Abstract
The purpose of this study was to determine the role of high-definition computed tomography (CT) in chronic otitis media (COM) patients and to present which parameters were useful or misleading for preoperative evaluation for management. Fifty cases of COM that underwent preoperative CT scanning at a tertiary referral center were retrospectively analyzed. Their CT scan reports were compared with the operative findings. The patients had undergone tympanoplasty with or without mastoidectomy for COM between April 2008 and January 2010. Patient charts were used to obtain the necessary data. In 62% (31/50) of cases, the CT scan showed the presence of cholesteatoma. Operative findings revealed cholesteatoma in 61.8% (19/31) of these cases. However, when a bone eroding soft tissue mass involved the epitympanum on CT, the presence of cholesteatoma was observed in 83.3% (15/18) of cases intraoperatively. Cholesteatoma was present in the mastoid or middle ear intraoperatively in 77.7% (7/9) of patients with an external ear bony canal defect found on CT. Despite 89.7, 85.29, and 90% agreement ratios for dehiscence of facial canal, lateral semicircular canal, and tegmen, respectively, CT could not detect dehiscence of these anatomic structures successfully. Based on these results, CT scanning has limitations but is a useful adjunct for the surgical management of COM patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomography (CT) imaging of the paranasal sinuses has been accepted as an essential step in the preoperative planning of endoscopic sinus surgery. Although routine CT of the temporal bone before chronic otitis media (COM) surgery is becoming more common, it has not gained wide acceptance as an essential aid to planning this form of surgery.
Historically, COM surgery has been undertaken with otoscopy, audiometry, and plain X-rays as the only preoperative investigations. The advent of high-definition CT scanning in the 1980s has allowed for superb preoperative imaging of temporal bone anatomy and its congenital variations, some evidence of location and extent of the disease, and as a screen for asymptomatic complications due to bony destruction.
However, there are concerns that CT cannot reliably distinguish cholesteatoma from mucosal disease and fluid. In addition, CT lacks a guaranteed sensitivity for erosive complications. It has been suggested that routine preoperative CT scanning before uncomplicated COM surgery is of questionable value [1].
Many experienced otologic surgeons seldom use CT scanning in their patients with COM, arguing that the nature and extent of pathology will become evident during surgical dissection. In contrast, other surgeons believe that a preoperative CT scan may identify potentially dangerous pathologic entities such as dehiscence of the lateral semicircular canal, facial canal dehiscence, erosion of tegmen or dural exposure, or low-lying dura. Prior knowledge about temporal bone anatomy and the extent of disease may help surgeons plan and choose the appropriate type of the surgery (e.g., canal wall up, canal wall down, atticoantrostomy) and avoid complications. In addition, temporal bone CT can be of medicolegal value as it provides preoperative documentation of disease.
The aim of this study is to assess the role of routine CT scanning before COM surgery.
Materials and methods
A series of 50 COM patients with preoperative CT scanning, operated on between April 2008 and January 2010, were included in the study. The mean age of the subjects was 29.20 ± 11.52 years, with a range of 12–66 years; 54% (n = 27) of the patients were females.
Each patient underwent a surgical procedure for treatment of their COM. The patients included in this retrospective study suffered from chronic tympanic membrane perforation and intermittent or refractory otorrhoea. Thirty-four patients had mastoidectomy as a part of their surgery (canal wall down, canal wall up). The results of CT scanning and the intraoperative findings were compared. The evaluation of the CT scan was based on the preoperative reports. The parameters of comparison were the presence of cholesteatoma, granulation tissue, attic blockage, presence of malleus, incus necrosis, lateral semicircular canal erosion, facial canal dehiscence, erosion of tegmen, erosion of the scutum or external ear bony canal, and status (intact or not) of the bony chain of the middle ear. In some patients, details regarding these parameters were missing in the operative notes. In these patients, available data were used for the statistical comparison.
Using Siemens Sensatron 40 equipment, CT scans were performed using 1.5 mm contiguous sections through the temporal bone. Both coronal and axial images were performed. The axial plane was defined as a line from the inferior orbital rim to the external auditory meatus. The coronal plane attempted to come 90o to this line. Because the various components of the temporal bone are often best seen in only one particular axis, we preferred to obtain scans in both planes of view.
Results
The results of the comparison between preoperative CT scanning and intraoperative findings are demonstrated in Table 1.
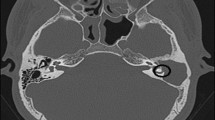
Cholesteatoma was noticed in 46% (23/50) cases intraoperatively. In 62% (31/50) of cases, the CT scan showed cholesteatoma. Surgical findings revealed cholesteatoma in 61.3% (19/31) of these cases. In four cases, although cholesteatoma was diagnosed during surgery, CT results indicated granulation tissue. In the remaining non-cholesteatoma cases, granulation tissue was noticed in 22.5% (7/31) (Fig. 1a). The presence of both abnormal soft tissue densities and the signs of bone erosion were found in 46% (23/50) of patients on CT and proved to be cholesteatoma in 60.8% (14/23) cases intraoperatively. In (17/50) 34% of cases, abnormal soft tissue density was observed in the absence of osseous erosion on CT. In 52.9% (9/17) of these cases, cholesteatoma was observed intraoperatively. The remainder of the cases were related to granulation tissue or fluid. Cholesteatoma was detected in 66.6% (14/21) of the cases where both soft tissue density and ossicular chain erosion were present together in the CT scan. In 20% of cases (10/50), the CT scan revealed no evidence of abnormal soft tissue collection. All of these ears were free of cholesteatoma (Fig. 1b).
CT sections from three patients. a Soft tissue density in mastoid on axial scan (cholesteatoma was reported on CT but was not present intraoperatively). b Pneumatization in the middle ear and mastoid and incudomalleolar joint in the attic region are seen via an axial section (neither CT nor intraoperative findings revealed cholesteatoma in this case). c Soft tissue density in attic region and prussac space and erosion of scutum are seen on coronal scan (both CT and surgery revealed cholesteatoma)
In 26% (13/50) of cases, CT showed a soft tissue mass blocking the attic region, although the surgery revealed no blockage. This ratio was the highest rate of a false positive result by CT scan. Attic blockage was noticed in 25 cases during surgery. Surgical findings revealed that attic blockage resulted from cholesteatoma in 52% of the cases (13/25). Cholesteatoma was noticed intraoperatively in 83.3% (15/18) of cases in which a bone eroding soft tissue mass was involved in the epitympanum on CT (Fig. 1c).
Our detection rate for an external ear bony canal defect was 90%; this was one of the highest ratios reached. In 77.7% (7/9) of these cases, cholesteatoma was present either in the mastoid or middle ear.
The external ear bony canal defect could not be seen on CT in four patients. In one patient, although CT demonstrated the defect, the canal was noticed to be intact intraoperatively.
Dehiscence of the facial nerve mostly was seen on the second part of facial nerve. Although our detection rate for facial nerves was 89.7%, four facial canal dehiscences were not detected.
CT scanning could not detect the lateral canal fistulae present in three cases. Preoperative evaluation of these cases revealed that one had total hearing loss, and the other had severe sensorineural hearing loss. In two cases, although the CT scan was reported as semicircular canal erosion, the canal was noticed to be intact intraoperatively.
Although we used both coronal and axial scans, we could detect tegmen erosion only in 2 out of 4 cases; there were three false positives (Fig. 2).
The heads of the malleus and incus were consistently visualized on both the axial and coronal planes, although the axial was the preferable view. Intactness of the ossicular chain, the presence of malleus, and the presence of incus necrosis were correctly detected by CT at a rate of 85.71, 94, and 86.67%, respectively. On the other hand, ossicular chain intactness could not be detected in seven cases; similarly, the presence of malleus in three cases and incus necrosis in six cases could not be demonstrated.
Discussion
CT scanning is the standard imaging technique for the temporal bone, but its exact role in the preoperative assessment of patients with COM is controversial. The use of preoperative routine temporal CT gives information about anatomy and extent of the disease, and also is important for of medicolegal reasons. However, the cost and exposure to radiation are limitations for routine use. Most otologists reserve scans for selected cases, such as patients with complications related to COM, those with suspected congenital abnormalities, loss of landmarks due to previous surgery, and an inability to visualize the tympanic membrane [2, 3].
To obtain maximum benefit from CT in COM, certain guidelines should be followed. In most cases, it is advisable to obtain two planes of view. It is also important to obtain similarly oriented and processed views of both temporal bones.
One topic of debate with the use of CT in the preoperative evaluation of COM patients is the effectiveness of CT in differentiating cholesteatoma, granulation tissue, and fluid. Soft tissue appearance in the mastoid, attic, and middle ear on CT may be a clue for cholesteatoma. However, granulation tissue and fluid may have a similar appearance. Although cholesteatoma is said to show a lower attenuation than granulation tissue, the difference is subtle, and only magnetic resonance imaging (MRI) can differentiate the two [4]. Although a discrete soft tissue collection involving the epitympanum and antrum found via CT has been highly suggestive of cholesteatoma in the previous reports [4–7], this may well be other benign inflammatory processes, such as granulation tissue or polypoid mucosal hypertrophy.
Our CT scans were able to detect soft tissue masses in the mastoid and middle ear in every case in which they were present. This reflects the experience of many other investigators [4–7]. On the other hand, although CT scans of chronically draining ears demonstrated abnormal soft tissue densities in the middle ear or mastoid in 80% (40/50) of our cases, surgical findings revealed that 57.5% (23/40) of them were cholesteatoma. In addition, there was soft tissue density in the attic area on CT scan in some patients, but only mucosal edema was present intraoperatively. No blockage due to soft tissue was observed during mastoidectomy. It was thought that appearance on CT might be due to recurrent otorrhea at the time of CT scanning. Using preoperative CT, we could not distinguish cholesteatoma from other soft tissue diseases and fluid. Other investigators have had a similar experience [5, 8, 9].
Although it has been reported that the frequency of cholesteatoma is higher in cases with coexistence of soft tissue density and bony erosion on CT scan [6, 8], we could not find that large of a difference between cholesteatoma cases with or without bone erosion. In our series, the presence of both abnormal soft tissue densities and signs of bone erosion were present in 46% (23/50) of patients and proved to be cholesteatoma in 60.8% (14/23) of cases. O’Donoghue et al. [6] and Phelps and Wright [9] reported that this ratio was 80% in their series. On the other hand, we found that if the bone eroding soft tissue mass involved the epitympanum on CT, the presence of cholesteatoma was 83.3% (15/18) intraoperatively. In addition, we noted that coexistence of an external ear bony canal defect and soft tissue density on CT may be a sign of cholesteatoma. Cholesteatoma was present in the mastoid or middle ear intraoperatively in 77.7% (7/9) of patients with an external ear bony canal defect found on CT.
When planning revision surgery, especially after intact canal wall procedures, residual diseased air cells in the sinodural angle, tegmen, mastoid tip, and petrous apex together with recurrent cholesteatoma can be demonstrated by CT. In the postoperative ear, it is argued that imaging can replace the “second look” tympanotomy [8]. Voorhees et al. [10] reported that a postoperative CT study which shows no evidence of unusual soft tissue within the mastoid or middle ear cleft indicates the probable absence of a significant sized cholesteatoma. We believe that patient symptoms (e.g., otalgia, discharge, vertigo), otoscopic/microscopic examination (e.g., the status of middle ear mucosa, the presence of cholesteatoma or discharge) and temporal CT evaluation can be used together to decide on the need for revision surgery. In our study, the CT scan revealed no evidence of abnormal soft tissue collection in 20% of cases (10/50). All of these ears were free of cholesteatoma.
Ossicles are generally observed with temporal CT; however, although the long processes of the malleus and incus and the stapes superstructure were the components most at risk in COM, they were only sporadically seen on axial scans and rarely imaged in the coronal plane. For this reason, we had to include in our study the presence of malleus, the presence of incus necrosis, and the intactness of the ossicular chain as parameters to evaluate the status of ossicles. In the literature, O’Reilly et al. [5] correctly predicted an intact ossicular chain in only 50% of cases. Mafee et al. [4] were able to define the state of ossicular chain in 89% of cases. In our series, the status of ossicular chain was correctly detected by CT at a rate of 85.1%.
The wise surgeon will always approach danger areas, such as the lateral semicircular canal, tegmen, the facial nerve, and stapes footplate, with caution. However, one can only detect bone erosion and abnormal exposure by dissection of cholesteatoma from these structures, with obvious hazards. If forewarned, the operator may decide to leave the cholesteatoma matrix as a protective cover, which becomes harmless once exteriorized. Temporal CT may show erosion of the tegmen, semicircular canal, and fascial canal in the preoperative evaluation and may alert the surgeon about possible complications. The tegmen is better visualized on coronal CT scans where it appears as a thin bony plate overlying the epitympanum and mastoid. It has been reported that the best technique to detect erosion of a bony canal of a facial nerve is to view it with multiple cross-sectional slices [5]. For this reason, a coronal scan is preferred for the horizontal portion of the fascial nerve, while an axial scan is the view of choice for the vertical portion.
The thin bone overlying the facial nerve and that forming the tegmen plate is difficult to assess because of partial volume averaging with adjacent soft tissue. It has been reported that the normal CT appearance of the tegmen frequently gives the false impression of dehiscence, especially where it forms the roof of the epitympanum [8]. MRI can confirm suspicion of defects in the tegmen tympani or dural plate on CT and is of special value to diagnose cerebral herniation [11]. Jackler et al. [8] detected all four of their cases of tegmen erosion but also had eight false positives. Mafee et al. [4] missed 3 out of 6 cases and had no false positives, and O’Reilly et al. [5] detected 5 out of 11 cases and had six false positives. Facial canal dehissence and tegmen erosion could not be demonstrated at a high rate in our series. We detected tegmen erosion in 2 out of 4 cases, but there were three false positives; additionally, we could not detect four facial canal dehiscence successfully.
Similarly, CT was not reported to be successful in the determination of fascial canal dehiscence in some previous studies. O’Reilly et al. [5] detected 4 out of 9 cases. Freng et al. [12] reported 1 in 4 cases. Although O’Donoghue et al. [6] were successful in finding all nine of their facial canal dehiscences, they also had six false positives.
Sheehy et al. [13] reported that lateral canal fistulae occured in about 10% of COM cases. Cholesteatoma can occasionally erode the lateral semicircular canal (LSCC) where it lies exposed on the medial wall of the antrum. It is important to detect erosion of the LSCC because fenestraton of LSCC may cause severe sensorineural hearing loss and vestibular dysfunction. If the surgeon had prior knowledge of the probability of lateral semicircular canal dehiscence, he/she would probably be more careful during dissection of the cholesteatoma from LSCC, and would not take the risk of getting the cholesteatoma matrix from this region. Preoperatively, the LSCC can be visualized full length on an axial CT scan and via a cross-section coronally. Unfortunately, our CT scan detected none of the three lateral canal fistulae. In addition, in two cases, although the CT scan was reported as a semicircular canal erosion, the canal was noticed to be intact intraoperatively. In contrast, O’Reilly et al. [5] detected 6 out of 8 cases and had a false positive rate of 3.5%. On the other hand, Jackler et al. [8] had a high incidence of false positives.
Despite its advantages, CT has a number of limitations. These include the inability of imaging to differentiate cholesteatomas from granulations, mucosal edema, or even effusion; a relative lack of sensitivity in providing data about complications such as a fistula or dehiscent facial nerve; and the difficulty in obtaining CT scans in those where it is most indicated (e.g., during emergencies, in children).
However, CT has some advantages in evaluating COM patients preoperatively compared with traditional methods. The most important advantage of CT over traditional radiographic techniques is its ability to provide excellent anatomic detail of both bony and soft tissue structures. Having prior knowledge of temporal bone anatomy and its relationship with the adjacent anatomical structures (e.g., dura, sigmoid sinus, jugular bulb), mastoid cellularity, extent of disease, and possible complications due to erosion of bony structures may determine surgeons’ decisions about the type of the surgery (i.e., intact canal wall vs. open techniques and the small cavity attico-antrostomy approach) [14]. The closed intact canal wall approach requires wide access, ideally through a large cellular mastoid, while the canal wall down approach is preferable in the small sclerotic system, which is commonly associated with cholesteatomas in adults. Low-lying dura lateral to the attic and anteriorly located sigmoid sinus are also potential hazards.
A discussion of CT images, demonstrating the course of the facial nerve, the relationship of the inner ear, and the damage to the ossicles can be of great help in preoperative counseling [15]. Such scans can illustrate both the need for and the hazards of surgery. Coronal scans are understood easily by the patient.
Interpretation of CT scans obviously requires an otologist prepared to benefit from the knowledge of an expert radiologist. With time, the surgeon and radiologist gain increased experience with correlating CT with eventual surgical findings.
In our practice, a CT evaluation has become the norm prior to the majority of chronic ear surgeries. This evaluation is especially helpful to obtain information about attico-antral pathology and to make a decision about the need for mastoid surgery.
Summary and Conclusion
Several conclusions were derived based on our study results:
-
CT is helpful in determining the anatomy of the middle ear and mastoid and the extent of the disease.
-
CT is useful for follow-up of residual or recurrent cholesteatoma after ear surgery. It also is helpful in making decisions regarding revision surgery.
-
CT cannot reliably distinguish cholesteatoma from mucosal disease and fluid.
-
Coexistence of soft tissue density in the epitympanic region and bone erosion is suggestive of cholesteatoma.
-
Coexistence of an external ear bony canal defect and soft tissue density may indicate cholesteatoma.
-
The total absence of abnormal soft tissue on CT scan essentially excludes cholesteatoma.
-
CT occasionally gives the erroneous impression of lateral semicircular canal fistulization, tegmen tympani erosion, and facial nerve involvement due to volume averaging of the thin bony covering of these structures with adjacent soft tissues.
-
CT may affect the decision regarding the type of operation (mastoid pneumotisation, attic blockage/intact canal wall, canal wall down, atticoantrotomy) and can provide surgeons with a warning about possible difficulties due to anatomical variations (e.g., low-lying dura, anteriorly placed sigmoid sinus). This could help prevent surgical complications.
Although our study was retrospective in nature, we believe it has revealed some of the practical uses of CT scanning. We conclude that CT scanning has limitations, but that it is a useful adjunct for the surgical management of COM patients.
References
Walshe P, Walsh RM, Brennan P, Brennan P, Walsh M (2002) The role of computerized tomography in the preoperative assesment of chronic suppurative otitis media. Clin Otolaryngol Allied Sci 27:95–97
Yates PD, Flood LM, Banerjee A, Clifford K (2002) CT scanning of middle ear cholesteatoma: what does the surgeon want to know? Br J Radiol 75:847–852
Leighton SEJ, Robson AK, Anslow P et al (1993) The role of CT imaging in the management of chronic suppurative otitis media. Clin Otolaryngol 18:23–29
Mafee MF, Levin BC, Applebaum EL, Campos M, James CF (1988) Cholesteatoma of middle ear and mastoid. A comparison of the CT scan and operative findings. Otolaryngol Clin North Am 2:265–293
O’Reilly BJ, Chevretton EB, Wylie I et al (1991) The value of CT scanning in chronic suppurative otitis media. J Laryngol Otol 105:990–994
O’Donoghue GM, Bates GJ, Anslow P et al (1987) The predictive value of high resolution computerized tomography in chronic suppurative ear disease. Clin Otolaryngol 12:89–96
Alzoubi FQ, Odat HA, Al-balas HA, Saeed SR et al (2009) The role of preoperative CT scan in patients with chronic otitis media. Eur Arch Otorhinolaryngol 266:807–809
Jackler RK, Dillon WP, Schindler RA (1984) Computed tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope 94:746–752
Phelps PD, Wright A (1990) Imaging cholesteatoma. Clin Radiol 41:156–162
Voorhees R, Johnson D, Lufkin RB, Hanafee W, Canalis R (1983) High resolution CT scanning for detection of cholesteatoma and complication in the postoperative ear. Laryngoscope 93:589–595
Martin N, Sterkers O, Murat M, Hahum N (1989) Brain herniation into the middle ear cavity: MR imaging. Neuroradiology 31:184–186
Freng A, Larsen PL, Nordhus T (1988) Cholesteatomas of the temporal bone. Preoperative CT versus preoperative findings. Scand Audiol Suppl 30:185–188
Sheehy JL, Brackmann DE, Graham MD (1977) Complications of cholesteatoma: a report on 1024 cases. In: McCabe BF, Sade J, Abramson M (eds) First International Conference on Cholesteatoma. Aesculapius, Birmingham, pp 420–429
Banerjee A, Flood LM, Yates P et al (2003) Computed tomography in suppurative ear disease: does it influence management? J Laryngol Otol 117:454–458
Watts S, Flood LM, Clifford K (2000) A systematic approach to interpretation of computed tomography scans prior to surgery of middle ear cholesteatoma. J Laryngol Otol 114:248–253
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tatlipinar, A., Tuncel, A., Öğredik, E.A. et al. The role of computed tomography scanning in chronic otitis media. Eur Arch Otorhinolaryngol 269, 33–38 (2012). https://doi.org/10.1007/s00405-011-1577-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1577-z