Abstract
This study was conducted to evaluate the existence of otoscopic abnormality, hearing status and radiological changes in contralateral ear of patients with chronic otitis media. 300 patients having unilateral Chronic Otitis Media attending OPD in the Department of Otorhinolaryngology, Institute of Medical Sciences, Banaras Hindu University, Varanasi during the period of March 2019 to March 2020 were selected. Otoscopy, Pure Tone Audiometry and Bilateral X-ray mastoids (lateral oblique view) and/or HRCT Temporal bone were done. Contralateral ear was affected in more than 30% cases. Out of 188 patients having Mucosal COM, 58 cases (30.9%) had abnormal TM. Out of 112 patients having Squamosal COM, 48 cases (42.9%) had abnormal CLE. Out of 300 cases, 231 (77.0%) of them had normal hearing in contralateral ear. It was followed by 65 cases (21.6%) with conductive hearing loss. Mixed hearing loss and SNHL were seen in 2 patients each. In contralateral ear of Mucosal COM, pneumatic pattern of pneumatisation was seen in 69.1% followed by Diploic pattern (30.9%). In squamosal COM, X-ray mastoid showed pneumatic pattern (64.3%) followed by Diploic pattern (33.9%) in the contralateral ear. Sclerotic pattern was seen in only 1.8% of cases in contralateral ear. Chronic otitis media as a disease is not limited to one ear. The precise and critical evaluation of both ears does not play a role in prognostic evaluation of the patient only, but it can also serve as a guide for early detection of probable evolution of the disease process in a patient in contralateral ear with unilateral chronic otitis media.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic Otitis Media (COM) implies a permanent abnormality of Pars tensa or Pars flaccida, most likely as a result of earlier Acute Otitis Media (AOM), negative middle ear pressure or Otitis Media with Effusion [1]. WHO estimated that 65–330 million people are worldwide affected by COM, of whom 50% suffer from hearing impairment and approximately 28,000 death per annum are attributable to the complications of Otitis Media [2]. Contralateral ear in this study is defined as the asymptomatic ear in the setting of unilateral chronic otitis media. Unilateral chronic otitis media in true sense is a rare event as evident from previous studies, chronic otitis media frequently involves both ears as many factors implicated in the pathogenesis of the disease affect a common drainage area i.e., nasopharynx. Evaluation of contralateral ear will throw a torch on the status of the asymptomatic ear which may show variable degree of drift from normalcy, indicator of an ongoing process leading to frank disease.
The aim of this study was clinical, audiological and radiological assessment of contralateral ear with both mucosal and squamosal type of chronic otitis media.
Materials and Methods
Ethical clearance was obtained from institutional ethical committee. 300 patients having unilateral Chronic Otitis Media attending OPD in a tertiary care centre during the period of March 2019–March 2020 were selected using random number table.
Patients having history of long-standing ear discharge associated with tympanic membrane perforation or retraction were selected after having informed consent. The patients belonging to age groups more than 10 years, irrespective of sex and of various socioeconomic status were included in the study. The Patients with perforation in both ears, congenital ear malformation in either ear previous history of surgery or grommet insertion in contralateral ear, or trauma to either ear were excluded from the study. Detailed history was taken followed by clinical examination, Otoendoscopy and Otomicroscopy and Pure Tone Audiometry were done. Bilateral X-ray mastoids (lateral oblique view) was done. HRCT Temporal bone was considered where relevant. Presence or absence of perforation in tympanic membrane, cholesteatoma, tympanosclerosis/thin TM and retraction and its grading if present were recorded. Retraction in pars tensa was classified according to Sadé and Berco [3] and that of pars flaccida according to Tos et al. [4] Imaging examinations, X-Ray mastoid (Schuller’s view) was done to have an idea of mastoid pneumatisation and certain anatomical structures. HRCT temporal bone was obtained wherever required. All the subjects with unilateral COM were divided into two groups i.e., either mucosal type or squamosal type. CLE was evaluated as normal or abnormal. CLE is again classified according to their otoscopic findings. That may be normal, fluid in the middle ear, tympanosclerosis, retraction of pars tensa and pars flaccida, granulation, atelectasis and healed thin membrane [5]. Pure tone audiometry was done to assess the type and degree of hearing loss; and was graded as per WHO classification. Data were compiled, stored and analysed using SPSS statistical software.
Result
Total 300 patients were included in the study, out of which 188 patients had Mucosal COM and 112 patients had Squamosal COM (Fig. 1), 40.0% were males and 60.0% were females.
Out of 188 patients having Mucosal COM, 58 cases (30.9%) had abnormal TM (Fig. 2) whereas TM was normal in 130 cases in CLE. Single abnormality of TM included thin TM (19 cases), TSP (14 cases) and retraction pockets (8 cases). 17 cases had two abnormalities consisting of 12 cases with TSP and thin TM, rest 5 cases had TSP in addition to retraction pockets. Out of 13 cases of Mucosal COM having retraction pocket in contralateral ear, grade 2 retraction pockets were seen in 7 patients whereas 4 patients had grade 1 retraction pocket. Two patients had grade 3 retraction pockets.
Out of 112 patients having Squamosal COM, 48 cases (42.9%) had abnormal CLE (Fig. 3). Single abnormality of TM included TSP (14 cases), thin TM (10 cases) and retraction pockets (12 cases). 12 cases had two abnormalities consisting of 6 cases with TSP and thin TM, rest 6 cases had TSP in addition to retraction pockets.
Out of 18 cases of Squamosal COM having retraction pocket in contralateral ear, 11 of them had grade 3 retraction pocket, 4 cases had grade 2 retraction pockets whereas rest 3 had grade 4 retraction pockets.
Out of 300 cases, 231 (77.0%) of them had normal hearing in contralateral ear. It was followed by 65 cases (21.6%) with conductive hearing loss. Mixed hearing loss and SNHL were seen in 2 patients each.
In patients with Mucosal COM, 34 patients had mild conductive hearing loss whereas moderate and profound conductive hearing loss were seen in 2 and 1 patients respectively in contralateral ear. Mixed hearing loss and SNHL of moderate degree were seen in 1 patient each in contralateral ear (Fig. 4).
In patients with Squamosal COM, 28 patients had mild conductive hearing loss whereas moderate conductive hearing loss was seen in 1 patient in contralateral ear. Only one patient had SNHL in contralateral ear of moderate degree (Fig. 5).
In contralateral ear of Mucosal COM, pneumatic pattern of pneumatisation was seen in 69.1% followed by Diploic pattern (30.9%).
In squamosal COM, X-ray mastoid showed pneumatic pattern (64.3%) followed by Diploic pattern (33.9%) in the contralateral ear. Sclerotic pattern was seen in only 1.8% of cases in contralateral ear (Fig. 6).
Discussion
The findings from our study emphasizes the fact that contralateral ear although asymptomatic, is not always normal.
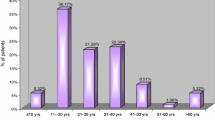
Nigam et al. [5] observed that CSOM was more prevalent among the age group of 20–30 years (41.6%) followed by 12–20 years (27%). In our study, maximum number of patients were from the age group 21–30 years (40.3%) and 11–20 years (28.3%). The range of age distribution was 13–56 years and mean age was 28.02 years. This is in line with the earlier study by Nigam et al. [5].
Out of 188 patients having Mucosal COM, 30.9% had abnormal TM whereas out of 112 patients having Squamosal COM, 48 cases 42.9% had abnormal CLE. Abnormality in CLE was reported to range from 20.1–87.69% [6,7,8,9,10,11,12,13,14,15] in the literature which was more prevalent in patients with squamosal COM [6, 7, 9, 14].
As in earlier studies, our study also reflects that contralateral ear is not always normal. Patients with TM perforation in bilateral ears were not included in our study so abnormalities in CLE are less common as compared to most of the previous literature available. TSP was the most common abnormality detected in CLE in patients with unilateral Mucosal COM whereas retraction pocket was the most common abnormality detected in CLE in patients with unilateral Squamosal COM.
Out of 13 cases of Mucosal COM having retraction pocket in contralateral ear, grade 2 retraction pockets were seen in 7 patients (53.8%) whereas 4 patients (30.8%) had grade 1 retraction pocket. Two patients had grade 3 retraction pockets. Sady Selaimen da Costa et al. [6] found in the NCCOM group mild retractions in 17.9% of the CLE, moderate retractions in 8.6%, and severe retractions in 3.6%. Jambunathan et al. [14] stated that the most common pathology in otoscopy was grade 2 retraction of tympanic membrane which was present in 43.20% patients among which the affected ear had mucosal type COM. There is less prevalence of grade 2 retractions in pars tensa of CLE in this study as compared to our study.
Out of 18 cases of Squamosal COM having retraction pocket in contralateral ear, 11 of them (61.1%) had grade 3 retraction pocket, 4 cases (22.2%) had grade 2 retraction pockets whereas rest 3 had grade 4 retraction pockets. Sady Selaimen da Costa et al. [6] observed that in the CCOM group, those with cholesteatoma in the most affected ear displayed severe retractions in 24.7% of the CLE, mild retractions in 14.1%, and moderate retractions in 11.2%. Jambunathan et al. [14] stated that the most common pathology in otoscopy was grade 2 retraction of tympanic membrane in squamosal COM followed by grade 3 retraction. There is less prevalence of grade 3 retractions in pars flaccida of CLE in this study as compared to our study.
Out of 300 cases, 231 (77.0%) of them had normal hearing in contralateral ear. It was followed by 65 cases (21.6%) with conductive hearing loss. Mixed hearing loss and SNHL were seen in 2 patients each.
In patients with Mucosal COM, 34 patients had mild conductive hearing loss whereas moderate and profound conductive hearing loss were seen in 2 and 1 patients respectively in contralateral ear. Mixed hearing loss and SNHL of moderate degree were seen in 1 patient each in contralateral ear.
In patients with Squamosal COM, 28 patients had mild conductive hearing loss whereas moderate conductive hearing loss was seen in 1 patient in contralateral ear. Only one patient had SNHL in contralateral ear of moderate degree.
Hearing loss in CLE ranged between 30 and 67.6% in various work done previously [9, 10, 13,14,15] When present, Squamosal cases had a slight increased incidence of hearing impairment [15].
In contralateral ear of Mucosal COM, pneumatic pattern of pneumatisation was seen in 69.1% followed by diploic pattern (30.9%).
In squamosal COM, X-Ray mastoids showed pneumatic pattern (64.3%) followed by diploic pattern (33.9%) in the contralateral ear. Sclerotic pattern was seen in only 1.8% of cases in contralateral ear. Reduced cellularity has been well observed in the ears affected with COM both in diseased as well as contralateral ears [8, 9, 11, 12, 14, 15].
Conclusions
In our study we found that contralateral ear was affected in more than 30% cases. The result of this study and previous studies shows that chronic otitis media as a disease is not limited to one ear. The precise and critical evaluation of both ears does not play a role in prognostic evaluation of the patient only, but it can also serve as a guide for early detection of probable evolution of the disease process in CLE in a patient with unilateral chronic otitis media. Patient with chronic otitis media in one ear are very likely to present with the onset of disease in another ear sooner or later. The importance of evaluation of contralateral ear helps in better understanding of the pathogenesis of chronic otitis media, treatment and counselling of the patient. Thus not only ear having complaint, but also CLE must be worked up of the patient.
References
Tong M, Van Hasselt C (2008) Otitis media with effusion in adults. In: Gleeson M (ed) Scott–Brown’s otorhinolaryngology: head and neck surgery, 7th edn. CRC Press, Boca Raton, pp 3388–3394
Chronic suppurative otitis media Burden of Illness and Management Options. WHO (2004)
Sadé J, Berco E (1976) Atelectasis and secretory otitis media. Ann Otol Rhinol Laryngol 85:66–72
Tos M, Stangerup SE, Larsen P (1987) Dynamics of eardrum changes following secretory otitis: a prospective study. Arch Otolaryngol Head Neck Surg 113:380–385
Nigam R, Bairwa RK, Goel A (2019) Study of clinical profile, pathological and functional changes in contralateral ear in patients of chronic suppurative otitis media. Int J Otorhinolaryngol Head Neck Surg 5:1368–1371
Selaimen da Costa S, Rosito LP, Dornelles C, Sperling N (2008) The contralateral ear in chronic otitis media: a series of 500 patients. Arch Otolaryngol Head Neck Surg 134:290–293
Adhikari P, Khanal S, Bhatta R, Sigdel S, Baral D (2009) Status of contralateral ear in patients with chronic otitis media. Internet J Health 10(2)
Damghani MA, Barazin A (2013) Alterations in the contra lateral ear in chronic otitis media. Iran J Otorhinolaryngol 25:99–102
Abushahma K, Ashish KM, Surendra P (2017) Status of contralateral ear in unilateral chronic otits media. Indian J Res 6(8):89–90
Dawood MR (2018) Otoscopic, radiological, and audiological status of the contralateral ears in patients with unilateral chronic suppurative otitis media. Indian J Otol 24:16–19
Joshi S et al (2018) Myth or reality! what the diseased ear was yesterday, the contralateral ear is today. Indian Journal of Basic and Applied Medical Research – Otorhinolaryngology Special Issue June 7(3):101–106
Kumar S, Kumari A (2018) Assessment of otoscopic findings of the contralateral ear in patients with chronic suppurative otitis media. Int J Med Res Prof 4(4):242–244. https://doi.org/10.21276/ijmrp.2018.4.4.056
Qader PK, Said SM (2019) Condition of contralateral ear in chronic otitis media. J Kurdistan Board Med Specialties 5(1)
Jambunathan P, Maan AS, Sharma K (2020) A study of status of contralateral ear in unilateral chronic otitis media in 500 patients. Int J Otorhinolaryngol Head Neck Surg 6:34–39
Thampi M, GuptaA SenK, Jain S (2020) Evaluation of contralateral ear in unilateral chronic otitis media: necessary or not? Indian J Otolaryngol Head Neck Surg. https://doi.org/10.1007/s12070-020-01824-x
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, D.K., Chaudhary, A.K., Jain, R.K. et al. Status of Contralateral Ear in Patients with Unilateral Chronic Otitis Media. Indian J Otolaryngol Head Neck Surg 74 (Suppl 3), 4428–4433 (2022). https://doi.org/10.1007/s12070-022-03086-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03086-1