Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) has become the most common form of chronic liver disease in the USA. Interestingly, most patients with NAFLD are unaware of having any liver disease (LD). We aimed to assess the awareness of suspected NAFLD and factors associated with being aware of LD.
Methods
Adult subjects with suspected NAFLD (BMI > 25) with elevated ALT in the absence of secondary causes of LD who participated in the continuous national health and nutrition examination survey (NHANES) during 2001–2016 were identified and analyzed. Trends of NAFLD awareness were then assessed in periods of 4 years each. Multivariable logistic regression analysis was performed to assess factors associated with LD awareness.
Results
A total of 7033 subjects were included in the final analysis (1731, 1757, 1711, and 1834 subjects for the periods of 2001–2004, 2005–2008, 2009–2012, and 2013–2016, respectively). Over the study duration, an increase in BMI, waist circumference, diabetes, and HbA1c; and a decrease in the number of smokers, platelets count, bilirubin, total cholesterol, and LDL level were noticed (p < 0.001). Awareness of having LD across study periods has increased over time from 1.5% in the 2001–2004 periods to 3.1% in the 2013–2016 periods. Multivariable logistic regression analysis showed that older age, ethnicity (non-black), having fewer drinks/week, metabolic syndrome, higher ALT, ALP, and GGT were associated with being aware of having LD.
Conclusions
Awareness of having LD among subjects with suspected NAFLD has increased over the last two decades, but more than 95% of these patients are still unaware of having LD. Educational programs to increase awareness of LD and risk factors for NAFLD should be implemented on a large scale.
Clinical Trial Registration Number
Not required, as we used de-identified NHANES data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, nonalcoholic fatty liver disease (NAFLD) has become the most common form of chronic liver disease, both in developed and developing countries. The imaging-based global prevalence of NAFLD has been estimated to be around 25%, affecting nearly 1.8 billion individuals worldwide [1]. The overall prevalence of NAFLD among US adults was found to be 21.9%, representing 51.6 million adults, and as many as 5 million adults were estimated to have advanced disease [2]. The pathological spectrum of NAFLD ranges from simple steatosis, which is considered as a benign condition, to nonalcoholic steatohepatitis (NASH) to advanced fibrosis (AF), cirrhosis, and end-stage liver disease (ESLD). NASH is considered the trigger for progression to AF and cirrhosis, further leading to complications related to ESLD. In a recent study, the prevalence of NASH-cirrhosis and NAFLD-associated fibrosis has increased by 2.5- and twofold in the US population [3]. Over the last decade, hepatitis C virus (HSV) infection has been the leading cause of liver transplantation in men, but a recent study reported NASH to be the leading cause of liver transplantation in women, and the second leading cause for men in 2016, indicating the rising healthcare burden from NASH and its associated complications [4].
Insulin resistance and other features of metabolic syndrome (MetS) have been postulated to be associated with the pathogenesis of NAFLD, although the exact mechanisms are still unknown [5]. With the ongoing obesity epidemic, an increasing prevalence of diabetes, and other features of MetS, the prevalence of NAFLD is on the rise with a fast pace [6, 7]. However, a majority of these patients will not develop liver-related complication with the most common cause of death being related to cardiovascular diseases, followed by malignancy [8, 9]. Patients with NAFLD are also at a higher risk of having chronic kidney disease [10] and other complication related to metabolic syndrome, especially in diabetics [11]. Despite the growing burden of NAFLD and its associated complications, there is a lack of awareness among primary care physicians, hospital specialists, and most importantly among the patients. In a survey of 302 patients in an outpatient clinical setting, only 18% of respondents were familiar with NAFLD. Interestingly, 67% of the unaware subjects had metabolic risk factors [6]. Another study from Hong Kong also showed low awareness (17%) of NAFLD among the general population, with misconceptions about the diagnosis and clinical presentation [12].
Low awareness of NAFLD among the general population is a matter of great concern as low awareness can delay healthcare screening and prevention of NAFLD and its related complications. This is also important for resource allocation, and the creation and implementation of awareness programs. Therefore, we aimed to assess the awareness of suspected NAFLD and factors associated with being aware of having a liver disease (LD) in a large adult (age ≥ 20 years) US sample population using the National Health and Nutrition Examination Survey (NHANES) database.
Methods
Data Source
The NHANES is a survey program conducted by the National Center for Health Statistics (NCHS), which is part of the Centers for Disease Control and Prevention (CDC). The program is designed to assess the health and nutritional status of adults and children in the USA. It began in the early 1960s and became a continuous program in 1999. It examines a sample of 5000 persons a year from different counties across the USA representing the US population of all ages. The survey includes interview questionnaires, standardized physical examination, and laboratory tests from blood samples collected at examination centers and analyzed at a central laboratory. The survey was approved by the Institutional Review Board at the Center for Disease Control and Prevention, and informed consent was obtained from all participants. Data obtained during the 2001–2004, 2005–2008, 2009–2012, and 2013–2016 cycles were analyzed.
Inclusion and Exclusion Criteria
Participants 18 years or older with available demographic (gender, age, and ethnicity) and clinical (body mass index [BMI], waist circumference, systolic blood pressure, and diastolic blood pressure) data were analyzed. The following laboratory data were collected for analysis: aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transpeptidase (GGT), alkaline phosphatase, albumin, total bilirubin, platelet count, creatinine, fasting glucose, fasting insulin, hemoglobin A1C (HbA1c), triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL).
Patients were included if they had suspected NAFLD defined as being overweight (BMI ≥ 25 kg/m2) and elevated ALT, or hepatic steatosis index (HSI) ≥ 36, in the absence of secondary causes of hepatic steatosis.
We excluded participants with viral hepatitis (B or C), excessive alcohol consumption, AST or ALT > 500 U/l, patients on hepatotoxic drugs (known use of cholesterol-lowering medications, steroids [prednisone or cortisone] or tuberculosis medications for preventing or treating disease), and participants who did not respond to the liver-related questionnaires (Table 1).
Definitions
MetS was defined according to the updated International Diabetes Federation (IDF) [13] criteria as follows:
Central Obesity (waist circumference ≥ 102 cm for men or ≥ 88 cm for women) plus at least 2 of the following:
Fasting plasma glucose > 110 mg/dL or history of oral hypoglycemic, insulin or diabetes.
Blood pressure > 130/85 mmHg.
Triglycerides > 150 mg/dL.
Low HDL.
Obesity was defined as BMI ≥ 30 kg/m2 and severe obesity as BMI ≥ 40 kg/m2.
Abnormal liver tests included one of the following: ALT > 30U/L for men and > 19 U/L for women, alkaline phosphatase > 113 U/L or total bilirubin > 1.3 mg/dL.
HSI [14] was calculated using the following formula: 8 × (AST/ALT) + BMI (+2, if DM; +2, if female). The noninvasive fibrosis scores (APRI, FIB-4, and NFS) were used to detect AF. We defined NAFLD-associated AF as one of the following fibrosis markers: AST/ALT > 1.4, APRI > 1.5, FIB-4 index > 2.67, or NFS > 0.676.
We used the following equation to calculate APRI: (AST [U/L]/ULN)/platelet [109/l]) × 100. ULN stands for upper limit of normal. FIB-4 was calculated from the following equation (Age [yrs.] × AST [U/L])/(platelets [10 9/l] × ALT [U/L] 1/2). NFS was calculated as: − 1.675 + (0.037 × Age [yrs.]) + (0.094 × BMI [kg/m2]) + (1.13 × impaired fasting glucose/diabetes) + (0.99 × AST/ALT) − (0.013 × platelet [10 9/L]) − (0.66 × albumin (g/dL)).
Excessive alcohol consumption was defined as > 2 drinks/day for men and > 1 drink/day for women in the past year. A current smoker was defined as reports of ongoing smoking. Hypertension was defined as systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg or use of antihypertensive medications.
Diabetes was defined as fasting blood glucose ≥ 126, HbA1c > 6%, history of use of oral hypoglycemic or insulin, and/or report of having diabetes. Hypercholesterolemia was defined as cholesterol > 200 mg/dl or LDL ≥ 139 mg/dl. Hypertriglyceridemia was defined as triglycerides > 150 mg/dl, and low HDL was defined as high-density lipoprotein ≤ 40 mg/dl for men or ≤ 50 mg/dl for women.
Awareness was defined according to the individual’s response to specific NHANES questionnaires (MCQ160L and MCQ170QL). The subjects were considered “aware” of ever having a LD or current LD, if they answered, “Yes” under questions MCQ160L (has a doctor or other health professional ever told you that you had any kind of liver condition?) and MC170QL (do you still have any kind of liver condition?) of the medical conditions questionnaire. An answer of “No” or “Don’t know” to MCQ160L or MCQ170L was considered as being “unaware.”
Statistical Analysis
Data are presented as a weighted mean ± standard error (SE) or percentage. Weighted linear and logistic regression analyses were used to assess trends across different time periods. In addition, multivariable weighted logistic regression analysis was performed to assess factors associated with LD awareness; all factors except steatosis and fibrosis scores were considered for inclusion, and a backward elimination method was used to choose the final model. All analyses were performed using SAS SURVEY procedures (version 9.4, The SAS Institute, Cary, NC), which account for the complex sampling design of NHANES and appropriately weight participants in statistical models. Fasting glucose weights were used in all analyses; combined weights were calculated following the guidelines provided in the NHANES analytic guidelines [15]. Survey sample weights account for oversampling as well as survey non-response; proper usage of these in analysis ensures the calculated estimates are representative of the US civilian non-institutionalized population. Also, data sub-setting was done following the inclusion/exclusion criteria described above but, to have a proper estimation of the parameters of interest, the entire set of data containing appropriate weights was used with the estimation procedure indicating which records were in the subgroup of interest [15]. A significance level of 0.05 was used for all analyses.
Results
Characteristics of Study Participants
After exclusions (Table 1), a total of 7033 subjects were included in the final analysis (1731, 1757, 1711, and 1834 subjects for the periods of 2001–2004, 2005–2008, 2009–2012, and 2013–2016, respectively). Table 2 shows the participants characteristics. Overall, there were no significant differences among different cycles regarding age, gender, and ethnicity. A significant increase in BMI, waist circumference, severe obesity, diabetes, MetS, and hypertriglyceridemia was noted from 2001–2004 to 2013–2016 cycles (p < 0.05 for all). Interestingly, there was no difference in central obesity among various cycles (p = 0.17). The percentage of current smokers decreased from 21.4% in 2001–2004 cycles to 14.4% during 2013–2016 (p < 0.001). In terms of laboratory data, a significant decrease in albumin, platelets, creatinine, total cholesterol, and LDL; and an increase in AST, ALT, bilirubin, triglycerides, and HbA1c were noted with progressive study intervals (p < 0.05 for all).
Based on HSI ≥ 36, there has been a progressive rise in the prevalence of suspected NAFLD from 71.6% in 2001–2004 to 74–74.5% in the next two cycles, and 76.1% during 2012–2016 (p = 0.04). A twofold increase in the prevalence of AF (NFS > 0.676) was noted during these progressive intervals (2.2–4.4%, p < 0.001) (Table 2).
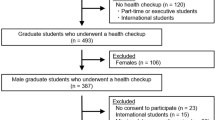
NAFLD Awareness in Different NHANES Cycles
In terms of awareness of LD, there was no difference in the awareness of participants regarding having an LD at any time (p = 0.29). But, awareness of having LD across study periods has increased over time from 1.5% in the 2001–2004 periods to 3.1% during 2013–2016 (p = 0.03) (Table 2) Also, the awareness of LD among subjects with suspected NAFLD and HSI > 36 have increased from 1.6 to 3.4% (p = 0.025) during these study intervals. The awareness of LD among patients with suspected NAFLD and AF (NFS > 0.676) initially increased from 3.5% in 2001–2004 cycles to 12.5% in 2005–2008. But, it decreased to 3% in 2009–2012 and 3.5% in 2013–2016 cycles (p = 0.88) (Fig. 1).
Awareness of currently having a liver disease among subjects with suspected NAFLD and a HSI > 36 or b NFS > 0.676. (Diamonds correspond to weighted percent. The whiskers represent the weighted 95% confidence interval estimates. p values correspond to unadjusted weighted trend test.) Abbreviations: HSI hepatic steatosis index, NAFLD nonalcoholic fatty liver disease, NFS nonalcoholic fatty liver disease fibrosis score
For multivariate analysis, age, gender, ethnicity, severe obesity, smoking, average number of drinks per day, MetS, albumin, platelet count, ALT, AST, alkaline phosphatase, bilirubin, creatinine, cholesterol, triglycerides, HDL, LDL, GGT and glycohemoglobin were considered for inclusion in the model. After using a backward elimination method gender, severe obesity, smoking, albumin, platelet count, AST, bilirubin, creatinine, cholesterol, triglycerides, HDL, LDL, and glycohemoglobin were not included in the final model. The results of multivariable regression analysis showed that older age and having fewer number of drinks/day was associated with being aware of having a LD (odd ratio [OR] 95% confidence interval {CI}; 1.1 (1.04, 1.2) (p = 0.002) and 0.47 (0.26, 0.88) (p = 0.018)). In terms of race, compared to blacks, Caucasian, other Hispanics (except Mexican-American), or other races (American Indian/Alaska Native/Asian/Pacific Islander/Native Hawaiian/multiracial) were more aware of having a LD (OR [95% CI]; 3.0 (1.3, 7.1), 4.2 (1.7, 10.7), and 4.5 (1.4, 14.1)) with p values of 0.011, 0.003, and 0.011, respectively. Subjects with MetS had twofold higher awareness of having an LD than without MetS (OR [95% CI]; 2.1 (1.3, 3.4) (p = 0.005)). Finally, subjects with higher ALT, ALP, and GGT were more aware of having a LD (OR [95% CI]; 1.3 (1.1, 1.5) (p < 0.001), 1.09 (1.00, 1.2) (p = 0.039), and 1.1 (1.04, 1.2) (p = 0.004), respectively) (Table 3).
Discussion
Our study highlights the critical findings that despite an increase in awareness of having a LD (1.5–3.1% during the study periods of 2001–2004 to 2013–2016 [p = 0.03]), especially among subjects with suspected NAFLD and HSI > 36 (1.6–3.4% [p = 0.025]), more than 95% of the adult US population with suspected NAFLD is still unaware of having any LD, suggesting the low awareness among this high-risk group. A twofold increase in the prevalence of AF was also noted during these progressive intervals (2.2–4.4%, p < 0.001), but only 3–3.5% of these high-risk patients had awareness of having LD over the past decade. There was no significant increase in awareness during different cycles in those with AF (p = 0.88). Over the study intervals, a significant increase in BMI, waist circumference, severe obesity, diabetes, MetS, and hypertriglyceridemia was noted among these participants (p < 0.05 for all), indicating the increase in risk factors for NAFLD. Older age, non-blacks, and subjects with MetS, and higher values of liver enzymes (ALT, ALP, and GGT) were found to have a higher awareness of having LD. To our knowledge, this is the first and largest study highlighting the low awareness of having an LD among the representative US population, especially in subjects with suspected NAFLD and AF.
With the ongoing obesity epidemic, increasing prevalence of diabetes, and other features of metabolic syndrome the prevalence of NAFLD, NASH-cirrhosis, and NAFLD-associated fibrosis is on the rise making it the leading cause of liver transplantation in USA [4]. Even in our study a twofold increase in the prevalence of AF was noted during progressive intervals (2.2–4.4%, p < 0.001). Despite all this, the overall awareness of NAFLD, especially with AF, has remained low in the general population. In 2012, in a survey of 302 patients, Wieland and colleagues [6] found that only 18% of the respondents were aware of NAFLD. Even in patients with major risk factors for NAFLD like overweight/obesity, insulin resistant, or both, the rates of NAFLD awareness were low at 19%, 23%, and 24%, respectively. The awareness of NAFLD in 2009–2012 in our study was 2.1% and 3.3% during 2013–2016 cycles, which is significantly lower than what was reported (18%) by Wieland and colleagues [6]. Inclusion of high-risk patients with higher education and motivation level appears to be responsible for higher awareness in the mentioned study. However, this limits the generalizability of the results but raises the concern of low awareness of NAFLD even in high-risk and medically engaged groups. Our results represent the US population sample and can be generalized. However, with the selection criteria’s of NAFLD based on obesity and high ALT, along with HSI ≥ 36 we might have underestimated the prevalence and awareness of NAFLD. As lack of obesity and normal liver enzymes does not necessarily eliminate one’s risk of NAFLD [16,17,18]. We also found an increasing prevalence of waist circumference, severe obesity, diabetes, MetS, and hypertriglyceridemia in our study population again raising the concerns of low awareness of NAFLD, despite an increase in the prevalence of metabolic risk factors for NAFLD. Interestingly, the majority of the participants in the survey by Wieland and colleagues, expressed interest in learning about NAFLD suggesting opportunities to raise awareness of NAFLD, particularly among patients with high metabolic risks, and to provide education to high-risk individuals with the goal of implementing early prevention strategies and optimizing care.
In our study, older age, non-black ethnicity, fewer drinks/day, and subjects having MetS, and higher liver enzymes were associated with being aware of having LD. The prevalence of NAFLD increases with age, and patients tend to seek more medical attention in older age groups providing more opportunities to learn about NAFLD [19]. African Americans (AA) tend to have a significantly lower prevalence of NAFLD compared with Caucasians and Hispanics [20]. Lower prevalence, poor socioeconomic status, and lower education levels in them could be the reasons for low awareness of NAFLD in this group [21]. But, once NAFLD develops, NASH occurs as frequently, and as severe, as in Caucasian patients. Therefore, AA with NAFLD should be screened for NASH with the same degree of clinical resolve as in Caucasian patients. Patients with MetS and high liver enzymes tend to get more attention and more testing for having LD, explaining higher awareness in these patients [16, 17]. This also highlights the poor understanding and awareness of NAFLD among patients and primary care physicians. In a telephone survey of 521 subjects in Hong Kong, only 17% were aware of NAFLD, and 78% of them had a misconception that NAFLD can be diagnosed with blood tests. Among the participants who were aware of NAFLD, their knowledge was perceived as either inadequate (46%) or highly inadequate (35%) [12]. Similarly, multiple studies have demonstrated the lack of awareness regarding prevalence, diagnosis, and guidelines among primary care/community physicians and non-hepatologist hospital specialists, which further reflects the poor awareness among general populations [22,23,24].
To increase the awareness of NAFLD, it is essential to understand the perceptions of patients regarding lifestyle, diet, exercise, and metabolic risk factors. In a prospective study [25] of 326 incidentally detected NAFLD patients, 79% were either overweight or obese, about 50% did not know that fast foods promoted obesity, about 24% did not know harmful effects of obesity. Additionally, 38.7% of the obese patients presumed that they had a normal body weight in comparison with lean NAFLD (38.7% vs. 67.6%; p < 0.0002), and 9.5% didn’t want to lose weight. Moreover, two-thirds of NAFLD patients were neither educated by their physicians about the effects of obesity nor advised to lose weight [25]. Dietary factors like higher intake of meat, fat, and fried food render an individual more susceptible to NAFLD [26, 27]. On the other aspect, coffee has been shown to have a favorable effect on liver enzymes and fibrosis stage [28]. Patients with NAFLD tend to have lower physical activity, and regular exercise has been shown to be reducing the risk of NAFLD, with an inverse relationship between exercise intensity and severity of liver injury [29]. Early intervention with intensive lifestyle modifications in high-risk diabetics has been shown to improve cardiovascular risk and glucose tolerance [30], which is one of the major causes of morbidity and mortality in patients with NAFLD. While counseling about weight loss, diet and exercise healthcare providers should mention about NAFLD to increase awareness and re-enforce counseling, and these patients should be put under surveillance programs due to the risk of progression to cirrhosis and HCC. This information is of utmost importance suggesting healthcare providers and policymakers to work together to facilitate opportunities for education, risk factor modifications, lifestyle intervention, resource allocation, and development of educational strategies to improve recognition and management of NAFLD.
Despite the relatively large sample size, we excluded a substantial number of patients (~ 40%), which could have impacted the results. There are certain other limitations of this study. First, due to the diagnostic criteria used for NAFLD diagnosis, we might have missed some patients with normal liver enzymes and/or normal BMI leading to underestimation of patients with NAFLD awareness. We excluded subjects with viral hepatitis and excessive alcohol use but did not exclude other liver diseases, and did not account patient symptoms which could have impacted patient’s perceptions of liver disease during the survey. Secondly, these results cannot be generalized due to the exclusion of prisoners, immigrants, and other institutionalized individuals which might have different prevalence and awareness of NAFLD. Thirdly, although HSI ≥ 36 has high sensitivity and specificity to diagnose NAFLD, it is not the “gold standard” diagnostic test for NAFLD. Fourthly, despite using the strict exclusion criteria, some degree of recall bias may have been present while evaluating for alcohol consumption and medication use. Fifthly, the cross-sectional nature of NHANES does not allow investigating outcomes of individuals with low awareness of having LD and NAFLD. Sixthly, even though the survey examines a nationally representative sample, these persons are in different counties across the country with different socioeconomic and education levels which could be a reason for the fluctuations in the awareness of LD and NAFLD over the study periods. Lastly, due to the use of backward elimination method to identify covariates for multivariate regression analysis, we might have excluded some factors of clinical significance. In conclusion, awareness of having LD among subjects with suspected NAFLD has increased over the last two decades but more than 95% of these patients are still unaware of having LD. Educational programs to increase awareness of liver diseases and risk factors for NAFLD should be implemented on a large scale.
Abbreviations
- AF:
-
Advanced fibrosis
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- APRI:
-
AST to platelet ration index
- BMI:
-
Body mass index
- CDC:
-
Centers for disease control and prevention
- ESLD:
-
End-stage liver disease
- FIB-4:
-
Fibrosis-4
- GGT:
-
γ-Glutamyl transpeptidase
- HSI:
-
Hepatic steatosis index
- HDL:
-
High-density lipoprotein
- HbA1c:
-
Hemoglobin A1c
- IDF:
-
International diabetes federation
- LDL:
-
Low-density lipoprotein
- LD:
-
Liver disease
- MCQ:
-
“Medical conditions” questionnaire
- MetS:
-
Metabolic syndrome
- NHANES:
-
National health and nutrition examination survey
- NAFLD:
-
Nonalcoholic fatty liver disease
- NFS:
-
NAFLD fibrosis score
- NASH:
-
Nonalcoholic steatohepatitis
- NCHS:
-
National center for health statistics
- ULN:
-
Upper limit of normal
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore, Md).. 2016;64:73–84.
Wong RJ, Liu B, Bhuket T. Significant burden of nonalcoholic fatty liver disease with advanced fibrosis in the US: a cross-sectional analysis of 2011–2014 National Health and Nutrition Examination Survey. Aliment Pharmacol Ther. 2017;46:974–980.
Kabbany MN, Conjeevaram Selvakumar PK, Watt K, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of national health and nutrition examination survey data. Am J Gastroenterol. 2017;112:581–587.
Noureddin M, Vipani A, Bresee C, et al. NASH leading cause of liver transplant in women: updated analysis of indications for liver transplant and ethnic and gender variances. Am J Gastroenterol. 2018;113:1649–1659.
Marchesini G, Brizi M, Bianchi G, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850.
Wieland AC, Mettler P, McDermott MT, Crane LA, Cicutto LC, Bambha KM. Low awareness of nonalcoholic fatty liver disease among patients at high metabolic risk. J Clin Gastroenterol. 2015;49:e6–e10.
Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34:216–219.
Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121.
Sanna C, Rosso C, Marietti M, Bugianesi E. Nonalcoholic fatty liver disease and extra-hepatic cancers. Int J Mol Sci. 2016;17:717.
Yasui K, Sumida Y, Mori Y, et al. Nonalcoholic steatohepatitis and increased risk of chronic kidney disease. Metab Clin Exp. 2011;60:735–739.
Yan LH, Mu B, Guan Y, et al. Assessment of the relationship between nonalcoholic fatty liver disease and diabetic complications. J Diabetes Investig. 2016;7:889–894.
Leung CM, Lai LS, Wong WH, et al. Nonalcoholic fatty liver disease: an expanding problem with low levels of awareness in Hong Kong. J Gastroenterol Hepatol. 2009;24:1786–1790.
Federation ID. The IDF Consensus Worldwide Definition of the Metabolic Syndrome 2011. https://www.pitt.edu/~super1/Metabolic/IDF1.pdf. Accessed 30 Jan 2019.
Lee JH, Kim D, Kim HJ, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis: Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2010;42:503–508.
Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2013;2:1–24.
Kim D, Kim WR. Nonobese Fatty Liver Disease. Clin Gastroenterol Hepatol: Off Clin Pract J Am Gastroenterol Assoc. 2017;15:474–485.
Yilmaz Y. Is nonalcoholic fatty liver disease the hepatic expression of the metabolic syndrome? World J Hepatol. 2012;4:332–334.
Dyson JK, Anstee QM, McPherson S. Nonalcoholic fatty liver disease: a practical approach to diagnosis and staging. Frontline Gastroenterol. 2014;5:211–218.
Lee MJ, Kim EH, Bae SJ, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver. 2019;13:67–76.
Lazo M, Hernaez R, Eberhardt MS, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the third national health and nutrition examination survey, 1988–1994. Am J Epidemiol. 2013;178:38–45.
Coogan PE, Wise LA, Cozier YC, Palmer JR, Rosenberg L. Lifecourse educational status in relation to weight gain in African American women. Ethn Dis. 2012;22:198–206.
Bergqvist CJ, Skoien R, Horsfall L, Clouston AD, Jonsson JR, Powell EE. Awareness and opinions of nonalcoholic fatty liver disease by hospital specialists. Intern Med J. 2013;43:247–253.
Grattagliano I, D’Ambrosio G, Palmieri VO, et al. Improving nonalcoholic fatty liver disease management by general practitioners: a critical evaluation and impact of an educational training program. J Gastrointestin Liver Dis. 2008;17:389–394.
Polanco-Briceno S, Glass D, Stuntz M, Caze A. Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialists. BMC Res Notes. 2016;9:157.
Singh Sp MB, Misra D, Pati GK, et al. Awareness and opinion of nonalcoholic fatty liver disease (NAFLD) patients about obesity and its consequences. J Hepatol. 2014;60:S352.
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Long term nutritional intake and the risk for nonalcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47:711–717.
Singh SP, Singh A, Misra D, et al. Risk factors associated with nonalcoholic fatty liver disease in Indians: a case-control study. J Clin Exp Hepatol. 2015;5:295–302.
Modi AA, Feld JJ, Park Y, et al. Increased caffeine consumption is associated with reduced hepatic fibrosis. Hepatology (Baltimore, Md).. 2010;51:201–209.
Kistler KD, Brunt EM, Clark JM, et al. Physical activity recommendations, exercise intensity, and histological severity of nonalcoholic fatty liver disease. Am J Gastroenterol. 2011;106:460–468. quiz 469.
Goldberg RB, Temprosa M, Haffner S, et al. Effect of progression from impaired glucose tolerance to diabetes on cardiovascular risk factors and its amelioration by lifestyle and metformin intervention: the Diabetes Prevention Program randomized trial by the Diabetes Prevention Program Research Group. Diabetes Care. 2009;32:726–732.
Author information
Authors and Affiliations
Contributions
AS, ASD, MG, and NA helped in study concept and design; AS contributed to acquisition of data; all authors helped in analysis and interpretation of data, drafting of the manuscript and critical revision of the manuscript for important intellectual content, and administrative, technical, or material support; RL, AS, and NA contributed to statistical analysis; ASD, SS, AK, AK, MN, WC, AM, and NA contributed to study supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, A., Dhaliwal, A.S., Singh, S. et al. Awareness of Nonalcoholic Fatty Liver Disease Is Increasing but Remains Very Low in a Representative US Cohort. Dig Dis Sci 65, 978–986 (2020). https://doi.org/10.1007/s10620-019-05700-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05700-9