Abstract
The aim of this study was to measure cone beam computed tomography (CBCT) derived bone density of 6 anatomic points around the otic capsule in preoperative assessment of patients with clinically suspected otosclerosis, and to compare these densities with control group. CBCT images of 21 patients (34 ears, the otosclerosis group) with surgically confirmed otosclerosis and 26 patients (52 normal ears, the control group) were evaluated in this prospective study. Six regions of interest (ROI) were set manually around the otic capsule with the slice thickness of 0.3 mm. The mean CBCT bone density these regions were measured and compared in the case and control groups. In the case group, the mean CBCT bone density at the fissula ante fenestram (FAF) was significantly lower than the control group. Moreover, at the 4 points of the other ROIs (3–6) CBCT bone densities were significantly lower in the case group compared to the control group (p < 0.01). In this group, among 13 bilateral otosclerosis, 22 ears had conductive hearing loss (CHL), 4 ears had mixed hearing loss (MHL) and among 8 unilateral otosclerosis, 5 ears had CHL, 3 ears had MHL. Our study showed the mean CBCT bone density of ROIs 1 and 6 were correlated with the average air–bone gap in the bilateral and unilateral otosclerosis group, respectively. Quantitative evaluation of CBCT with a slice thickness of 0.3 mm can be used as a suitable tool for diagnosis and follow-up of otosclerosis in temporal bone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Otosclerosis, the most common cause of conductive hearing loss in adult human beings, is an inflammatory bone disorder with unknown cause, particularly affecting otic capsule in temporal bone [1]. This disease is more prevalent in Caucasians with approximately 1% involvement [2]. It is frequently the disease of adult women in the age range of 15–55 years and usually starts at the age of 20 [1].
The most significant symptom of the disease is conductive hearing loss (CHL). However, sensory neural and mixed hearing loss (SNHL, and MHL) might also occur [2].
The disease mechanism is replacement of normal endochondral bone by spongy vascular bone, and it is also called ‘otospongiosis’ [3]. With disease progression in the final stages, the decalcified foci tend to become less vascular and sclerotic [4].
In patients, initially, anterior footplate of stapes also called Fissula Ante Fenestram (FAF), becomes demineralized and then the lesion extends to the vestibule and cochlea [5]. Consequently, based on the location and extent of demineralization, lesions are divided into fenestral and cochlear or retrofenestral otosclerosis, which are bilateral in 80% of cases [6].
Principally, otosclerosis diagnosis occurs as a result of patient's history of progressive hearing loss, positive family history, clinical, and audiometric examinations. Frequently, in otoscopy and clinical examination, tympanic membrane is normal. Air-bone-gap (ABG) more than 10 dB in audiometry implies the stapedial fixation, which is the cause of CHL [7, 8]. However, considering the positive and negative false results obtained from clinical and audiometric examinations in patients with vague symptoms, such as dizziness and hearing loss, the diagnosis of otosclerosis can potentially be a confusing and difficult process [3]. In recent years, pre-operative imaging has prevented blinded and unnecessary operations and increased patient’s awareness regarding the treatment process.
High-resolution CT (HRCT) of the temporal bone is the modality of choice for the preoperative evaluation of otosclerosis due to its ability to accurately show anatomy and pathological changes in ossicular chain and tiny structures of middle and inner ear [9]. Numerous studies have confirmed high resolution computed tomography (HRCT) as an effective tool for determining the presence and extension of hypocalcified foci of bony labyrinthine in otosclerosis [2, 10].
Today, Cone beam computed tomography (CBCT), has an extensive application in producing three dimensional reconstructed images of the maxillofacial structures with high spatial resolution, and no magnification, superimposition or distortion [11,12,13,14]. Several studies have evaluated the practicality of CBCT in diagnosing temporal bone abnormalities [6, 8]. Previous studies demonstrated that gray density accuracy of CBCT is comparable with CT imaging systems and there is high correlation between the bone density value of CBCT and CT [16,17,18,19,20].
Findings show that CBCT might be a proper imaging method to define hypodense lesions of otic capsule otosclerosis in a manner similar to HRCT [1, 9].
To the best of our knowledge, there is no study that has quantitatively evaluated temporal bone density by CBCT in patients suspicious of otosclerosis. Therefore, this study was designed to measure CBCT bone density of six anatomic points around the otic capsule and its correlation with clinical and surgical findings.
Materials and Methods
This prospective case–control study was conducted 2017 to 2018 and the research was approved by the ethical board of institutional committee. The case group included 21 patients (10 men and 11 women, mean age of 32.51 ± 6.83 years) with otosclerosis in at least one ear. The control group consisted of 26 participants (12 men and 14 women, mean age of 34.76 ± 13.79 years), who had referred to imaging center for temporomandibular joint CBCT scanning due to various diagnostic tasks. All subjects underwent a complete clinical examination, including otoscopy, pure-tone and vocal audiometry and a CBCT scan. Preoperative CBCT scan in the case group was requested by the consultant otologist to rule out any other pathologic causes for hearing loss. Exclusion criteria were poor quality CBCT images for detecting ear structures, abnormal audiometric findings and history of hearing loss of any type amongst the control group. Patients with history of trauma and surgery in temporal bone, otitis media and other ear disorders were excluded from the control and case groups.
The Otologist (with more than 10 years' experience) reported the ABG and types of hearing loss including CHL, SNHL, and MHL according to the audiometric results. The average ABG was defined as the mean air conduction threshold minus the mean bone conduction threshold.
Clinical diagnosis of otosclerosis was based on normal tympanic membrane, CHL, SNHL, and MHL as well as ABG more than 10 db. Otosclerosis was confirmed in all case subjects during surgical procedure by stapedial fixation.
All CBCT images were captured by a NewTom VGi CBCT machine (QR- SRL, Verona, Italy) by the same clinician. Exposure factors were set at 110 KVP, 7.84 mAs and exposure time of 0.75 ms. A field of view (FOV) of 15 × 12 cm was selected to cover the entire temporal bones. Sectional images were reconstructed in axial, coronal and sagittal plans with slice thickness of 0.3 mm.
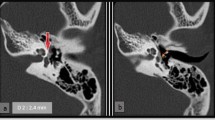
Around the oval window and cochlea, in axial views passing through the oval window six anatomic points were selected (Table 1). 1mm2 rectangular regions of interest (ROIs) were set manually in these points, and CBCT bone density was automatically measured in each ROI (Fig. 1, 2).
Qualitative and quantitative variables were compared between groups using chi-square and Mann–Whitney tests, respectively. The relationship between CBCT bone density in each ROI and hearing loss in otosclerosis cases was evaluated by Spearman Correlation Analysis. A p-value less than 0.05 was considered to be statistically significant.
Results
In this research, no significant statistical differences in terms of age, gender and side were detected between the otosclerosis and control subjects. (Table 2).
In otosclerosis group, among 21 cases, 13 had bilateral (26 ears) and 8 had unilateral otosclerosis.
Our study showed 11 patients (22 ears) had bilateral CHL with average ABG of 42.27 ± 9.72 dB, 2 (4 ears) had bilateral MHL with average ABG of 38.00 ± 13.03 dB, 5 ears had unilateral CHL and average ABG of 44.00 ± 8.94 dB, 3 ears had unilateral MHL and average ABG was 50 ± 0.00 dB in otosclerosis group. The average ABG in the otosclerosis group was 42.28 ± 9.72 dB.
In otosclerosis cases, ROI 2 had the lowest CBCT bone density and ROI 6 had a relatively the highest CBCT bone density compared to ROIs 1, 3, 4 and 5 (Fig. 3). The mean CBCT bone density was significantly lower in the case group in comparison with the control group at the ROIs 2, 3, 4, 5 and 6. However, at ROI 1, there was no statistically significant difference in CBCT bone density between the otosclerosis and control groups (Table 3).
In bilateral otosclerosis group, the CBCT bone density of ROIs 1 correlated with the average ABG in a negative trend (Spearman correlation, n = 22, r = -0.636, p = 0.001) (Fig. 4). Also, in patients with unilateral otosclerosis, there was a significant negative correlation between CBCT bone density of ROI 6 and average ABG (Spearman correlation, n = 7, r = -0.802, p = 0.03) (Fig. 5).
Discussion
Considering the higher spatial resolution, lower radiation dose, availability and ease of CBCT examination compared to CT, this research was conducted to evaluate the feasibility of CBCT in diagnosing otosclerosis by measuring CBCT bone density number or voxel value (VV) of six anatomic points adjacent to oval window and around the cochlea.
Several studies have revealed that gray density accuracy of CBCT is comparable with CT imaging systems [15, 16]. In Nomura et al. [17] study, they compared bone density value in CT and CBCT and showed a high correlation between VV of CBCT and CT number in MSCT. On the other hand, many studies have shown that the obtained density values from CBCT are not absolute, but interestingly reported a positive high linear correlation between CBCT bone density and HU in MSCT [17, 19,20,21].
The results of present investigation show that the mean CBCT bone densities in ROI 2 to 6 for otosclerosis patients were significantly lower than the control group.
For the first time in 2012, Redfors et al. [9] used a visual grading system to detect fenestral and retrofenestral lesions of otosclerosis in multi-slice CT (MSCT) and CBCT images, which reported the preoperative CBCT to have a sensitivity of up to 85% with a slice thickness of 0.5 to 0.6 mm in patients with clinical otosclerosis. Their study indicates that in many ways, CBCT is equivalent to MSCT for detecting hypodense foci in the temporal bone imaging. But they did not quantitatively evaluate in their study.
Therefore, in the present study, we used CBCT to evaluate bone density of some temporal bone anatomic points for diagnosing otosclerosis.
In another study, Haghanifar et al. [19] analyzed the relationship between gray density and VV of two CBCT imaging systems and CT. According to their results, there was a high correlation and linear relationship between the different studied imaging systems. Therefore, we can compare the results of the present study with previous studies that had used CT in their research.
In a histological study by Schuknecht et al. [22] the foci of otosclerosis were mainly situated in the FAF, as shown in this study.
Grayeli et al. [5] reported the CT number only in the FAF (corresponding to ROI 2 in our study) and posterior semicircular canal (close to ROI 2) to be lesser in the otosclerosis group than the control group. While in the present study, the mean CBCT bone densities in other ROIs (2–6) in otosclerosis group were significantly lower than the control group. Also, Tringali et al. [23] stated that the mean CT value in the area anterior to the oval window (FAF) and the area anterior to the internal auditory canal were significantly lower in the otosclerosis group than control group.
Mean CBCT bone density of the posterior to the oval window (ROI 1) was higher than the controls in this study; however, this difference was not significant. This finding was in contrast to the results of Zhu et al. [8] which reported significantly lower mean CT values in ROI 1 in otosclerotic ears comparing to the control group. Variations in the results of these studies can be contributed to the extent of sclerotic foci, different ethnicity, and difference in imaging method (less possibility).
Studies of Naumann et al. [24] found that the size of the ABG was determined by the extent and degree of pathological effects of otosclerosis at the posterior stapediovestibular joint area (corresponding to ROI 1). Kiyomizu et al. [25] stated that greater ABG associated with greater extent of sclerotic lesions might be due to progressive sclerotic lesions at the oval window. On the other hand, Min et al. [6] and Schuknecht et al. [22] did not find a significant relationship between the size of otosclerosis lesions in CT grading of sclerotic lesions and thresholds of bone conduction and ABG. In the present study, a significant negative correlation was observed between ABG and CBCT bone density for the ROIs 1 and 6 in bilateral and unilateral otosclerosis, respectively. This means that the more reduction in CBCT bone density, the more severe was the hearing loss.
Due to limited number of studies on CBCT imaging for diagnosing otosclerosis, further studies on CBCT evaluation of otosclerosis with more patients is recommended. future study using CBCT in diagnosing cochlear otosclerosis in cases with familial SNHL or MHL also is recommended.
Conclusion
Bone density measurements of temporal bone using CBCT with a slice thickness less than 0.5 mm indicated a significant lower value in otosclerosis lesions in comparison with the controls. Therefore, CBCT bone densitometry potentially appears to be a valuable and effective method for quantitatively determining the existence of otosclerosis in temporal bone.
References
Liktor B, Révész P, Csomor P, Gerlinger I, Sziklai I, Karosi T (2014) Diagnostic value of cone-beam CT in histologically confirmed otosclerosis. Eur Arch Otorhinolaryngol 271(8):2131–2138
Lagleyre S, Sorrentino T, Calmels M-N, Shin Y-J, Escudé B, Deguine O et al (2009) Reliability of high-resolution CT scan in diagnosis of otosclerosis. Otol Neurotol 30(8):1152–1159
Emmett SD, Seshamani M, Otolaryngology in the Elderly. in: Flint PW, Haughey BH, Robbins KT, Thomas JR, Niparko JK, Lund VJ, et al, editors. Cummings Otolaryngology-Head and Neck Surgery. 6th ed. Kennedy Blvd. Philadelphia: Elsevier Health Sciences; 2015. p. 231–38.
Gros A, Vatovec J, Šereg-Bahar M (2003) Histologic changes on stapedial footplate in otosclerosis: correlations between histologic activity and clinical findings. Otol Neurotol 24(1):43–47
Grayeli AB, Yrieix CS, Imauchi Y, Cyna-Gorse F, Ferrary E, Sterkers O (2004) Temporal bone density measurements using CT in otosclerosis. Acta Otolaryngol 124(10):1136–1140
Min J-Y, Chung W-H, Lee WY, Cho YS, Hong SH, Kim HJ et al (2010) Otosclerosis: incidence of positive findings on temporal bone computed tomography (TBCT) and audiometric correlation in Korean patients. Auris Nasus Larynx 37(1):23–28
Révész P, Liktor B, Liktor B, Sziklai I, Gerlinger I, Karosi T (2016) Comparative analysis of preoperative diagnostic values of HRCT and CBCT in patients with histologically diagnosed otosclerotic stapes footplates. Eur Arch Otorhinolaryngol 273(1):63–72
Zhu M-m, Sha Y, Zhuang P-y, Olszewski AE, Jiang J-q, Xu J-h et al (2010) Relationship between high-resolution computed tomography densitometry and audiometry in otosclerosis. Auris Nasus Larynx 37(6):669–675
Redfors YD, Gröndahl HG, Hellgren J, Lindfors N, Nilsson I, Möller C (2012) Otosclerosis: anatomy and pathology in the temporal bone assessed by multi-slice and cone-beam CT. Otol Neurotol 33(6):922–927
Mafee M, Henrikson G, Deitch R, Norouzi P, Kumar A, Kriz R et al (1985) Use of CT in stapedial otosclerosis. Radiology 156(3):709–714
Adibi S, Paknahad M (2017) Comparison of cone-beam computed tomography and osteometric examination in preoperative assessment of the proximity of the mandibular canal to the apices of the teeth. Br J Oral Maxillofac Surg 55(3):246–250
Paknahad M, Shahidi S, Zarei Z (2017) Sexual Dimorphism of Maxillary Sinus Dimensions Using Cone-Beam Computed Tomography. J Forensic Sci 62(2):395–398
Paknahad M, Shahidi S, Khaleghi I (2017) A cone beam computed tomographic evaluation of the size of the sella turcica in patients with cleft lip and palate. J Orthod 44(3):164–168
Paknahad M, Shahidi S, Abbaszade H (2016) Correlation between condylar position and different sagittal skeletal facial typesZusammenhang zwischen Kondylenposition und sagittalen skelettalen Strukturmustern im Gesicht. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie 77(5):350–356
Mah P, Reeves TE, McDavid WD (2010) Deriving Hounsfield units using grey levels in cone beam computed tomography. Dentomaxillofac Radiol 39:323–335
Parsa A, Ibrahim N, Hassan B, Motroni A, van der Stelt WD (2012) Reliability of voxel values in computed tomography for preoperative implant planning assessment. Int J Oral Maxillofacial Implants. 27:1438–1442
Nomura Y, Watanabe H, Honda E, Kurabayashi T (2010) Reliability of voxel values from cone-beam computed tomography for dental use in evaluating bone mineral density. Clin Oral Implant Res 21(5):558–562
Cassetta M, Stefanelli L, Di Carlo S, Pompa G, Barbato E (2012) The accuracy of CBCT in measuring jaws bone density. Eur Rev Med Pharmacol Sci 16(10):1425–1429
Haghanifar S, Yousefi S, Moudi E, Abesi F, Bijani A, Moghadamnia AA et al (2017) Accuracy of densitometry of two cone beam computed tomography equipment in comparison with computed tomography. Electron phys 9(5):4384
Soardi CM, Zaffe D, Motroni A, Wang HL (2014) Quantitative comparison of cone beam computed tomography and microradiography in the evaluation of bone density after maxillary sinus augmentation: a preliminary study. Clin Implant Dent Relat Res 16(4):557–564
Cassetta M, Stefanelli LV, Pacifici A, Pacifici L, Barbato E (2014) How Accurate Is CBCT in Measuring Bone Density? A Comparative CBCT-CT In Vitro Study. Clin Implant Dent Relat Res 16(4):471–478
Schuknecht HF, Barber W (1985) Histologic variants in otosclerosis. Laryngoscope 95(11):1307–1317
Tringali S, Pouget J-F, Bertholon P, Dubreuil C, Martin C (2007) Value of temporal bone density measurements in otosclerosis patients with normal-appearing computed tomographic scan. Annals of Otol Rhinol Laryngol 116(3):195–198
Naumann IC, Porcellini B, Fisch U (2005) Otosclerosis: incidence of positive findings on high-resolution computed tomography and their correlation to audiological test data. Annals Otol, Rhinol Laryngol 114(9):709–716
Kiyomizu K, Tono T, Yang D, Haruta A, Kodama T, Komune S (2004) Correlation of CT analysis and audiometry in Japanese otosclerosis. Auris Nasus Larynx 31(2):125–129
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Izadparast, Y., Shahidi, S., Paknahad, M. et al. Feasibility of CBCT in Diagnosing Otosclerosis by Measuring CBCT Bone Density: A Preliminary Study. Indian J Otolaryngol Head Neck Surg 74, 322–328 (2022). https://doi.org/10.1007/s12070-021-02502-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-021-02502-2