Abstract
This study aimed to compare the veracity of computed tomography findings on patients undergoing surgery for chronic otitis media (COM) with the surgical findings, and to determine to what extent the preoperative computerized tomography (CT) findings are useful to the surgeon. A series of 56 patients with COM undergoing preoperative CT scanning followed by surgical exploration of the middle ear and mastoid. Operative notes were recorded and data collected on the nature of soft tissue masses, the status of the ossicles, presence or absence of facial canal dehiscence and semicircular canal (SCC) dehiscence and the presence or absence of dural plate erosion, and sigmoid sinus thrombosis. Fifty-six patients were recruited in the study, 30 males and 26 females. The age range was from 16 to 67 years with a mean of 26.51 ± 1.4 years. The preoperative CT scan imaging in cases of cholesteatoma, ossicular chain erosion and SCC dehiscence have good correlation with the intraoperative findings. The specificity of preoperative CT scan in detecting facial canal dehiscence, dural plate erosion and sigmoid sinus thrombosis in patient of COM were weak. Preoperative computed tomography evaluation is fairly useful especially in cases of cholesteatoma. According to the results of this study, CT is of value particularly in the definition of cholesteatoma, and in determining ossicular chain erosion and semicircular canal fistula.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgery is widely used to treat various pathologic conditions of the middle ear such as chronic otitis media including cholesteatoma, otosclerosis, congenital malformations, traumas, tumors, etc., [1]. The decision for the choice of surgical technique is of particular importance to preserve a higher hearing rate and prevent complications such as infection, cerebral hernia, recurrence, and treatment failure [2, 3]. Imaging of the temporal bone, with CT and magnetic resonance imaging (MRI), is playing an increasingly important role for diagnosis, surgical decision, and follow up. Evidence of location and extent of disease and of asymptomatic complications, secondary to bony destruction should also influence management. Computerized tomography can undoubtedly provide reliable details of temporal bone anatomy and its congenital malformations. However, there are concerns that CT can not reliably distinguish cholesteatoma from mucosal disease and that it lacks guaranteed sensitivity for erosive complications. Such concerns have cast doubts on its value [4].
The aim of this study is to evaluate preoperative CT scanning and to determine the accuracy and the usefulness of this imaging methods in patients with COM undergoing surgery.
Material and Methods
This prospective study was conducted between 2006 and 2009 in the Department of Otolaryngology. A series of 56 patients with COM underwent preoperative CT scanning followed by surgical exploration of the middle ear and mastoid. Patients with revision surgery, history of temporal bone fracture, known cases of temporal bone neoplastic/granulomatic disease, and cases unsuitable for surgery or scanning (such as ischemic heart disease or pregnancy) were excluded. Radiographs were evaluated with particular reference to those anatomic structures important in the preoperative evaluation of COM and without knowledge of the operative findings. Operative notes were recorded and data collected on the nature of soft tissue masses, the status of the ossicles, the presence or absence of facial canal dehiscence and semicircular canal dehiscence and the presence or absence of dural plate erosion, and sigmoid sinus thrombosis. The surgery was carried out by four specialist surgeons. All the scans were reported or verified by single senior radiologist.
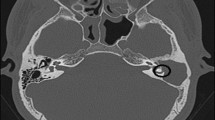
The CT scanner used in the study was multiscan Philips Brilliance; contiguous sections (1 mm thick) were obtained in the axial plane with bone window.
Results
Fifty-six patients were recruited in the study, 30 males and 26 females. The age range was from 16 to 67 years with a mean of 26.51 ± 12.4 years. Radical mastoidectomy was performed on 12 patients, modified radical mastoidectomy on 12 patients, and simple mastoidectomy with or without tympanoplasty on 42 patients.
At surgery, cholesteatoma was present in 19 out of 56 patients (33.9%). There were 18 patients (94.7%) in whom the cholesteatoma was predicted correctly by the CT scan, and 34 patients (91.9%) where it was excluded correctly. In one patient (5.3%) it was excluded by CT scan but was present at surgery. From the above data, the sensitivity of the scan in detecting cholesteatoma is 91.9%, specificity is 94.7%, positive predictive value is 97.1%, negative predictive value is 85.7% (Tables 1, 2; Fig. 1).
Ossicular chain erosion was present in 28 out of 56 patients. Ossicular chain erosion was reported on 29 of the 56 CT scans. There were 24 patients in whom the ossicular chain erosion was predicted correctly by the CT scan, and 23 patients where it was excluded correctly. In five patients it was excluded by CT scan but was present at surgery. From the above data, the sensitivity of the scan in detecting ossicular chain erosion is 82.1%, specificity is 85.7%, positive predictive value is 85.2%, negative predictive value is 82.8% (Table 3; Fig. 1).
During surgery, semicircular canal dehiscence was seen to be present in three out of 56 patients. Semicircular canal dehiscence was reported on four of the 56 CT scans. There were three patients in whom the semicircular canal dehiscence was predicted correctly by the CT scan, 52 patients where it was excluded correctly, two patients where it was predicted incorrectly and in the remaining one patient it was excluded by CT scan but was present at surgery. From the above data, the sensitivity of the scan in detecting semicircular canal dehiscence is 98.1%, specificity is 75.0%, positive predictive value is 98.1%, negative predictive value is 75% (Table 4; Fig. 1).
The ability of the scan to detect the involvement of other structures was variable. The results are shown in Tables 1, 5, 6, 7 and Fig. 1.
Discussion
The exact role of CT in the preoperative assessment of patients with chronic otitis media is controversial [5]. Some authors have reported a high degree of accuracy in the pathological diagnosis of ossicular chain and inner ear conditions [6] and others have concluded that CT has poor ability to diagnose cholesteatoma and should not be relied on to visualize abnormalities of the previously mentioned structures [7]. The results of this study suggest that cholesteatoma can be accurately diagnosed by computed tomography. The hallmarks of cholesteatoma on CT scan are the bone erosion and smooth expansion with soft tissue mass. Conversely, one should be aware of the limitations of CT to pick out early or limited disease, since it is difficult to diagnose cholesteatoma on the scan if the soft tissue mass is not associated with bone erosion [8].
Our study results are similar to those in literature [9–11]. Where our results differ is that some studies maintain that CT is not sufficient to diagnose cholesteatoma [1, 5]. Computerized tomography may give an incorrect diagnosis in the early stage of cholesteatoma. We believe that this may be the reason for the difference in literature.
While a definitive diagnosis of cholesteatoma can only be made at the time of surgery, the scan picture may at times influence the decision and timing of surgical exploration. Scan evidence of cholesteatoma with significant bony destruction or other complications could prompt the surgeon to operate earlier, particularly if polyps or a tortuous bony canal obscures visualization of the tympanic membrane and hinders clinical diagnosis. On the other hand, the threshold to explore the ear may be higher when the scan is non-confirmatory, particularly if the patient has medical risk for surgery [9]. Therefore, CT findings enable the surgeon to be informed of the risk factors and to be prepared for the possibility of complications.
Our study confirmed that CT is substantially reliable in the determination of the status of the ossicular chain. This result conforms with other studies [6, 9, 10]. Presurgical knowledge of the status of the ossicular chain would allow the surgeon to be ready for ossicular chain reconstruction and to better advise the patient on the degree of hearing attainable after surgery.
According to the results of our study, CT gives a good idea about the dehiscence of the semicircular canal. Thus, it warns the surgeon to take more care during the operation. Preoperative CT can give the surgeon information about the possibility of bone fistula in the area of the cholesteatoma matrix to be dissected.
In this study, there was low CT sensitivity in determining sigmoid sinus thrombosis. We believe that the reason for this is the dose at which the CT of the temporal bone was taken.
Financial cost, radiation dosage, the inability to differentiate between granulation, effusion or mucosal oedema, the lack of specificity to facial canal dehiscence, dural erosion, and sigmoid sinus thrombosis are all controversial points of CT scans. Despite the limitations, the results of this study suggest that radiological scanning is useful. In as much as CT scanning is of benefit to the surgeon, we believe there are strings attached. Some studies have emphasized the importance of preoperative CT evaluation [12, 13]. The results of the study by Reilly et al. [14] were similar to ours. They concluded that CT is sensitive to the presence of soft tissue disease and bone erosion, moderately sensitive to the presence of lateral canal fistulae but less sensitive to the presence of small areas of exposed dura, ossicular continuity and facial canal dehiscence.
In conclusion, the results of this study suggest that the preoperative CT scan imaging in cases of cholesteatoma, ossicular chain erosion, and SCC dehiscence have good correlation with intraoperative findings. However, the there was weak specificity of the preoperative CT scan in detecting facial canal dehiscence, dural plate erosion, and sigmoid sinus thrombosis in COM patients. CT of the temporal bone is therefore a useful guide to the surgeon in managing patients with COM. We believe that CT is a guide as to the nature of the disease (destructive/non-destructive), potential dangers (such as SCC fistula) and possible complications and this information can assist the surgeon in the choice of surgery to be performed (simple or radical mastoidectomy, with or without tympanoplasty).
References
Alzoubi FQ, Odat HA, Al-Balas HA, Saeed SR (2009) The role of preoperative CT scan in patients with chronic otitis media. Eur Arch Otorhinolaryngol 266:807–809
Singh B, Maharaj TJ (1993) Radical mastoidectomy: its place in otitic intracranial complications. J Laryngol Otol 107:1113–1118
Dhooge IJ, Vandenbussche T, Lemmerling M (1998) Value of computed tomography of the temporal bone in acute otomastoiditis. Rev Laryngol Otol Rhinol (Bord) 119:91–94
Banerjee A, Flood LM, Yates P, Clifford K (2003) Computed tomography in suppurative ear disease: does it influence management? J Laryngol Otol 117:454–458
Walshe P, McConn Walsh R, Brennan P, Walsh M (2002) The role of computerized tomography in the preoperative assessment of chronic suppurative otitis media. Clin Otolaryngol Allied Sci 27:95–97
O’Donoghue GM, Bates GJ, Anslow P, Rothera MP (1987) The predictive value of high resolution computerized tomography in chronic suppurative ear disease. Clin Otolaryngol Allied Sci 12:89–96
Garber LZ, Dort JC (1994) Cholesteatoma: diagnosis and staging by CT scan. J Otolaryngol 23:121–124
Jackler RK, Dillon WP, Schindler RA (1984) Computed tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope 94:746–752
Chee NW, Tan TY (2001) The value of pre-operative high resolution CT scans in cholesteatoma surgery. Singap Med J 42:155–159
Mafee MF, Levin BC, Applebaum EL, Campos M, James CF (1988) Cholesteatoma of the middle ear and mastoid: a comparison of CT scan and operative findings. Otolaryngol Clin N Am 21:265–293
Gerami H, Naghavi E, Wahabi-Moghadam M, Forghanparast K, Akbar MH (2009) Comparison of preoperative computerized tomography scan imaging of temporal bone with the intra-operative findings in patients undergoing mastoidectomy. Saudi Med J 30:104–108
Watts S, Flood LM, Clifford K (2000) A systematic approach to interpretation of computed tomography scans prior to surgery of middle ear cholesteatoma. J Laryngol Otol 114:248–253
Jang CH, Wang PC (2004) Preoperative evaluation of bone destruction using three-dimensional computed tomography in cholesteatoma. J Laryngol Otol 118:827–829
O’Reilly BJ, Chevretton EB, Wylie I, Thakkar C, Butler P, Sathanathan N et al (1991) The value of CT scanning in chronic suppurative otitis media. J Laryngol Otol 105:990–994
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yildirim-Baylan, M., Ozmen, C.A., Gun, R. et al. An Evaluation of Preoperative Computed Tomography on Patients with Chronic Otitis Media. Indian J Otolaryngol Head Neck Surg 64, 67–70 (2012). https://doi.org/10.1007/s12070-011-0271-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-011-0271-1