Abstract
Background
Otoacoustic Emission (OAE) is frequently recorded in various body positions for infants. However, little is available about whether these deviations will produce non-pathological effects on the clinical results. The current study assessed body position’s effect on infants’ inner ear function.
Methods
Sixty normally hearing infants participated in an analytical cross-sectional study. Distortion-product OAEs (DPOAEs) were measured in the supine, side-lying, and upright positions. The DPOAE amplitude and signal-to-noise ratio (SNR) were recorded across the 1500 to 6000 Hz range.
Results
The mean DPOAE amplitude and SNR values were significantly greater in the upright position than supine and side-lying positions (p < 0.05). These differences were more pronounced in the 3000 to 6000 Hz range. The effects of gender and ear asymmetry on DPOAEs were not statistically significant.
Conclusion
Our findings suggested that the upright position could be regarded as the best position for assessing DPOAEs in infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Otoacoustic emissions (OAEs) are by-products of active processes in the cochlea and provide a non-invasive measure of cochlear amplification. These sounds can be measured, either spontaneously or evoked by an acoustic stimulus, through a highly sensitive microphone located in the external auditory canal. In recent years, OAEs have received widespread acceptance for various clinical applications, including identification of cochlear dysfunction, hearing screening, and site of lesion assessment [1,2,3,4,5].
There are pathological (e.g., ototoxicity), non-pathological (e.g., age), instrumental, and environmental (e.g., noise level) factors that may influence the OAE responses [6,7,8,9,10]. However, the impact of body position as a non-pathological factor has received less attention. The effects of body position on the outcomes of other audiological measurements, such as sound localization, hearing thresholds, and middle ear measurements, have been well documented [11,12,13,14,15]. The proposed mechanism for these alternations in auditory function is thought to be an increase in intracranial pressure (ICP) level and, consequently, intracochlear pressure (ICoP) reflected in the cochlea, leading to increased stiffness in the middle ear system through the outward motion of the stapes footplate. Therefore, a change in body position and the subsequent changes in ICP could induce concomitant changes in the forward transmission of auditory stimuli and backward transmission of ear emissions [16,17,18,19].
OAEs are usually assessed in an upright (e.g., sitting) position, but it is not uncommon for OAE testing to be conducted with the subject in a supine or even side-lying orientation. The latter test positions (i.e., supine and side-lying) are generally utilized with newborns and infants, or patients who cannot be seated upright because of medical conditions. The present study was conducted to determine the impacts of postural changes on the DPOAEs in infants with normal hearing levels.
Materials and Methods
Participants
During an analytical cross-sectional design, 60 infants (32 boys and 28 girls) were recruited. All selected infants were full-term babies (38 weeks of gestational age or older) with no risk factors for hearing loss, as identified by the Joint Committee on Infant Hearing (2007). All infants were required to pass an automated auditory brainstem response (AABR) test to be included in the present study. A “pass” response in the AABR test is necessary to exclude neonates with significant hearing loss, which may influence the interpretation of OAE findings.
The institutional ethics committee reviewed and approved the experimental design of the current study. Written parental consent was obtained before the commencement of the assessment.
Procedure
Otoscopy and tympanometry (MADSEN OTOFlex 100, GN-Otometrics) assessments were conducted before testing OAEs to exclude obstruction of the external auditory canal and middle-ear effusion. DPOAE analysis was performed using the ERO-SCAN system (MAICO Co., Germany), connected to a personal computer. DPOAE responses were elicited using a pair of primaries at f2/f1 = 1.2, L1 = 65 dB SPL, and L2 = 55 dB SPL. DPOAEs were measured at six frequencies, including 1500, 2000, 3000, 4000, 5000, and 6000 Hz. All participants had an amplitude higher than − 5 dB and a signal-to-noise ratio (SNR) higher than 6 dB across different frequencies. DPOAE measurement was conducted three times for each ear, with the infant in 3 different positions: “supine”, “upright” (head-raised), and “side-lying” (one-sided). These test positions were chosen because they are common positions for infants to be placed in during testing. The time delay between testing in each position was controlled (using a 30-second interval) to stabilize the emissions and avoid any potential order effects on the results. After every posture change, the probe was reinserted into the external auditory canal to ensure optimal testing conditions.
Statistical Analysis
Statistical analyses were conducted utilizing SPSS v.21.0. Numerical variables were expressed as mean, and standard deviation (SD), and categorical variables were expressed as numbers or percentages. A multivariate analysis of variance (ANOVA) was carried out to investigate the impact of body position on DPOAE parameters (SNR and amplitude) at each of the f2 frequencies. When Mauchly’s Sphericity test indicated sphericity violations, the Greenhouse-Geisser correction was used. Furthermore, a Tukey post-hoc test was used for pairwise comparisons when initial analysis showed a significant main effect. A p-value of < 0.05 was considered statistically significant.
Results
The mean age of the participants was 4.32 (± 3.24) months. For analysis of DPOAE parameters, a three-way ANOVA was conducted with the within-subject variables of body position (three levels: side-lying, supine, and upright) and frequency (five levels: 1500, 2000, 3000, 4000, and 6000 Hz) and between-subjects variable of gender (two levels: girls and boys).
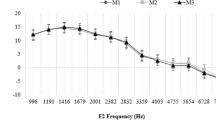
Table 1 shows the mean DPOAE amplitudes across different test positions. For the main outcome parameters, the ANOVA test exhibited a significant main effect for body position (p < 0.001) and frequency (p = 0.032) but not for body position × frequency interaction effect (p = 0.651). Post-hoc comparisons of DPOAE amplitudes across different positions indicated that DPOAEs were generally higher when infants tested in the head-raised (upright) position. This effect was insignificant for the f2 test frequencies of 1500 and 2000 Hz. The interaction effects between body position and gender, and between frequency and gender were not statistically significant (p > 0.05).
Table 2 shows the mean DPOAE SNR values across three different body positions. The ANOVA demonstrated a significant main effect for body position (p < 0.001) and frequency (p < 0.001) but not for body position × frequency (p = 0.153). Post-hoc comparisons of SNR values in different body positions exhibited that mean SNRs were generally higher in upright than supine and side-lying positions. This effect was more pronounced for the f2 test frequencies of 3000 and 4000 Hz. Furthermore, the effects of gender on DPOAE SNR in different positions did not reach a statistically significant level (p > 0.05).
Discussion
The main objective of our study was to assess postural changes’ effects on cochlear function using DPOAEs in full-term infants with normal hearing sensitivity. Our findings showed that the non-pathological factor of body position significantly affected the DPOAEs.
Analysis of the DPOAE amplitude demonstrated that the largest and smallest amplitudes were recorded in the upright and side-lying positions, respectively. We found that the influence of body position was not uniform across the f2 frequency range. The DPOAE amplitudes were higher in the mid frequencies (1500 and 2000 Hz). Our results also indicated that the mean SNR values were significantly greater in the supine orientation than in side-lying and upright positions for the mid frequencies 1500 and 2000 Hz.
Our findings suggest that infants produced stronger emissions in upright position than the other test positions. Buki et al. [20] studied the effects of postural changes on transient-evoked OAEs (TEOAEs). Their results exhibited that following a downward posture change, the TEOAE phase may increase, and the TEOAE amplitude may decrease, especially for frequency regions below 2000 Hz. They proposed OAEs as a non-invasive approach for monitoring alternations in intracranial pressure through stapes displacements. In another study, de Kleine et al. [21] showed that the amplitude, width, and frequency of the spontaneous OAE (SOAE) spectrum changed in positive and negative directions in response to positional changes (from upright to a recumbent head-down orientation), with these changes being most obvious at frequencies less than 2000 Hz.
The inner ear fluid is connected to the CSF via the endolymphatic duct. Therefore, changes in pressure of the cerebrospinal fluid in the subarachnoid produce changes in hydrostatic ICoP. As the elevations in ICP lead to elevations in the ICoP level, at least two different mechanisms have been proposed to explain OAE alternations following postural changes. Firstly, the ICoP may alter cochlear responses by acting directly on the sensory cells. Secondly, the ICoP may change the stiffness of the middle ear annular ligament that connects the ossicular chain (i.e., stapes) to the oval window of the inner ear [16, 22,23,24].
According to our results, the most prominent alternations on DPOAEs occurred at mid frequencies (≤ 2000 Hz). Histological findings have also demonstrated that the cochlear aqueduct is rather narrow (about 0.1 mm) and is filled with loose connective tissue, and is thus probably to transmit low- and mid-frequency waves from the CSF to cochlear compartments.
Conclusion
The present study revealed that the non-pathological factor of body position significantly influences cochlear function. Our findings support this notion that testing neonates in an upright orientation may produce stronger emissions, especially in the mid-frequency range.
References
Saki N, Bayat A, Hoeinabadi R, Nikakhlagh S, Karimi M, Dashti R (2017) Universal newborn hearing screening in southwestern of Iran. Int J Pediatr Otorhinolaryngol 97:89–92
Shetty S, Bhandary SK, Bhat V, Aroor R, Shetty J, Dattatreya T (2023) Role of otoacoustic emission in early detection of cisplatin induced ototoxicity. Indian J Otolaryngol Head Neck Surg 74(Suppl 1):164–169
Kondziella D, Jensen AM, Hjuler T, Bille M, Kjaergaard J (2018) Otoacoustic emissions for outcome prediction in postanoxic brain injury. Front Neurol 9:706
Shera CA (2004) Mechanisms of mammalian otoacoustic emission and their implications for the clinical utility of otoacoustic emissions. Ear Hear 25:86–97
Rai N, Yashveer JK (2022) Role of Otoacoustic Emission Test in early diagnosis of hearing impairment in infant. Indian J Otolaryngol Head Neck Surg 74(Suppl 3):4258–4263
Ferreira Penêda J, Barros Lima N, Ribeiro L, Helena D, Domingues B, Condé A (2018) Cochleotoxicity monitoring protocol. Acta Otorrinolaringol Esp 69(2):105–109
Manley GA (2022) Otoacoustic emissions in non-mammals. Audiol Res 12(3):260–272
Shetty S, Bhandary SK, Bhat V, Aroor R, Shetty J, Dattatreya T (2022) Role of Otoacoustic Emission in early detection of Cisplatin Induced Ototoxicity. Indian J Otolaryngol Head Neck Surg 74(Suppl 1):164–169
Fukai N, Shyu, Driscoll C, Kei J (2005) Effects of body position on transient evoked otoacoustic emissions: the clinical perspective. Int J Audiol 44:8–14
Vaden KI Jr, Matthews LJ, Dubno JR (2018) Transient evoked otoacoustic emissions reflect audiometric patterns of age-related hearing loss. Trends Hear 22:2331216518797848
Lackner JR (1974) Changes in auditory localization during body tilt. Acta Otolaryngol 77:19–28
Buki B, Chomicki A, Dordain M (2000) Middle ear influence on otoacoustic emissions: contributions of posture and intracranial pressure. Hear Res 140:189–201
Bershad EM, Urfy MZ, Pechacek A, McGrath M, Calvillo E, Horton NJ, Voss SE (2014) Intracranial pressure modulates distortion product otoacoustic emissions: a proof-of-principle study. Neurosurgery 75:445–454
Loiselle AR, de Kleine E, van Dijk P, Jansonius NM (2018) Noninvasive intracranial pressure assessment using otoacoustic emissions: an application in glaucoma. PLoS ONE 13:e0204939
Kei J, dah Mazlan R, Chall Kim SC, Pont J, Schilt SA, Sewak R et al (2012) High frequency tympanometry findings in neonates: does it depend on head position? Int J Audiol 51:475–479
Voss SE, Horton NJ, Tabucchi TH, Folowosele FO, Shera CA (2006) Posture induced changes in distortion-product otoacoustic emissions and the potential for non-invasive monitoring of changes in intracranial pressure. Neurocrit Care 4:251–257
Voss S, Adegoke M, Horton N, Sheth K, Rosand J, Shera C (2010) Posture systematically alters ear-canal reflectance and DPOAE properties. Hear Res 263:43–51
Williams MA, Malm J, Eklund A, Horton NJ, Voss SE (2016) Distortion product otoacoustic emissions and intracranial pressure during CSF infusion testing. Aerosp Med Hum Perform 87:844–851
Ezerarslan H, Beriat GK, Nurhat RH, Kazancı B, Çelikkan FT, Sabuncuoğlu B et al (2016) Non-invasive detection and monitoring of experimental hydrocephalus with distortion product otoacoustic emissions. Auris Nasus Larynx 43(4):404–411
Buki B, Avan P, Lemaire JJ, Dordain M, Chazal J, Ribári O (1996) Otoacoustic emissions: a new tool for monitoring intracranial pressure changes through stapes displacements. Hear Res 94(1–2): 125 – 39
de Kleine E, Wit HP, van Dijk P, Avan P (2000) The behaviour of spontaneous otoacoustic emissions during and after postural changes. J Acoust Soc Am 107:3308–3316
Buki B, de Kleine E, Wit HP, Avan P (2002) Detection of intracochlear and intracranial pressure changes with otoacoustic emissions: a gerbil model. Hear Res 167:180–191
Yucel E, Ardıç FN, Tümkaya F, Kara CO, Topuz B (2020) Detecting intralabyrinthine pressure increase by postural manipulation with wideband tympanometry and distortion product otoacoustic emission. Turk Arch Otorhinolaryngol 58(4):203–207
Atcherson SR, Mattheis A (2011) Distortion product otoacoustic emissions: body position effects with simultaneous presentation of tone pairs. Audiol Res 1(2):e29
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Guidelines
The current study was approved by the local ethical committee (registration number: IR.AJUMS.REC.1402.356). Informed consent was obtained from all parents.
Financial Support and Sponsorship
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of Interest
The authors declare that they are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bayat, A., Saki, N. & Mirmomeni, G. Effects of Body Position on Cochlear Function in Infants: An Otoacoustic Emission Study. Indian J Otolaryngol Head Neck Surg 76, 934–937 (2024). https://doi.org/10.1007/s12070-023-04327-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04327-7