Abstract
Aim of this paper is to present a literature review among bone conduction hearing aids particularly focusing on their surgical and functional outcomes.
Methods: A detailed review of the English literature to date on bone conduction hearing aids and outcomes have been performed using Pubmed, Scopus, Google Scholar and Medline databases. The literature review was performed using the guidelines proposed by the study “Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)” for scoping review.
Results: a total of 30 full text articles were included in this review, collecting 660 patients. All the studies examined reported an improvement, in terms of PTA and speech audiometry, following the implantation of bone-conduction devices. The subjective outcome of patients was also evaluated, which was positive in terms of improved quality of life perception.
Conclusions: Bone conduction devices represent an excellent rehabilitative solution allowing adequate functional gain. Nowadays, the variability of devices consents an appropriate customization of the surgical indication based on the functional and general needs of the patient, to achieve a tailored approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization estimates that hearing loss impacts more than 1.5 billion people worldwide, meaning 20% of the world’s population [1]. Several hearing rehabilitative options are now available for individuals with conductive hear impairment. Bone-conduction hearing aids are used to treat these conditions bypassing the affected conductive mechanisms and by stimulating the cochlea directly through the skull bone [2]. In general, bone-anchored hearing aids are indicated for patients with uni- or bilateral conductive (CHL) and mixed hearing loss (MHL) who cannot be rehabilitated with conventional hearing aids or surgery and, more lately, for the treatment of unilateral sensorineural deafness to advantage the contralateral routing of sound signals (CROS) [2]. Other indications are malformations of the outer ear and chronic middle ear infections that prevent the use of prostheses.
There are several types of bone conduction devices that can be categorized into:
-
cutaneous, in which the vibration is transmitted through the skin. This is the case of passive transcutaneous devices such as Sophono [Medtronic, Minneapolis, USA] and BAHA® Attract [Bone Anchored Hearing Aid, Cochlear Co., Australia],
-
direct, in which vibration is transmitted to the bone directly. These are divided into (i) percutaneous (Ponto [Oticon Medical AB, Askim, Sweden] and BAHA® Connect) and (ii) active transcutaneous (Bonebridge® [MED-EL, Innsbruck, Austria] and Cochlear Osia OSI200 implant [Cochlear Co., Australia] [3].
Percutaneous systems include an osteo-integrated titanium implant with a skin-penetrating abutment to which a bone-conducting sound processor can be coupled. These systems have excellent functional results but require meticulous care of the skin located around the abutment [4]. Although the percutaneous system provides good auditory and clinical results, it has some disadvantages related to recurrent soft tissue infections around the abutment and potential cosmetic problems linked to the percutaneous abutment [4].
In recent years, new transcutaneous active bone conduction implants have been introduced: Bonebridge and Osia are examples of this technology [4]. In addition to these numerous proposals, ADHEAR [MED-EL, Innsbruck, Austria] was introduced in 2018. ADHEAR is an adhesive bone conduction hearing aid introduced to overcome the skin pressure issues of transcutaneous implants and the skin complications associated to percutaneous implants [5].
Since the introduction of bone conduction hearing devices, numerous case series have been published, while a comprehensive review of the relevant literature is still lacking. Aim of this study is to present a literature review on currently available bone conduction hearing aids, including their surgical and functional outcomes.
Materials and Methods
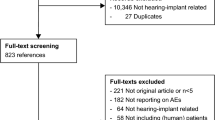
A detailed review of the English literature to date on bone conduction hearing aids and its outcomes was performed using Pubmed, Scopus, Google Scholar and Medline databases. The literature search was performed using the guidelines proposed by the study “Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)” for scoping review. Figure 1 [6, 7].
The use of the keywords “Osia”, “Ponto”, “Bonebridge”, “BAHA”, “ADHEAR”, ”sophono”, “active bone conduction implant”, “bone conduction hearing device” and “bone-anchored hearing aid” identified 477 articles on this topic.
Inclusion criteria were: (i) studies published in the last 5 years (from 2018 to 2023), (ii) studies reporting patients in which at least one device was placed and correctly activated, (iii) studies with results presented in homogeneous groups and (iv) studies with objective and quantifiable results in terms of functional hearing outcome (tonal and/or speech audiometry).
Data on number of patients, number of devices implanted, age, gender, cause of deafness, pre and post audiometry, pre and post speech audiometry, subjective evaluation of patients, and complications of surgery or related to the device were collected and then compared.
Exclusion criteria were: articles that only described the surgical technique without reporting audiological or subjective results; case reports.
At the end of the full-text revision, 30 articles were included in this review, giving a total of 660 patients [2,3,4,5, 8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34].
Results
Percutaneous Devices
Ponto
Two selected articles matched the inclusion criteria and report the results among 57 patients (see also Table 1). The average gain in pure tone average (PTA) achieved using the device was 34.56 dB; gain on speech recognition was also evaluated and showed objective improvements. Skarzynski et al. also proposed a subjective assessment for patients that showed good subjective results on questionnaires [32]. Complications were as expected for percutaneous devices, i.e., infection and skin complications reported by Amaral et al. as affecting 45% of patients [21].
Baha Connect
No articles on Baha Connect were found that met the aforementioned inclusion criteria.
Passive Transcutaneous Devices
Sophono
No articles on Sophono were found that met the aforementioned inclusion criteria.
Baha Attract
Four articles matched the inclusion criteria and were therefore included, for a total of 118 patients. These results are summarized in Table 2. The average gain of PTA obtained by the subjects using Baha Attract was 28.98 dB, and a good subjective tolerance has been reported in all items examined although with different questionnaires.
Only 1 case, among those reported, required implant removal due to persistent skin complications. Other cases reported minor complications such as paresthesias, seromas, hematomas, discomfort, and skin infections were temporary and did not require surgical revision.
Active Transcutaneous
Osia
The thirteen selected articles about the Osia system and its outcomes are summarized in Table 3.
Data were collected on a total of 237 implants, since 17 patients were implanted bilaterally. Of the 220 patients reported within the selected papers, 33 were under 18 years of age.
Etiologies of hearing impairment were: 55 chronic otitis media (COM), 42 aural atresia with or without microtia or canal stenosis, 43 SSD, 5 ossicular anomalies, 2 previous tumors and 2 traumas. In the remaining cases the cause of deafness was not specified.
An improvement of PTA was reported by all studies, in particular the average gain in PTA after Osia activation was 37.2 dB. Speech audiometry threshold values are not numerically comparable, despite being objectively quantifiable in most of the identified papers, as in some cases are expressed as Speech Recognition Threshold (SRT) and in other in terms of Word Recognition Score (WRS) at different dB levels (see also Tab II). In particular, Willemborg et al. found an average increase at the WRS at 65 dB from 3 to 95%, while Briggs et al. observed an increase in the WRS at 50 dB of 62.3% [8, 11]. The SRT recorded by You et al. underwent a change from 63.2 dB to 22 dB, similarly Lau et al. also report an improvement in SRT from 38.2. dB to 22.7 dB [9, 12].
In all cases included in the present review, patients were given questionnaires to assess subjective improvements in quality of life. There were several questionnaires selected for this purpose, the main ones being the Abbreviated Profile of Hearing Aid Benefit (APHAB) [35], Glasgow Benefit Inventory (GBI) [36], and Speech, Spatial and Qualities of Hearing Scale (SSQ) [37]. Scores obtained from questionnaires were reported to be improved after the application of the OSIA system; however, we could not retrieve numerical values since not always expressed, and this precluded the calculation of average scores pre and post device placement. All subjective data collections were found to be positive with an objectively measurable improvement in quality of life in all studies.
Reported surgical complications were 7 surgical site infections, 3 of which required explantation and were therefore excluded from the analysis of functional outcomes [8, 17].
Other reported minor complications were overly weak or strong magnet force causing low processor retention or painful discomfort, which were both overcome by adjusting the magnet strength [9, 16].
Bonebridge
7 papers met the inclusion criteria and were therefore selected for a total of 214 patients. Of these, 5 were bilaterally implanted (see also Table 4), and 6 were younger than 5 years of age.
The average gain in PTA was 40.34 dB; concerning the speech audiometry, although WRS was used in almost all cases, the results, even if good, are difficult to compare objectively since they were performed at different sound intensities. The work proposed by Bae et al., examining patients younger than 5 years, reported one major complication of increased endocranial pressure with left sixth cranial nerve palsy, resolved after explantation [22]. Only 5 other devices were explanted out of the entire population considered: 2 due to infection and skin dehiscence, 2 due to poor benefit, and 1 due to device failure.
Adhesive Devices
ADHEAR
Four articles have been selected according to the review criteria, for a total of 51 patients using the ADHEAR device (see also Table 5). The PTA showed an average increase of 17.54 dB with discrete gains on speech audiometry. No skin complications or adverse reactions have been reported.
Discussion
Hearing loss affects more than 1.5 billion people worldwide with major social consequences affecting about 20% of the population [1]. Bone conduction hearing aids can be used to treat some of these conditions by skipping the middle and outer ears and stimulating the cochlea directly. In general, bone-conduction devices are indicated for patients with conductive and mixed hearing loss who cannot be rehabilitated with conventional hearing aids (e.g., due to chronic otitis or malformations of the outer ear that make it impossible to use a prosthesis) or with surgery. More recently, an indication has also been proposed for the treatment of SSD for the benefit of contralateral routing of signal (CROS) [2].
Bone-conduction devices that can be classified according to the mode of conduction into:
-
cutaneous, in which the vibration is transmitted through the skin (this is the case with passive transcutaneous devices such as Sophono and BAHA® Attract);
-
direct, in which the vibration is transmitted directly to the bone. These are divided into (i) percutaneous (Ponto and BAHA® Connect and (ii) active transcutaneous (Bonebridge® and Cochlear Osia OSI200 implant) [3].
Percutaneous devices give excellent functional results and have been used for many years; however, they require meticulous care of the skin around the abutment, which is particularly susceptible to infection and inflammatory reactions. Ponto was introduced in 2009 and belongs to the category of percutaneous devices. Although the aesthetic problems related to the permanent percutaneous abutment and possible skin complications are well known, Ponto is a solution that can be effectively applied in cases of severe-to-profound conductive or mixed hearing loss that could poorly benefit from other bone-conduction devices [32]. In addition, in 2011 Hultcrantz developed the Minimally Invasive Ponto Surgery (MIPS) technique, which was later compared by Amaral et al. to the classical technique proving to be an effective and fast procedure for device application under local anesthesia [21, 38]. Baha Connect also belongs to the category of percutaneous devices and similarly achieved great success especially at its debut since its applicability to profound conductive or mixed hearing loss. However, according to the most recent literature examined, the interest among this device has decreased within the recent years.
Transcutaneous devices have been introduced aiming to overcome the problems of percutaneous devices and particularly those related to the skin. Among passive transcutaneous devices, Sophono was the first to be introduced, in 2006, and after an initial interest with promising results, the attention around this means has decreased within the recent years [39]. Baha attract was presented in Europe in 2013 and consists of a passive subcutaneous implant that is magnetically attached to an external processor (the magnet is available with six different strengths) [30]. Reported functional results are good although slightly inferior to the performance of percutaneous devices with the benefit of decreased skin complications. Despite the resolution of the problems related to the percutaneous abutment, Nevoux et al. still suggested caution and careful monitoring of the skin at the implantation site, as this can be subjected to skin pressure with discomfort and possible complications that should not be ignored [30]. Although skin complications are rare, when they occur, can lead to wound dehiscence or implant extrusion. For this reason, Chen et al. suggested a possible ultrasound verification in cases of doubtful skin flap distress at clinical monitoring [24].
The active bone conduction transcutaneous devices available are Osia and Bonebridge. The Osia system is a new generation of bone-anchored transcutaneous active prosthesis. It consists of an implant (OSI200) connected via a piezoelectric actuator to an osseointegrated screw (BI300 implant) placed to the mastoid. The sound signal is transmitted by an external processor that is connected to the implant electromagnetically [9]. Osia became available worldwide in 2020 and has been authorized in Europe in 2021 [10, 15, 17]. Speech audiometry shows very good results in those using this system, although these are hardly comparable among the selected studies, since not performed using the same means. Several authors have also reported an improvement within high-frequency perception, in those rehabilitated with this device, superior to that obtained with other bone-anchored active prostheses [10, 19]. In particular, Goycoolea et al. compared the Osia system with the percutaneous Baha implant using a Baha 5 Power processor; they observed significantly better performance with the Osia and this result was confirmed by Gawecki et al. [14, 16] Gawecki et al. also presented quality-of-life outcomes of patients who received the Osia system and those who used the Baha Attract; they reported greater improvements in the Osia group at the cost of more invasive and time-consuming surgery [16]. Furthermore, You et al. described that a series of patients who switched from Baha Attract or Baha Softband to Osia: all reported subjective improvement of the quality of sound perception [9]. Among all cases included in this review, 7 surgical site infections were reported as complications that were successfully treated by antibiotic therapy. Three of these required a device explant. One wound dehiscence without extrusion was also reported. Authors recommended for revision surgery to place the device in a site different from the initial surgery [8, 10]. Other minor complications reported were pain related to excessive magnet power that was easily adjusted with good outcome. Care should be taken with the retaining magnet strength to avoid either pain (too strong) or poor retention (too weak) [2]. Finally, Rauch et al. point out that the Osia system creates artifacts on MRI and that removal of the magnet for 3 Tesla MRI is necessary: patients should be informed about this issue at pre-surgical counseling [15].
Among the transcutaneous active devices, Bonebridge is the device available the longest, since it has been introduced in 2012 [25]. This has allowed longer follow-up, such as the 6-year study by Brkic et al., and further in-depth studies [23]. In particular, Kim et al. demonstrated a statistically significant decrease in tinnitus with the use of Bonebridge while Cywka et al. demonstrated safety and efficacy in the paediatric population [25, 29]. In addition, Bae et al. proposed the application of the device under 5 years of age, therefore allowing an earlier rehabilitation [22]. The study recorded a major complication (increased intracranial pressure) in one of 6 implanted patients resolved after the device removal, and promising functional results in the other cases [22]. Further investigations should be necessary to clarify the role of this major event and the applicability before 5 years of age. Finally, Carnevale et al. highlighted a risk of extrusion in case of revision surgery for the Bonebridge [3].
ADHEAR [MED-EL, Innsbruck, Austria] is an adhesive bone conduction hearing aid introduced in 2018 to overcome the skin pressure issues of transcutaneous implants and the skin complications associated with percutaneous implants [5]. It consists of processor attached to an adhesive adapter with a snap-on attachment which is secured to the mastoid plane [31]. Contact is maintained only through the adhesive glue of the adapter [5]. This device is characterized by little to no complications and the absence of surgical intervention for its placement, which makes it quickly and effectively applicable in any case. However, its significantly lower functional gain compared to implantable prostheses limits its application to cases with mild deficits, not undergoing surgery for any reason.
Conclusions
Bone conduction hearing aids represent a viable option for hearing rehabilitation in conductive or mixed hearing loss and SSD. Nowadays, the variability of these devices and their features allow tailoring the hearing rehabilitative treatment depending on patients’ personal needs and residual hearing features. In fact, all the examined devices show worthy results on both PTA gain and speech audiometry, and in the era of precision and tailored medicine, these means can represent feasible treatment options.
Further studies will be necessary to confirm these promising results and in particular to study the incidence of complications in larger populations and to refine the indications of each device.
References
Ratuszniak A, Skarzynski PH, Gos E, Skarzynski H (2022) Self-rated benefits of auditory performance after Bonebridge implantation in patients with conductive or mixed hearing loss, or single-sided deafness. Life (Basel) 12(2):137. https://doi.org/10.3390/life12020137
Almuhawas F, Alzhrani F, Saleh S, Alsanosi A, Yousef M (2021) Auditory performance and subjective satisfaction with the ADHEAR system. Audiol Neuro-otol 26(1):1–10. https://doi.org/10.1159/000507775
Carnevale C, Morales-Olavarría C, Til-Pérez G, Sarría-Echegaray P (2023) Bonebridge® bone conduction implant. Hearing outcomes and quality of life in patients with conductive/mixed hearing loss. Eur Arch Otorhinolaryngol 280(4):1611–1619. https://doi.org/10.1007/s00405-022-07631-0
den Besten CA, Monksfield P, Bosman A et al (2019) Audiological and clinical outcomes of a transcutaneous bone conduction hearing implant: six-month results from a multicentre study. Clin Otolaryngol 44(2):144–157. https://doi.org/10.1111/coa.13248
Urík M, Hošnová D, Šlapák I et al (2019) First experiences with a new adhesive bone conduction hearing device in children. Int J Pediatr Otorhinolaryngol 126:109614. https://doi.org/10.1016/j.ijporl.2019.109614
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Willenborg K, Avallone E, Maier H, Lenarz T, Busch S (2022) A new active Osseointegrated implant system in patients with single-sided deafness. Audiol Neurootol 27(1):83–92. https://doi.org/10.1159/000515489
You P, Choi A, Drob J, Hunsaker SM, Liu YC, Silva R (2022) Early outcomes of a new active transcutaneous bone conduction implant in pediatric patients. Otol Neurotol 43(2):212–218. https://doi.org/10.1097/MAO.0000000000003426
Florentine MM, Virbalas J, Chan DK (2022) Early surgical and audiologic outcomes of active, transcutaneous, osseointegrated bone-conduction hearing device (Osia 2® system) placement. Int J Pediatr Otorhinolaryngol 156:111114. https://doi.org/10.1016/j.ijporl.2022.111114
Briggs R, Birman CS, Baulderstone N et al (2022) Clinical performance, safety, and patient-reported outcomes of an active osseointegrated steady-state implant system. Otol Neurotol 43(7):827–834. https://doi.org/10.1097/MAO.0000000000003590
Lau K, Scotta G, Wright K et al (2020) First United Kingdom experience of the novel Osia active transcutaneous piezoelectric bone conduction implant. Eur Arch Otorhinolaryngol 277(11):2995–3002. https://doi.org/10.1007/s00405-020-06022-7
Marszał J, Gibasiewicz R, Błaszczyk M, Gawłowska M, Gawęcki W (2021) Piezoelectric bone conduction hearing implant Osia® - audiological and quality of life benefits. Otolaryngol Pol 75(6):11–22. https://doi.org/10.5604/01.3001.0014.9342
Goycoolea M, Ribalta G, Tocornal F et al (2020) Clinical performance of the Osia™ system, a new active osseointegrated implant system. Results from a prospective clinical investigation. Acta Otolaryngol 140(3):212–219. https://doi.org/10.1080/00016489.2019.1691744
Rauch AK, Wesarg T, Aschendorff A, Speck I, Arndt S (2022) Long-term data of the new transcutaneous partially implantable bone conduction hearing system Osia®. Eur Arch Otorhinolaryngol 279(9):4279–4288. https://doi.org/10.1007/s00405-021-07167-9
Gawęcki W, Gibasiewicz R, Marszał J, Błaszczyk M, Gawłowska M, Wierzbicka M (2022) The evaluation of a surgery and the short-term benefits of a new active bone conduction hearing implant - the Osia®. Braz J Otorhinolaryngol 88(3):289–295. https://doi.org/10.1016/j.bjorl.2020.05.021
Mylanus EAM, Hua H, Wigren S et al (2020) Multicenter clinical investigation of a new active osseointegrated steady-state implant system. Otol Neurotol 41(9):1249–1257. https://doi.org/10.1097/MAO.0000000000002794
Kim Y, Choe G, Oh H, Choi BY (2023) A comparative study of audiological outcomes and compliance between the Osia system and other bone conduction hearing implants. Eur Arch Otorhinolaryngol 280(5):2217–2224. https://doi.org/10.1007/s00405-022-07715-x
Pla-Gil I, Redó MA, Pérez-Carbonell T et al (2021) Clinical performance assessment of a new active osseointegrated implant system in mixed hearing loss: results from a prospective clinical investigation. Otol Neurotol 42(7):e905–e910. https://doi.org/10.1097/MAO.0000000000003116
Young A, Fechtner L, Brennan C, Rende S, Wazen J (2023) Clinical performance, audiological outcomes, and quality of life of the Cochlear Osia ® system. Am J Otolaryngol 44(5):103951. https://doi.org/10.1016/j.amjoto.2023.103951
Amaral MSAD, Santos FRD, Danieli F, Massuda ET, Reis ACMB, Hyppolito MA (2022) Surgical and audiological results of bone-anchored hearing aids: comparison of two surgical techniques. Braz J Otorhinolaryngol 88(4):533–538. https://doi.org/10.1016/j.bjorl.2020.07.003
Bae SH, Jung Y, Jung J, Choi JY (2022) Clinical experience of using active transcutaneous bone conduction implants (Bonebridge) in children under 5 years old. Clin Exp Otorhinolaryngol 15(2):194–196. https://doi.org/10.21053/ceo.2021.02208
Brkic FF, Riss D, Scheuba K et al (2019) Medical, technical and audiological outcomes of hearing rehabilitation with the Bonebridge transcutaneous bone-conduction implant: a single-center experience. J Clin Med 8(10):1614. https://doi.org/10.3390/jcm8101614
Chen Y, Ren LJ, Gao N et al (2022) Long-term hearing performance and soft tissue outcomes of the Baha® attract system in patients with bilateral congenital microtia in a single centre. Clin Otolaryngol 47(2):357–363. https://doi.org/10.1111/coa.13901v
Cywka KB, Skarżyński H, Król B, Skarżyński PH (2021) The Bonebridge BCI 602 active transcutaneous bone conduction implant in children: objective and subjective benefits. J Clin Med 10(24):5916. https://doi.org/10.3390/jcm10245916
Dahm V, Baumgartner WD, Liepins R, Arnoldner C, Riss D (2018) First results with a new, pressure-free, adhesive bone conduction hearing aid. Otol Neurotol 39(6):748–754. https://doi.org/10.1097/MAO.0000000000001829
Garcier M, Lavedrine A, Gagneux C, Eluecque T, Bozorg Grayeli A (2021) Bone-anchored and closed skin Bonebridge implant in adults: hearing performances and quality of life. Audiol Neurootol 26(5):310–316. https://doi.org/10.1159/000512496
Hirth D, Weiss R, Stöver T, Kramer S (2021) Audiological benefit and subjective satisfaction with the ADHEAR hearing system in children with unilateral conductive hearing loss. Eur Arch Otorhinolaryngol 278(8):2781–2788. https://doi.org/10.1007/s00405-020-06364-2
Kim H, Park MK, Park SN et al (2023) Efficacy of the Bonebridge BCI602 for adult patients with single-sided deafness: a prospective multicenter study. Otolaryngol Head Neck Surg 170(2):490–504. https://doi.org/10.1002/ohn.520
Nevoux J, Coudert C, Boulet M et al (2018) Transcutaneous Baha attract system: long-term outcomes of the French multicenter study. Clin Otolaryngol 43(6):1553–1559. https://doi.org/10.1111/coa.13214
Pfiffner F, Kegel A, Probst R (2021) ADHEAR device in bone conduction audiometry. JASA Express Lett 1(12):122001. https://doi.org/10.1121/10.0009082
Skarzynski PH, Dziendziel B, Wlodarczyk E, Skarzynski H (2022) The Oticon Ponto system in adults with severe-to-profound and mixed hearing loss: audiologic outcomes and patient satisfaction. Otol Neurotol 43(9):987–994. https://doi.org/10.1097/MAO.0000000000003664
Skarżyński PH, Ratuszniak A, Król B et al (2019) The Bonebridge in adults with mixed and conductive hearing loss: audiological and quality of life outcomes. Audiol Neurootol 24(2):90–99. https://doi.org/10.1159/000499363
Ye T, Guo C, Fu X, Xia Y (2023) Long-term outcome of sound localization with Baha ® attract system. J Craniofac Surg 34(5):e513–e516. https://doi.org/10.1097/SCS.0000000000009398
Cox RM, Alexander GC (1995) The abbreviated profile of hearing aid benefit. Ear Hear 16(2):176–186. https://doi.org/10.1097/00003446-199504000-00005
Robinson K, Gatehouse S, Browning GG (1996) Measuring patient benefit from otorhinolaryngological surgery and therapy. Ann Otol Rhinol Laryngol 105(6):415–422. https://doi.org/10.1177/000348949610500601
Gatehouse S, Noble W (2004) The speech, spatial and qualities of hearing scale (SSQ). Int J Audiol 43(2):85–99. https://doi.org/10.1080/14992020400050014
Hultcrantz M (2011) Outcome of the bone-anchored hearing aid procedure without skin thinning: a prospective clinical trial. Otol Neurotol 32(7):1134–1139. https://doi.org/10.1097/MAO.0b013e31822a1c47
Bezdjian A, Bruijnzeel H, Daniel SJ, Grolman W, Thomeer HGXM (2017) Preliminary audiologic and peri-operative outcomes of the Sophono™ transcutaneous bone conduction device: a systematic review. Int J Pediatr Otorhinolaryngol 101:196–203. https://doi.org/10.1016/j.ijporl.2017.08.014
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manuelli, M., Migliorelli, A., Moretti, C. et al. Bone-conduction Hearing Aids: A Scoping Review. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-05042-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-05042-7