Abstract
Owing to high global prevalence, incidence and associated mortality, cancer of head and neck particularly oral cancer remains a cardinal domain for research and trials. Immune-modulatory therapies that employ patients own immune system for therapeutic benefits in oral cancer seems promising. The aim of this review is to gauge the potential of immunotherapy as fourth domain of Oral cancer therapeutics. Articles were searched using suitable search terms in MEDLINE and Google Scholar database to include clinical trials, meta-analyses, and research in humans/animals/cell lines published in peer reviewed journals. A total of 97 articles were included in this review. Literature has several studies and trials where different types of immunotherapies has been attempted but it is crucial to identify precise biomarkers of genome based targeted agents and to find parameters to select patients who might benefit from immunotherapy. Also further research is required to estimate predictive value of tumor mutational burden and mutational signatures so as to aid in personalized prediction of oral cancer therapeutic response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The crux of cancer immunotherapy lies in the recognition of cancer cells as non-self/foreign and subsequent attack by an activated immune system.
In routine, immune surveillance actively destroys the suspected/altered cells (premalignant cells) before transformation into a tumor, but alterations in the transformed cells (allowing immune escape) or any derangements in the immune system enable cancer embodiment.
Owing to high global prevalence, incidence, and associated mortality, cancer of the head and neck particularly oral cancer remains a cardinal domain for research and trials [1].
The triple combination therapy comprising chemotherapy, radiotherapy, and surgery has been the routine line of treatment followed for decades, however poor outcomes in the form of a stunted 5-year survival rate make it imperative to find a more effective treatment.
In the past two decades, research directed toward optimizing therapeutic regimes to improve the outcomes of cancer is persevering. This has resulted in new strategies based on an understanding of the pathology and molecular details of oral cancer.
Immunotherapy has emerged as the most promising potential treatment of choice in oral cancer.
It is well known that the various physical, chemical, and biological carcinogenic factors that cause either genetic or epigenetic alterations, endow the cell to attain different peculiar carcinogenic traits (hallmarks of cancer) leading to the development of cancer [2].
Out of all, the escape from immune surveillance plays a critical role bestowing, cancer cells capability to resist the host immune system either by developing an immunosuppressive state with lower absolute lymphocyte counts than those found in healthy subjects, impaired natural killer (NK)–cell activity, and poor antigen-presenting function or by inculcating a genetically modified immune resistant state.
Therefore, immune-modulatory therapies that overcome immune suppressive signals in oral cancer patients have therapeutic promise. These include various cancer immunotherapeutic methods such as immune checkpoint inhibitors (ICIs), cancer vaccines using tumor peptide antigens, or viral, bacterial, and DNA-based vectors as well as tumor antigen–specific monoclonal antibodies (moAbs), cell-based therapies, and cytokines therapy [3,4,5,6,7].
This review aims to gauge the potential of immunotherapy as the fourth domain of Oral cancer therapeutics. The initial section of this discussion provides an overview of role of immune system in oral carcinogenesis directing for various types of immunotherapeutic regimes for oral cancer. The later sections of describe the status of research in the field intending future directions for development of newer strategies based on individual cancer cells’ characteristics determined by specific genes to obtain a “personalized treatment”.
Material and Method
The MEDLINE and Google Scholar database search was done for scientific literature about immunotherapy in oral cancer. The search terms used were “Oral Cancer”, “Oral Squamous Cell Carcinoma” OR “OSCC”, “head and neck neoplasm” OR “HNSCC” AND “immunotherapy”, “combination therapy”, “immunotherapy”. The final search encompassed articles published from 2012 to 2022 (10 years) and was limited to clinical trials, meta-analyses, and research in humans/animals/cell lines published in peer reviewed journals having impact factor > 1. The articles were screened to include only papers with clinically accurate and relevant information and to remove duplicate articles from independent searches. The bibliography was supplemented with additional articles that were found appropriate and necessary for a comprehensive literature review.
Results
The initial search resulted in the retrieval of nearly 491 manuscripts, which on further screening resulted in 123 manuscripts that were considered (Fig. 1).
Discussion
The immune system plays a key role in almost all stages of oral carcinogenesis. A thorough know-how becomes essential to explore the potential of various types of immunotherapeutic regimes for oral cancer is described in Table 1.
Immunology of Oral Carcinogenesis
It is well understood that for attaining malignancy, phenotypically normal cells exploit the host tissue to facilitate growth [8]. In a groundbreaking study, Scully (1983) addressed immunological anomalies in head and neck cancer patients as well as the data linking the immune system to carcinogenesis. Additionally, he provided an overview of the therapeutic approaches that use immune response modification (immunotherapy) [9].
There is ample evidence in the literature to demonstrate the close interaction between the immune system and tumours throughout the whole course of cancer genesis, progression, and metastasis. One significant and well-established characteristic of cancer is the tumor's ability to evade the immune response's damaging components. Therefore, identifying prognostic indicators, lowering medication resistance, and creating novel treatments all depend on our ability to comprehend the interplay between the tumour and the host immune system [10].
Both positive and negative effects might result from the intricate interactions or cross-talk between immune cells and cancer cells, i.e., tumour growth inhibition and enhancement. The final result is determined by the balance of these activities and can either be effective tumour elimination or tumour immune evasion. The gradual development of an immune-suppressive environment within the tumour and the selection of tumour variations resistant to immune effectors, or “immunoediting,” are necessary for immunoevasion. T lymphocyte-mediated response, or cell-mediated immunity, is compromised in oral cancer. This is shown as a reduction in T lymphocyte counts and subpopulations, which lowers lymphokine production and impairs T lymphocyte lymphoproliferative responses to mitogens and antigens [11].
When Boncinelli et al. (1978) examined the mononuclear cell infiltration linked to oral cancer, they found that a significant fraction of T lymphocytes (a cell-mediated immune response) was present, although negligible amounts of plasma cells were seen [12, 13]. While cell-mediated immune responses are not substantial in other carcinomas, they are in head and neck cancers, and this is the most visible immunologic shift linked to the disease. It is challenging to determine whether the immune abnormalities are primary or secondary to the carcinoma; however, since patients with oral carcinoma continue to have depressed cell-mediated immune responses following surgical treatment, while patients with other tumours recover, the defect may be primary in oral carcinoma patients [14, 15].
The dysplastic epithelial cells in oral cancer exhibit mononuclear cell infiltration in the connective tissue [16]. The more severe the dysplasia, the higher the density of the inflammatory cell infiltration. When there is a dense infiltration of mononuclear cells around the tumour, the prognosis of the illness is improved. Throughout the whole course of cancer's formation, progression, and metastasis, the immune system is seen to be involved. Early-stage tumours release immunoinhibitory molecules [17], which suppresses both systemic and local immunity. In more advanced instances, however, there is a significant loss of immune effector cells [18].
Role of Immune Response in Development of Oral Cancer
The interaction of cancer cells, healthy stromal cells, and host defense systems is a complicated process in the development of oral cancer. It has been observed that initially acute inflammation tends to resolve tumors but when they fail, chronic inflammation sets in to promote tumor cell growth and angiogenesis as demonstrated in animal tumor models and human cancers. Because of their ability to selectively recognize non-self-peptides from cellular compartments and to orchestrate a variety of immune responses that ultimately result in T cell-mediated tumour cell death, T cells have been a central focus of an antitumor response. Through the generation of cytotoxins and interferon (IFN)-γ, CD8 + cytotoxic T lymphocytes (CTL) and CD4 + helper T lymphocytes (Th)1 cells generally prevent the growth of cancer [19].
Three phases may be used to summarise the T cell-mediated immune response: (1) Immune synapse, where tumour antigens attached to the MHC molecule on the surface of antigen-presenting cells are delivered to T cell receptor; (2) A confirmatory co-stimulatory signal, like the CD 28/B7 interaction, or an inhibitory signal is sent; (3) immune-activating cytokines, like interleukin 12 or type I interferon (IFN), confirm signal 2, which points the cell in the direction of stimulation or inhibition [20,21,22].
An immune response to an antigen can become stronger thanks to stimulatory receptors. Normally, the inhibitory checkpoint receptors are present to prevent both an excessive immune response to non-self-antigens and autoimmunity to self-antigens. However, via a process known as “immune-editing,” which involves the overexpression of inhibitory receptors, the recruitment of suppressive cells into the tumour Micro Environment (TME), and the inefficient presentation of antigen to T cells, tumour cells evolve a variety of strategies to evade immune detection and response [23]. Whether malignant cells are able to withstand an activated antitumor T cell response depends on the final balance between effector cells, such as cytotoxic CD8-positive (CD81) T lymphocytes (CTL), and suppressive cells, such as Treg and myeloid-derived suppressor cells (MDSC) [24].
Role of Immune Response in the Progression of Oral Cancer
There is enough data in the literature that shows tumours can occasionally go dormant in people for years before coming back. As far as is known, tumour cells take advantage of a number of variables to thwart the immune response. These variables include aberrant antigen presentation, tolerance and immunological deviation, the production of immune-suppressive cytokines, and regulatory cells, which can be produced by either cancerous or non-cancerous cells in the tumour microenvironment.
When tumours down-regulate the antigen processing machinery that affects the major histocompatibility complex (MHC) I pathway, the proteosome components latent membrane protein (LMP) 2 and LMP7, and the transporter associated with antigen processing (TAP) protein, defective antigen presentation results. Tumour antigen expression is therefore down-regulated, which may increase the incidence and spread of tumours because cytotoxic T lymphocytes (CTL) are unable to identify target antigens on tumour cells. By interacting with the T cell receptor but not producing costimulatory molecules, tumour cells can cause tolerance in T cells. Furthermore, tumours elude immune response by tipping the scales from Th1 to Th2 (immune deviation), a process that is dependent on IL-10 and TGF-β. Additionally, there is evidence that both CTLs and natural killer (NK) cells are unable to kill tumour cells through death ligand-mediated inhibition of death receptors.
According to studies, CTLs regulate the death of tumour cells via regulating the p53 tumour suppressor gene. Cancer immune evasion is therefore significantly influenced by variables that promote tolerance and immunological deviation. TGF-β, tumour necrosis factor (TNF)-α, IL-1, IL-6, colony stimulating factor (CSF)-1, IL-8, IL-10, and type I IFNs are examples of immune suppressive cytokines whose production plays a significant role in the growth of tumours. A variety of suppressive cell types, such as CD4 + CD25 + FoxP3 + regulatory T cells (Tregs), can mediate immune suppression within the tumour microenvironment. The generation of chemokines by tumour cells attracts tumor-derived Tregs, which are characterised by a greater suppressive activity than those found in normal tissues [15].
Role of Immune Response in the Prognosis of Oral Cancer
Oral cancer prognosis is well-established in connection to local immune responses, and when there is a substantial infiltration of mononuclear cells, the prognosis appears to be better [25]. When the local lymph nodes exhibit an enlarged inner cortex, a higher number of germinal centres, and a lymphocyte predominance pattern, they are also considered “active,” which improves the prognosis [26]. The heterogeneity of oral cancer is another significant aspect that influences the immune response and determines the prognosis. Genetic instability introduces heterogeneity in terms of both shape and physiology, which is manifested as a plurality of cell surface molecule expression and varying proliferative and angiogenic potential, even though tumours are known to start from a single altered cell. As a result, a large range of antigens, either tumor-specific or tumor-associated, are expressed by the tumour cells. The discovery of possible targets, the effectiveness of treatment, and diagnosis are all significantly impacted by this variability.
It is commonly known that a tiny percentage of cells within a primary tumour subpopulation develop the ability to spread to other locations by eluding immune clearance. The cancer cells' secretion of TGF-β plays a significant role in the spread of tumours. Furthermore, in a way that is dependent on VEGF, inducible nitric oxide synthase (iNOS), and hypoxia in and around tumour vasculature, hypoxia also aids in the metastatic spread of cancer cells. Notably, hypoxia induces lysyl oxidase synthesis, which facilitates the establishment of pre-metastatic habitats. It also modifies pre-metastatic niches by drawing in MDSCs and inhibiting the activities of NK cells [27].
In a comprehensive review published recently, Sievilainen et al. examined the prognostic significance of immune checkpoints in OSCC from 1985 to 2017. They found that seven immune checkpoints—PD‐L1, FKBP51, B7‐H4, B7‐H6, ALHD1, IDO1, and B7‐H3—had been linked to a lower chance of survival [28]. Huang et al. conducted a meta-analysis to determine the prognostic value of TILs in OSCC. They discovered that whereas high infiltration of CD163 + and CD68 + macrophages was linked with a bad prognosis, high infiltration of CD8 + TILs, CD45RO + TILs, and CD57 + TILs was related with favourable survival [29]. Hadler-Olsen et al. discovered in another meta-analysis that there was a positive correlation between the outcome of patients with OSCC and CD163 + M2 and CD57+ [30].
Immunotherapy: Potential in Oral Cancer Therapy
Unquestionably effective against a few of cancer types, immunotherapeutic strategies hold up the prospect of even faster advancement when developed and paired with already available conventional treatments. Even though a great deal of information has been gathered about how tumours evade immune destruction, researchers and clinicians still face enormous challenges in their quest to find effective cancer medicines. Immunotherapy can be said to as active based on its mechanism of action when the immune system targets and attacks the tumour cells directly. To combat the tumour cells, immune cells obtained from blood or biopsied cancer tissue are cultivated, collected, and grown in vitro before being reintroduced into the body. In active immunotherapy, dendritic cells, cytotoxic T cells, and natural killer cells were often used. On the other hand, when immune cells' cell surface receptors are activated or increased, immunotherapy is regarded as passive. Thus, antibody-dependent cell-mediated (immunity) cytotoxicity is created, such as that caused by ipilimumab [31].
Based on type of immunotherapy various sub categories have been identified. These can be studied as under.
Antibody Based
Immune Checkpoint Inhibitors (ICIs)
The identification of inhibitory pathways that promote tumour development by reducing T-cell activity marked a significant turning point in the area of immunotherapy. It is known that the use of so-called checkpoint inhibitors to disrupt these inhibitory pathways might cause a tumour to retreat [32].
Anti-CTLA-4 and anti-PD-1 antibodies are two checkpoint inhibitors that are often utilised therapeutically. Compared to anti-PD-1 antibodies, anti-CTLA-4 antibodies have a wider range of T cell activity, supporting the notion that anti-CTLA-4 has more adverse consequences than anti-PD-1. Membrane-bound PD-1 receptors represent immune cells such as T cells. When PD-L1, a ligand expressed by tumor cells, binds to PD-1, it can block cytolytic T cells from attacking and allow cancer cells to evade immune monitoring. Therefore, ICIs that can inhibit the PD1/PD-L1 interaction provide a viable course of treatment [33].
Numerous clinical trials are testing immunotherapy that targets immunological checkpoints, either in isolation or in combination with chemotherapeutic or targeted therapeutic medications. Other checkpoint inhibitor receptors, such as lymphocyte-activation gene 3 (LAG3) and T cell immunoglobulin mucin (Tim) 3, have shown therapeutic benefits in clinical studies when combined with PD-1 medicines, in addition to anti-PD-1 and anti-CTLA-4 antibodies [34, 35].
The most researched biomarker, according to a thorough study by Kujan et al. (2020), was PD-L1, followed by PD-1, CTLA-4, TIM-3, and LAG-3. According to Ngamphaiboon et al., PD-L1 was expressed positively in 83.9% of OSCC samples in their cohort (n = 203) [36]. There is additional evidence linking elevated tumor-infiltrating lymphocytes (TILs) to PD-1/PD-L1 expression in OSCC [37, 38]. Poor clinical outcome was linked to high expression of PD-L1 [39]. Pembrolizumab and nivolumab, two immune checkpoint inhibitors (ICIs) that target programmed cell death-1 (PD-1) were authorised in 2016 as second-line treatments for recurrent and metastatic (R/M) head and neck cancer [40]. In 2019, pembrolizumab was approved as first-line treatment for advanced-stage HNC [41]. Lately, anti-PD-L1 ligand has entered the final stages of commercial development under the trade name durvalumab for use in clinical settings. In the therapy of cancer, it has been demonstrated that PD-1 inhibition and radiation work well together [42].
Checkpoint inhibitors frequently cause immunological side effects, particularly when used with anti-CTLA-4 antibodies since they function during the priming phase. Hepatitis, rash, hypothyroidism, adrenal insufficiency, colitis, and other autoimmune responses were among the symptoms [43]. While maintaining long-term quality of life, it is critical to reevaluate these medicines due to the unfavourable responses and poor prognosis in locally-advanced oral malignancies. Immunocheckpoint inhibitors (ICI) are recommended for the treatment of squamous cell carcinoma (SCC) of the head and neck based on the data that is currently available. The combination of neoadjuvant and adjuvant nivolumab as Immune Checkpoint inhibition in resectable locally-advanced oral cavity tumours was studied in a study conducted by Brooker et al. [44].
In order to determine the feasibility of targeting immune checkpoint molecules before to the advancement of oral potential malignant diseases (OPMDs) to OSCC, researchers have recently investigated the involvement of PD-1 and PD-L1. Actinic cheilitis patients had greater levels of PD-1/PD-L1 over-expression than healthy volunteers, but lower levels than those seen in OSCC [45]. Inhibiting the PD-1/PD-L1 pathway can stop malignant transformation in OPMDs, and dysplastic lesions expressing PD-L1 on epithelium and subepithelial cells can elude the immune system. These findings are reported by Yagyuu et al. and Zhou et al. [46,47,48].
Targeted Monoclonal Antibodies
Human or murine monoclonal antibodies with the capacity to attach to antigens linked to tumours can be produced. Nivolumab, pembrolizumab, and cetuximab are the three monoclonal antibodies that the US FDA has authorised. However, additional signalling pathway inhibitors, such as temsirolimus and rapamycin, as well as monoclonal antibodies, such as cetuximab and bevacizumab, which target the EGFR and VEGFR, respectively, are also being evaluated for the treatment of head and neck squamous cell carcinoma (HNSCC). Treatment options for unresectable recurrent or metastatic HNSCCs are limited. Because VEGF plays a crucial role in both cancer and immunosuppression, addressing it in both situations may be quite beneficial. A phase 2 study including R/M HNSCC indicated the potency of axitinib as an inhibitor of VEGFR 1, 2, and 3, with therapy linked with a median overall survival of 9.8 months and a 6-month overall survival rate of 70% in patients substantially pretreated [49].
In 95% of instances of HNSCC, there is a rise in EGFR expression, which inhibits invasion, metastasis, and apoptosis and causes the tumour to develop [50, 51]. Treating HNSCC using monoclonal antibodies that target EGFR, including cetuximab and panitumumab, has been shown to be successful whether used alone or in conjunction with radiation treatment [52]. Similarly, Muc-1 levels are found to increase in HNSCC and antibodies against Muc-1 have shown regression in the tumor in advanced cancer [53]. Immunoglobulins against mutated p53 have demonstrated efficacy in treating HNSCC, especially in cases where node involvement is present. Gain-of-function activity of mutant p53, which inhibits both cell autonomous and non-cell autonomous surveillance mechanisms, is another factor that promotes the growth of cancer [54, 55].
Adoptive Cell Transfer
The T cells obtained from blood or biopsied cancer tissue can be cultivated/harvested, grown in vitro, and then reintroduced back into the body to combat the tumour cells, as previously mentioned in the section. By genetically engineering certain antigen receptors into the cells, one can increase T cells' efficacy and improve their capacity to identify tumour antigen [56]. Adoptive cell transfer (ACT) has shown promise in treating a variety of tumour types that were previously challenging to treat with traditional methods. ACT's success rate is driving improvements in the programme [57].
Antigen receptors may be engineered by two methods: (1) enhanced MHC complex presentation, and (2) chimeric antigen receptor (CAR). Viral vectors are used in the CAR T-cell immunotherapy process. The ability to tailor this technique to particular tumour antigens is by far its greatest benefit [58,59,60].
Cancer Vaccines
Cancer vaccines are created using the tumour cells from patients. They are engineered to contain the desired antigen, which can be a single antigen like RNA, DNA, or peptides, or multiple antigens like pulsed dendritic cells or whole cells that can teach T cells to identify and eliminate the cancer cells in the tumour [61].
Vaccines can be used in conjunction with other immunotherapy methods to produce less harmful, long-lasting immunity. In addition to being costly, these vaccinations have other drawbacks, such as the inability to treat tumours that grow quickly and the potential for a lengthy immune response [62]. Vaccines may be categorised as follows based on their nature and method of action: (a) antigen vaccine; (b) dendritic cell vaccine; (c) DNA/RNA vaccine; and (d) whole cell vaccination.
Certain antigens from tumour tissue, which have the ability to kill cancer cells, are the components of antigen vaccines. Future developments in genetic engineering make large-scale manufacturing possible.
Dendritic Cell Vaccines
Vaccines against tumour cells employ a dendritic cell's capacity to identify and target such cells. The vaccination that was created in the lab shows a lot of promise for tumour regression. It has been demonstrated that dendritic cell immunotherapy is a viable, safe, and successful treatment for a number of cancer types, including prostate cancer, glioblastoma, lung adenocarcinoma, lung adenocarcinoma, and oropharyngeal adenocarcinoma [63,64,65,66,67,68,69,70,71]. On the other hand, there aren't many reports of DC-based immunotherapy for oral cancer yet. Thus, DC vaccination offers cancer patients a fresh and bright future, either by itself or in conjunction with other medications such as immune checkpoint inhibitors [72]. DNA or RNA vaccines are composed of RNA or DNA have shown to be great options for tumour regression. Whole-cell vaccines are created from whole cancer cells as opposed to particular antigens, DNA, or RNA [31, 61]. Effectiveness challenges for T-cell-based immunotherapy, such as the existence of genetic changes in IFN response genes and antigen presentation machinery, may be addressed by natural killer (NK)-cell-based immunotherapy. Many solid tumour forms, including head and neck squamous cell carcinoma (HNSCC), have an immunosuppressive tumour microenvironment that can negate the effects of all immunotherapy treatments. In HNSCC, NK-cell activity is suppressed by myeloid-derived suppressor cells (MDSC). Significant amounts of CD14 + monocytic-MDSC and CXCR1/2 + CD15 + PMN-MDSC are seen in tumour infiltrating and circulating in patients with HNSCC. Compared to circulation-source MDSC, tumour MDSC showed more immunosuppression. TGFβ and nitric oxide were two of the several, distinct, cell-specific pathways that mediated the immunosuppression of HNSCC tumour MDSCs [63].
Cytokine Immunotherapy
Cytokines are chemicals that help immune system cells interact with one another in order to produce a coordinated response to a target antigen, such as a cancer cell.
Immunotherapy based on cytokines activates immune cells via an intricate process, improving the synchronisation of stromal cells and tumour cells. A number of cytokines have been created recently to treat cancer. At present, the FDA has authorised interferon α (IFN α) and interleukin 2 (IL-2) as two cytokines for clinical use. Subcutaneous injections of IFN α cytokines have demonstrated remarkable outcomes in terms of tumour shrinkage. Nevertheless, IFN α exhibited a partial response and increased toxicity when paired with IL-2 [73]. IL-2 is a cytokine that has FDA approval that raises the number of TILs (tumor-infiltrating lymphocytes) and NK cells in the lesion. Patients with HNSCC who had monoclonal antibody treatment following surgery had a higher chance of survival when perilymphatic IL-2 injection boosted the number of tumor-reactive T cells in their bodies [74]. Because of their greater degree of pleiotropism, cytokines present difficulties in their therapeutic use. They affect a wide variety of cell types in the body, which has a variety of opposing effects, including exhaustion, diarrhoea, pancytopenia, and weariness [31, 75].
Current Standing of Immunotherapy in Oral Cancer and Head and Neck Cancer Therapeutics
Since the development of cancer immunotherapy, attention has been continually drawn to the treatment of head and neck cancer as well as oral cancer. Determining the specific indicators of genome-based targeted medicines and developing selection criteria for individuals who may benefit from this therapy approach become imperative [76]. Patients with metastases from oral cancer or head and neck cancer are often not expected to recover, and few treatment strategies have been demonstrated to enhance overall survival (OS) or progression-free survival (PFS) [77].
Many prognostic indicators are used to evaluate the clinical outcome of chemotherapy; nevertheless, the most significant elements that might affect the response are the stage of the malignancy and previous treatments (chemo/radiation, surgery, or other) [58]. Additionally, a number of pharmaceutical substances, in particular monoclonal antibodies, have demonstrated significant promise in the management of HNSCC, and several of them are presently undergoing clinical trials [78]. Immunotherapy was first authorised for recurring or metastatic instances of oral cancer, just as other head and neck malignancies. Recently, preoperative neoadjuvant immunotherapy has been offered for untreated oral cancer [79, 80].
Certain traditional anticancer medications, including lenalidomide, have immune-stimulating properties that can work in concert with other immune-based therapies. The idea that radiation treatment can strengthen the immune system's reaction to cancer is also thrilling. Even so, radiation dosage optimisation is still in its infancy [81, 82]. To evaluate cancer response to immunotherapy, the gathered proof from systematic reviews and meta-analyses by Sievilainen et al. [28]; Huang et al. [29], and Hadler-Olsen et al. [30] has been quite fruitful in disclosing the immune profile and their prognostic significance in tumors.
Antibodies against both programmed cell death-1 (anti-PD-1) and programmed cell death ligand-1 (anti-PD-L1) are essential components of the presently authorised immunotherapy for head and neck cancer, which includes oral cancer [20, 83]. Using samples from patients receiving immunotherapy, several researchers have examined the two pertinent biomarkers (PD-1 and PD-L1) in order to determine which instances are more likely to benefit from such treatment. For instance, in recent head and neck cancer trials, expression of PD-L1 shown a substantial correlation with response to durvalumab, an anti-PD-L1 antibody. According to these investigations, a threshold of 25% for PD-L1-stained cancer cells can be used to assess a patient's reaction to durvalumab immunotherapy [84].
In a different investigation on the anticancer efficacy of pembrolizumab-based immunotherapy, Chow et al. recommended that PD-L1 score be taken into consideration for both immune and cancer cells, with a 1% cutoff point [85]. In a similar vein, Emancipator et al. reported that a “combined positive score,” which calculates the impact of pembrolizumab on a cell's response by analysing the ratio of PD-L1-expressing cells (i.e., immune cells and cancer cells) to each viable cancer cell multiplied by 100 [86].
Such immunotherapy enhanced patient survival in a phase 3 study comprising 361 patients with recurrent HNSCC treated with nivolumab. PD-L1 expression, however, did not have a major impact on how well the therapy responded [87,88,89]. Dorta-Estremera et al. (2019) tested methods for boosting anti-PD-1 therapeutic effectiveness using a preclinical HPV+ oral tumour model. While PD-1 blocking antibody monotherapy was shown to be ineffective against tumours implanted in the flank, it did cause regression in 54% of mice with orthotopic tongue tumours. A 100-day survival rate of 93.3% was seen when combination immunotherapy that targeted both CTLA-4 and PD-1 simultaneously was studied. In 71% of mice, systemic therapy with α-PD-1 and α-CTLA-4 antibodies together with the delivery of an agonist for Stimulator of Interferon Induced Genes (STING) into the flank tumours led to persistent tumour reduction. Thus, it was shown that α-PD-1 therapy in combination with CTLA-4 inhibition and/or STING agonist to induce IFN-α/β signalling may be a viable treatment option for patients with oral cancer, particularly those who do not react to α-PD-1 monotherapy [90].
Other known parameters, such as tumour mutational load and mutational signatures, may also be linked to the response to immunotherapy, in addition to immune response and immunological biomarkers [91]. The quantity of somatic mutations per coding region in a tumor's genome is referred to as the tumour mutational load. It has been demonstrated that, in addition to having a predictive value in many malignancies, tumour mutational load has a considerable value in predicting response to immunotherapy with pembrolizumab [91,92,93]. Pembrolizumab has been advised for cases with a high tumour mutational burden (≥ 10 mutations/megabase), however some researchers have cautioned against applying this universal threshold and emphasised the fact that cytotoxic chemotherapy is frequently administered to cancer patients, which may result in a higher level of tumour mutational burden [94].
Therefore, in order to identify the subset of tumours that may benefit from immunotherapy, the ideal cutoff threshold for tumour mutational load in each kind of tumour still has to be determined. Furthermore, it is imperative to acknowledge that the intricate tumour immunological milieu must be taken into account when evaluating the clinical outcome. Moreover, there is a correlation between comorbidities and hypercalcemia and poor clinical outcomes, higher recurrence rates, and shorter survival periods [77].
This might draw attention to the challenge of comparing the results from several trials using PD-L1 as a prognostic marker in the event that the immunotherapeutic drugs were different. It is also crucial to remember that the results on PD-1and/or PD-L1 that were previously discussed were derived from investigations that encompassed several head and neck cancer subsites with well-known variations in their clinical behaviour. Furthermore, based on further research, it will be necessary to decide whether to assess PD-L1 expression in immune cells only or in both cancer cells and immune cells. Furthermore, as immunorelated signature has demonstrated a strong predictive value for immunotherapy in other tumour types, techniques other than immunohistochemistry for evaluating immunological biomarkers have to be explored in instances of OSCC receiving immunotherapy [88, 89].
Conclusion
Immunotherapy has been a therapeutically useful treatment for oral cancer thanks to the incredibly successful use of immune response over the last three decades in grading, immunoscore identification, and biomarker discovery. When it comes to both determining which patients would benefit from immunotherapy and monitoring the course of treatment, a clinically appropriate assessment of the immune response might be deemed essential. Validation studies are desperately needed in order to validate the results of biomarkers that take advantage of the immune response, making it easier to identify cases of oral cancer that can benefit from immunotherapy and to gauge the patient's response. We have hardly begun to learn how to apply these new medicines optimally, logically mix them, or combine them with proven treatments, despite significant recent advancements. The majority of immunotherapies have toxicity as a result of either a lack of significant effectiveness or specificity.
It is important that in order to accurately anticipate the response to immunotherapy, trials in the future should take into account particular research on oral cancer. Additionally, research is still needed since the digital evaluation of immune biomarkers in oral cancer is still in its early stages. Likewise, more investigation is needed to determine the predictive significance of tumour mutational load and mutational signatures in order to provide tailored prediction of oral cancer treatment outcome.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
https://gco.iarc.fr/today/data/factsheets/cancers/1-Lip-oral-cavity-fact-sheet.pdf [accessed 09 Oct,2023]
Hanahan D (2022) Hallmarks of cancer: new dimensions. Cancer Discov 12(1):31–46
Kuss I, Hathaway B, Ferris RL, Gooding W, Whiteside TL (2004) Decreased absolute counts of T lymphocyte subsets and their relation to disease in squamous cell carcinoma of the head and neck. Clin Cancer Res 10(11):3755–3762
Bauernhofer T, Kuss I, Henderson B, Baum AS, Whiteside TL (2003) Preferential apoptosis of CD56dim natural killer cell subset in patients with cancer. Eur J Immunol 33(1):119–124
Dasgupta S, Bhattacharya-Chatterjee M, O’Malley BW, Chatterjee SK (2005) Inhibition of NK cell activity through TGF-β1 by down-regulation of NKG2D in a murine model of head and neck cancer. J Immunol 175(8):5541–5550
López-Albaitero A, Nayak JV, Ogino T, Machandia A, Gooding W, DeLeo AB, Ferrone S, Ferris RL (2006) Role of antigen-processing machinery in the in vitro resistance of squamous cell carcinoma of the head and neck cells to recognition by CTL. J Immunol 176(6):3402–3409
Ferris R, Whiteside TL, Ferrone S (2006) Clinical significance of downregulated antigen processing machinery in head and neck cancer. Clin Cancer Res 12:3890
Dwivedi R, Pandey R, Chandra S, Mehrotra D (2020) Apoptosis and genes involved in oral cancer-a comprehensive review. Oncol Rev 14(2):472
Scully C (1983) Immunology and oral cancer. Br J Oral Surg 21(2):136–146
Li B, Severson E, Pignon JC, Zhao H, Li T, Novak J, Jiang P, Shen H, Aster JC, Rodig S, Signoretti S (2016) Comprehensive analyses of tumor immunity: implications for cancer immunotherapy. Genome Biol 17(1):1–6
Bier J, Bitter K, Nicklisch U (1978) Unspecific cellular immunity before therapy in patients with squamous cell carcinoma of head and neck. J Maxillofac Surg 1(6):75–93
Boncinelli U, Fornieri C, Muscatello U (1978) Relationship between leukocytes and tumor cells in pre-cancerous and cancerous lesions of the lip: a possible expression of immune reaction. J Investig Dermatol 71(6):407–411
Löning T, Burkhardt A (1979) Plasma cells and immunoglobulin-synthesis in oral precancer and cancer: correlation with dysplasia, cancer differentiation, radio-and chemotherapy. Virchows Arch A 384:109–120
Chretien PB, Twomey PL, Trahan EE, Catalona WJ (1974) Quantitative dinitrochlorobenzene contact sensitivity in preoperative and cured cancer patients1. In: Conference on the use of BCG in therapy of cancer, No 39. National Cancer Institute, p 263
Twomey PL, Catalona WJ, Chretien PB (1974) Cellular immunity in cured cancer patients. Cancer 33(2):435–440
Johnson NW (1976) Medical disease and the anæsthetist: the role of histopathology in diagnosis and prognosis of oral squamous cell carcinoma. Proc R Soc Med 69(10):740–747
Whiteside TL (2005) Immunobiology of head and neck cancer. Cancer Metastasis Rev 24:95–105
Hoffmann TK, Dworacki G, Tsukihiro T, Meidenbauer N, Gooding W, Johnson JT, Whiteside TL (2002) Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res 8(8):2553–2562
Pardoll DM (2014) Cancer immunology. In: Abeloff’s clincial oncology, 5th edn, Vol 6. Saunders, Philadelphia, pp 78–97
Cramer JD, Burtness B, Ferris RL (2019) Immunotherapy for head and neck cancer: recent advances and future directions. Oral Oncol 1(99):104460
Sckisel GD, Bouchlaka MN, Monjazeb AM, Crittenden M, Curti BD, Wilkins DE, Alderson KA, Sungur CM, Ames E, Mirsoian A, Reddy A (2015) Out-of-sequence signal 3 paralyzes primary CD4+ T-cell-dependent immunity. Immunity 43(2):240–250
Moskovitz J, Moy J, Ferris RL (2018) Immunotherapy for head and neck squamous cell carcinoma. Curr Oncol Rep 20:1–7
Kim R (2007) Cancer immunoediting: from immune surveillance to immune escape. Cancer Immunother 1:9–27
Badoual C, Sandoval F, Pere H, Hans S, Gey A, Merillon N, Van Ryswick C, Quintin-Colonna F, Bruneval P, Brasnu D, Fridman WH (2010) Better understanding tumor–host interaction in head and neck cancer to improve the design and development of immunotherapeutic strategies. Head Neck 32(7):946–958
Jones JH, Coyle JI (1969) Squamous carcinoma of the lip: a study of the interface between neoplastic epithelium and the underlying mesenchyma. J Dent Res 48(5):702–708
Berlinger NT, Tsakraklides V, Pollak K, Adams GL, Yang M, Good RA (1976) Immunologic assessment of regional lymph node histology in relation to survival in head and neck carcinoma. Cancer 37(2):697–705
Vinay DS, Ryan EP, Pawelec G, Talib WH, Stagg J, Elkord E, Lichtor T, Decker WK, Whelan RL, Kumara HS, Signori E (2015) Immune evasion in cancer: mechanistic basis and therapeutic strategies. In: Seminars in cancer biology, vol 35. Academic Press, pp S185–S198
Sieviläinen M, Almahmoudi R, Al-Samadi A, Salo T, Pirinen M, Almangush A (2019) The prognostic value of immune checkpoints in oral squamous cell carcinoma. Oral Dis 25(6):1435–1445
Huang Z, Xie N, Liu H, Wan Y, Zhu Y, Zhang M, Tao Y, Zhou H, Liu X, Hou J, Wang C (2019) The prognostic role of tumour-infiltrating lymphocytes in oral squamous cell carcinoma: a meta-analysis. J Oral Pathol Med 48(9):788–798
Hadler-Olsen E, Wirsing AM (2019) Tissue-infiltrating immune cells as prognostic markers in oral squamous cell carcinoma: a systematic review and meta-analysis. Br J Cancer 120(7):714–727
Mohan SP, Bhaskaran MK, George AL, Thirutheri A, Somasundaran M, Pavithran A (2019) Immunotherapy in oral cancer. J Pharm Bioallied Sci 11(Suppl 2):S107
Darvin P, Toor SM, Sasidharan Nair V, Elkord E (2018) Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp Mol Med 50(12):1–1
Gong J, Chehrazi-Raffle A, Reddi S, Salgia R (2018) Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J Immunother Cancer 6:1–8
FDA U. S. Pembrolizumab (KEYTRUDA) (2016). Available at: https://www.fda.gov/drugs/resources-information-approved-drugs/pembrolizumab-keytruda.) (FDA, U. S . Nivolumab for SCCHN (2016). Available at: https://www.fda.gov/drugs/resources-information-approved-drugs/nivolumab-scchn) [Accessed 28 September 2023]
(FDA, U. S . FDA Approves Pembrolizumab for First-Line Treatment of Head and Neck Squamous Cell Carcinoma (2019). Available at: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pembrolizumab-first-line-treatment-head-and-neck-squamous-cell-carcinoma [Accessed 28 September,2023]
Ngamphaiboon N, Chureemas T, Siripoon T, Arsa L, Trachu N, Jiarpinitnun C, Pattaranutaporn P, Sirachainan E, Larbcharoensub N (2019) Characteristics and impact of programmed death-ligand 1 expression, CD8+ tumor-infiltrating lymphocytes, and p16 status in head and neck squamous cell carcinoma. Med Oncol 36:1
Wu L, Mao L, Liu JF, Chen L, Yu GT, Yang LL, Wu H, Bu LL, Kulkarni AB, Zhang WF, Sun ZJ (2019) Blockade of TIGIT/CD155 signaling reverses T-cell exhaustion and enhances antitumor capability in head and neck squamous cell carcinoma. Cancer Immunol Res 7(10):1700–1713
Lechner A, Schlößer H, Rothschild SI, Thelen M, Reuter S, Zentis P, Shimabukuro-Vornhagen A, Theurich S, Wennhold K, Garcia-Marquez M, Tharun L (2017) Characterization of tumor-associated T-lymphocyte subsets and immune checkpoint molecules in head and neck squamous cell carcinoma. Oncotarget 8(27):44418
Lin YM, Sung WW, Hsieh MJ, Tsai SC, Lai HW, Yang SM, Shen KH, Chen MK, Lee H, Yeh KT, Chen CJ (2015) High PD-L1 expression correlates with metastasis and poor prognosis in oral squamous cell carcinoma. PLoS ONE 10(11):e0142656
Krcik EM (2016) Radiation therapy plus anti-programmed death ligand 1 immunotherapy: a review on overall survival. Radiol Technol 88(1):123–128
Huang RY, Eppolito C, Lele S, Shrikant P, Matsuzaki J, Odunsi K (2015) LAG3 and PD1 co-inhibitory molecules collaborate to limit CD8+ T cell signaling and dampen antitumor immunity in a murine ovarian cancer model. Oncotarget 6(29):27359
Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC (2010) Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med 207(10):2187–2194
Weber JS, Antonia SJ, Topalian SL, Schadendorf D, Larkin JM, Sznol M, Liu HY, Waxman I, Robert C (2015) Safety profile of nivolumab (NIVO) in patients (pts) with advanced melanoma (MEL): a pooled analysis
Brooker RC, Schache AG, Sacco JJ (2021) NICO Phase II clinical trial–focus on an emerging immunotherapy strategy for the adjuvant treatment of locally-advanced oral cancers. Br J Oral Maxillofac Surg 59(8):959–962
de Souza Malaspina TS, Gasparoto TH, Costa MR, de Melo EF, Ikoma MR, Damante JH, Cavassani KA, Garlet GP, da Silva JS, Campanelli AP (2011) Enhanced programmed death 1 (PD-1) and PD-1 ligand (PD-L1) expression in patients with actinic cheilitis and oral squamous cell carcinoma. Cancer Immunol Immunother 60:965–974
Yagyuu T, Hatakeyama K, Imada M, Kurihara M, Matsusue Y, Yamamoto K, Obayashi C, Kirita T (2017) Programmed death ligand 1 (PD-L1) expression and tumor microenvironment: Implications for patients with oral precancerous lesions. Oral Oncol 1(68):36–43
Zhou G, Zhang J, Ren XW, Hu JY, Du GF, Xu XY (2012) Increased B7–H1 expression on peripheral blood T cells in oral lichen planus correlated with disease severity. J Clin Immunol 32:794–801
Kujan O, van Schaijik B, Farah CS (2020) Immune checkpoint inhibitors in oral cavity squamous cell carcinoma and oral potentially malignant disorders: a systematic review. Cancers 12(7):1937
Swiecicki PL, Bellile EL, Brummel CV, Brenner JC, Worden FP (2021) Efficacy of axitinib in metastatic head and neck cancer with novel radiographic response criteria. Cancer 127(2):219–228
Normanno N, De Luca A, Bianco C, Strizzi L, Mancino M, Maiello MR, Carotenuto A, De Feo G, Caponigro F, Salomon DS (2006) Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 366(1):2–16
Salomon DS, Brandt R, Ciardiello F, Normanno N (1995) Epidermal growth factor-related peptides and their receptors in human malignancies. Crit Rev Oncol Hematol 19(3):183–232
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer HR, Cupissol D, Peyrade F (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 359(11):1116–1127
Rabassa ME, Croce MV, Pereyra A, Segal-Eiras A (2006) MUC1 expression and anti-MUC1 serum immune response in head and neck squamous cell carcinoma (HNSCC): a multivariate analysis. BMC Cancer 6(1):1–3
Ghosh M, Saha S, Bettke J, Nagar R, Parrales A, Iwakuma T, van der Velden AW, Martinez LA (2021) Mutant p53 suppresses innate immune signaling to promote tumorigenesis. Cancer Cell 39(4):494–508
Chow V, Yuen AP, Lam KY, Ho WK, Wei WI (2001) Prognostic significance of serum p53 protein and p53 antibody in patients with surgical treatment for head and neck squamous cell carcinoma. Head Neck 23(4):286–291
Sadelain M, Rivière I, Brentjens R (2003) Targeting tumours with genetically enhanced T lymphocytes. Nat Rev Cancer 3(1):35–45
Rosenberg SA, Restifo NP (2015) Adoptive cell transfer as personalized immunotherapy for human cancer. Science 348(6230):62–68
Curran KJ, Pegram HJ, Brentjens RJ (2012) Chimeric antigen receptors for T cell immunotherapy: current understanding and future directions. J Gene Med 14(6):405–415
Klebanoff CA, Rosenberg SA, Restifo NP (2016) Prospects for gene-engineered T cell immunotherapy for solid cancers. Nat Med 22(1):26–36
Park JH, Brentjens RJ (2015) Are all chimeric antigen receptors created equal? J Clin Oncol Off J Am Soc Clin Oncol 33(6):651–653
Lollini PL, Cavallo F, Nanni P, Forni G (2006) Vaccines for tumour prevention. Nat Rev Cancer 6(3):204–216
Morton DL, Foshag LJ, Hoon DS, Nizze JA, Famatiga E, Wanek LA, Chang C, Davtyan DG, Gupta RK, Elashoff R (1992) Prolongation of survival in metastatic melanoma after active specific immunotherapy with a new polyvalent melanoma vaccine. Ann Surg 216(4):463
Greene S, Robbins Y, Mydlarz WK, Huynh AP, Schmitt NC, Friedman J, Horn LA, Palena C, Schlom J, Maeda DY, Zebala JA (2020) Inhibition of MDSC trafficking with SX-682, a CXCR1/2 inhibitor, enhances NK-cell immunotherapy in head and neck cancer models. Clin Cancer Res 26(6):1420–1431
Mackensen A, Herbst B, Chen JL, Köhler G, Noppen C, Herr W, Spagnoli GC, Cerundolo V, Lindemann A (2000) Phase I study in melanoma patients of a vaccine with peptide-pulsed dendritic cells generated in vitro from CD34+ hematopoietic progenitor cells. Int J Cancer 86(3):385–392
Banchereau J, Palucka AK, Dhodapkar M, Burkeholder S, Taquet N, Rolland A, Taquet S, Coquery S, Wittkowski KM, Bhardwaj N, Pineiro L (2001) Immune and clinical responses in patients with metastatic melanoma to CD34+ progenitor-derived dendritic cell vaccine. Cancer Res 61(17):6451–6458
Flörcken A, Kopp J, van Lessen A, Movassaghi K, Takvorian A, Jöhrens K, Möbs M, Schönemann C, Sawitzki B, Egerer K, Dörken B (2013) Allogeneic partially HLA-matched dendritic cells pulsed with autologous tumor cell lysate as a vaccine in metastatic renal cell cancer: a clinical phase I/II study. Hum Vaccines Immunother 9(6):1217–1227
Liau LM, Prins RM, Kiertscher SM, Odesa SK, Kremen TJ, Giovannone AJ, Lin JW, Chute DJ, Mischel PS, Cloughesy TF, Roth MD (2005) Dendritic cell vaccination in glioblastoma patients induces systemic and intracranial T-cell responses modulated by the local central nervous system tumor microenvironment. Clin Cancer Res 11(15):5515–5525
Schuler-Thurner B, Schultz ES, Berger TG, Weinlich G, Ebner S, Woerl P, Bender A, Feuerstein B, Fritsch PO, Romani N, Schuler G (2002) Rapid induction of tumor-specific type 1 T helper cells in metastatic melanoma patients by vaccination with mature, cryopreserved, peptide-loaded monocyte-derived dendritic cells. J Exp Med 195(10):1279–1288
Boudewijns S, Westdorp H, Koornstra RH, Aarntzen EH, Schreibelt G, Creemers JH, Punt CJ, Figdor CG, De Vries IJ, Gerritsen WR, Bol KF (2016) Immune-related adverse events of dendritic cell vaccination correlate with immunologic and clinical outcome in stage III and IV melanoma patients. J Immunother (Hagerstown, Md.: 1997) 39(6):241
Wojas-Krawczyk K, Krawczyk P, Buczkowski J, Walkowska A, Jankowska O, Czekajska-Chehab E, Milanowski J (2012) Immunotherapy of lung adenocarcinoma patient with Peptide-pulsed dendritic cells: a case report. Arch Immunol Ther Exp 60:69–77
Small EJ, Fratesi P, Reese DM, Strang G, Laus R, Peshwa MV, Valone FH (2000) Immunotherapy of hormone-refractory prostate cancer with antigen-loaded dendritic cells. J Clin Oncol 18(23):3894–3903
Kumar C, Kohli S, Chiliveru S, Jain M, Sharan B (2017) Complete remission of rare adenocarcinoma of the oropharynx with APCEDEN®(dendritic cell-based vaccine): a case report. Clin Case Rep 5(10):1692
Urba SG, Forastiere AA, Wolf GT, Amrein PC (1993) Intensive recombinant interleukin-2 and alpha-interferon therapy in patients with advanced head and neck squamous carcinoma. Cancer 71(7):2326–2331
Whiteside TL, Letessier E, Hirabayashi H, Vitolo D, Bryant J, Barnes L, Snyderman C, Johnson JT, Myers E, Herberman RB, Rubin J (1993) Evidence for local and systemic activation of immune cells by peritumoral injections of interleukin 2 in patients with advanced squamous cell carcinoma of the head and neck. Cancer Res 53(23):5654–5662
Dadian G, Riches PG, Henderson DC, MacLennan K, Lorentzos A, Moore J, Hobbs JR, Gore ME (1993) Immune changes in peripheral blood resulting from locally directed interleukin-2 therapy in squamous cell carcinoma of the head and neck. Eur J Cancer B Oral Oncol 29(1):29–34
Marur S, Forastiere AA (2016) Head and neck squamous cell carcinoma: update on epidemiology, diagnosis, and treatment. In: Mayo clinic proceedings, vol 91, no 3. Elsevier, pp 386–396
Colevas AD (2006) Chemotherapy options for patients with metastatic or recurrent squamous cell carcinoma of the head and neck. J Clin Oncol 24(17):2644–2652
Kozakiewicz P, Grzybowska-Szatkowska L (2018) Application of molecular targeted therapies in the treatment of head and neck squamous cell carcinoma. Oncol Lett 15(5):7497–7505
Zandberg DP, Algazi AP, Jimeno A, Good JS, Fayette J, Bouganim N, Ready NE, Clement PM, Even C, Jang RW, Wong S (2019) Durvalumab for recurrent or metastatic head and neck squamous cell carcinoma: Results from a single-arm, phase II study in patients with≥ 25% tumour cell PD-L1 expression who have progressed on platinum-based chemotherapy. Eur J Cancer 1(107):142–152
Schoenfeld JD, Hanna GJ, Jo VY, Rawal B, Chen YH, Catalano PS, Lako A, Ciantra Z, Weirather JL, Criscitiello S, Luoma A (2020) Neoadjuvant nivolumab or nivolumab plus ipilimumab in untreated oral cavity squamous cell carcinoma: a phase 2 open-label randomized clinical trial. JAMA Oncol 6(10):1563–1570
Hsu AK, Quach H, Tai T, Prince HM, Harrison SJ, Trapani JA, Smyth MJ, Neeson P, Ritchie DS (2011) The immunostimulatory effect of lenalidomide on NK-cell function is profoundly inhibited by concurrent dexamethasone therapy. Blood J Am Soc Hematol 117(5):1605–1613
Vacchelli E, Bloy N, Aranda F, Buqué A, Cremer I, Demaria S, Eggermont A, Formenti SC, Fridman WH, Fucikova J, Galon J (2016) Trial Watch: Immunotherapy plus radiation therapy for oncological indications. Oncoimmunology 5(9):e1214790
Chen DS, Mellman I (2017) Elements of cancer immunity and the cancer–immune set point. Nature 541(7637):321–330
Rebelatto MC, Midha A, Mistry A, Sabalos C, Schechter N, Li X, Jin X, Steele KE, Robbins PB, Blake-Haskins JA, Walker J (2016) Development of a programmed cell death ligand-1 immunohistochemical assay validated for analysis of non-small cell lung cancer and head and neck squamous cell carcinoma. Diagn Pathol 11:1–4
Chow LQ, Haddad R, Gupta S, Mahipal A, Mehra R, Tahara M, Berger R, Eder JP, Burtness B, Lee SH, Keam B (2016) Antitumor activity of pembrolizumab in biomarker-unselected patients with recurrent and/or metastatic head and neck squamous cell carcinoma: results from the phase Ib KEYNOTE-012 expansion cohort. J Clin Oncol 34(32):3838
Emancipator K, Huang L, Aurora-Garg D, Bal T, Cohen EE, Harrington K, Soulières D, Le Tourneau C, Licitra L, Burtness B, Swaby R (2021) Comparing programmed death ligand 1 scores for predicting pembrolizumab efficacy in head and neck cancer. Mod Pathol 34(3):532–541
Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE, Even C, Worden F (2016) Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med 375(19):1856–1867
Wang Y, Chen L, Yu M, Fang Y, Qian K, Wang G, Ju L, Xiao Y, Wang X (2020) Immune-related signature predicts the prognosis and immunotherapy benefit in bladder cancer. Cancer Med 9(20):7729–7741
Xiao Y, Cui G, Ren X, Hao J, Zhang Y, Yang X, Wang Z, Zhu X, Wang H, Hao C, Duan H (2020) A novel four-gene signature associated with immune checkpoint for predicting prognosis in lower-grade glioma. Front Oncol 30(10):605737
Dorta-Estremera S, Hegde VL, Slay RB, Sun R, Yanamandra AV, Nicholas C, Nookala S, Sierra G, Curran MA, Sastry KJ (2019) Targeting interferon signaling and CTLA-4 enhance the therapeutic efficacy of anti-PD-1 immunotherapy in preclinical model of HPV+ oral cancer. J Immunother Cancer 7:1–2
Oliva M, Spreafico A, Taberna M, Alemany L, Coburn B, Mesia R, Siu LL (2019) Immune biomarkers of response to immune-checkpoint inhibitors in head and neck squamous cell carcinoma. Ann Oncol 30(1):57–67
Sha D, Jin Z, Budczies J, Kluck K, Stenzinger A, Sinicrope FA (2020) Tumor mutational burden as a predictive biomarker in solid tumors. Cancer Discov 10(12):1808–1825
Cristescu R, Mogg R, Ayers M, Albright A, Murphy E, Yearley J, Sher X, Liu XQ, Lu H, Nebozhyn M, Zhang C (2018) Pan-tumor genomic biomarkers for PD-1 checkpoint blockade–based immunotherapy. Science 362(6411):eaar3593
Strickler JH, Hanks BA, Khasraw M (2021) Tumor mutational burden as a predictor of immunotherapy response: is more always better? Clin Cancer Res 27(5):1236–1241
Padmanabhan TK, Balaram P, Vasudevan DM (1987) Role of levamisole immunotherapy as an adjuvant to radiotherapy in oral cancer. I. A three-year clinical follow up. Neoplasma 34(5):627–632
Hadden J, Verastegui E, Barrera JL, Kurman M, Meneses A, Zinser JW, de la Garza J, Hadden E (2003) A trial of IRX-2 in patients with squamous cell carcinomas of the head and neck. Int Immunopharmacol 3(8):1073–1081
Tímár J, Ladányi A, Forster-Horváth C, Lukits J, Döme B, Remenár É, Godény M, Kásler M, Bencsik B, Répássy G (2005) Neoadjuvant immunotherapy of oral squamous cell carcinoma modulates intratumoral CD4/CD8 ratio and tumor microenvironment: a multicenter phase II clinical trial. J Clin Oncol 23(15):3421–3432
Yoshitake Y, Fukuma D, Yuno A, Hirayama M, Nakayama H, Tanaka T, Nagata M, Takamune Y, Kawahara K, Nakagawa Y, Yoshida R (2015) Phase II clinical trial of multiple peptide vaccination for advanced head and neck cancer patients revealed induction of immune responses and improved OS. Clin Cancer Res 21(2):312–321
Powell SF, Gitau M, Reynolds JT, Terrell AM, Lohr M, McGraw S, Nowak RK, Jensen AW, Blanchard MJ, Fischer CD (2018) Pembrolizumab in combination with chemoradiotherapy (CRT) in human papilloma virus (HPV)-associated head and neck squamous cell carcinoma (HNSCC). J Immunother Cancer 117
Cohen EE, Soulières D, Le Tourneau C, Dinis J, Licitra L, Ahn MJ, Soria A, Machiels JP, Mach N, Mehra R, Burtness B (2019) Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet 393(10167):156–167
Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, Psyrri A, Basté N, Neupane P, Bratland Å, Fuereder T (2019) Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 394(10212):1915–1928
Saba NF, Blumenschein G Jr, Guigay J, Licitra L, Fayette J, Harrington KJ, Kiyota N, Gillison ML, Ferris RL, Jayaprakash V, Li L (2019) Nivolumab versus investigator’s choice in patients with recurrent or metastatic squamous cell carcinoma of the head and neck: efficacy and safety in CheckMate 141 by age. Oral Oncol 1(96):7–14
Xiong Y, Neskey DM, Horton JD, Paulos CM, Knochelmann HM, Armeson KE, Young MR (2020) Immunological effects of nivolumab immunotherapy in patients with oral cavity squamous cell carcinoma. BMC Cancer 20(1):1
Rodriguez CP, Wu Q, Voutsinas J, Fromm JR, Jiang X, Pillarisetty VG, Lee SM, Santana-Davila R, Goulart B, Baik CS, Chow LQ (2020) A phase II trial of pembrolizumab and vorinostat in recurrent metastatic head and neck squamous cell carcinomas and salivary gland cancer. Clin Cancer Res 26(4):837–845
Machiels JP, Tao Y, Burtness B, Tahara M, Licitra L, Rischin D, Waldron J, Simon C, Gregoire V, Harrington K, Alves GV (2020) Pembrolizumab given concomitantly with chemoradiation and as maintenance therapy for locally advanced head and neck squamous cell carcinoma: KEYNOTE-412. Future Oncol 16(18):1235–1243
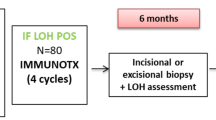
Gurizzan C, Lorini L, Paderno A, Tomasoni M, Zigliani G, Bozzola A, Ardighieri L, Battocchio S, Bignotti E, Ravaggi A, Romani C (2021) Immunotherapy for the prevention of high-risk oral disorders malignant transformation: the IMPEDE trial. BMC Cancer 21:1–6
Liu S, Bellile E, Nguyen A, Zarins K, D’Silva N, Rozek L, Wolf GT, Sartor MA, Moyer J, Patel M, Erman A (2021) Characterization of the immune response in patients with cancer of the oral cavity after neoadjuvant immunotherapy with the IRX-2 regimen. Oral Oncol 1(123):105587
Hwang M, Seiwert TY (2021) Are taxanes the future for head and neck cancer? Pragmatism in the immunotherapy era. Lancet Oncol 22(4):413–415
Sacco AG, Chen R, Worden FP, Wong DJ, Adkins D, Swiecicki P, Chai-Ho W, Oppelt P, Ghosh D, Bykowski J, Molinolo A (2021) Pembrolizumab plus cetuximab in patients with recurrent or metastatic head and neck squamous cell carcinoma: an open-label, multi-arm, non-randomised, multicentre, phase 2 trial. Lancet Oncol 22(6):883–892
Liu S, Knochelmann HM, Lomeli SH, Hong A, Richardson M, Yang Z, Lim RJ, Wang Y, Dumitras C, Krysan K, Timmers C (2021) Response and recurrence correlates in individuals treated with neoadjuvant anti-PD-1 therapy for resectable oral cavity squamous cell carcinoma. Cell Rep Med 2(10):100411
Li X, Fang Q, Du W, Zhang X, Dai L, Qiao Y (2021) Induction chemotherapy combined with immunotherapy in locally advanced head and neck squamous cell carcinoma. BMC Cancer 21(1):1–9
Vos JL, Elbers JB, Krijgsman O, Traets JJ, Qiao X, van der Leun AM, Lubeck Y, Seignette IM, Smit LA, Willems SM, van den Brekel MW (2021) Neoadjuvant immunotherapy with nivolumab and ipilimumab induces major pathological responses in patients with head and neck squamous cell carcinoma. Nat Commun 12(1):7348
Poulose JV, Kainickal CT (2022) Immune checkpoint inhibitors in head and neck squamous cell carcinoma: a systematic review of phase-3 clinical trials. World J Clin Oncol 13(5):388
Dzienis MR, Cundom JE, Fuentes CS, Hansen AR, Nordlinger MJ, Pastor AV, Oppelt P, Neki A, Gregg RW, Lima IP, Franke FA (2022) 651O Pembrolizumab (pembro)+ carboplatin (carbo)+ paclitaxel (pacli) as first-line (1L) therapy in recurrent/metastatic (R/M) head and neck squamous cell carcinoma (HNSCC): Phase VI KEYNOTE-B10 study. Ann Oncol 1(33):S839–S840
Wong DJ, Fayette J, Guo Y, Kowgier M, Cohen E, Nin RM, Dechaphunkul A, Prabhash K, Geiger J, Bishnoi S, Schafer H (2019) Abstract CT123: IMvoke010: Randomized Phase III study of atezolizumab as adjuvant monotherapy after definitive therapy of squamous cell carcinoma of the head and neck (SCCHN). Cancer Res 79(13_Supplement):CT123
Fuereder T, Minichsdorfer C, Mittlboeck M, Wagner C, Heller G, Putz EM, Oberndorfer F, Müllauer L, Aretin MB, Czerny C, Schwarz-Nemec U (2022) Pembrolizumab plus docetaxel for the treatment of recurrent/metastatic head and neck cancer: A prospective phase I/II study. Oral Oncol 1(124):105634
Gross N, Ferrarotto R, Nagarajan P, Bell D, El-Naggar A, Johnson JM, Yuan Y, Glisson BS, Wong M, Rosenthal D, Esmaeli B (2019) Phase II study of neoadjuvant cemiplimab prior to surgery in patients with stage III/IV (M0) cutaneous squamous cell carcinoma of the head and neck (CSCC-HN). Ann Oncol 1(30):v910
Acknowledgements
None to acknowledge
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
RD—Methodology, resources, formal analysis, writing original draft. AJ—Methodology, resources, formal analysis, writing original draft. SG—Conceptualization, validation, supervision, review, editing of manuscript. SC—Validation, supervision, review and editing of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
“This article does not contain any studies with human participants performed by any of the authors.” “This article does not contain any studies with animals performed by any of the authors.” “This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dwivedi, R., Jain, A., Gupta, S. et al. Immunotherapy: The Fourth Domain in Oral Cancer Therapeutics. Indian J Otolaryngol Head Neck Surg 76, 2257–2272 (2024). https://doi.org/10.1007/s12070-024-04565-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04565-3