Abstract
Reduced-intensity conditioning (RIC) has been facilitating allogeneic hematopoietic cell transplantation (allo-HCT) for patients originally considered ineligible for HCT with myeloablative conditioning. Fludarabine (Flu) with reduced doses of busulfan (Bu) (Flu + Bu) and Flu with reduced doses of melphalan (Mel) (Flu + Mel) are widely used RIC regimens for acute myeloid leukemia (AML). A nationwide retrospective study comparing clinical outcomes of adult patients with AML receiving first allo-HCT after RIC between 2001 and 2010 was performed. Cumulative incidences of relapse were not significantly different among the Flu + ivBu-based (FBiv), Flu + poBu-based (FBpo), and Flu + Mel-based (FM) groups (p = 0.29). Non-relapse mortality (NRM) was significantly lower in patients receiving FBiv compared with FBpo (p = 0.003) and FM (p < 0.001). On multivariate analysis, there was no significant difference in overall survival, but FM was associated with a significantly lower risk of relapse (hazard ratio (HR) = 0.65, 95% confidence interval (CI): 0.50–0.85, p = 0.002), higher NRM (HR = 1.60, 95% CI: 1.10–2.33, p = 0.013) and better leukemia-free survival (HR = 0.77, 95% CI: 0.63–0.95, p = 0.015) compared with FBiv. These results suggest that Flu + Mel has a more intense disease control potential and Flu + ivBu is less toxic than the other. Both RIC regimens provide similar survival outcomes and are effective and useful regimens for patients with AML who received allo-HCT.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic cell transplantation (allo-HCT) is the most curative treatment options for hematological malignancies [1,2,3]. Conditioning regimens are among the important structural elements of HCT. This procedure has two primary goals: to provide sufficient immunoablation for the host to allow adequate engraftment of the donor cells, and to reduce the tumor burden of the underlying disease [4]. Historically, to achieve these goals, myeloablative conditioning (MAC) regimens such as cyclophosphamide combined with total body irradiation (TBI) [5] or with busulfan (Bu) [6] have been developed over the past 40 years. However, in the early years, toxicity from MAC was one of the major causes of mortality after HCT, so many patients were considered ineligible for transplantation because of advanced age or unacceptable risks associated with this treatment [7]. Over the past two decades, as immunologic reactions of donor cells against host leukemic cells after HCT were recognized, less toxic and more tolerable conditioning regimens called reduced-intensity conditioning (RIC) or nonmyeloablative conditioning have been developed. Though these regimens must have sufficient immunosuppression for engraftment, they can attenuate their cytotoxicity without compromise of their antileukemic action because of the presence of graft-versus-leukemia effects [7].
A purine analog, fludarabine (Flu), was introduced in the development of the conditioning regimens for allo-HCT in the 1990s [8]. Flu is generally well tolerated and has a sufficient immunosuppressive effect, along with a synergistic effect with alkylating agents [9]. This drug serves as the backbone of most RIC regimens with a reduced dose of alkylating agents and/or a reduced dose of TBI [7]. In allo-HCT for acute myeloid leukemia (AML), Flu with reduced doses of Bu (Flu + Bu) [10] and Flu with reduced doses of melphalan (Mel) (Flu + Mel) [11] are widely used RIC regimens [12,13,14]. There have been several studies for evaluation of Flu-based RIC regimens for AML, but most of them were retrospective analyses or prospective single-arm trials [15,16,17,18,19,20]. The results of these studies were fairly comparable. In some of these studies, the oral form of Bu (poBu) was used. However, interpatient variation of intestinal absorption is a problem with oral Bu [21]. In the late 1990s, an intravenous formulation of Bu (ivBu) was developed. IvBu is expected to stabilize the pharmacokinetics of Bu in each patient and perhaps improve clinical outcomes [22,23,24,25]. In Japan, ivBu was introduced in 2006 [26].
In this nationwide retrospective study, the clinical outcomes of allo-HCT for AML, especially focusing on Flu + ivBu-based (FBiv) RIC regimens, compared with Flu + poBu-based (FBpo) and Flu + Mel-based (FM) ones, were evaluated.
Patients and methods
Study design and data collection
This study was a retrospective multicenter study. Data were provided by the Transplant Registry Unified Management Program, which is managed by the Japan Society for Hematopoietic Cell Transplantation [27]. The population selection criteria included adult patients aged 16 years or older with AML, who received allo-HCT after RIC regimens between 2001 and 2010. We defined a RIC regimen as including the following dosage level according to the report from the Center for International Blood and Marrow Transplant Research [28]: TBI ≤ 5 Gy (nonfractionated) or ≤8 Gy (fractionated), poBu < 9 mg/kg or ivBu < 7.2 mg/kg and Mel < 140 mg/m2. Variables related to patients, diseases and transplants were extracted from the database. Transplant outcomes including engraftment, graft-versus-host disease (GVHD), complications, relapse or disease progression and survival were also collected. Patients lacking the information about key variables, i.e., sex, outcomes, endpoints, a stem cell source and a conditioning regimen, were excluded. The protocol was approved by the institutional review board of St. Luke’s International Hospital. Informed consent was obtained from recipients and donors in accordance with the principles of the Declaration of Helsinki.
Study endpoints and definitions
The primary endpoint of this study was leukemia-free survival (LFS). Secondary endpoints included engraftment, incidences of acute and chronic GVHD, non-relapse mortality (NRM), cumulative incidence of relapse (CIR) and overall survival (OS). All the times to the endpoint were calculated from the date of HCT (day 0). LFS was defined as time to progression of the underlying disease or death from any cause, whichever came first. OS was defined as time to death irrespective of the cause. Relapse was defined as hematological recurrence of AML, with NRM considered a competing event. NRM was defined as time to death while in remission, with relapse considered a competing event. Surviving patients who were free from events were censored at the date of last follow-up. If patients transplanted in active disease failed to achieve complete remission after HCT, the date of relapse was defined as day 0. Times to neutrophil and platelet recovery were defined as the first of 3 consecutive days with an absolute neutrophil count ≥500/µL and a platelet count ≥50,000/µL without transfusion, respectively. Acute GVHD and chronic GVHD were diagnosed and graded by standard criteria [29, 30]. For engraftment and GVHD, relapse and NRM were considered competing events. Cytogenetic abnormalities were classified according to the cytogenetic risk status classification system of the National Comprehensive Cancer Network [31].
Statistical analysis
Probabilities of LFS and OS were calculated by the Kaplan–Meier method. Engraftment, GVHD, NRM, and CIR were estimated by the cumulative incidence method. The log-rank test was used to compare LFS and OS curves and Gray’s test was used for the comparison of cumulative incidence curves. Multivariate analyses were performed using Cox proportional hazards model for LFS and OS, and the Fine–Gray model was used for engraftment, GVHD, relapse, and NRM. All p values were two-sided and p values < 0.05 were considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria, version 3.3.2). More precisely, EZR is a modified version of R commander (version 2.3–2) that was designed to add statistical functions frequently used in biostatistics [32].
Results
Patient characteristics
A total of 1743 patients with AML received first allo-HCT with RIC regimens from January 1, 2001 through December 31, 2010. The regimens were FBiv for 347 (20%) patients, FBpo for 444 (25%), and FM for 430 (25%). These 1221 patients were included in this analysis.
Patient, disease, and transplantation characteristics are summarized in Table 1. The median age of the 1221 patients included in this study was 58 (range: 16–82) years, and 38% (n = 470) were female. Patients whose disease status at transplant was high risk were more frequent in the FM group (61%) than in the FBiv (41%) and FBpo (47%) groups. Nearly half of the patients (48%) in the FBiv group received unrelated bone marrow transplantation, and 60% of the patients in the FM group underwent unrelated cord blood transplantation. FM might be expected to reduce the risk of graft failure after cord blood transplantation [33].
In addition to Flu and Bu or Mel, 66%, 53% and 76% of the patients (n = 806) received low-dose (≤8 Gy) fractionated TBI in the FBiv, FBpo, and FM groups, respectively. Low-dose TBI was expected to reduce the risk of graft failure [34]. The majority of patients in the three groups were given Flu (125–180 mg/m2), and ivBu (6.4 mg/kg), poBu (8 mg/kg), or Mel (80 mg/m2). In the 806 patients who received irradiation, 72% of them (n = 581) received 4 Gy of fractionated TBI. The median doses of TBI were similar in the three groups. The median follow-up of survivors was 600 days in the FBiv group, 1947 days in the FBpo group, and 897 days in the FM group.
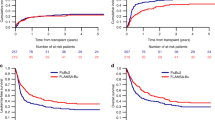
LFS and OS
Both LFS and OS were significantly better in patients with FBiv conditioning than with FM (p = 0.018; p < 0.001, respectively) (Table 2). However, when the patients were stratified by disease status at transplant, LFS and OS among the three conditioning regimens were not significantly different in patients receiving HCT in both standard-risk (p = 0.64; p = 0.74, respectively) and high-risk (p = 0.32; p = 0.089, respectively) cases (data not shown). Multivariate analysis showed that LFS was significantly better in patients with FM (hazard ratio (HR) = 0.77, 95% confidence interval (CI): 0.63–0.95, p = 0.015) than with FBiv conditioning, but there was no significant difference in OS of the FBpo group (HR = 1.21, 95% CI: 0.97–1.51, p = 0.095) and the FM group (HR = 0.90, 95% CI: 0.72–1.13, p = 0.36) compared with the FBiv group (Table 3 and Supplementary Table 1). Adjusted LFS and OS at 3 years were 30.5 (95% CI: 24.3–38.3)% and 35.7 (28.7–44.5)% in patients with FBiv, 28.3 (23.3–34.4)% and 32.8 (27.5–39.2)% with FBpo, and 41.1 (35.4–47.6)% and 47.1(41.4–53.6)% with FM, respectively (Fig. 1). There were significant differences in both adjusted LFS (p = 0.003) and OS (p = 0.018) among the FBiv, FBpo, and FM groups. On the other hand, multivariate analysis only for patients who received allo-HCT between 2006 and 2010 showed that there were no significant differences in both LFS and OS of the FBpo group and the FM group compared with the FBiv group (Supplementary Table 2).
Relapse and NRM
CIRs at 3 years were 42.8 (37.2–48.3)% in the FBiv group, 39.3 (34.7–43.9)% in the FBpo group and 39.4 (34.6–44.2)% in the FM group (Table 2). There was no significant difference in CIR among the three groups. NRMs at 3 years were 18.8 (14.1–24.0)% in the FBiv group, 27.6 (23.5–31.9)% in the FBpo group and 30.2 (25.8–34.6)% in the FM group (Table 2). NRM was significantly lower in patients receiving FBiv regimens compared with FBpo (p = 0.003) and FM (p < 0.001) regimens. Stratified by disease status at transplant, CIRs in the FBiv group (63.5% at 3 years) were significantly higher than in the FM group (50.2% at 3 years) in high-risk (p = 0.008) cases (Fig. 2). NRMs in the FBiv group (17.1 and 21.1% at 3 years) were significantly lower than in the FM group (24.9 and 32.1% at 3 years) both in standard-risk (p = 0.026) and high-risk (p = 0.033) cases (Fig. 3). Multivariate analysis showed that the risk of relapse was significantly lower in patients receiving FM conditioning (HR = 0.66, 95% CI: 0.50–0.85, p = 0.002) than FBiv, and that NRM was significantly higher in the FBpo (HR = 1.84, 95% CI: 1.27–2.64, p = 0.001) and FM (HR = 1.60, 95% CI: 1.10–2.33, p = 0.013) groups than in the FBiv group (Table 3). Only for patients who received allo-HCT between 2006 and 2010, multivariate analysis showed that the risk of relapse was still significantly lower in patients receiving FM conditioning (HR = 0.73, 95% CI: 0.53–0.99, p = 0.042) than FBiv, but that there was no significant difference in NRM of the FBpo group and the FM group compared with the FBiv group (Supplementary Table 2).
The major causes of NRM were graft failure/hematological disorder, infection, GVHD and organ failure in this study. The differences in cumulative incidences of NRM by graft failure, GVHD, and organ failure were not significant among the three conditioning regimens. However, on multivariate analysis, NRM by infection was a higher trend in the patients receiving FM than in those receiving FBiv (Table 4).
Engraftment
Neutrophil engraftment was significantly higher in the FBiv group than in the FBpo and FM groups when the patients received related and unrelated bone marrow and unrelated cord blood. Platelet engraftment was not significantly different among the three groups irrespective of stem cell source (Table 2). On multivariate analysis, there was no significant difference in neutrophil and platelet recovery among the three groups (Table 3).
GVHD
The cumulative incidence of grade II to IV acute GVHD at day 100 was 33.3 (28.2–38.5) % in the FBiv group, 37.3 (32.5–42.2)% in the FBpo group, and 44.9 (39.7–50.0)% in the FM group (Table 2). It was significantly lower in patients undergoing FBiv regimens, compared with FM (p = 0.003). The cumulative incidence of grade III to IV acute GVHD was significantly lower in the FBiv group than in the FM groups. After adjustment for variables with a different distribution in the FBiv and FM groups, the incidences of grade II to IV acute GVHD and chronic GVHD were significantly higher in patients with FM than in those with FBiv (Table 3).
Discussion
In the present study, the clinical outcomes of adult patients with AML who underwent allo-HCT with RIC regimens were evaluated, focusing on FBiv conditioning compared with FBpo and FM.
In allo-HCT for AML, Flu + Bu, and Flu + Mel are widely used RIC regimens. Flu + Bu (Flu 180 mg/m2 and poBu 8 mg/kg) was first reported by Slavin et al. [10]. Since then, several investigators have further explored this regimen in myeloid malignancies [15,16,17,18]. Investigators at MD Anderson Cancer Center first reported results with a RIC regimen consisting of Flu 125 mg/m2 and Mel 100–140 mg/m2 in patients [11]. This regimen has subsequently been investigated at other centers, yielding similar results [19].
The studies of Flu + Bu conducted in the 1990s contained poBu, which was associated with individual variations in intestinal absorption and plasma Bu levels [21]. In the late 1990s, ivBu was developed and was expected to stabilize the plasma concentration of Bu in each patient. Decreased variability in plasma Bu levels with ivBu was reported to reduce sinusoidal obstruction syndrome and 100-day mortality [24, 35, 36].
In the present study, multivariate analysis showed there was no significant difference in OS among patients with AML receiving allo-HCT with the FBiv, FBpo, and FM regimens, but the FM group had a significant advantage in LFS compared with the FBiv group. The present results also indicated that the risk of relapse for the patients receiving FM decreased significantly compared with FBiv, while NRM was significantly higher in patients with FBpo or FM than that in patients with FBiv. These results could be affected by the progress in supportive care during the study period. Multivariate analysis only for patients who received allo-HCT between 2006 and 2010 showed no significant difference in survival outcomes among transplant recipients with the three regimens. We also analyzed the impact of conditioning regimens on transplant outcomes by stem cell source, but there was no significant difference in OS among the patients with the FBiv, FBpo, and FM regimens in each stem cell source. But about LFS, the FBpo group had a significant disadvantage among the patients who received related bone marrow transplantation, and the FM group had a marginally significant advantage among those who received unrelated cord blood transplantation, compared with the FBiv group (Supplementary Table 3).
There are already several retrospective studies comparing Flu + Bu with Flu + Mel. Three of these studies are summarized in Supplementary Table 4 (refs. [37,38,39]). The present study, as well as these three studies, showed that CIR was significantly lower for patients receiving FM than for those receiving FBiv. In the present study, the total Mel dose was limited to less than 140 mg/m2 according to the definition of RIC, and most patients were given 80 mg/m2 [40]. But in the three studies, the Flu + Mel regimens consisted of 100–140 or 130–150 mg/m2 of Mel. This result indicated that, despite the use of a reduced dose of Mel, Flu + Mel might be more intense and have inherently higher antileukemia potential than Flu + Bu.
In the present study, NRM was significantly lower in the FBiv group than in the FBpo and FM groups. This finding was in agreement with Shimoni et al. and Eapen et al., and the study from the European Society for Blood and Marrow Transplantation also suggested a lower NRM for patients with Flu + Bu than for those with Flu + Mel. This increase in NRM might be attributable to the severe toxicities of Mel. In the present study, NRM by infection was a higher trend in the patients receiving FM than in those receiving FBiv. Severe infection during the early phase of HCT following mucosal barrier damage caused by Mel as a part of a conditioning regimen may have contributed to the increase of NRM [37]. The higher incidence of acute GVHD with FM observed in the present comparison was also likely the result of the increased tissue injury caused by Mel and release of inflammatory cytokines involved in GVHD pathogenesis [41, 42].
Baron et al. suggested that patients receiving Flu + Bu were more likely to have a mixed chimera early after HCT and a higher incidence of graft failure than those receiving Flu + Mel [39, 43]. However, in the present study, multivariate analysis showed there were no significant differences in neutrophil and platelet recoveries between the FBiv and FM groups. We examined the impact of TBI on transplant outcomes. Multivariate analysis by conditioning regimen showed that TBI had a positive impact on LFS and OS only in the FBpo group (Supplementary Table 5). Another subgroup analysis stratified by stem cell source indicated that low-dose TBI significantly reduced the risk of relapse only in the HCT recipients of related peripheral blood or unrelated bone marrow (Supplementary Table 3). These results suggest that TBI had a certain role in engraftment and antileukemia effect, but the influence of low-dose TBI on the FBiv and FM regimens was limited in this comparative study.
It is important to recognize that this retrospective study had some limitations. First, there was no information related to why individual patients were designated to receive specific conditioning regimens. Second, there were diverse characteristics among the patient groups such as age, disease status at transplant, and stem cell sources. Therefore, multivariate analyses were performed to adjust for the effects of these differences on the results. Another limitation is that there was not enough information about late complications for analysis in the dataset. Quality of life in long-term survivors should be one of the critical factors in the comparison of RIC regimens.
In summary, a nationwide retrospective study was performed using a cohort of adult patients with AML undergoing allo-HCT to compare the clinical outcomes of FBiv with those of FBpo and FM. LFS was significantly higher and CIR was significantly lower in the FM group than in the FBiv group. Thus, Flu + Mel appears to have a more intense antileukemia potential than Flu + ivBu. On the other hand, NRM was significantly lower in the FBiv group than in the FBpo and FM groups. This finding indicates that Flu + ivBu is a less toxic RIC regimen than Flu + Mel. Introduction of ivBu instead of poBu also contributed to decreased toxicity. Finally, the three groups had almost the same OS. Though prospective randomized studies are needed to confirm these results, the results from the present study offer convincing evidence that both Flu + ivBu and Flu + Mel are effective and useful RIC regimens for patients with AML who receive allo-HCT.
References
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N. Engl J Med. 2008;358:1909–18.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301:2349–61.
Cornelissen JJ, van Putten WL, Verdonck LF, Theobald M, Jacky E, Daenen SM, et al. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood. 2007;109:3658–66.
Gyurkocza B, Sandmaier BM. Conditioning regimens for hematopoietic cell transplantation: one size does not fit all. Blood. 2014;124:344–53.
Thomas ED, Clift RA, Hersman J, Sanders JE, Stewart P, Buckner CD, et al. Marrow transplantation for acute nonlymphoblastic leukemic in first remission using fractionated or single-dose irradiation. Int J Radiat Oncol Biol Phys. 1982;8:817–21.
Tutschka PJ, Copelan EA, Klein JP. Bone marrow transplantation for leukemia following a new busulfan and cyclophosphamide regimen. Blood. 1987;70:1382–8.
Sengsayadeth S, Savani BN, Blaise D, Malard F, Nagler A, Mohty M. Reduced intensity conditioning allogeneic hematopoietic cell transplantation for adult acute myeloid leukemia in complete remission—a review from the Acute Leukemia Working Party of the EBMT. Haematologica. 2015;100:859–69.
Jethava YS, Sica S, Savani B, Socola F, Jagasia M, Mohty M, et al. Conditioning regimens for allogeneic hematopoietic stem cell transplants in acute myeloid leukemia. Bone Marrow Transpl. 2017;52:1504–11.
Shimoni A, Nagler A. Optimizing the conditioning regimen for allogeneic stem-cell transplantation in acute myeloid leukemia; dose intensity is still in need. Best Pr Res Clin Haematol. 2011;24:369–79.
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood. 1998;91:756–63.
Giralt S, Estey E, Albitar M, vanBesien K, Rondon G, Anderlini P, et al. Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy. Blood. 1997;89:4531–6.
Sandmaier BM, Mackinnon S, Childs RW. Reduced intensity conditioning for allogeneic hematopoietic cell transplantation: current perspectives. Biol Blood Marrow Transpl. 2007;13:87–97.
McClune BL, Weisdorf DJ, Pedersen TL, Tunes da Silva G, Tallman MS, Sierra J, et al. Effect of age on outcome of reduced-intensity hematopoietic cell transplantation for older patients with acute myeloid leukemia in first complete remission or with myelodysplastic syndrome. J Clin Oncol. 2010;28:1878–87.
Chevallier P, Szydlo RM, Blaise D, Tabrizi R, Michallet M, Uzunov M, et al. Reduced-intensity conditioning before allogeneic hematopoietic stem cell transplantation in patients over 60 years: a report from the SFGM-TC. Biol Blood Marrow Transpl. 2012;18:289–94.
Kröger N, Schetelig J, Zabelina T, Krüger W, Renges H, Stute N, et al. A fludarabine-based dose-reduced conditioning regimen followed by allogeneic stem cell transplantation from related or unrelated donors in patients with myelodysplastic syndrome. Bone Marrow Transpl. 2001;28:643–7.
Ho AY, Pagliuca A, Kenyon M, Parker JE, Mijovic A, Devereux S, et al. Reduced-intensity allogeneic hematopoietic stem cell transplantation for myelodysplastic syndrome and acute myeloid leukemia with multilineage dysplasia using fludarabine, busulphan, and alemtuzumab (FBC) conditioning. Blood. 2004;104:1616–23.
Mohty M, Bay JO, Faucher C, Choufi B, Bilger K, Tournilhac O, et al. Graft-versus-host disease following allogeneic transplantation from HLA-identical sibling with antithymocyte globulin-based reduced-intensity preparative regimen. Blood. 2003;102:470–6.
Valcarcel D, Martino R, Caballero D, Martin J, Ferra C, Nieto JB, et al. Sustained remissions of high-risk acute myeloid leukemia and myelodysplastic syndrome after reduced-intensity conditioning allogeneic hematopoietic transplantation: chronic graft-versus-host disease is the strongest factor improving survival. J Clin Oncol. 2008;26:577–84.
Oran B, Giralt S, Saliba R, Hosing C, Popat U, Khouri I, et al. Allogeneic hematopoietic stem cell transplantation for the treatment of high-risk acute myelogenous leukemia and myelodysplastic syndrome using reduced-intensity conditioning with fludarabine and melphalan. Biol Blood Marrow Transpl. 2007;13:454–62.
Nakamura R, Rodriguez R, Palmer J, Stein A, Naing A, Tsai N, et al. Reduced-intensity conditioning for allogeneic hematopoietic stem cell transplantation with fludarabine and melphalan is associated with durable disease control in myelodysplastic syndrome. Bone Marrow Transpl. 2007;40:843–50.
Grochow LB. Busulfan disposition: the role of therapeutic monitoring in bone marrow transplantation induction regimens. Semin Oncol. 1993;20:18–25. quiz 26.
Andersson BS, Madden T, Tran HT, Hu WW, Blume KG, Chow DS, et al. Acute safety and pharmacokinetics of intravenous busulfan when used with oral busulfan and cyclophosphamide as pretransplantation conditioning therapy: a phase I study. Biol Blood Marrow Transpl. 2000;6:548–54.
Andersson BS, Gajewski J, Donato M, Giralt S, Gian V, Wingard J, et al. Allogeneic stem cell transplantation (BMT) for AML and MDS following i.v. busulfan and cyclophosphamide (i.v. BuCy). Bone Marrow Transpl. 2000;25:S35–8.
Andersson BS, Kashyap A, Gian V, Wingard JR, Fernandez H, Cagnoni PJ, et al. Conditioning therapy with intravenous busulfan and cyclophosphamide (IV BuCy2) for hematologic malignancies prior to allogeneic stem cell transplantation: a phase II study. Biol Blood Marrow Transpl. 2002;8:145–54.
Shimoni A, Bielorai B, Toren A, Hardan I, Avigdor A, Yeshurun M, et al. Intravenous busulfan-based conditioning prior to allogeneic hematopoietic stem cell transplantation: myeloablation with reduced toxicity. Exp Hematol. 2003;31:428–34.
Kim SW, Mori SI, Tanosaki R, Fukuda T, Kami M, Sakamaki H, et al. Busulfex (i.v. BU) and CY regimen before SCT: Japanese-targeted phase II pharmacokinetics combined study. Bone Marrow Transpl. 2009;43:611–7.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–74.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transpl. 2009;15:367–9.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17.
National Comprehensive Cancer Network. Acute myeloid leukemia (Version 2.2018). 2018. https://www.nccn.org/professionals/physician_gls/default.aspx#aml. Accessed 17 Aug 2018.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Miyakoshi S, Yuji K, Kami M, Kusumi E, Kishi Y, Kobayashi K, et al. Successful engraftment after reduced-intensity umbilical cord blood transplantation for adult patients with advanced hematological disease. Clin Cancer Res. 2004;10:3586–92.
Onishi Y, Mori S, Kusumoto S, Sugimoto K, Akahane D, Morita-Hoshi Y, et al. Unrelated-donor bone marrow transplantation with a comditioning regimen including fludarabine, busulfan, and 4 Gy total body irradiation. Int J Hematol. 2007;85:256–63.
Kashyap A, Wingard J, Cagnoni P, Roy J, Tarantolo S, Hu W, et al. Intravenous versus oral busulfan as part of a busulfan/cyclophosphamide preparative regimen for allogeneic hematopoietic stem cell transplantation: decreased incidence of hepatic venoocclusive disease (HVOD), HVOD-related mortality, and overall 100-day mortality. Biol Blood Marrow Transpl. 2002;8:493–500.
Sobecks RM, Rybicki L, Yurch M, Kalaycio M, Dean R, Andresen S, et al. Intravenous compared with oral busulfan as preparation for allogeneic hematopoietic progenitor cell transplantation for AML and MDS. Bone Marrow Transpl. 2012;47:633–8.
Shimoni A, Hardan I, Shem-Tov N, Rand A, Herscovici C, Yerushalmi R, et al. Comparison between two fludarabine-based reduced-intensity conditioning regimens before allogeneic hematopoietic stem-cell transplantation: fludarabine/melphalan is associated with higher incidence of acute graft-versus-host disease and non-relapse mortality and lower incidence of relapse than fludarabine/busulfan. Leukemia. 2007;21:2109–16.
Baron F, Labopin M, Peniket A, Jindra P, Afanasyev B, Sanz MA, et al. Reduced-intensity conditioning with fludarabine and busulfan versus fludarabine and melphalan for patients with acute myeloid leukemia: A report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer. 2015;121:1048–55.
Eapen M, Brazauskas R, Hemmer M, Perez WS, Stenert P, Horowitz MM, et al. Hematopoietic cell transplant for acute myeloid leukemia and myelodysplastic syndrome: conditioning regimen intensity. Blood Adv. 2018;2:2095–103.
Yuji K, Miyakoshi S, Kato D, Miura Y, Myojo T, Murashige N, et al. Reduced-intensity unrelated cord blood transplantation for patients with advanced malignant lymphoma. Biol Blood Marrow Transpl. 2005;11:314–8.
Ferrara JL. Pathogenesis of acute graft-versus-host disease: cytokines and cellular effectors. J Hematother Stem Cell Res. 2000;9:299–306.
Harris AC, Ferrara JL, Braun TM, Holler E, Teshima T, Levine JE, et al. Plasma biomarkers of lower gastrointestinal and liver acute GVHD. Blood. 2012;119:2960–3.
Baron F, Sandmaier BM. Chimerism and outcomes after allogeneic hematopoietic cell transplantation following nonmyeloablative conditioning. Leukemia. 2006;20:1690–700.
Acknowledgements
The authors would like to acknowledge all of the HCT recipients, donors, and their families, all of the HCT teams in Japan, and the members of the adult AML working group of the Japan Society for Hematopoietic Cell Transplantation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yamashita, T., Takami, A., Uchida, N. et al. Reduced-intensity stem cell transplantation for acute myeloid leukemia with fludarabine-based conditioning with intravenous busulfan versus melphalan. Bone Marrow Transplant 55, 1955–1965 (2020). https://doi.org/10.1038/s41409-020-0856-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0856-y
- Springer Nature Limited
This article is cited by
-
Predicting non-relapse mortality following allogeneic hematopoietic cell transplantation during first remission of acute myeloid leukemia
Bone Marrow Transplantation (2021)