Abstract
Objective
To describe the operative findings and surgical results of unilateral congenital middle ear malformations with intact external ear.
Methods
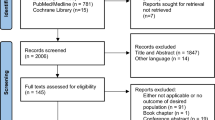
A retrospective review was performed on 64 patients with unilateral congenital middle ear malformations and intact external ear who underwent exploratory tympanotomy from 2011 to 2016. Demographic data, clinical data, high-resolution computed tomography findings, audiometric data and intraoperative findings were collected. Audiological evaluations before and 6 months after surgery were analyzed in 47 patients.
Results
The most common malformation were mobile stapes with missing incus long process and stapes suprastructure. The air conduction pure tone average was 58.9 ± 10.5 dB HL (range 34.4–78.1 dB HL) preoperatively and 28.8 ± 10.6 dB HL (range 9.4–55.6 dB HL) postoperatively (P = 0.000). Twenty-five cases (53.2%) acquired an air conduction hearing gain exceeding 30 dB. Mean air-bone gap (ABG) was 44.5 ± 9.4 dB (range 22.5–66.4 dB HL) before surgery and 15.6 ± 9.3 dB (range 0–35.6 dB) after surgery (P = 0.000) for an average gain of 28.8 ± 11.5 dB. Thirty-four cases (72.3%) showed a postoperative ABG of less than 20 dB, 15 had an ABG within 10 dB, and 4 had 0 dB ABG after operation. No significant difference was observed for air conduction hearing gain regarding age (P = 0.261) or types of malformations (mobile stapes footplate with or without a suprastructure anomaly, P = 0.058).
Conclusion
Unilateral congenital middle ear malformations with intact external ear can be complex and diverse. Functional ossiculoplasty for patients with unilateral congenital middle ear malformations can achieve good hearing outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital ear malformations can be broadly divided into major and minor ear anomalies. Congenital malformations of the middle ear with intact external ear belong to minor ear anomalies, which are restricted to the middle ear without involving the external meatus or auricle. There have been numerous reports on minor ear malformations [1,2,3,4]. However, there are few reports on unilateral minor ear anomalies in the literature. Non-progressive and conductive hearing loss can lead to diagnostic difficulties. Generally, diagnosis is easier in bilateral malformations than that in unilateral types. Therefore, the most efficient method of accurate diagnosis is exploratory tympanotomy.
The main goal of this study was to describe intraoperative findings and to evaluate surgical hearing outcomes in unilateral congenital middle ear malformations with intact external ear.
Materials and methods
Patients with unilateral congenital middle ear malformations who had undergone exploratory tympanotomy from 2011 to 2016 were identified for a retrospective review study. The diagnostic process involved clinical examination, audiometric testing, high-resolution computed tomography (HRCT) and finally confirmation by exploratory tympanotomy. All of the patients had a history of non-progressive hearing loss caused by middle ear malformations with no external meatus or auricle anomalies. Patients with inflammatory conditions, bilateral hearing loss, progressive hearing loss, inner ear anomaly, head injury and previous history of otologic surgeries were excluded from this study. A total of 64 patients with diagnosis confirmed by exploratory tympanotomy were included. All the procedures were done under microscopic view. Demographic data, age of deafness diagnosis, age at surgery, types of malformations, ossiculoplasty and hearing outcomes were collected. The postoperative follow-up was longer than 6 months. Pre- and postoperative audiologic results were compared in 47 patients with complete data sets.
Surgical methods
All patients underwent exploratory tympanotomy via an endaural incision. The anatomy of the ossicular chain and facial nerve was carefully assessed, especially their relations to each other. Types of ossiculoplasty were chosen based on the surgical findings in a particular patient. Partial ossicular replacement prostheses (PORP, Fig. 1), autologous incus and total ossicular replacement prostheses (TORP, Fig. 2) were used in cases with mobile footplate. Stapedotomy was performed for stapes fixation, with piston prosthesis placement. Oval window drill-out was performed in cases without stapes footplate and oval window, with piston prosthesis for ossiculoplasty.
Audiologic evaluation
Preoperative air conduction (AC) and bone conduction (BC) mean hearing thresholds, and air–bone gap (ABG) at 0.5, 1, 2, 3 and 4 kHz were recorded and used to assess surgical efficacy. The last audiogram recorded was used to represent postoperative hearing.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 18.0. Paired t test was used to compare the preoperative and postoperative AC and BC hearing thresholds and ABG. Independent-samples t test was used to compare AC gain among age groups and deformity types. A P value < 0.05 was considered statistically significant.
Results
Sixty-four patients were included. Exploratory tympanotomy was performed on the right ear in 37 cases (57.8%) and on the left ear in 27 cases (42.2%). Of the cases, 40.6% were female and 59.4% were male, with the age ranging from 7 to 66 years (mean 21.28±12.53 years, median 17 years). The average age of hearing loss diagnosis was 11.33 ± 6.92 years.
The preoperative HRCT scan showed ossicular anomaly confirmed by surgery in 40 cases (62.5%) and normal in 24 cases (37.5%), among which 10 cases (100%) had ossicles fixation to adjacent bony walls, 34 cases (34/56, 60.7%) had ossicular chain discontinuity, 2 cases had ptotic facial nerve (100%) and 1 case (50%) had dehiscent horizontal segment.
Categorization of malformations was based on the status of stapes according to the Teunissen and Cremers classification [5], including class 1 (congenital isolated stapes ankylosis, n = 2), class 2 (congenital stapes ankylosis in combination with a congenital anomaly of the ossicular chain, n = 8) (Table 1), class 3 (congenital anomalies of the ossicular chain and at least a mobile stapes footplate, n = 47) (Table 2) and class 4 (aplasia or severe dysplasia of the oval window or round window, n = 7) (Table 3).
Tympanoplasty was performed to improve hearing, but had to be aborted in two cases for the following reasons: one case had ptotic facial nerve and the other case had unexposed vestibule cisterna after drilling 2 mm at the position of the oval window. In one case with the malleus fused to the lateral attic wall, no prosthesis was needed as the ossicular chain was intact and functional after the bony column was abraded. Prostheses used in 61 cases included autologous incus (n = 8), PORP (n = 13), TORP (n = 23) and piston prosthesis (n = 17).
Hearing in the contralateral ear was normal in these cases. Postoperative hearing results were available in 47 cases (Table 4), whereas data in the other 17 cases were incomplete and resulted in their exclusion from pre- and postoperative hearing analysis. AC hearing gain exceeded 30 dB in 25 cases (53.2%). Of 47patients, 34 had an ABG within 20 dB, 15 had an ABG within 10 dB, and 4 had 0 dB ABG after operation. No significant difference was observed for AC hearing gain among different age groups or different types of malformations (Table 5).
Discussion
Congenital unilateral middle ear malformations are rare. Park reported that 47.4% of congenital middle ear malformations with intact external ear were unilateral [1]. In this study, we reported the characteristics, types and hearing outcomes of unilateral middle ear malformations for the first time.
Non-progressive conductive hearing loss with normal tympanic membrane, and no history of trauma or infection, is highly suggestive of congenital middle ear malformation [6]. Most patients discover unilateral hearing loss by themselves when listening to music or communicating verbally with others due to normal contralateral hearing and speech functions, although ossicular chain discontinuity may be seen on CT and thickness of the oval window may serve as an important CT criterion for identifying possible stapes footplate ankyloses [7,8,9]. Preoperative HRCT showed ossicular anomaly features confirmed by surgery in 62.5% of the cases in our study. HRCT could effectively distinguish ossicles fixation to adjacent bony walls including malleus, incus fixation to lateral attic wall and stapes fixation to facial nerve canal during surgery. Incudostapedial anomaly induced ossicular chain discontinuity may be misdiagnosed by preoperative HRCT. We observed that it is difficult to diagnose stapes ankylosis and oval window absence by preoperative HRCT. Therefore, stapes ankylosis and oval window absence should be taken into account in case of conductive hearing loss with normal preoperative HRCT. Meanwhile, the otologist can also acquire important information on the course of facial nerve, which is helpful for avoiding facial nerve injury. Preoperative HRCT is also necessary to exclude inner ear malformations, including enlarged vestibular aqueducts, Mondini dysplasia, common cavity dysplasia and wide internal auditory canals, and to reduce the risk of a stapes gusher and sensorineural hearing loss.
Diagnosis is more difficult when it comes to unilateral hearing loss, with the diagnosis generally made at the age of 6 years [10]. In this study, the average age of hearing loss diagnosis was 11.33 ± 6.92 years, and the age at surgery was 21.28 ± 12.53 years, showing a delay of 9.95 ± 12.72 years between diagnosis and surgery. There is no research showing postoperative hearing differences in relation to surgical age [11, 12]. In this study, surgery before and after 15 years of age made no significant difference, although unilateral hearing loss may still have a negative effect on school performance and we feel that ossiculoplasty performed at an early age may be of benefit to the patient. Surgery can be delayed to adult age for any specific reasons prohibiting surgery.
There is no universally accepted classification for middle ear malformations. In 1993, Teunissen and Cremers analyzed surgical findings in 144 ears with middle ear malformations and developed a classification system which is widely recognized. The Cremers and Teunissen classification proposes four main classes of minor ear malformations [5], i.e., congenital isolated stapes ankylosis (class 1), congenital stapes ankylosis in combination with a congenital anomaly of the ossicular chain (class 2), congenital anomalies of the ossicular chain and at least a mobile stapes footplate (class 3), and aplasia or severe dysplasia of the oval window or round window (class 4). Park further divided class 3 in the Teunissen and Cremers classification system into two types according to whether the suprastructure exists on a mobile stapes footplate. This classification was described on the basis of the severity of stapes footplate malformations and is relevant to postoperative hearing improvements [1]. However, having suprastructure on a mobile stapes footplate or not made no significant differences in postoperative hearing in our study.
The types of anomaly appear to be different between unilateral and bilateral middle ear malformations. Austin reported that cases of missing incus long process alone represents 59% of all ossicular anomalies; while loss of the incudal long process together with stapes superstructure accounts for 23% of the cases [13]. Researches also show that the most common middle ear malformation is simple stapes footplate fixation, of which 86.1% are bilateral (up to 90% in some series) [1, 3, 14, 15]. In the present study, 47 cases (73.44%) showed ossicular chain anomaly but with a mobile stapes footplate, and 24 cases (37.5%) showed missing incus long process and stapes suprastructure. Only two cases (3.1%) were found to have fixed stapes footplate in our study. It is in accordance with opinions of some reports that stapes footplate fixation is seen mostly in cases of bilateral malformations. Diagnosis is relatively easy when stapes footplate fixation is combined with other anomalies. Simple congenital stapes footplate fixation can be difficult to distinguish from otosclerosis, but the latter is often characterized by progressive hearing loss. Congenital stapes footplate fixation can be misdiagnosed if definite proof of progressive deafness is not available [10]. It is therefore necessary to monitor for hearing changes over a period time rather than relying on subjective description of hearing loss.
Significant hearing gain achieved by exploratory tympanotomy has been reported in the literature [2, 3, 16,17,18,19]. Different ossiculoplasty techniques and prosthesis were applied to osscular chain reconstruction in our series. All patients acquired various levels of postoperative hearing improvement, averaging 30.1 ± 10.5 dB with 25 cases (53.2%) exceeding 30 dB. Postoperative ABG was less than 20 dB in 34 cases (72.3%) with 4 achieving 0 dB ABG. While there was no significant difference between pre- and postoperative BC PTA, BC PTA decrease exceeded 10 dB in four cases. Sensorineural hearing loss was usually defined as a change in BC thresholds exceeding 10 dB. In the past studies, stapes surgery in case of congenital middle ear malformations has been thought to be associated with an increased risk of sensorineural hearing loss [20]. In the present study, only one of the four cases underwent stapedotomy. Since there were no intraoperative complications reported, there is no clear explanation for the change in bone conduction thresholds.
In this study, 17 cases were lost to follow-up, among which 11 were lost due to change of phone numbers and addresses, 2 had failed ossicular chain reconstruction, and the remaining 4 declined re-evaluation due to inability to travel long distance and unaffordable cost.
Conclusion
Unilateral congenital middle ear malformations are diverse, and the proportion of various anomaly types in unilateral congenital middle ear malformations is different from bilateral congenital middle ear malformation. Our study can help characterize unilateral middle ear malformations. Exploratory tympanotomy and ossiculoplasty are effective methods for diagnosing and treating unilateral congenital middle ear malformations.
References
Park K, Choung YH (2009) Isolated congenital ossicular anomalies. Acta Otolaryngol 129:419–422. https://doi.org/10.1080/00016480802587846
Baba S, Ikezono T, Pawankar R, Yagi T (2004) Congenital malformations of the middle ear with an intact external ear: a review of 38 cases. ORL J Otorhinolaryngol Relat Spec 66:74–79. https://doi.org/10.1159/000077799
Hashimoto S, Yamamoto Y, Satoh H, Takahashi S (2002) Surgical treatment of 52 cases of auditory ossicular malformations. Auris Nasus Larynx 29:15–18. https://doi.org/10.1016/s0385-8146(01)00125-0
Snik F, Teunissen B, Cremers W (1994) Speech recognition in patients after successful surgery for unilateral congenital ear anomalies. Laryngoscope 104:1029–1034. https://doi.org/10.1288/00005537-199408000-00020
Teunissen EB, Cremers WR (1993) Classification of congenital middle ear anomalies. Report on 144 ears. Ann Otol Rhinol Laryngol 102:606–612. https://doi.org/10.1177/000348949310200807
Su Y, Yuan H, Song YS, Shen WD, Han WJ, Liu J, Han DY, Dai P (2014) Congenital middle ear abnormalities with absence of the oval window: diagnosis, surgery, and audiometric outcomes. Otol Neurotol 35:1191–1195. https://doi.org/10.1097/mao.0000000000000277
Yuen HY, Ahuja AT, Wong KT, Yue V, van Hasselt AC (2003) Computed tomography of common congenital lesions of the temporal bone. Clin Radiol 58:687–693. https://doi.org/10.1016/s0009-9260(03)00208-3
Swartz JD, Faerber EN (1985) Congenital malformations of the external and middle ear: high-resolution CT findings of surgical import. AJR 144:501–506. https://doi.org/10.2214/ajr.144.3.501
Lagleyre S, Sorrentino T, Calmels MN, Shin YJ, Escude B, Deguine O, Fraysse B (2009) Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol 30:1152–1159. https://doi.org/10.1097/MAO.0b013e3181c2a084
Albert S, Roger G, Rouillon I et al (2006) Congenital stapes ankylosis: study of 28 cases and surgical results. Laryngoscope 116:1153–1157. https://doi.org/10.1097/01.mlg.0000227501.78004.f6
House JW, Sheehy JL, Antunez JC (1980) Stapedectomy in children. Laryngoscope 90:1804–1809. https://doi.org/10.1288/00005537-198011000-00007
Welling D, Merrell J, Merz M, Dodson E (2003) Predictive factors in pediatric stapedectomy. Laryngoscope 113:1515–1519. https://doi.org/10.1097/00005537-200309000-00018
Austin DF (1971) Ossicular reconstruction. Arch Otolaryngol 94:525–535. https://doi.org/10.1001/archotol.1971.00770070825007
Park HY, Han DH, Lee JB, Han NS, Choung YH, Park K (2009) Congenital stapes anomalies with normal eardrum. Clin Exp Otorhinolaryngol 2:33–38. https://doi.org/10.3342/ceo.2009.2.1.33
Schlosser WD, Goldman BR, Winchester RA (1964) Further experiences with the diagnosis and surgical management of congenital mixed deafness. Laryngoscope 74:773–789. https://doi.org/10.1288/00005537-196406000-00002
Jahrsdoerfer R (1980) Congenital malformations of the ear. Analysis of 94 operations. Ann Otol Rhinol Laryngol 89:348–352. https://doi.org/10.1177/000348948008900410
Thomeer HG, Kunst HP, Cremers CW (2012) Congenital ossicular chain anomalies associated with a mobile stapes footplate: surgical results for 23 ears. Ann Otol Rhinol Laryngol 121:275–281. https://doi.org/10.1177/000348941212100414
Philippon D, Laflamme N, Leboulanger N, Loundon N, Rouillon I, Garabedian EN, Denoyelle F (2013) Hearing outcomes in functional surgery for middle ear malformations. Otol Neurotol 34:1417–1420. https://doi.org/10.1097/MAO.0b013e3182a1a8fd
Quesnel S, Benchaa T, Bernard S, Martine F, Viala P, Van Den Abbeele T, Teissier N (2015) Congenital middle ear anomalies: anatomical and functional results of surgery. Audiol Neurootol 20:237–242. https://doi.org/10.1159/000380940
Vincent R, Wegner I, Kamalski DM, Bittermann AJ, Grolman W (2016) Congenital stapes ankylosis in children: surgical findings and results in 35 cases. Otol Neurotol 37:367–373. https://doi.org/10.1097/mao.0000000000000923
Funding
National Natural Science Foundation of China, code: 81470683. National Natural Science Foundation of China, code: 81770992.
Author information
Authors and Affiliations
Contributions
Each of the authors has contributed to reading and approving this manuscript.
Corresponding author
Ethics declarations
For this type of study formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tang, C., Zhang, J., Yang, S. et al. Unilateral congenital malformations of middle ear with intact external ear: a review of 64 cases. Eur Arch Otorhinolaryngol 275, 2467–2472 (2018). https://doi.org/10.1007/s00405-018-5099-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5099-9