Abstract
This study describes the clinical profile, operative findings, surgical technique, type of implant and complications encountered in implantation of abnormal cochlea by the transcanal (veria) technique in a tertiary care centre. This is a retrospective study done amongst 337 patients who underwent cochlear implantation by veria technique between January 2013 to August 2023. Based on pre-operative imaging with high-resolution computed tomography and magnetic resonance imaging the cochleovestibular malformations in this study were classified according to Sennaroglu classification and the cochlear ossification was graded from I to IV. Amongst the 337 patients who underwent cochlear implantation during the study period there were 79 cases (23.4%) with abnormalities of cochlea. This included 45 patients (13.4%) with congenital malformations, 20 patients (5.9%) with cochlear fibrosis and 14 patients (4.2%) with cochlear ossification. The commonest cochlear malformation was Incomplete Partition 2 which was present in 21 patients (46.7%). The other common malformations were cochlear hypoplasia (31.1%), Incomplete Partition 1(13.3%) and common cavity (8.9%). Out of the 20 patients with cochlear fibrosis, 17 patients had fibrosis only in the basal turn. Out of the 14 patients with cochlear ossification 8 patients (57.1%) had a grade 1 ossification, 2 patients (14.3%) had a grade 2 ossification and 4 patients (28.6%) had a grade 3 ossification. One of the patients required re-exploration for correcting the placement of electrode. The type of implant were chosen depending on individual malformation or length of ossification and fibrosis. In the past, inner ear anomalies were considered as a contraindication for cochlear implantation however it is now possible to implant most of these abnormal cochlea by careful planning, a modification of the surgical technique and the type of electrode used.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cochlear implants have revolutionized the treatment of congenital sensorineural hearing loss in the past few decades. About 20% of children with congenital sensorineural hearing loss (SNHL) are estimated to have inner ear abnormalities according to Jensen [1]. These patients may present with a wide range of hearing acquity and the rate of progression of hearing loss may be different in different anomalies and they may also be associated with non-otological anomalies. In the past, inner ear anomalies were considered as a contraindication for cochlear implantation based on histopathological reports of substantially reduced population of spiral ganglion cells in congenital inner ear anomalies [2, 3]. First implantation in a malformed cochlea was reported by Mangabeira-Albernaz in 1983, but the malformation was only realised during the revision surgery [4]. Following this there has been several reports of cochlear implantation in inner ear anomalies however the numbers are usually limited due to the rarity of these pathologies and it is usually a challenge for the implanting team.
In cases of acquired hearing loss an anatomically normal cochlea can undergo fibrosis and subsequent ossification which can arise due to various causes such as meningitis, autoimmune inner ear disease, cochlear otosclerosis, trauma or a lack of blood supply. Although cochlear implantation in cochlear ossification is no longer a contraindication, it remains a surgical challenge due to a range of surgical techniques and approaches available for the same and lack of consensus and unpredictability associated with the outcome. Through this study we would like to report our surgical experience of cochlear implantation in inner ear anomalies and cochlear fibrosis and ossification via the transcanal approach.
Materials and Methods
This is a retrospective study involving a tertiary referral centre in India amongst 337 patients between the ages of 1 year to 61 years who underwent cochlear implantation between January 2013 to August 2023. Preoperative evaluation included otologic examination to make sure of the absence of any external or middle ear pathologies. Audiological evaluation was performed by experienced audiologists using behavioural audiometry and electrophysiological tests, including auditory brainstem response and distortion product otoacoustic emissions testing. After evaluation with high-resolution computed tomography (HRCT) and magnetic resonance imaging (MRI) the cochleovestibular malformations in this study were classified according to Sennaroglu classification for the purpose of uniformity [5]. According to this he classified the inner ear anomalies into 8 categories such as complete labyrinthine aplasia, rudimentary otocyst, cochlear aplasia, common cavity, cochlear hypoplasia, incomplete partition (IP) of the cochlea, enlarged vestibular aqueduct and cochlear aperture abnormalities out of which the first three are not amenable to implantation. The cochlear ossification was graded from I-IV based on the extend of ossification and the area of cochlear fibrosis was noted based on T2 weighted MRI images [6]. Data was collected regarding the age, sex, hearing loss on audiological evaluation, radiological findings, intra operative findings, type of implant placed and complications if any. All the patients underwent cochlear implantation by transcanal (Veria) approach. All patients were followed up at least once a month following initial activation for a total of 6 months and at 3 month intervals thereafter.
Results
Amongst the 337 patients who underwent cochlear implantation during the study period there were 79 cases (23.4%) with abnormalities of cochlea. This included 45 patients (13.4%) with congenital malformations and 34 patients (10.1%) with acquired abnormalities out of which 20 (5.9%) had cochlear fibrosis and 14 (4.2%) had cochlear ossification (Fig. 1).
The average age of patients with cochlear malformation was 6.21 years and male to female ratio was 2:5. Out of the 45 patients with congenital malformations 1 patient had post lingual deafness (cochlear hypoplasia) and the remaining had pre lingual bilateral profound hearing loss. The commonest malformation was incomplete partition 2 (IP II) which was present in 21 patients (46.7%) out of which it was accompanied by enlarged vestibular aqueduct (EVA) and dilated vestibule (Mondini’s dysplasia) in 11 patients (Fig. 2). The second commonest malformation was cochlear hypoplasia which was present in 14 patients (31.1%) out of which it was associated with enlarged vestibular aqueduct in 3 patients. There were 4 patients (8.9%) with common cavity anomaly and 6 patients (13.3%) with incomplete partition type I (IP I) amongst which one patient had an absent cochlear nerve on the right side and thus underwent implant on the left. Besides this there was anomalous facial nerve in one patient with cochlear hypoplasia and intraoperative perilymph oozer was present in 8 patients with EVA and cerebrospinal fluid (CSF) gusher was present in 2 patients with IP I. The type of implant were chosen depending on individual malformation and cochlear duct length. The different types of Med-el electrodes used were standard electrodes (n = 22), medium electrode (n = 13), form electrode (n = 10) (Fig. 3).
Out of the 20 patients with cochlear fibrosis, 7 had pre-lingual bilateral profound hearing loss and 13 had post lingual hearing loss. The average age of patients with cochlear fibrosis was 21 years and male to female ratio was 3:4. The cochlear fibrosis was idiopathic in 14 patients (70%), post-meningitic in 4 patients (20%) and a sequelae of idiopathic sudden sensorineural hearing loss in 2 patients (10%) (Fig. 4). In 17 patients the fibrosis was limited to the basal turn, 2 patients had both apical and middle turn fibrosis and in 1 patient there was fibrosis only in the apical turn (Fig. 5). 16 of these patients were implanted using standard electrodes, 2 medium electrode was used and compressed electrode was used in 2 patients.
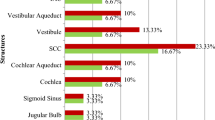
The average age of patients with cochlear ossification was 12 years with a male to female ratio of 6:5. Amongst this 6 patients had prelingual deafness while 8 had postlingual deafness. The etiology for cochlear ossification was idiopathic in 7 patients, post-meningitic in 4 patients, due to cochlear otosclerosis in 1 patient and as a result of sudden SNHL in 2 patients (Fig. 6). Eight patients (57.1%) had a grade 1 ossification out of which 6 had a scala tympani insertion and 2 had scala vestibuli insertion. Two patients (14.3%) had a grade 2 ossification of cochlea who underwent scala vestibuli insertion and 4 patients (28.6%) had a grade 3 ossification in which basal turn drill out was required. Amongst the type of implants used, 7 standard and 1 medium was used in the patients with grade 1 ossification. In grade 2 ossification 2 medium electrodes were used and in patients with grade 3 ossification 3 medium electrode and 1 compressed electrode was used (Table 1). There was displacement of electrode in one patient with grade 3 ossification who underwent revision and was successfully implanted in the second surgery.
Discussion
A number of factors can affect the normal development of the inner ear amongst which the most important are genetic abnormalities and environmental factors such as radiation. They directly affect the membranous labyrinth by decreasing the vascular supply or increasing the pressure inside the inner ear [7]. The first classification system of inner ear anomalies was proposed by Jackler et al. in 1987 which was based on embryogenesis and developmental arrest [8]. He concluded that arrest of development at different weeks produced different anomalies and based on polytomography classified anomalies into five different groups namely Michel deformity, cochlear aplasia, common cavity, cochlear hypoplasia and incomplete partition. However with the advent of radiological techniques this classification underwent further modification and IP I, IP II and subsequently incomplete partition 3 (IP III) or X-linked deafness were added [9].
In a retrospective study by Sennaroglu et al. in which amongst 240 cochlear implants performed there were 20 patients (8.33%) with congenital malformations of the inner ear [10]. In a similar study in the Indian subcontinent by Grover et al. amongst total 323 children who underwent cochlear implantation the incidence of inner ear malformations was 7.43% [11]. In our study amongst 337 patients who underwent cochlear implant, there were 45 patients (16.4%) with malformed cochlea. In the study by Grover et al. the most common anomalies were IP-2 (46.06%) followed by enlarged vestibular aqueduct (35.29%). In our study population the commonest anomaly was IP-II (46.7%) followed by cochlear hypoplasia (31.1%) (Fig. 7).
(a) Showing HRCT temporal bone image of cochlear hypoplasia (yellow arrows) (b) showing MRI images of hypoplastic cochlea (yellow arrows) of a child who was implanted successfully (c) HRCT temporal bone images of a child with absent cochlear nerve on the right with an incomplete partition I type anomaly of cochlea on the left (yellow arrow) who underwent successful implantation on left (d) showing HRCT temporal bone images of a child with Mondini’s deformity who was successfully implanted shows the cochlea with incomplete partition II anomaly (red arrow) (e) shows the associated enlarged vestibular aqueduct (yellow arrow) (f) post-operative Xray skull in trans-orbital showing the implant in situ (black arrow) in a patient with common cavity anomaly of cochlea, (g) Intraoperative image showing the tunnel being drilled in the posterior canal wall using Trifon perforator (h) Intraoperative image showing the cochleostomy (yellow arrow) site in a case of IP II (i) Intraoperative image showing a standard implant inserted through the tunnel into the cochlea (white arrow)
Cochlear implantation in a malformed ear comes with its own set of challenges for the operating team the most commonest being associated abnormal course of facial nerve and CSF gusher. As a result of the inner ear malformation, particularly those involving the lateral semi-circular canal the facial nerve may take an abnormal course thus resulting in a difficult access [10]. A CSF gusher usually arises due to a defect at the lateral end of the internal auditory canal (IAC) and these patients are prone to develop meningitis in the postoperative period. This defect may also cause the electrode array to be inserted into the IAC. Besides this the distribution of neural tissue in inner ear anomalies especially in common cavity is highly unpredictable and thus there is high uncertainity in the final outcome after implantation. This has to be kept in mind during the preoperative counselling of such patients and a guarded prognosis should be explained in such cases. In our series one patient with cochlear hypoplasia had an anomalous facial nerve who was successfully implanted by the transcanal route and the patient had normal facial nerve function in the postoperative period.
There were 8 patients in our series with an intraoperative perilymph oozer all of whom had an enlarged vestibular aqueduct on preoperative imaging. In all the cases the CSF ooze was controlled with packing of the cochleostomy site using soft tissue and none of these patients developed meningitis in the post-operative period. There were also 2 patients with IP-1 who has CSF gushers intraoperatively which was managed successfully with a soft tissue seal and use of electrodes with stopper (Form electrode). Besides all this the inner ear malformations may sometimes be associated with an absent cochlear nerve. We had one such patient with an IP I anomaly who had an absent cochlear nerve on the right side and therefore the patient underwent implant on the contralateral side (Fig. 7). The type of implant inserted was chosen based on the type of malformation, the measured cochlear duct length and the intraoperative presence of a CSF gusher/oozer. The most common implant used in the congenital malformation group was the standard implant followed by medium and form electrode.
Cochlear fibrosis and subsequent ossification are the most common acquired abnormalities of the cochlea. This can arise as a result of a plethora of causes such as meningitis (meningogenic), otitis media (tympanogenic), otosclerosis, autoimmune inner ear disease and also miscellaneous causes such as trauma, labyrinthine artery occlusion, temporal bone tumours and wegener’s granulomatosis [12,13,14,15,16,17,18]. There are two types of neo-ossification in cochlea namely metaplastic and osteoplastic [13]. The metaplastic form seen in meningitis and otitis media comprises of high cellularity, low osteoblasts and ill-defined margins and it is confined to cochlear lumen with endosteal preservation. On the other hand the osteoplastic form which is seen in trauma and otosclerosis causes endosteal disruption leading to new bone formation which is less cellular, lamellar and has clear margins. Otosclerosis can also present with otosclerotic lesions around the cochlea in addition to intracochlear ossification. The area of round window, close to the cochlear aqueduct followed by scala tympani of the basal turn are usually affected first and most severely [19, 20]. However a relatively small population do not follow this pattern and present with isolated patches of ossification only in the middle or apical turns of the cochlea [12]. In a study of 24 human temporal bones by Green et al. 3 temporal bones had a patent round window niche and basal turn, but significant apical and middle-turn ossification [12]. In our study although there were 20 patients with cochlear fibrosis amongst these 2 patients had a patent basal turn with fibrosis of apical and middle turn and 1 patient had isolated fibrosis of apical turn (Fig. 8).
(a) showing the MRI images of a post-meningitic patient with fibrosis of the right proximal basal turn (red arrow) who was successfully implanted (b) Intraoperative picture after a cochleostomy showing new bone formation inside the cochlear lumen (yellow arrow) (c) Postoperative Xray skull in transorbital view showing the compressed electrode in situ (white arrow) in a child with fibrosis of the middle and apical turn of the right cochlea
Cochlear fibrosis and ossification remains a challenge in cochlear implantation due to required modifications of surgical approaches (posterior tympanotomy/transcanal / subtotal petrosectomy), type of electrode arrays to be used (standard/compressed/double array), extend of drilling (Round window niche / basal turn/middle turn/ circum- modioloar drill out) to location and extend of electrode insertion (scala tympani/scala vestibuli and partial/ complete) [18, 21]. Variable postoperative auditory outcomes may be attributed to extend of electrode insertion, higher impedence and charge for electrode and high risk for electrode migration [15, 22, 23].
The advantages of transcanal technique in comparison with the conventional posterior tympanotomy technique is that it provides a panoramic view of the mesotympanum and thus helps in the early identification of round window niche [24,25,26,27,28]. Besides this it helps in the early identification of the limits of the promontory and its relations to the surrounding structures especially in cases where a cochleostomy has to be performed [29]. As mentioned by Sennaroglu et al. transcanal technique is beneficial in hypoplastic cochlea in which the promontory may not have the usual protuberance and it may be difficult to identify promontory and round window through the facial recess [5]. In case of those malformations associated with CSF gusher, the transcanal approach provides a wide access for packing. In cases of cochlear ossification where a drill out is required, it is easy to follow the curve of the basal turn in a transcanal technique versus the posterior tympanotomy in which the access is limited. Some of the cases of cochlear malformations are associated with a high riding jugular bulb which can limit the view of the round window niche through a posterior tympanotomy which can be very easily accessed via a transcanal approach. When posterior tympanotomy is used for the implantation of cochlear malformations usually a modification of the classical technique is required such as extended posterior tympanotomy, anterior transposition of posterior canal or removal of incus. Even while approaching a case of difficult malformation of cochlea via a posterior tympanotomy method, we can elevate the tympanomeatal flap to provide a wider exposure. In those cases of cochlear malformations which has a very narrow facial recess, posterior tympanotomy is often dangerous whereas there is no such hindrance in a transcanal technique. In cases of cochlear hypoplasia where the cochlea is smaller than usual it is possible to do a tympanotomy followed by cochleostomy and insertion of a test device before proceeding with the surgery. Some patients may have grade 2-grade 3 retraction of the tympanic membrane which will impede the view offered by a posterior tympanotomy. In cases with a rotated cochlea, a 2.4 mm endoscope inserted through the canal after elevation of tympanomeatal flap can be used to properly visualize the round window niche.
The transcanal technique is however not without disadvantages, the tympanic membrane can get perforated during the elevation which will need to be reinforced with a temporalis fascia graft. While drilling the tunnel in the posterior canal wall, there can be inadvertent entry into the external auditory canal in which case it should be sealed with bone dust.
Conclusion
Cochlear malformations are no longer a contraindication for cochlear implant if properly evaluated. Team work between radiologists, operating surgeons and audiologists is of utmost importance in the surgical planning and rehabilitation of such patients. Transcanal approach provides good access for the implantation of abnormal cochlea.
Data Availability
Data transparency has been maintained.
References
Jensen S (1969) Malformation of the inner ear in deaf children. Acta Radiol 286(suppl):1–97.
Tucci DL, Telian SA, Zimmerman-Philips S, et al. Cochlear implantation in patients with cochlear malformations. Arch Otolaryngol Head Neck Surg 1995;121:833Y8.
Schmidt JM. Cochlear neuronal populations in developmental defects of the inner ear. Acta Otolaryngol (Stockh) 1985;99:14Y20.
Mangabeira-Albernaz PL. The Mondini dysplasia from early diagnosis to cochlear implant. Acta Otolaryngol 1983;95:627Y 31.
Sennaroğlu L, Bajin MD. Classification and current management of inner ear malformations. Balkan Med J. 2017;34(5):397–411.
Sanna M, Free R, Merkus P, Falcioni M. Surgery for Cochlear and Other Auditory Implants. eds; Stuttgart:Thieme,2016.
Sennaroglu L. Histopathology of inner ear malformations: do we have enough evidence to explain pathophysiology? Cochlear Implants Int. 2016;17(1):3–20.
Jackler RK, Luxford WM, House WF (1987) Congenital malformations of the inner ear: a classification based on embryogenesis. Laryngoscope 97: 2–14.
Sennaroglu L, Saatci I, Aralasmak A, Gursel B, Turan E (2002) Magnetic resonance imaging versus computed tomography in pre-operative evaluation of cochlear implant candidates with congenital hearing loss. Journal of Laryngology and Otology 116: 804–810.
Sennaroglu L, Sarac S, Turan E (2006) Surgical results of Cochlear Implantation in Malformed Cochlea. Otology & Neurotology 27: 615–623.
Grover M, Sharma S, Bhargava S, Singh SN, Gupta G, Sharma MP. Cochlear implantation in children with anomalous Cochleovestibular anatomy: our experience. Indian J Otolaryngol Head Neck Surg. 2017;69(4):504–508.
Green JD Jr, Marion MS, Hinojosa R. Labyrinthitis ossificans: histopathologic consideration for cochlear implantation. Otolaryngol Head Neck Surg 1991;104:320–6.
Kotzias SA, Linthicum FH Jr. Labyrinthine ossification: differences between two types of ectopic bone. Am J Otol 1985;6:490–4.
Kaya S, Paparella MM, Cureoglu S. Pathologic findings of the cochlea in labyrinthine ossificans associated with the round window membrane. Otolaryngol Head Neck Surg 2016;155:635–40.
Wang L, Zhang D. Surgical methods and postoperative results of cochlear implantation in 79 cases of ossified cochlea. Acta Otolaryngol 2014;134:1219–24.
Rottoveel LJ, Proops DW, Ramsden RT, Saeed SR, van Olphen AF, Mylanus EA. Cochlear implants in 53 patients with otosclerosis: demographics, computed tomographic scanning, surgery and complications. Otol Neurotol 2004;25:943–52.
Bacciu A, Pasanisi E, Di Lella F, Guida M, Bacciu S, Vincenti V. Cochlear implantation in patients with Cogan syndrome: long term results. Eur Arch Otorhinolaryngol 2015;272:3201–7.
Coelho DH, Roland JT Jr. Implanting obstructed and malformed cochleae. Otolaryngol Clin North Am 2012;45:91–110.
Nabili V, Brodie HA, Neverov NI, Tinling SP. Chronology of labyrinthitis ossificans induced by Streptococcus pneumoniae meningitis. Laryngoscope. 1999;109(6):931–5.
Tinling SP, Colton J, Brodie HA. Location and timing of initial osteoid deposition in postmeningitic labyrinthitis ossificans determined by multiple fluorescent labels. Laryngoscope. 2004;114(4):675–80.
Sanna M, Free R, Merkus P, et al. Surgery for Cochlear and other auditory implants. Stuttgart: Georg Thieme Verlag; 2016.
Durisin M, Buchner A, Lesinski-Schiedat A, Bartling S, Warnecke A, Lenarz T. Cochlear implantation in children with bacterial meningitic deafness: the influence of the degree of ossification and obliteration on impedance and charge of the implant. Cochlear Implants Int 2015;16:147–58.
Connell SS, Balkany TJ, Hodges AV, Telischi FF, Angeli SI, Eshraghi AA. Electrode migration after cochlear implantation. Otol Neurotol 2008;29:156–9.
Sennaroglu L, Aydin E (2002) Anteroposterior approach with split ear canal for cochlear implantation in severe malformations. Otology & Neurotology 23: 39–43.
Weber BP, Dillo W, Dietrich B, Maneke I, Bertram B, Lenarz T (1998) Pediatric cochlear implantation in cochlear malformations. American Journal of Otology 19: 747–753.
Jain R, Tiwari P, Kumar S, Mishra P, Pearly PK, Keshri A. A clinico-radiological study: Veria technique of Cochlear Implant-A Study of 50 cases. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 2):1553–1561.
Hans JM, Prasad R. Cochlear Implant surgery by the Veria technique: how and why? Experience from 1400 cases. Indian J Otolaryngol Head Neck Surg. 2015;67(2):107–109.
Singhal P, Nagaraj S, Verma N, et al. Modified Veria technique for Cochlear Implantation by Postaural Approach. Indian J Otolaryngol Head Neck Surg. 2020;72(3):370–374.
Kiratzidis T (2000) ‘Veria operation’: cochlear implantation without a mastoidectomy and a posterior tympanotomy. A new surgical technique. Advances in Otorhinolaryngology 57: 127–130.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors made substantial contribution to this paper and all the authors have approved the version to be published.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institution ethics committee.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
The participants have consented to the submission of the case details for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hameed, N., Keshri, A., Manogaran, R.S. et al. Cochlear Implantation by Veria Technique in Abnormal Cochlea: Our Experience. Indian J Otolaryngol Head Neck Surg 76, 2646–2653 (2024). https://doi.org/10.1007/s12070-024-04492-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04492-3