified (i.e., The Somme), unmatched numbers of war neuroses occurred elevating the trauma-pension debate into crisis (e.g., Brunner, 2003). European powers replaced the holistic, authentic posttraumatic stress paradigm (e.g., traumatic neuroses) espoused by Oppenheim and others, with a paradigm of hysteria, considered a pseudo-illness caused primarily by predisposed individual weakness, cowardice, malingering, and pension-seeking neuroses (e.g., Lerner, 2003). Residual effects of the 1916 paradigm shift are evident in the US Army’s Textbook on War Psychiatry: “It is important to remember that most psychiatric casualties are soldiers who, because of the influence of negative psychological, social, and physiological factors, unconsciously seek a medical exit from combat. Most cases, therefore, will mimic features of other medical disorders that would be “legitimate” forms of escape from combat, thus becoming evacuation syndromes” (Jones, 1995b, pp. 37–38).
Consequently, a uniform frontline doctrine emerged with strict prohibition against psychiatric labeling, evacuation, discharge, and pensioning (e.g., Jones & Wessely, 2007). In addition, aggressive methods replaced putatively ineffectual gentle approaches in treating war hysteria, including battlefield executions, faradization (electric shock), and the infamous Kauffman Cure (severe, sometimes fatal electric shocks) resulting in claims of 90% RTD to the frontlines (e.g., Holden, 1998).
In 1916, the British Army Council issued a directive replacing “shell shock” diagnosis with a Not Yet Diagnosed (NYD) (Nervous) classification due to concerns about rampant attrition and pensions for malingerers (e.g., Holden, 1998). Efforts to increase social pressure on combatants to avoid seeking psychiatric care included intensification of stigma with labels such as Lacking Moral Fiber (LMF) written on the uniforms of war-stressed air crews (e.g., Jones & Wessely, 2007).
Reasons for the military’s new classification schemes are apparent in a US Army’s summary: “Soldiers in World War I who were called “shell shocked” indeed acted as though they had sustained a shock to the central nervous system” and the diagnosis of “war neurosis” conveyed chronic or severe mental illnesses. This problem was remedied when medical personnel were instructed to tag such casualties as NYD (nervous) which gave soldiers nothing definite to cling to and no suggestion had been made to help them in formulating their disorder into something that was generally recognized as incapacitating and requiring hospital treatment, thus honorably releasing them from combat duty” (Jones, 1995a, p. 10). Naturally, stigma associated with war stress injuries became intensified and served as a viable tool in managing the military’s mental health crisis.
Toleration of Psychiatry in WWI to Reduce Attrition and Pensions
At the outset of WWI, the newly established mental health disciplines of psychiatry (1808) and psychology (1879) were still in their infancy. However, epidemic numbers of psychiatric casualties among the military service members and heightened publicity regarding psychiatric attrition and pensioning costs of shell-shocked members forced military leaders to solicit the services of mental health specialists (e.g., Lerner, 2003). However, ambiguity toward mental health in both military and civilian sectors was widespread, as articulated by the British Secretary of Navy and future Prime Minister Winston Churchill (1942): “I am sure it would be sensible to restrict as much as possible the work of these gentlemen, who are capable of doing an immense amount of harm with what may very easily degenerate into charlatanry” (cited in Holden, 1998, p. 94).
That said, some military experts realized the value of military evaluation. Myers, who coined the controversial term shell shock (Myers, 1915), observed the French Army’s use of frontline psychiatric interventions in WWI to achieve a 91% RTD (e.g., Myers, 1940). Myers studied British hospital disposition records and noted the correlation of lower RTD rates the greater the distance soldiers were evacuated from the front (Myers, 1915). He went on to help improve upon the French system of managing psychiatric injury in WWI by developing respite and restorative treatment and deploying mental health professionals to the war zone to prevent attrition (e.g., Myers, 1940).
Proving the Value and Benefit of Psychiatry to the Military
Myers efforts to improve frontline psychiatry in WWI initially had beneficial effects. British frontline psychiatry programs initially reported promising results with over 31% of war stress casualties RTD that would eventually improve to 90% RTD (Myers, 1940). The remaining portion of war stress casualties was assigned to neuropsychiatric rehabilitation centers at or near the war zone, reflective of the new WWI military policy of prohibiting psychiatric evacuation, discharge, and pensioning except in the most extreme cases of obvious, chronic, and profound “decompensation” (e.g., Holden, 1998).
In 1917, the American Expeditionary Forces sent Army Psychiatrist Major Thomas Salmon to observe British efforts to manage the psychiatric problem in preparation for the US entry into the war in 1918. Salmon (1917) adopted the European system of restorative care, as well as the frontline policy of avoiding psychiatric labeling (e.g., shell shock), evacuation, and discharge. The principles of frontline psychiatry that were adopted mandated simple, immediate treatment at the frontlines with clear expectation of RTD. To formalize military doctrine, Artiss (1963) later coined the acronym PIE (Proximity—at or near the frontlines, Immediacy—as soon as possible after developing a CSR/COSR, Expectancy—expected RTD after brief respite versus evacuation) to formalize military doctrine. Throughout WWI, the US military reported RTD rates of 65 to 90% due to its frontline psychiatry doctrine thus demonstrating how mental health disciplines can benefit the military mission (e.g., Jones, 1995a; Strecker, 1919).
Initial Mistrust of Frontline Psychiatry and Mental Health Services
However, Jones et al. (2010) reexamined historical records at the Convalescent NYDN Depot, which admitted 66,800 British soldiers between August 1917 and January 1919. They reported that very few war stress casualties were actually returned to their fighting units, in contradiction to the military’s past claims (Jones et al., 2010). Furthermore, after reanalyzing medical records from the PIE unit at 4 Stationary Hospital, only 606 British soldiers (19. 6%) were RTD, with a significant number believed to have relapsed (Jones et al., 2010). The authors concluded that a 19.6% combatant RTD was considerably lower than previously claimed by the military (Jones et al., 2010). British army leaders began to doubt the validity of frontline psychiatry claims, prompting an internal investigation by the Army’s chief neurology consultant Gordon Holmes who had played a pivotal role in establishing frontline psychiatry (Johnson & Row, 1923). After auditing three frontline psychiatry centers in 1917, Holmes reported an 80% RTD rate within 3 weeks, in contrast to 30 to 40% at base hospitals in France, and only 4 to 5% RTD in UK hospitals (Holmes, 1939). These findings appeared to reaffirm frontline psychiatry’s value to the military in preserving the fighting force. In addition, Holmes reported that only 10% of soldiers RTD subsequently relapsed for “shell shock,” but then proceeded to close several PIE units (Johnson & Rows, 1923). Nevertheless, an empirical foundation was built during WWI establishing the efficacy of frontline psychiatry doctrine as an effective tool for the military to end evacuation syndromes.
Reported Adverse Effects from Psychiatric Evacuation and Hospitalization
Before the US army entered WWI, it noted with respect to “shell shock” care and treatment in the British army that, “It is evident that the outcome in the war neuroses is good from a medical point of view and poor from a military point of view” (Salmon, 1917, p. 41). The clear majority of war stress casualties eventually recovered, especially when the service members were given proper specialized treatment. However, Salmon (1917) also noted that few British soldiers evacuated to England as psychiatric patients ever returned to military service, let alone the frontlines. For instance, of 5473 soldiers admitted to the hospital at Netley, England, from 1914 to 1917, only 53 were RTD. In 1917, only 153 or 21% of 731 military patients admitted to Maghull Military Hospital remained in the military (Salmon, 1917). Salmon’s (1917) findings reinforced the British army’s report (e.g., Holmes, 1939), whereby lower RTD rates are interpreted as evidence of psychiatric harm caused by evacuating soldiers away from their frontline units in that “Proximity and immediacy are important because the soldier’s time away from his unit weakens his bonds with it and allows time for consolidation of his rationalization of his symptoms” (Jones, 1995a, p. 9). It is important to note, however, that the military’s messaging around the deleterious psychiatric impact of evacuating war stress casualties is premised almost exclusively on data related to conserving the fighting force as measured by RTD rates and not based on empirical evidence of differential clinical outcomes.
Hidden Lessons of Inadequate Definitive Treatment and Faulty Discharge Policies
The military’s narrative on lessons of WWI and frontline psychiatry places great emphasis on harm to psychiatrically evacuated and admitted military patients (e.g., Myers, 1940). However, both Myers (1940) and Salmon (1917) warned about the adverse impact on military retention and RTD from grossly inadequate, nonspecialized treatment provision, such as admission to civilian insane asylums, ill-trained staff, and entrenched military bias to liberally discharge psychiatric patients versus an approach to treat and attempt to salvage military careers. For example, after studying the British treatment of shell shock and related conditions, Leese (2002) concluded that, considering the 746 case notes reviewed, most service members had not been treated in specialist centers, but instead on the specialist wards of large “General War” hospitals. Alternatively, they had been treated in nonspecialist wards of small medical centers (p. 98). Leese (2002) added that treatment would vary based upon how much his medic was qualified and that the system lacked the ability to provide the necessary specialist care. As well, lack of basic resources could worsen treatment (p. 98). Therefore, military claims of poor outcomes from psychiatrically hospitalized WWI soldiers must be tempered by what, if any, actual treatment was available and the quality of such treatment.
Conversely, reports of vastly improved outcomes, including RTD, indicate the potential benefit when soldiers receive adequate treatment at specialty hospitals for war stress injury by well-trained specialists. For example, in 1940, Myers noted “successful immediate treatment of such cases of shell shock.” Similarly, Salmon (1917) reported 60% of soldiers RTD to their frontline units after successful treatment at the Granville Canadian Special Hospital at Ramsgate England, and he noted even better rates in the special wards established in France (p. 41). In conclusion, the WWI record shows that when suitable treatment was provided, most service members could be retained in the military as opposed to immediate discharge and pensioning (e.g., Salmon, 1917).
Frontline Psychiatry and Clinical Treatment Outcomes
With regard to military research on therapeutic outcomes of service members evacuated and treated for war stress injury, Salmon (1917) admitted that there are no statistics available. Moreover, the impact of delayed treatment has never been examined. Furthermore, there has been no research to confirm recent US military policy for frontline psychiatry. After 1916, shell shock was considered a response to stress that is “temporary, reversible and related to a weakness of character” (Department of Navy and U.S. Marine Corps, 2010, pp. 1–3).
Psychiatry’s Short-Lived Victory
During the so-called interwar period between WWI and WWII, the demonstrated successes of WWI frontline psychiatry programs in terms of RTD and preventing psychiatric attrition were either ignored or intentionally disregarded following military and government investigations into the economic and political fall-out from the military’s massive psychiatric problem (e.g., Report of the War Office Committee of Enquiry into “Shell Shock;” Kullmann, 1922). On the American side, 72,000 US soldiers were discharged for neuropsychiatric conditions in WWI, with 40,000 claiming disability (Institute of Medicine, 2007) after just 3 months of exposure to modern warfare. Conclusions by investigative commissions almost universally blamed pre-existing individual weaknesses and the corrosive influence of psychiatry (i.e., psychiatric diagnosing, disability pensions), as well as inadequate military training, leadership, and unit morale. The potential contributory role of the military’s frontline psychiatric policies with regard to postwar prevalence of psychiatric disability and pensions was never entertained.
Consequently, European and American militaries disbanded their mental health services including all frontline psychiatry programs and their personnel. Instead, the militaries embarked on unprecedented, comprehensive psychiatric screening programs. The intent was to prevent those with “overt and covert mental disorders” entry into the military (Glass, 1966a, p. 7). From the military’s perspective, the role of mental health specialists is to prevent their future service members who could not handle rigorous military discipline, training, unit cohesion, combat, etc., from entering their work force.
Relearning the Realities of Modern War and Military Benefit of Frontline Psychiatry
In all, from 1942 to 1945, despite rejecting over 1,680,000 psychiatrically predisposed or even remotely defective inductees, rates 7.6 times higher than WWI (Berlien & Waggoner, 1966), once service members entered the military, psychiatric discharges during WWII were significantly higher than in WWI. There were over 1,103,000 US Army and 150,000 US Navy/Marine Corps psychiatric hospital admissions, resulting in 504,000 (72%) Army and 100,000 (67%) Navy/Marine Corps personnel psychiatrically discharged (e.g., Brill & Kupper, 1966; Chermol, 1985). In September 1943 alone, almost as many soldiers were discharged from the Army (112,500) than accessed (118,600), with most of those discharged for psychiatric reasons, which raised considerable alarm among war planners (Jones, 1995a). Consequently, the extensive mental predisposition screening policy was abandoned in 1943 (e.g., Glass, 1966b).
As for frontline psychiatry, during the 1942 North Africa Tunisian Campaign, 20 to 34% of all nonfatal US battle casualties were psychiatric in nature, 97% of whom were evacuated out of the war zone (e.g., Glass, 1966b). During the 1942 Guadalcanal invasion, 40% of 1st Division Marine evacuees were psychiatric casualties (Jones, 1995b). In March 1943, US Army Captain Frederick Hanson, utilizing “brief periods of sedation and rest along with the techniques of suggestion and ventilation,” showed that 30% of acute psychiatric patients were RTD within 30 h (Drayer & Glass, 1973, p. 9). Later that year, Hanson (1949) reported 70% of 494 neuropsychiatric casualties were RTD after 48 h. Thus, in April 1943, General Omar Bradley issued a directive establishing a holding period of 7 days for psychiatric patients at evacuation hospitals, disavowing psychiatric labeling, and advocating the use of the term “exhaustion” for all combat psychiatric cases (Drayer & Glass, 1973). In June 1943, U.S. Army Circular Letter No. 17, Neuropsychiatric Treatment in the Combat Zone was issued stating that military “patients in the Tunisian theater could be RTD within 3 to 4 days” (Drayer & Glass, 1973, p. 11). Overall, reports throughout WWII war zones of 80 to 90% stress casualties RTD were common.
Paradigm Shift Toward Universal Vulnerability and Normalizing Transient Breakdown
In November 1943, Chief of the Army General George C. Marshall ended the social experiment to screen out predisposed weakness and reintroduced mental health specialists and frontline psychiatry back into the rank and file (Glass, 1966b). In addition, military researchers reaffirmed a dosage effect from combat exposure. They found that seasoned veterans would break down on average after 80 to 90 combat days prompting US Army psychiatrists to observe “One of our cultural myths has been that only weaklings break down psychologically (and that) strong men with the will to do so can keep going indefinitely” (Beebe & Appel, 1958, p. 164).
The military’s 1943 paradigm constituted a middle-of-the-road view that normalized acute, transient psychiatric breakdown, but maintained the stigmatizing paradigm of hysteria for chronic conditions. In October 1945, the US Army introduced the new diagnosis transient personality reactions (TPR) that included combat exhaustion and acute situational maladjustments from noncombat stressors (Glass, 1966b). The American Psychiatric Association (APA) renamed TPR as gross stress reaction in the first diagnostic and statistical manual (Diagnostic and Statistical Manual of Mental Disorders, DSM; APA, 1952). The revised traumatic stress paradigm gave credence to a universal adaptation to extreme stress (i.e., war, natural disasters) wherein anyone’s coping capacity could be exceeded and temporary emotional breakdown would occur (e.g., Jones, 1995a). Inherent predispositions, personality disorder, or malingering was not invoked in this formulation, unless symptoms became chronic and resistant to treatment. Subsequent terms, such as combat exhaustion, battle fatigue, combat fatigue, fliers’ fatigue, operational fatigue, combat stress reactions, and COSR, together represent a continuation of the WWII paradigm.
In short, it could be argued that just as the 1916 paradigm shift to hysteria suited the military’s narrative in WWI to stigmatize psychiatric breakdown and end evacuation syndromes, the revised WWII paradigm of universal transient gross stress reaction represented justification of the military’s frontline psychiatry doctrine to conserve the fighting force while also limiting disability pensions. The latter was accomplished by attributing chronic war stress injury to pre-existing weakness, personality disorder, and/or malingering, all of which exacerbates stigma and barriers to seeking care.
Justification of Frontline Psychiatry as Beneficial to Individual Military Members
Efforts to justify the military’s frontline psychiatry doctrine as preventing harm to individuals were substantially magnified during and since WWII. Increasingly, military researchers and psychiatry scholars cited research on the importance of maintaining resilience factors, such as unit cohesion, morale, and leadership (Drayer & Glass, 1973). Also, Jones (1995a) noted: “Prospective studies by Stouffer (1949) conclusively showed that units with good morale and leadership had fewer combat stress casualties than those without these attributes when variables of combat intensity were comparable” (p. 14). Therefore, the inference made is that frontline psychiatry and RTD prevent war stress casualties by maintaining social ties to one’s unit.
In general, military psychiatrists in both world wars were under scrutiny. Some medical colleagues and commanders doubted the wisdom of employing them (e.g., Holden, 1998; Jones & Wessely, 2007). Their worth would be shown if they could demonstrate that psychological casualties of battle could be returned to fighting units within a few weeks (Jones & Wessely, 2003). For instance, per the US Army’s official psychiatric lessons learned on WWII: “an almost universal experience of medical officers in World War II concerned the deleterious effect of hospitalization” (Glass, 1966b, p. 746). Such claims routinely failed to mention that those hospitalized may have been more serious cases, and/or the quality of treatment received, as well as comparative clinical outcomes for those hospitalized versus RTD. On the other hand, medical opinion at that time raised the possibility of malingering: “others, perhaps the majority, viewed gain in illness as a conscious evasion of duty and used such terms as “goldbricking,” “malingering,” and “misfits”” (Glass, 1966b, p. 748).
In 1949, military retirement laws were revised to make medical discharge more complicated and time-consuming, resulting in “a marked decrease of medical separation for all causes, including psychiatric disorders,” resulting in a fewer medical discharge rate for psychiatric reasons right into the Korean War (Glass, 1966b, p. 757). Per the US Army: “Thus a solution was found for the excessive medical discharge of “psychoneurotic” cases, which consisted of both a change of psychiatric nomenclatures and a tightening of the medical discharge process” (Glass, 1966a, p. 757).
The military’s new messaging at that time reinforced the notion that frontline psychiatry prevents harm to service members (Glass, 1966b, p. 749). The US Army’s retelling of WWII lessons learned from frontline psychiatry conveys little of the health benefit to individual service members or their families, other than the fact that the farther military personnel are evacuated from their units, the lower the RTD rates. The assumption made by them, and for every war cohort, was that frontline psychiatry prevents psychiatric disability and that RTD is healthier for individuals (e.g., Jones, 1995b). However, as shown above, the only systematic review of frontline psychiatry at the time raised serious questions about the validity of such beneficial claims to military personnel (Jones & Wessely, 2003).
Continuing Evolution of Frontline Psychiatry in the Twentieth Century
The abruptness of the Korean War caught US military medical planners off guard, so no psychiatrists or consultation services were readily available (e.g., Jones, 1995a). Consequently, nearly 90% or more of psychiatric casualties were evacuated out of the war zone, about 20 per week from June to October 1950 (e.g., Ritchie, 2002). By October 1950, a three-echelon frontline treatment system was developed under Mental Hygiene Consultation Services utilizing PIE principles that resulted in 50 to 70% RTD (e.g., Glass, 1966b). By war’s end, most reports were describing a RTD rate of 60 to 90%. Significantly, there were few “repeaters” among those diagnosed with combat stress, treated, and returned to duty, e.g., 5 to 10% (Ritchie, 2002, p. 900). Prior to reconstituting frontline psychiatry in October 1950, only 50% of evacuated psychiatric casualties maintained their military careers and were RTD in noncombat roles (e.g., Ritchie, 2002). Again, like the world wars, no military studies were conducted comparing clinical outcomes of military personnel RTD versus those evacuated and treated for war stress injury.
The Vietnam War
The history of frontline psychiatry has been well-documented for the war in Vietnam (e.g., Camp, 2014). Of import, military medical leaders credited frontline psychiatry as responsible for historically low rates of war stress casualties identified in the war zone, with over 90% RTD and a meager 2 to 5% of total evacuated casualties identified as neuropsychiatric (Camp, 2014). However, Kulka et al. (1990) reported millions of Vietnam veterans experiencing PTSD, including 30% of combat veterans. These findings, along with news media stories of veterans experiencing depression, substance abuse, traumatic grief, moral pain, medically unexplained physical conditions, interpersonal violence, incarceration, homelessness, and suicide (e.g., Russell & Figley, 2015b), were in stark contradiction to the military’s narrative of effective psychiatric help for war stress injury. Consequently, accusations of widespread malingering appeared, and as well as the narratives of politically motivated antiwar therapists (e.g., Shepard, 2001), while the military and governmental institutions resorted to narratives that would avoid pension costs (e.g., Dean, 1997). In short, there was a recycling of the generational trauma-pension debates born out of WWI.
Recently, however, the US military has amended its historical interpretation of the lessons of Vietnam with regard to the controversy over psychiatric casualties reported in the war zone versus home front. For instance, Camp (2014) noted that the incidence of service members either hospitalized or excused from duty status ranged between 12 and 16.5 per 1000 per year. Camp continued that, although this rate appears positive compared to rates for prior wars, the Korean War (73/1000/year) and World War II (28–101/1000/year), it is “misleading” (p. ix). The author elaborated that the indicated rate addresses only one measure of psychological or behavioral dysfunction. Also, the average masked the fourfold rate increase in the last years of the Vietnam War (Camp, 2014, p. ix). In addition, the rate did not consider delayed clinical presentation (e.g., Camp, 1994). As with prior wars, no military research was conducted that compared outcomes for frontline psychiatry RTD and psychiatric evacuations and treatment.
Paradigm Conflict of PTSD and Transient Gross Stress Reaction
At war’s end, heated controversies ensued after the 1980 adoption of a PTSD diagnostic construct by the APA (1980) in the DSM-III that reattributed primary cause of injury to traumatic stress exposure versus individual weakness (e.g., Dean, 1997). For instance, military historians opined that before 1980: “The idea that a soldier of previously sound mind could be so emotionally disturbed by combat that he could no longer function was not entertained; that he might suffer long-term psychological consequences of battle was also dismissed” (Jones & Wessely, 2007, p. 165). The hotly contested PTSD debates have been reviewed elsewhere (e.g., Dean, 1997; Shepard, 2001). From the military’s perspective at that time, legitimizing chronic war stress injury as primarily caused by traumatic stress exposure, versus hysteria or predisposed weakness, significantly undermines its paradigm of transient personality or gross stress reactions, destigmatizes chronic stress-related conditions, and opens a virtual floodgate of pension-seekers. In response, although bound to adhere to current professional standards of medical and psychiatric practice, such as found in the DSM on PTSD, the military has largely resisted change to its paradigm of stigmatizing hysteria for chronic stress injury. For example, per the US Army’s Textbook of Military Medicine: War Psychiatry, chronic PTSD occurs: “in those with social and biological predispositions in whom the stressor is meaningful when social supports are inadequate” (Jones, 1995b, p. 416) and that: “Other mechanisms such as positive reinforcement (secondary gain in Freud’s model) seem more important in the chronic maintenance of symptoms” (Jones, 1995b, p. 417).
First Persian Gulf War
The Persian Gulf War (1990–1991) reinvigorated the trauma-pension debate, as 500,000 US military personnel participated in Operation Desert Storm (ODS) involving a 4-day ground war. Like in previous wars, frontline psychiatry was utilized as the prime treatment of war stress injury. However, Martin and Cline (1996) cited problems with organization, coordination, mobility, staffing, and training of the military’s CSC program. The authors expressed dissatisfaction with the reported high 90% RTD and low 3 to 5% psychiatric evacuation rates (Martin & Cline, 1996). About 6 to 12 months after returning home, 34% of ODS veterans reported significant psychological distress, including dazed feelings, numbing, agitation, and estrangement, as well as difficulty making emotional contact and participating in practical life problems (Institute of Medicine, 2008). Approximately 18 months after returning home, PTSD rates jumped to 9.4% (males) and 19.8% (females). Even more perplexing was a new controversial war syndrome, Gulf War Illness, consisting of a diverse pattern of medically unexplained physical symptoms that may have affected over 100,000 Gulf War veterans (e.g., Institute of Medicine, 2008). Like prior wars, no research was conducted comparing the administrative or clinical outcomes of military personnel evacuated or RTD via frontline psychiatry.
Twenty-First Century Afghanistan and Iraq Wars and Frontline Psychiatry Research
As reported earlier, the US military has continued to rely extensively on its frontline psychiatry programs to prevent chronic war stress injury. Since 2004, the US Army’s Walter Reed medical research facility has conducted and published empirical studies on the level of combat exposure, effects of multiple deployments, prevalence of war stress injury like PTSD, effects of stigma and barriers to care, pre- and postdeployment health screenings, and utilization of mental health services of service members returning from deployment. With regard to frontline psychiatry, the military has conducted annual field surveys via Army Mental Health Advisory Team (MHAT) reports and Joint-MHAT (J-MHAT) that includes Marine Corps, as well as research on medical evacuations, suicide, and other high profile issues. We review the results next.
MHAT/J-MHAT Studies
The DoD has conducted unprecedented annual surveying of the mental health of deployed personnel on the status of mental health services in the war zones through MHAT and J-MHAT studies. The MHAT studies offered real-time snapshots on the prevalence of a variety of risk (e.g., combat exposure, stigma, war stress injury, psychotropic medication) and resilience (e.g., morale, cohesion, leadership, coping) factors, as well as incidence of war stress injury (e.g., ASD/PTSD, anxiety, depression, suicide, traumatic brain injury, misconduct stress behaviors).
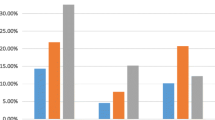
Effectiveness of Frontline Psychiatry
Table 1 summarizes the prevalence of psychiatric diagnoses tracked by the US military in the Afghanistan and Iraq war zones revealing ASD/PTSD rates between 8.5 and 17.9% from 2003 to 2013. These conditions were diagnosed by frontline psychiatrists or other trained personnel (e.g., J-MHAT, 2013). With regard to outcome, the data indicated a rate of 95 to 100% RTD, as well as limiting psychiatric evacuations to about 6 to 7% of medical evacuations. Historically, the military interprets high RTD as evidence of preventing harm to service members from psychiatric evacuations.
Frontline Psychiatry Benefit to the Military Mission and Personnel
Table 2 confirms the military’s long-standing reports of decreased RTD rates where farther individuals are evacuated from the frontlines. Since WWI, lower RTD rates have been used by the military to indicate possible harm to military personnel whose psychological conditions worsened due to the separation from their units. Therefore, interpretation of high RTD is traditionally viewed by the military as evidence of avoiding harm associated with being labeled and treated as a psychiatric patient, and thus beneficial to the well-being of service members and their families.
Beneficial Effects of Frontline Psychiatry in Enhancing Resilience and PTG
The US Army’s MHAT studies have tracked various protective factors, including soldier ratings of unit cohesion, morale, leadership, and PTG, as well as stigma and behavioral healthcare utilization. For example, according to the most recent J-MHAT survey, over 60% of soldiers deployed to Afghanistan are satisfied with the quality of their unit leadership, 74.3% reported a high level of unit cohesion, 41.4% reported high or very high morale, 59.4% received resilience training prior to deployment, 43.6% felt pride of what they have accomplished during deployment, 60.7% felt more self-confident as a result of their deployment experiences, and 28.6% reported enhanced stress coping as a result of their deployment (J-MHAT, 2013). The inference from these generally positive findings is that aggregated high self-ratings of protective factors should translate to resilience from war stress injury. Unfortunately, akin to previous wars, we are unaware of follow-up studies to ascertain outcomes. In addition, the recent J-MHAT (2013) survey reported that although 18% of deployed soldiers visited a behavioral health-related specialists during deployment, many continue to face stigma. For instance, of deployed soldiers screening positive for a mental health condition, 48.8% reported barriers to seeking mental health treatment over being perceived as weak, 45.2% felt their unit leaders would treat them differently, and 38.4% expressed fear over career damage (J-MHAT, 2013).
Potential Harm from Frontline Psychiatry
The US Army’s MHAT studies also track a host of risk factors, including combat exposure, number of deployments, presence of a mental health condition, and prescription of psychotropic medications. For example, the most recent J-MHAT (2013) report indicates a dosage effect between ASD/PTSD rates and number of deployments: 5.5% (first), 8.3 (second), and 14.6 (third or more). In addition, 66% of soldiers reported being attacked or ambushed, as well as knowing someone seriously injured or killed, 15.6% reported experiencing a blast that knocked them over (but only 56% received the mandatory TBI screening), 21.4% threatened physical violence toward a unit member, 8.5% endorsed suicidal ideation, 49.3% reported sleep disturbance, 10% screened positive for a current mental disorder, 2.6% were taking psychotropic medications during deployment, and 12% indicated marital problems leading to divorce (J-MHAT, 2013). In terms of aggregative data, one can surmise a moderate level of risk factors. However, on an individual level, concerns appear over possible harm from frontline psychiatry centers around dosage effects of cumulative exposure and war stress injury, along with barriers to seeking timely and adequate mental health treatment. Of course, the absence of frontline psychiatry research on outcomes prohibits anything but conjecture.
Changing DoD Deployment Policy Regarding Psychiatric Diagnoses
Since WWI, it has long been the military’s practice to screen out and reject potential recruits with a history of psychiatric illness, as well as prevent service members from deploying to war zones with a previously diagnosed psychological disorder (e.g., Glass, 1966a). The rationale for rigid psychiatric screenings was premised on decades of research showing that military personnel previously diagnosed with a psychological health condition, particularly PTSD, were at greater risk for a repeat diagnosis in theater (Larson et al., 2011) and after deployment (e.g., Kulka et al., 1990). However, in contradiction to its long held mental health screening and deployment policies, the Assistant Secretary of Defense for Health Affairs (ASD-HA, 2006) issued a policy change openly permitting service members with psychiatric diagnoses to be deployed to war zones. Per the 7 November 2006 memorandum Policy Guidance for Deployment-Limiting Psychiatric Conditions and Medications, military personnel who have been diagnosed and/or treated for any mental health condition, including PTSD, whether before, during, or after deployment, may be eligible for deployment or RTD if already in war zones. The diagnosis of PTSD or other psychiatric conditions in war zones will no longer trigger evacuation (ASD-HA, 2006). The main exceptions to the military’s new deployment policies pertain to diagnosis of bipolar and psychotic disorders (ASD-HA, 2006). The military’s explanation for reversing its century-old deployment policy appears to be framed as an effort to destigmatize mental illness and its treatment by labeling conditions like PTSD as treatable (ASD-HA, 2006). Benefit to service members and their families due to this new policy were noted, including retention versus discharge (ASD-HA, 2006). Military personnel who did not fully recover from their war stress injury or psychiatric disorder after 1 year of treatment would be recommended for discharge (ASD-HA, 2006). On the face of it, the policy reversal appears well-intended to eliminate barriers to seeking care. However, one could also argue that, as in other major wars, psychiatric attrition from stringent mental health policies threatened the military/government’s capacity to fight the war, especially with an all-volunteer force.
Three Major Failings of Frontline Psychiatry/COSC Doctrine
Readers may understandably question the validity of some of the above assertions with regard to the historical context of the military’s frontline psychiatry doctrine, especially in relation to political and economic motives. However, in 2010, the Department of Navy and US Marine Corps published its revised COSC guidance for leaders that included the limits associated with frontline psychiatry from its inception to present day: “The model of combat stress adopted after 1916 succeeded in reducing the rates of medical evacuations from theater for psychological reasons, which is one of the principal reasons this model remained the basis for combat stress control efforts for the rest of the 20th century. Now, seen through the lens of 21st century science, this model had serious shortcomings” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–5). Specifically, the Department of Navy and U.S. Marine Corps (2010) acknowledges the following three major deficiencies of frontline psychiatry:
-
1.
Overemphasizing RTD at the Expense of Deployed Personnel’s Long-Term Health
Two branches of the US military (Navy and Marine Corps) have recently acknowledged the potential harm from its frontline psychiatry policies that overemphasize RTD at the expense of individual service member’s long-term mental health. They wrote: “first, it considered only occupational functioning in its definition of psychological health, without sufficient regard for the extent to which less apparent distress or alterations in function may significantly impact current readiness or future health and wellbeing” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–6).
-
2.
Using Mental Health Stigma to Reduce Psychiatric Attrition
Perhaps the most striking public revelations by the Department of Navy and U.S. Marine Corps (2010) about frontline psychiatry policies that served to intensify mental health stigma and barriers to care were by deliberately misattributing the primary cause of war stress injury as due to individual weakness and predisposition rather than the effects of stress. They wrote: “The belief that stress problems arising during deployment are not “real” illnesses or injuries and merely “in the minds” of those afflicted has given rise to two comforting, though dangerous, assumptions—that any Service member who is not complaining doesn’t need attention and deployed Marines or Sailors who say they are “good to go” after developing stress problems can be safely considered psychologically well and fit without further medical monitoring or care” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–6).
-
3.
Promulgating a Faulty Etiological Paradigm of War Stress Injuries
Lastly, with regard to the military’s tendency to wrongfully attribute primary cause of war stress injury to predisposed individual weakness, pre-existing personality disorder, cowardice, and/or secondary gain, the Department of Navy and U.S. Marine Corps (2010) now publicly acknowledges that: “While it is true that pre-existing risk factors that contribute to vulnerability for stress-related problems have been identified, everyone is at risk and no one is immune. Studies of the causes of combat-related posttraumatic stress disorder (PTSD), for example, have shown again and again that the degree and frequency of exposure to combat and other intense stressors are a much more powerful determinant of outcome than maturity level, early life experience, or personality style” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–6). Also, the guidance states that: “The social stigma surrounding stress problems may have contributed to lower numbers of stressed Service members seeking treatment that might result in medical evacuation, but this stigmatizing conception of combat stress and psychological health has also discouraged Marines and Sailors from ever seeking professional help for stress problems of any kind. Without early treatment, problems are more likely to become chronic and entrenched” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–6).
Final Thoughts on the History of Frontline Psychiatry
As depicted in this and other historical reviews, the military’s frontline psychiatry doctrine emerged nearly exclusively out of concern for the military mission and government economics, and not the explicit well-being of war fighters or their families. This conclusion is exemplified by the Department of Navy and U.S. Marine Corps (2010) recent admission about “stress-related problems” creating “epidemics of stress casualties” (pp. 1–2). Consequently, the military has attempted to reframe its frontline psychiatry policies. However, is the DoD’s apparent paradigmatic change on stigma and etiology of war stress injury reflected on the ground? Unfortunately, the Government Accountability Office (2016) reported that stigma and barriers to care have not significantly been altered in policy or practice despite six previous sets of recommendations from independent investigations. Below is a brief overview of the US military’s current frontline doctrine.
Current Policy, Organization, and Services of US Frontline Psychiatry/COSC
The US military’s current COSC policies and procedures are outlined in a Department of Defense Instruction 6409.09 of 27 February 2012 Maintenance of Psychological Health in Military Operations (DoD, 2013) and implemented by each service branch via the U.S. Army’s (2009) Combat and Operational Stress Control Field Manual; U.S. Air Force Instruction 44-153 29 May 2014 Disaster Mental Health and Combat and Operational Stress Control; and U.S. Navy and U.S. Marine Corps 1-15M December 2010, Combat and Operational Stress Control. Today, as in the past, the US Army is designated as the lead agent within DoD with regard to training and implementation of frontline psychiatry in the war zones. Consequently, although nuances exist between each military branches’ frontline psychiatry policy, the US military remains firmly entrenched in traditional Army doctrine (e.g., Department of Army, 2009). This is particularly relevant given the Department of Navy and U.S. Marine Corps’ (2010) new stress continuum model reflecting a return to pre-1916 paradigm of traumatic stress injuries and offering a possible bridge between the dichotomy of RTD versus referral for definitive treatment for war stress injuries like PTSD. At the risk of major oversimplification and incompleteness, below we briefly outline contemporary frontline psychiatry exclusively with regard to war zones. Interested readers wanting a fuller understanding of the breadth and scope of these programs should consult primary sources (e.g., Department of the Army, 2009; Department of Navy & U.S. Marine Corps, 2010).
Guidelines for the Management of COSR
Individuals presenting with acute COSR are managed by frontline medical and mental health personnel applying BICEPS principles. Per the Department of the Army (2009), the key to treatment success involves returning the soldier to her/his original unit. For severely combat-stressed soldiers, “medical personnel at the battalion aid station level” need to evaluate them as soon as possible. RTD mitigates against recurrence. “In rare instances, however, it is in the best interest of the individual to be reassigned to other jobs or units” (pp. 3–11).
BICEPS Principles of Frontline Psychiatry
The more “masculine” BICEPS replaces the military’s original PIE acronym adopted in WWI (Department of the Army, 2006), but in all practicality, the two sets of principles are identical. In addition to conserving the fighting force, the military’s emphasis on normalizing COSR also serves to dispel stigma and negative attributions of individuals being predisposed, emotionally weak, psychiatrically ill, or otherwise incapable of continuing the mission. We have already given a definition of BICEPS in the above, but it is instructive to look at a full-scale description of BICEPTS before concluding (slightly modified). The Department of Army (2009) defines BICEPS as:
-
1.
Brevity. Initial rest and replenishment at COSC facilities located close to the soldier’s unit should last no more than 1 to 3 days. Those requiring further treatment are moved to the next role of care. Since many require no further treatment, commanders should expect their soldiers to RTD rapidly.
-
2.
Immediacy. It is essential that COSC measures be initiated as soon as possible when operations permit. Intervention is provided as soon as symptoms appear.
-
3.
Contact/Centrality. The soldier must be encouraged to continue to think of her/himself as a soldier, rather than a patient or a sick person. The chain of command remains directly involved in the soldier’s recovery and RTD. The COSC team coordinates with the unit’s leaders to learn whether the overstressed individual was a good performer prior to the COSR. Whenever possible, representatives of the unit or messages from the unit tell the soldier that she/he is needed and wanted back. The COSC team coordinates with the unit leaders, through unit medical personnel or chaplains, any special advice on how to assure quick reintegration when the soldier returns to his unit.
-
4.
Expectancy. The individual is explicitly told that she/he is reacting normally to extreme stress and is expected to recover and return to full duty in a few hours or days. A military leader is extremely effective in this area of treatment. Of all the things said to a soldier suffering from COSR, the words of his small-unit leader have the greatest impact due to the positive bonding process that occurs. A simple statement from the small-unit leader to the soldier stating that he is reacting normally to excessive stress and that he is expected back to duty soon will have positive impact. Small-unit leaders should tell soldiers that their comrades need and expect them to return. When they do return, the unit treats them as every other soldier and expects them to perform well.
-
5.
Proximity. Soldiers requiring observation or care beyond the unit level are evacuated to facilities in close proximity to, but separate from, the medical or surgical patients at the battalion aid station or medical company nearest the soldier’s unit. It is best to send soldiers who cannot continue their mission and require more extensive intervention to a facility other than a hospital, unless no other alternative is possible. Combat and operational stress reactions are often more effectively managed in areas close to the soldier’s parent unit. On the noncontiguous battlefield characterized by rapid, frequent maneuver and continuous operations, COSC personnel must be innovative and flexible in designing interventions that maximize and maintain the soldier’s connection to his parent unit.
-
6.
Simplicity. This principle indicates the need to use brief and straightforward methods to restore physical well-being and self-confidence. The actions used for COSR control (commonly referred to as the six Rs) involve the following actions:
-
Reassure normality.
-
Rest (respite from combat or break from the work).
-
Replenish bodily needs (such as thermal comfort, water, food, hygiene, and sleep).
-
Restore confidence with purposeful activities and contact with his unit.
-
Return to duty and reunite soldier with her/his unit.
-
Remind the soldier, as appropriate before, during, and after combat that: She/he is an American soldier here to complete a lawful mission. An American soldier behaves honorably because it is the right thing to do. Harming or killing noncombatants dishonors him and his fellow soldiers (living and dead). Stepping down to revenge helps the enemy to discredit the soldier and her/his unit, and the ultimate objective is to return home with honor (pp. 3-11–3-12).
-
Organization and Procedures
Today’s frontline psychiatry/COSC programs are a command-driven program at all levels in the military, providing a full spectrum of behavioral health support services throughout the deployment cycle (e.g., predeployment, deployment, postdeployment). The military’s COSC program utilizes five behavioral health disciplines (clinical psychology, social work, psychiatry, occupational therapy, and psychiatric nursing), along with peer mentors (enlisted specialists). It aims to implement a wide variety of preventive and restorative interventions, in keeping with BICEPS principles to reduce the occurrence and severity of COSR and behavioral disorders. A behavioral health staffing ratio of 1:700 has been established as ideal (e.g., J-MHAT-7, 2011). BICEPS constitutes a set of principles referred to later in the paper. It is critical to the new frontline psychiatry.
Echelons of Care/Functional Areas
Akin to previous generations, contemporary forward psychiatry employs a graded echelon of respite and restorative care. Per the Department of the Army (2009), COSC interventions are organized in nine functional areas that cover the full spectrum of behavioral health activities from prevention to clinical treatment. The nine areas include (1) unit needs—assessment, monitoring of the longitudinal health of their organizations, and offer the ability to identify and address any BH (behavioral health) or stress-related concerns; (2) consultation and education, including resiliency building (e.g., Battlemind training modules for military personnel and family members to strengthen coping skills across the deployment cycle); (3) traumatic events management (TME)—stress management for individuals or units after traumatic events (e.g., cool-down meetings); (4) reconstituting support—assistance—provided to entire units following major traumatic event or transition; (5) triage—identifying COSR and optimal level of care; (6) stabilization—initial management of severe COSR or behavioral disorders and assessment of RTD; (7) restoration—1–3-day management of COSR or behavior disorders normally near a medical treatment facility in close proximity to one’s unit, using BICEPS and the six R’s; (8) behavioral health treatment—routine outpatient mental health services, such as assessment, brief psychotherapy, psychotropic medication, and follow-up; and (9) reconditioning or extended restoration, involving intensive intervention typically up to 7 days, but can be extended to 14 days, with the primary goal of restoring soldiers who still have good potential for RTD. Reconditioning involves physical training, occupational therapy, military training, and brief psychotherapy for behavioral disorders within the outer limits of the war zone.
Embedded Mental Health Providers
Per the IOM (2014), “In theater there are no routine required psychological health screenings, although DOD is making an effort to identify service members who display signs of psychological stress during deployment and is improving access to psychological health care. Based on a recommendation from the DOD Task Force on Mental Health (2007), all branches employ the concept of embedded behavioral health by bringing psychological health clinicians closer to service members to improve access to care, increase mission readiness, identify service members with psychological challenges as early as possible, and improve communication between psychological health professionals and operational unit leaders (Cho-Stutler, 2013)” (p. 67). For example, the IOM (2014) goes onto report that “In the Marine Corps, for example, the OSCAR program attaches psychological health providers directly to units throughout the training and deployment cycles. For a more detailed description of OSCAR, see Chapter 4 of this report. As of August 2013, the Army’s Embedded Behavioral Health program had 45 embedded teams in place at U.S. and European installations with plans to expand to all deployable units by 2016 (U.S. Army, 2013)” (p. 67).
Functions and Responsibilities of Military Mental Health Sections
The military assigns mental health providers to be embedded in infantry units, combat ships, air wings, etc., to improve access, reduce stigma, and most importantly, reduce attrition. For instance, per the Department of the Army (2006), “All military mental health sections provide COSC for their units by identifying soldiers with COSRS who need to be provided rest/Soldier restoration within or near their unit area for rapid RTD. These programs are designed to maximize the RTD rate of Soldiers who are either impaired, have a diagnosed behavioral disorder, or have stress-related conditions” (pp. 11–12).
BH Treatment Within the War Zone
The Department of the Army (2006) policy regarding behavioral health treatment, such as psychotherapy, in war zones is contradicted for some conditions, such as behavioral disordered patient (BDP) (p. 11-1). Further, clinicians are warned to avoid promoting “dependency” and the “patient” role (Department of Army, 2006, p. 11-1). The goal of psychotherapy is to prevent symptoms of behavioral disorder from worsening in their severity and to help improve level of functioning. It is noted that “Treatment should not interfere with the Soldier’s duties or the unit’s mission” (Department of Army, 2006, p. 11-1) (which appears to emphasize priority of the military mission and not individual psychological health). Environmental barriers to providing recommended evidence-based psychotherapies for ASD/PTSD are delineated, such as related to transportation and assuring reliable meeting times (Department of Army, 2006, p. 11-1).
Standards of BH Treatment in War Zones
With regard to clinical practice standards, the Department of Army (2006) reports that standards for treatment are the same in the deployed environment and in the garrison (p. 11-1). Also, short-term treatment is more practical than longer term ones. If the latter is necessary, the treatment should be offered in time-limited modules. Treatment should never reduce the service member’s capacity to provide self-care or to defend her/himself. Providers need to consider as exceptions cases with emergency stabilization and preparation for evacuation (Department of Army, 2006, p. 11-1). In addition, military healthcare specialists are advised that “the VA/DoD Clinical Practice Guidelines website (http://www.oqp.med.va.gov/cpg/cpg.htm) offer clinicians evidence-based assessment and treatment algorithms for acute stress disorder, PTSD, and many other behavioral disorders” (p. 11-1), although implementation of recommended evidence-based therapies is generally prohibitive within war zones aside from psychotropic medication. Consequently, 2.6% of deployed soldiers reported taking psychotropic medications and another 11.6% of soldiers are using prescribed sleep medication (J-MHAT-9, 2013).
Contemporary Definitions of Frontline Psychiatry/COSC
The Department of Army (2006) defines COSC as “programs developed and actions taken by leadership to prevent, identify, and manage adverse COSRs (Combat and Operational Stress Reaction) in units” (p. 1-1). Over time, the military’s definition and description of its forward psychiatry programs has increasingly emphasized the individual benefits to service personnel and families throughout the entire deployment cycle including reintegration and not just in war zones (Bruscher, 2011, p. 65). Per the Department of the Army (2009), a potentially traumatic event (PTE) should be perceived as part of a range of possible outcomes that each person will experience with a range from “positive growth behaviors to negative and sometimes disruptive reactions” (p. vi).
Combat and Operational Stress Behaviors (COSB)
The military has extensively documented the diverse manner human beings respond to combat and/or operational stress, both in the immediate and long term. The experience of war is perceived by most as life changing in both positive and negative ways.
Adaptive or Positive Stress Reactions
The Department of the Army (2009) defines adaptive stress reactions as ones that can enhance individual and unit performance” (pp. 1–4). The benefits include developing trust, loyalty, and cohesiveness between ones’ peers and leaders, esprit de corps, and fostering unit cohesion.
Combat and Operational Stress Reactions
COSR is the DoD-approved term replacing earlier terminology, including “battle fatigue” or “combat exhaustion,” used to normalize acute stress responses (ASR) related to deployment and war-zone stressors and acute combat stress reactions (CSR) related to combat exposure (i.e., VA/DoD, 2004; Department of Army, 2006). The COSR reflects a “normal” universal human adaptive stress response involving a broad spectrum of symptoms, including physical (i.e., fatigue, muscle tremors, rapid heart rate, chest pain, nausea, bruxism, headaches), cognitive (i.e., intrusive images, hypervigilance, poor concentration, nightmares, memory problems), emotional (i.e., anxiety, grief, fear, guilt, emotional shock, depression, irritability, emotional numbing), and behavioral (i.e., insomnia, somatic complaints, exaggerated startle, pacing, alcoholism, antisocial acts, withdrawal, change in communication) that could last from 1 to 4 days (i.e., Department of Army, 2006; VA/DoD, 2004; Jones, 1995a).
Transient COSRs are universal and not signs of psychopathology (Jones, 1995a). In Menninger’s (1948) study on “normal battle reaction,” about 50% of soldiers experienced symptoms. Although the stress adaptation is universal, individual symptoms range from many to some to none (Ranson, 1949, p. 3). Differences in severity, type, and length of COSR associated with acute breakdown are highly individualized and determined by a wide range of risk and protective factors, but the most important determinant of when and how breakdown occurs is the intensity, severity, and duration of war stress (i.e., IOM, 2008).
Postcombat and Operational Stress (PCOS)
Aside from combat and operational stress, the US Army defines PCOS as a range of possible outcomes that could develop weeks to years after the end of combat and operational stress exposure (pp. 1–4). PCOS includes “adaptive PTG, mild COSR, and more severe symptoms, such as associated with PTSD (Department of Army, 2009, pp. 1–5).
Posttraumatic Growth
The Department of the Army (2009) has recently added the construct of PTG to its frontline psychiatry doctrine. For the army, it refers to positive outcomes involving improved social relationships, renewed hope and appreciation of life, a better sense of personal strength, and spiritual development (pp. 1–5).
Maladaptive and Long-Term Stress Reactions
If COSR is unabated after 1–4 days of frontline intervention, service personnel are usually triaged and transitioned to more definitive levels of care (e.g., VA/DoD, 2010). When COSR is associated with traumatic war or combat stressors, symptoms may involve re-experiencing (i.e., distressful intrusive recollections, nightmares, flashbacks), hyperarousal (i.e., insomnia, exaggerated startle, hypervigilance, irritability), avoidance (i.e., avoiding reminders, restricted range of affect, withdrawal), and dissociation (i.e., emotional numbing, detachment, alexithymia), resulting in a diagnosis of ASD (APA, 2013). When ASD symptoms persists beyond 4 weeks, which happens in at least 75% of cases (i.e., Bryant, 2007), the diagnosis shifts to PTSD (APA, 2013), which can be acute (3 months) or chronic (VA/DoD, 2010).
Posttraumatic Stress Disorder
Per the Department of the Army (2009), PTSD can develop following a traumatic event (such as combat exposure), when the event involved a threat of injury or death to the soldier or someone else (pp. 1–5). This approach to PTSD is consistent with that found in the DSM-5 (APA, 2013).
Stress-Injury Paradigm
The revised Department of Navy and U.S. Marine Corps (2010) COSC guidance reintroduces the pre-1916 construct of traumatic neuroses when it defines a stress-injury as, “More severe and persistent distress or loss of functioning caused by disruptions to the integrity of the brain, mind, or spirit after exposure to overwhelming stressors. Stress injuries are invisible, but literal, wounds caused by stress, but, like more visible physical wounds, they usually heal, especially if given proper care” (pp. 1–3). Shifting to a stress-injury paradigm is intended to serve as a “bridging concept between normal reactions and pathological illnesses” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–7) and is conceptually justified because it: “(a) Is consistent with 21st century scientific evidence regarding the effects on the brain, body, and mind that is suffering severe or prolonged stress, (b) Reduces the burden of stigma associated with persistent stress problems of all kinds, (c) Gives leaders a marker of psychological health risk and possible need for early intervention to restore health and wellness” (Department of Navy & U.S. Marine Corps, 2010, pp. 1–7).
The stress continuum model is a paradigm shift recognizing the entire spectrum of stress responses and outcomes and includes adaptive coping and wellness (color coded Green as the “Ready” Zone), mild and reversible distress or loss of function (the Yellow “Reacting” Zone), more severe and persistent distress or loss of function (the Orange “Injured” Zone), and mental disorders arising from stress and unhealed stress injuries (the Red “Ill” Zone) (Department of Navy & U.S. Marine Corps, 2010). Unfortunately, the recent paradigm shift is not widely adopted throughout DoD. The Department of Navy and U.S. Marine Corps (2010) publication represents a nonbinding guidance limited to leaders in the Navy and Marine Corps. As mentioned previously, Department of Army (2006) field guidance is the US military’s primary doctrine in the current war zones of Iraq and Afghanistan, and the US Army and US Air Force have yet to adopt the stress injury paradigm.
Differentiating COSB Along the COSR Continuum
The military readily acknowledges the inherent complexity in differentiating between the various manifestations of COSR. For example, the Department of the Army (2009) notes that: “The distinctions among adaptive stress reactions, misconduct stress behaviors, COSR casualties, PTG, and PTSD are not always clear” (pp. 1–5) as well as “Excellent combat Soldiers that have exhibited bravery and acts of heroism may also commit misconduct stress behaviors” (pp. 1–5). Although considerable overlap exists between the Department of Army’s (2009) designation of mild, moderate, and severe COSR symptoms in comparison to the Department of Navy/Marine Corps’ (2010) stress injury continuum, there is definite benefit to approaching the wide variability of COSR manifestations as a continuum versus discreet afflictions. The advantage of this designation is that it differs primarily in terms of severity and degree of impairment, as opposed to the traditional dichotomy of normal versus maladaptive reactions that has fueled the inappropriate reference to personal weakness and stigma associated with severe and chronic stress injury (Department of Navy & U.S. Marine Corps, 2010). In practical terms, however, the way different military branches triage and manage COSR is essentially the same. Emphasis is placed centrally on RTD and avoided psychiatric attrition/evacuations. Mental health treatment for severe or “red-level” stress injury, like PTSD, remains largely avoided within war zones (e.g., Department of Navy & U.S. Marine Corps, 2010).
Deferring Diagnosis of Behavioral Disorders
With regard to clinical diagnoses within war zones, its DoD policy that during assessment, COSC personnel must always consider BH disorders that resemble COSR, but defer making a psychiatric diagnosis to preserve the soldier’s expectations of normalcy and eventual RTD (e.g., Department of Army, 2009). This is also reportedly done to avoid stigma associated with BH disorders and to prevent the soldier identifying with a patient or sick role (Department of Army, 2006). Deferral is also preferred because some diagnoses require extensive history collection or documentation that is unavailable during deployment situations (such as about pre-existing personality disorders and attention deficit hyperactive disorder). Deferral of diagnosis is always preferred (e.g., Department of Army, 2006), but diagnosis can be considered if the soldier: (a) presents for reemerging symptoms of a previously diagnosed and/or treated BH disorder, (b) presents for refill prescription of psychotropic medication, (c) has a medical condition or serious BH disorder, (d) is enrolled in a reconditioning program, (e) fails to improve after having received 4 to 5 days of continuous COSC interventions and activities at hold or refer status, (f) requires individual BH treatment, or (g) is referred for multiple episodes of COSR (e.g., Department of Army, 2006). Overall, the military’s policy of deferring mental health diagnosis and treatment in war zones appears to contradict its claim that “early identification and treatment are keys to continuation of or return to duty for military members who experience mental health conditions” (ASD-HA, 2006, p. 3) to prevent chronic disability.
Preventing and Managing Combat and Operational Stress
The military’s frontline psychiatry doctrine places great emphasis on preventing and proactive management of COS to minimize war stress casualties. Leadership manuals (e.g., Department of Army, 2009) contain detailed guidance describing the importance of building individual and unit resilience through enhancing protective factors, such as cohesion and morale, leadership, and managing environmental risk and protective factors (e.g., hydration, sleep, nourishment, etc.).
Unit Cohesion and Morale
Since WWI, a major emphasis behind frontline psychiatry is the preventive role of maintaining and enhancing unit/group cohesion and morale. The military routinely cites research showing “high cohesion and morale enhance adaptive stress reactions in soldiers and organizations and are the best predictors of resiliency within a unit” as well as lowering COSR levels (Bruscher, 2011, p. 65). The “80% solution” is an Army reference to the positive impact of unit cohesion and morale in reducing COSR (Bruscher, 2011). Research on the beneficial impact of cohesion, morale, and esprit de corps on individual psychological adjustment and resilience is the most cited explanation why forward psychiatry policy of preventing psychiatric evacuation is good for individuals.
Leadership
Since WWI, the positive perception of unit leadership has been recognized as a critical protective factor. For example, a J-MHAT (2013) survey revealed that when soldiers rate both their NCOs (enlisted noncommissioned officers) and officers as being “effective,” there is a significantly lower rate (5.8%) of psychological problems showing a significant lower rate (5.8%) compared to other combinations of leadership. When soldiers rate both types of leaders as “ineffective,” there are more psychological problems (22.6%). Findings are described as “robust and evident with most outcome measures” (J-MHAT, 2013, p. 54). COSC guidance emphasizes leadership role in managing COSR, including “Strengthen (create confidence, forewarn; inoculate to extreme stress; and foster unit cohesion), Identify (know unit and individual stress load; recognize reactions, injuries, illnesses), Mitigate (Remove unnecessary stressors; ensure adequate sleep and rest; after-Action Reviews [AARs] in small groups); Treat (rest and restoration [24–72 hours]; use services of chaplains, BH/MH or medical providers as needed); Reintegrate (keep with unit if at all possible; expect return to full duty; don’t allow retribution or harassment; continuously assess fitness; communicate with treating professionals [both ways])” (Department of Navy & U.S. Marine Corps, 2010, p. 103).
Referrals of Deployed Personnel with COSR or Other Severe Reactions
Deployed personnel access COSC or behavioral health services either via voluntary referral by the affected service member or command-directed evaluation. The latter happens whenever an individual’s unit commander believes that the person’s mental state renders them a risk to self or others, or may be affecting their ability to carry out the designated mission (Department of Army, 2006).
Documentation
Per the Department of Army (2006), soldiers receiving restoration interventions must be tracked from the beginning of the process to the unit return. The tracking needs to include a record of “interventions and activities,” as well as the participant’s response (p. 10-4).
Evacuation Policy
Per Department of the Army (2006), COSR casualties who do not respond to frontline psychiatry interventions at the reconditioning level are typically medically evacuated after 7 days of reconditioning treatment. However, the theater COSC consultant is free to request permission to extend the theater evacuation policy to up to 14 days (pp. 12–13?). US Army guidance on psychiatric evacuations concludes that “Lastly, the increase in RTD is important in operations such as stability and reconstruction operations, where reducing personnel attrition becomes an important factor” (Department of the Army 2006, pp. 12–13). Contemporary frontline psychiatry/COSC models emphasize resilience building, deemphasize personal weakness, and adopt a more holistic model of authentic stress injury, harkening back to Oppenheim’s 1914 defense of the traumatic neuroses paradigm cited earlier (Lerner, 2003). For instance, in 2007, the Department of Navy and U.S. Marine Corps (2010) adopted a stress continuum model of COSC that is without stigma and focuses on resilience building in that stress injury in severe or prolonged stress lies on a spectrum between normal reactions and pathological illnesses, which is consistent with twenty-first century scientific evidence.
Conclusions
In summarizing the US military’s policy in its frontline psychiatry programs, contemporary military authors conclude that: “As future battlefields will likely look as different from OIF as OIF does from World War II, it is reassuring to know that there will be at least one constant in the provision of mental health services. That constant is the BICEPS approach to combat and operational stress reactions” (Cooper et al., 2011, p. 148). However, there has never been a systematic review of the evidence for and against the military’s beneficial claims of its frontline psychiatry doctrine for service personnel or their families. What if the military’s century-old policy of repeatedly returning traumatized personnel to war zones until the point of incapacitating stress-injury, imminent suicide, and/or legal misconduct is responsible for the pattern of wartime behavioral health crises since WWI (Russell & Figley, 2015b)? Does the frontline psychiatry policy render the DoD vulnerable to a potential class action akin to the MoD? The second part of this analysis reviews the empirical evidence in support of the military’s beneficial claims of its unchallenged mental health doctrine.
References
Acosta, J. D., Becker, A., Cerully, J. L., Fisher, M. P., Martin, L. T., Vardavas, R., … Schell, T. L. (2014). Mental health stigma in the military. Prepared for the Office of the Secretary of Defense Center for Military Health Policy Research. Santa Monica, CA: RAND.
American Psychiatric Association. (1952). Diagnostic and statistical manual of mental disorders. Washington, DC: Author.
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Artiss, K. L. (1963). Human behavior under stress: From combat to social psychiatry. Military Medicine, 128, 1011–1015.
Assistant Secretary of Defense for Health Affairs. (2006). Policy guidance on deployment-limiting psychiatric conditions and medications. Memorandum issued by William Winkenwerder, Jr., MD., to Secretary of Army, Secretary of Navy, Secretary of Air Force, and Chairman of the Joint Chiefs of Staff. Washington, DC: Pentagon.
Beard, G. (1869). Neurasthenia and nervous exhaustion. Boston Medical and Surgical Journal, 3, 217–221.
Beebe, G. W., & Appel, J. W. (1958). Variation in psychological tolerance to ground combat in World War II. Washington, DC: National Academy of Sciences.
Berlien, I. C., & Waggoner, R. W. (1966). Selection and induction. In A. J. Glass, R. J. Bernucci, & R. S. Anderson (Eds.), Neuropsychiatry in World War II: Zone of interior (Vol. I, pp. XX–XX). Washington, DC: Office of the Surgeon General, U.S. Army.
Bryant, R. A. (2007). Does dissociation further our understanding of PTSD? Journal of Anxiety Disorders, 21, 183–191.
Brill, N. Q., & Kupper, H. I. (1966). Problems of adjustment in return to civilian life. In A. J. Glass & R. J. Bernucci (Eds.), Medical Department United States Army. In Neuropsychiatry in World War II: Zone of interior (Vol. I, pp. 721–733). Washington, DC: Office of the Surgeon General, Department of the Army.
Brunner, J. (2003). Trauma in court: Medico-legal dialectics in the late nineteenth-century German discourse on nervous injuries. Theoretical Inquiries in Law, 4, 697–727.
Brusher, E. A. (2011). Combat and operational stress control. In E. C. Ritchie (Ed.), Textbooks of military medicine: Combat and operational behavioral health. Falls Church: Office of the Surgeon General, Department of the Army.
Camp, N. M. (1994). Ethical challenges for the psychiatrist during the Vietnam conflict. In F. D. Jones, L. R. Sparacino, V. L. Wilcox, & J. M. Rothberg (Eds.), Textbook of military medicine, military psychiatry: Preparing in peace for war. Washington, DC: Office of the Surgeon General, U. S. Army. Borden Institute.
Camp, N. M. (2014). U.S. army psychiatry in the Vietnam War: New challenges in extended counterinsurgency warfare. Fort Sam Huston: Borden Institute, U.S. Army Medical Department Center and School.
Chermol, B. H. (1985). Wounds without scars: Treatment of battle fatigue in the U.S. armed forces in the Second World War. Military Affairs, 49, 9–12.
Cho-Stutler, L. (2013). Staff Voices: Q & A on the Army’s Embedded Behavioral Health (EBH) Program. http://www.deploymentpsych.org/blog/staff-voices-q-army%E2%80%99s-embedded-behavioralhealth-ebhprogram. Accessed 29 August 2013.
Cohen, S. P., Brown, C., Kurihara, C., Plunkett, A., Nguyen, C., & Strassels, S. A. (2010). Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: A prospective cohort study. Lancet, 375, 301–309.
Cooper, M. A., Newton, S. M., & Yarvis, J. S. (2011). Provision of mental health services in Operation Iraqi Freedom 04-07. In E. C. Ritchie (Ed.), Textbooks of military medicine, combat and operational behavioral health. Falls Church: Office of the Surgeon General, Department of the Army.
Da Costa, J. M. (1871). On irritable heart: A clinical study of a form of functional cardiac disorder and its consequences. American Journal of Medicine, 11, 559–567 (Reprinted in 1951).
Daubert v. Merrell Dow Pharmaceuticals. (1993). 509 U.S. 579.
Dean, E. T. (1997). Shook over hell: Post-traumatic stress Vietnam and the Civil war. Cambridge, MA: Harvard University Press.
Department of Defense. (2013). Maintenance of psychological health in military operations. DoD instruction 6490.05 of October 2, 2013. Washington, DC: Defense Logistics Agency.
Department of Defense Task Force on Mental Health. (2007). An achievable vision: Report of the Department of Defense Task Force on Mental Health. Falls Church: Defense Health Board.
Department of Navy. (2015). OPNAVINST 6520.1. Operational stress control program. Defense Logistics Agency N17. Washington, DC: Chief of Naval Operations. Retrieved from https://doni.daps.dla.mil/Directives/…/6520.1.pdf
Department of Navy and U.S. Marine Corps. (2010). Combat and operational stress control. U.S. Navy, NTTP 1-15M; U.S. Marine Corps, MCRP 6-11C. Washington, DC.
Department of the Army. (1994). Leader’s manual for combat stress control: Field manual (pp. 22–51). Washington, DC: Headquarters.
Department of the Army. (2006). Combat and operational stress control: Field manual 4-02.51 (FM 8-51). Washington, DC: Headquarters, Department of the Army.
Department of the Army. (2009). Combat and operational stress control manual for leaders and soldiers: Field manual 6-22.5 (FM 6-22.5). Washington, DC: Headquarters, Department of the Army.
Department of Veterans Affairs. (2015). Analysis of VA Health Care Utilization among Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn Veterans, from 1st Qtr FY 2002 through 1st Qtr FY 2015. Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration. Washington, DC: Author. Retrieved from http://www.publichealth.va.gov/epidemiology
Department of Veterans Affairs & Department of Defense. (2004). VA/DoD clinical practice guideline for the management of post-traumatic stress. Washington, DC: Veterans Health Administration, Department of Veterans Affairs and Health Affairs, Department of Defense. Office of Quality and Performance publication 10Q-CPG/PTSD-04.
Department of Veterans Affairs & Department of Defense. (2010). VA/DoD clinical practice guideline for the management of post-traumatic stress. Washington, DC: Veterans Health Administration, Department of Veterans Affairs and Health Affairs, Department of Defense. Office of Quality and Performance publication 10Q-CPG/PTSD-10.
Dohrenwend, B. P., Yager, T. J., Wall, M. M., & Adams, B. G. (2013). The roles of combat exposures, personal vulnerability, and involvement in harm to civilians or prisoners in Vietnam War-related posttraumatic stress disorder. Clinical Psychology Science, 1, 223–238.
Drayer, C. S., & Glass, A. J. (1973). Introduction. In W. S. Mullins & A. J. Glass (Eds.), Neuropsychiatry in World War II: Overseas theaters. Washington, DC: Office of the Surgeon General, U.S. Army.
Erichsen, J. E. (1866). On railway and other injuries of the nervous system. London: Walton & Maberly.
Fear, N. T., Jones, M., Murphy, D., Hull, L., Iversen, A. C., Coker, B., … Wessely, S. (2010). What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet, 375, 1783–1797.
Friedman, M. (2004). PBS frontline: The soldier’s heart. Retrieved from: http://www.pbs.org/wgbh/pages/frontline/shows/heart/interviews/friedman.html
Friedman, M. J., Keane, T. M., & Resick, P. A. (2014). Handbook of PTSD: Science and practice (2nd ed.). New York: Guilford Press.
Glass, A. J. (1966a). Introduction: Army psychiatry before World War II. In R. S. Anderson, A. J. Glass, & R. J. Bernucci (Eds.), Neuropsychiatry in World War II: Zone of interior (Vol. I, pp. 3–19). Washington, DC: Office of the Surgeon General, U.S. Army.
Glass, A. J. (1966b). Lessons learned. In R. S. Anderson, A. J. Glass, & R. J. Bernucci (Eds.), Neuropsychiatry in World War II: Zone of interior (Vol. I, pp. 335–359). Washington, DC: Office of the Surgeon General, U.S. Army.
Glynn. T. R. (1910). The traumatic neuroses. The Lancet, 1332–1336.
Government Accountability Office. (2010). Defense health care: Status of efforts to direct lack of compliance with personality disorder separation requirements. GAO-10-1013T. Washington, DC: Author.
Government Accountability Office. (2016). Human capital: Additional actions needed to enhance DoD’s efforts to address mental health care stigma. GAO-16-404. Washington, DC: Author.
Hanson, F. R. (Ed.). (1949). Combat psychiatry: Experiences in the North African and Mediterranean theaters of operation American ground forces, World War II. Honolulu, HI: U.S. Army Medical Department. University Press of Pacific.
Holden, W. (1998). Shell shock: The psychological impact of war. London: Macmillan.
Holmes, G. (1939). Report of conference (PRO, PIN15/2402/15B, 10 November 1939, p. 12). Cited in Jones, E., & Wessely, S. W. (2007).
Howe, E. G., & Jones, F. D. (1994). Ethical issues in combat psychiatry. In F. D. Jones, L. R. Sparacino, V. L. Wilcox, & J. M. Rothberg (Eds.), Textbook of military medicine, military psychiatry: Preparing in peace for war (pp. XXX–XXX). Washington, DC: Office of the Surgeon General, U. S. Army. Borden Institute.
Institute of Medicine. (2007). PTSD compensation and military service. Committee on Veteran’s Compensation for Posttraumatic Stress Disorder. Washington, DC: The National Academies Press.
Institute of Medicine. (2008). Gulf War and health: Physiologic, psychologic and psychosocial effects of deployment-related stress (Vol. 6). Washington, DC: The National Academies Press.
Institute of Medicine. (2014). Preventing psychological disorders in service members and their families: An assessment of programs. Washington, DC: The National Academies Press.
Johnson, W., & Rows, R. G. (1923). Neurasthenia and war neuroses. In W. G. Macpherson, W. P. Herringham, T. R. Elliott, & A. Balfour (Eds.), History of the Great War based on official documents, medical services, diseases of the war (Vol. 2, pp. 2–61). London: HMSO.
Joint Mental Health Advisory Team-7. (2011, February 22). Operation enduring freedom 2010 Afghanistan. Office of the Surgeon General United States Army Medical Command and Office of the Command Surgeon HQ, USCENTCOM and Office of the Command Surgeon U.S. Forces Afghanistan (USFOR-A).
Joint Mental Health Advisory Team-8. (2013, August 12). Operation enduring freedom 2013 Afghanistan. Office of the Surgeon General United States Army Medical Command and Office of the Command Surgeon HQ, USCENTCOM and Office of the Command Surgeon U.S. Forces Afghanistan (USFOR-A).
Jones, F. D. (1995a). Psychiatric lessons of war. In R. Zatchuk & R. F. Bellamy (Eds.), Textbook of military medicine: War psychiatry (pp. 1–34). Washington, DC: Office of the Surgeon General, U. S. Army, Borden Institute.
Jones, F. D. (1995b). Psychiatric lessons of war. In R. Zatchuk & R. F. Bellamy (Eds.), Textbook of military medicine: War psychiatry (pp. XXX–XXX). Washington, DC: Office of the Surgeon General, U. S. Army. Borden Institute.
Jones, E., & Wessely, S. (2003). Forward psychiatry in the military: Its origin and effectiveness. Journal of Traumatic Stress, 16, 411–419.
Jones, E., & Wessely, S. (2007). A paradigm shift in the conceptualization of psychological trauma in the 20th century. Journal of Anxiety Disorders, 21, 164–175.
Jones, E., Thomas, A., & Ironside, S. (2007). Shell shock: an outcome study of a first world war ‘PIE’ unit. Psychological Medicine, 37, 215–23
Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R., & Weiss, D. S. (1990). Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel.
Kullmann, D. M. (Ed.). (1922). Report of the war office committee of enquiry into “shell shock”. London: Imperial War Museum.
Lande, R. G. (2003). Madness, malingering & malfeasance. Washington, DC: Potomac Books.
Larson, G. E., Hammer, P. S., Conway, T. L., Schmied, E. A., Galarneau, M. R., Konoske, P., … Johnson, D. C. (2011). Predeployment and in-theater diagnoses of American military personnel serving in Iraq. Psychiatric Services, 62(1), 15–21.
Leese, P. (2002). Shell shock: Traumatic neurosis and the British soldiers of the First World War. New York: Palgrave Macmillan.
Lerner, P. (2003). Hysterical men: War, psychiatry, and the politics of trauma in Germany (pp. 1890–1930). London: Cornell University Press.
Lilienfeld, S. O. (2005). The 10 commandments of helping students distinguish science from pseudoscience in psychology. APS Observer, 18, 1–6. Retrieved from: http://www.psychologicalscience.org/observer/getArticle.cfm?id=1843
Martin, J. A., & Cline, W. R. (1996). Mental health lessons from the Persian Gulf War. In J. A. Martin, L. R. Sparacino, & G. Belenky (Eds.), The Gulf War and mental health: A comprehensive guide (pp. 161–178). Westport: Praeger.
McGeorge, T., Hughes, J. H., & Wessely, S. (2006). The MoD PTSD decision: A psychiatric perspective. Occupational Health Review, 122, 21–28.
Menninger, W. C. (1948). Reactions to combat. Psychiatry in a troubled world (pp. 134–152). New York: Macmillan.
Mental Health Advisory Team-I. (2003). MHAT Operation Iraqi Freedom. U.S. Army Surgeon General.
Mental Health Advisory Team-II. (2005). Operation Iraqi Freedom-II, Mental Health Advisory Team (MHAT-II). U.S. Army Surgeon General.
Mental Health Advisory Team-III. (2006). Mental Health Advisory Team (MHAT-III), Operation Iraqi Freedom 04-06. Office of the Surgeon Multinational Force-Iraq & Office of the Surgeon General, United States Army Medical Command.
Mental Health Advisory Team-IV. (2006). Mental Health Advisory Team (MHAT-IV) Operation Iraqi Freedom 05-07. Office of the Surgeon Multinational Force-Iraq & Office of the Surgeon General, United States Army Medical Command.
Mental Health Advisory Team-V. (2008), Mental Health Advisory Team (MHAT-V) Operation Enduring Freedom 06-08. Office of the Surgeon Multinational Force-Iraq & Office of the Surgeon General, United States Army Medical Command.
Mental Health Advisory Team-VI. (2009). Mental Health Advisory Team (MHAT-6) Operation Enduring Freedom 2009 Afghanistan. Office of the Command Surgeon US Forces Afghanistan (USFOR-A) and Office of the Surgeon General, United States Army Medical Command.
Myers, C. S. (1915). Contributions to the study of shell shock. The Lancet, I, 316–320.
Myers, C. S. (1940). Shell shock in France: 1914–1918. London: Cambridge University Press.
Nash, W. P. (2011). U.S. Marine Corps and Navy combat and operational stress continuum model: A tool for leaders. In E. C. Ritchie (Ed.), Textbooks of military medicine, combat and operational behavioral health (pp. XXX–XXX). Falls Church: Office of the Surgeon General, Department of the Army.
Oppenheim, H. (1889). Die traumatischen neurosen. Berlin: Hirschwald.
Palinkas, L. A., & Cohen, P. (1987). Psychiatric disorders among United States Marines wounded in action in Vietnam. Journal of Nervous Mental Disease, 175, 291–300.
Rabasca, L. (2000). More psychologists in the trenches. APA Monitor, 31, 50. Retrieved from: http://www.apa.org/monitor/jun00/trenches.aspx
Ranson, S. W. (1949). The normal battle reaction. In F. R. Hanson (Ed.), Combat psychiatry, special supplement, the bulletin of the U.S. Army Medical Department (Vol. IX).
Ritchie, E. C. (2002). Psychiatry in the Korean War: Perils, PIES, and prisoners of war. Military Medicine, 167, 898–903.
Russell, M. C., Butkus, S., & Figley, C. R. (2016a). Contribution of military organization and leadership factors in perpetuating generational cycle of preventable wartime mental health crises: Part one. Psychological Injury and Law, 9, 55–72.
Russell, M. C., Butkus, S., & Figley, C. R. (2016b). Is it time for a behavioral health corps? Ending the generational cycle of preventable wartime mental health crises—Part 2. Psychological Injury and Law, 9, 73–86.
Russell, M. C., & Figley, C. R. (2015a). Generational wartime behavioral health crises: Part one of a preliminary analysis. Psychological Injury and Law, 8, 106–131.
Russell, M. C., & Figley, C. R. (2015b). Investigating recurrent generational wartime behavioral health crises: Part 2 of a preliminary analysis. Psychological Injury and Law, 8, 132–152.
Russell, M. C., Figley, C. R., & Robertson, K. R. (2015). Investigating the psychiatric lessons of war and pattern of preventable wartime behavioral health crises. Journal of Psychology and Behavioral Science, 3, 1–16.
Russell, M. C., Zinn, B., & Figley, C. R. (2016). Exploring options including class action to transform military mental healthcare and ends the generational cycle of preventable wartime behavioral health crises. Psychological Injury and Law, 9, 166–197.
Salmon, T. W. (1917). The care and treatment of mental diseases and war neuroses (‘shell shock’) in the British Army. Mental Hygiene, 1, 509–547.
Shepard, B. (2001). A war of nerves: Soldiers and psychiatrists in the twentieth century. Cambridge: Harvard University Press.
Solomon, Z., Shklar, R., & Mikulincer, M. (2005). Frontline treatment of combat stress reaction: A 20-year longitudinal study. The American Journal of Psychiatry, 162, 2319–2314.
Stouffer, S. A., Lumsdaine, A. A., Lumsdaine, M. H., Williams, R. M., Smith, M. B., Janis, I. L., … Cottrell, L. S. (1949). The American soldier: Combat and its aftermath volume 2. New Jersey: Princeton University Press.
Strecker, E. A. (1919). Experiences in the immediate treatment of war neuroses. American Journal of Insanity, 76, 45–69.
U.S. Army (2013). Ready and Resilient Campaign: Embedded Behavioral Health. http://www.army.mil/standto/archive_2013-08-13. Accessed 7 January 2013.
U.S. War Department (1944). War department technical bulletin (TB-MED)-80 convalescent treatment program for neuropsychiatric patients. Published on 30 August 1944 by Surgeon General’s Office, Washington, DC.
Wanke, P. (2005). Russian/Soviet military psychiatry: 1904–1945. London: Frank Cass.
Wooley, C. F. (2002). The irritable heart of soldiers and the origins of Anglo-American cardiology. London: Ashgate.
Acknowledgements
We thank David Gellman for his assistance with the literature review. This study was unfunded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s12207-017-9283-9.
Rights and permissions
About this article
Cite this article
Russell, M.C., Figley, C.R. Do the Military’s Frontline Psychiatry/Combat and Operational Stress Control Doctrine Help or Harm Veterans?—Part One: Framing the Issue. Psychol. Inj. and Law 10, 1–23 (2017). https://doi.org/10.1007/s12207-016-9278-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12207-016-9278-y