Abstract
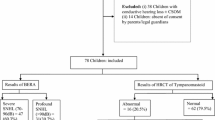
(1) To find the presence of middle ear diseases present in the patients with congenital bilateral severe to profound SNHL (2) If it poses as a threat to rehabilitative efforts for the existing severe to profound SNHL. Study setting: Department of ENT, C U Shah medical college and hospital. Study design: Prospective study Study population: Patients attending ENT department with complaints of congenital bilateral severe to profound sensorineural hearing loss. A total of 50 cases were studied during the study period. Methods of data collection: The Proforma was designed based on objective of the study. Detailed history was taken followed by thorough ENT and systemic examinations. Otoscopy and otoendoscopy were carried out and all patients were subjected to hearing tests consisting of Pure Tone Audiometry (PTA), Impedance Audiometry (IA), Brainstem Evoked Response Audiometry (BERA) and Oto Acoustic Emissions (OAE). HRCT and MRI scanning of temporal bones of all the patients was included as a part of the routine workup. Out of the 50 children with bilateral congenital hearing loss studied in this study, 13(26%) children were observed to have concurrent middle ear pathologies. 2 patients had bilateral retracted drum with tympanosclerosis; 3 had bilateral retraction pocketswith mastoiditis; 1 had bilateral SOM; 1 had right SOM and left retracted drum; 2 had bilateral PSQ cholesteatoma; 1 had left SOM and right sided tympanic membrane perforation, 3 had right sided tympanic membrane perforation with left sided normal ears. Children with congenital bilateral severe to profound hearing loss should be examined for middle ear pathologies, which can most often be overlooked otherwise, hence rendering the patient unfit for definitive management of the severe to profound SNHL in the form of Hearing Aid trial or Cochlear Implantation, further delaying the development of speech. Hence, all children with congenital bilateral severe to profound hearing loss should undergo regular screening for assessment of middle ear pathologies with prompt treatment when any middle ear pathology is encountered, therefore rendering the patient fit for fitting of cochlear implantation at the earliest possible to decrease permanent impairment of speech.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Permanent childhood hearing impairment (PCHI) includes hearing impairment that results from a structural abnormality in the outer ear, middle ear as well as sensorineural hearing loss. Permanent childhood hearing impairment (PCHI) is defined as a confirmed permanent bilateral hearing impairment ≥ 40 dB HL (hearing level) averaged over the frequencies of 0.5, 1, 2 and 4 kHz in the better hearing ear. A PCHI can be conductive, sensorineural or mixed. The onset of hearing loss may be prenatal, peri-natal or postnatal. The aetiology may be congenital or acquired.
The hearing loss may occur before (pre-lingual deafness) or after the child has acquired the ability to speak (post-lingual deafness). This distinction has important implications for education and management. Early identification and appropriate audiological, medical and educational intervention will help maximize the child’s potential.
Identifying and understanding the consequences of associated medical conditions, impairments and disabilities is also extremely important to provide the best opportunity for the child and the parents to make informed choices and plans for the future.
Earlier identification with universal new-born hearing screening is now practised in many developing -and most developed- countries. Improved audiological assessment techniques have provided a unique opportunity to confirm the exact nature and extent of the hearing loss within 8 weeks of birth, leading to very early rehabilitation with precise amplification and with diagnostic verification using well-developed and internationally agreed techniques. Improved knowledge and understanding of aetiologies has made it possible to provide better information on the nature of the hearing loss, preventing deterioration in some cases and aiding identification of other system involvement, for example, retinitis pigmentosa in Usher syndrome and enlarged vestibular aqueduct in Pendred syndrome. Early confirmation of hearing loss, early amplification, early assessment of benefit from hearing aids, early understanding of important medical and aetiological factors, and early cochlear implantation have all led to much better audiological, educational and longer-term outcomes. This progress depends on multidisciplinary working, agreed professional guidelines, and the involvement of families and those with a hearing loss themselves. Hearing loss in a child may be present at birth (‘ Congenital’) or may develop after birth (‘acquired’). Management of a child with confirmed PCHI requires a wholistic approach for optimal audiological care with supporting services for the child and the family and also appropriate medical management, which includes offering and arranging necessary investigations to determine the aetiology. Most children with a PCHI have a Sensorineural Hearing Loss (SNHL). Those children who have a purely conductive hearing loss may have some congenital conditions, such as ossicular abnormalities and bilateral aural atresia. Some may have a mixed hearing loss; many have a fixed loss but others have a progressive hearing loss. In children, especially during the first 5–6 years of life, acute otitis media (AOM) and middle ear effusions (‘glue ear’) are common with a much greater prevalence than PCHI. Children with PCHI especially with craniofacial abnormalities are also vulnerable to AOM and to middle ear effusions, making their hearing loss temporarily worse.
There is no proven or recommended treatment or cure for SNHL; management of hearing loss is usually by hearing strategies and hearing aids. In cases of profound or total deafness, a cochlear implant or a hearing aid may restore a functional level of hearing.
Otitis media either suppurative or non-suppurative is common in children in the developing countries. If these problems affect children with sensorineural hearing loss (SNHL), it will eventually delay the treatment options like hearing aids or cochlear implants or may aggravate the present hearing loss.
If any middle ear disease is present, cochlear implantation is not done, as it could lead to serious complications like labyrinthitis, meningitis and dreaded complication like extrusion of implant and hence it is strongly recommended to not perform implantation until middle ear pathology is completely cured.
Otitis media is one of the most common infectious diseases of childhood. The peak incidence of middle ear disease in children was noted to occur during the second 6 months of life with a second lesser peak noted between 4 and 5 years of age. Males were found to be at greater risk for otitis media than females and recurrent acute otitis media in a sibling was a strong predictor of recurrent otitis media in a study child. So, risk features for recurrent otitis media in children are male gender, sibling history of recurrent otitis media, early occurrence of the infection, not being breast fed, being in group day care, and exposure to smoke in the household. The etiologic correlates of SNHL, such as perinatal high risk factors, craniofacial anomalies and genetic disorders may place at least some children with SNHL at an increased risk for otitis media with effusion. So, close audiological follow up is essential for effective treatment of children with SNHL.
The aim of this study is to know the prevalence of middle ear problems in children with bilateral SNHL among the children presenting at ENT OPD of C U Shah medical college with congenital bilateral severe to profound hearing loss for the candidacy of cochlear implantation.
The study aims at finding the different types of middle ear pathologies encountered in these children, and if it poses as a threat to the rehabilitative efforts for the congenital bilateral severe to profound hearing loss.
Methods
Study Setting
This study was carried out in the department of ent, c u shah medical college and hospital.
Study Duration
3 years
Study Design
Prospective study.
Study Population
Patients attending ENT department in C U Shah medical college and hospital and also patients referred from other department in the same hospital with complaints of congenital bilateral severe to profound sensorineural hearing loss. A total of 50 cases were studied during the study period.
Inclusion Criteria
-
(1) Children under the age of 6 years.
-
(2) Children with bilateral severe to profound hearing loss.
-
(3) Children presenting to the outpatient department of CUSMC, Surendranagar for candidacy of cochlear implantation.
Exclusion Criteria
None.
Methods of Data Collection
The Proforma was designed based on objectives of the study. And it was pretested and used after modification. As per proforma detailed history was taken followed by thorough ENT and systemic examination and clinical diagnosis was arrived in support with the relevant investigations.
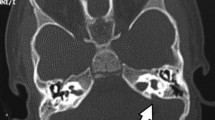
Otoscopy and oto-endoscopy were carried out in all 50 patients as a part of local examination. All patients were subjected to hearing tests consisting of Pure Tone Audiometry (PTA), Impedance Audiometry (IA), Auditory Steady State Response (ASSR), Brainstem Evoked Response Audiometry (BERA) and Oto Acoustic Emissions (OAE). HRCT and MRI scanning of temporal bones of all the patients was included as a part of the routine workup.
Working Indices and Analysis of Data
Thus, obtained data was analysed with the aid of calculator and presented in the forms of tables, figure, graphs and diagrams wherever necessary.
Results
All the children in the study were subjected to audiometric evaluation with BERA and PTA and were found to have bilateral severe to profound sensorineural hearing loss. The purpose of this study, is to find out middle ear disease in children with congenital bilateral severe to profound hearing loss. As shown in Table 1, out of the 50 children with bilateral congenital hearing loss studied in this study, 13(26%) children were observed to have concurrent middle ear pathologies. A variety of middle ear pathologies were encountered, the description of which has been done in further analysis. The middle ear diseases were diagnosed based on otoscopy findings with concurrent relevant findings on tympanograms and HRCT scans of temporal bones carried out as a part of the routine workup.
Table 2 depicts that the 13 patients were diagnosed to have middle ear diseases based on otoscopic and oto-endoscopic findings. 2 patients had bilateral retracted drum with tympanosclerosis; 3 had bilateral retraction pockets with mastoiditis; 1 had bilateral SOM; 1 had right SOM and left retracted drum; 2 had bilateral PSQ cholesteatoma; 1 had left SOM and right sided tympanic membrane perforation, 3 had right sided tympanic membrane perforation with left sided normal ears. Chi square test revealed a value of 16.49, with a p value of 0.0009 showing a strong association of middle ear pathologies and otoscopic findings.
The different types of middle ear diseases encountered are shown in Table 3.Out of the 13 patients diagnosed with middle ear diseases, 2 (15.38%) patients had bilateral inactive squamous COM, 3 (23.08%) patients had bilateral inactive squamous COM (retraction pockets) with chronic mastoiditis, 1 (7.69%) had bilateral SOM with chronic mastoiditis, 1 (7.69%) had right sided SOM(secretory otitis media) with left sided inactive Squamous COM, 2 (15.38%) had bilateral active squamous COM (cholesteatoma), 1 (7.69%) had right active mucosal COM (tympanic membrane perforation) and left SOM (secretory otitis media), 2(15.38%) have right active mucosal COM with mastoiditis, 1 (7.69%) had right inactive mucosal COM (dry old pars tensa perforation).
Discussion
The purpose of this study, is to find out middle ear disease in children with congenital bilateral severe to profound hearing loss. All the children in the study were subjected to audiometric evaluation with BERA and PTA and were found to have bilateral severe to profound sensorineural hearing loss. Out of the 50 children with bilateral congenital hearing loss evaluated in this study, 13(26%) children were observed to have concurrent middle ear pathologies. The middle ear diseases were diagnosed based on otoscopy findings with concurrent relevant findings on tympanograms and HRCT scans of temporal bones carried out as a part of the routine workup. Brookhouser et al. [1] studied 437 children with sensorineural hearing loss, and found middle ear pathologies in 71.6% children, out of which, 36.4% suffered from some middle ear disease which resolved with medical therapy and 35.2% had middle ear diseases refractory to medical treatment. K.-E.A. Abou-Elhamd et al. [2] discovered that 70% of cases were normal, 25% had middle ear problem with intact tympanic membrane and 5% had chronic suppurative otitis media with perforation. The prevelance of middle ear disease has been evaluated and documented in a large number of studies. Tos and co workers [3] found that the prevalence of abnormal tympanograms(type B and C) ranged from 10% in neonates to 60% by the age of 12 months in a large study cohort. Teele and his colleagues [4] studied the epidemiology of otitis media in young children among age up to 7 years and reported 62% of children had a bout of otitis media before 1 years of age and 83% had experienced at least one episode of otitis media by the age of 3 years. The peak incidence was noted during the second six months of life with a second peak at the age of 4–5 years. Stool et al. [5] in 1980 evaluated 446 patients between the ages 2 to 21 years and found 85 middle ear pathologies, suggesting 29% of patients had middle ear problems at some time during that period. Out of these, 8% had middle ear effusion and/or otorrhoea. Twenty-one percent patients had high negative pressure, 26% had residual middle ear disease and 1% had inactive disease. Compared to above studies,Brooks et al. [6] reported a lower percentage 20%, in 1974. A higher percentage (57%) was reported by Das in 1990 [7].
Out of the 13 patients diagnosed with middle ear diseases, 2 (15.38%) patients had bilateral inactive squamous COM (retraction pockets in pars flaccida with tympanosclerosis), 3 (23.08%) patients had bilateral inactive squamous COM (retraction pockets) with chronic mastoiditis, 1 (7.69%) had bilateral SOM with chronic mastoiditis, 1 (7.69%) had right sided SOM(secretory otitis media) with left sided inactive Squamous COM, 2 (15.38%) had bilateral active squamous COM (cholesteatoma), 1 (7.69%) had right active mucosal COM (tympanic membrane perforation) and left SOM (secretory otitis media), 2(15.38%) have right active mucosal COM with mastoiditis, 1 (7.69%) had right inactive mucosal COM (dry old pars tensa perforation). According to K.-E.A. Abou-Elhamd et al. [2], on otoscopic examination and after doing audiograms and tympanograms of patients, 70% of cases were normal, 25% had otitis media with intact tympanic membrane and 5% had otitis media with perforation. The patients with SOM and retraction underwent medical management also with the correction of underlying pathology and the patients with cholesteatoma, tympanic membrane perforation underwent surgical management before they could be treated with cochlear implantation and this was found to significantly delay the definitive treatment for the underlying congenital severe to profound hearing loss.
Conclusion
On observing the various type of middle ear diseases encountered in children with bilateral congenital severe to profound hearing loss in this study, 26% children in study were found with ongoing middle ear pathologies at the time of examination.
On otoscopy, 4 children had retracted drums and 4 had tympanic membrane perforation hence making the commonest otoscopy finding encountered in children with congenital bilateral severe to profound hearing loss.
The most common middle ear pathology encountered during this study was otitis media with acute or chronic mastoiditis, with Secretory otitis media being a close second. 2 patients were found to have cholesteatoma in the postero superior quadrant and were planned for immediate surgical management of the same.
If any middle ear disease is present, cochlear implantation is not done, as it could lead to serious complications like labyrinthitis, meningitis and dreaded complication like extrusion of implant and hence it is strongly recommended not to perform implantation until middle ear pathology is completely cured.
Hence, based on all the above observations, it can be summarized that children with congenital bilateral severe to profound hearing loss should be examined for middle ear pathologies, which can most often be overlooked otherwise, hence rendering the patient unfit for definitive management of the severe to profound SNHL in the form of Hearing Aid trial or Cochlear Implantation, thus further delaying the development of speech. Hence, all children with congenital bilateral severe to profound hearing loss should undergo regular screening for assessment of middle ear pathologies with prompt treatment when any middle ear or any concurrent nasal pathology is encountered, therefore rendering the patient fit for fitting of cochlear implantation at the earliest possible to decrease permanent impairment of speech.
References
Brookhouser PG, Worthington DW, Kelly WJ (1993) Middle ear disease in young children with sensorineural hearing loss. Laryngoscope 103:371–378
Abou-Elhamd * KEA, Moussa AE, Soltan MAE (2006) Prevalence of middle ear pathologies in children with bilateral sensorineural hearing loss. Int J Pediatric Otorhinolaryngol 70(6):1081–1084
Tos M, Poulsen G, Hancke AB (1979) Hancke screening tympanometry during the first year of life. Acta Oto-Laryngologica 88:388–394
Teele DW, Klein JO, Rosner BA et al (1989) Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective cohort study. J Infect Dis 160:83–94
Stool SE, Craig HB, Laird MA (1980) Screening for middle ear disease in a school for the deaf. Ann. Otol. Rhinolaryngol. 68(3):172–177
Brooks DN (1974) Impedance bridge studies on normal hearing and hearing impaired children. Acta Otorhinolaryngol Belg 28:140–145
Das VK (1990) Prevalence of otitis media with effusion in children with bilateral sensorineural hearing loss. Arch Dis Childhood 65:757–759
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dhingani, G., Jadav, B. A Study of Middle Ear Diseases in Children with Congenital Bilateral Severe to Profound Sensorineural Hearing Loss. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 4276–4280 (2022). https://doi.org/10.1007/s12070-021-02864-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02864-7