Abstract
Mycophenolate mofetil (MMF) has been widely used for the prophylaxis of graft-versus-host disease (GvHD) in hematopoietic stem cell transplantation (HSCT), based on clinical evidence established in organ transplantations. MMF is not a cytotoxic, but rather a cytostatic agent, and there have been several reports of significant advantages in engraftment as well as greatly reduced stomatitis compared to methotrexate (MTX). MMF has been preferred for MTX-free immunosuppression, especially in reduced intensity conditioning, but it is suitable for GvHD prophylaxis for any type of HSCT. Some clinicians doubt its effectiveness, due to the lack of advantage over MTX in acute GvHD prophylaxis, especially in myeloablative conditioning. Pharmacokinetics studies of mycophenolic acid (MPA), the active form of MMF, show large inter- and intra-patient variation, which make interpretations of its clinical usefulness difficult. Nevertheless, several studies, including ours, have demonstrated that relatively higher area under the curve (AUC) of the MPA group leads to significant suppression of acute GvHD in prophylactic use. We propose a model algorithm for optimal dose finding using therapeutic drug monitoring (TDM) for MPA. Preemptive strategies depending on plasma MPA levels could yield more effective approaches to GvHD prophylaxis, alternative to MTX.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prophylaxis for graft-versus-host disease (GvHD) after hematopoietic stem cell transplantation (HSCT) has been developed in the last two decades. Although a combination of calcineurin inhibitor (CI), such as cyclosporin (CsA) or tacrolimus (FK506), plus short-term methotrexate (MTX) has been widely used in clinical practice [1–6], other immunosuppressive drugs, such as steroids, anti-thymocyte globulin (ATG), and campath-1H, are also used as alternative or additional immunosuppressants. Mycophenolate mofetil (MMF) is a type II inosine monophosphate dehydrogenase inhibitor that exerts its immunosuppressive effect by blocking the production of guanosine nucleotide synthesis through the de novo pathway [7, 8]. MMF is widely used for prevention of rejection in organ transplantations. MMF is highly selective, specifically in the suppression of lymphocytes but not myeloid cells; hence, it enables faster engraftment and causes less cytotoxicity, especially stomatitis, compared to MTX. Many clinicians who conduct HSCT favor this drug for GvHD prophylaxis. In addition, MMF has also been utilized as first-line or salvage treatment of acute GvHD, as well as chronic GvHD [9–20]. Despite the increasing infectious complications associated with combined MMF and prednisone regimen, current data have suggested that MMF is an active agent in the treatment of acute and chronic GvHD. MMF dosage for GvHD prophylaxis ranges from 1 to 3 g/day according to institutions, because the optimal dose is not provided by therapeutic drug monitoring (TDM). Several studies fail to establish the range of MMF dosage because the concentration of mycophenolic acid (MPA), which is the active and hydrolyzed form of MMF, differs in each individual. Moreover, plasma MPA concentrations after HSCT are apparently lower than after organ transplantation. In this review, the efficacy/limitations in the field of HSCT and analysis of MMF usage based on conditioning, timing, and stem cell source are discussed.
MMF pharmacokinetics and pharmacodynamics in HSCT
Figure 1 shows the pharmacodynamics of MMF. MMF is a morpholinoethyl ester formulation, which enhances the bioavailability of MPA. MPA was first isolated from a Penicillium culture, but its efficacy as an antibiotic was limited [21]. MPA was later shown to be a potent inhibitor of nucleic acid synthesis, largely by its ability to inhibit the enzyme IMP dehydrogenase (IMPDH) selectively, reversibly, and noncompetitively. IMPDH is the rate-limiting enzyme in the de novo synthesis of guanosine monophosphate (GMP) from IMP. Then it was focused for anti-tumor activity [22–26].
Summary of pharmacology and pharmacodynamics of MMF. After MMF is administered, MMF is hydrolyzed to MPA, which is the active form, and causes reversible inhibition of IMPDH. MPA is reabsorbed via the enterohepatic circulation. MMF mycophenolate mofetil, MPA mycophenolic acid, IMPDH inosine monophosphate dehydrogenase, IMP inosine monophosphate, GMP guanosine monophosphate, MPAG MPA glucuronide, UGTs uridine diphosphate glucuronosyl transferases, EHC enterohepatic circulation, CsA cyclosporine
The GMP synthesis in lymphocytes is highly dependent on the de novo pathway, while other cells utilize the salvage pathway. Therefore, the blockade of GMP synthesis leads to prevention of T-cell activation, as well as B-cell activation. Thereafter, MMF has been widely used as an immunosuppressive agent.
The bioavailability of MMF after oral administration in healthy individuals was reported to be approximately 94 % [27]. Once orally or intravenously administered, MMF rapidly undergoes de-esterification to form its active compound, MPA [7]. Maximum peak concentrations (C max) of MPA generally occur within 1 or 2 h after MMF administration. MPA is primarily metabolized in the liver by uridine diphosphate glucuronosyl transferases (UGTs) to form the metabolites phenolic MPA-glucuronide (MPAG) and, to a lesser extent, acyl-MPAG (AcMPAG). The latter is pharmacologically active and has been linked to the occurrence of MMF-related adverse effects. The excretion of MPAG is primarily renal. Over 90 % of the administered dose is eventually excreted in the urine, mostly as MPAG. The pharmacokinetics of MMF is complicated by the enterohepatic circulation (EHC) of MPAG, which is excreted into the bile and subsequently hydrolyzed in the intestine and reabsorbed as MPA giving rise to a secondary peak of MPA 6–12 h after MMF administration. However, most studies reported that the second peak of MPA was not found in HSCT, because mucosal damage partly due to conditioning regimen interfered with EHC [28, 29]. Even though EHC is active, detection of the second peak is difficult because of the low plasma MPA levels of HSCT patients 6 h after MMF administration. Furthermore, MPA binds extensively to plasma albumin, and the free MPA fraction is less than 3 %. The free MPA fraction is thought to be responsible for the immunosuppressive effect of MPA. Systemic exposure to MPA when MMF is given in combination with CsA is approximately 30–40 % lower than when given alone or with FK506 or sirolimus. It is because CsA inhibits multidrug resistance associated protein 2 (MRP-2), which has been reported to be responsible for the biliary excretion of MPAG and subsequent MPA EHC [30, 31]. The interference associated with the concomitant use of CsA would be one reason for the inter-patient, as well as intra-patient variations in the plasma MPA levels. While the recommended target range for the MPA area under the curve (AUC0–12 h) in renal transplant recipients is 30–60 mg h/L [32], no standard target range in HSCT has been proposed.
Generally, the plasma MPA levels in HSCT are lower than those in organ transplantation, such as renal transplantation. Considerations on MMF pharmacokinetics for HSCT are listed in Table 1. The major factors are bioavailability and MPA clearance. Indeed, the intestinal mucosal damage due to the myeloablative regimen, including total body irradiation (TBI) and high-dose chemotherapy, and/or the use of broad-spectrum antibiotics deteriorate the bioavailability after oral administration of MMF. However, because the intravenous formulation of MMF still achieved ten times lower trough blood level of MPA in myeloablative HSCT compared with healthy volunteers [33], the bioavailability of MMF might not be mainly the reason for the lower MPA levels. For MPA clearance, a higher clearance has been reported to be associated with decreased EHC, lower serum albumin levels [34, 35], and in combination with CsA [30, 31]. Pediatric HSCT study using intravenous and oral MMF in combination with FK506 showed that there was a trend in increased MPA clearance following myeloablative conditioning, which caused a more severe mucosal damage and decreased EHC compared to reduced intensity conditioning (RIC) [36]. However, there was no difference in the plasma MPA concentrations in both oral and intravenous regimens. Recently, a pharmacokinetics study has revealed that MPA clearance was increased in HSCT patients compared to renal transplant recipients [37]. Interestingly, the correlation between MPA clearance and CsA trough levels and plasma albumin was significant in a multivariate model. One explanation for the lower MPA levels in HSCT patients compared to those who received organ transplant could be the high MPA clearance as a result of combination with CsA and the high trough and low plasma albumin levels. However, another report on patients treated with RIC did not find a positive correlation between total MPA AUC and serum albumin levels [38]. Therefore, there is still no clear explanation for the lower MPA concentration in HSCT patients.
Beginning of utilizing MMF for HSCT
The usefulness of MMF in the field of organ transplantation, especially renal transplantation, by randomized controlled studies had been reported since the mid-1990s [39–41]. In the late 1990s, Storb et al. conducted experimental studies to show the effectiveness of CsA plus MMF in canine HSCT after non-myeloablative conditioning [42, 43]. Subsequently, MMF was introduced for GvHD prophylaxis in human HSCT. The Seattle group showed that the combination of CsA plus MMF was comparable to CsA plus MTX. Thereafter, MMF has been practically employed in the HSCT field, especially for RIC [44, 45], with less clinical trials compared to the application in renal transplantation.
Conventional usage of MMF for acute GvHD prophylaxis
Generally, MMF is initiated at 15–45 mg/kg orally or intravenously twice or thrice daily (the dose is rounded off to the nearest multiple of 250 mg for internal use) from day 0 for 27–40 days, and then it is either stopped or tapered through day 96–180 [29, 38, 46–48]. A report from Fred Hutchinson Cancer Research Center demonstrated that MMF given thrice daily allowed durable engraftment in unrelated HSCT after RIC (fludarabine 90 mg/m2 plus TBI 2 Gy) [49]. The infection rate with thrice daily administration was slightly higher than that with twice daily, but treatment-related mortality (TRM) was not increased in thrice daily administration. The probability of acute GvHD was similar in both groups. Another report from the same institute also documented that post-grafting immunosuppression with extended (up to day 180) MMF and shortened (up to day 80) CsA increased the incidence of acute GvHD in unrelated HSCT given RIC [50]. Our small cohort showed that extended MMF administration beyond day 30 is recommended depending on individual risk factors for GvHD, namely (1) HSCT from a mismatched donor, (2) concurrent acute GvHD, (3) eosinophilia (>0.5 × 109/L), or (4) fever without infection. The median extended dosing period of MMF was 64.5 days (50–94). The cumulative incidence of grade II–IV acute GvHD was significantly lower (12.5 %) compared to the cessation of MMF administration at day 30 (42.3 %)[51].
The optimal MMF dose is not elucidated so far, but 2–3 g daily of MMF in combination with CI has been mostly used in Western countries, and it might be acceptable to taper according to the patients’ status beyond day 30 before CI withdrawal.
Engraftment issue
Primary as well as secondary engraftment failure is one of the most important concerns, especially in HSCT given RIC or cord blood transplantation (CBT). Previous reports demonstrated that the intensification of the immunosuppressive regimens was the key factor for promotion of engraftment. Conditioning with the use of immunosuppressive agents, such as ATG, campath-1H, fludarabine, cyclophosphamide, and TBI, is an effective way of engraftment [52–56]. As a multicenter experience, fludarabine plus low dose TBI in 38 cases of salvage HSCT for allograft rejection was reported to be well tolerated and resulted in an engraftment rate of 87 % [56]. In this study, MMF was employed for GvHD prophylaxis in combination with CI. Our preliminary experiences also found that the intensification of immunosuppression with MMF in combination with CI enabled the achievement of a successful engraftment as a salvage CBT [57]. Although the mechanism has not been elucidated, several reports have suggested that GvHD prophylaxis regimen containing MMF is associated with faster engraftment [58–61]. One possible explanation is that short-term MTX, but not MMF, often interferes with emerging neutrophil engraftment due to its cytotoxic effect.
Another possibility is that MMF itself might enhance engraftment because patients with mean MPA concentration steady state (C ss) less than 2.5 μg/mL were reported to come across graft rejection [38]. It is well known that treatment with thrice daily MMF significantly increased MPA C ss in plasma [38, 49, 62], despite a negative report [63]. Because free MPA binds reversibly to IMPDH and interrupts de novo purine pathway transiently, high fractionated administration is reasonable to enhance its activity [45]. It is of interest whether the pharmacological increase in C ss by tid could contribute to the clinical efficacies to prevent GVHD as well as graft failure.
Trends toward MTX-free immunosuppression
Stomatitis is a frequent complication of the conditioning regimen. Severe oral stomatitis occurs in up to 75 % of cases with myeloablative conditioning [64]. Severe stomatitis often causes problems and increases early mortality rate after HSCT [65]. MTX for GvHD prophylaxis impairs mucosal regeneration after conditioning-related mucosal damage, as well as faster engraftment. In RIC of patients over 55 years old, which is the upper limit for myeloablative conditioning in most facilities, or younger patients with concomitant complications, such as cardiac or infectious diseases, the lesser occurrence of stomatitis and early mortality and faster engraftment by utilizing an alternative immunosuppressant to MTX would be attractive for a safe and secure HSCT.
Thus, the concept of “MTX-free immunosuppression” has emerged. Sirolimus is the first available inhibitor of the mammalian target of rapamycin (mTOR) used in HSCT. Since sirolimus poses less nephrotoxicity and neurotoxicity, combination therapy with CI is appealing. There have been many clinical trials of sirolimus and FK506 without MTX for GvHD prophylaxis mainly at Dana-Faber Cancer Institute so far [66–70]. These results indicate that sirolimus may reduce the incidence of acute GvHD, while the severity and incidence of stomatitis and cytomegalovirus (CMV) reactivation are decreased as compared to the MTX-containing regimen [68, 69, 71]. Unfortunately, these results have been discouraged by the increased risk of sinusoidal obstruction syndrome (SOS), especially with busulfan-based conditioning [72]. Moreover, thrombotic microangiopathy (TMA) and renal failure are also documented in GvHD prophylaxis and treatment trials using the sirolimus and CI combination [73–75]. Because MMF has not been shown to increase the risk of SOS or TMA, MTX-free immunosuppression, such as CI plus MMF, might be suitable for GvHD prophylaxis, especially in busulfan-containing regimen. Indeed, MMF has been used as part of the front-line regimen for the prevention of GvHD, especially in the setting of RIC regimen. Similarly to sirolimus, MMF reduces stomatitis [58, 76] and facilitates engraftment [58–61, 76–78].
A recent retrospective study in the comparison of CsA plus MMF and CsA plus MTX after RIC from human leukocyte antigen (HLA)-identical siblings showed a lower tendency of non-relapse mortality (NRM) at day 100 (6 vs. 18 %, P = 0.04) [79]. Comparisons of MTX, sirolimus, and MMF for GvHD prophylaxis are summarized in Table 2. Representative reports of comparison for prophylaxis on the use of CI plus MMF versus CI plus MTX are also shown in Table 3.
Why do some clinicians stay away from MMF as conventional prophylaxis?
MMF usage in myeloablative conditioning is controversial. A prospective randomized trial that compared CsA plus MTX and CsA plus MMF for GvHD prophylaxis in myeloablative HSCT showed significantly less severe stomatitis and more rapid neutrophil engraftment in the MMF arm. The incidence of grade II–IV acute GvHD was similar in the two arms (48 % in the MMF arm and 37 % in the MTX arm) [58] (Table 3). On the other hand, phase I/II study, in which 45 mg/kg/day MMF was given thrice daily for 27 days in combination with CsA, suggested the lack of a significant improvement in the prevention of GvHD compared with historical data for CsA and MTX after myeloablative HSCT from HLA-matched sibling donors [29]. In this study, the incidence of acute GvHD was 62 %. For some physicians, this is the rationale why the combination of CsA plus MMF is considered only when MTX is contraindicated. However, there are not significant differences on the pharmacokinetics of MMF in myeloablative conditioning versus RIC in adult HSCT to date. There is no clear explanation why the benefit of MMF is superior in RIC regimen compared to myeloablative conditioning.
Prophylactic use for related donors (especially from HLA-mismatched donors)
Some studies showed that GvHD prophylaxis by MMF plus CI for either myeloablative or RIC achieved successful engraftment and prevented GvHD similar to MTX plus CI [29, 80, 81] (Table 4). Of note, MMF is also used for HSCT from HLA-mismatched related donors, as well as HLA-matched ones. In Asia, Japanese, and Chinese recipients with no HLA-matched sibling donors received HSCT from two or three loci-mismatched related donor. The usual conditioning regimens, including ATG, and multiple immunosuppressants, such as MMF, were used for GvHD prophylaxis [82, 83]. Moreover, clinical trials from Johns Hopkins University recently evaluated the efficacy of high-dose, post-transplantation cyclophosphamide in addition to FK506 and MMF to prevent GvHD after non-T cell-depleted transplantation from partially HLA-mismatched related donors [84, 85].
Prophylactic use for unrelated donors (except for umbilical cord blood)
Representative reports of MMF prophylaxis for unrelated donors are listed in Table 4 [38, 45, 47, 49, 77, 78, 86–88]. A large-scale study of eighty-nine patients transplanted under RIC using either oral or intravenous MMF and CsA showed 93 % engraftment. The rates of grade II, III, and IV acute GvHD were 42, 8, and 2 %, respectively [45]. We also showed 15 cases of myeloablative or RIC HSCT from unrelated donors using oral MMF and FK506. All, except one, were engrafted, and grade II–IV acute GvHD occurred in 6 patients (42.8 %) [89]. These results indicate that prophylactic use of MMF plus CI seems not to interfere with primary engraftment and prevent acute GvHD, as well as MTX plus CI, in HSCT from unrelated donors.
Prophylactic use for CBT
MMF is usually a feasible option for GvHD prophylaxis in CBT, wherein primary graft failure due to limited stem cell numbers is a concern. Large prospective study consisting of 110 adult umbilical cord blood transplantations demonstrated that the combination of MMF and CsA for GvHD prophylaxis facilitated engraftment (neutrophil engraftment was achieved in 92 % at a median of 12 days) and suppressed grade II to IV acute and chronic GvHD (59 and 29 %, respectively)[90]. In dual CBT, FK506 and MMF (1,000 mg twice daily) were given to 27 patients until at least 60 days after myeloablative conditioning [fludarabine (160 mg/m2) plus TBI 1.350 cGy]. Neutrophil engraftment was achieved in 80 % with a median of 24 days. Grade II to IV acute GvHD occurred in 37 %. Cumulative incidence of total parental nutrition usage was up to 56 %. This reflected the less gastrointestinal mucosal damage caused by MMF than MTX even under myeloablative conditioning [91]. A Japanese group also reported 29 elderly (median age 62) RIC-CBT patients who received FK506 and MMF for acute GvHD prophylaxis. The patients were compared with matched-pair historical controls who received FK506 alone [92]. Primary engraftment until day 60 was significantly higher (90 %) in the FK506 plus MMF group than the control group (69 %). Cumulative incidence of grade II to IV acute GvHD was 63 %. Interestingly, severe pre-engraftment immune reaction (PIR), which was a factor that negatively affected overall survival [93–95], was significantly lower (16 %) in the FK506 plus MMF group than the control group (52 %). Consequently, NRM in the FK506 plus MMF group within 30 days was significantly lower compared to the control group (0 vs. 21 %). Our experiences with 21 adult myeloablative CBT patients, who received FK506 and MMF, also showed 85.7 % engraftment and only 20 % grade II to IV acute GvHD. In pediatric CBT study, the combination of FK506 and MMF was used for GvHD prophylaxis in 22 cases with either myeloablative or RIC regimen [96]. The median time to recovery was 23 days, and grade II to IV acute GvHD occurred in 33.3 % among the evaluated patients.
Collectively in CBT setting, the addition of MMF to CI for the prophylaxis of acute GvHD seems to be feasible in RIC, as well as myeloablative conditioning.
Dose-finding studies and TDM
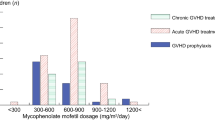
Many pharmacokinetics studies on MMF had been reported for organ transplantation, especially in renal transplantation. However, limited pharmacokinetics studies for finding the optimal dosage in HSCT have been observed to date. Table 5 shows the summary of pharmacokinetics studies in HSCT. In general, there is a large inter-patient, as well as intra-patient, variation in plasma MPA levels of HSCT patient as seen in organ transplantation. However, the peak of MPA levels in HSCT is significantly lower than those in organ transplantation. Some pharmacokinetics studies on MMF used for acute and chronic GvHD treatment showed that concentration at trough (C trough) of MPA was significantly greater in the treatment responder than the non-responder [97, 98]. However, correlations between the efficacy on the prevention of acute GvHD and the MPA concentration have not been elucidated. Our small retrospective cohort showed that in patients with adjusted MPA AUC0–24 h over 30 mg h/L (C ss > 1.25 mg/L), acute GvHD, as well as chronic GvHD, occurred significantly less, especially in HSCT from unrelated bone marrow donors. On the contrary, lower MPA levels were enough to control acute and chronic GvHD in CBT. Moreover, a higher MPA level in CBT posed a tendency of GvHD relapse possibly due to weakened graft-versus-leukemia/lymphoma (GVL) effect of cord blood [89]. This finding is encouraging for prospective dose-finding studies depending on each donor source. Recently, one small prospective study demonstrated that at day 7, patients with AUC0–8 h ≥ 22.5 mg h/L (concentration at steady state (C ss) ≥ 2.8 mg/L) displayed no grade II to IV acute GvHD [99]. As a target range after organ transplantation, it has been suggested to keep C ss MPA between 2.5 and 5 mg/L. In Japan, where HLA homogeneity and less GvHD incidence are more common than in Western countries, lower C ss might be enough to prevent severe acute GvHD. Although MMF of 45 mg/kg/day dose reached a relatively high median C ss MPA, 2.73–3.2 mg/L, it did not significantly reduce the occurrence of acute GvHD compared to historical controls receiving MTX instead of MMF for GvHD prophylaxis [29]. Further pharmacokinetics studies should be carried out for optimal MMF dose finding, as well as understanding the precise pharmacodynamics of MPA in HSCT and the prevention of GvHD.
Surrogate marker for the prediction of MPA AUC, C trough or C max?
With limited evidences, there is a need to monitor the concentrations of MPA AUC or C ss for evaluating the efficacy in HSCT, as well as in organ transplantation. As a surrogate marker for MPA AUC, the C trough or C max was often monitored. Haetzcshel et al. [100] reported that a significant correlation was observed between C max and AUC for MPA in 28 patients evaluable at all points. Our data also showed that the concentration at 2 h (C 2h) after MMF administration was well correlated with AUC of MPA [89]. These results were encouraging for the utilization of C max as surrogate marker of the AUC of MPA.
Toxicities and adverse effects
The adverse effects of MMF are listed in Table 6. The most common toxicities are gastrointestinal toxicity, opportunistic infections, and pancytopenia. Most of the physicians’ concern is the gastrointestinal toxicity, which is usually manifested as diarrhea. MMF can produce colitis with focal ulcerations, marked apoptosis, and intense acute and chronic inflammation [101]. Histological features of MMF-related colitis are remarkably similar to the ones associated with intestinal GvHD. We are able to distinguish MMF-related colitis from intestinal GvHD only when there is improvement or resolution of symptoms on the withdrawal or reduction of MMF. This may cause some problems when we estimate the efficacy of MMF for salvage therapy of acute interstitial GvHD. However, few previous reports on prophylactic use of MMF discontinuation due to diarrhea until day 30 after HSCT have been published. There are insufficient data on whether MMF can also produce lesions in the upper gut or not.
Infectious complications, including CMV reactivation, are also common and can be serious adverse effects. In HSCT patients within day 100 after the transplantation, CMV infection, as well as antigenemia, are most likely to happen because of insufficient immune recovery after conditioning regimen and probably with acute GvHD. Prospective trial of 85 patients for HCST with RIC demonstrated that an elevated unbound C ss was significantly associated with CMV reactivation [38]. A retrospective study of 21 consecutive patients with acute and extensive chronic GvHD showed the occurrence of 22 opportunistic or serious viral or bacterial infections in 10 patients [12]. Because MMF also prevents immune recovery, preemptive therapy should be required for CMV reactivation by monitoring CMV antigenemia, as well as empiric therapy for bacterial and fungal infections. Leukocytopenia, anemia, and thrombocytopenia are alarming when we worry about primary and secondary engraftment after HSCT.
A relationship between high MPA AUC values and drug-related adverse effects has been reported in some studies [102–105]. In a prospective, randomized, double-blind, multicenter, controlled study in 150 renal transplant patients, a dose-dependent increase in adverse effects was reported in the first 6 months post-transplant [106]. According to these data, it appears that an MPA AUC0–12 h above 60 mg h/L may increase the risk of toxicity, although such high plasma MPA levels could be hardly achieved in HSCT as described above.
Conclusions and future directions
The relationship between MMF pharmacokinetics/pharmacodynamics and its effectiveness in HSCT is still obscure. However, MMF has been widely used for GvHD prophylaxis, as well as treatment of HSCT, in Europe and the USA.
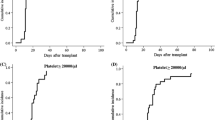
One of the most important aspects of the pharmacokinetics of MMF is the wide intra-patient and inter-patient variations in the plasma MPA levels even under the same daily dose. On the other hand, similar to organ transplantation where higher MPA is correlated with lower rejection rate, higher MPA would correlate with the suppression of immune reactions, such as acute GvHD in HSCT. Then, we proposed a model of algorithm for the optimal dose finding using TDM of MMF (Fig. 2). For GvHD prophylaxis, MMF should be started at 2–3 g/day. In the earlier days after HSCT, such as at the pre-engraftment phase, the plasma MPA levels should be monitored (MPA AUC is preferred, but MPA C 2 h might be an alternative). If the MPA level is low, based on the prediction of upcoming GvHD as determined by individual risk factors such as conditioning, donor type and combination immunosuppressant, MMF dosage should be increased up to the maximum (3 g/day), or other immunosuppressants, such as steroids if the maximum dose had been administered, should be added/shifted to. For example, MPA AUC0–24 h at day 9 or 16 should be >30 mg h/L for Japanese ordinary unrelated BMT. On the other hand, if MPA levels are high enough to prevent acute GvHD, MMF should be tapered as soon as the engraftment is achieved. In our study, we could predict that MPA AUC0–24 h <30 mg h/L at day 9 or 16 would be usually enough for single unit Japanese CBT. The risk for relapse is higher at higher MPA levels. Thus, the MMF dose must be keep at the minimal requirement.
New proposal algorithm for optimizing MMF dose. First, start MMF at 2–3 g/day. Second, monitor MPA concentration at pre-engraftment phase after transplantation. Third, adjust the MMF dosage according to the estimation of GvHD risk or switch to/add another immunosuppressant, such as steroids, if MPA concentration is too low
In conclusion, MMF is a safe and effective prophylaxis for the prevention of acute GvHD, as well as its treatment. MMF has been frequently used in RIC regimen and CBT. In a myeloablative setting, MMF has not been used by some clinicians due to limited clinical studies. To elucidate the advantage of the prophylactic use of MMF depending on the donor sources in the myeloablative regimen as well as RIC, larger prospective studies accompanying TDM are needed.
References
Storb R, Deeg HJ, Whitehead J, Appelbaum F, Beatty P, Bensinger W, et al. Methotrexate and cyclosporine compared with cyclosporine alone for prophylaxis of acute graft versus host disease after marrow transplantation for leukemia. N Engl J Med. 1986;314(12):729–35.
Storb R, Deeg HJ, Fisher L, Appelbaum F, Buckner CD, Bensinger W, et al. Cyclosporine v methotrexate for graft-v-host disease prevention in patients given marrow grafts for leukemia: long-term follow-up of three controlled trials. Blood. 1988;71(2):293–8.
Storb R, Deeg HJ, Pepe M, Appelbaum F, Anasetti C, Beatty P, et al. Methotrexate and cyclosporine versus cyclosporine alone for prophylaxis of graft-versus-host disease in patients given HLA-identical marrow grafts for leukemia: long-term follow-up of a controlled trial. Blood. 1989;73(6):1729–34.
Ratanatharathorn V, Nash RA, Przepiorka D, Devine SM, Klein JL, Weisdorf D, et al. Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood. 1998;92(7):2303–14.
Horowitz MM, Przepiorka D, Bartels P, Buell DN, Zhang MJ, Fitzsimmons WE, et al. Tacrolimus vs. cyclosporine immunosuppression: results in advanced-stage disease compared with historical controls treated exclusively with cyclosporine. Biol Blood Marrow Transplant. 1999;5(3):180–6.
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96(6):2062–8.
Bullingham RE, Nicholls AJ, Kamm BR. Clinical pharmacokinetics of mycophenolate mofetil. Clin Pharmacokinet. 1998;34(6):429–55.
Allison AC, Eugui EM. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology. 2000;47(2–3):85–118.
Basara N, Blau WI, Romer E, Rudolphi M, Bischoff M, Kirsten D, et al. Mycophenolate mofetil for the treatment of acute and chronic GVHD in bone marrow transplant patients. Bone Marrow Transplant. 1998;22(1):61–5.
Mookerjee B, Altomonte V, Vogelsang G. Salvage therapy for refractory chronic graft-versus-host disease with mycophenolate mofetil and tacrolimus. Bone Marrow Transplant. 1999;24(5):517–20.
Basara N, Kiehl MG, Blau W, Romer E, Bischoff M, Schmetzer B, et al. Mycophenolate mofetil in the treatment of acute and chronic GVHD in hematopoietic stem cell transplant patients: four years of experience. Transplant Proc. 2001;33(3):2121–3.
Baudard M, Vincent A, Moreau P, Kergueris MF, Harousseau JL, Milpied N. Mycophenolate mofetil for the treatment of acute and chronic GVHD is effective and well tolerated but induces a high risk of infectious complications: a series of 21 BM or PBSC transplant patients. Bone Marrow Transplant. 2002;30(5):287–95.
Busca A, Locatelli F, Marmont F, Audisio E, Falda M. Response to mycophenolate mofetil therapy in refractory chronic graft-versus-host disease. Haematologica. 2003;88(7):837–9.
Kim JG, Sohn SK, Kim DH, Lee NY, Suh JS, Lee KS, et al. Different efficacy of mycophenolate mofetil as salvage treatment for acute and chronic GVHD after allogeneic stem cell transplant. Eur J Haematol. 2004;73(1):56–61.
Krejci M, Doubek M, Buchler T, Brychtova Y, Vorlicek J, Mayer J. Mycophenolate mofetil for the treatment of acute and chronic steroid-refractory graft-versus-host disease. Ann Hematol. 2005;84(10):681–5.
Takami A, Mochizuki K, Okumura H, Ito S, Suga Y, Yamazaki H, et al. Mycophenolate mofetil is effective and well tolerated in the treatment of refractory acute and chronic graft-versus-host disease. Int J Hematol. 2006;83(1):80–5.
Furlong T, Martin P, Flowers ME, Carnevale-Schianca F, Yatscoff R, Chauncey T, et al. Therapy with mycophenolate mofetil for refractory acute and chronic GVHD. Bone Marrow Transplant. 2009;44(11):739–48.
Alousi AM, Weisdorf DJ, Logan BR, Bolanos-Meade J, Carter S, Difronzo N, et al. Etanercept, mycophenolate, denileukin, or pentostatin plus corticosteroids for acute graft-versus-host disease: a randomized phase 2 trial from the Blood and Marrow Transplant Clinical Trials Network. Blood. 2009;114(3):511–7.
Onishi C, Ohashi K, Sawada T, Nakano M, Kobayashi T, Yamashita T, et al. A high risk of life-threatening infectious complications in mycophenolate mofetil treatment for acute or chronic graft-versus-host disease. Int J Hematol. 2010;91(3):464–70.
Jacobson PA, Huang J, Wu J, Kim M, Logan B, Alousi A, et al. Mycophenolate pharmacokinetics and association with response to acute graft-versus-host disease treatment from the Blood and Marrow Transplant Clinical Trials Network. Biol Blood Marrow Transplant. 2010;16(3):421–9.
Franklin TJ, Cook JM. The inhibition of nucleic acid synthesis by mycophenolic acid. Biochem J. 1969;113(3):515–24.
Jackson RC, Weber G, Morris HP. IMP dehydrogenase, an enzyme linked with proliferation and malignancy. Nature. 1975;256(5515):331–3.
Nagai M, Natsumeda Y, Konno Y, Hoffman R, Irino S, Weber G. Selective up-regulation of type II inosine 5’-monophosphate dehydrogenase messenger RNA expression in human leukemias. Cancer Res. 1991;51(15):3886–90.
Nagai M, Natsumeda Y, Weber G. Proliferation-linked regulation of type II IMP dehydrogenase gene in human normal lymphocytes and HL-60 leukemic cells. Cancer Res. 1992;52(2):258–61.
Carr SF, Papp E, Wu JC, Natsumeda Y. Characterization of human type I and type II IMP dehydrogenases. The Journal of biological chemistry. 1993;268(36):27286–90.
Gharehbaghi K, Burgess GS, Collart FR, Litz-Jackson S, Huberman E, Jayaram HN et al. p210 bcr-abl confers overexpression of inosine monophosphate dehydrogenase: an intrinsic pathway to drug resistance mediated by oncogene. Leukemia (official journal of the Leukemia Society of America, Leukemia Research Fund, UK). 1994;8(8):1257–63.
Bullingham R, Monroe S, Nicholls A, Hale M. Pharmacokinetics and bioavailability of mycophenolate mofetil in healthy subjects after single-dose oral and intravenous administration. J Clin Pharmacol. 1996;36(4):315–24.
van Hest RM, Doorduijn JK, de Winter BC, Cornelissen JJ, Vulto AG, Oellerich M, et al. Pharmacokinetics of mycophenolate mofetil in hematopoietic stem cell transplant recipients. Ther Drug Monit. 2007;29(3):353–60.
Nash RA, Johnston L, Parker P, McCune JS, Storer B, Slattery JT, et al. A phase I/II study of mycophenolate mofetil in combination with cyclosporine for prophylaxis of acute graft-versus-host disease after myeloablative conditioning and allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2005;11(7):495–505.
Hesselink DA, van Hest RM, Mathot RA, Bonthuis F, Weimar W, de Bruin RW, et al. Cyclosporine interacts with mycophenolic acid by inhibiting the multidrug resistance-associated protein 2. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2005;5(5):987–94.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin Pharmacokinet. 2007;46(1):13–58.
Shaw LM, Holt DW, Oellerich M, Meiser B, van Gelder T. Current issues in therapeutic drug monitoring of mycophenolic acid: report of a roundtable discussion. Ther Drug Monit. 2001;23(4):305–15.
Jenke A, Renner U, Richte M, Freiberg-Richter J, Platzbecker U, Helwig A, et al. Pharmacokinetics of intravenous mycophenolate mofetil after allogeneic blood stem cell transplantation. Clin Transplant. 2001;15(3):176–84.
Shaw LM, Korecka M, Aradhye S, Grossman R, Bayer L, Innes C, et al. Mycophenolic acid area under the curve values in African American and Caucasian renal transplant patients are comparable. J Clin Pharmacol. 2000;40(6):624–33.
van Hest RM, van Gelder T, Vulto AG, Mathot RA. Population pharmacokinetics of mycophenolic acid in renal transplant recipients. Clin Pharmacokinet. 2005;44(10):1083–96.
Bhatia M, Militano O, Jin Z, Figurski M, Shaw L, Moore V, et al. An age-dependent pharmacokinetic study of intravenous and oral mycophenolate mofetil in combination with tacrolimus for GVHD prophylaxis in pediatric allogeneic stem cell transplantation recipients. Biol Blood Marrow Transplant. 2010;16(3):333–43.
de Winter BC, Mathot RA, Sombogaard F, Neumann I, van Hest RM, Doorduijn JK, et al. Differences in clearance of mycophenolic acid among renal transplant recipients, hematopoietic stem cell transplant recipients, and patients with autoimmune disease. Ther Drug Monit. 2010;32(5):606–14.
Giaccone L, McCune JS, Maris MB, Gooley TA, Sandmaier BM, Slattery JT, et al. Pharmacodynamics of mycophenolate mofetil after nonmyeloablative conditioning and unrelated donor hematopoietic cell transplantation. Blood. 2005;106(13):4381–8.
European Mycophenolate Mofetil Cooperative Study Group. Placebo-controlled study of mycophenolate mofetil combined with cyclosporin and corticosteroids for prevention of acute rejection. Lancet. 1995;345(8961):1321–5.
Sollinger HW. Mycophenolate mofetil for the prevention of acute rejection in primary cadaveric renal allograft recipients. US Renal Transplant Mycophenolate Mofetil Study Group. Transplantation. 1995;60(3):225–32.
The Tricontinental Mycophenolate Mofetil Renal Transplantation Study Group. A blinded, randomized clinical trial of mycophenolate mofetil for the prevention of acute rejection in cadaveric renal transplantation. Transplantation. 1996;61(7):1029–37.
Storb R, Yu C, Wagner JL, Deeg HJ, Nash RA, Kiem HP, et al. Stable mixed hematopoietic chimerism in DLA-identical littermate dogs given sublethal total body irradiation before and pharmacological immunosuppression after marrow transplantation. Blood. 1997;89(8):3048–54.
Yu C, Seidel K, Nash RA, Deeg HJ, Sandmaier BM, Barsoukov A, et al. Synergism between mycophenolate mofetil and cyclosporine in preventing graft-versus-host disease among lethally irradiated dogs given DLA-nonidentical unrelated marrow grafts. Blood. 1998;91(7):2581–7.
McSweeney PA, Niederwieser D, Shizuru JA, Sandmaier BM, Molina AJ, Maloney DG, et al. Hematopoietic cell transplantation in older patients with hematologic malignancies: replacing high-dose cytotoxic therapy with graft-versus-tumor effects. Blood. 2001;97(11):3390–400.
Maris MB, Niederwieser D, Sandmaier BM, Storer B, Stuart M, Maloney D, et al. HLA-matched unrelated donor hematopoietic cell transplantation after nonmyeloablative conditioning for patients with hematologic malignancies. Blood. 2003;102(6):2021–30.
Gupta V, Daly A, Lipton JH, Hasegawa W, Chun K, Kamel-Reid S, et al. Nonmyeloablative stem cell transplantation for myelodysplastic syndrome or acute myeloid leukemia in patients 60 years or older. Biol Blood Marrow Transplant. 2005;11(10):764–72.
Baron F, Maris MB, Storer BE, Sandmaier BM, Stuart MJ, McSweeney PA, et al. HLA-matched unrelated donor hematopoietic cell transplantation after nonmyeloablative conditioning for patients with chronic myeloid leukemia. Biol Blood Marrow Transplant. 2005;11(4):272–9.
Baron F, Maris MB, Storer BE, Sandmaier BM, Panse JP, Chauncey TR et al. High doses of transplanted CD34+ cells are associated with rapid T-cell engraftment and lessened risk of graft rejection, but not more graft-versus-host disease after nonmyeloablative conditioning and unrelated hematopoietic cell transplantation. Leukemia (official journal of the Leukemia Society of America, Leukemia Research Fund, UK). 2005; 19(5):822–8.
Maris MB, Sandmaier BM, Storer BE, Maloney DG, Shizuru JA, Agura E, et al. Unrelated donor granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cell transplantation after nonmyeloablative conditioning: the effect of postgrafting mycophenolate mofetil dosing. Biol Blood Marrow Transplant. 2006;12(4):454–65.
Baron F, Sandmaier BM, Storer BE, Maris MB, Langston AA, Lange T, et al. Extended mycophenolate mofetil and shortened cyclosporine failed to reduce graft-versus-host disease after unrelated hematopoietic cell transplantation with nonmyeloablative conditioning. Biol Blood Marrow Transplant. 2007;13(9):1041–8.
Nishikawa S, Okamura A, Yamamori M, Minagawa K, Kawamori Y, Kawano Y, et al. Extended mycophenolate mofetil administration beyond day 30 in allogeneic hematopoietic stem cell transplantation as preemptive therapy for severe graft-versus-host disease. Transplant Proc. 2009;41(9):3873–6.
Jabbour E, Rondon G, Anderlini P, Giralt SA, Couriel DR, Champlin RE, et al. Treatment of donor graft failure with nonmyeloablative conditioning of fludarabine, antithymocyte globulin and a second allogeneic hematopoietic transplantation. Bone Marrow Transplant. 2007;40(5):431–5.
Chewning JH, Castro-Malaspina H, Jakubowski A, Kernan NA, Papadopoulos EB, Small TN, et al. Fludarabine-based conditioning secures engraftment of second hematopoietic stem cell allografts (HSCT) in the treatment of initial graft failure. Biol Blood Marrow Transplant. 2007;13(11):1313–23.
Heinzelmann F, Lang PJ, Ottinger H, Faul C, Bethge W, Handgretinger R, et al. Immunosuppressive total lymphoid irradiation-based reconditioning regimens enable engraftment after graft rejection or graft failure in patients treated with allogeneic hematopoietic stem cell transplantation. Int J Radiat Oncol Biol Phys. 2008;70(2):523–8.
Byrne BJ, Horwitz M, Long GD, Gasparetto C, Sullivan KM, Chute J, et al. Outcomes of a second non-myeloablative allogeneic stem cell transplantation following graft rejection. Bone Marrow Transplant. 2008;41(1):39–43.
Gyurkocza B, Cao TM, Storb RF, Lange T, Leisenring W, Franke GN, et al. Salvage allogeneic hematopoietic cell transplantation with fludarabine and low-dose total body irradiation after rejection of first allografts. Biol Blood Marrow Transplant. 2009;15(10):1314–22.
Kawamori Y, Yakushijin K, Okamura A, Nishikawa S, Minagawa K, Shimoyama M, et al. Successful engraftment in reduced-intensity cord blood transplantation (CBT) as a salvage therapy for graft failure after primary CBT in adults. Transplantation. 2007;83(9):1281–2.
Bolwell B, Sobecks R, Pohlman B, Andresen S, Rybicki L, Kuczkowski E, et al. A prospective randomized trial comparing cyclosporine and short course methotrexate with cyclosporine and mycophenolate mofetil for GVHD prophylaxis in myeloablative allogeneic bone marrow transplantation. Bone Marrow Transplant. 2004;34(7):621–5.
Bornhauser M, Schuler U, Porksen G, Naumann R, Geissler G, Thiede C, et al. Mycophenolate mofetil and cyclosporine as graft-versus-host disease prophylaxis after allogeneic blood stem cell transplantation. Transplantation. 1999;67(4):499–504.
Kiehl MG, Schafer-Eckart K, Kroger M, Bornhauser M, Basara N, Blau IW, et al. Mycophenolate mofetil for the prophylaxis of acute graft-versus-host disease in stem cell transplant recipients. Transplant Proc. 2002;34(7):2922–4.
Neumann F, Graef T, Tapprich C, Vaupel M, Steidl U, Germing U, et al. Cyclosporine A and mycophenolate mofetil vs cyclosporine A and methotrexate for graft-versus-host disease prophylaxis after stem cell transplantation from HLA-identical siblings. Bone Marrow Transplant. 2005;35(11):1089–93.
Okamura A, Yamamori M, Shimoyama M, Kawano Y, Kawano H, Kawamori Y, et al. Pharmacokinetics-based optimal dose-exploration of mycophenolate mofetil in allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2008;88(1):104–10.
Jacobson P, El-Massah SF, Rogosheske J, Kerr A, Long-Boyle J, DeFor T, et al. Comparison of two mycophenolate mofetil dosing regimens after hematopoietic cell transplantation. Bone Marrow Transplant. 2009;44(2):113–20.
Woo SB, Sonis ST, Monopoli MM, Sonis AL. A longitudinal study of oral ulcerative mucositis in bone marrow transplant recipients. Cancer. 1993;72(5):1612–7.
Sonis ST, Oster G, Fuchs H, Bellm L, Bradford WZ, Edelsberg J, et al. Oral mucositis and the clinical and economic outcomes of hematopoietic stem-cell transplantation. J Clin Oncol. 2001;19(8):2201–5.
Cutler C, Antin JH. Sirolimus for GVHD prophylaxis in allogeneic stem cell transplantation. Bone Marrow Transplant. 2004;34(6):471–6.
Cutler C, Kim HT, Hochberg E, Ho V, Alyea E, Lee SJ, et al. Sirolimus and tacrolimus without methotrexate as graft-versus-host disease prophylaxis after matched related donor peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2004;10(5):328–36.
Cutler C, Li S, Kim HT, Laglenne P, Szeto KC, Hoffmeister L, et al. Mucositis after allogeneic hematopoietic stem cell transplantation: a cohort study of methotrexate- and non-methotrexate-containing graft-versus-host disease prophylaxis regimens. Biol Blood Marrow Transplant. 2005;11(5):383–8.
Cutler C, Li S, Ho VT, Koreth J, Alyea E, Soiffer RJ, et al. Extended follow-up of methotrexate-free immunosuppression using sirolimus and tacrolimus in related and unrelated donor peripheral blood stem cell transplantation. Blood. 2007;109(7):3108–14.
Cutler C, Stevenson K, Kim HT, Brown J, McDonough S, Herrera M, et al. Double umbilical cord blood transplantation with reduced intensity conditioning and sirolimus-based GVHD prophylaxis. Bone Marrow Transplant. 2011;46(5):659–67.
Marty FM, Bryar J, Browne SK, Schwarzberg T, Ho VT, Bassett IV, et al. Sirolimus-based graft-versus-host disease prophylaxis protects against cytomegalovirus reactivation after allogeneic hematopoietic stem cell transplantation: a cohort analysis. Blood. 2007;110(2):490–500.
Cutler C, Stevenson K, Kim HT, Richardson P, Ho VT, Linden E, et al. Sirolimus is associated with veno-occlusive disease of the liver after myeloablative allogeneic stem cell transplantation. Blood. 2008;112(12):4425–31.
Cutler C, Henry NL, Magee C, Li S, Kim HT, Alyea E, et al. Sirolimus and thrombotic microangiopathy after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005;11(7):551–7.
Couriel DR, Saliba R, Escalon MP, Hsu Y, Ghosh S, Ippoliti C, et al. Sirolimus in combination with tacrolimus and corticosteroids for the treatment of resistant chronic graft-versus-host disease. Br J Haematol. 2005;130(3):409–17.
Johnston LJ, Brown J, Shizuru JA, Stockerl-Goldstein KE, Stuart MJ, Blume KG, et al. Rapamycin (sirolimus) for treatment of chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2005;11(1):47–55.
Perkins J, Field T, Kim J, Kharfan-Dabaja MA, Fernandez H, Ayala E, et al. A randomized phase II trial comparing tacrolimus and mycophenolate mofetil to tacrolimus and methotrexate for acute graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant. 2010;16(7):937–47.
Niederwieser D, Maris M, Shizuru JA, Petersdorf E, Hegenbart U, Sandmaier BM, et al. Low-dose total body irradiation (TBI) and fludarabine followed by hematopoietic cell transplantation (HCT) from HLA-matched or mismatched unrelated donors and postgrafting immunosuppression with cyclosporine and mycophenolate mofetil (MMF) can induce durable complete chimerism and sustained remissions in patients with hematological diseases. Blood. 2003;101(4):1620–9.
Mizumoto C, Kanda J, Ichinohe T, Ishikawa T, Matsui M, Kadowaki N, et al. Mycophenolate mofetil combined with tacrolimus and minidose methotrexate after unrelated donor bone marrow transplantation with reduced-intensity conditioning. Int J Hematol. 2009;89(4):538–45.
Pinana JL, Valcarcel D, Fernandez-Aviles F, Martino R, Rovira M, Barba P, et al. MTX or mycophenolate mofetil with CsA as GVHD prophylaxis after reduced-intensity conditioning PBSCT from HLA-identical siblings. Bone Marrow Transplant. 2010;45(9):1449–56.
Sabry W, Le Blanc R, Labbe AC, Sauvageau G, Couban S, Kiss T, et al. Graft-versus-host disease prophylaxis with tacrolimus and mycophenolate mofetil in HLA-matched nonmyeloablative transplant recipients is associated with very low incidence of GVHD and nonrelapse mortality. Biol Blood Marrow Transplant. 2009;15(8):919–29.
Iida M, Fukuda T, Ikegame K, Yoshihara S, Ogawa H, Taniguchi S, et al. Use of mycophenolate mofetil in patients received allogeneic hematopoietic stem cell transplantation in Japan. Int J Hematol. 2011;93(4):523–31.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006;107(8):3065–73.
Ogawa H, Ikegame K, Kaida K, Yoshihara S, Fujioka T, Taniguchi Y, et al. Unmanipulated HLA 2-3 antigen-mismatched (haploidentical) bone marrow transplantation using only pharmacological GVHD prophylaxis. Exp Hematol. 2008;36(1):1–8.
O’Donnell PV, Luznik L, Jones RJ, Vogelsang GB, Leffell MS, Phelps M, et al. Nonmyeloablative bone marrow transplantation from partially HLA-mismatched related donors using posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2002;8(7):377–86.
Kasamon YL, Luznik L, Leffell MS, Kowalski J, Tsai HL, Bolanos-Meade J, et al. Nonmyeloablative HLA-haploidentical bone marrow transplantation with high-dose posttransplantation cyclophosphamide: effect of HLA disparity on outcome. Biol Blood Marrow Transplant. 2010;16(4):482–9.
Rodriguez R, Parker P, Nademanee A, Smith D, O’Donnell MR, Stein A, et al. Cyclosporine and mycophenolate mofetil prophylaxis with fludarabine and melphalan conditioning for unrelated donor transplantation: a prospective study of 22 patients with hematologic malignancies. Bone Marrow Transplant. 2004;33(11):1123–9.
Perez-Simon JA, Martino R, Caballero D, Valcarcel D, Rebollo N, de la Camara R, et al. Reduced-intensity conditioning allogeneic transplantation from unrelated donors: evaluation of mycophenolate mofetil plus cyclosporin A as graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant. 2008;14(6):664–71.
Zohren F, Schroeder T, Czibere A, Fenk R, Bruns I, Kondakci M, et al. Tacrolimus and mycofenolate mofetil as GvHD prophylaxis following nonmyeloablative conditioning and unrelated hematopoietic SCT for adult patients with advanced hematologic diseases. Bone Marrow Transplant. 2011;46(5):747–55.
Wakahashi K, Yamamori M, Minagawa K, Ishii S, Nishikawa S, Shimoyama M, et al. Pharmacokinetics-based optimal dose prediction of donor source-dependent response to mycophenolate mofetil in unrelated hematopoietic cell transplantation. Int J Hematol. 2011;94(2):193–202.
Brunstein CG, Barker JN, Weisdorf DJ, DeFor TE, Miller JS, Blazar BR, et al. Umbilical cord blood transplantation after nonmyeloablative conditioning: impact on transplantation outcomes in 110 adults with hematologic disease. Blood. 2007;110(8):3064–70.
Kanda J, Rizzieri DA, Gasparetto C, Long GD, Chute JP, Sullivan KM, et al. Adult dual umbilical cord blood transplantation using myeloablative total body irradiation (1350 cGy) and fludarabine conditioning. Biol Blood Marrow Transplant. 2011;17(6):867–74.
Uchida N, Wake A, Nakano N, Ishiwata K, Takagi S, Tsuji M, et al. Mycophenolate and tacrolimus for graft-versus-host disease prophylaxis for elderly after cord blood transplantation: a matched pair comparison with tacrolimus alone. Transplantation. 2011;92(3):366–71.
Kishi Y, Kami M, Miyakoshi S, Kanda Y, Murashige N, Teshima T, et al. Early immune reaction after reduced-intensity cord-blood transplantation for adult patients. Transplantation. 2005;80(1):34–40.
Miyakoshi S, Yuji K, Kami M, Kusumi E, Kishi Y, Kobayashi K, et al. Successful engraftment after reduced-intensity umbilical cord blood transplantation for adult patients with advanced hematological diseases. Clin Cancer Res. 2004;10(11):3586–92.
Uchida N, Wake A, Takagi S, Yamamoto H, Kato D, Matsuhashi Y, et al. Umbilical cord blood transplantation after reduced-intensity conditioning for elderly patients with hematologic diseases. Biol Blood Marrow Transplant. 2008;14(5):583–90.
Osunkwo I, Bessmertny O, Harrison L, Cheung YK, Van de Ven C, del Toro G, et al. A pilot study of tacrolimus and mycophenolate mofetil graft-versus-host disease prophylaxis in childhood and adolescent allogeneic stem cell transplant recipients. Biol Blood Marrow Transplant. 2004;10(4):246–58.
Kiehl MG, Shipkova M, Basara N, Blau IW, Schutz E, Armstrong VW, et al. Mycophenolate mofetil in stem cell transplant patients in relation to plasma level of active metabolite. Clin Biochem. 2000;33(3):203–8.
Hiwarkar P, Shaw BE, Tredger JM, Brown NW, Kulkarni S, Saso R, et al. Mycophenolic acid trough level monitoring: relevance in acute and chronic graft versus host disease and its relation with albumin. Clin Transplant. 2011;25(2):222–7.
Royer B, Larosa F, Legrand F, Gerritsen-van Schieveen P, Berard M, Kantelip JP, et al. Pharmacokinetics of mycophenolic acid administered 3 times daily after hematopoietic stem cell transplantation with reduced-intensity regimen. Biol Blood Marrow Transplant. 2009;15(9):1134–9.
Haentzschel I, Freiberg-Richter J, Platzbecker U, Kiani A, Schetelig J, Illmer T, et al. Targeting mycophenolate mofetil for graft-versus-host disease prophylaxis after allogeneic blood stem cell transplantation. Bone Marrow Transplant. 2008;42(2):113–20.
Papadimitriou JC, Cangro CB, Lustberg A, Khaled A, Nogueira J, Wiland A, et al. Histologic features of mycophenolate mofetil-related colitis: a graft-versus-host disease-like pattern. Int J Surg Pathol. 2003;11(4):295–302.
Mourad M, Malaise J, Chaib Eddour D, De Meyer M, Konig J, Schepers R, et al. Correlation of mycophenolic acid pharmacokinetic parameters with side effects in kidney transplant patients treated with mycophenolate mofetil. Clin Chem. 2001;47(1):88–94.
Mourad M, Malaise J, Chaib Eddour D, De Meyer M, Konig J, Schepers R, et al. Pharmacokinetic basis for the efficient and safe use of low-dose mycophenolate mofetil in combination with tacrolimus in kidney transplantation. Clin Chem. 2001;47(7):1241–8.
Kuypers DR, Claes K, Evenepoel P, Maes B, Vanrenterghem Y. Clinical efficacy and toxicity profile of tacrolimus and mycophenolic acid in relation to combined long-term pharmacokinetics in de novo renal allograft recipients. Clin Pharmacol Ther. 2004;75(5):434–47.
Tredger JM, Brown NW, Adams J, Gonde CE, Dhawan A, Rela M, et al. Monitoring mycophenolate in liver transplant recipients: toward a therapeutic range. Liver Transpl. 2004;10(4):492–502.
van Gelder T, Hilbrands LB, Vanrenterghem Y, Weimar W, de Fijter JW, Squifflet JP, et al. A randomized double-blind, multicenter plasma concentration controlled study of the safety and efficacy of oral mycophenolate mofetil for the prevention of acute rejection after kidney transplantation. Transplantation. 1999;68(2):261–6.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Minagawa, K., Yamamori, M., Katayama, Y. et al. Mycophenolate mofetil: fully utilizing its benefits for GvHD prophylaxis. Int J Hematol 96, 10–25 (2012). https://doi.org/10.1007/s12185-012-1086-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-012-1086-x