Abstract
Eustachian tube appears to be central to the pathogenesis of all forms of otitis media. The reported frequency of bilateral disease ranges from 27 to 55%. The affected ear may well be the end point of the pathology in the contra lateral ear (CLE). Cross sectional observational study. One hundred patients who had unilateral chronic otitis media (COM) were enrolled in the study. Diseased ear was divided into either mucosal or squamosal type. Otoendoscopy, pure tone audiometry, impedance audiometry and X-ray mastoid (Schuller’s view) findings of CLE were noted. Considering all the changes including tympanic membrane, X-ray mastoid, hearing assessment and tympanometry, we found that 70% of patients had alterations in the CLE. Our study was consistent with many previous studies that there was an increased risk of COM in the CLE of unilateral COM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The diagnosis of COM implies permanent abnormality of the pars tensa or flaccida, most likely a result of earlier acute otitis media, negative middle ear pressure or otitis media with effusion [1]. Prevalence of COM in India comes to about 5.7% [2] COM etiology is multifunctional and complex. One of the theories regarding the pathogenesis is the continuum which describes otitis media as dynamic and continuous sequence of events, initiated by an insult, probably functional obstruction of the eustachian tube (ET), which when not managed properly, can lead to irreversible alterations in the middle ear cleft [3]. It suggests that the earlier phases of otitis media may progress over time into more advanced pathologies [4]. The affected ear may well be the end point of the pathology in the CLE.
Materials and Methods
The study was conducted at ABVIMS & Dr. Ram Manohar Lohia Hospital, New Delhi after obtaining the ethical clearance. One hundred Patients, aged 16–60 years, with unilateral COM were included. Patients never had any aural symptoms in the healthy ear. The diseased ear was divided as Mucosal or Squamosal COM. Otoendoscopic, Audiometric and X-ray Mastoid (Schuller’s view) findings of CLE were noted. HRCT findings of CLE in cases of Squamosal type of COM were also noted.
Otoendoscopic findings noted as:
-
(a)
Retraction
-
(b)
Thinning
-
(c)
Tympanosclerosis (TS)
-
(d)
Effusion.
Result
We found that 70% of all patients had CLE changes. In mucosal COM, 24 out of 34 patients had at least one abnormal finding in CLE (Table 1) where as in squamosal COM 46 out of 66 patients had the opposite ear involvement (Table 2). There was no statistically significant difference between Mucosal and squamosal COM.
In mucosal type, 41.17% cases had an abnormal TM. Pars Tensa (PT) retraction was the most common followed by TS patch. Thinnning of TM was seen in four patients. Only one patient had Pars Flaccida (PF) retraction (Table 3).
In squamosal disease, the retraction of PT was most common (36.36%), followed by retraction of PF (12.12%), TS (9.09%) and Thinning of TM (7.57%) (Table 4).
CLE ear was pneumatized in 59% of total cases. 54.5% of CLE were pneumatised in squamosal cases as compared to 67.6% in mucosal cases (Table 5). Only 14% of the mastoids were pneumatized in diseased ear, with lower percentage of pnematisation seen in the diseased ear of squamosal cases (Table 6).
70% of the CLE had no hearing impairment. When present, Squamosal cases had a slight increased incidence of hearing impairment.
We found significant correlation between CLE X-ray mastoid and TM findings (Table 7).
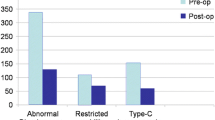
80% of the cases had normal tympanometry finding. Mucosal disease had higher incidence of B & C type curve. Tympanometry findings of CLE were also significantly correlated with TM finding.
Discussion
In our study, 66% of patients had unilateral squamosal disease and majority of patients (61%) had involvement of right ear. The mean age of duration of symptoms was 4.27 years. Numerous studies had been done to study the CLE in unilateral COM since Chalton and Sterns [5] performed the first study in 1984. Our results were similar to the study by Vartiainen et al. [6] who found 67% of the patients having CLE changes however; they found atrophy of the PT, and TS as the most common abnormal findings, followed by PT and PF retractions. We found lesser incidence of otoscopic CLE change as compare to the study conducted by Jadia et al. [7]. Our study results were also similar to study by Adhikari et al. [8] where 71.4% patients had abnormal CLE. The most common finding, in both group of patients, was retraction of the tympanic membrane followed by TS.
Our study showed 30% of cases had hearing impairment, majority being mild conductive hearing loss (63%). Munish et al. [9] had audiological evaluation which revealed similar finding with 32% patients in CLE. Damghani et al. [10] and Chung et al. [11] found 48% and 40% patients having impaired hearing in CLE, respectively.
As far as the radiology of contralateral ear is concerned, we found pneumatisation in 60% of patients while partial pneumatisation and sclerosed mastoid were seen in 40% patients, which are coherent with the finding of Silva et al. [12], Jadia et al. [7] and Damghani and Barazin [10]. We found significant correlation between X ray mastoid findings of CLE with the CLE TM findings. 20% of patient had abnormal tympanometric findings in CLE which is similar to the studies of Damghani and Barazin [10] and Jadia et al. [7] where similar changes were seen in 38% and 28% respectively. Munish et al. with 20.7% also had similar finding as our study.
HRCT temporal bone scan of two cases of squamosal COM showed soft tissue density in the the region of attic and epitympanum in the CLE.
Previous studies have predominantly focused on the condition of the CLE via otoscopy, but in our study we used PTA, tympanometry, and radiography in addition to otoscopy for the evaluation of the CLE in COM. These addition evaluation have led us to a higher percentage of CLE changes and giving us more insight regarding the disease.
Conclusion
Considering all changes, 70% of our patients had alterations in the CLE. There was higher incidence of PF retraction in the CLE of patients with squamosal type of COM. However we could not find any significant difference, in terms of changes in tympanic membrane of CLE, between mucosal and squamosal disease. This study was consistent with many previous studies that supported the theory that there was an increased risk of COM in the CLE of unilateral COM.
Limitations
We could not compare the severity of the changes in the CLE with respect to the extent and the location of the disease in the affected ear.
Key Message
We emphasize the importance of early treatment of any suspicious lesions, and continuous follow-up to look for any changes even after diseased ear has been treated.
References
Tong M, Van Hasselt C (2008) Otitis media with effusion in adults. In: Gleeson M (ed) Scott-Brown’s otorhinolaryngology: head and neck surgery, 7th edn. CRC Press, Boca Raton, pp 3388–3394
Santoshi Kumari M, Madhavi J, Bala Krishna N, Raja Meghanadh K, Jyothy A (2016) Prevalence and associated risk factors of otitis media and its subtypes in South Indian population. Egypt J Ear Nose Throat Allied Sci 17(2):57–62
Yoon TH, Schachern PA, Paparella MM, Lindgren BR (1990) Morphometric studies of the continuum of otitis media. Ann Otol Rhinol Laryngol 99(6_suppl):23–27
Rosito LPS, da Costa SS, Schachern PA, Dornelles C, Cureoglu S, Paparella MM (2007) Contralateral ear in chronic otitis media: a histologic study. Laryngoscope 117(10):1809–1814
Chalton RA, Stearns MP (1984) The incidence of bilateral chronic otitis media. J Laryngol Otol 98(4):337–339
Vartiainen E, Kansanen M, Vartiainen J (1996) The contralateral ear in patients with chronic otitis media. Am J Otol 17(2):190–192
Jadia S, Mourya A, Jain L, Qureshi S (2016) Pre and post operative status of contralateral ear in unilateral chronic otitis media. Indian J Otolaryngol Head Neck Surg 68(1):20–24
Adhikari P, Khanal S, Bhatta R, Sigdel S, Baral D (2009) Status of contralateral ear in patients with chronic otitis media. Internet J Health 10(2)
Munish KS (2017) Type of chronic suppurative otitis media as prognostic indicator for contralateral ear pathology—an observational study. Med Innov 6(1):1–3
Damghani MA, Barazin A (2013) Alterations in the contra lateral ear in chronic otitis media. Iran J Otorhinolaryngol 25(71):99–102
Chung JH, Lee SH, Min HJ, Park CW, Jeong JH, Kim KR (2014) The clinical and radiological status of contralateral ears in unilateral cholesteatoma patients. Surg Radiol Anat 36(5):439–445
da Silva MNL, dos Muller JS, Selaimen FA, Oliveira DS, Rosito LPS, da Costa SS (2013) Tomographic evaluation of the contralateral ear in patients with severe chronic otitis media. Braz J Otorhinolaryngol 79(4):475–479
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declare conflicts of interest.
Ethical Standard
Ethical clearance was obtained from the Institutional Ethical Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thampi, M., Gupta, A., Sen, K. et al. Evaluation of Contralateral Ear in Unilateral Chronic Otitis Media: Necessary or Not?. Indian J Otolaryngol Head Neck Surg 74 (Suppl 1), 62–65 (2022). https://doi.org/10.1007/s12070-020-01824-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-01824-x