Abstract
The term nonalcoholic fatty liver disease (NAFLD) comprises a spectrum of increasingly harmful conditions ranging from nonalcoholic fatty liver (NAFL) to nonalcoholic steatohepatitis (NASH) to liver fibrosis and end-stage cirrhosis. NAFLD is the currently most common form of chronic liver disease in both adults and children worldwide. As NAFLD evolves as a global pandemic alongside the still growing prevalence of metabolic syndrome, obesity, and diabetes, it is inevitable to develop effective counterstrategies. Over the last decades, great effort has been dedicated to the understanding of the pathogenesis of NAFLD. This includes the development of an array of models for NAFLD, ranging from advanced in vitro (primary cells, 3D cultures, biochip, spheroids, organoids) to in vivo rodent models (particularly in mice). Based on these approaches novel therapies have been proposed and subsequently evaluated for patients with advanced forms of NAFLD, in particular those with NASH and liver fibrosis or cirrhosis. In this review, we delineate the current understanding of disease pathophysiology and depict how novel therapeutic strategies aim to exploit these different mechanisms to ameliorate, treat, or stop progression of NASH. We also discuss obstacles and chances along the way from basic models to promising clinical treatment options.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decade, the prevalence of obesity, type 2 diabetes, and the metabolic syndrome continued to rise dramatically. The hepatic consequences thereof lie within the development of a spectrum of diseases summarized as nonalcoholic fatty liver disease (NAFLD). NAFLD represents a continuum of conditions, which start as relatively benign—since completely reversible—hepatic steatosis. If left undiagnosed and subsequently unopposed it can transition into nonalcoholic steatohepatitis (NASH), characterized by hepatocellular injury, hepatocyte ballooning, inflammation, and varying degrees of fibrosis [1]. NASH may finally result in severe fibrosis and cirrhotic end-stage liver disease potentially developing hepatocellular carcinoma (HCC) [2, 3]. Meta-analytic data of 729 review articles including more than eight million biopsy-confirmed patients revealed a global NAFLD prevalence of 25.4% with the highest disease burden experienced in South America (30.45%) and the Middle East (31.79%) and the lowest in Africa (13.48%) [4]. Despite Hepatitis B remaining the number one cause of liver cirrhosis in the Asia–Pacific region, NAFLD numbers are on the rise in this region as well—mainly due to dietary changes and urbanization, adapting a western lifestyle [5]. Definitive diagnosis of NASH currently relies on a liver biopsy, displaying varying degrees of steatosis, hepatocellular ballooning, lobular inflammation, and—according to the stage of disease—presence or absence of fibrosis graded by scoring systems [6]. Among these specificities, fibrosis stage is the strongest predictor of disease specific mortality in NASH [7, 8]. Recent data on long-term outcomes and evaluation of the effects of clinical and histologic parameters on disease progression in patients with advanced NAFLD revealed that patients with NAFLD cirrhosis suffer from predominantly liver-related events, whereas those with bridging fibrosis develop mainly non-hepatic cancers and vascular events [9]. Reflecting the tremendous increase in humans affected by NAFLD, it is now the second leading cause of registration for a liver transplant, and even the leading cause for the latter in women in the United States [10]. Currently, there are only few specific pharmaceutical strategies available to treat NAFLD [11]. During the last decades, basic science leapt a huge step forward in deciphering pathophysiological processes underlying fibrosis and liver disease. To date, the most accepted concept explaining the pathogenesis of NAFLD encompasses multiple damaging ‘hits’ [12]. Characterized by the incidence of parallel or sequential events, these hits result from multifaceted interactions between factors in the macro- or micromilieu, genetics, and gut microbiome and involve both intrahepatic and extrahepatic pathways [13,14,15]. These interactions might promote isolated steatosis, innate immune activation, inflammation, cell death, or fibrosis with progressive liver damage [12]. Many of the promising results from rodent studies have fueled hopes to implement novel therapeutic approaches and targets in humans, too.
In this review, we outline the current understanding of pathomechanisms involved in NAFLD development, potential therapeutic targets in their wake, and highlight the status quo of drug development and NAFLD treatment. Particular emphasis lies on lessons learned from currently running and recently completed phase 3 clinical trials for promising compounds to avoid past pitfalls and enhance future NAFLD trials and therapy development.
Key findings from basic models with therapeutic implications
Due to the rising impact of steatosis-related liver disease worldwide, much effort has been put into uncovering pathomechanisms with the clear aim to find new therapeutic points of action in NAFLD. Current most promising targets include cell death and metabolic pathways, inflammatory mechanisms, the interplay between gut and liver, and directly inhibiting fibrogenic myofibroblast activation and extracellular matrix deposition (Table 1). Inherently, these approaches focused on pathomechanisms in the liver, while (largely) neglecting systemic consequences of the associated metabolic alterations (e.g. cardiovascular or renal diseases, extrahepatic malignancies), a major contributor of NAFLD-associated morbidity and mortality.
Cell death
In the past years, a correlation between the extent of liver cell death and the degree of fibrosis became evident, designating more advanced stages of NAFLD [16]. While the ability of the liver to eliminate dysfunctional cells is essential to prevent an excessive inflammatory milieu leading to further tissue destruction and carcinogenic transformation, processes of cell death themselves were shown to trigger fibrosis [17]. Extensive studies on cell death pathways uncovered a more diverse landscape off the beaten track of regulated cell death (apoptosis) and autolysis of damaged tissue (necrosis). Basic cellular and molecular biology research revealed the existence of regulated forms of necrosis, such as necroptosis, pyroptosis, ferroptosis, and autophagy-induced cell death—pathways which can be partially modulated by metabolic signals [18]. In the liver, different cell types contribute to a pro- or antifibrotic milieu. While inhibiting the death of hepatocytes seems to stop fibrosis, apoptosis of hepatic stellate cells (HSC) might be essential for the reversal of fibrosis, supporting the concept of cell-type specific therapeutic agents [17, 19]. A long known agent to dampen the effects of cell damage on the surrounding healthy tissue in the liver is α-tocopherol, vitamin E [20]. Its properties as an antioxidant are thought to alleviate oxidative stress during fulminant cell death and have been studied in a large randomized placebo controlled phase three trial against pioglitazone, the PIVENS study [21, 22]. Indeed, vitamin E proved superior to placebo in reducing hepatic steatosis and inflammation [21]. Nonetheless, concerns about long-term risks of vitamin E (e.g. hemorrhagic stroke, bladder cancer) prevented its broad long-term use in NAFLD [23].
A more specific treatment option is implied by inhibiting the common trunk of the extrinsic and intrinsic pathways of apoptosis, which is carried out by enzymes termed caspases. The pan-caspase inhibitor emricasan was successfully administered in a mouse model of NASH, leading to the reduction of inflammation and fibrosis against placebo [24]. A subsequent randomized controlled phase 2 trial administering emricasan vs. placebo in NASH patients showed significant reduction of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels in the serum of patients who received emricasan [24]. However, emricasan failed to improve fibrosis in a recent phase 2 clinical trial in NASH patients with fibrosis (ENCORE-NF, ClinicalTrials.gov identifier NCT02686762).
A third promising target in modulating cell death to ameliorate or halt NASH is inhibiting the apoptosis signal-regulating kinase (ASK) 1. ASK1 activates intracellular signaling cascades leading to apoptosis. Inhibition of ASK1 subsequently leads to reduced apoptosis rates and amelioration of hepatic steatosis in diabetic obese mice [25, 26]. After promising data from a phase 2 trial (ClinicalTrials.gov identifier NCT02466516) with a signal on fibrosis reduction, the ASK1 inhibitor selonsertib was recently investigated in two large phase 3 trials, subdivided by the severity of NASH (NASH-fibrosis, STELLAR 3, ClinicalTrials.gov identifier NCT03053050; and compensated NASH cirrhosis, STELLAR 4, ClinicalTrials.gov identifier NCT03053063) [27]. Both trials failed to reach the primary endpoint in the interim analysis after 48 weeks [28, 29].
Metabolism
As NAFLD is triggered by the excessive supply of nutrients, which dysbalances the metabolic situation, it seemed an apparent idea to target the aberrant hepatic fatty acid and glucose metabolism to prevent exuberant storage of fatty acids and generation of a profibrotic milieu. Key mechanisms in the altered metabolism in NAFLD include an excess of fatty acids, which leads to local oxidative bursts and endoplasmic reticulum stress, enormous triglyceride accumulation in hepatocytes, causing disturbances in the function of mitochondria and autophagy, and lipolysis triggered by insulin resistance [30]. In the past years, a panoply of potentially modifiable metabolic pathways was uncovered by the use of basic models. These include targets such as the family of peroxisome proliferator-activated receptors (PPARs), the nuclear receptor FXR (farnesoid X receptor), liver-derived metabolic signaling via the fibroblast growth factor (FGF) 21, inhibiting the key enzyme of fatty acid synthesis, acetyl-CoA carboxylase (ACC) and applying already accredited agonists of glucagon-like peptide (GLP) 1 [31,32,33,34,35,36].
6α-ethyl-chenodeoxycholic acid, better known as obeticholic acid (OCA), a synthetic variant of the natural bile acid chenode oxycholic acid, is FXR ligand, which showed the ability to reduce insulin resistance, protects against steatosis, and ameliorates liver fibrosis in rodents [37,38,39]. OCA is already approved as the second-line therapy for patients with primary biliary cholangitis and inadequate response to ursodeoxycholic acid [40]. It successfully completed a phase 2b trial in NASH patients, improving fibrosis in the OCA group vs. placebo (FLINT, ClinicalTrials.gov identifier NCT01265498) [41] and is currently investigated in a large phase 3 trial in NASH patients with either fibrosis (REGENERATE, ClinicalTrials.gov identifier NCT02548351) or with compensated cirrhosis due to NASH (REVERSE, ClinicalTrials.gov identifier NCT03439254) [42]. In this phase 3 trial, OCA resulted in significantly more patients achieving a ≥ 1 stage improvement in fibrosis by histological analysis after 72 weeks compared with placebo. Long-term results of this trial are still pending.
Various substances targeting different subtypes of PPARs are currently under preclinical and clinical investigation. Elafibranor (also known as GFT505), a dual PPARα/δ agonist, reduced steatosis, inflammation and fibrosis in a variety of murine models of NAFLD [43]. In the phase 2b GOLDEN-505 study (ClinicalTrials.gov identifier NCT01694849), elafibranor demonstrated the ability to induce resolution of NASH without worsening of fibrosis in a subgroup of patients [44]. Patients with biopsy-proven NASH are currently recruited in a phase 3 trial to further evaluate elafibranor in a larger cohort (RESOLVE-IT, ClinicalTrials.gov identifier NCT02704403). Other promising PPAR agonists are evaluated in randomized controlled phase 2 trials in NASH patients and include saroglitazar, a dual PPARα/γ agonist (EVIDENCES-IV, ClinicalTrials.gov identifier NCT03061721) and lanifibranor, a PPARα/γ/δ agonist (NATIVE, ClinicalTrials.gov identifier NCT03008070).
Pegbelfermin, a polyethylene glycol-conjugated (PEGylated) FGF21 analogue, is currently evaluated in randomized controlled phase 2b clinical trial with either patients with NASH fibrosis (FALCON1, ClinicalTrials.gov identifier NCT03486899) or NASH cirrhosis (FALCON2, ClinicalTrials.gov identifier NCT03486912) after successfully passing a 2a trial, wherein it significantly reduced liver fat content compared to placebo in NASH patients [45]. More compounds aiming to target the deranged metabolism in NAFLD include GLP1-analoga liraglutide and semaglutide [46,47,48,49]. Liraglutide was successfully evaluated in a randomized, placebo-controlled phase 2 study (LEAN, ClinicalTrials.gov identifier NCT01237119) by meeting the primary endpoint, which was defined as histological resolution of NASH [32]. Another promising target in NAFLD is Acetyl-CoA Carboxylase (ACC), an important enzyme in fatty acid metabolism and de novo lipogenesis in the liver. The ACC-inhibitor firsocostat (also known as GS-0976) was able to reduce hepatic steatosis, improve glucose-stimulated insulin secretion, and limit de novo lipogenesis in both rat models of NAFLD and humans in an open-label phase 2 study [50, 51]. This compound is currently under clinical evaluation as part of a combination therapy with selonsertib, semaglutide, and cilofexor in phase 2 studies.
Gut–liver axis
Conjointly working together in nutrient uptake, gut and liver are often referred to as an anatomical and functional unit—the ‘gut–liver axis’. Mixed among the nutrients reaching the liver via the portal vein are many signals, including hormones, growth factors and chemokines, from the intestinal tract. In return, the liver is able to secrete different soluble messengers, such as bile acids or IgA, via the bile into the intestine [52]. Several studies in animal models have illustrated the impact of the intestinal mucus layer, the presence of toll-like receptors (e.g. TLR4), and the composition of the intestinal microbiome on fibrotic responses in the liver [53,54,55]. Respecting the complexity of the gut microbiome and its regulation [56], it seems to need thought-out concepts on how to intervene in favor of resolving NAFLD, e.g. targeting fibroblast growth factors (FGF) promoting beneficial metabolic effects [30]. One of these might be NGM282, an engineered FGF19 analogue, demonstrating the ability to resolve steatohepatitis, liver fibrosis, and inflammation in mice [57, 58]. It has been evaluated in phase 2 randomized, placebo-controlled clinical trials, showing significant reduction of liver fat content vs. placebo and signals of histological improvement [59, 60].
Myofibroblast activation and extracellular protein deposition
Targeting liver fibrosis right at the origin of extracellular matrix production seems an elegant approach to halt or reverse fibrogenesis along the transition from steatosis to cirrhosis. Hepatic stellate cells (HSC) form the center of interest in this pathogenesis, since they represent the main source of collagen-producing myofibroblasts in liver fibrosis after being transdifferentiated from their resting phenotype [61]. HSC transdifferentiation, however, involves a number of complex intra- and extracellular signals provided by chemokines, macrophages, surrounding hepatocytes, cell metabolism, and has been extensively studied over the years [19, 62]. A key mechanism to achieve extracellular collagen accumulation involves the collagen-crosslinking enzyme lysyl oxidase-like (LOXL) 2. Simtuzumab is a monoclonal antibody binding to LOXL2, whereby it blocks fibrogenesis by crosslinking collagen fibers [63]. The results of inhibiting the LOXL2 with a monoclonal antibody in animal models of fibrotic and cancerous diseases bore legitimate excitement that this strategy might be effective in human fibrotic disease as well, inhibiting profibrotic pathways and even resulting in reversal of fibrosis in mice [64, 65]. However, clinical trials in humans aiming to treat idiopathic pulmonary fibrosis and liver fibrosis with simtuzumab failed to reproduce the strong effects observed in the rodent models [66, 67].
Inflammation
Hepatic inflammatory pathways are involved in all of the aforementioned pathomechanisms leading to liver fibrosis and cirrhosis. Upon cell damage, stressed hepatocytes, Kupffer cells, HSCs, and endothelial cells release chemokines guiding inflammatory cells, e.g. monocytes, dendritic cells, neutrophil granulocytes, and lymphocytes to the site of inflammation [68]. Monocyte subsets attracted by the C–C chemokine receptor type 2 (CCR2) seem to play a key role in setting up and maintaining the inflammatory environment [69,70,71]. CCR2 binds to its ligand, the C–C chemokine ligand type 2 (CCL2, also known as monocyte chemoattractant protein-1 or MCP-1). Several studies in experimental animal models have shown that steatohepatitis, liver fibrosis, and insulin resistance can be dampened by targeting and inhibiting either CCR2 or its ligand CCL2 [72,73,74,75].
Another immunologic target is the vascular adhesion protein (VAP) 1, which on the one hand regulates oxidative stress and inflammatory signaling, and on the other hand recruits lymphocytes to the site of inflammation [76]. By blocking VAP-1 liver fibrosis could be ameliorated in rodent models [76]. Furthermore, the molecule Galectin-3 was identified as an important player in liver fibrosis, since it is upregulated in inflammatory monocytes. Its inhibition proved significant reduction of fibrosis in experimental rat models [77].
Such anti-inflammatory targets are the aim of clinically investigated anti-NASH agents, the dual CCR2/CCR5 inhibitor cenicriviroc, the VAP-1 (AOC3) inhibitor BI-1467335 (formerly known as PXS-4728A) and the Galectin-3 inhibitor GR-MD-02 [75, 77, 78]. Cenicriviroc is currently evaluated in a large phase 3 clinical trial, the AURORA study (ClinicalTrials.gov identifier NCT03028740).
Common preclinical models in NAFLD research
The wide range of proposed ‘druggable’ disease mechanisms in NAFLD is a reflection of intense basic research. As a fundament, a plethora of in vitro and in vivo models have been developed to study various aspects of NASH. Larger animal models, such as the Ossabaw pig model of NASH, are logistically difficult in handling, expensive, and still unable to model a human NASH macro- and micromilieu [79]. Thus, in vivo modeling strategies almost exclusively rely on rodents. To realistically mimic human NAFLD, models for the evaluation of novel therapeutic compounds should display a phenotype as close to human disease as possible. Ideally, preclinical models in NAFLD should, therefore, develop obesity, insulin resistance, dyslipidemia, and the proinflammatory milieu of steatohepatitis when fed a specific high caloric diet, possibly in conjunction with hepatotoxins. Liver pathology should include macrovesicular steatosis, lobular inflammation, hepatocellular ballooning, and hepatic fibrosis, the histopathological hallmarks of NASH in humans. The development of a histopathological NAFLD score in rodents aimed to simplify the translatability into humans [80]. On the cellular and molecular level, the activation of key cellular pathways for fibrosis, de novo lipogenesis, the occurrence of oxidative stress, apoptosis, and the unfolded protein response should prove similar to the human one. Finally, transcriptomic and metabolomic analyses should confirm a similar molecular signature in human disease and in the model throughout different stages of NAFLD.
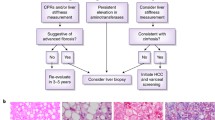
To date, none of the widespread used in vivo NASH models meets all these criteria constraining NAFLD researchers to focus on investigating certain aspects of the disease in the most suitable model for their specific hypothesis (Fig. 1). There is consensus that no single “perfect model” provides optimal insight into the efficacy of interventions across all mechanisms of action. Therefore, the joint workshop by the European and the American Association of the Study of the Liver (EASL & AASLD) recommended the rational use of models that best reflect the pathogenic aspect targeted by a new compound as the most appropriate approach [81].
Selection of appropriate in vivo models for non-alcoholic steatohepatitis (NASH). Selected mouse models of non-alcoholic fatty liver disease (NAFLD) are displayed that either reflect predominantly metabolic or fibrotic characteristics of NAFLD. Combined approaches have been developed to better mimic the phenotypic spectrum of human NAFLD in mice. ALIOS, American Lifestyle-Induced Obesity Syndrome; AMLN, Amylin liver NASH model; BDL, bile duct ligation; CCl4, carbon tetrachloride; CDAA-HFD, choline deficient L-amino acid-defined, high-fat diet; db/db, diabetic/diabetic, resulting in leptin receptor deficiency; DEN, diethylnitrosamine; DIAMOND mouse, diet-induced animal model of non-alcoholic fatty liver disease C57BL/6 J x 129S1/SvImJ (B6/129 mice) fed with WD + soluble glucose and fructose; FATZO, C57BL/6 J x AKR/J mice fed HFD and FD; FD, fructose diet; foz/foz, ‘fat Aussie’ mice, ALMS1 (Alström syndrome 1) deficiency; HFD, high fat diet; MCD, methionine and choline deficient diet; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; ob/ob, obese/obese, results in leptin deficiency; STAM, Stelic model NASH, STZ + HFD; STZ, streptozotocin; TAA, thioacetamide; WD, western diet
Mimicking the natural etiology of NAFLD resulting from overnutrition and a predominantly sedentary lifestyle, a good part of in vivo NASH models follows the concept of diet-induced obesity (DIO). Virtually any mouse strain can be fed a high-caloric, high fat (HF), high cholesterol (HC), high fructose (HF), or western diet (WD) to induce a steatotic phenotype. The phenotype, however, is strain dependent, e.g. C57Bl/6 mice are more susceptible to high fat diets than BALB/c mice [82]. Moreover, the composition of dietary lipids not only differentially affects the phenotype of NASH in mice, but also shapes the transcriptome of inflammatory cells such as Kupffer cells and infiltrating macrophages [83].
A main disadvantage of pure DIO models for the study of NASH pathogenesis is the low rate of fibrogenesis induced in these animals. To circumvent this, specific nutrient-deficient diets have been applied either alone or in combination with obesity-inducing diets, including the methionine and choline deficient diet (MCD) or a variant thereof, the choline deficient L-amino acid defined (CDAA) diet. Further models comprise chemically and mechanically induced liver damage, mono- and polygenetic models of NAFLD, and models combining multiple strategies to achieve more complete NASH pathology in accordance with the multiple hit hypothesis. Three recent reviews by Hansen et al., Santhekadur et al. and Febbraio et al. provide an in-depth overview of current preclinical modeling in NAFLD research [84,85,86]. Important and widely used NAFLD models are summarized in Table 2, alongside an overview of current and recent compounds in advanced clinical trials that had recently been evaluated in the respective model(s).
Alternatives to murine models include in vitro studies with cell cultures or human tissue samples (e.g. liver biopsies or liver slices). While 2D single cultures (on plastic dishes) are considered very artificial, 3D cultures of primary cells, biochip-based culture systems, hepatic spheroids and organoids allow a better assessment of cellular stress responses. Recently, advances were made in the ex vivo development of human tissue and in generating functional organoids from induced pluripotent stem cells (iPSC). For instance, an artificial liver system on a chip could be generated using either freshly isolated primary mouse hepatocytes, stellate cells, sinusoidal endothelium, and Kupffer cells or respective cell-lines [87, 88]. Furthermore, disease modeling could be implemented in human-derived ex vivo models, as shown in an organoid steatohepatitis model created from human stem cells [89]. The hope with these approaches lies within the creation of conditions closer to human (patho-)physiology and in gaining independence from animal-based modeling. Nonetheless, some aspects of the pathophysiology of NAFLD (e.g. recruitment of and interaction with inflammatory cells from the circulation, impact of gut-derived or microbial signals, impact of NAFLD on extrahepatic organs) will be inherently difficult to model in an ex vivo system.
Pitfalls in clinical studies
In response to the encouraging results from studies in numerous preclinical NAFLD models and, of course, driven by commercial interests, a range of clinical trials in humans was initiated. Table 3 summarizes important recently conducted and now running phase 3 studies in patients with NAFLD. To maintain inter-study comparability and address challenges in the field of drug development for NAFLD, the Center for Drug Evaluation and Research (CDER) of the Food and Drug Administration (FDA) in the United States Department of Health and Sciences published a draft guidance for the industry [90]. A similar reflection paper has been released by the European Medicines Agency (EMA) [91]. These documents provide a voluntarily applicable framework with recommendations on the specifications of patient cohorts including enrollment criteria, trial design, efficacy endpoints, and safety considerations. Currently, there are seven ongoing phase 3 trials in NASH, six of them testing recently developed, NASH-specific compounds (refer to Table 3). The scientific associations for hepatology in Europe and the US, EASL and AASLD, have provided evidence-based recommendations on clinical trial endpoints in NASH as well [81].
Selonsertib—ASK1 inhibition
Before entering the clinical trial phase, the ASK1 inhibitor GS-4997 (selonsertib) was successfully tested in a DIO rodent model of NASH, namely that C57Bl/6 mice were fed a diet high in fructose, cholesterol, and fat content [92]. The resulting NASH phenotype including steatohepatitis, fibrosis and an altered hepatic lipid and bile acid metabolism was successfully ameliorated by selonsertib [92]. Subsequently, selonsertib was investigated in 72 NASH patients with grade 2–3 fibrosis in a randomized, multicenter, open-label phase 2 trial [93]. It was initially designed to assign patients randomly 2:2:1:1:1 into groups treated with either 6 mg or 18 mg selonsertib, a combination of either 6 mg or 18 mg selonsertib and 125 mg of the LOXL2 inhibitor simtuzumab or simtuzumab alone. After simtuzumab was proven inefficient in another clinical trial, treatment groups of simtuzumab and selonsertib were pooled. Treatment outcome was verified by liver biopsy, magnetic resonance elastography of the liver and noninvasive markers of liver injury after 24 weeks of treatment. Patients treated with selonsertib showed an improvement in fibrosis associated with a decreased liver collagen content and reduced inflammation upon biopsy; findings which were mirrored in the magnetic elastography after treatment with selonsertib that showed reduction of liver stiffness [93]. However, the patient cohort in this study was small, the interval between baseline and end-of-treatment biopsy was short (24 weeks), and differences did not reach statistical significance. Nonetheless, the positive signals from this ‘pilot trial’ led to the initiation of two large phase 3 trials in either NASH patients with bridging fibrosis (STELLAR-3) or cirrhotic NASH patients (STELLAR-4). In February and April 2019, respectively, Gilead confirmed termination of first the STELLAR-4 and 2 months later the STELLAR-3 trial after selonsertib failed to reach the interim analysis endpoint of improving fibrosis by at least one stage without the worsening of NASH in the respective cohorts [28, 29]. However, selonsertib is still part of a phase 2b trial investigating a triple combination therapy with the ACC inhibitor firsocostat and the FXR agonist cilofexor in NASH patients with fibrosis and compensated cirrhosis (ATLAS trial, ClinicalTrials.gov identifier NCT03449446).
Obeticholic acid—FXR agonism
The synthetic bile acid obeticholic acid (OCA) was shown to reduce pathogenic features in various rodent models of NASH. It first proved halting of hepatic steatosis alongside amelioration of insulin resistance and altered lipid metabolism in leptin receptor mutated Zucker fa/fa rats [38]. Four years later, a different laboratory showed OCA to significantly reduce portal hypertension in two different cirrhotic rat models [39].
Encouraged by these positive effects, OCA entered the clinical trial phase and is now evaluated in phase 3 trials in patients with NASH fibrosis (REGENERATE) and those with compensated NASH cirrhosis (REVERSE). In the randomized, multicenter, double-blind, placebo-controlled, parallel group phase 2 FLINT study, 283 patients with non-cirrhotic, liver biopsy proven NASH were enrolled and received either OCA or placebo during a 72 weeks timespan [41]. The overall results of the FLINT study were highly positive as all components of the NAFLD activity score (hepatocellular ballooning, lobular inflammation, and steatosis) as well as fibrosis improved in the OCA group vs. placebo [41]. However, adverse effects in the OCA groups included 23% of patients complaining of pruritus. In addition, an increase in serum cholesterol levels was seen in OCA-treated patients as compared to those receiving placebo, which can be managed by adding a statin or dose-adjusting an existing statin therapy. The clinical relevance of the LDL increase on OCA regarding cardiovascular events or cardiovascular mortality is currently unclear. A possible explanation for increased serum cholesterol levels lies within the mechanism of action of the FXR receptor. Activation of this receptor leads to a blockade in the conversion of cholesterol to bile acids and might thus lead to cholesterol accumulation [41]. These findings will need further assessment during the above mentioned phase 3 trials. Both REGENERATE and REVERSE studies are currently ongoing. In patients with non-cirrhotic NASH (REGENERATE), significantly more patients on OCA displayed fibrosis improvement by ≥ 1 stage without worsening of NASH compared to placebo after 72 weeks of treatment, while the alternative primary endpoint (NASH resolution without worsening of fibrosis) was not met. Pruritus was reported in up to 51% of patients exposed to the highest dose of OCA (25 mg daily), and LDL increase occurred in 17% of OCA-exposed patients (7% in placebo). OCA is already approved as a second-line treatment option for primary biliary cholangitis in the US as well as in Europe [94].
Cenicriviroc—CCR2/CCR5 antagonism
The efficacy of inhibiting macrophage infiltration and HSC activation as mediated by the dual CCR2/CCR5 antagonist cenicriviroc in NASH was investigated and proven extensively in a large number of different rodent models in different independent laboratories. These models include chemically induced liver injury by thioacetamide (TAA), acetaminophen, and carbon tetrachloride (CCl4), combined chemically and dietary induced NASH via streptozotocin (STZ) and HFD, cholestatic fibrosis after bile duct ligation, and dietary models fed with WD or MCD (see Table 2 for details) [73, 75, 95,96,97,98]. Cenicriviroc successfully reduced monocyte recruitment to the inflammation site, effectively reduced liver fibrosis, and was able to significantly reduce the NAFLD activity score in the investigated NASH models [75]. Cenicriviroc has recently been evaluated in a randomized, double-blind, placebo-controlled, multinational phase 2b study in 289 patients with noncirrhotic NASH and fibrosis stages 1–3, the CENTAUR trial [99]. After 1 year into the study, cenicriviroc demonstrated a significant reduction of fibrosis stage against placebo without the worsening of steatohepatitis by histology. An analysis after 2 years into the study confirmed reduction of fibrosis stage in the cenicriviroc group vs. placebo in patients treated for 1 year, but no additional benefit for a longer treatment period for this endpoint [100]. A phase 3 trial, the AURORA study with planned enrollment of 2000 fibrotic NASH patients is currently running and awaits first results in 2021.
Elafibranor—PPAR agonism
The dual PPARα/δ agonist elafibranor showed positive effects on liver inflammation, steatosis, and serum liver enzymes in three different rodent models of NASH: WD-fed human apolipoprotein E2 transgenic mice, MCDD-fed db/db mice, and CCl4-induced fibrosis [43]. Consequently, elafibranor was assessed in a phase 2b multicenter, randomized placebo-controlled trial, the GOLDEN-505 study [44]. In the initial intention-to-treat cohort, the predefined primary endpoint was not met, however, after modification a post hoc analysis confirmed NASH resolution without fibrosis worsening in the elafibranor group for patients with ‘active’ disease (defined by a histological activity score) [44]. A clinical phase 3 trial in 2000 NASH patients is currently running (RESOLVE-IT), and initial results are being expected in 2020.
Discrepancy between preclinical models and clinical reality: potential reasons
Several of the recently conducted phase 2 and 3 trials in NASH failed to reproduce the promising antifibrotic or NASH-resolving effects clearly observed in rodent models. Reasons for these differences are likely manifold. First, no model can ever test compounds in the original physiological environment of heterogeneous human patient populations. In fact, experiments in mice usually try to reduce variability (heterogeneity) by controlling for potential confounders (e.g., same genetic background, oftentimes only male mice, same microbiota by cohousing, same calorie/food intake). This aspect may become even more relevant if mechanisms are not fully translatable between two different species. It is likely that mechanisms of disease are divergent in mice and men, just as differences in the steatogenesis of different diets affect various mouse strains to a varying degree [82]. Following this argumentation, there might be differences in drug biodistribution, target engagement or efficacy in mice and humans that influence susceptibility to treatment with certain drugs. Furthermore, none of the available NASH models used for preclinical trials satisfactorily represents all the human disease characteristics from the macroscopic to the molecular level. This irrevocably leads to an insufficient disease modeling and potentially biased translatability of drug effects seen in these models into the human system. Moreover, only few NAFLD models reflect associated extrahepatic diseases (such as atherosclerosis, obesity or insulin resistance; see Table 2). In addition, a higher heterogeneity in men concerning genetics, the gut microbiota, sex, and present comorbidities leads to further complications. It is, therefore, of the highest interest to generate preclinical models that model human physiology the closet possible to ameliorate the outcome of clinical trials in NAFLD drug development.
Clinical development of new drugs for NAFLD: What can we learn from basic models?
Well-conducted animal studies can provide important information on efficacy, safety and the mechanism of action of a certain compound for clinical development. Solid preclinical data are required before moving into human studies. To effectively test novel drug candidates, it is essential to know (and understand) the preclinical tools and choose wisely among the (partially insufficiently characterized) models available. In some cases, it appears reasonable to have the targeted pathway rather than all aspects of NAFLD pathology represented in a mouse model [81]. The above discussed compounds selonsertib, OCA, elafibranor, and cenicriviroc were all preclinically evaluated in at least two different murine NASH models. This robustness of findings in at least two different model systems is needed, and might be improved by reproducing the results in independent laboratories before entering the clinical trial phase. Following this approach, the effect of different microbiota, strains, and handling can be addressed, further supporting the translational relevance of findings from animal models before proceeding into clinical trials.
Conclusion and perspectives
Preclinical models of NAFLD have contributed enormously to unravel the complexity of NAFLD pathophysiology. Furthermore, they have led to the development, implementation, and clinical investigation of promising treatment strategies in NASH and NAFLD. To benefit from this valuable resource and subsequently be able to utilize it, it is of crucial importance to know about the advantages and drawbacks of preclinical models. Several clinical trials, as discussed above, have unfortunately taught us that what works in mice does not necessarily work for humans. Improving NAFLD diagnostics—potentially rendered non-invasive and enhanced by the help of deep learning methods [101], choosing the right model, and conducting clear cut clinical trials may pave the way towards successful drug development to treat NASH. Eventually, in the light of the dramatically increasing prevalence of NAFLD, it is important to remember the roots of and the risk factors leading to NASH, as establishment of a healthy lifestyle as well as effective treatment and the prevention of metabolic disorders such as type 2 diabetes, dyslipidemia, and obesity withdraw the fertile ground for NAFLD to flourish. However, as 95% of 7013 patients in a US NAFLD cohort were unaware of suffering from a liver disease, it is also imminent to increase the awareness of NAFLD and implement patient education programs [102].
References
Brunt EM, Neuschwander-Tetri BA, Oliver D, Wehmeier KR, Bacon BR. Nonalcoholic steatohepatitis: histologic features and clinical correlations with 30 blinded biopsy specimens. Hum Pathol. 2004;35(9):1070–82 (Epub 2004/09/).
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113–21 (Epub 2005/07/14).
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413–9 (Epub 1999/05/29).
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore, Md). 2016;64(1):73–84. https://doi.org/10.1002/hep.28431(Epub 2015/12/29).
Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia–Pacific region. Nat Rev Gastroenterol Hepatol. 2019;16(1):57–73. https://doi.org/10.1038/s41575-018-0055-0(Epub 2018/08/31).
Bedossa P. Pathology of non-alcoholic fatty liver disease. Liver Int. 2017;37(Suppl 1):85–9. https://doi.org/10.1111/liv.13301(Epub 2017/01/05).
Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology (Baltimore, Md). 2015;61(5):1547–54. https://doi.org/10.1002/hep.27368(Epub 2014/08/16).
Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology (Baltimore, Md). 2017;65(5):1557–65. https://doi.org/10.1002/hep.29085(Epub 2017/01/29).
Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443-57 e17. https://doi.org/10.1053/j.gastro.2018.04.034.
Noureddin M, Vipani A, Bresee C, Todo T, Kim IK, Alkhouri N, et al. NASH leading cause of liver transplant in women: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol. 2018;113(11):1649–59. https://doi.org/10.1038/s41395-018-0088-6(Epub 2018/06/09).
EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64(6):1388–402. doi: 10.1016/j.jhep.2015.11.004.
Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology (Baltimore, Md). 2010;52(5):1836–46. https://doi.org/10.1002/hep.24001(Epub 2010/11/03).
Bechmann LP, Hannivoort RA, Gerken G, Hotamisligil GS, Trauner M, Canbay A. The interaction of hepatic lipid and glucose metabolism in liver diseases. J Hepatol. 2012;56(4):952–64. https://doi.org/10.1016/j.jhep.2011.08.025(Epub 2011/12/17).
Wree A, Kahraman A, Gerken G, Canbay A. Obesity affects the liver - the link between adipocytes and hepatocytes. Digestion. 2011;83(1–2):124–33. https://doi.org/10.1159/000318741(Epub 2010/11/03).
Tacke F, Weiskirchen R. An update on the recent advances in antifibrotic therapy. Expert Rev Gastroenterol Hepatol. 2018;12(11):1143–52. https://doi.org/10.1080/17474124.2018.1530110(Epub 2018/09/29).
Eguchi A, Wree A, Feldstein AE. Biomarkers of liver cell death. J Hepatol. 2014;60(5):1063–74. https://doi.org/10.1016/j.jhep.2013.12.026(Epub 2014/01/15).
Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147(4):765-83.e4. https://doi.org/10.1053/j.gastro.2014.07.018(Epub 2014/07/22).
Schwabe RF, Luedde T. Apoptosis and necroptosis in the liver: a matter of life and death. Nat Rev Gastroenterol Hepatol. 2018;15(12):738–52. https://doi.org/10.1038/s41575-018-0065-y(Epub 2018/09/27).
Tsuchida T, Friedman SL. Mechanisms of hepatic stellate cell activation. Nat Rev Gastroenterol Hepatol. 2017;14(7):397–411. https://doi.org/10.1038/nrgastro.2017.38(Epub 2017/05/11).
Nagashimada M, Ota T. Role of vitamin E in nonalcoholic fatty liver disease. IUBMB Life. 2019;71(4):516–22. https://doi.org/10.1002/iub.1991(Epub 2018/12/29).
Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362(18):1675–85. https://doi.org/10.1056/NEJMoa0907929(Epub 2010/04/30).
Chalasani NP, Sanyal AJ, Kowdley KV, Robuck PR, Hoofnagle J, Kleiner DE, et al. Pioglitazone versus vitamin E versus placebo for the treatment of non-diabetic patients with non-alcoholic steatohepatitis: PIVENS trial design. Contemp Clin Trials. 2009;30(1):88–96. https://doi.org/10.1016/j.cct.2008.09.003(Epub 2008/09/23).
Roeb E, Steffen HM, Bantel H, Baumann U, Canbay A, Demir M, et al. S2k Guideline non-alcoholic fatty liver disease. Z Gastroenterol. 2015;53(7):668–723. https://doi.org/10.1055/s-0035-1553193(Epub 2015/07/15).
Barreyro FJ, Holod S, Finocchietto PV, Camino AM, Aquino JB, Avagnina A, et al. The pan-caspase inhibitor Emricasan (IDN-6556) decreases liver injury and fibrosis in a murine model of non-alcoholic steatohepatitis. Liver Int. 2015;35(3):953–66. https://doi.org/10.1111/liv.12570(Epub 2014/04/23).
Ichijo H, Nishida E, Irie K, ten Dijke P, Saitoh M, Moriguchi T, et al. Induction of apoptosis by ASK1, a mammalian MAPKKK that activates SAPK/JNK and p38 signaling pathways. Science (New York, NY). 1997;275(5296):90–4. https://doi.org/10.1126/science.275.5296.90(Epub 1997/01/03).
Yamamoto E, Dong YF, Kataoka K, Yamashita T, Tokutomi Y, Matsuba S, et al. Olmesartan prevents cardiovascular injury and hepatic steatosis in obesity and diabetes, accompanied by apoptosis signal regulating kinase-1 inhibition. Hypertension (Dallas, Tex : 1979). 2008;52(3):573–80. https://doi.org/10.1161/hypertensionaha.108.112292.
Anstee QM, Lawitz EJ, Alkhouri N, Wong VW, Romero-Gomez M, Okanoue T, et al. Noninvasive tests accurately identify advanced fibrosis due to NASH: baseline data from the STELLAR trials. Hepatology (Baltimore, Md). 2019. https://doi.org/10.1002/hep.30842.
Gilead Sciences I. Gilead Announces Topline Data From Phase 3 STELLAR-3 Study of Selonsertib in Bridging Fibrosis (F3) Due to Nonalcoholic Steatohepatitis (NASH) [Press release]. Gilead Sciences, Inc.; 2019 [updated 25.04.2019; cited 2019 17.07.2019]. https://www.gilead.com/news-and-press/press-room/press-releases/2019/4/gilead-announces-topline-data-from-phase-3-stellar3-study-of-selonsertib-in-bridging-fibrosis-f3-due-to-nonalcoholic-steatohepatitis-nash.
Gilead Sciences I. Gilead Announces Topline Data From Phase 3 STELLAR-4 Study of Selonsertib in Compensated Cirrhosis (F4) Due to Nonalcoholic Steatohepatitis (NASH) [Press release]. Gilead Sciences, Inc.; 2019 [updated 11.02.2019; cited 2019 17.07.2019]. https://www.gilead.com/news-and-press/press-room/press-releases/2019/2/gilead-announces-topline-data-from-phase-3-stellar4-study-of-selonsertib-in-compensated-cirrhosis-f4-due-to-nonalcoholic-steatohepatitis-nash.
Arab JP, Arrese M, Trauner M. Recent insights into the pathogenesis of nonalcoholic fatty liver disease. Annu Rev Pathol. 2018;13:321–50. https://doi.org/10.1146/annurev-pathol-020117-043617(Epub 2018/02/).
Fisher FM, Chui PC, Nasser IA, Popov Y, Cunniff JC, Lundasen T, et al. Fibroblast growth factor 21 limits lipotoxicity by promoting hepatic fatty acid activation in mice on methionine and choline-deficient diets. Gastroenterology. 2014;147(5):1073-83.e6. https://doi.org/10.1053/j.gastro.2014.07.044(Epub 2014/08/02).
Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679–90. https://doi.org/10.1016/s0140-6736(15)00803-x(Epub 2015/11/27).
Gross B, Pawlak M, Lefebvre P, Staels B. PPARs in obesity-induced T2DM, dyslipidaemia and NAFLD. Nat Rev Endocrinol. 2017;13(1):36–49. https://doi.org/10.1038/nrendo.2016.135(Epub 2016/11/04).
Fuchs CD, Traussnigg SA, Trauner M. Nuclear receptor modulation for the treatment of nonalcoholic fatty liver disease. Semin Liver Dis. 2016;36(1):69–86. https://doi.org/10.1055/s-0036-1571296(Epub 2016/02/13).
Jain MR, Giri SR, Bhoi B, Trivedi C, Rath A, Rathod R, et al. Dual PPARalpha/gamma agonist saroglitazar improves liver histopathology and biochemistry in experimental NASH models. Liver Int. 2018;38(6):1084–94. https://doi.org/10.1111/liv.13634(Epub 2017/11/23).
Abu-Elheiga L, Jayakumar A, Baldini A, Chirala SS, Wakil SJ. Human acetyl-CoA carboxylase: characterization, molecular cloning, and evidence for two isoforms. Proc Natl Acad Sci. 1995;92(9):4011–5. https://doi.org/10.1073/pnas.92.9.4011.
Fickert P, Fuchsbichler A, Moustafa T, Wagner M, Zollner G, Halilbasic E, et al. Farnesoid X receptor critically determines the fibrotic response in mice but is expressed to a low extent in human hepatic stellate cells and periductal myofibroblasts. Am J Pathol. 2009;175(6):2392–405. https://doi.org/10.2353/ajpath.2009.090114(Epub 2009/11/17).
Cipriani S, Mencarelli A, Palladino G, Fiorucci S. FXR activation reverses insulin resistance and lipid abnormalities and protects against liver steatosis in Zucker (fa/fa) obese rats. J Lipid Res. 2010;51(4):771–84. https://doi.org/10.1194/jlr.M001602(Epub 2009/09/29).
Verbeke L, Farre R, Trebicka J, Komuta M, Roskams T, Klein S, et al. Obeticholic acid, a farnesoid X receptor agonist, improves portal hypertension by two distinct pathways in cirrhotic rats. Hepatology (Baltimore, Md). 2014;59(6):2286–98. https://doi.org/10.1002/hep.26939(Epub 2013/11/22).
Practice guideline autoimmune liver diseases—AWMF-Reg. No. 021-27. Z Gastroenterol. 2017;55(11):1135–226. doi: 10.1055/s-0043-120199.
Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, Abdelmalek MF, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;385(9972):956–65. https://doi.org/10.1016/s0140-6736(14)61933-4(Epub 2014/12/04).
Ratziu V, Sanyal AJ, Loomba R, Rinella M, Harrison S, Anstee QM, et al. Regenerate: design of a pivotal, randomised, phase 3 study evaluating the safety and efficacy of obeticholic acid in patients with fibrosis due to nonalcoholic steatohepatitis. Contemp Clin Trials. 2019. https://doi.org/10.1016/j.cct.2019.06.017(Epub 2019/07/02).
Staels B, Rubenstrunk A, Noel B, Rigou G, Delataille P, Millatt LJ, et al. Hepatoprotective effects of the dual peroxisome proliferator-activated receptor alpha/delta agonist, GFT505, in rodent models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Hepatology (Baltimore, Md). 2013;58(6):1941–52. https://doi.org/10.1002/hep.26461(Epub 2013/05/25).
Ratziu V, Harrison SA, Francque S, Bedossa P, Lehert P, Serfaty L, et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor-alpha and -delta, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150(5):1147-59.e5. https://doi.org/10.1053/j.gastro.2016.01.038(Epub 2016/02/14).
Sanyal A, Charles ED, Neuschwander-Tetri BA, Loomba R, Harrison SA, Abdelmalek MF, et al. Pegbelfermin (BMS-986036), a PEGylated fibroblast growth factor 21 analogue, in patients with non-alcoholic steatohepatitis: a randomised, double-blind, placebo-controlled, phase 2a trial. Lancet. 2019;392(10165):2705–17. https://doi.org/10.1016/s0140-6736(18)31785-9(Epub 2018/12/18).
Knudsen LB, Lau J. The discovery and development of liraglutide and semaglutide. Front Endocrinol (Lausanne). 2019;10:155. https://doi.org/10.3389/fendo.2019.00155(Epub 2019/04/30).
Rakipovski G, Rolin B, Nohr J, Klewe I, Frederiksen KS, Augustin R, et al. The GLP-1 analogs liraglutide and semaglutide reduce atherosclerosis in ApoE(−/−) and LDLr(−/−) mice by a mechanism that includes inflammatory pathways. JACC Basic Transl Sci. 2018;3(6):844–57. https://doi.org/10.1016/j.jacbts.2018.09.004(Epub 2019/01/10).
Iogna Prat L, Tsochatzis EA. The effect of antidiabetic medications on non-alcoholic fatty liver disease (NAFLD). Hormones (Athens). 2018;17(2):219–29. https://doi.org/10.1007/s42000-018-0021-9(Epub 2018/06/03).
Petit JM, Cercueil JP, Loffroy R, Denimal D, Bouillet B, Fourmont C, et al. Effect of liraglutide therapy on liver fat content in patients with inadequately controlled type 2 diabetes: the lira-NAFLD study. J Clin Endocrinol Metab. 2017;102(2):407–15. https://doi.org/10.1210/jc.2016-2775(Epub 2016/10/13).
Loomba R, Kayali Z, Noureddin M, Ruane P, Lawitz EJ, Bennett M, et al. GS-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;155(5):1463-73.e6. https://doi.org/10.1053/j.gastro.2018.07.027(Epub 2018/07/31).
Lawitz EJ, Coste A, Poordad F, Alkhouri N, Loo N, McColgan BJ, et al. Acetyl-CoA carboxylase inhibitor GS-0976 for 12 weeks reduces hepatic de novo lipogenesis and steatosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2018;16(12):1983-91.e3. https://doi.org/10.1016/j.cgh.2018.04.042(Epub 2018/05/01).
Delacroix DL, Hodgson HJ, McPherson A, Dive C, Vaerman JP. Selective transport of polymeric immunoglobulin A in bile. Quantitative relationships of monomeric and polymeric immunoglobulin A, immunoglobulin M, and other proteins in serum, bile, and saliva. J Clin Investig. 1982;70(2):230–41. https://doi.org/10.1172/JCI110610.
Seki E, De Minicis S, Osterreicher CH, Kluwe J, Osawa Y, Brenner DA, et al. TLR4 enhances TGF-beta signaling and hepatic fibrosis. Nature medicine. 2007;13(11):1324–32. https://doi.org/10.1038/nm1663(Epub 2007/10/24).
De Minicis S, Rychlicki C, Agostinelli L, Saccomanno S, Candelaresi C, Trozzi L, et al. Dysbiosis contributes to fibrogenesis in the course of chronic liver injury in mice. Hepatology (Baltimore, Md). 2014;59(5):1738–49. https://doi.org/10.1002/hep.26695(Epub 2013/08/21).
Hartmann P, Chen P, Wang HJ, Wang L, McCole DF, Brandl K, et al. Deficiency of intestinal mucin-2 ameliorates experimental alcoholic liver disease in mice. Hepatology (Baltimore, Md). 2013;58(1):108–19. https://doi.org/10.1002/hep.26321(Epub 2013/02/15).
Wree A, Geisler LJ, Tacke F. Microbiome & NASH—partners in crime driving progression of fatty liver disease. Z Gastroenterol. 2019;57(7):871–82. https://doi.org/10.1055/a-0755-2595(Epub 2019/07/10).
Zhou M, Learned RM, Rossi SJ, DePaoli AM, Tian H, Ling L. Engineered FGF19 eliminates bile acid toxicity and lipotoxicity leading to resolution of steatohepatitis and fibrosis in mice. Hepatol Commun. 2017;1(10):1024–42. https://doi.org/10.1002/hep4.1108(Epub 2018/02/07).
Luo J, Ko B, Elliott M, Zhou M, Lindhout DA, Phung V, et al. A nontumorigenic variant of FGF19 treats cholestatic liver diseases. Sci Transl Med. 2014;6(247):247ra100. https://doi.org/10.1126/scitranslmed.3009098(Epub 2014/08/01).
Harrison SA, Rossi SJ, Paredes AH, Trotter JF, Bashir MR, Guy CD, et al. NGM282 improves liver fibrosis and histology in 12 weeks in patients with nonalcoholic steatohepatitis. Hepatology (Baltimore, Md). 2019. https://doi.org/10.1002/hep.30590(Epub 2019/02/26).
Harrison SA, Rinella ME, Abdelmalek MF, Trotter JF, Paredes AH, Arnold HL, et al. NGM282 for treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2018;391(10126):1174–85. https://doi.org/10.1016/s0140-6736(18)30474-4(Epub 2018/03/10).
Wells RG, Schwabe RF. Origin and function of myofibroblasts in the liver. Semin Liver Dis. 2015;35(2):e1. https://doi.org/10.1055/s-0035-1554915(Epub 2015/05/270).
Krenkel O, Hundertmark J, Ritz TP, Weiskirchen R, Tacke F. Single cell RNA sequencing identifies subsets of hepatic stellate cells and myofibroblasts in liver fibrosis. Cells. 2019. https://doi.org/10.3390/cells8050503(Epub 2019/05/30).
Barry-Hamilton V, Spangler R, Marshall D, McCauley S, Rodriguez HM, Oyasu M, et al. Allosteric inhibition of lysyl oxidase-like-2 impedes the development of a pathologic microenvironment. Nature medicine. 2010;16(9):1009–17. https://doi.org/10.1038/nm.2208(Epub 2010/09/08).
Ikenaga N, Peng ZW, Vaid KA, Liu SB, Yoshida S, Sverdlov DY, et al. Selective targeting of lysyl oxidase-like 2 (LOXL2) suppresses hepatic fibrosis progression and accelerates its reversal. Gut. 2017;66(9):1697–708. https://doi.org/10.1136/gutjnl-2016-312473(Epub 2017/01/12).
Yang J, Savvatis K, Kang JS, Fan P, Zhong H, Schwartz K, et al. Targeting LOXL2 for cardiac interstitial fibrosis and heart failure treatment. Nat Commun. 2016;7:13710. https://doi.org/10.1038/ncomms13710(Epub 2016/12/15).
Harrison SA, Abdelmalek MF, Caldwell S, Shiffman ML, Diehl AM, Ghalib R, et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis. Gastroenterology. 2018;155(4):1140–53. https://doi.org/10.1053/j.gastro.2018.07.006(Epub 2018/07/11).
Raghu G, Brown KK, Collard HR, Cottin V, Gibson KF, Kaner RJ, et al. Efficacy of simtuzumab versus placebo in patients with idiopathic pulmonary fibrosis: a randomised, double-blind, controlled, phase 2 trial. Lancet Respir Med. 2017;5(1):22–32. https://doi.org/10.1016/s2213-2600(16)30421-0(Epub 2016/12/13).
Marra F, Tacke F. Roles for chemokines in liver disease. Gastroenterology. 2014;147(3):577-94.e1. https://doi.org/10.1053/j.gastro.2014.06.043(Epub 2014/07/30).
Karlmark KR, Weiskirchen R, Zimmermann HW, Gassler N, Ginhoux F, Weber C, et al. Hepatic recruitment of the inflammatory Gr1+ monocyte subset upon liver injury promotes hepatic fibrosis. Hepatology (Baltimore, Md). 2009;50(1):261–74. https://doi.org/10.1002/hep.22950(Epub 2009/06/26).
Zimmermann HW, Seidler S, Nattermann J, Gassler N, Hellerbrand C, Zernecke A, et al. Functional contribution of elevated circulating and hepatic non-classical CD14CD16 monocytes to inflammation and human liver fibrosis. PloS One. 2010;5(6):e11049. https://doi.org/10.1371/journal.pone.0011049(Epub 2010/06/16).
Seki E, de Minicis S, Inokuchi S, Taura K, Miyai K, van Rooijen N, et al. CCR71 promotes hepatic fibrosis in mice. Hepatology (Baltimore, Md). 2009;50(1):185–97. https://doi.org/10.1002/hep.22952(Epub 2009/05/15).
Baeck C, Wehr A, Karlmark KR, Heymann F, Vucur M, Gassler N, et al. Pharmacological inhibition of the chemokine CCL2 (MCP-1) diminishes liver macrophage infiltration and steatohepatitis in chronic hepatic injury. Gut. 2012;61(3):416–26. https://doi.org/10.1136/gutjnl-2011-300304(Epub 2011/08/05).
Krenkel O, Puengel T, Govaere O, Abdallah AT, Mossanen JC, Kohlhepp M, et al. Therapeutic inhibition of inflammatory monocyte recruitment reduces steatohepatitis and liver fibrosis. Hepatology (Baltimore, Md). 2018;67(4):1270–83. https://doi.org/10.1002/hep.29544(Epub 2017/09/25).
Parker R, Weston CJ, Miao Z, Corbett C, Armstrong MJ, Ertl L, et al. CC chemokine receptor 2 promotes recruitment of myeloid cells associated with insulin resistance in nonalcoholic fatty liver disease. Am J Physiol Gastrointest Liver Physiol. 2018;314(4):G483-g93. https://doi.org/10.1152/ajpgi.00213.2017(Epub 2018/02/09).
Lefebvre E, Moyle G, Reshef R, Richman LP, Thompson M, Hong F, et al. Antifibrotic effects of the dual CCR75/CCR75 antagonist cenicriviroc in animal models of liver and kidney fibrosis. PloS One. 2016;11(6):e0158156. https://doi.org/10.1371/journal.pone.0158156(Epub 2016/06/28).
Weston CJ, Shepherd EL, Claridge LC, Rantakari P, Curbishley SM, Tomlinson JW, et al. Vascular adhesion protein-1 promotes liver inflammation and drives hepatic fibrosis. J Clin Investig. 2015;125(2):501–20. https://doi.org/10.1172/jci73722(Epub 2015/01/07).
Traber PG, Chou H, Zomer E, Hong F, Klyosov A, Fiel MI, et al. Regression of fibrosis and reversal of cirrhosis in rats by galectin inhibitors in thioacetamide-induced liver disease. PloS One. 2013;8(10):e75361. https://doi.org/10.1371/journal.pone.0075361(Epub 2013/10/17).
Harrison SA, Marri SR, Chalasani N, Kohli R, Aronstein W, Thompson GA, et al. Randomised clinical study: GR-MD-02, a galectin-3 inhibitor, vs placebo in patients having non-alcoholic steatohepatitis with advanced fibrosis. Aliment Pharmacol Ther. 2016;44(11–12):1183–98. https://doi.org/10.1111/apt.13816.
Lee L, Alloosh M, Saxena R, Van Alstine W, Watkins BA, Klaunig JE, et al. Nutritional model of steatohepatitis and metabolic syndrome in the Ossabaw miniature swine. Hepatology (Baltimore, Md). 2009;50(1):56–67. https://doi.org/10.1002/hep.22904(Epub 2009/05/13).
Liang W, Menke AL, Driessen A, Koek GH, Lindeman JH, Stoop R, et al. Establishment of a general NAFLD scoring system for rodent models and comparison to human liver pathology. PloS One. 2014;9(12):e115922. https://doi.org/10.1371/journal.pone.0115922.
Rinella ME, Tacke F, Sanyal AJ, Anstee QM. Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. J Hepatol. 2019. https://doi.org/10.1016/j.jhep.2019.04.019(Epub 2019/07/14).
Farrell GC, Mridha AR, Yeh MM, Arsov T, Van Rooyen DM, Brooling J, et al. Strain dependence of diet-induced NASH and liver fibrosis in obese mice is linked to diabetes and inflammatory phenotype. Liver Int. 2014;34(7):1084–93. https://doi.org/10.1111/liv.12335(Epub 2013/10/11).
McGettigan B, McMahan R, Orlicky D, Burchill M, Danhorn T, Francis P, et al. Dietary lipids differentially shape nonalcoholic steatohepatitis progression and the transcriptome of kupffer cells and infiltrating macrophages. Hepatology (Baltimore, Md). 2019;70(1):67–83. https://doi.org/10.1002/hep.30401(Epub 2018/12/06).
Hansen HH, Feigh M, Veidal SS, Rigbolt KT, Vrang N, Fosgerau K. Mouse models of nonalcoholic steatohepatitis in preclinical drug development. Drug Discov Today. 2017;22(11):1707–18. https://doi.org/10.1016/j.drudis.2017.06.007.
Santhekadur PK, Kumar DP, Sanyal AJ. Preclinical models of non-alcoholic fatty liver disease. J Hepatol. 2018;68(2):230–7. https://doi.org/10.1016/j.jhep.2017.10.031(Epub 2017/11/13).
Febbraio MA, Reibe S, Shalapour S, Ooi GJ, Watt MJ, Karin M. Preclinical models for studying NASH-driven HCC: how useful are they? Cell Metab. 2019;29(1):18–26. https://doi.org/10.1016/j.cmet.2018.10.012(Epub 2018/11/20).
Feaver RE, Cole BK, Lawson MJ, Hoang SA, Marukian S, Blackman BR, et al. Development of an in vitro human liver system for interrogating nonalcoholic steatohepatitis. JCI Insight. 2016;1(20):e90954. https://doi.org/10.1172/jci.insight.90954(Epub 2016/12/13).
Rennert K, Steinborn S, Groger M, Ungerbock B, Jank AM, Ehgartner J, et al. A microfluidically perfused three dimensional human liver model. Biomaterials. 2015;71:119–31. https://doi.org/10.1016/j.biomaterials.2015.08.043(Epub 2015/09/01).
Ouchi R, Togo S, Kimura M, Shinozawa T, Koido M, Koike H, et al. Modeling steatohepatitis in humans with pluripotent stem cell-derived organoids. Cell Metabolism. 2019. https://doi.org/10.1016/j.cmet.2019.05.007.
(CDER) USDoHaHSFaDACfDEaR. Nonalcoholic Steatohepatitis with Compensated Cirrhosis: Developing Drugs for Treatment Guidance for Industry [Guidance document]. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER); 2019 [updated June 2019; cited 2019 17.07.2019]. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/nonalcoholic-steatohepatitis-compensated-cirrhosis-developing-drugs-treatment-guidance-industry.
(EMA) EMA. Draft reflection paper on regulatory requirements for the development of medicinal products for chronic non-infectious liver diseases (PBC, PSC, NASH) [guidance paper]. European Medicines Agency (EMA); 2018 [updated 12.12.2018; cited 2019 22.07.2019]. https://www.ema.europa.eu/en/draft-reflection-paper-regulatory-requirements-development-medicinal-products-chronic-non-infectious.
Budas G, Karnik S, Jonnson T, Shafizadeh T, Watkins S, Breckenridge D, et al. Reduction of liver steatosis and fibrosis with an ask1 inhibitor in a murine model of nash is accompanied by improvements in cholesterol, bile acid and lipid metabolism. J Hepatol. 2016;64(2):S170. https://doi.org/10.1016/S0168-8278(16)01686-X.
Loomba R, Lawitz E, Mantry PS, Jayakumar S, Caldwell SH, Arnold H, et al. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: a randomized, phase 2 trial. Hepatology (Baltimore, Md). 2018;67(2):549–59. https://doi.org/10.1002/hep.29514(Epub 2017/09/12).
Markham A, Keam SJ. Obeticholic acid: first global approval. Drugs. 2016;76(12):1221–6. https://doi.org/10.1007/s40265-016-0616-x(Epub 2016/07/14).
Yu D, Cai SY, Mennone A, Vig P, Boyer JL. Cenicriviroc, a cytokine receptor antagonist, potentiates all-trans retinoic acid in reducing liver injury in cholestatic rodents. Liver Int. 2018;38(6):1128–38. https://doi.org/10.1111/liv.13698(Epub 2018/01/23).
Puengel T, Krenkel O, Kohlhepp M, Lefebvre E, Luedde T, Trautwein C, et al. Differential impact of the dual CCR96/CCR96 inhibitor cenicriviroc on migration of monocyte and lymphocyte subsets in acute liver injury. PloS One. 2017;12(9):e0184694. https://doi.org/10.1371/journal.pone.0184694(Epub 2017/09/15).
Kruger AJ, Fuchs BC, Masia R, Holmes JA, Salloum S, Sojoodi M, et al. Prolonged cenicriviroc therapy reduces hepatic fibrosis despite steatohepatitis in a diet-induced mouse model of nonalcoholic steatohepatitis. Hepatol Commun. 2018;2(5):529–45. https://doi.org/10.1002/hep4.1160(Epub 2018/05/16).
Mossanen JC, Krenkel O, Ergen C, Govaere O, Liepelt A, Puengel T, et al. Chemokine (C-C motif) receptor 2-positive monocytes aggravate the early phase of acetaminophen-induced acute liver injury. Hepatology (Baltimore, Md). 2016;64(5):1667–82. https://doi.org/10.1002/hep.28682(Epub 2016/10/22).
Friedman S, Sanyal A, Goodman Z, Lefebvre E, Gottwald M, Fischer L, et al. Efficacy and safety study of cenicriviroc for the treatment of non-alcoholic steatohepatitis in adult subjects with liver fibrosis: CENTAUR Phase 2b study design. Contemp Clin Trials. 2016;47:356–65. https://doi.org/10.1016/j.cct.2016.02.012(Epub 2016/03/06).
Ratziu V, Sanyal A, Francque S, Wai-Sun Wong V, Loomba R, Goodman Z, Lefebvre E, Aithal GP, Harrison, SA, Abdelmalek MF, Friedman SL, Tacke F. Cenicriviroc treatment for adults with non-alcoholic steatohepatitis: year 2 analysis of the phase 2b CENTAUR study [conference talk]. International Liver Congress 2019, EASL, Paris: EASL; 2018 [updated 16.04.2018; cited 2019 17.07.2019]. https://livertree.easl.eu/easl/2018/international.liver.congress/210644/vlad.ratziu.cenicriviroc.treatment.for.adults.with.non-alcoholic.html.
Cao W, An X, Cong L, Lyu C, Zhou Q, Guo R. Application of deep learning in quantitative analysis of 2-dimensional ultrasound imaging of nonalcoholic fatty liver disease. J Ultrasound Med. 2019. https://doi.org/10.1002/jum.15070(Epub 2019/06/22).
Singh A, Dhaliwal AS, Singh S, Kumar A, Lopez R, Gupta M, et al. Awareness of nonalcoholic fatty liver disease is increasing but remains very low in a representative US cohort. Dig Dis Sci. 2019. https://doi.org/10.1007/s10620-019-05700-9(Epub 2019/06/13).
Corey KE, Wilson LA, Altinbas A, Yates KP, Kleiner DE, Chung RT, et al. Relationship between resolution of non-alcoholic steatohepatitis and changes in lipoprotein sub-fractions: a post-hoc analysis of the PIVENS trial. Aliment Pharmacol Ther. 2019;49(9):1205–13. https://doi.org/10.1111/apt.15216(Epub 2019/03/12).
Tully DC, Rucker PV, Chianelli D, Williams J, Vidal A, Alper PB, et al. Discovery of tropifexor (LJN452), a highly potent non-bile acid FXR agonist for the treatment of cholestatic liver diseases and nonalcoholic steatohepatitis (NASH). J Med Chem. 2017;60(24):9960–73. https://doi.org/10.1021/acs.jmedchem.7b00907(Epub 2017/11/18).
Kaul U, Parmar D, Manjunath K, Shah M, Parmar K, Patil KP, et al. New dual peroxisome proliferator activated receptor agonist—Saroglitazar in diabetic dyslipidemia and non-alcoholic fatty liver disease: integrated analysis of the real world evidence. Cardiovasc Diabetol. 2019;18(1):80. https://doi.org/10.1186/s12933-019-0884-3.
Odegaard JI, Ricardo-Gonzalez RR, Red Eagle A, Vats D, Morel CR, Goforth MH, et al. Alternative M2 activation of Kupffer cells by PPARdelta ameliorates obesity-induced insulin resistance. Cell Metab. 2008;7(6):496–507. https://doi.org/10.1016/j.cmet.2008.04.003(Epub 2008/06/05).
Lee CH, Olson P, Hevener A, Mehl I, Chong LW, Olefsky JM, et al. PPARdelta regulates glucose metabolism and insulin sensitivity. Proc Natl Acad Sci USA. 2006;103(9):3444–9. https://doi.org/10.1073/pnas.0511253103(Epub 2006/02/24).
Leone TC, Weinheimer CJ, Kelly DP. A critical role for the peroxisome proliferator-activated receptor alpha (PPARalpha) in the cellular fasting response: the PPARalpha-null mouse as a model of fatty acid oxidation disorders. Proc Natl Acad Sci USA. 1999;96(13):7473–8. https://doi.org/10.1073/pnas.96.13.7473(Epub 1999/06/23).
Harriman G, Greenwood J, Bhat S, Huang X, Wang R, Paul D, et al. Acetyl-CoA carboxylase inhibition by ND-630 reduces hepatic steatosis, improves insulin sensitivity, and modulates dyslipidemia in rats. Proc Natl Acad Sci. 2016;113(13):E1796–805. https://doi.org/10.1073/pnas.1520686113.
Struik D, Dommerholt MB, Jonker JW. Fibroblast growth factors in control of lipid metabolism: from biological function to clinical application. Curr Opin Lipidol. 2019;30(3):235–43. https://doi.org/10.1097/mol.0000000000000599(Epub 2019/03/21).
McCommis KS, Hodges WT, Brunt EM, Nalbantoglu I, McDonald WG, Holley C, et al. Targeting the mitochondrial pyruvate carrier attenuates fibrosis in a mouse model of nonalcoholic steatohepatitis. Hepatology (Baltimore, Md). 2017;65(5):1543–56. https://doi.org/10.1002/hep.29025(Epub 2016/12/28).
McCommis KS, Chen Z, Fu X, McDonald WG, Colca JR, Kletzien RF, et al. Loss of mitochondrial pyruvate carrier 2 in the liver leads to defects in gluconeogenesis and compensation via pyruvate-alanine cycling. Cell Metab. 2015;22(4):682–94. https://doi.org/10.1016/j.cmet.2015.07.028(Epub 2015/09/08).
Bricker DK, Taylor EB, Schell JC, Orsak T, Boutron A, Chen YC, et al. A mitochondrial pyruvate carrier required for pyruvate uptake in yeast, Drosophila, and humans. Science (New York, NY). 2012;337(6090):96–100. https://doi.org/10.1126/science.1218099(Epub 2012/05/26).
Nagampalli RSK, Quesnay JEN, Adamoski D, Islam Z, Birch J, Sebinelli HG, et al. Human mitochondrial pyruvate carrier 2 as an autonomous membrane transporter. Sci Rep. 2018;8(1):3510. https://doi.org/10.1038/s41598-018-21740-z(Epub 2018/02/24).
Kelly MJ, Pietranico-Cole S, Larigan JD, Haynes NE, Reynolds CH, Scott N, et al. Discovery of 2-[3,5-dichloro-4-(5-isopropyl-6-oxo-1,6-dihydropyridazin-3-yloxy)phenyl]-3,5-dio xo-2,3,4,5-tetrahydro[1,2,4]triazine-6-carbonitrile (MGL-3196), a Highly Selective Thyroid Hormone Receptor beta agonist in clinical trials for the treatment of dyslipidemia. J Med Chem. 2014;57(10):3912–23. https://doi.org/10.1021/jm4019299(Epub 2014/04/10).
Taub R, Chiang E, Chabot-Blanchet M, Kelly MJ, Reeves RA, Guertin MC, et al. Lipid lowering in healthy volunteers treated with multiple doses of MGL-3196, a liver-targeted thyroid hormone receptor-beta agonist. Atherosclerosis. 2013;230(2):373–80. https://doi.org/10.1016/j.atherosclerosis.2013.07.056(Epub 2013/10/01).
Dibba P, Li AA, Perumpail BJ, John N, Sallam S, Shah ND, et al. Emerging therapeutic targets and experimental drugs for the treatment of NAFLD. Diseases. 2018. https://doi.org/10.3390/diseases6030083(Epub 2018/09/22).
Roth JD, Veidal SS, Fensholdt LKD, Rigbolt KTG, Papazyan R, Nielsen JC, et al. Combined obeticholic acid and elafibranor treatment promotes additive liver histological improvements in a diet-induced ob/ob mouse model of biopsy-confirmed NASH. Sci Rep. 2019;9(1):9046. https://doi.org/10.1038/s41598-019-45178-z(Epub 2019/06/23).
Lindstrom P. The physiology of obese-hyperglycemic mice [ob/ob mice]. Sci World J. 2007;7:666–85. https://doi.org/10.1100/tsw.2007.117(Epub 2007/07/11).
Mayer J, Bates MW, Dickie MM. Hereditary diabetes in genetically obese mice. Science (New York, NY). 1951;113(2948):746–7. https://doi.org/10.1126/science.113.2948.746(Epub 1951/06/29).
Hummel KP, Dickie MM, Coleman DL. Diabetes, a new mutation in the mouse. Science (New York, NY). 1966;153(3740):1127–8. https://doi.org/10.1126/science.153.3740.1127(Epub 1966/09/02).
Hum D SA, Harrison S, et al. Elafibranor: a liver targeted PPARα/δ agonist for a global management of nash patients. In: EASL, editor. Poster session presented at: The International Liver Congress Meeting, EASL; 2016 April 13–17; Barcelona, Spain. 2016.
Poekes L, Legry V, Farrell G, Leclercq I. Role of ciliary dysfunction in a new model of obesity and non-alcoholic steatohepatitis: the foz/fozmice. Arch Publ Health. 2014;72(1):O7. https://doi.org/10.1186/2049-3258-72-s1-o7.
Heydet D, Chen LX, Larter CZ, Inglis C, Silverman MA, Farrell GC, et al. A truncating mutation of Alms1 reduces the number of hypothalamic neuronal cilia in obese mice. Dev Neurobiol. 2013;73(1):1–13. https://doi.org/10.1002/dneu.22031(Epub 2012/05/15).
Arsov T, Silva DG, O’Bryan MK, Sainsbury A, Lee NJ, Kennedy C, et al. Fat Aussie—a new alström syndrome mouse showing a critical role for ALMS1 in obesity, diabetes, and spermatogenesis. Mol Endocrinol. 2006;20(7):1610–22. https://doi.org/10.1210/me.2005-0494.
Liepelt A, Wehr A, Kohlhepp M, Mossanen JC, Kreggenwinkel K, Denecke B, et al. CXCR127 protects from inflammation and fibrosis in NEMO(LPC-KO) mice. Biochim Biophys Acta Mol Basis Dis. 2019;1865(2):391–402. https://doi.org/10.1016/j.bbadis.2018.11.020(Epub 2018/11/27).
Luedde T, Beraza N, Kotsikoris V, van Loo G, Nenci A, De Vos R, et al. Deletion of NEMO/IKKgamma in liver parenchymal cells causes steatohepatitis and hepatocellular carcinoma. Cancer Cell. 2007;11(2):119–32. https://doi.org/10.1016/j.ccr.2006.12.016(Epub 2007/02/13).
Horie Y, Suzuki A, Kataoka E, Sasaki T, Hamada K, Sasaki J, et al. Hepatocyte-specific Pten deficiency results in steatohepatitis and hepatocellular carcinomas. J Clin Investig. 2004;113(12):1774–83. https://doi.org/10.1172/JCI20513.
Stiles B, Wang Y, Stahl A, Bassilian S, Lee WP, Kim Y-J, et al. Liver-specific deletion of negative regulator Pten results in fatty liver and insulin hypersensitivity. Proc Natl Acad Sci. 2004;101(7):2082–7. https://doi.org/10.1073/pnas.0308617100.
Cole BK, Feaver RE, Wamhoff BR, Dash A. Non-alcoholic fatty liver disease (NAFLD) models in drug discovery. Expert Opin Drug Discov. 2018;13(2):193–205. https://doi.org/10.1080/17460441.2018.1410135(Epub 2017/12/01).
Kawashita E, Ishihara K, Nomoto M, Taniguchi M, Akiba S. A comparative analysis of hepatic pathological phenotypes in C57BL/6J and C57BL/6N mouse strains in non-alcoholic steatohepatitis models. Sci Rep. 2019;9(1):204. https://doi.org/10.1038/s41598-018-36862-7(Epub 2019/01/20).
Mells JE, Fu PP, Sharma S, Olson D, Cheng L, Handy JA, et al. Glp-1 analog, liraglutide, ameliorates hepatic steatosis and cardiac hypertrophy in C57BL/6J mice fed a Western diet. Am J Physiol Gastrointest Liver Physiol. 2012;302(2):G225–35. https://doi.org/10.1152/ajpgi.00274.2011(Epub 2011/11/01).
Matsumoto M, Hada N, Sakamaki Y, Uno A, Shiga T, Tanaka C, et al. An improved mouse model that rapidly develops fibrosis in non-alcoholic steatohepatitis. Int J Exp Pathol. 2013;94(2):93–103. https://doi.org/10.1111/iep.12008.
Fujii M, Shibazaki Y, Wakamatsu K, Honda Y, Kawauchi Y, Suzuki K, et al. A murine model for non-alcoholic steatohepatitis showing evidence of association between diabetes and hepatocellular carcinoma. Med Mol Morphol. 2013;46(3):141–52. https://doi.org/10.1007/s00795-013-0016-1(Epub 2013/02/23).
Lo L, McLennan SV, Williams PF, Bonner J, Chowdhury S, McCaughan GW, et al. Diabetes is a progression factor for hepatic fibrosis in a high fat fed mouse obesity model of non-alcoholic steatohepatitis. J Hepatol. 2011;55(2):435–44. https://doi.org/10.1016/j.jhep.2010.10.039(Epub 2010/12/28).
Stefano JT, Pereira IV, Torres MM, Bida PM, Coelho AM, Xerfan MP, et al. Sorafenib prevents liver fibrosis in a non-alcoholic steatohepatitis (NASH) rodent model. Braz J Med Biol Res. 2015;48(5):408–14. https://doi.org/10.1590/1414-431x20143962(Epub 2015/02/26).
Kluwe J, Pradere JP, Gwak GY, Mencin A, De Minicis S, Österreicher CH, et al. Modulation of hepatic fibrosis by c-Jun-N-terminal kinase inhibition. Gastroenterology. 2010;138(1):347–59. https://doi.org/10.1053/j.gastro.2009.09.015.
Tag CG, Sauer-Lehnen S, Weiskirchen S, Borkham-Kamphorst E, Tolba RH, Tacke F, et al. Bile duct ligation in mice: induction of inflammatory liver injury and fibrosis by obstructive cholestasis. J Vis Exp. 2015. https://doi.org/10.3791/52438.
Asgharpour A, Cazanave SC, Pacana T, Seneshaw M, Vincent R, Banini BA, et al. A diet-induced animal model of non-alcoholic fatty liver disease and hepatocellular cancer. J Hepatol. 2016;65(3):579–88. https://doi.org/10.1016/j.jhep.2016.05.005(Epub 2016/06/05).
Hernandez ED, Zheng L, Kim Y, Fang B, Liu B, Valdez RA, et al. Tropifexor-mediated abrogation of steatohepatitis and fibrosis is associated with the antioxidative gene expression profile in rodents. Hepatol Commun. 2019;3(8):1085–97. https://doi.org/10.1002/hep4.1368(Epub 2019/08/08).
Tetri LH, Basaranoglu M, Brunt EM, Yerian LM, Neuschwander-Tetri BA. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. Am J Physiol Gastrointest Liver Physiol. 2008;295(5):G987–95. https://doi.org/10.1152/ajpgi.90272.2008.
Schierwagen R, Maybuchen L, Zimmer S, Hittatiya K, Back C, Klein S, et al. Seven weeks of Western diet in apolipoprotein-E-deficient mice induce metabolic syndrome and non-alcoholic steatohepatitis with liver fibrosis. Sci Rep. 2015;5:12931. https://doi.org/10.1038/srep12931(Epub 2015/08/12).
Sun G, Jackson CV, Zimmerman K, Zhang LK, Finnearty CM, Sandusky GE, et al. The FATZO mouse, a next generation model of type 2 diabetes, develops NAFLD and NASH when fed a Western diet supplemented with fructose. BMC Gastroenterol. 2019;19(1):41. https://doi.org/10.1186/s12876-019-0958-4(Epub 2019/03/20).
Shalapour S, Lin XJ, Bastian IN, Brain J, Burt AD, Aksenov AA, et al. Inflammation-induced IgA+ cells dismantle anti-liver cancer immunity. Nature. 2017;551(7680):340–5. https://doi.org/10.1038/nature24302(Epub 2017/11/17).
Nakagawa H, Umemura A, Taniguchi K, Font-Burgada J, Dhar D, Ogata H, et al. ER stress cooperates with hypernutrition to trigger TNF-dependent spontaneous HCC development. Cancer Cell. 2014;26(3):331–43. https://doi.org/10.1016/j.ccr.2014.07.001.
Weglarz TC, Degen JL, Sandgren EP. Hepatocyte transplantation into diseased mouse liver Kinetics of parenchymal repopulation and identification of the proliferative capacity of tetraploid and octaploid hepatocytes. Am J Pathol. 2000;157(6):1963–74. https://doi.org/10.1016/s0002-9440(10)64835-3.
Funding
This work was funded by German Research Foundation (WR173/3-1, TA434/3-1, SFB/TRR57 and CRC1382 to AW and FT) and German Cancer Aid (Deutsche Krebshilfe 70113000 to AW).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tacke’s group has received research funding from Allergan, Inventiva, Bristol Myers Squibb, and Galapagos. The other authors state no conflict of interest.
Research involving human and animals participants
This article is a review of the literature and does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reimer, K.C., Wree, A., Roderburg, C. et al. New drugs for NAFLD: lessons from basic models to the clinic. Hepatol Int 14, 8–23 (2020). https://doi.org/10.1007/s12072-019-10001-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-10001-4