Abstract
Inguinal hernia is a common disorder of childhood that requires surgical repair at diagnosis. Traditionally, it is operated upon by open inguinal incision. However, with the introduction of laparoscopic repair in 1990, opinion of scientific community is divided concerning the best method of pediatric herniotomy. Educated parents, who long to have the choicest of the best, often gather information from internet and prefer to discuss their concerns with primary care physicians. This descriptive review is intended to provide practicing pediatricians with updated evidence-based information which will enable them to counsel parents regarding the choice of hernia repair. Based on careful analysis of current literature, unacceptable standards are defined in this paper and rationalized recommendations are proposed. Laparoscopy appears to be beneficial in bilateral hernia of girls, giant hernia, recurrence following failed open repair and in hernia associated with undescended testis or ambiguous genitalia. On the other hand, open herniotomy appears to be advantageous in male inguinal hernia, unilateral female hernia, premature newborns, failed laparoscopic repair and in hernia associated with serious co-morbidity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
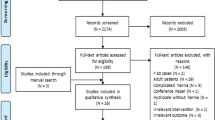
Introduction
Inguinal hernia (IH) is an extremely common disorder of childhood that necessitates surgical repair at diagnosis [1]. Its incidence is variously reported as 0.5% to 14% [2]. By projecting this upon the 363 million pediatric population of India [3], it is roughly estimated that every year, 4 to 6 lakhs children must have been undergoing inguinal hernia repair (IHR) in the Indian subcontinent. Therefore, a practicing pediatrician is likely to see, on an average, one or two cases every week. Parents often prefer to discuss their concerns with primary care physicians rather than surgeons. Prior to 1990s, pre-operation counseling was relatively easy because all IH were repaired by a standard groin-incision technique. However, with the advent of laparoscopic surgery it became difficult to keep track of the newly introduced surgical techniques and their relative ‘merits and demerits’. The scenario is further complicated by free availability of medical information through internet, improved public awareness, utopian desire of every parent to give their child the choicest of the best, growing intolerance of even minor adverse events and an increasingly litigious society. Therefore, accurate and evidence-based counseling is essential to avoid parental dissatisfaction and legal disputes. This review is intended to provide pediatricians with scientific information as to the best method of repairing pediatric IH.
General Comparison of Available Options
The basic aim of all IHRs is to prevent protrusion of abdominal viscera by obliterating the hernial sac. In adults, as the hernial sac is acquired due to weakness of abdominal musculatures, prosthetic mesh reinforcement (hernioplasty) is invariably required for radical cure. Contrarily, as pediatric IH is due to congenital patency of processus vaginalis, surgical disconnection of the sac (herniotomy) is sufficient. This principal difference prohibits drawing of pediatric inferences from adult literature.
Pediatric IH is conventionally repaired by open herniotomy (OH) in which the hernial sac is dissected off the cord structures and divided at the level of the deep ring through a 2 to 3 cm- long inguinal incision. Technical variations of OH are fewer (Table 1), rarely practiced and they do not differ significantly in their outcome [4].
Laparoscopic herniotomy (LH) is classically done by 3-port technique in which the optical telescope (representing the surgeon’s eyes) is inserted through the central port and working instruments (representing the surgeon’s two arms) are inserted on either side of it. Suturing the neck of hernial sac rather than its complete excision is typical of LH (Fig. 1a, b). In contrast to OH, technical variations are plenty in laparoscopy (Table 2). Reducing the number of access ports, method of dealing with the neck of hernial sac and the technique of suturing are the principal themes of modifications. Quite dissimilar to OH, technical modifications of LH significantly differ in their outcome. For example, repair integrity is better with Dissection-Division-Suturing (DDS) of the neck of hernial sac than with other techniques [5]. Recurrences are fewer with linear suturing of deep ring than with purse-string closure [6]. Non-absorbable sutures give better long-term cure than absorbable materials [7]. However, the final outcome was not dependant on the number of access ports [8]. Further, LH in general, and each of its variations in particular, have a definite learning curve [9]. Therefore, outcome of LH varies not only with different techniques but also according to the level of surgeon’s experience.
Comparison of Outcome Parameters
Owing to its technical simplicity, high success and low complication rates Ferguson’s OH is widely considered as the Gold Standard against which all other techniques are evaluated. Several parameters [10] have been suggested for comparative assessment of outcome (Table 3). Superiority of a technique is sometimes claimed on the basis of logical extrapolations and hypothetical assumptions. Conclusions of randomized controlled trials (RCT) and meta-analyses simply demonstrate statistical superiority while critical appraisal is essential to infer clinical relevance [11].
Operation Time
In bilateral lesions, LH is consistently found to be quicker than OH [12,13,14]. This is because laparoscopy saves time by utilizing the same set of ports to repair both sides whereas OH requires separate incisions for each side. Unlike in OH, layers of abdominal wall are not sutured in LH. Probably this compensates the initial time spent in establishing laparoscopic pneumoperitoneum. In contrast to bilateral hernia there is no consensus in unilateral cases. Duration of LH is variously concluded in different meta-analyses as longer [12], similar [13] or shorter [14] than OH. This suggests that operation time is determined more by dexterity of surgeons rather than by surgical techniques. The reported mean difference of 5 to 15 min between OH and LH may be statistically significant; but it is of no practical importance.
Collateral Injury to Adjacent Structures
IHR involves dissection of hernial sac from the vas deferens and testicular vessels. Therefore, in every hernia repair, iatrogenic injury to these structures is a theoretical risk. Vas injury is reported in 0.13% to 0.5% of pediatric herniotomies [15] and it is responsible for 6.6% of male infertility [16]. In LH, dissection of hernial sac is altogether avoided by suturing the neck of sac. Even in DDS technique of LH, dissections are minimal and are done at internal ring level where the vas and vessels are divergent. Further, optical magnification of laparoscope is hypothesized to reduce operative injury. However, actual clinical data in support of these assumptions are extremely scarce. In adults undergoing bilateral hernia repair, obstructive azoospermia was noted in 0.03% of open repairs and 2.5% of laparoscopic procedures [17]. In a small retrospective series, intraoperative vas injury was recognized in 7% of LH as compared to 0% in OH [18]. Nevertheless, unilateral injury to the vas deferens is extremely difficult to recognize as it remains asymptomatic and is well compensated by contralateral spermatogenesis. None of the RCTs comparing LH with OH has sufficient sample size to assess true risk of vas injury.
Ischemic atrophy of testis has been reported in 0.5% to 5.8% of boys undergoing herniotomy [19]. Atrophy rate goes as high as 10% in incarcerated hernias. Recent studies have shown that both OH and LH do not significantly alter testicular perfusion although it is transiently impaired in OH [20, 21].
Chronic groin pain, reported in 5% to 13% of OH, is attributed to operative disruption or suture entrapment of groin nerves [22]. LH is expected to avoid nerve injury as it approaches the hernial sac from peritoneal surface. Electrophysiological studies have indeed confirmed that conductivity of genitofemoral nerve is significantly better with LH than with OH [23]. However, practical implications of this observation are yet to be established. Interestingly, deliberate prophylactic neurectomy of inguinal nerves is recommended in adults to avoid chronic groin pain [24].
Post-operative Pain
Laparoscopy, being a minimally invasive procedure, is generally expected to cause less pain and hence less analgesic requirement. Three single-blind RCTs reached contradicting conclusions. A Chinese study [25] confirmed that LH is less painful; while a Finnish RCT found it actually more painful than OH [26]. Increased pain of laparoscopy is thought to be due to stretching of peritoneum by CO2 pneumoperitoneum. Another RCT from Turkey found that pain scores and analgesic requirement were not statistically different between LH and OH [27]. One meta-analysis [13] concluded that postoperative pain in LH is comparable to that of OH while another meta-analysis [12] found the evidences insufficient to make any firm conclusion. These contradictory results can be explained by the practical problem of quantifying pain. Being a subjective sensation, children often find it difficult to accurately express their pain. Further, patient bias and observer bias could not excluded in the absence of a well designed double-blind RCT.
Noteworthily, shoulder pain which is seen in 5% to 17% of LH patients has never been reported in OH [26, 27]. As this referred pain is attributed to phrenic nerve irritation caused by pneumoperitoneum, it is an exclusive complication of LH. Intraperitoneal instillation of local anesthetics at the conclusion of laparoscopy is suggested to reduce shoulder pain.
Immediate Post-operative Complications
Unlike OH extensive tissue dissection is not done in LH. Therefore dissection-related complications such as hematoma, wound infection and scrotal edema are expected to be lesser with LH [14]. Pooled data of a systematic review suggested that these complications occur in 0.9% of LH as against 2.7% of OH [28]. However, a meta-analysis did not find any significant difference in the complication rate of LH and OH [13]. This discrepancy is probably due to reporting bias and selection bias.
Recurrence
Recurrence after surgical repair of hernia may be of two types: ipsilateral recurrences (ILR) indicate failure of repair while contralateral recurrences (CLR) are de novo lesions of the opposite side. In published literature, the term ‘recurrence’ has often been confusingly used to denote both of them.
Initially, LH was apprehended to have more ILR as the sac is simply ligated rather than excised. Reported incidence of ILR is 0% to 6% in OH and 0% to 5.5% in LH. Pooled data of 11,142 patients [28] and a meta-analysis [13] confirmed that a mean ILR rate of 1.4% is identical between the two groups. Correlation between ipsilateral recurrence and various techniques of LH is well known (vide supra). Prematurity, age less than 1 y, obstructed hernia and presence of co-morbidities may also increase ILR as high as 15% in both the groups [29, 30].
In unilateral hernias the chances of having a patent sac on the opposite side is as high as 50% [31]. Several decades ago pediatric surgeons routinely performed bilateral exploration in unilateral hernias. However, only 7% of such children developed contralateral hernia implying that all patent sacs need not necessarily become clinical hernia [32, 33]. Therefore the routine practice of contralateral exploration has been given up in open surgery. Introduction of laparoscopy rekindled the interest in contralateral patent sac [34]. Laparoscopy enables examination and suturing of contralateral sac without the need for any additional incision. Indeed, studies have shown that routine prophylactic suturing of contralateral sac reduces metachronous hernia from 7% to 0.3% [29, 35]. This approach required ligation of 4 to 6 sacs to prevent one future hernia [35]. Thus a vast majority of children underwent needless intervention. Further, negative laparoscopy did not completely eliminate the risk of future CLR. It is found to occur in 1% to 3% within 3 mo to 5 y of negative laparoscopy [36, 37]. Incidence of CLR is proportionate to the length of follow-up. Several studies quoting a low rate of CLR with LH suffer from insufficient follow-up. Routine bilateral intervention increases the operation time and thereby, substantially increases the cost of care [38].
Hospital Stay
Pediatric herniotomy is usually done as a day-care surgery. Therefore, the benefit of shorter hospital stay that is typical of laparoscopy is not expected in LH. Although an RCT [26] reported that LH needed prolonged hospital stay than OH (5 h vs. 3.8 h), this difference is of no practical significance. Recent meta-analysis [13] affirmed that there is no significant difference in the duration of hospital stay between the two procedures.
Time to Resume Full Activity
In both LH and OH children resume normal activities within 2.5 d [26]. A meta-analysis also confirmed that there is no significant difference between the procedures [13]. This could be a corollary to the fact that OH and LH do not differ significantly in post-operative pain score.
Cost of Treatment
Laparoscopy requires costly instruments and general anesthesia. Hence the cost of LH is 2 to 3-fold higher than that of OH [39]. It is not known whether this high cost is justified in terms of improved quality of life in pediatric age group. Unlike other laparoscopic surgeries the high instrument cost of LH is not compensated by shorter hospital stay in pediatric IHR.
Cosmesis and Parental Satisfaction
Cosmetic results of LH are slightly better than that of OH in the early post-operative period. Unsightly scars were noted in 4% of OH while none in LH [40]. However this difference tends to fade away with passage of time as scars mature and flatten. An RCT found that cosmetic score of LH is better than that of OH in bilateral hernia but not in unilateral cases [27]. Another RCT found that parental satisfaction scores of OH and LH were no different at 2 y of repair [26]. It is also pointed out that cosmetic emphasis is unimportant, given the location of OH scar which is well concealed even by swim suits (Fig. 2) [11].
Scar cosmesis of herniotomy (a) shows two inguinal scars (arrows) of bilateral hernia repair. As early as 6 mo after surgery they are camouflaged by the skin crease and are very well below the swim-suite line. Over subsequent years the scars are expected to further flatten-out and become barely visible (b) shows two working-port scars (arrows) of laparoscopic unilateral hernia repair. (Scar of telescopic port has merged with umbilical folds) Even after 8 y of repair they are prominently visible above the waist line (Figure 2b courtesy of Prof. Y. K. Sarin, New Delhi)
Procedure Specific Complications
In LH, as the sac is simply ligated rather than being excised, exudates trapped inside the distal sac were apprehended to cause hydrocele. The reported incidence of hydrocele is 0.2% to 5.7% in LH as compared to 2.9% to 6.6% in OH [28]. However a meta-analysis found this difference statistically insignificant. Further, such hydroceles are noted to resolve spontaneously within 3 wk [40].
Testicular displacement during open dissection was thought to cause post-operative ascend of testis (iatrogenic cryptorchidism). LH, which altogether avoids handling testis is expected to annihilate this complication [41]. Surprisingly, it is reported to occur in 0% to 5.9% of LH while only 1.7% to 3.2% in OH [28]. A recent study even suggested that tissue adhesions formed between cord structure and inguinal canal in OH is actually protective while the intact smooth sac left behind in LH facilitates upward migration of testis [42]. However, a meta-analysis found no significant difference between the groups [13].
Visualization of internal ring in LH confirms the patency of sac and hence the mistake of operating on wrong side is unlikely in LH. However, hard data to support this assumption is lacking.
Anesthesia Related Concerns
Unlike OH which can be done under regional or local anesthesia, LH invariably requires general anesthesia. The later is widely acknowledged to be riskier than the former especially in preterm infants and in the presence of cardio-respiratory disorders. General anesthesia also increases the risk of post-operative apnea, prolongs recovery time and escalates cost of care. Drugs used in inhalation anesthesia are now thought to adversely affect the developing brain.
Pneumoperitoneum of laparoscopy, not only impedes venous return by increasing intrabdominal pressure but also leads to acidosis by absorption of carbon dioxide. A recent study has shown that these factors really affect brain oxygenation during LH [43]. Fortunately, the changes are quickly compensated by homeostatic adaptive mechanism.
Surgeon’s Learning Curve
LH is associated with a definite learning curve which is much longer than OH [44]. Consultants required 13 operations while residents needed 30 operations to learn the proper technique [9]. It is really not known if surgeons with sub-optimal exposure compromise patient safety.
Comparison of Specific Situations
Unilateral vs. Bilateral
Bilateral LH has been acknowledged to be better than OH or unilateral LH in terms of shorter operation time and short-term cosmetic results [14]. Even in unilateral hernias routine prophylactic repair of opposite side sac may be theoretically advantageous [34].
Infants and Neonates vs. Older Children
Post-operative apnea and carbon dioxide pneumoperitoneum of LH were initially considered harmful to neonates and premature infants. Several studies attested the safety of laparoscopy in these vulnerable infants [45, 46]. It is even suggested that in neonates LH is technically less demanding than OH as it avoids any dissection of sac [47]. However, post-operative complications were 5.5% in term babies while it increased to 20% in preterm infants [48]. Similarly, serious respiratory compromise following LH occurred in 5% of premature babies as against only 1.5% of term newborn [48]. This raises serious concerns against LH in premature babies.
Male vs. Female
Although the trouble of dissecting vas and vessels is circumvented in LH, purse-string suture sans dissection is feared to cause kinking of vas. However in practice, vas injury of OH and LH are identical (vide supra). In females, often a loop of fallopian tube is found adherent to hernial sac. Unintentional ligation of fallopian tube is predicted to be less likely with LH because the internal anatomy is well visualized before ligation of sac [49]. Rarely androgen insensitivity (male pseudohermaphroditism) may present with female phenotype and bilateral inguinal hernia. In such patients laparoscopy offers the advantage of easy inspection of pelvic organs to confirm absence of uterus.
Giant vs. Regular Size Hernia
Huge hernial sacs involve extensive dissection in OH and hence are associated with increased risk of hematoma, scrotal edema and injury to adjacent structures. Laparoscopic suturing of internal ring without any attempt to dissect the sac is expected to minimize these complications [50]. However, large hernias post enormous technical challenges during LH so that 6% of the procedures have to be converted to OH [50].
Emergency vs. Elective Herniotomy
Edematous hard structures of obstructed hernia are highly vulnerable for operative injuries during emergency repair. LH is considered to be advantageous as it avoids dissection of vas and vessels [51]. In a small series, serious complications were noted in 8% of emergency OH as compared to 1.6% with emergency LH [52]. Further, LH facilitates reduction of strangulated intestine by widening the internal ring and also helps in confirming the viability of reduced bowel. Contrarily, distended or gangrenous bowel may pose technical limitations to LH. An English study found that both OH and LH are of comparable results in emergency settings [52].
Presence vs. Absence of Co-morbidity
Anecdotal observations suggest that LH is advantageous in the presence of co-morbidities such as obesity, ambiguous genitalia and multiple hernias which occur in 0.1% of pediatric inguinal hernias. On the other hand LH may be potentially detrimental in co-morbidities such as congenital heart diseases, respiratory problems and connective tissue disorders. In hernias associated with undescended testis a combined repair of both using a laparoscope is probably comparable to that of open surgery [53].
Recurrent vs. Virgin Hernia
Adhesions of previous operation pose great technical hindrance during re-operation for ipsilateral recurrence [54, 55]. In such a scenario, surgical approach avoiding previous route is desirable. Therefore recurrence after LH is better repaired by OH and vice versa [56].
Concluding Recommendations
An international survey of pediatric surgeons found that OH is often preferred than LH [57]. In the absence of clear superiority of one procedure over the other, the choice of repair should be left to preferences of parents and treating surgeon. Decision making is facilitated by clearly defining criteria of unacceptable results (Table 3). Hospital stay more than 1 d (2 nights), any death attributable to hernia repair, re-admission within 30 d for complications or re-operation within 1 y for recurrence should be considered unacceptable with either OH or LH [10]. After carefully weighing of current evidences authors’ recommendation as to choice of pediatric hernia repair is summarized in Table 4.
References
Esposito C, Escolino M, Turrà F, et al. Current concepts in the management of inguinal hernia and hydrocele in pediatric patients in laparoscopic era. Semin Pediatr Surg. 2016;25:232–40.
Pan ML, Chang WP, Lee HC, et al. A longitudinal cohort study of incidence rates of inguinal hernia repair in 0- to 6-y-old children. J Pediatr Surg. 2013;48:2327–31.
Office of the Registrar General & Census Commissioner, India. Available at: http://censusindia.gov.in. Accessed on 16 Feb 2017.
Ibrahim M, Ladan MA, Abdussalam US, et al. Open inguinal herniotomy: analysis of variations. Afr J Paediatr Surg. 2015;12:131–5.
Mora MC, Bittner KR, Wong KE, et al. Laparoscopic pediatric inguinal hernia repair: a pilot study in a novel guinea pig animal model. J Laparoendosc Adv Surg Tech A. 2016; doi:10.1089/lap.2016.0486.
Lee SR, Choi SB. The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia. 2016; doi:10.1007/s10029-016-1546-y.
Grimsby GM, Keays MA, Villanueva C, et al. Non-absorbable sutures are associated with lower recurrence rates in laparoscopic percutaneous inguinal hernia ligation. J Pediatr Urol. 2015;11:e1–4.
Jun Z, Juntao G, Shuli L, Li L. A comparative study on trans-umbilical single-port laparoscopic approach versus conventional repair for incarcerated inguinal hernia in children. J Minim Access Surg. 2016;12:139–42.
Yoshizawa J, Ashizuka S, Kuwashima N, et al. Laparoscopic percutaneous extraperitoneal closure for inguinal hernia: learning curve for attending surgeons and residents. Pediatr Surg Int. 2013;29:1281–5.
Bisgaard T, Kehlet H, Oehlenschlager J, Rosenberg J. Acceptable nationwide outcome after paediatric inguinal hernia repair. Hernia. 2014;18:325–31.
Ponsky TA, Nalugo M, Ostlie DJ. Pediatric laparoscopic inguinal hernia repair: a review of the current evidence. J Laparoendosc Adv Surg Tech A. 2014;24:183–7.
Alzahem A. Laparoscopic versus open inguinal herniotomy in infants and children: a meta-analysis. Pediatr Surg Int. 2011;27:605–12.
Yang C, Zhang H, Pu J, Mei H, Zheng L, Tong Q. Laparoscopic vs open herniorrhaphy in the management of pediatric inguinal hernia: a systemic review and meta-analysis. J Pediatr Surg. 2011;46:1824–34.
Feng S, Zhao L, Liao Z, Chen X. Open versus laparoscopic inguinal herniotomy in children: a systematic review and meta-analysis focusing on postoperative complications. Surg Laparosc Endosc Percutan Tech. 2015;25:275–80.
Steigman CK, Sotelo-Avila C, Weber TR. The incidence of spermatic cord structures in inguinal hernia sacs from male children. Am J Surg Pathol. 1999;23:880–5.
Yavetz H, Harash B, Yogev L, Homonnai ZT, Paz G. Fertility of men following inguinal hernia repair. Andrologia. 1991;23:443–6.
Kordzadeh A, Liu MO, Jayanthi NV. Male infertility following inguinal hernia repair: a systematic review and pooled analysis. Hernia. 2017;21:1–7.
Hassan ME, Mustafawi AR. Laparoscopic flip-flap technique versus conventional inguinal hernia repair in children. JSLS. 2007;11:90–3.
Leung WY, Poon M, Fan TW, et al. Testicular volume of boys after inguinal herniotomy: combined clinical and radiological follow-up. Pediatr Surg Int. 1999;15:40–1.
Çelebi S, Yıldız A, Üçgül A, et al. Do open repair and different laparoscopic techniques in pediatric inguinal hernia repairs affect the vascularization of testes? J Pediatr Surg. 2012;47:1706–10.
Parelkar SV, Oak S, Bachani MK, et al. Laparoscopic repair of pediatric inguinal hernia--is vascularity of the testis at risk? A study of 125 testes. J Pediatr Surg. 2011;46:1813–6.
Kristensen AD, Ahlburg P, Lauridsen MC, Jensen TS, Nikolajsen L. Chronic pain after inguinal hernia repair in children. Br J Anaesth. 2012;109:603–8.
Celebi S, Aksoy D, Cevik B, Yildiz A, Kurt S, Dokucu AI. An electrophysiologic evaluation of whether open and laparoscopic techniques used in pediatric inguinal hernia repairs affect the genitofemoral nerve. J Pediatr Surg. 2013;48:2160–3.
Barazanchi AW, Fagan PV, Smith BB, Hill AG. Routine neurectomy of inguinal nerves during open onlay mesh hernia repair: a meta-analysis of randomized trials. Ann Surg. 2016;264:64–72.
Chan KL, Hui WC, Tam PK. Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc. 2005;19:927–32.
Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP. A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics. 2009;123:332–7.
Celebi S, Uysal AI, Inal FY, Yildiz A. A single-blinded, randomized comparison of laparoscopic versus open bilateral hernia repair in boys. J Laparoendosc Adv Surg Tech A. 2014;24:117–21.
Esposito C, Peter SD, Escolino M, Juang D, Settimi A, Holcomb GW 3rd. Laparoscopic versus open inguinal hernia repair in pediatric patients: a systematic review. J Laparoendosc Adv Surg Tech A. 2014;24:811–8.
Miyake H, Fukumoto K, Yamoto M, et al. Risk factors for recurrence and contralateral inguinal hernia after laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia. J Pediatr Surg. 2017;52:317–21.
Xiang B, Jin S, Zhong L, Li F, Jiang X, Xu Z. Reasons for recurrence after the laparoscopic repair of indirect inguinal hernia in children. J Laparoendosc Adv Surg Tech A. 2015;25:681–3.
Sumida W, Watanabe Y, Takasu H, Oshima K, Komatsuzaki N. Incidence of contralateral patent processus vaginalis in relation to age at laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia. Surg Today. 2016;46:466–70.
Zhong H, Wang F. Contralateral metachronous hernia following negative laparoscopic evaluation for contralateral patent processus vaginalis: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2014;24:111–6.
Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg. 2007;94:804–11.
Zhao J, Chen Y, Lin J, et al. Potential value of routine contralateral patent processus vaginalis repair in children with unilateral inguinal hernia. Br J Surg. 2017;104:148–51.
Chang YT, Lin JY, Lee JY, Tsai CJ, Chiu WC, Chiu CS. Comparative mid-term results between inguinal herniotomy and single-port laparoscopic herniorrhaphy for pediatric inguinal hernia. Surg Laparosc Endosc Percutan Tech. 2012;22:526–31.
Tam YH, Wong YS, Pang KK, et al. Unexpected metachronous hernia development in children following laparoscopic unilateral hernia repair with negative evaluation for contralateral patent processus vaginalis. J Laparoendosc Adv Surg Tech A. 2013;23:287–90.
Watanabe T, Yoshida F, Ohno M, et al. Morphology-based investigation of metachronous inguinal hernia after negative laparoscopic evaluation - is it acquired indirect inguinal hernia? J Pediatr Surg. 2016;51:1548–51.
Muensterer OJ, Woller T, Metzger R, Till H. The economics of contralateral laparoscopic inguinal hernia exploration. Cost calculation of herniotomy in infants. Chirurg. 2008;79:1065–71.
Koivusalo A, Pakarinen MP, Rintala RJ. Laparoscopic herniorrhaphy after manual reduction of incarcerated inguinal hernia. Surg Endosc. 2007;21:2147–9.
Shalaby R, Ibrahem R, Shahin M, et al. Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg. 2012;2012:484135. doi:10.1155/2012/484135.
Shono T, Izaki T, Nakahori R, Yoshimaru K. Testicular ascent after laparoscopic percutaneous extraperitoneal closure for inguinal hernias. Eur J Pediatr Surg. 2015;25:105–8.
Wang F, Zhong H, Zhao J. Ascending testis after repair of pediatric inguinal hernia and hydrocele: a misunderstood operative complication. J Pediatr Urol. 2017;13:53.e1–5.
Pelizzo G, Bernardi L, Carlini V, et al. Laparoscopy in children and its impact on brain oxygenation during routine inguinal hernia repair. J Minim Access Surg. 2017;13:51–6.
Bertozzi M, Melissa B, Magrini E, Bini V, Appignani A. Laparoscopic herniorrhaphy in the pediatric age group: what about the learning curve? J Endourol. 2013;27:840–4.
Yoshimaru K, Kinoshita Y, Shono T. The safety and efficacy of laparoscopic percutaneous extraperitoneal closure for inguinal hernia in neonates and infants younger than 1-y of age in comparison to older patients. J Laparoendosc Adv Surg Tech A. 2017;27:91–6.
Chan IH, Lau CT, Chung PH, et al. Laparoscopic inguinal hernia repair in premature neonates: is it safe? Pediatr Surg Int. 2013;29:327–30.
Pastore V, Bartoli F. Neonatal laparoscopic inguinal hernia repair: a 3-year experience. Hernia. 2015;19:611–5.
Burgmeier C, Schier F. Cardiorespiratory complications after laparoscopic hernia repair in term and preterm babies. J Pediatr Surg. 2013;48:1972–6.
Ishii T, Yonekura T, Yamauchi K, et al. Laparoscopic repair of sliding inguinal hernia in female children. Pediatr Surg Int. 2016;32:895–9.
Oak SN, Parelkar SV, K R, et al. Large inguinal hernia in infants: is laparoscopic repair the answer? J Laparoendosc Adv Surg Tech A. 2007;17:114–8.
Nah SA, Giacomello L, Eaton S, et al. Surgical repair of incarcerated inguinal hernia in children: laparoscopic or open? Eur J Pediatr Surg. 2011;21:8–11.
Mishra PK, Burnand K, Minocha A, Mathur AB, Kulkarni MS, Tsang T. Incarcerated inguinal hernia management in children: 'a comparison of the open and laparoscopic approach'. Pediatr Surg Int. 2014;30:621–4.
Radmayr C, Corvin S, Studen M, Bartsch G, Janetschek G. Cryptorchidism, open processus vaginalis, and associated hernia: laparoscopic approach to the internal inguinal ring. Eur Urol. 1999;36:631–4.
Yildiz A, Celebi S, Akin M, et al. Laparoscopic hernioraphy: a better approach for recurrent hernia in boys? Pediatr Surg Int. 2012;28:449–53.
Shalaby R, Ismail M, Gouda S, et al. Laparoscopic management of recurrent inguinal hernia in childhood. J Pediatr Surg. 2015;50:1903–8.
Chan KL. Laparoscopic repair of recurrent childhood inguinal hernias after open herniotomy. Hernia. 2007;11:37–40.
Zani A, Eaton S, Hoellwarth M, et al. Management of pediatric inguinal hernias in the era of laparoscopy: results of an international survey. Eur J Pediatr Surg. 2014;24:9–13.
Author information
Authors and Affiliations
Contributions
VR conceived the topic and will act as guarantor for the paper. Both VR and PA took part in literature analysis, writing preliminary drafts, critical revision of manuscript and approval of final form.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Raveenthiran, V., Agarwal, P. Choice of Repairing Inguinal Hernia in Children: Open Versus Laparoscopy. Indian J Pediatr 84, 555–563 (2017). https://doi.org/10.1007/s12098-017-2354-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2354-9