Abstract
Purpose
To analyze the correlation between contrast-enhanced ultrasound image features and axillary lymph node metastasis of primary breast cancer and its diagnostic value.
Methods
In this study, 64 patients with axillary lymph node metastasis of primary breast cancer diagnosed and treated in our hospital from February 2011 to March 2013 were collected as an observation group, and 54 patients without axillary lymph node metastasis were collected as a control group. All patients underwent a contrast-enhanced ultrasound examination, and the correlation between the contrast-enhanced ultrasound image features and axillary lymph node metastasis and its diagnostic value were analyzed. They were divided into two groups according to their survival conditions: the group with good efficacy and group with poor efficacy, and the prognostic factors of breast cancer in the two groups were analyzed.
Results
There were statistical differences in the peripheral acoustic halo, blood flow classification, ratio of length to diameter (L/D), maximum cortical thickness, and enhancement mode of lymph nodes between the two groups (p < 0.05). The area under ROC curve for diagnosis of axillary lymph node metastasis by contrast-enhanced ultrasound was 0.854, sensitivity was 83.33%, and specificity was 87.5%; L/D and enhancement mode were independent prognostic factors for breast cancer.
Conclusions
Contrast-enhanced ultrasound image features have diagnostic and prognostic value for axillary lymph node metastasis of breast cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequently diagnosed malignant tumor in the world. It is the most common cause of cancer death for women in developing countries and the second leading cause of cancer death in developed countries [1]. The number of breast cancer cases accounts for 23% of the total number of malignant tumor cases in the world, and its mortality is as high as 14% [2]. Morbidity and mortality increased by 20% and 14% in 2012 compared with 2008 [3]. It has been reported that the high prevalence of breast cancer is the result of over-detection; but it is important that after correcting many more and more cases, the death toll from breast cancer continues to rise in the world [4]. Some studies have found that 5 years after endocrine therapy, the recurrence of breast cancer is still occurring steadily [5]. Although the treatment progress of breast cancer improves the prognosis of patients, the condition of axillary lymph nodes is still the most critical prognostic factor [6]. Therefore, determining the diagnosis method of axillary lymph node metastasis is of great significance to improve the prognosis of patients.
Clinically, radiotherapy, chemotherapy, and surgery are usually used to treat breast cancer, and axillary lymph node metastasis is an important factor affecting the treatment. Traditional axillary lymph node dissection has a large incision and many adverse complications, which cause the patients’ mobility disorder and affect their quality of life [7]. Sentinel lymph node biopsy has gradually replaced it [8]. The updated clinical practice guideline of the American Society of clinical oncology has also pointed out that women without sentinel lymph node metastasis should not receive axillary lymph node dissection [9]. However, some studies have reported that the false-negative rate of sentinel lymph node biopsy is in the range of 0–29%, with an average false-negative rate of 7.3% [10], and a few patients may have local disease recurrence [11]. Therefore, we need to seek a new diagnostic method for axillary lymph node metastasis. Research reports that contrast-enhanced ultrasound is relatively accurate, noninvasive, easy to operate, and more cost-effective, and is widely used in the examination of axillary lymph node metastasis of breast cancer [12]. Contrast-enhanced ultrasound can display more Doppler signals, show blood flow, and reveal tumor perfusion characteristics [13]. Therefore, studying the contrast-enhanced ultrasound image features can provide valuable reference basis for early diagnosis, treatment selection, and prognosis of breast cancer.
To sum up, this study will analyze the correlation between the contrast-enhanced ultrasound image features and axillary lymph node metastasis of breast cancer, as well as its diagnostic and prognostic value.
Materials and methods
Clinical data of patients
In this study, 64 patients with axillary lymph node metastasis of primary breast cancer diagnosed for the first time and treated in our hospital from February 2011 to March 2013 were collected as the observation group, and 54 patients without axillary lymph node metastasis of primary breast cancer were collected as the control group. All patients underwent a contrast-enhanced ultrasound examination before the operation. This study was approved by the Medical Ethics Committee, and all of them were informed and signed informed consent forms.
Inclusion and exclusion criteria
Inclusion criteria were as follows: all patients were diagnosed with axillary lymph node metastasis/non-metastasis of primary breast cancer for the first time by chest x-ray, chest and axilla FNAC; the diagnostic criteria referred to the 2015 EMSO diagnosis and treatment guidelines [14]; the patients’ clinical data were perfect, the tumor diameter was >5 cm, and they had not undergone radiotherapy, chemotherapy and other anti-tumor treatments; they were in the know and participated in the study voluntarily.
Exclusion criteria were as follows: distant metastasis of tumor, male patients, combined with other malignant tumors, severe liver, and kidney dysfunction, contrast agent allergy, mental dysfunction, cardiovascular diseases, pregnancy, lactation, or axillary surgery history.
Contrast-enhanced ultrasound examination method
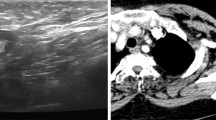
In this study, the color Doppler ultrasound diagnostic instrument (Royal Philips of the Netherlands, IU22) was used for ultrasound examination, IL9-3 broadband linear array probe (the frequency was 9 MHz), and pulse-inversion contrast harmonic imaging (PICHI) (the mechanical index was 0.07) were used. The patient shall lie on the back with his arms raised up to fully expose his armpits. After the location of the tumor was determined, its scope, blood flow, and morphology were observed. Then it was switched to the ultrasound contrast mode, and 2.4 ml of contrast agent Sono Vue (Italian Bracco Company) was injected immediately after 5 ml of normal saline was injected, and image information larger than 3 min was collected for analysis. The peripheral acoustic halo, blood flow classification, boundary, microcalcification, aspect ratio, and other contrast images of axillary lymph nodes were recorded for analysis, including contrast agent perfusion sequence, enhancement mode, and other conditions. If the image shows uniform enhancement, it is negative, and if it shows local and peripheral enhancement, it is positive.
Follow-up of patients
The follow-up start from the time when the surgery is finished in December 2018. The median follow-up time is 26 months (7.4–60 months). The survival of the patients was followed up for 5 years by telephone and outpatient reexamination from the time they underwent surgery. They were followed up at the 6th, 12th, 24th, 36th, 48th and 60th months after treatment.
Outcome measures
Main outcome measures: taking pathological examination results as gold standard, the correlation between contrast-enhanced ultrasound image features and axillary lymph node metastasis in the observation group and control group was compared, and the diagnostic value of contrast-enhanced ultrasound image features on axillary lymph node metastasis of breast cancer was analyzed by drawing ROC curve.
Secondary outcome measures: contrast-enhanced ultrasound image features of the observation group and control group were compared. Multivariate logistic regression was used to analyze the risk factors of axillary lymph node metastasis of breast cancer. Survival curves were drawn according to the patients’ 5-year survival conditions. They were divided into groups with good efficacy (patients who survived within the follow-up period) and groups with poor efficacy (who died during the follow-up period) according to the survival conditions. Multivariate logistic regression was used to analyze the prognostic factors of breast cancer patients.
Statistical analysis
This study used SPSS20.0 (SPSS Inc., Chicago, USA) medical statistical analysis software to carry out statistical analysis on the collected data, and used GraphPad Prism 7 (GraphPad Software Co., Ltd., SD, USA) to draw pictures of them. The counting data usage (%) was conducted by the Chi-square test and expressed by χ2. The measurement data were expressed by mean ± standard deviation (means ± SD), and all those were in accordance with the normal distribution. Independent-samples T test was used for comparison between the two groups. The ROC curve was used to evaluate the diagnostic value of contrast-enhanced ultrasound image features in patients with axillary lymph node metastasis of breast cancer. Multivariate logistic regression was used to analyze the risk factors of axillary lymph node metastasis and prognosis factors of breast cancer patients. A p value >0.05 was considered to be statistically significant.
Results
Comparison of clinical data of patients
According to the data in Table 1, there was no significant difference in age, BMI, history of smoking, history of alcoholism, family history, place of residence, menstrual status, type of surgery, tumor size, TNM stage [15] and pathological type between the two groups (p > 0.05), which was comparable.
Univariate analysis of contrast-enhanced ultrasound images of patients in the two groups
Contrast-enhanced ultrasound images of patients in the two groups were collected for univariate analysis. There was no difference in lymph node boundary, microcalcification and perfusion sequence between the two groups (p > 0.05), while there were statistical differences in peripheral acoustic halo, blood flow classification, L/D, maximum cortical thickness and enhancement mode of lymph nodes between the two groups (p < 0.05), as shown in Table 2.
Multivariate analysis of axillary lymph node metastasis in breast cancer
Indicators with differences in univariate analysis were included in the assignment (Table 3), and then back: LR was selected for multivariate logistic regression analysis. The results revealed that peripheral acoustic halo was not an independent risk factor for axillary lymph node metastasis, while blood flow classification (OR 5.494, 95% CI 1.102–27.388), L/D (OR 2.553, 95% CI 0.727–8.970), maximum cortical thickness (OR 1.395, 95% CI 0.372–5.228) and enhancement mode (OR 19.448, 95% CI 4.656–81.238) were independent risk factors for axillary lymph node metastasis, as shown in Table 4.
Diagnostic value of contrast-enhanced ultrasound image features in patients with axillary lymph node metastasis
Judging from the contrast-enhanced ultrasound diagnostic criteria, the results showed that 56 patients in the observation group were diagnosed with axillary lymph node metastasis and 8 patients did not metastasize, while 9 patients in the control group were diagnosed with axillary lymph node metastasis and 45 patients did not metastasize, as shown in Table 5. According to the detection of axillary lymph node metastasis by contrast-enhanced ultrasound of patients in the two groups, ROC curves were drawn to analyze the diagnostic value of contrast-enhanced ultrasound in patients with axillary lymph node metastasis. The results manifested that the area under ROC curves was 0.854, 95% CI was 0.780–0.929, sensitivity was 83.33%, specificity was 87.5%, Youden index was 70.83%, and cut-off value was >0.5, as shown in Fig. 1.
Comparison of survival conditions of patients between the two groups
Statistics on the 5-year survival of patients in the two groups displayed that 118 patients were followed up without any defect, and their overall survival rate was 83.05%. Comparing the survival conditions of patients in the two groups, we found that the overall survival rate of the control group (90.74%) was significantly higher than that of the observation group (76.56%), and the survival conditions between the two groups were significantly different (p = 0.043), as shown in Fig. 2.
Prognostic univariate analysis of breast cancer patients
According to the 5-year follow-up survival of the patients, they were divided into two groups: the group with good efficacy (survival patients) and group with poor efficacy (death patients). The contrast-enhanced ultrasound images of the two groups were collected for univariate analysis; there was no difference in the peripheral acoustic halo, boundary, microcalcification, and perfusion sequence of the lymph nodes between the two groups (p > 0.05). Nevertheless, there were statistical differences in lymph node blood flow classification, L/D, maximum cortical thickness, and enhancement mode between the two groups (p < 0.05), as shown in Table 6.
Multivariate analysis of prognosis of breast cancer patients
Indicators with differences in univariate analysis were included in the assignment (Table 7), and then back: LR was selected for multivariate logistic regression analysis. The results showed that blood flow grade and maximum cortical thickness were not independent prognostic factors for patients with axillary lymph node metastasis, while L/D (OR 1.865, 95% CI 0.746–8.325) and enhancement mode (OR 17.120, 95% CI 2.754–78.468) were prognostic risk factors for axillary lymph node metastasis, as shown in Table 8.
Discussion
The incidence and mortality of breast cancer are both on the rise. It is predicted that by 2050, 3.2 million new cases of breast cancer will occur in women worldwide every year [16]. Some studies have reported that the risk factors related to the increased risk of breast cancer are usually divided into internal factors and external factors, internal factors such as age and genetic susceptibility, and external factors such as lifestyle [17]. Compared with women who are not active, those who are active have a lower risk of breast cancer [18]. Breast cancer has become a potential safety hazard for women’s health all over the world. The prevention, diagnosis, and treatment of breast cancer have become an urgent social demand. The first stage of breast cancer metastasis is axillary lymph nodes. The status of axillary lymph nodes is an important factor in determining the stage, treatment, and prognosis of breast cancer patients [19]. In this study, the correlation between the image features and axillary lymph node metastasis, the diagnosis and prognosis value of patients were studied by contrast-enhanced ultrasound.
Firstly, the contrast-enhanced ultrasound images of the observation group and the control group were collected for univariate analysis. The results showed that there was no difference in lymph node boundary, microcalcification, and perfusion sequence between the two groups. However, there were significant differences in the peripheral acoustic halo, blood flow classification, L/D, maximum cortical thickness, and enhancement mode between the two groups. The results suggested that the peripheral acoustic halo, blood flow grade, L/D, maximum cortical thickness, and enhancement mode of lymph nodes were closely related to axillary lymph node metastasis. If there were peripheral acoustic halo, blood flow grade < grade II, L/D < 2 cm and uneven enhancement of axillary lymph nodes of patients, the tumor might have axillary lymph node metastasis, which indicated that contrast-enhanced ultrasound images had diagnostic value in distinguishing whether axillary lymph node metastasis existed. Zhang et al. [20] reported that contrast agents accompanied by blood flow, which helped prevent the occurrence of false images and enabled ultrasound contrast to have higher diagnostic accuracy. Therefore, it is of great significance to analyze the correlation between contrast-enhanced ultrasound and axillary lymph node metastasis by studying its image features. Choi et al. [21] verified that lymph nodes of patients with axillary lymph node metastasis signified enhancement, which was consistent with our research results. We speculate that cortical thickening may be the rapid proliferation and death of tumor cells, local cortical thickening of attachment, and connective tissue. We further carried out multivariate logistic regression analysis on metastasis-related indicators. The results showed that peripheral acoustic halo was not an independent risk factor for axillary lymph node metastasis, while blood flow classification, L/D, maximum cortical thickness, and enhancement mode were independent risk factors for axillary lymph node metastasis.
The results of the univariate analysis in this study showed the differences between the contrast-enhanced ultrasound images of patients in the two groups. Given the close association between ultrasound contrast images and axillary lymph node metastasis of breast cancer, we consider that ultrasound contrast may have a certain value in the diagnosis of axillary lymph node metastasis. Therefore, we drew the ROC curve according to the detection of axillary lymph node metastasis by contrast-enhanced ultrasound of patients in the two groups. The results revealed that the area under the ROC curve was 0.854, sensitivity was 83.33%, and specificity was 87.5%, suggesting that contrast-enhanced ultrasound could detect axillary lymph node metastasis and had diagnostic value. Previous studies [22–24] also reported that ultrasound contrast is a valuable technique in the diagnosis of breast cancer axillary lymph node metastasis, which is based on its non-invasive, non-radiative, and easy to operate, which confirms the results of our research. Then we carried out statistical analysis on the survival of patients in the two groups through a 5-year follow-up, and the results demonstrated that their overall survival rate in the observation group was significantly lower than that in the control group, indicating that axillary lymph node metastasis of breast cancer affected the prognosis of them, and the prognosis of those without lymph node metastasis was better, which was consistent with the research reports of Sharma [25] and others. Rojas et al. [26] reported that between 2005 and 2011, the 5-year relative survival rate of breast cancer patients was 89%, similar to our statistical result of 83.05%. Then we divided them into two groups according to their survival conditions: the group with good efficacy and group with poor efficacy, and collected the contrast-enhanced ultrasound images of the two groups to analyze the correlation of prognosis. Univariate results showed that there was no difference in the peripheral acoustic halo, boundary, microcalcification, and perfusion sequence of patients between the two groups. However, there were statistical differences in lymph node blood flow classification, L/D, maximum cortical thickness, and enhancement mode between both groups, which indicated that blood flow classification, L/D, maximum cortical thickness, and enhancement mode had a significant correlation with the prognosis of patients. When the axillary lymph node blood flow classification of patients was less than grade II, L/D was >2 cm and they had uneven enhancement, they might have a poor prognosis and could be used as a predictor of 5-year prognosis. Zhao et al. [27] also confirmed the value of contrast-enhanced ultrasound in the diagnosis and prognosis of breast cancer patients. In the end, we made a multivariate logistic regression analysis on the contrast-enhanced ultrasound images with differences of patients between the two groups. The results showed that blood flow classification and maximum cortical thickness were not independent prognostic factors for patients with axillary lymph node metastasis, while L/D and enhancement mode were independent prognostic factors for axillary lymph node metastasis. If L/D was >2 cm and there was the uneven enhancement of axillary lymph nodes in patients, axillary lymph nodes occurred, indicating poor prognosis of patients. Ki-67 is a prognostic indicator of early breast cancer. Its positive expression indicates that tumor cell proliferation is accelerated, and its high expression is related to lymph node metastasis [28]. c-erb-B2 is also positively expressed in breast cancer, and its positive expression is related to the characteristics of ultrasound images [29]. As to the qualitative and quantitative analysis of contrast-enhanced ultrasound images of breast cancer patients, Vraka et al. [30] confirmed that the contrast-enhanced ultrasound image features were strongly linked to the prognosis of cancer, which was basically consistent with our research.
Although great progress has been made in this study, quantitative analysis of the contrast-enhanced ultrasound image features is not carried out, and errors may occur in the judgment of the results. Studies display that there is still a high risk of recurrence 5 years after treatment [31]. Therefore, we hope to increase the number of samples for quantitative analysis of contrast-enhanced ultrasound images in future studies and extend the follow-up time to study the recurrence rate of breast cancer and its influencing factors.
Conclusion
In a word, contrast-enhanced ultrasound image features have diagnostic and prognostic value for axillary lymph node metastasis of breast cancer.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–403.
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, Naghavi M. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378:1461–84.
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, Peto R, Pritchard KI, Bergh J, Dowsett M, Hayes DF, EBCTCG. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836–46.
Berg WA, Bandos AI, Mendelson EB, Lehrer D, Jong RA, Pisano ED. Ultrasound as the primary screening test for breast cancer: analysis from ACRIN 6666. J Natl Cancer Inst. 2015; 108 [pii: djv367]
Gié O, Matthey-Gié ML, Marques-Vidal PM, Demartines N, Matter M. Impact of the ultrasonic scalpel on the amount of drained lymph after axillary or inguinal lymphadenectomy. BMC Surg. 2017;17:27.
Lyman GH, Giuliano AE, Somerfield MR, Benson AB 3rd, Bodurka DC, Burstein HJ, Cochran AJ, Cody HS 3rd, Edge SB, Galper S, Hayman JA, Kim TY, Perkins CL, Podoloff DA, Sivasubramaniam VH, Turner RR, Wahl R, Weaver DL, Wolff AC, Winer EP. American Society of clinical oncology: American society of clinical oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23:7703–20.
Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE. Sentinel lymph node biopsy for patients with early-stage breast cancer: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35:561–4.
Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a meta-analysis. Cancer. 2006;106:4–16.
Naik AM, Fey J, Gemignani M, Heerdt A, Montgomery L, Petrek J, Port E, Sacchini V, Sclafani L, VanZee K, Wagman R, Borgen PI, Cody HS 3rd. The risk of axillary relapse after sentinel lymph node biopsy for breast cancer is comparable with that of axillary lymph node dissection: a follow-up study of 4008 procedures. Ann Surg. 2004;240:462–71.
Matsuzawa F, Einama T, Abe H, Suzuki T, Hamaguchi J, Kaga T, Sato M, Oomura M, Takata Y, Fujibe A, Takeda C, Tamura E, Taketomi A, Kyuno K. Accurate diagnosis of axillary lymph node metastasis using contrast-enhanced ultrasonography with Sonazoid. Mol Clin Oncol. 2015;3:299–302.
Li K, Su ZZ, Xu EJ, Ju JX, Meng XC, Zheng RQ. Improvement of ablative margins by the intraoperative use of CEUS-CT/MR image fusion in hepatocellular carcinoma. BMC Cancer. 2016;16:277.
Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E, Zackrisson S, Cardoso F. ESMO guidelines committee: primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26:v8–v30.
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ. WHO classification of tumours. 4th ed. Lyon: IARC WHO classification of tumours IARC Press; 2012.
Tao Z, Shi A, Lu C, Song T, Zhang Z, Zhao J. Breast cancer: epidemiology and etiology. Cell Biochem Biophys. 2015;72:333–8.
Kamińska M, Ciszewski T, Łopacka-Szatan K, Miotła P, Starosławska E. Breast cancer risk factors. Menopause Rev. 2015;14:196–202.
Lynch BM, Neilson HK, Friedenreich CM. Physical activity and breast cancer prevention. Phys Activ Cancer. 2011;186:13–42.
Layeequr Rahman R, Crawford SL, Siwawa P. Management of axilla in breast cancer—the saga continues. Breast. 2015;24:343–53.
Zhang YX, Wang XM, Kang S, Li X, Geng J. Contrast-enhanced ultrasonography in qualitative diagnosis of sentinel lymph node metastasis in breast cancer: A meta-analysis. J Cancer Res Ther. 2015;11:697.
Choi HY, Park M, Seo M, Song E, Shin SY, Sohn YM. Preoperative axillary lymph node evaluation in breast cancer: current issues and literature review. Ultrasound Q. 2017;33:6–14.
Dellaportas D, et al. Contrast-enhanced color Doppler ultrasonography for preoperative evaluation of sentinel lymph node in breast cancer patients. Breast Care (Basel). 2015;10(5):331–5.
Cheng W, et al. Percutaneous contrast-enhanced ultrasonography to observe the sentinel lymph node metastasis of tumor-bearing rabbit breast cancer. Chin J Med Imag Technol. 2014;30(8):1161–4.
Liu J, et al. Percutaneous contrast-enhanced ultrasound for localization and diagnosis of sentinel lymph node in early breast cancer. Sci Rep. 2019;9(1):1–6.
Sharma N, Cox K. Axillary nodal staging with contrast-enhanced ultrasound. Curr Breast Cancer Rep. 2017;9:259–63.
Rojas K, Stuckey A. Breast cancer epidemiology and risk factors. Clin Obstet Gynecol. 2016;59:651–72.
Zhao YX, Liu S, Hu YB, Ge YY, Lv DM. Diagnostic and prognostic values of contrast-enhanced ultrasound in breast cancer: a retrospective study. Oncol Target Ther. 2017;10:1123.
de Azambuja E, Cardoso F, de CastroJr G, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer. 2007;96(10):1504–13.
Zhao XY, et al. Diagnostic and prognostic values of contrast-enhanced ultrasound in breast cancer: a retrospective study. Oncol Target Ther. 2017;10:1123.
Vraka I, Panourgias E, Sifakis E, Koureas A, Galanis P, Dellaportas D, Gouliamos A, Antoniou A. Correlation between contrast-enhanced ultrasound characteristics (qualitative and quantitative) and pathological prognostic factors in breast cancer. Vivo. 2018;32:945–54.
Colleoni M, Sun Z, Price KN, Karlsson P, Forbes JF, Thürlimann B, Gianni L, Castiglione M, Gelber RD, Coates AS, Goldhirsch A. Annual hazard rates of recurrence for breast cancer during 24 years of follow-up: results from the international breast cancer study group trials I to V. J Clin Oncol. 2019;34:927.
Author information
Authors and Affiliations
Contributions
HX and GLX are responsible for the conception or design of the work. HX, XDL, QHS and CZD contribute the acquisition, analysis, or interpretation of data for the work. HX and XDL provide the tissue samples. QHS helps in the follow-up of the patients. CZD helps in reviewing the histopathology slides. All authors finally approved the manuscript version to be published. CZD is the guarantor of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by Ethical Committee of The First Hospital of Jilin University and conducted in accordance with the ethical standards.
Informed consent
Yes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, H., Xu, G.L., Li, X.D. et al. Correlation between the contrast-enhanced ultrasound image features and axillary lymph node metastasis of primary breast cancer and its diagnostic value. Clin Transl Oncol 23, 155–163 (2021). https://doi.org/10.1007/s12094-020-02407-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02407-6