Abstract
A conditioning regimen with fludarabine and myeloablative dose of busulfan (FLU/BU4) has been commonly used in allogeneic hematopoietic cell transplantation (allo-HCT). However, there are two major problems with this regimen: insufficient anti-leukemic effect, especially in advanced cases, and slow time to complete donor-type chimerism, especially T-cell chimerism. To overcome these issues, we designed a combination regimen with FLU (150 mg/m2), intravenous BU (12.8 mg/kg), and melphalan (100 mg/m2) (FLU/BU4/MEL) and conducted retrospective analyses of treatment outcomes at our institute. Forty-two patients with myeloid malignancies received allogeneic bone-marrow transplantation or peripheral blood stem-cell transplantation (allo-BMT/PBSCT) with FLU/BU4/MEL regimen. The median age of patients was 46.5 years (20–63 years). Thirteen patients (31%) did not achieve complete hematological remission at transplantation. All patients examined achieved complete whole and T-cell chimerism within 1 month after allo-HCT. The 4-year overall survival and disease-free survival rates were 66.0% [95% confidence interval (CI) 49.4–78.3%] and 59.5% (95% CI 43.2–72.6%) in all patients, and 49.4% (95% CI 19.7–73.6%) and 38.5% (95% CI 14.1–62.8%) in patients who were not in remission. In conclusion, FLU/BU4/MEL showed curative potential, even in patients with advanced myeloid malignancies, accompanied by achievement of rapid complete chimerism after allo-BMT/PBSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decade, a combination regimen with fludarabine and myeloablative dose of busulfan (FLU/BU4) has been widely used as a reduced intensity myeloablative conditioning regimen for myeloid malignancies, and it is applicable even to elderly patients [1,2,3]. The FLU/BU4 regimen retained anti-leukemic effects with lower transplant-related mortality than that by busulfan and cyclophosphamide (BU/CY), especially in patients with stable disease [4,5,6,7]. However, FLU/BU4 has two major disadvantages. The first is insufficient anti-leukemic effect in advanced cases [1, 8]. Although overall survival (OS) after FLU/BU4 treatment is up to 50–80% for myeloid malignancies in the first complete remission (CR) [1, 7, 8], the regimen has resulted in unsatisfactory outcomes with 19–32% OS in patients with advanced disease [1, 8]. The second disadvantage is the slow achievement of complete donor-type chimerism, especially T-cell chimerism [4], which also affects the outcome of allo-SCT, especially relapse [8,9,10]. The rate of complete donor T-cell chimerism at day 30 after transplantation was significantly lower in the FLU/BU4 group than in the BU/CY group (42% vs. 83%, p = 0.00026) [4].
To overcome these disadvantages, we formulated a new conditioning regimen, FLU/BU4/MEL, in which melphalan 100 mg/m2 was added to FLU/BU4 for myeloid malignancies. Since 2009, 42 patients have been treated with this regimen in our institute. In this study, we conducted a retrospective evaluation of the efficacy and safety of FLU/BU4/MEL.
Patients and methods
Patients and study design
Patients who were > 45 years of age and/or with higher comorbidity risks, such as higher hematopoietic cell transplantation-specific comorbidity index (HCT-CI), received the FLU/BU4/MEL regimen. Among 56 patients who received FLU/BU4/MEL conditioning between January 2009 and March 2016 in our institute, 42 with myeloid malignancies who underwent allogeneic bone-marrow transplantation (BMT) or peripheral blood stem-cell transplantation (PBSCT) were retrospectively reviewed. Patients who underwent a second transplantation, had lymphoid malignancies, underwent cord blood transplantation (CBT), and had excessive reduction or increase in anti-tumor drugs were excluded. Our study complied with the Declaration of Helsinki, and was approved by the institutional review board of the Osaka University Hospital (approval number: 16265). Written informed consent was obtained from all patients analyzed in this study.
Conditioning regimen
The conditioning regimen comprised 30 mg/m2 FLU for 5 days (150 mg/m2), 3.2 mg/kg BU for 4 days (12.8 mg/kg), and 50 mg/m2 MEL for 2 days (100 mg/m2) administered by intravenous (IV) infusion. Total body irradiation (TBI) of 3 Gy was given to patients in cases of unrelated transplantation, and 5 mg/kg anti-thymocyte globulin (ATG, thymoglobuline®) was added for human leukocyte antigen (HLA)-mismatch transplantation. Dose reduction of anti-tumor drugs was permitted; 80 mg/m2 MEL for elderly patients (aged ≥ 60 years) and/or 9.6 mg/kg BU for patients with liver damage (alanine transaminase > 2.5 N, hepatitis B virus antigen positive, hepatitis C virus antibody positive, and/or liver hemosiderosis).
Graft vs. host disease prophylaxis
Most of the patients received standard prophylaxis of graft vs. host disease (GVHD) with IV tacrolimus (FK506; 0.015 mg/kg/day, starting on day − 1) or IV cyclosporin A (3 mg/kg/, starting on day − 1) and IV methotrexate (MTX) (10 mg/m2 on day 1 and 7 mg/m2 on days 3 and 6).
Transplantation procedure and supportive care
All patients were treated in HEPA-filtered rooms and received fungal, herpes simplex virus, bacterial, and Pneumocystis jiroveci prophylaxis. Cytomegalovirus (CMV) reactivation was monitored by CMV pp65 antigenemia assay (C7-HRP) at least once a week. Preemptive therapy (ganciclovir, valganciclovir, or foscarnet) was administered to patients in case of CMV reactivation. Oral valproic acid was started on the day before BU therapy and continued until the day of final BU administration.
Toxicity was scored using the Common Terminology Criteria for Adverse Events version 4.0 (NCI, Bethesda, MD).
Engraftment and chimerism
The time of neutrophil engraftment was considered the first of three successive days with an absolute neutrophil count of ≥ 500/µL during recovery after transplantation and time of platelet engraftment was defined as the first day with a platelet count of ≥ 2 × 104/µL during recovery without platelet transfusion.
The chimerism status after transplantation was determined using either quantitative polymerase chain reaction analysis for microsatellite DNA markers or fluorescent in situ hybridization of X and Y chromosomes. The chimeric status of T lymphocytes was analyzed after positive selection of CD3-positive cells using Dynabeads™ CD3 (Thermo Fisher Scientific) or RosetteSep™ Human T-Cell Enrichment Cocktail (STEMCELL Technologies). Complete donor chimerism was defined as the presence of more than 95% of donor cells.
GVHD assessment and treatment
Patients who achieved neutrophil engraftment were evaluable for acute GVHD according to the standard criteria [12]. Patients were evaluable for chronic GVHD if engraftment occurred and the patient survived 100-day post-transplantation. The diagnosis of chronic GVHD and the grades of chronic GVHD were based on the National Institute of Health criteria [13].
Corticosteroids usually comprised the first-line therapy for acute (grades II–IV) and moderate–severe chronic GVHD. The second-line treatment was at the discretion of treating physicians.
Statistical analyses
Survival probability was estimated by Kaplan–Meier method. The log-rank test was used to compare survival probability between subgroups of patients. The cumulative incidence of non-relapse mortality (NRM) was estimated by considering death due to disease relapse and/or resistance, or any other nontreatment-related cause as a competing risk. The landmark method was used to evaluate the effect of GVHD on OS and cumulative incidence of relapse and NRM among patients who were alive at 60 days for acute GVHD and at 100 days for chronic GVHD after transplantation. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [14]. The results with p values < 0.05 were deemed statistically significant.
Results
Patient characteristics
Between January 2009 and March 2016, 42 patients, including 33 with acute myeloid leukemia (AML) and 9 with myelodysplastic syndromes, received the FLU/BU4/MEL conditioning regimen. The characteristics of these patients are shown in Table 1. The median patient age at transplantation was 46.5 years (range, 20–63 years) and the median follow-up was 1513.5 days (range, 214–2975 days). Approximately one-third of the patients had adverse/poor/very poor karyotypes [15] and high/very high disease risk index (DRI) [16]. Furthermore, 29 patients (69%) were in hematological CR at transplantation and 13 (31%) were not in CR. The HCT-CI score was high (≥ 3) in 12 (29%) patients. All patients received BMT or PBSCT after the conditioning regimen. Only three patients required dose reduction: MEL 80 mg/m2 for 2 patients and MEL 80 mg/m2 plus BU 9.6 mg/kg for 1 patient.
Engraftment and chimerism
The rate of neutrophil and platelet engraftment was 100% and 95.2% [95% confidence interval (CI) 81.6–98.8%] and the median time for engraftment was 19 days (13–30 days) and 25 days (14–108 days), respectively. Among the patients, whose chimerism was examined on day 28 after transplantation (n = 32), donor chimerism in whole blood was achieved in all the tested patients. In addition, we confirmed the achievement of donor-type complete chimerism in the T-cell fraction in half of the tested patients (n = 16).
Toxicity
The frequency of grade 3 to 4 regimen-related toxicity (RRT) occurring during the first 20 days after transplantation are listed in Table 2. The most frequent toxicities were febrile neutropenia and oral/pharyngeal mucositis. Although there was no occurrence of sinusoidal obstruction syndrome, thrombotic microangiopathy occurred in four (10%) patients. The cumulative incidence of grade II–IV and grade III–IV acute GVHD at day 100 + was 42.2% (95% CI 25.0–55.6%) and 22.7% (95% CI 8.0–35.1%), respectively, and the cumulative incidence of moderate to severe and severe chronic GVHD was 33.0% (95% CI 14.4–53.0%) and 13.5% (95% CI 3.3–30.9%), respectively.
Overall survival, disease-free survival, non-relapse mortality, and relapse rate
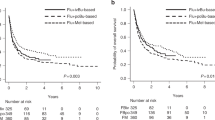
At the last follow-up, 28 of 42 patients were alive. Fourteen patients died because of infection (n = 9: bacterial 8 and viral 1), primary disease (n = 2), interstitial pneumonia (n = 2), and thrombotic microangiopathy (n = 1) (Table 2). The 1-year OS, disease-free survival (DFS), NRM, and relapse rate (RR) in all patients were 73.7% (95% CI 57.5–84.5%), 66.7% (95% CI 50.3–78.7%), 19.0% (95% CI 8.8–32.2%), and 14.3% (95% CI 5.7–26.7%), respectively. The 4-year OS, DFS, NRM, and RR were 66.0% (95% CI 49.4–78.3%), 59.5% (95% CI 43.2–72.6%), 19.0% (95% CI 10.2–32.1%), and 21.4% (95% CI 10.5–34.9%), respectively (Fig. 1a–c). In patients who had not been in remission at the time of allo-HCT, the 4-year OS, DFS, NRM, and RR were 49.4% (95% CI 19.7–73.6%) (Fig. 2), 38.5% (95% CI 14.1–62.8%), 7.7% (95% CI 0.4–30.4%), and 53.8% (95% CI 22.8–77.2%), respectively. In contrast, the 4-year OS and DFS of patients who had been in remission at the time of allo-HCT were 72.4% (95% CI 52.3–85.1%) (Fig. 2) and 69.0% (95% CI 48.8–82.5%), respectively. Although the relapse incidence in patients who had been in CR at allo-HCT was exceedingly low [1-year 0.0% (95% CI 0.0–0.0%); 4-year 3.4% (95% CI 0.2–15.4%)] (Fig. 3a), the NRM after HCT in this group was comparatively high [1-year, 24.1% (95% CI 10.4–40.9%) and 4-year, 27.6% (95% CI 12.8–44.6%)] (Fig. 3b).
Univariate analysis of risk factors for OS of patients in CR
To elucidate the risk factors that affected the outcome of patients who had been in CR at transplantation, we conducted univariate analysis. Table 3 summarizes the results. Despite the intensification of conditioning regimen, higher HCT-CI (≥ 3) did not negatively affect the outcome in patients. However, grade II–IV acute GVHD exhibited significant negative correlation on the OS.
Discussion
We formulated a new FLU/BU4/MEL regimen with the aim to improve the performance of FLU/BU4 by adding MEL, and this regimen has been in clinical practice since 2009 in our institute. In this study, we retrospectively evaluated the efficacy and safety of FLU/BU4/MEL regimen in patients with myeloid malignancies following BMT or PBSCT. The results showed excellent outcomes, even in the relapsed/refractory state.
In recent years, the efficacy of combination regimen with FLU, BU, and MEL for myeloid malignancy has been examined and reported independently from several institutes. Two pediatric hematology groups demonstrated the safety and efficacy of a regimen with FLU, BU, and MEL for AML at childhood or adolescence following transplantation [17, 18]. In addition, another group evaluated the effectiveness of a conditioning regimen with FLU, BU, and MEL in adult patients with myeloid malignancies who underwent CBT [19]. The results showed that, besides reduced toxicity, the conditioning treatment was highly effective as a CBT conditioning regimen in myeloid malignancies, even in elderly patients who were not in remission; the 2-year OS and progression-free survival (PFS) were both 54.9%, and the 2-year NRM was 25.5% [19]. Although the FLU/BU4/MEL regimen in our study was not identical to regimens in other studies, the overall treatment outcomes were in line with those in other studies.
The addition of MEL to the original FLU/BU4 regimen benefits clinical practice in at least two ways. First, it intensifies the conditioning effects against myeloid malignancies. Although MEL is not administered in conventional chemotherapies, such as induction, consolidation, and maintenance therapy, it is known as an effective anti-tumor drug for myeloid malignancies and is often included in conditioning regimens. Indeed, a conditioning regimen with FLU and MEL (FLU/MEL) has been reported to achieve good outcomes for myeloid malignancies [20,21,22]. The FLU/BU4 regimen resulted in insufficient outcomes, with 19–32% OS in patients with advanced disease [1, 8]. However, our FLU/BU4/MEL regimen demonstrated superior overall outcomes, with 49.4% 4-year OS in patients with no complete hematological remission (non-CR). Patients with high/very high DRI also showed satisfactory outcomes with 38.1% (95% CI 13.1–63.2%) 4-year OS. These results indicated the improvement in the OS of patients with uncontrolled disease by the addition of MEL to FLU/BU4. Furthermore, the FLU/BU4/MEL regimen results in faster achievement of complete donor chimerism than that by FLU/BU4 [4]. Although the proportion of complete donor T-cell chimerism at day 30 with the FLU/BU4 regimen was as low as 42% [4], FLU/BU4/MEL resulted in complete T-cell chimerism within 30 days in all tested patients. The rapid achievement of donor-type complete chimerism, particularly T-cell chimerism, is extremely important, because it affects the outcome of allo-HCT, especially by reducing disease relapse [8,9,10]. Therefore, immediate reconstitution of the immune system with donor-derived T cells is desirable to improve the OS and DFS of patients with myeloid malignancy undergoing transplantation.
A disadvantage of the FLU/BU4/MEL regimen is the relatively high NRM, especially in patients in remission, which mainly occurred within 1 year. A retrospective study comparing FLU/BU2 and FLU/BU4 for AML in the first CR showed that in patients aged < 50 years, the 2-year OS and leukemia-free survival (LFS) were not different between the two regimens. Nevertheless, in patients aged ≥ 50 years, the 2-year OS and LFS after FLU/BU2 were superior to those after FLU/BU4 because of the lower incidence of NRM [23]. A high-intensity regimen is necessary for refractory or relapsed leukemia; a less intensified regimen would be enough for patients in a stable disease state, particularly in the first CR. To improve the outcomes of our FLU/BU4/MEL regimen, we should try to minimize toxicities, especially in patients with stable disease. The most problematic and life-threatening toxicity of FLU/BU4/MEL was bacterial infection, which was closely related to high incidence of mucositis. Given the very low incidence of relapse in stable patients (Fig. 3), the FLU/BU4/MEL regimen can be modified to reduce NRM in such cases. In this respect, dose reduction from 4 to 2–3 days for BU treatment and/or 100 mg to 80 mg for MEL might reduce toxicities without reducing the anti-leukemic effect in stable disease. The pharmacokinetic-targeted dose adjustment of BU can contribute to the reduction in toxicities [24]. In addition, we should also pay attention to acute GVHD. The achievement of T-cell chimerism strongly correlates with the occurrence of acute GVHD [25, 26]. In fact, we experienced higher incidence of grade II–IV acute GVHD than that with FLU/BU4 [4], which affected the OS of patients in CR (Table 3). Although acute GVHD was not a direct cause of death, mucosal damage due to acute GVHD and the intensification of immuno-suppressive therapy, coupled with the severe mucositis, occurred as RRT, causing life-threatening infection in some cases. Intensification of GVHD prophylaxis should also be pursued to improve outcomes. Moreover, the use of mycophenolate mofetil instead of MTX would help to reduce mucositis [27,28,29]. In contrast, higher HCT-CI score did not negatively affect the OS of patients in our study. This indicates that HCT-CI might not correctly reflect the comorbidity risk of FLU/BU4/MEL. It was partly because we reduced the dosage of BU for patients with liver damage, which was included in the HCT-CI score and should be closely related to the toxicity of FLU/BU4/MEL. Based on these results, we should further examine the way of reducing NRM.
There were certain limitations to this study. First, this is a retrospective, small-scale, single-arm cohort study, and therefore, the effect of addition of MEL was not statistically determined. A large-scale, prospective, randomized study comparing FLU/BU4/MEL and FLU/BU4 might solve this issue. In addition, we lack the information on molecular aberrations of leukemic cells, such as NPM1, internal tandem duplication of FLT3, and c-KIT, which might also influence the outcome [30,31,32]. Second, we cannot ignore the influence of ATG and TBI, which were added for HLA-mismatch transplantation and for unrelated transplantation, respectively. The addition of ATG might have enhanced the chimerism status after transplantation. However, in the CBT setting, in which we experienced engraftment failure more frequently than that in the BMT and PBSCT setting, the FLU/BU4/MEL regimen resulted in complete donor T-cell chimerism within 3 weeks among all patients [19]. Therefore, FLU/BU4/MEL might have resulted in rapid complete donor-type chimerism even in BMT and PBSCT cases without ATG, and this should also be applicable to the case of TBI. We administered 3 Gy TBI for unrelated transplantation to promote complete donor-type chimerism, because insufficient achievement of complete donor-type chimerism was reported in the FLU/BU4 regimen. Nevertheless, the results shown in CBT [19] indicated that TBI is not necessarily required for complete chimerism achievement with the FLU/BU4/MEL regimen. Conversely, TBI is known to cause oral/pharyngeal mucositis, and it might have increased the frequency and severity of mucositis in our study. Thus, the need for ATG and TBI in addition to FLU/BU4/MEL remains to be addressed in the future and should be carefully considered depending on the circumstances in each case.
In conclusion, the FLU/BU4/MEL regimen is a promising strategy, with high curative potential in BMT and PBSCT, even for uncontrolled myeloid malignancies in adults. To optimize the doses of BU and MEL, and GVHD prophylaxis with fewer therapy-related toxicities, further studies should be conducted in the future.
References
Alatrash G, de Lima M, Hamerschlak N, Pelosini M, Wang X, Xiao L, et al. Myeloablative reduced-toxicity i.v. busulfan-fludarabine and allogeneic hematopoietic stem cell transplant for patients with acute myeloid leukemia or myelodysplastic syndrome in the sixth through eighth decades of life. Biol Blood Marrow Transplant. 2011;17(10):1490–6.
de Lima M, Couriel D, Thall PF, Wang X, Madden T, Jones R, et al. Once-daily intravenous busulfan and fludarabine: clinical and pharmacokinetic results of a myeloablative, reduced-toxicity conditioning regimen for allogeneic stem cell transplantation in AML and MDS. Blood. 2004;104(3):857–64.
Chunduri S, Dobogai LC, Peace D, Saunthararajah Y, Quigley J, Chen YH, et al. Fludarabine/i.v. BU conditioning regimen: myeloablative, reduced intensity or both? Bone Marrow Transplant. 2008;41(11):935–40.
Rambaldi A, Grassi A, Masciulli A, Boschini C, Micò MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16(15):1525–36.
Eapen M, Brazauskas R, Hemmer M, Perez WS, Steinert P, Horowitz MM, et al. Hematopoietic cell transplantat for acute myeloid leukemia and myelodysplastic syndrome: conditioning regimen intensity. Blood Adv. 2018;2(16):2095–103.
Ben-Barouch S, Cohen O, Vidal L, Avivi I, Ram R. Busulfan fludarabine vs busulfan cyclophosphamide as a preparative regimen before allogeneic hematopoietic cell transplantation: systematic review and meta-analysis. Bone Marrow Transplant. 2015;51(2):232–40.
Liu H, Zhai X, Song Z, Sun J, Xiao Y, Nie D, et al. Busulfan plus fludarabine as a myeloablative conditioning regimen compared with busulfan plus cyclophosphamide for acute myeloid leukemia in first complete remission undergoing allogeneic hematopoietic stem cell transplantation: a prospective and multicenter study. J Hematol Oncol. 2013;6:15.
Shimoni A, Hardan I, Shem-Tov N, Yerushalmi R, Nagler A. Allogeneic hematopoietic stem-cell transplantation in AML and MDS using myeloablative versus reduced-intensity conditioning: long-term follow-up. Leukemia. 2010;24(5):1050–2.
Saito B, Fukuda T, Yokoyama H, Kurosawa S, Takahashi T, Fuji S, et al. Impact of T cell chimerism on clinical outcome in 117 patients who underwent allogeneic stem cell transplantation with a busulfan-containing reduced-intensity conditioning regimen. Biol Blood Marrow Transplant. 2008;14(10):1148–55.
Koreth J, Kim HT, Nikiforow S, Milford EL, Armand P, Cutler C, et al. Donor chimerism early after reduced-intensity conditioning hematopoietic stem cell transplantation predicts relapse and survival. Biol Blood Marrow Transplant. 2014;20(10):1516–21.
Peterlin P, Delaunay J, Guillaume T, Gastinne T, Mahé B, Dubruille V, et al. Complete donor T cell chimerism predicts lower relapse incidence after standard double umbilical cord blood reduced-intensity conditioning regimen allogeneic transplantation in adults. Biol Blood Marrow Transplant. 2015;21(1):180–4.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Bone Marrow Transplant. 1995;15(6):825–8.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11(12):945–56.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2012;48(3):452–8.
Schanz J, Tuchler H, Sole F, Mallo M, Luno E, Cervera J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30(8):820–9.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123(23):3664–71.
Ishida H, Adachi S, Hasegawa D, Okamoto Y, Goto H, Inagaki J, et al. Comparison of a fludarabine and melphalan combination-based reduced toxicity conditioning with myeloablative conditioning by radiation and/or busulfan in acute myeloid leukemia in Japanese children and adolescents. Pediatr Blood Cancer. 2015;62(5):883–9.
Jaiswal SR, Chakrabarti A, Chatterjee S, Bhargava S, Ray K, O’Donnell P, et al. Haploidentical peripheral blood stem cell transplantation with post-transplantation cyclophosphamide in children with advanced acute leukemia with fludarabine-, busulfan-, and melphalan-based conditioning. Biol Blood Marrow Transplant. 2016;22(3):499–504.
Yamamoto H, Uchida N, Yuasa M, Kageyama K, Ota H, Kaji D, et al. A novel reduced-toxicity myeloablative conditioning regimen using full-dose busulfan, fludarabine, and melphalan for single cord blood transplantation provides durable engraftment and remission in nonremission myeloid malignancies. Biol Blood Marrow Transplant. 2016;22(10):1844–50.
Vokurka S, Steinerova K, Karas M, Koza V. Characteristics and risk factors of oral mucositis after allogeneic stem cell transplantation with FLU/MEL conditioning regimen in context with BU/CY2. Bone Marrow Transplant. 2009;44(9):601–5.
Popat U, de Lima MJ, Saliba RM, Anderlini P, Andersson BS, Alousi AM, et al. Long-term outcome of reduced-intensity allogeneic hematopoietic SCT in patients with AML in CR. Bone Marrow Transplant. 2012;47(2):212–6.
Baron F, Labopin M, Peniket A, Jindra P, Afanasyev B, Sanz MA, et al. Reduced-intensity conditioning with fludarabine and busulfan versus fludarabine and melphalan for patients with acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer. 2015;121(7):1048–55.
Kharfan-Dabaja MA, Labopin M, Bazarbachi A, Hamladji RM, Blaise D, Socie G, et al. Comparing i.v. BU dose intensity between two regimens (FB2 vs FB4) for allogeneic HCT for AML in CR1: a report from the Acute Leukemia Working Party of EBMT. Bone Marrow Transplant. 2014;49(9):1170–5.
Russell JA, Kangarloo SB, Williamson T, Chaudhry MA, Savoie ML, Turner AR, et al. Establishing a target exposure for once-daily intravenous busulfan given with fludarabine and thymoglobulin before allogeneic transplantation. Biol Blood Marrow Transplant. 2013;19(9):1381–6.
Morty M, Avinens O, Faucher C, Viens P, Blaise D, Eliaou JF. Predictive factors and impact of full donor T-cell chimerism after reduced intensity conditioning allogeneic stem cell transplantation. Haematologica. 2007;92(7):1004–6.
El-Cheikh J, Vazquez A, Crocchiolo R, Furst S, Calmels B, Castagna L, et al. Acute GVHD is a strong predictor of full donor CD3+ T cell Chimerism after reduced intensity conditioning allogeneic stem cell transplantation. Am J Hematol. 2012;87:1074–8.
Minagawa K, Yamamori M, Katayama Y, Matsui T. Mycophenolate mofetil: fully utilizing its benefits for GvHD prophylaxis. Int J Hematol. 2012;96:10–25.
Miyamoto T, Takashima S, Kato K, Takase K, Yoshimoto G, Yoshida S, et al. Comparison of cyclosporine and tacrolimus combined with mycophenolate mofetil in prophylaxis for graft-versus-host disease after reduced-intensity umbilical cord blood transplantation. Int J Hematol. 2017;105(1):92–9.
Nakane T, Nakamae H, Yamaguchi T, Kurosawa S, Okamura A, Hidaka M, et al. Use of mycophenolate mofetil and a calcineurin inhibitor in allogeneic hematopoietic stem-cell transplantation from HLA-matched siblings or unrelated volunteer donors: Japanese multicenter phase II trials. Int J Hematol. 2017;105(4):485–96.
Verhaak RG, Goudswaard CS, van Putten W, Bijl MA, Sanders MA, Hugens W, et al. Mutations in nucleophosmin (NPM1) in acute myeloid leukemia (AML): association with other gene abnormalities and previously established gene expression signatures and their favorable prognostic significance. Blood. 2005;106(12):3747–54.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98(6):1752–9.
Cairoli R, Beghini A, Grillo G, Nadali G, Elice F, Ripamonti CB, et al. Prognostic impact of c-KIT mutations in core binding factor leukemias: an Italian retrospective study. Blood. 2006;107(9):3463–8.
Acknowledgements
This study was conducted at the Department of Hematology and Oncology, Osaka University Hospital. We would like to thank all clinicians and patients who contributed to this research. Funding was provided by Otsuka Pharmaceutical (Grant no. 12908149).
Author information
Authors and Affiliations
Contributions
TU and TM designed the study and analyzed the data. Transplantation was performed by TU, TM, SK, JF, and KF with assistance from TY, HS, YT, and YK. The manuscript was written by TU, TM, TY, and YK with assistance from KF, JF, HS, and YT.
Corresponding author
Ethics declarations
Conflict of interest
The authors received research funding from Otsuka Pharmaceutical Co., Ltd.
About this article
Cite this article
Ueda, T., Maeda, T., Kusakabe, S. et al. Addition of melphalan to fludarabine/busulfan (FLU/BU4/MEL) provides survival benefit for patients with myeloid malignancy following allogeneic bone-marrow transplantation/peripheral blood stem-cell transplantation. Int J Hematol 109, 197–205 (2019). https://doi.org/10.1007/s12185-018-2562-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-018-2562-8