Abstract
Aims
Non-cirrhotic portal fibrosis (NCPF) is a rare cause of pediatric portal hypertension. There is abundant literature in adults but paucity of data in children. We aimed to evaluate and compare the endoscopic and long-term outcomes of children with NCPF.
Methods
Consecutive children (≤ 18 years) diagnosed with NCPF evaluated for clinical and endoscopic profile and outcome. The cohort underwent 3 weekly endoscopic sessions until esophageal variceal eradication followed by 6–12 monthly endoscopic surveillance. Non-bleeders and bleeders were compared for endoscopic outcome.
Results
Forty-five NCPF children with median age of 14.5 (6–18) years and symptom duration 12 (1–120) months presented with spleen-related issues (78%), esophageal varices (96%), primary gastric varices (56%), and portal hypertensive gastropathy (89%). Thirty-three patients undergoing endotherapy (secondary prophylaxis n = 22, primary prophylaxis n = 11) showed primary eradication of varices after 5 (2–12) sessions. 36% showed recurrence of esophageal varices in 11 (6–42) months and secondary gastric varices developed in 12%. Overall 87% patients required endoscopic intervention at onset or follow-up. Poor outcome was observed in ten patients (n = 9 bleeders). Three children died of variceal bleeding before endoscopic eradication of esophageal varices. Three developed decompensation after a median follow-up of 48 (3–120) months and referred for liver transplantation. Four patients required surgery for portal hypertension.
Conclusions
Overall, endoscopic outcome of NCPF is favorable. One-third patients have recurrence of esophageal varices. Small proportion of bleeders have poor outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-cirrhotic portal hypertension (NCPH) is characterized by a presinusoidal portal hypertension in the absence of cirrhosis of the liver or hepatic venous outflow obstruction. NCPH includes non-cirrhotic portal fibrosis (NCPF) and extrahepatic portal vein obstruction (EHPVO). Essentially, the patency of the portal vein clinically differentiates the two conditions [1]. Both disorders are more commonly seen in lower socioeconomic groups of developing countries. Since liver functions are usually preserved, these diseases have potentially favorable outcome in terms [2,3,4,5,6]. The consequences of portal hypertension require attention, most importantly variceal bleeding. Traditionally, NCPF is viewed as a disease of adults. While there is abundant pediatric literature in natural history and endoscopic outcome in EHPVO, there is scanty information on NCPF in children. We aimed to (1) analyze the overall presentation and outcome of children with NCPF and (2) compare the endoscopic profile of bleeders versus non-bleeders.
Methods
We studied children ≤ 18 years diagnosed as NCPF (January 2007–December 2017) and evaluated in our department. The clinical, laboratory, endoscopic, and follow-up data were retrieved from electronic records.
Inclusion criteria and definitions
The diagnosis of NCPF was based on all of the following criteria [7, 8]: (a) presence of unequivocal signs of portal hypertension (splenomegaly, dilated portal vein on imaging ± gastroesophageal varices on endoscopy); (b) liver biopsy showing absence of cirrhosis, steatosis, or any other features of chronic liver diseases ± presence of characteristic histological features of NCPF; (c) absence of thrombosis of the hepatic veins and portal vein on imaging; and (d) exclusion of known common sinusoidal causes of chronic liver disease (Wilson’s disease, autoimmune liver disease, chronic hepatitis B and C). Duration of disease was defined as first episode of variceal bleeding (bleeders) or first detection of splenomegaly (non-bleeders) to diagnosis of NCPF. Spleen-related issues included hypersplenism, splenic infarction, pain or dragging sensation, fullness in the left hypochondrium, or adjoining areas. Hypersplenism was defined as thrombocytopenia (platelet count < 50,000/mm3) and/or leucopenia (WBC < 4000/mm3) with splenomegaly [9]. Deranged synthetic function was defined as INR > 1.3 and/or serum albumin < 3.5 g/dL [10]. Liver biopsy was performed to differentiate NCPF from cirrhosis by either percutaneous or trans-jugular route (international normalized ratio > 1.5 or platelets count < 60,000/mm3 [11, 12]. Histopathology consistent with NCPF considered in our study was preserved lobular architecture with one or more of the following: portal phlebosclerosis, ectasia of intrahepatic portal vein, sinusoidal dilatation, portal and periportal fibrosis, and nodular regenerative hyperplasia.
Endoscopic management protocol and endoscopic definitions
All patients were subjected to upper gastrointestinal endoscopy for the assessment of varices. Endoscopic procedures were performed or supervised by pediatric endoscopy consultants of > 15 year experience. Endoscopic grading for classification of varices used was Paquet (esophageal varix), Sarin (gastric varix location), and Taor (portal hypertensive gastropathy) [13,14,15,16]. Grade II with red color signs (RCS), grade III and grade IV esophageal varices were intervened by primary prophylaxis (endoscopic band ligation) in non-bleeders and secondary prophylaxis (endoscopic band ligation followed by 1% polidocanol sclerotherapy) in bleeders. All patients underwent 3 weekly endoscopic sessions until esophageal variceal eradication followed by 6–12 monthly endoscopic surveillance. Esophageal varices grade I or II without red color signs in bleeders and non-bleeders were followed up 6–12 monthly and intervened if they enlarged (≥ grade II with red color signs). Primary eradication: eradication of naïve esophageal varix until no varix is persisting or tag ± neovascularization formation. Secondary eradication: eradication of recurrent esophageal varices (≥ grade II with red color signs) until no varix is persisting or tag formation. Recurrence: appearance of ≥ grade I esophageal varices after eradication. Interval bleeding: variceal bleeding between two sessions of endoscopy before eradication. Gastric varices were labeled as primary when present at the time of initial endoscopic examination and secondary if they developed after endoscopic eradication of esophageal varices [14]. Gastric variceal bleeders were managed by N-butyl, 2-cyanoacrylate glue injections (0.5–2 mL) into the bleeding varices. Repeat glue injections were decided as per endoscopic assessment at follow-up. Non-selective beta-blocker (propranolol 1–2 mg/kg/day, maximum 80 mg) was offered in those patients with recurrent esophageal variceal bleeding and large gastric varices (bled or unbled) until shunt surgery.
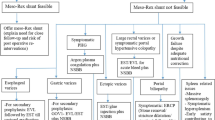
Surgery
Porto-systemic shunt surgery or splenectomy with devascularisation was considered if patient had uncontrolled variceal bleeding or discomforting spleen-related issues. Feasibility of surgical porto-systemic shunt was assessed by computed tomography (CT) venography of portal venous system.
Statistical analysis
Variables were expressed as median (range). Categorical variables were compared using the Chi-square test or Fisher’s exact test. Continuous variables were compared using a Student’s t test or Mann–Whitney U tests depending on the distribution of variables. Kaplan–Meir curve was used to plot recurrence of varices among bleeders and non-bleeders. Differences were considered significant if the p value was < 0.05. Statistical analysis was done using SPSS software for windows version 23.0 (SPSS, Chicago, USA).
Results
Clinical presentation and laboratory features
Out of the total 1370 referral cases of portal hypertension, 45 (3.3%) were diagnosed as NCPF (female gender, n = 24). Overall age at diagnosis and duration of symptoms was 14.5 (6–18) years and 12 (1–120) months, respectively. Majority (37, 82%) presented in second decade. Overall, spleen-related issues (pain, dragging sensation, and lump left hypochondrium) were present in 35 (78%). Of the 39 who had hypersplenism, 12 (30%) were symptomatic for skin bleeds, epistaxis, menorrhagia, and anemia. Almost half of our patients (n = 22) presented with variceal bleed. Post-bleed ascites was observed in 9 (20%). Clinico-laboratory and endoscopic parameters are given in Table 1. Elevated AST and ALT levels (> 40 U/L) were present in 11 (40%) and 14 (31%) of patients, respectively. On ultrasonography (USG), liver echotexture was nodular in 14 (31%). Doppler USG showed median diameter of portal vein and splenic vein 12.5 (6.5–15.5) mm and 8.8 (4.5–13.8) mm, respectively. Histopathological features were reported portal fibrosis (26, 58%), sinusoidal dilatation (25, 56%), nodular regenerative hyperplasia (5, 11%) intrahepatic portal venous ectasia (20, 44%), obliterative portal venopathy (12, 27%), and portal phlebosclerosis (3, 7%).
Initial endoscopic details
Upper gastrointestinal endoscopy (n = 45; bleeders, n = 22; non-bleeders, n = 23) showed the presence of esophageal varices in 43 (96%), primary gastric varices in 25 (56%), and portal hypertensive gastropathy in 40 (89%) (mild, n = 30; severe, n = 10) at initial evaluation. Among those with variceal bleeding, 19 had bleeding from esophageal varices (grade IV, n = 10; grade III, n = 7; grade II with RCS, n = 2) and three from gastric varices (IGV1, n = 2; GOV2, n = 1). Of non-bleeders (n = 23), 11 patients required primary prophylactic endotherapy for esophageal varices (grade IV, n = 7; grade III, n = 3; grade II with RCS, n = 1). Table 1 shows comparison of bleeders and non-bleeders. There were no endoscopy-related complications noted during endotherapy. Thirty-three patients undergoing endotherapy (secondary prophylaxis n = 22, primary prophylaxis n = 11) showed primary eradication of varices after 5 (2–12) sessions (Table 2).
Endoscopic follow-up and outcome
Of the 33 patients who required endotherapy, 12 (36%) showed recurrence of esophageal varices after 11 (3–42) months and developed secondary gastric varices in 4 (12%) (GOV2, n = 1; IGV1, n = 3) after 14 (9–38) months of the first eradication of esophageal varices. Recurrence of esophageal varices among bleeders and non-bleeders is shown in Kaplan–Meir curve (Fig. 1). All four patients with secondary (large) gastric varices were started on beta-blocker therapy. In this group, only one patient (IGV1) bled after 9 months of first esophageal variceal eradication and the rest three did not bleed from the gastric varices until last follow-up. Twelve non-bleeder patients with unintervened small esophageal varices at presentation were systematically followed up with 6–12 monthly endoscopic surveillance. Among them, 6 (50%) developed large esophageal varices, required endotherapy after median follow-up of 13 (8–39) months, of which two presented with acute esophageal variceal bleeding after 9 and 12 months. In this subset of 12 patients, new gastric varices and new PHG evolved in four and two patients, respectively. Overall, 87% patients required endoscopic intervention at onset or follow-up. Three of 45 NCPF patients were lost to follow-up. The median follow-up of the remaining 42 patients was 48 (3–120) months. Poor outcome was seen in ten patients (n = 9 bleeders). Three patients died before reaching endoscopic services due to interval bleeding from large varices. Three bleeders developed advanced liver disease [n = 2, recurrent ascites not responding to salt restriction and diuretics and requiring intermittent large volume paracentesis after 4 and 5 years of diagnosis; n = 1, hepato-pulmonary syndrome (HPS) after 7 years of diagnosis]. The above three patients were referred for liver transplantation. Four patients (bleeders, n = 3; non-bleeder, n = 1) required surgery (n = 3, elective central end-to-side spleno-renal shunt procedure with splenectomy for symptomatic hypersplenism; n = 1, emergency splenectomy with devascularization for gastric variceal bleeding). No overt hepatic encephalopathy was reported in the shunt surgery patients and was reported to have gainful living until last follow-up. The rest 32 (76%) out of 42 patients continue to be on regular endoscopic surveillance program and are asymptomatic until their last follow-up. The natural history of NCPF in our study is compared with other large studies (pediatric and adult) in Table 3.
Discussion
Non-cirrhotic portal fibrosis accounts for 15–30% of portal hypertension in Asian adults [4, 5, 17, 18]. In children, it accounts for 3.3% of all pediatric portal hypertension as seen in our study, similar to 4.6% reported by Sood et al. [19]. Previously, it was thought that NCPF occurs in the third-to-fourth decade of life based on adult literature [5, 6]. It is now evident that it is fairly common in pediatric population as evidenced by various case series [19,20,21,22]. In the pediatric age group, the disease remains largely undiagnosed due to lack of awareness, most often mistaken for cryptogenic cirrhosis. In contrast to the idiopathic etiology in Asian adults and children, interestingly Franchi-Abella et al. reported 48 patients of obliterative portal venopathy from different etiological subgroups (familial, syndromic, post chemotherapy, others) [22]. Except for the age of symptom onset and presentation, the overall natural history and outcome of NCPF in adults are not different in children from our series (Table 3). Complications related to portal hypertension dominate the signs and symptoms present in patients with NCPF. Frequency of variceal bleeding (15.7–55%) is lesser in children as compared to adults (70–95%) with NCPF possibly due to longer duration of illness in adults [19, 20]. In the present study, half of our cohort presented with variceal bleeding. In contrast, two other pediatric series showed left upper quadrant lump (splenomegaly) as the main presenting symptom [19, 21]. The splenomegaly sizes were comparable to those reported by Sood et al. [19]. In the present study, spleen-related issues were in 78% with near normal liver functions as seen in other adult and pediatric studies too [21, 23].
Unlike other pediatric series, our study has provided a comprehensive analysis on the endoscopic outcome, which is the mainstay of therapy in NCPF. In the present cohort, the presence of esophageal varices, primary gastric varices, and portal hypertensive gastropathy were in 96%, 56%, and 89%, respectively. In terms of clinico-laboratory profile and endoscopic outcomes of esophageal varices, NCPF bleeders were no different from NCPF non-bleeders. With our stringent 3 weekly endoscopy protocol, esophageal varices requiring endotherapy (n = 33) could achieve primary eradication in 5 (2–12) sessions. Recurrence of esophageal varices occurred in one-third of patients indicating persistence of high portal pressure. When this group underwent second phase of eradication, a shorter number of sessions were needed. With respect to gastric varices, a large proportion (60%) of GOV1 disappeared and the rest persisted after endotherapy. Endoscopic band ligation and a small volume of sclerosants for esophageal varices are ineffective to obliterate gastroesophageal varices. 12% of the cohort also developed secondary gastric varices (GOV2 and IGV1) in splenic vein drainage territory. Most of the PHG was mild in severity at onset and resolved in one-third of the cohort possibly because of overall control of portal hypertension. The presence of PHG at the onset was significantly higher in bleeders as compared to non-bleeders possibly due to higher portal pressures. It would be unlikely that beta-blockers contributed to the significant difference in the resolution of portal hypertensive gastropathy between bleeders and non-bleeders. Both groups have similar recurrences of esophageal and large gastric varices requiring beta-blockers. We postulate that with time, the severity of portal hypertension continued to rise, and hence, half of the unintervened cohort developed large esophageal varices at follow-up. Hence, in totality, 87% of our cohort required endoscopic intervention at onset or follow-up. We understand that it is not possible to ascertain the exact time of onset of the disease. Duration of disease as defined in our study could be well underestimated. The question that needs to be analysed in a future prospective cohort studies is whether “true” duration of disease is a significant factor for deciding the timing of variceal bleeding.
The NCPF endoscopic outcome works quite similar to the EHPVO model [24]. In EHPVO, our group in the past have shown esophageal varices, primary gastric varices and portal hypertensive gastropathy in 70%, 61%, and 12%, respectively. After sclerotherapy, recurrence of esophageal varices (40%), appearance of secondary gastric varices (28%) and increase in portal hypertensive gastropathy (from 12 to 41%) are encountered [25]. Endoscopic findings in adult NCPF have been well documented. In adults with NCPF, esophageal varices have been reported in 85–95%, which is similar to children. Gastric varices are more common in NCPF adults (31–43%) which is higher than pediatric NCPF [19]. In 72 adult patients with NCPF, esopahgeal variceal obliteration was achieved in 90% in a mean of 5.7 sessions of endoscopic sclerotherapy and over a follow-up period of 21.4 ± 20.4 months. Rebleeding recurrent esopahgeal varices are seen in 9.2% [26].
Data on long-term follow-up are lacking specially in pediatric literature. Normally, NCPF have preserved liver functions as reiterated in our series too [23, 27]. Ascites and hypoalbuminemia are rare. Our study showed transient ascites and hypoalbuminemia in 20% and 11% patients, respectively, after variceal bleeding. A small subgroup (10%) of NCPF with deranged liver function tests has, however, been recognized [23]. A subset is known to behave similar to cirrhotics or end-stage liver disease requiring liver transplantation [4, 5]. In our study, three patients were lost to follow-up. Poor outcomes (death, decompensation, and requirement of surgery) were seen in 10 (24%) out of 42 remaining patients. The overall survival of NCPF is relatively favorable. A Dutch study reported an overall and native liver survival of 78% and 72%, respectively, at 5 years [28]. Similarly, the Spanish cohort of adults reported 86% of native liver survival at 5 years [29].
The surgical option for NCPF is a matter of considerable debate with paucity of literature in adults and children. In comparison with the EHPVO model, where Meso–Rex shunt is favored, NCPF patients with predominant spleen-related issues would require a surgery that ameliorates the same. Non-selective porto-systemic shunts such as central end-to-side spleno-renal shunt with splenectomy would be a favorable compromise, but it is fraught with limitations. In a study of 41 adults with NCPF who underwent prophylactic lienorenal shunt, long-term complications observed were hepatic encephalopathy, glomerulonephritis, pulmonary arterio-venous fistulae and ascites [30]. In all our patients who underwent surgery with a modest follow-up period, no long-term morbidity was noted. However, the effects of the surgery after transition into adulthood would remain underestimated.
The limitations of our study are its retrospective design. Our endoscopic grading system of varices and portal hypertensive gastropathy may have had interobserver variation. We did not perform hepatic venous pressure gradient and correlate the endoscopic features or outcome. We also did not objectively assess for quality of life or other portal hypertensive complications (biliopathy and colopathy) of NCPF, as they were asymptomatic for the same.
Conclusions
Endoscopic variceal intervention is required in the natural history of 87% of pediatric NCPF. Bleeders and non-bleeders have near similar outcome and mandate the need for vigilant endoscopic surveillance. Though there is progression in portal hypertension in unbled patients, majority of NCPF have preserved liver functions. Small proportion of bleeders have poor outcome and need for surgery.
Abbreviations
- NCPF:
-
Non-cirrhotic portal hypertension
- EHPVO:
-
Extrahepatic portal vein obstruction
- INR:
-
International normalized ratio
- PHG:
-
Portal hypertensive gastropathy
- RCS:
-
Red color signs
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- LT:
-
Liver transplantation
References
Khanna R, Sarin SK. Non-cirrhotic portal hypertension—diagnosis and management. J Hepatol. 2014;60:421–41.
Nayak NC, Ramalingaswami B. Obliterative portal venopathy of the liver. Arch Pathol Med. 1969;87:359–69.
Sarin SK, Aggarwal SR. Idiopathic portal hypertension. Digestion. 1998;59:420–3.
Sarin SK, Kumar A. Noncirrhotic portal hypertension. Clin Liver Dis. 2006;10:627–51.
Dhiman RK, Chawla Y, Vasishta RK, et al. Non-cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol. 2002;17:6–16.
Pande C, Kumar A, Sarin SK. Non-cirrhotic portal fibrosis: a clinical profile of 366 patients. Am J Gastroenterol. 2006;101:S191.
Schouten JNL, Garcia-Pagan JC, Valla DC, Janssen HLA. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011;54:1071–81.
Sarin SK, Kumar A, Chawla YK, et al. Noncirrhotic portal fibrosis idiopathic portal hypertension: APASL recommendations for diagnosis and treatment. Hepatol Int. 2007;1:398–413.
Bajaj JS, Bhattacharjee J, Sarin SK. Coagulation profile and platelet function in patients with extrahepatic portal vein obstruction and noncirrhotic portal fibrosis. J Gastroenterol Hepatol. 2001;16:641–6.
Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365:147–56.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy. Hepatology. 2009;49:1017–44.
McAfee JH, Keeffe EB, Lee RG, Rosch J. Transjugular liver biopsy. Hepatology. 1992;15:726–32.
Paquet KJ. Prophylactic endoscopic sclerosing treatment of the esophageal wall in varices—a prospective controlled randomized trial. Endoscopy. 1982;14:4–5.
Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9.
Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc. 1990;36:276–80.
Taor RE, Fox B, Ware J, Johnson AG. Gastritis: gastroscopic and microscopic. Endoscopy. 1975;7:209–15.
Hillaire S, Bonte E, Denninger MH, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patients. Gut. 2002;51(2):275–80.
Datta DV, Bhagwat AG. Idiopathic portal hypertension—A review. Bull PGI. 1981;15:173–92.
Sood V, Lal BB, Khanna R, Rawat D, Bihari C, Alam S. Non-cirrhotic portal fibrosis in pediatric population. J Pediatr Gastroenterol Nutr. 2017;64:748–53.
Yachha SK. Portal hypertension in children: an Indian perspective. J Gastroenterol Hepatol. 2002;17:S228–31.
Poddar U, Thapa BR, Puri P, et al. Non-cirrhotic portal fibrosis in children. Indian J Gastroenterol. 2000;19:12–3.
Franchi-Abella S, Fabre M, Mselati E, et al. Obliterative portal venopathy: a study of 48 children. J Pediatr. 2014;165(190–3):e2.
Tandon BN, Nundy S, Nayak NC. Non-cirrhotic portal hypertension in Northern India: clinical features and liver function tests. In: Okuda K, Omata M, editors. Idiopathic portal hypertension. Tokyo: University of Tokyo Press; 1983. p. 377–86.
Koshy A. Relationship between NCPF and EHO. In: Okuda K, Omata M, editors. idiopathic portal hypertension. Tokyo: University of Tokyo Press; 1983. p. 13–8.
Itha S, Yachha SK. Endoscopic outcome beyond esophageal variceal eradication in children with extrahepatic portal venous obstruction. J Pediatr Gastroenterol Nutr. 2006;42:196–200.
Chawla YK, Dilawari JB, Dhiman RK, Goenka MK, Bhasin DK, Kochhar R. Sclerotherapy in noncirrhotic portal fibrosis. Dig Dis Sci. 1997;42:1449–53.
Sarin SK, Sachdev G, Nanda R. Follow-up of patients after variceal eradication. A comparison of patients with cirrhosis, non-cirrhotic portal fibrosis and extrahepatic obstruction. Ann Surg. 1986;202:78–82.
Siramolpiwat S, Seijo S, Miquel R, et al. Idiopathic portal hypertension: natural history and long-term outcome. Hepatology. 2014;59:2276–85.
Schouten JNL, Nevens F, Hansen B, et al. Idiopathic noncirrhotic portal hypertension is associated with poor survival: results of a long-term cohort study. Aliment Pharmacol Ther. 2012;35:1424–33.
Pal S, Radhakrishna P, Sahni P, Pande GK, Nundy S, Chattopadhyay TK. Prophylactic surgery in non-cirrhotic portal fibrosis: is it worthwhile? Indian J Gastroenterol. 2005;24:239–42.
Acknowledgements
We thank Dr Anup Kumar, PhD, Assistant Professor, Department of Biostatistics and Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow for verifying the statistical analysis.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Durga Prasad, Moinak Sen Sarma, Surender Kumar Yachha, Anshu Srivastava, and Ujjal Poddar declare that they have no conflicts of interest.
Ethical approval
Ethical clearance and waiver of consent was obtained from Institutional Ethics Committee (IEC code 2017-236-IP-EXP).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prasad, D., Sen Sarma, M., Yachha, S.K. et al. Pediatric non-cirrhotic portal fibrosis: role of endoscopic management in determining long-term outcome. Hepatol Int 14, 281–287 (2020). https://doi.org/10.1007/s12072-019-09979-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09979-8