Abstract
High resolution computed tomography (HRCT) is a tool which provide fine details of temporal bone and its associated pathologies which are of extreme use in making diagnosis, to evaluate extension of disease and most important to plan surgical approach. Aim of the present study was to correlate HRCT findings with operative findings in different ear pathologies. This observational, prospective study enrolled 70 patients of different ear pathologies required surgical intervention. They were subjected to HRCT temporal bone and its findings were correlated with surgical findings. Mean age of the study population was 20.3 ± 12.04 years with M: F = 1.12: 1. HRCT showed specificity and sensitivity of 100% and 92.31% respectively in detecting ossicular erosion. It was 100% sensitive and 98.51% specific in detecting LSCC erosion, 85.71% sensitive and 96.83% specific in detecting facial canal dehiscence, 100% sensitive and 98.11% specific in detecting scutum erosion, 75% sensitive and 96.97% specific to detect tegmen erosion, 100% sensitive and 97.01% specific in detecting sinus plate erosion, 100% sensitive and 95.38% specific in detecting high jugular bulb, sensitivity and specificity both are 100% in detecting labyrinthitis ossificans and 100% sensitive in detecting otosclerotic foci. HRCT findings showed a good association with operative findings in terms of sensitivity and specificity. Thus, HRCT is a acceptable tool to make diagnosis and to plan surgical approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aural pathologies constitute the third most common cause of visiting to the door of an otorhinolaryngologist and being a frequent reason to prescribe medicines or to perform surgery [1].
Earlier, the clinical examination was the sole method to make a diagnosis. However, in current scenario it is not sufficient, owing to prevalence, complications and recurrence of various pathologies of the temporal bone. There are various ear pathologies which can be diagnosed properly on the basis of clinical examination alone without getting any extra aid from imaging. However, numerous pathologies are associated with high morbidity, recurrence and complications. In such cases and many more, imaging plays an important role to confirm existence of disease along with its site and extent. This information is quite beneficial to plan surgical approach prior to surgical exploration [2].
A revolution took place in field of imaging of temporal bone in 1980 by development of high-resolution computed tomography (HRCT). HRCT is a modality of routine computed tomogram. In temporal bone it precisely delineates the bony structures as well as the soft tissue component which is helpful to examine the region in an organized and systematic fashion. It provides a practical approach to understanding temporal bone anatomy, localizing a pathologic process with a focus on inflammatory and neoplastic processes, identifying pertinent positives and negatives, and formulating a differential diagnosis. Thus, HRCT plays a crucial role in making diagnosis and assessing the disease extent, helping to decide appropriate management [3].
This study was aimed to understand the role of HRCT in diagnosis of various temporal bone pathologies and to correlate them with intra-operative findings.
Methods
This hospital based, observational, prospective study was conducted in Department of ENT and Head Neck Surgery of our institute from March 2017 to November 2018. Total 70 patients presented in ENT OPD with complaints related to ear and clinically diagnosed as various ear pathologies which required surgical intervention were included in the study after taking written and informed consent. Those who were previously operated/required revision surgery, were unfit for surgery and were not willing to participate in the study were excluded.
After taking consent all study participants underwent history taking, thorough ENT examination, general physical and systemic examination. Pure tone audiometry and hematological investigations were done as a routine of all patients. All participants were subjected to go through radiological examination in form of HRCT temporal bone. Scans were acquired in the helical mode to reduce motion artifacts. The images were reconstructed with a bone algorithm. Coronal and sagittal reformatting was done to a slice thickness of 0.69 mm. Each HRCT image were analyzed for specific features relevant to the evaluation of pathologies of temporal bone.
After getting anesthetic clearance surgery was planned. Surgeries were done by senior otorhinolaryngologists of our institute. Intra-operatively we noted the findings whom we were concerned. At the same time, we had HRCT of the patients when they were on operating table. We compared the findings both radiologically and clinically which were in front of us. Then we prepared our results accordingly. Pre-operative CT scan findings were compared with operative findings in order to correlate soft tissue mass, ossicular erosion, bony erosion, extension of the disease, temporal as well as intracranial complications.
Categorical variables were presented in numbers and percentage and continuous variables were presented as mean ± standard deviation. Diagnostic test was used to find sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy. P < 0.05 was considered as statistically significant. Data analysis was done using Statistical Package for Sciences version 21.0. (IBM, Chicago, USA).
Results
Total 70 patients presented in ENT OPD of our institute with various ear pathologies which required surgical interventions were enrolled in the study. Mean age of the study population was 20.3 ± 12.04 years. Among 70 subjects, 37 were males and 33 were females (M: F = 1.12: 1).
Table 1 is showing distribution of study subjects according to their disease. Maximum subjects (58.5%) had chronic otitis media (COM).
Ossicular Erosion
In our study on HRCT temporal bone, 36 cases were reported to have eroded ossicles and rest 34 cases with intact ossicles, while intra-operatively, they were found to be eroded in 39 patients and were intact in 31 patients (Fig. 1). HRCT showed specificity and sensitivity of 100% and 92.31% respectively in detecting ossicular erosion. It showed 100% PPV, 91.18% NPV and 95.71% diagnostic accuracy in detecting the same. When we studied erosion of ossicles separately than HRCT reported malleus to be eroded in 10, incus in 34 and stapes in 26 cases. Intra-operatively, we noted that malleus was eroded in 8, incus in 40 and stapes in 29 cases. Sensitivity, specificity, PPV, NPV and diagnostic accuracy of HRCT in diagnosing ossicles erosion individually is mentioned in Table 2.
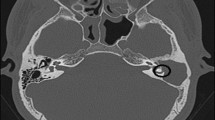
Lateral Semicircular Canal Erosion (LSCC)
In present study HRCT temporal bone reported erosion of LSCC in 4 cases out of which 3 cases found to have its erosion intra-operatively. HRCT was 100% sensitive and 98.51% specific in detecting LSCC erosion with 75% PPV and 100% NPV. It has 98.57% diagnostic accuracy (Fig. 2).
Facial Canal Dehiscence (FCD)
In our study total 8 subjects had dehiscent facial canal on HRCT out of which 6 had similar finding intra-operatively. Out of 62 subjects having intact facial canal on HRCT (Fig. 3), 1 found to had dehiscence intra-operatively. Thus, HRCT has 85.71% sensitivity and 96.83% specificity with 75% PPV and 98.39% NPV in detecting facial canal dehiscence. Diagnostic accuracy in this aspect was 95.71%.
Scutum Erosion
In current study out of 18 subjects which showed scutum erosion on HRCT, 17 subjects had same findings when examined during surgery. Rest 52 cases had intact scutum both radiologically and intra-operatively (Fig. 4). So, in detecting scutum erosion HRCT has 100% sensitivity and 98.11% specificity. Here PPV was 94.44% and NPV was 100% with 98.57% diagnostic accuracy.
Tegmen Erosion
Here, 5 cases had eroded tegmen on HRCT scan (Fig. 5). Among these 5 subjects only 3 were found to show similar findings during surgery rest 2 had intact tegmen. Rest 65 cases had intact tegmen on HRCT out of which only one was such case that presented eroded tegmen intra-operatively. So, to detect tegmen erosion HRCT showed 75% sensitivity and 96.97% specificity with PPV 60% and NPV 98.46%. Diagnostic accuracy was 95.71%.
Sinus Plate Erosion
In our study, on HRCT 5 cases had eroded sinus plate and 65 had intact sinus plate. Whereas intra-operatively only 3 cases showed its erosion which were from those 5 cases which had similar findings on HRCT (Fig. 6). In this aspect HRCT is 100% sensitive and 97.01% specific with 60% PPV and 100% NPV. Its diagnostic accuracy was 97.14%.
High Jugular Bulb
In present study, out of 70 subjects, 8 had high jugular bulb seen in HRCT (Fig. 7). When we explored during surgery only 5 subjects out of these 8 found to had similar finding. Another 62 subjects which didn’t showed presence of high jugular bulb on HRCT, also not showed any variation from this finding during surgery. So, HRCT is 100% sensitive and 95.38% specific in detecting this finding. Here PPV was 62.5% and NPV was 100% with 95.71% diagnostic accuracy.
Labyrinthitis Ossificans
Ossification of labyrinth was noted in 4 subjects during both HRCT evaluation and surgical exploration (Fig. 8). Rest of the 66 subjects which had normal labyrinth on HRCT also found to had similar findings when examined during surgery. Thus, in this aspect sensitivity, specificity, PPV, NPV and diagnostic accuracy all were 100%.
Cochlear Abnormalities
In our study 3 cases were identified with enlarged vestibular aqueduct on HRCT and intra operatively CSF gusher was present in those cases (Fig. 9). Following Sennaroglu classification there was 1 case of common cavity deformity, 1 of incomplete partition type 1 and one of incomplete partition type 2 identified on HRCT, intraoperatively there was presence of CSF gusher and difficult identification of round window.
Otosclerosis
In our study there were 7 patients who were diagnosed with otosclerosis on HRCT (Fig. 10) and intra operatively there was a positive finding and stapes footplate was found fixed in all cases showing that HRCT is 100% sensitive in detecting abnormalities of stapes footplate.
Congenital Cholesteatoma, EAC Stenosis, Keratosis Obturans and Microtia with Facial Palsy
In our study one patient was diagnosed with congenital cholesteatoma with HRCT findings of expansile cystic lytic lesion in petrous part of right temporal bone, and middle ear cavity involving right carotid canal, internal acoustic canal and right vestibule with thinning of underlying bone (Fig. 11). Intra operatively HRCT served a good guide for locating the disease involving retrotympanum, mesotympanum, retrofacial, retrocochlear, petrous apex, extending from sigmoid sinus to internal carotid artery, around internal acoustic canal and removal of the disease without damaging the surrounding structures. HRCT in 2 cases of external auditory canal stenosis helped in deciding the plan of surgery and explaining the prognosis of surgery to the patient as lumen for EAC seen occluded and middle ear and ossicular chain normal in HRCT and intraoperatively too only external ear was found affected (Fig. 12). In 2 cases of keratosis obturans HRCT helped in diagnosing the patient and therefore planning accordingly (Fig. 13). In 1 case of microtia with facial palsy, HRCT showed disease extent in aditus, antrum, epitympanum, hypotympanum, mesotympanum, Prussack’s space with extending into EAC and retro auricular region with erosion of bony EAC, opacification of mastoid air cells, with a note of microtia. Intraoperatively it was revealed that a lot of glue was present which was removed, there was no cholesteatoma seen. Bony canal was eroded. Facial canal was normal with erosion of tegmen plate and therefore exposing dura.
Extent of Disease
In our study HRCT showed a good sensitivity and specificity in detecting the extent of disease in chronic otitis media in mastoid, attic and middle ear cavity.
Table 3 is describing characteristics of HRCT temporal bone in detecting various ear findings pre-operatively. Table 4 is describing correlation of HRCT findings with operative findings.
Discussion
The role of high-resolution computed tomography (HRCT) in evaluating complex lesions of the temporal bone is now well recognized. It has enabled the experienced observer to identify and characterize complex osseous abnormalities with great accuracy. With large traumatic, inflammatory, or neoplastic lesions that involve large areas of the surface of the temporal bone, however, it can be difficult for the clinician who is accustomed to the classical surgical projections to appreciate disease extent and relationship to nearby structures from the multi-section images alone. A comprehensive view may highly facilitate planning of the approach and as well as its results to some extent in pre-surgical period.
The detail and clarity of high-resolution CT remain unsurpassed and unchallenged. However, the use of thin-section imaging creates an additional complexity of its own-a potentially overwhelming array of images spanning the temporal bone in various projections.
Our study showed male dominance which was similar to studies of Dashottar et al. [4] and Kanotra et al. [5]. To the best of our knowledge no previous literatures showed variety of ear diseases in such type of study in a single setting.
Ossicular Erosion
In a study carried out by Kanotra et al. [5] malleus was reported to be eroded in 28 patients by HRCT, while intra-operatively, it was eroded in three more patients, making the HRCT, sensitivity = 90%, specificity = 100%, incus was observed to be eroded in 45 cases on HRCT, while intra-operatively, it was found to be eroded in all the 47 cases, therefore, HRCT was found to be 95.74% sensitive and stapes superstructure erosion was reported by HRCT in nine patients, while intra-operatively, it was found in one more patient, making HRCT, sensitivity = 90%, specificity = 100%.
Prakash and Tarannum A carried out a perspective study in 30 patients and found that ossicular erosion was found in 80% of cases. Incus was the most commonly involved ossicle in 80% of cases. HRCT showed 95.8% sensitivity and 100% specificity in detecting incus erosion. Malleus was eroded in 60% of cases (89.4% sensitivity and 90.9% specificity). Delineation of stapes erosion had a moderate sensitivity of 81.8% and specificity of 88.88% [6].
Mandal et al. [7] conducted a prospective observational study in 49 patients and reported that malleus, incus and stapes were found to be eroded in 69.4, 85.7 and 63.3% respectively in HRCT and 67.3, 89.8 and 67.3% respectively intraoperatively.
Lateral Semicircular Canal Erosion
Kanotra et al. [5] showed that HRCT temporal bone had sensitivity of 66.66%, specificity 95.74%, PPV 100%, and NPV 97.77%. Mandal and co-workers in their study found that there was 97.7% specificity and 80% sensitivity of HRCT in detecting LSCC dehiscence [7]. Payal et al. [8] reported 66.67% sensitivity and 83.33% specificity in detecting the same.
Mahmutoğlu et al. [9] found an excellent compatibility between CT and surgical findings and reported 100% sensitivity and 100% specificity. Gul et al. [10] showed 100% sensitivity and 99.7% specificity in identifying LSC dehiscence with CT. A prospective study of 30 patients by Prakash and Tarannum [6] suggested that erosion of the LSCC was seen in 10% cases with sensitivity 75% which is similar to study by Rogha et al. [11] and specificity 100% which is also in correlation with the study by Gul et al. [10]. Tatlipinar et al. [12] reported 0% sensitivity and 93.6% specificity of HRCT.
Facial Canal Dehiscence (FCD)
There are various studies which reflect role of HRCT in detecting facial canal dehiscence. Mandal and his colleagues noted 11 out of 21 patients with FCD and 30 out of 34 patients with an intact canal were accurately predicted with HRCT findings [7]. Gerami et al. [13] evaluated 80 patients and reported that none of the 12 patients whose FCD was found at surgery were preoperatively identified using HRCT. In study of Keskin et al. [14] who assessed 56 patients showed that facial canal irregularity was preoperatively demonstrated in four patients using CT among six patients who were diagnosed during surgery. CT demonstrated FCD in only one out of four patients in the study by Yildirim-Baylan et al. [15] who evaluated 56 patients of COM . None of the four FCD patients were preoperatively identified using CT in the study by Tatlipinar et al. [12] who assessed 50 patients. Mahmutoğlu et al. [9] found two patients with FCD during surgery among 71 patients., these two patients were also preoperatively identified with CT imaging; on the other hand, two other patients who were preoperatively identified with dehiscence were found to be intact during surgery. Payal et al. [8] studied 60 patients who were diagnosed with chronic suppurative otitis media (CSOM) and found that CT had low efficacy in identifying FCD. In a retrospective study evaluating 31 patients Ng et al. [16] reported that 11 dehiscence patients were identified with CT imaging among 14 patients diagnosed with FCD during surgery, 3 patients who were reported as having an intact canal were diagnosed with dehiscence in surgery. Among 350 patients with CSOM, FCD was identified with a CT scan in 5 out of 30 patients who were perioperatively diagnosed with dehiscence, while surgery did not confirm diagnosis in four patients reported as having dehiscence with a CT scan in the study by Gül et al. [10].
Scutum Erosion
Scutum erosion was reported in 18 cases in pre-operative HRCT, out of which only 1 showed intact scutum intra operative making CT 100% sensitive and 98.11% specific compared to a study which showed erosion in 65% cases with cholesteatoma and reported 100% sensitivity and specificity of HRCT carried out by Rai T [17]. Gaurano JL and Joharjy IA found it in 86% [18]. Scutum erosion was visualized in 34(52.30%) patients in CT, whereas intra operatively it was visualized in 33(50.76%) in a prospective study of 65 patients done by Karki and co-workers [19].
Tegmen Erosion
In our study HRCT had a sensitivity of 75% and specificity of 96.97% compared to sensitivity, specificity of 98% and 25% by Yildirim-Baylan et al. [15] in identifying dural plate erosion. The sensitivity was 100% and specificity was 96% in a series by Mandal et al. [7] in detecting tegmen erosion. In a prospective, analytical study on 65 patients by Karki et al. [19] HRCT had a sensitivity of 100% and specificity of 100% with regards to detection of erosion of tegmen plate, which is comparable to study by Jackler et al. [20].
Sinus Plate Erosion
In our study HRCT had sensitivity and specificity of 100% and 97.01 respectively compared to impressive 100% sensitivity and 100% specificity of CT scan in detecting sigmoid plate erosion by Karki et al. [19], which is similar to study by Rogha et al. [11] which showed precision of CT scan in a prospective descriptive study of (100%). In a study by Yildirim et al. [15] found out that out of 56 patients sinus plate erosion was present in only 1 on HRCT while intra operatively it was present in 4 patients.
High Jugular Bulb
In a study carried out by Alam-Eldeen et al. [21] radiological assessment of the jugular bulb revealed normal jugular bulb in 30 patients (60%), high bulb in 10 (20%), whereas surgical evaluation revealed normal bulb position in 35 patients (70%), high bulb in 8 (16%). This is contrary to a study performed by Júnior et al. [22] who found that the sensitivity of CT was 36.36% and the specificity was 86.36%.
Labyrinthitis Ossificans
We found 4 cases of ossificans on HRCT which was present intra operatively also making HRCT 100% sensitive and specific compared to study by Digge P and her colleagues, where 4 cases of labyrinthine ossificans were observed and only 2 cases were detected by CT. With regard to cochlear ossification, a multicenter retrospective analysis revealed that the accuracy of high-resolution CT (HRCT) in predicting LO was 94.6%, with 100% specificity and 71% sensitivity [23].
Cochlear Abnormalities
Westerhof et al. [24], studied congenital malformations of the inner ear and the vestibulo-cochlear nerve in children with SNHL. Twentyone children (42 inner ears) were studied with high resolution MR and helical CT examinations who were candidates for cochlear implants. They identified 99 malformations. Mondini abnormality and Mondini variants (12/42).
Otosclerosis
On manual reading of the HRCT scans, fenestral otosclerosis was found in 70% to 74% of cases in a study by Naumann et al. [25]. Swartz et al. [26] found that 26 of 35 patients (74%) had fenestral otosclerosis on CT scans. Shin et al. [27] found a fenestral otosclerotic focus on axial CT scans in 119 of 153 patients with otosclerosis (78%). A contemporary literature review regarding the use of HRCT imaging in the diagnosis of otosclerosis was undertaken by Kanzara et al. [28] and quantitative synthesis analysis demonstrated low sensitivity of 58% (95% CI: 49.4–66.9), a high specificity of 95% (95% CI 89.9–98.0) and a positive predictive value of 92% (95% CI: 84.1–95.8). Negative predictive value was 71% (95% CI: 66.1–74.7). The majority of the otosclerotic foci identified on CT were in the fenestral region and a combination of fenestral and retrofenestral foci was second most common.
Extent of Disease
Gomma et al. [29] conducted a prospective study and HRCT had accuracy and sensitivity of 96.4% in detecting location and extension of disease. Buckingham and Valvossori did a study and correlated HRCT findings with surgical findings of cholesteatoma and found that the tomographs accurately predicted the extent of the surgical lesion in most of the cases. 80 of the 100 cases of cholesteatoma correlated well. In the remaining 11 cases, the extent of the cholesteatoma into the antrum and mastoid could not be accurately predicted [30].
Congenital Cholesteatoma, EAC Stenosis and Kertosis Obturans
Thukral et al. [2] conducted a prospective study on 50 patients of ear diseases and they noted the sensitivity and specificity of HRCT to diagnose cholesteatoma preoperatively was 89.29% and 77.22% respectively. Jackler et al. [20] in their study observed sensitivity of 87% and specificity of 66% in detecting cholesteatoma. Maqsood et al. [31] noted 1 case of congenital cholesteatoma in HRCT scan. Similarly, Sankhla et al. [32] noted 1 out of 100 cases as presence of congenital cholesteatoma by HRCT scan.
Thukral et al. [2] noted 1 (11.1%) case of isolated congenital aural atresia on HRCT with normal middle ear and this case had similar operative findings. Sankhla et al. [32] noted 2 cases out of 100, of microtia through HRCT temporal bone. To the best of our knowledge there are only few literatures which described various characteristics of HRCT in detecting aural atresia and microtia.
In conclusion the results of present study described a good consensus between HRCT temporal bone and surgical findings. It reflects that pre-operative HRCT temporal bone is a precise technique for the evaluation of external auditory canal, soft-tissue masses within the air-filled middle ear and mastoid cavities, defining the extent of disease, ossicular chain status, otosclerotic foci and inner ear status including cochlear abnormalities.
Key Message
HRCT temporal bone is useful guide to the surgeon for detection of various temporal bone pathologies, defining their extent, planning of surgery and approach, prognosticating the patient despite its pit fall like radiation exposure.
References
Brogan M, Chakeres DW (1986) Computed tomography and magnetic resonance imaging of the normal anatomy of the temporal bone. In: Seminars in ultrasound, CT, and MR 1989, vol 10, no 3, pp 178–194
Thukral CL, Singh A, Singh S, Sood AS, Singh K (2015) Role of high resolution computed tomography in evaluation of pathologies of temporal bone. Journal of Clinical and Diagnostic Research: JCDR. 9(9):TC07
Parida S, Routray PN, Mohanty J, Pattanaik S (2018) Role of HRCT in temporal bone diseases-a study of 100 cases. JK Science 20(1):34
Dashottar S, Bucha A, Sinha S, Nema D (2019) Preoperative temporal bone HRCT and intra-operative findings in middle ear cholesteatoma: a comparative study. Int J Otorhinolaryngol Head Neck Surg 5(1):77
Kanotra S, Gupta R, Gupta N, Sharma R, Gupta S, Kotwal S (2015) Correlation of high-resolution computed tomography temporal bone findings with intra-operative findings in patients with cholesteatoma. Indian J Otolo 21(4):280
Prakash MD, Tarannum A (2018) Role of high resolution computed tomography of temporal bone in preoperative evaluation of chronic suppurative otitis media. Int J Otorhinolaryngol Head Neck Surg 4(5):1287
Mandal S, Muneer K, Roy M (2019) High resolution computed tomography of temporal bone: the predictive value in atticoantral disease. Indian J Otolaryngol Head Neck Surg 71(2):1391–1395
Payal G, Pranjal K, Gul M, Mittal MK, Rai AK (2012) Computed tomography in chronic suppurative otitis media: value in surgical planning. Indian J Otolaryngol Head Neck Surg 64(3):225–229
Mahmutoglu AS, Çelebi I, Sahinoglu S, Çakmakçi E, Sözen E (2013) Reliability of preoperative multidetector computed tomography scan in patients with chronic otitis media. J Craniofacial Surg 24(4):1472–1476
Gül A, Akdag M, Kinis V, Yilmaz B, Sengül E, Teke M, Meriç F (2014) Radiologic and surgical findings in chronic suppurative otitis media. J Craniofacial Surg 25(6):2027–2029
Rogha M, Hashemi SM, Mokhtarinejad F, Eshaghian A, Dadgostar A (2014) Comparison of preoperative temporal bone CT with intraoperative findings in patients with cholesteatoma. Iran J Otorhinolaryngol 26(74):7
Tatlipinar A, Tuncel A, Öğredik EA, Gökçeer T, Uslu C (2012) The role of computed tomography scanning in chronic otitis media. Eur Arch Otorhinolaryngol 269(1):33–38
Gerami H, Naghavi E, Wahabi-Moghadam M, Forghanparast K, Akbar MH (2009) Comparison of preoperative computerized tomography scan imaging of temporal bone with the intra-operative findings in patients undergoing mastoidectomy. Saudi Med J 30(1):104–108
Keskin S, Çetin H, Gürkan Töre H (2011) The correlation of temporal bone CT with surgery findings in evaluation of chronic inflammatory diseases of the middle ear. Eur J General Med 8(1)
Yildirim-Baylan M, Ozmen CA, Gun R, Yorgancilar E, Akkuş Z, Topcu I (2012) An evaluation of preoperative computed tomography on patients with chronic otitis media. Indian J Otolaryngol Head Neck Surg 64(1):67–70
Ng JH, Zhang EZ, Soon SR, Tan VY, Tan TY, Mok PK, Yuen HW (2014) Pre-operative high resolution computed tomography scans for cholesteatoma: has anything changed? Am J Otolaryngol 35(4):508–513
Rai T (2014) Radiological study of the temporal bone in chronic otitis media: prospective study of 50 cases. Indian J Otol 20(2):48
Gaurano JL, Joharjy IA (2004) Middle ear cholesteatoma: characteristic CT findings in 64 patients. Ann Saudi Med 24(6):442–447
Karki S, Pokharel M, Suwal S, Poudel R (2017) Correlation between preoperative high resolution computed tomography (CT) findings with surgical findings in chronic otitis media (com) squamosal type. Kathmandu Univ Med J 15(57):84–87
Jackler RK, Dillon WP, Schindler RA (1984) Computed tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope 94(6):746–752
Alam-Eldeen MH, Rashad UM (2017) Radiological requirements for surgical planning in cochlear implant candidates. Indian J Radiol Imaging 27(3):274
Júnior LR, Rocha MD, Walsh PV, Antunes CA, Calhau CM (2008) Evaluation by imaging methods of cochlear implant candidates: radiological and surgical correlation. Braz J Otorhinolaryngol 74(3):395–400
Digge P, Solanki RN, Shah DC, Vishwakarma R, Kumar S (2016) Imaging modality of choice for pre-operative cochlear imaging: HRCT vs. MRI temporal bone. J Clin Diagn Res: JCDR 10(10):1
Westerhof JP, Rademaker J, Weber BP, Becker H (2001) Congenital malformations of the inner ear and the vestibulocochlear nerve in children with sensorineural hearing loss: evaluation with CT and MRI. J Comput Assist Tomogr 25(5):719–726
Naumann IC, Porcellini B, Fisch U (2005) Otosclerosis: incidence of positive findings on high-resolution computed tomography and their correlation to audiological test data. Ann Otol Rhinol Laryngol 114(9):709–716
Swartz JD, Faerber EN, Wolfson RJ, Marlowe FI (1984) Fenestral otosclerosis: significance of preoperative CT evaluation. Radiology 151(3):703–707
Shin YJ, Calvas P, Deguine O, Charlet JP, Cognard C, Fraysse B (2001) Correlations between computed tomography findings and family history in otosclerotic patients. Otol Neurotol 22(4):461–464
Kanzara T, Virk JS (2017) Diagnostic performance of high resolution computed tomography in otosclerosis. World J Cli Cases 5(7):286
Gomaa MA, Karim AR, Ghany HS, Elhiny AA, Sadek AA (2013) Evaluation of temporal bone cholesteatoma and the correlation between high resolution computed tomography and surgical finding. Clin Medi Insights: Ear Nose Throat 6: CMENT–S10681
Buckingham RA, Valvassori GE (1970) Tomographic and surgical pathology of cholesteatoma. Arch Otolaryngol. 91(5):464–469
Maqsood S, Dar IH, Bhat SA (2018) Role of high resolution computed tomography in evaluation of temporal bone diseases. IAIM 5(12):15–22
Sankhla AK, Dubey N. Assessment of temporal bone diseases by high resolution computed tomography–institution based study
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics Approval
From institutional ethics committee.
Consent to Participate
Written and informed consent taken from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kataria, T., Sehra, R., Grover, M. et al. Correlation of Preoperative High-resolution Computed Tomography Temporal Bone Findings with Intra-operative Findings in Various Ear Pathologies. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 190–199 (2022). https://doi.org/10.1007/s12070-020-01950-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-01950-6